Abstract
Background
Functional mitral regurgitation (FMR) is a common finding of advanced heart failure with detrimental effects. The prognostic impact of uncorrected FMR prior to left ventricular assist device (LVAD) implantation remains controversial.
Methods
Between 2016 and 2019 77 patients underwent continuous-flow LVAD implantation at our institution. 34 patients showed FMR ≥ 2 (MR-group), whereas 43 patients showed FMR < 2 (Control-group). Data was retrospectively analyzed. Primary composite endpoint comprised freedom from death, stroke, pump-thrombosis, major bleeding and right heart failure (RHF) after 1 year.
Results
Baseline characteristics, including the severity of left and right ventricular dysfunction, and periprocedural results were comparable. The overall survival during a mean follow up of 24.9 months was 55.9% in the MR-group versus 58.1% in the Control-group (p = 0.963), whereas 1-year event-free survival was 35.3% in the MR-group compared to 44.2% in the Control-group (p = 0.404). RHF within the first postoperative year occurred more frequently in the MR-group (35.3% vs. 11.6%; p = 0.017). Furthermore, RV function was significantly reduced in comparison to baseline values in the MR-group. 12 months after surgery, 74% of patients in the MR-group were classified as NYHA III in comparison to 24% of patients in the Control-group (p < 0.001).
Conclusions
Preoperative uncorrected FMR prior to LVAD implantation did not affect overall survival, nevertheless it was associated with an impaired RV function and increased incidence of right heart failure during follow-up. Furthermore, preoperative FMR ≥ 2 was associated with persistent symptoms of heart failure.
Keywords: Heart failure, Left ventricular assist device, Right heart failure, Functional mitral regurgitation, Mitral valve repair, Mitral leaflet tethering
Background
Functional mitral regurgitation (FMR) is a common manifestation of left ventricular (LV) distortion. During the progression of advanced heart failure global and regional LV remodeling results in mitral annulus dilatation along with severe leaflet tethering [1] (Fig. 1). FMR related chronic LV volume overload is associated with an increased diastolic wall stress, an aggravation of LV dilatation and promotes heart failure itself. Furthermore, it is accompanied by an increased rate of adverse cardiac events and mortality, independent of the degree of the underlying LV dysfunction [2].
Fig. 1.
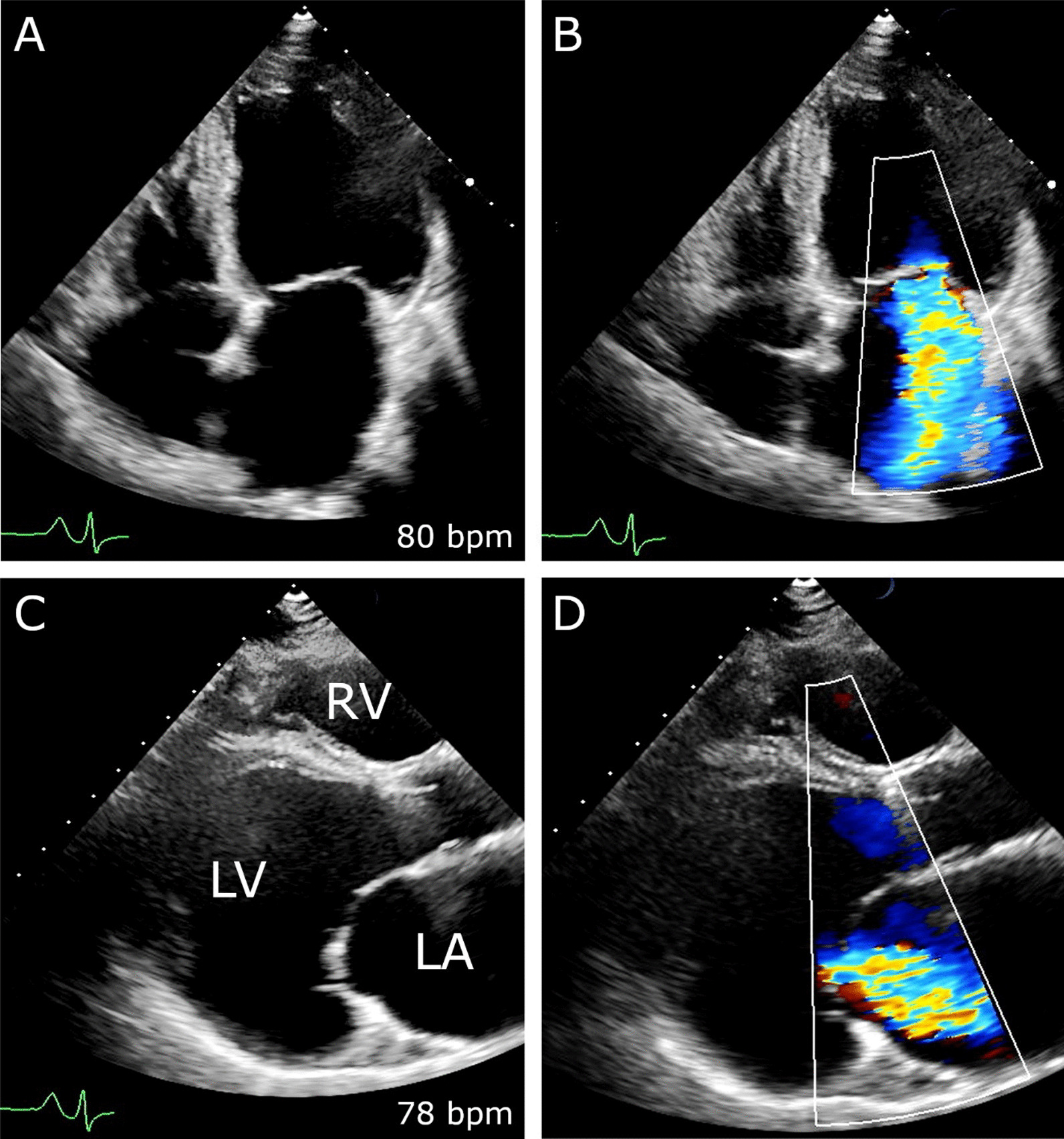
Severe FMR due to left ventricular remodeling. Preoperative transthoracic echocardiogram. Severe functional mitral regurgitation due to advanced LV distortion and mitral leaflet tethering in apical four chamber (A, B) and parasternal long-axis view (C, D)
In addition to optimized guideline-directed medical therapy surgical and percutaneous transcatheter mitral valve repair might be an option for highly-selected heart failure patients with appropriate anatomical features [3–6]. Nevertheless, particularly end-stage heart failure patients with severe FMR due to advanced LV remodeling might not benefit from mitral valve intervention [7].
Continuous flow left ventricular assist device (LVAD) implantation has evolved as an alternative to heart transplantation (HTx) in the treatment of symptomatic advanced heart failure [8–11]. Via LV mechanical unloading long-term LVAD therapy decreases LV dilatation, thereby promoting LV reverse remodeling [12–14] and potentially improving mitral leaflet coaptation [15]. Consequently, preoperative FMR due to advanced LV distortion might be partially resolved via mechanical unloading after LVAD implantation [16, 17]. Furthermore, as uncorrected FMR prior to LVAD implantation does not to affect primary outcome and overall survival after LVAD implantation [18], concomitant routine mitral valve surgery at the time of LVAD implantation is not recommended and currently limited to selected patients [19, 20].
Nevertheless, the prognostic impact of uncorrected FMR prior to LVAD implantation remains controversial [21].
Patients and methods
Patients
Pre-, peri- and postoperative data of 77 consecutive patients who underwent continuous-flow LVAD implantation at our department between 2015 and 2018 was retrospectively collected, using a standardized protocol. Patients were selected for LVAD therapy according to current guidelines due to persistent advanced heart failure as bridge to recovery, bridge to heart HTx or destination therapy [22]. Data were retrospectively analyzed, and all patients were categorized according to preoperative FMR severity. Patients with degenerative MR or concomitant mitral valve procedures were not included. Follow-up at our Heart Failure Clinic was complete. The study was approved by our institutional ethics board and is compliant with the ISHLT ethics statement.
Surgical setup and technique of LVAD implantation
Surgery was performed under general anesthesia in a standard operating room by a dedicated heart failure surgery team, either via full-sternotomy, or minimally invasively using a left-sided thoracotomy approach. Normothermic cardiopulmonary bypass (CBP) was used in all patients. Regardless of the extend of preoperative FMR, no patient underwent any concomitant mitral valve procedure. Concomitant procedures (e.g., aortic valve replacement, tricuspid valve repair) were performed following our institutional standards without major modification during the study period. Implantation of a temporary right ventricular assist device (tRVAD) was done due to unsuccessful weaning from CBP or increased pharmacological inotropic support. Postoperatively phenprocoumon with a target international normalized ratio of 2.0 to 2.5 was administered in addition to acetylsalicylic acid (100 mg per day). All patients underwent a systematic follow-up every 3 to 6 months including a standardized clinical examination, a 6-min walk test (6 MWT), a routine blood test and an echocardiographic assessment at our institution.
Echocardiography
A standardized echocardiographic assessment was performed preoperatively and during follow-up to evaluate left and right ventricular (RV) function and dimensions [23, 24]. The degree of MR was determined either quantitatively or semi-quantitatively [25]. For the purpose of this study, we defined two study-groups, consisting of patients with FMR ≥ 2 (MR-group) and FMR < 2 (Control-group) at baseline.
Endpoints
Primary composite endpoint included freedom from death, stroke, pump-thrombosis, major bleeding and right heart failure (RHF) 1 year after LVAD implantation. Stroke was defined as neurologic deficit and an associated positive cranial computed tomography scan. Pump thrombosis was defined as the combination of an increased energy consumption, an increased calculated forward flow, as well as elevated serum markers of hemolysis. The definition of RHF was adapted from the INTERMACS definition and comprised elevated central venous pressure (CVP) > 16 mmHg or the dilatation of the inferior vena cava leading to clinical manifestations of congestion (e.g., ascites, edema) or increased serum levels of bilirubin [26]. A major bleeding complication was considered whenever urgent transfusion of red blood cells was indicated.
Statistical analysis
Baseline, perioperative and follow-up variables were collected in a dedicated institutional LVAD database. All patients underwent a systematic follow-up every 4 to 6 months including a standardized clinical examination, a 6 MWT, a routine blood and echocardiographic assessment at our institution. Data are presented as absolute numbers and percentages for categorical variables and mean values ± standard deviation for continuous variables, unless stated otherwise. SPSS 24 software was used for all statistical analyzes. Univariate analysis was performed using t-test for numeric variables (i.e., after confirmation of normal distribution) and chi-square-test/Fisher’s exact test for categorical variables. Kaplan–Meier method was used for the composite endpoint, as well as rates of survival and RHF. Univariate comparisons were performed by log-rank test. Results were considered statistically significant if the p value was < 0.05.
Results
Study population and patient characteristics
77 consecutive patients suffering from advanced heart failure underwent continuous-flow LVAD implantation at our institution between 2015 and 2018. According to preoperative echocardiography 34 patients (44.2%) showed moderate to severe FMR (MR-group) (e.g., Fig. 1), whereas 43 patients (55.8%) showed less than moderate FMR (Control-group). Predominantly male patients (84.4%) with a mean age of 54 years were treated (Table 1). Patients in the Control-group suffered significantly more often from an ischemic cardiomyopathy compared to the MR-group (i.e., 28 (65.1%) vs. 11 (32.4%); p = 0.004). Furthermore, the prevalence of arterial hypertension, previous sternotomy and previous coronary artery bypass grafting (CABG) was significantly higher in the Control-group (Table 1). Other comorbidities, including atrial fibrillation, previous stroke, chronic obstructive pulmonary disease (COPD), chronic renal failure and previous hemodialysis were comparable in both study-groups (Table 1). All study patients presented with severe symptoms (i.e., NYHA III/IV) of congestive heart failure and elevated serum levels of natriuretic peptide (i.e., 10,336 ± 8360 pg/ml in the MR-group vs. 9692 ± 8816 pg/ml in the Control-group; p = 0.766) (Table 1). Preoperative serum levels of creatinine, glutamic oxaloacetic transaminase (GOT), glutamic pyruvic transaminase (GPT) and bilirubin as signs of secondary end-organ damage due to advanced heart failure, were comparably elevated in both study-groups (Table 1). Short-term mechanical circulatory support until LVAD implantation was necessary in both study-groups (i.e., 9 (26.5%) MR-group vs. 13 (30.2%); p = 0.717) (Table 1).
Table 1.
Preoperative patient characteristics
| Variables | MR-group (n = 34) | Control-group (n = 43) | p value |
|---|---|---|---|
| Age (years), mean ± SD | 52.0 ± 13.2 | 56.3 ± 10.9 | 0.126 |
| Male, n (%) | 27 (79.4) | 38 (88.4) | 0.282 |
| BMI, kg/m2, mean ± SD | 24.9 ± 4.5 | 26.9 ± 6.3 | 0.115 |
| Ischemic cardiomyopathy, n (%) | 11 (32.4) | 28 (65.1) | 0.004 |
| Non-ischemic dilated cardiomyopathy, n (%) | 23 (67.6) | 15 (34.9) | 0.004 |
| Arterial hypertension, n (%) | 10 (29.4) | 23 (53.5) | 0.034 |
| Diabetes mellitus, n (%) | 11 (32.4) | 14 (32.6) | 0.985 |
| COPD > GOLD II, n (%) | 4 (11.8) | 10 (23.3) | 0.194 |
| Atrial fibrillation, n (%) | 16 (47.1) | 23 (58.1) | 0.102 |
| Previous stroke, n (%) | 4 (11.8) | 5 (11.6) | 0.985 |
| Chronic renal failure, n (%) | 26 (76.5) | 26 (60.5) | 0.136 |
| Previous hemodialysis, n (%) | 5 (14.7) | 6 (14.0) | 0.925 |
| Serum creatinin level (mg/dl), mean ± SD | 1.6 ± 0.6 | 1.7 ± 0.7 | 0.279 |
| Serum NT-proBNP level (pg/dl), mean ± SD | 10,336 ± 8360 | 9692 ± 8816 | 0.766 |
| Destination therapy, n (%) | 12 (35.3) | 23 (53.5) | 0.113 |
| Serum GOT level (U/l), mean ± SD | 73.8 ± 114.7 | 103.5 ± 237.1 | 0.482 |
| Serum GPT level (U/l), mean ± SD | 80.1 ± 142.6 | 93.9 ± 159.2 | 0.691 |
| Serum bilirubin level (mg/dl), mean ± SD | 1.3 ± 0.8 | 1.2 ± 0.8 | 0.547 |
| Previous short-term MCS, n (%) | 9 (26.5) | 13 (30.2) | 0.717 |
| Previous sternotomy, n (%) | 5 (14.7) | 16 (37.2) | 0.028 |
| Previous CABG, n (%) | 3 (8.8) | 11 (25.6) | 0.026 |
BMI body mass index, COPD chronic obstructive pulmonary disease, GOLD Global Initiative for Chronic Obstructive Lung Disease, NYHA New York Heart Association, NT-pro-BNP N-terminal pro-B natriuretic peptide, GOT glutamic oxaloacetic transaminase, GPT glutamic pyruvic transaminase
Baseline systolic LV and RV functions were similar in both study-groups (i.e., LVEF 19.7 ± 6% MR-group vs. 21.0 ± 6% Control-group; p = 0.341; TAPSE 14.9 ± 4 mm MR-group vs. 14.9 ± 5 mm Control-group; p = 0.979) (Table 2). Severe dilatation of the left ventricle and left atrium could be shown in both study-groups (Table 2). Concomitant aortic regurgitation (AR) was comparable in both study-groups, whereas relevant tricuspid regurgitation (TR) was more frequent in the MR-group (i.e., 21 (61.8%) vs. 11 (25.6%); p = 0.001) (Table 2).
Table 2.
Preoperative echocardiographic characteristics
| Variables | MR-group (n = 34) | Control-group (n = 43) | p value |
|---|---|---|---|
| LVEF (%), mean ± SD | 19.7 ± 5.7 | 21 ± 6.4 | 0.341 |
| LVEDD (mm), mean ± SD | 76.0 ± 13.8 | 70.4 ± 8.7 | 0.101 |
| TAPSE (mm), mean ± SD | 14.9 ± 4.3 | 14.9 ± 5.2 | 0.979 |
| LA-volume (ml), mean ± SD | 105.7 ± 32.3 | 95.2 ± 38.0 | 0.397 |
| Tricuspid regurgitation ≥ 3, n (%) | 21 (61.8) | 11 (25.6) | 0.001 |
| Aortic regurgitation ≥ 2, n (%) | 5 (14.7) | 4 (9.3) | 0.464 |
LVEF left ventricular ejection fraction, LVEDD left ventricular end-diastolic diameter, LA-volume left atrial volume, TAPSE tricuspid annular plane systolic excursion
Procedural outcome of LVAD implantation
Predominantly full-sternotomy was used (i.e., 79.2%) as surgical access and patients were mainly treated with the Medtronic HVAD device (95%) (Table 3). Normothermic cardiopulmonary bypass (CBP) was used in all patients. Notably, regardless of the extend of preoperative FMR no patient underwent any concomitant mitral valve procedure. The rate of concomitant aortic valve replacement was comparable in both study-groups (5 (14.7%) MR-group vs. 6 (14.0%) Control-group; p = 0.925), however, tricuspid valve repair was performed more frequently in the MR-group (4 (11.8%) vs. Control-group 1 (2.3%); p = 0.095) (Table 3). Due to unsuccessful weaning from CBP or increased pharmacological inotropic support in addition to echocardiographic signs of RHF, the implantation of a temporary right ventricular assist device (tRVAD) was performed equally in both study-groups (12 (35.3%) in MR-group vs. 9 (20.9%) in Control-group; p = 0.160). The overall duration of the surgery (300 ± 100 min MR-group vs. 333 ± 94 min Control-group; p = 0.155), as well as cardiopulmonary bypass time (155 ± 69 min MR-group vs. 154 ± 62 min Control-group; p = 0.930) were comparable in both study-groups (Table 3). There was no intraprocedural mortality within both study-groups.
Table 3.
Periprocedural outcome
| Variables | MR-group (n = 34) | Control-group (n = 43) | p value |
|---|---|---|---|
| Full-sternotomy, n (%) | 26 (76.5) | 35 (81.4) | 0.597 |
| Medtronic HVAD device, n (%) | 33 (97.1) | 40 (93.0) | 0.428 |
| Implantation of tRVAD, n (%) | 12 (35.3) | 9 (20.9) | 0.160 |
| Additional AVR, n (%) | 5 (14.7) | 6 (14.0) | 0.925 |
| Additional TV repair, n (%) | 4 (11.8) | 1 (2.3) | 0.095 |
| Duration of surgery (min), mean ± SD | 300.5 ± 100.2 | 332.9 ± 93.7 | 0.155 |
| Cardiopulmonary bypass time (min), mean ± SD | 155.6 ± 68.7 | 154.2 ± 61.5 | 0.930 |
tRVAD temporary right ventricular assist device, AVR aortic valve replacement, TV repair tricuspid valve repair
Primary composite study endpoint
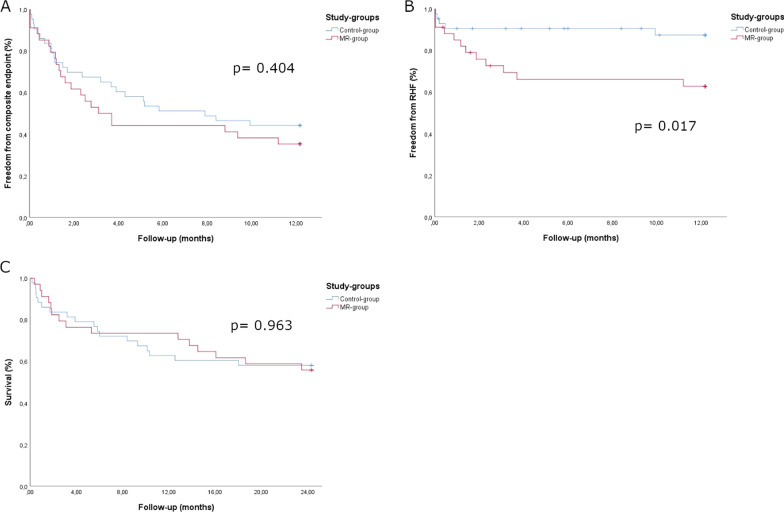
There was no significant difference regarding the primary composite study endpoint between both study-groups. Freedom from death, stroke, pump-thrombosis, major bleeding or RHF within the first year after LVAD implantation occurred in 12 (35.3%) patients in the MR-group versus 19 (44.2%) patients in the Control-group (p = 0.404) (Fig. 2A).
Fig. 2.
Primary study endpoint, RHF and survival. Kaplan–Meier curves: A primary composite outcome of all-cause mortality, stroke, pump-thrombosis, major bleeding and right heart failure (RHF) after 1 year. Secondary outcomes: B right-heart failure within first postoperative year and C all-cause mortality. p values reflecting log-rank test between both study-groups
Overall survival and secondary adverse events
Overall survival during follow-up was 57.1% (55.9% MR-group vs. 58.1% Control-group; p = 0.963) (Fig. 2C). The main cause of death was persisting RHF leading to multi-organ failure. Furthermore, RHF within the first year after LVAD implantation occurred more frequently in the MR-group (35.3% MR-group vs. 11.6% Control-group; p = 0.017) (Fig. 2B). The rate of HTx within the first 2 years after LVAD implantation was comparable between both study-groups (23.5% MR-group vs. 9.3% Control-group; p = 0.123).
Echocardiographic outcome at 1-year postoperatively
1-year after LVAD-implantation LVEDD decreased significantly in both study-groups in comparison to preoperative (baseline) values (from 76 ± 14 mm (baseline) to 66 ± 12 mm (1y-FU), p = 0.019 MR-group; from 70 ± 9 mm (baseline) to 64 ± 10 mm (1y-FU), p = 0.025 Control-group) (Fig. 3A), whereas the extent of LV-dysfunction remained unchanged (Table 4). The prevalence of residual MR ≥ 2 was significantly higher in the MR-group in comparison to the Control-group (8 (34.8%) MR-group vs. 2 (7.4%) Control-group; p = 0.016) (Table 4). 1-year postoperatively, RV-function, measured as tricuspid annular plane systolic excursion (TAPSE), was significantly reduced in the MR-group in comparison to baseline values (TAPSE 14.9 ± 4 mm vs. 11.8 ± 3 mm; p = 0.005), whereas no differences occurred in the Control-group (TAPSE 14.9 ± 5 mm vs. 13.9 ± 3 mm; p = 0.381) (Fig. 3B). Furthermore, RV-function, measured as TAPSE, was significantly lower in the MR-group in comparison to the Control-group, 1 year after LVAD implantation (Table 4).
Fig. 3.
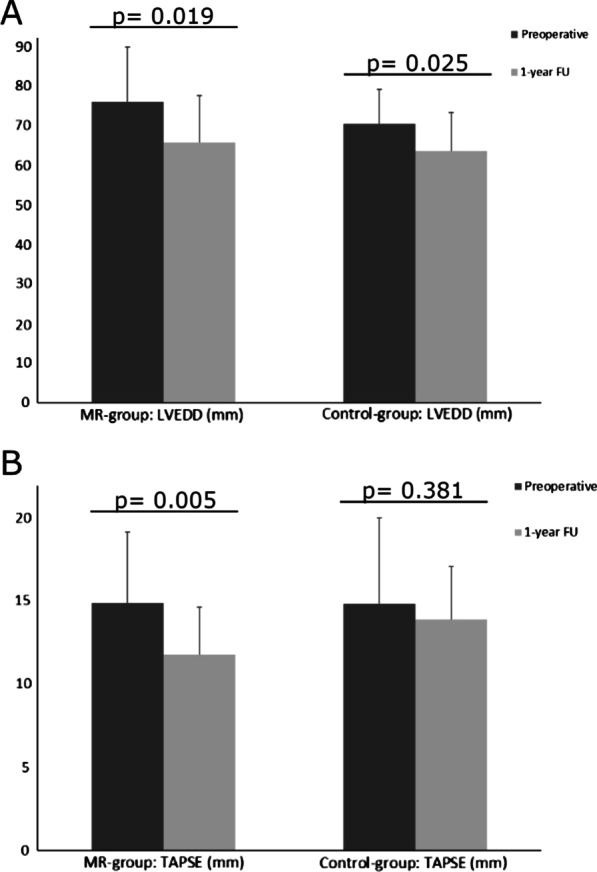
Echocardiographic follow-up. Echocardiographic outcome parameters 1 year after LVAD implantation in comparison to preoperative values. A LVEDD: left ventricular end-diastolic diameter. B TAPSE: tricuspid annular plane systolic excursion
Table 4.
1-year follow-up outcome
| Variables | MR-group (n = 23) | Control-group (n = 27) | p value |
|---|---|---|---|
| LVEF (%), mean ± SD | 20.9 ± 4.8 | 22.5 ± 5.9 | 0.278 |
| LVEDD (mm), mean ± SD | 65.7 ± 11.8 | 63.5 ± 9.7 | 0.568 |
| TAPSE (mm), mean ± SD | 11.8 ± 2.9 | 13.9 ± 3.2 | 0.029 |
| Residual mitral regurgitation ≥ 3, % (n) | 8 (34.8) | 2 (7.4) | 0.016 |
| Tricuspid regurgitation ≥ 3, n (%) | 9 (39.1) | 2 (7.4) | 0.007 |
| NYHA III–IV, n (%) | 17 (73.9) | 6 (24.0) | < 0.001 |
| 6 MWT (meter), mean ± SD | 363 ± 163 | 405 ± 86 | 0.316 |
| Serum NT-proBNP level (pg/dl), mean ± SD | 7297 ± 10,682 | 1988 ± 1590 | 0.024 |
| Serum GOT level (U/l), mean ± SD | 27.3 ± 18.7 | 28.0 ± 19.6 | 0.898 |
| Serum GPT level (U/l), mean ± SD | 30.0 ± 26.2 | 25.3 ± 13.8 | 0.442 |
| Serum bilirubin level (mg/dl), mean ± SD | 0.9 ± 0.6 | 0.8 ± 0.4 | 0.503 |
| Serum creatinin level (mg/dl), mean ± SD | 1.8 ± 0.9 | 1.6 ± 0.4 | 0.490 |
NYHA New York Heart Association, 6 MWT 6-min walk test, NT-pro-BNP N-terminal pro-B natriuretic peptide, GOT glutamic oxaloacetic transaminase, GPT glutamic pyruvic transaminase
Functional outcome at 1-year postoperatively
At 1-year follow-up, a significant improvement in NYHA functional class was found in the whole study-cohort (100% NYHA III/IV preoperatively vs. 46% NYHA III/IV postoperatively (excluded are 25 patients who died and two patients who underwent HTx during the first postoperative year; p < 0.001) (Table 4). Notably, significantly more patients within the MR-group (73.9%) were categorized as NYHA III/IV at 1-year-follow up in comparison to the Control-group (22.2%) (p < 0.001) (Table 4). Accordingly, serum levels of NT-proBNP, which decreased significantly 1-year after LVAD implantation in the Control-group (9692 ± 8816 pg/ml at baseline vs. 1988 ± 1590 pg/ml at 1-year; p < 0.001), remained significantly higher in the MR-group (10,336 ± 8360 pg/ml at baseline vs. 7297 ± 10,682 pg/ml at 1-year; p = 0.262) (p = 0.024) (Table 4).
Whereas serum levels of GOT, GPT and bilirubin decreased significantly within the Control-group, the decline of serum levels of GPT and bilirubin did not reach statistical significance in the MR-group 1 year after LVAD-implantation (Table 4).
Discussion
Due to mitral annulus dilatation along with severe leaflet tethering, FMR is a common feature of advanced LV remodeling during the progression of chronic heart failure, leading to an impaired outcome [1, 2]. Despite mechanical LV unloading followed by reverse cardiac remodeling and improved mitral leaflet coaptation [14–16], uncorrected FMR persists in up to 30% of LVAD recipients [17, 21, 27]. Although, routine concomitant mitral valve surgery during LVAD implantation is not recommended, the prognostic impact of uncorrected FMR prior to LVAD implantation remains controversial.
Study population
As a consequence of advanced LV remodeling, 44.2% of the patients in our study-cohort showed moderate to severe FMR (MR-group) prior to LVAD implantation. Consequentially increased left atrial pressure, secondary pulmonary congestion and an increased RV afterload, may result in the development of functional TR (FTR) [28]. Of note, the prevalence of FTR was increased within the MR-group. Nevertheless, due to its dependence on the patient’s volume status and a missing standardization, the assessment of FTR and its potential consequences remains challenging, particularly in the context of acute cardiogenic shock and the presence of temporary mechanical circulatory support devices. Apart from an increased prevalence of ischemic cardiomyopathy in the Control-group, baseline characteristics including age, gender and relevant comorbidities were comparable between both study-groups. Notably, preoperative symptoms of congestive heart failure (e.g. NYHA class), as well as signs of secondary end-organ damage (e.g. prevalence of renal failure, previous hemodialysis and hepatic congestion) emerged comparably in both study-groups. Furthermore, the magnitude of systolic LV dysfunction and dilatation was comparable in both study-groups. Despite presumably elevated left-sided filling pressures and pulmonary congestion due to FMR [29] in the MR-group, systolic RV function (measured as TAPSE) prior to LVAD implantation was comparable in both study-groups. Nevertheless, the increased prevalence of significant FTR within the MR-group might impact the assessment of RV function as severe pendulous volume caused by atrio-ventricular regurgitation potentially leads to hyperdynamic RV function to maintain sufficient stroke volume [30].
Periprocedural outcome
In accordance with comparable baseline characteristics, periprocedural outcome was similar in both study-groups. Although, tricuspid valve repair was performed more frequently in the MR-group, implantation of a tRVAD due to unsuccessful weaning from CBP, was performed equally in both study-groups. While approximately one third of patients needed short-term MCS prior to LVAD implantation, emphasizing an increased surgical risk of our study patients, there was no procedural mortality within both study-groups.
Primary study endpoint, survival and secondary adverse events
In accordance with previously published data [16, 18], we found no significant difference regarding the primary composite study endpoint (Fig. 2A). Furthermore, overall survival was similar within both study-groups (Fig. 2C). After a mean follow-up of 24.9 months overall survival was 57.1%, whereas the rate of HTx within the first 2 years after LVAD implantation was 15.6% within the whole study-cohort. Of note, a high proportion of patients, who were included in the current analysis had an increased mortality risk, reflected in the high prevalence of preoperative short-term mechanical circulatory support of 28.6%. Additionally, all of those patients suffered from progressive heart failure or ongoing cardiogenic shock and were classified as INTERMACS class I or II. Furthermore, a high proportion of HVAD implantations within the current analysis might have negatively influenced long-term survival, as there is growing evidence of a higher frequency of neurological adverse events and mortality among HVAD recipients as compared to other commercially available durable LVADs [31].
Although we found a comparable RV function prior to LVAD implantation, RHF within the first postoperative year after LVAD implantation occurred more frequently in the MR-group (Fig. 2B). Despite mechanical unloading after LVAD implantation, residual FMR might lead to persisting pulmonary congestion and subsequently increased RV afterload [32]. Additionally, the preoperatively increased rate of significant FTR might emphasize an increased susceptibility for RHF in the MR-group [33], as the evaluation of RV function and the potential risk of RHF after LVAD implantation remains challenging.
Echocardiographic and functional outcome
One year after LVAD implantation mechanical unloading leads to a significant reduction of LV dilatation, in both study-groups (Fig. 3A). Irrespectively of the remarkable LV size reduction, uncorrected moderate to severe FMR prior to LVAD implantation persisted in 35% of patients in the MR-group. In addition to mitral annulus dilatation, advanced LV remodeling leads to apicolateral displacement of both papillary muscles, resulting in severe mitral leaflet tethering. Interestingly, severe uncorrected leaflet tethering leading to relevant FMR, seems to be associated with persisting FMR after LVAD implantation [17]. Therefore, one could speculate, that patients with persisting FMR after LVAD implantation, exhibited aggravated LV remodeling and consecutive leaflet tethering prior to LVAD implantation, despite a comparable extend of LV dilatation.
In accordance with an increased rate of RHF in the MR-group, RV function was significantly reduced 1 year after LVAD implantation in the MR-group, whereas RV function remained unchanged in the Control-group (Fig. 3B). Furthermore, TAPSE, was significantly lower in the MR-group in comparison to the Control-group, 1 year after LVAD implantation (Table 4). Increased RV afterload due to persisting MR after LVAD implantation, presumably promotes the impairment of RV function leading to an increased rate of RHF [21]. Whereas serum markers for hepatic congestion due to RV dysfunction decreased significantly within the Control-group, the decline of serum levels of GPT and bilirubin did not reach statistical significance in the MR-group 1 year after LVAD-implantation (Table 4).
In the treatment of symptomatic advanced heart failure “destination LVAD therapy” evolved as an alternative to HTx. Consequently, the improvement of heart failure symptoms as well as the reduction of adverse cardiac events acquired an increased importance. Herein, we could demonstrate, that 1 year after LVAD implantation a significant improvement in NYHA functional class was found in the whole study-cohort (100% NYHA III/IV preoperatively vs. 46% NYHA III/IV postoperatively; p < 0.001) (Table 4). Notably, significantly more patients within the MR-group (73.9%) were categorized as NYHA III/IV at 1-year-follow up in comparison to the Control-group (22.2%) (p < 0.001) (Table 4). Accordingly, serum levels of NT-proBNP, which decreased 1-year after LVAD implantation in the Control-group remained significantly higher in the MR-group (Table 4). In addition to significantly reduced RV function, FMR prior to LVAD implantation seems to be associated with persisting symptoms of heart failure. Therefore, to further improve long-term patient outcome, concomitant mitral valve surgery in addition to LVAD implantation, especially addressing mitral leaflet tethering [34], might be an option for highly selected heart failure patients with an increased risk of persisting FMR [35] despite LVAD implantation.
Study limitations
We are aware of a limited patient-cohort treated in a single-center. Furthermore, up to now our follow-up period is limited to 2 years. Nevertheless, due to the inclusion of all consecutive LVAD recipients at our institution and the collection of pre-, peri- and postoperative data using a standardized protocol, a potential selection bias is neglectable. Furthermore, comparable baseline characteristics emphasize the homogeneity of our study-cohort.
Conclusion
Despite significant LV remodeling due to mechanical unloading after LVAD implantation, residual FMR persisted in one third of the patients. Preoperative uncorrected FMR ≥ 2 prior to LVAD implantation did not affect overall survival, nevertheless it was associated with an impaired RV function and increased rates of RHF within the first postoperative year. Furthermore, preoperative FMR was associated with persistent symptoms of heart failure and increased levels of natriuretic peptide. Therefore, detailed preoperative echocardiographic assessment regarding FMR characteristics (e.g., extend of leaflet tethering) as well as RV function, including the evaluation of possible concomitant mitral valve surgery, are recommendable to further improve patient outcome.
Acknowledgements
Not applicable.
Abbreviations
- AR
Aortic regurgitation
- CABG
Coronary artery bypass grafting
- CBP
Cardiopulmonary bypass
- FMR
Functional mitral regurgitation
- GDMT
Guideline-directed medical therapy
- GOT
Glutamic oxaloacetic transaminase
- GPT
Glutamic pyruvic transaminase
- LV
Left ventricle
- LVAD
Left ventricular assist device
- LVEDD
Left ventricular end-diastolic diameter
- LVEF
Left ventricular ejection fraction
- MCS
Mechanical circulatory support
- MR
Mitral regurgitation
- NT-pro-BNP
N-terminal pro-B natriuretic peptide
- NYHA
New York Heart Association
- RHF
Right heart failure
- RV
Right ventricle
- TAPSE
Tricuspid annular plane systolic excursion
- TR
Tricuspid regurgitation
- tRVAD
Temporary right ventricular assist device
- 6 MWT
6-Min walk test
Authors' contributions
JP and AMB analyzed and interpreted the patient data and wrote the manuscript. JP, OB and JM were involved in data collection and literature review. LC, BS, MB and HR were involved in reviewing the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used for this study are available from the corresponding authors on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by our institutional ethics board and is compliant with the ISHLT ethics statement.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Meeting presentation ISHLT 41th Annual Meeting 2021, 24–28 April 2021
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Nasser R, Van Assche L, Vorlat A, Vermeulen T, Van Craenenbroeck E, Conraads V, et al. Evolution of functional mitral regurgitation and prognosis in medically managed heart failure patients with reduced ejection fraction. JACC Heart Fail. 2017;5(9):652–659. doi: 10.1016/j.jchf.2017.06.015. [DOI] [PubMed] [Google Scholar]
- 2.Rossi A, Dini FL, Faggiano P, Agricola E, Cicoira M, Frattini S, et al. Independent prognostic value of functional mitral regurgitation in patients with heart failure. A quantitative analysis of 1256 patients with ischaemic and non-ischaemic dilated cardiomyopathy. Heart. 2011;97(20):1675–1680. doi: 10.1136/hrt.2011.225789. [DOI] [PubMed] [Google Scholar]
- 3.Girdauskas E, Pausch J, Harmel E, Gross T, Detter C, Sinning C, et al. Minimally invasive mitral valve repair for functional mitral regurgitation. Eur J Cardiothorac Surg. 2019;55(Supplement_1):I17–I25. doi: 10.1093/ejcts/ezy344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379(24):2307–2318. doi: 10.1056/NEJMoa1806640. [DOI] [PubMed] [Google Scholar]
- 5.Obadia JF, Messika-Zeitoun D, Leurent G, Iung B, Bonnet G, Piriou N, et al. Percutaneous repair or medical treatment for secondary mitral regurgitation. N Engl J Med. 2018;379(24):2297–2306. doi: 10.1056/NEJMoa1805374. [DOI] [PubMed] [Google Scholar]
- 6.Feldman T, Kar S, Rinaldi M, Fail P, Hermiller J, Smalling R, et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol. 2009;54(8):686–694. doi: 10.1016/j.jacc.2009.03.077. [DOI] [PubMed] [Google Scholar]
- 7.Petrus AHJ, Klautz RJM, De Bonis M, Langer F, Schafers HJ, Wakasa S, et al. The optimal treatment strategy for secondary mitral regurgitation: a subject of ongoing debate. Eur J Cardiothorac Surg. 2019;56(4):631–642. doi: 10.1093/ejcts/ezz238. [DOI] [PubMed] [Google Scholar]
- 8.Rose EA, Gelijns AC, Moskowitz AJ, Heitjan DF, Stevenson LW, Dembitsky W, et al. Long-term use of a left ventricular assist device for end-stage heart failure. N Engl J Med. 2001;345(20):1435–1443. doi: 10.1056/NEJMoa012175. [DOI] [PubMed] [Google Scholar]
- 9.Slaughter MS, Rogers JG, Milano CA, Russell SD, Conte JV, Feldman D, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361(23):2241–2251. doi: 10.1056/NEJMoa0909938. [DOI] [PubMed] [Google Scholar]
- 10.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson L, Miller M, et al. Long-term mechanical circulatory support (destination therapy): on track to compete with heart transplantation? J Thorac Cardiovasc Surg. 2012;144(3):584–603. doi: 10.1016/j.jtcvs.2012.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller LW, Pagani FD, Russell SD, John R, Boyle AJ, Aaronson KD, et al. Use of a continuous-flow device in patients awaiting heart transplantation. N Engl J Med. 2007;357(9):885–896. doi: 10.1056/NEJMoa067758. [DOI] [PubMed] [Google Scholar]
- 12.Drakos SG, Mehra MR. Clinical myocardial recovery during long-term mechanical support in advanced heart failure: insights into moving the field forward. J Heart Lung Transplant. 2016;35(4):413–420. doi: 10.1016/j.healun.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Uriel N, Sayer G, Annamalai S, Kapur NK, Burkhoff D. Mechanical unloading in heart failure. J Am Coll Cardiol. 2018;72(5):569–580. doi: 10.1016/j.jacc.2018.05.038. [DOI] [PubMed] [Google Scholar]
- 14.Drakos SG, Terrovitis JV, Anastasiou-Nana MI, Nanas JN. Reverse remodeling during long-term mechanical unloading of the left ventricle. J Mol Cell Cardiol. 2007;43(3):231–242. doi: 10.1016/j.yjmcc.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Morgan JA, Brewer RJ, Nemeh HW, Murthy R, Williams CT, Lanfear DE, et al. Left ventricular reverse remodeling with a continuous flow left ventricular assist device measured by left ventricular end-diastolic dimensions and severity of mitral regurgitation. ASAIO J. 2012;58(6):574–577. doi: 10.1097/MAT.0b013e31826e4267. [DOI] [PubMed] [Google Scholar]
- 16.Goodwin M, Nemeh HW, Borgi J, Paone G, Morgan JA. Resolution of mitral regurgitation with left ventricular assist device support. Ann Thorac Surg. 2017;104(3):811–818. doi: 10.1016/j.athoracsur.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Kitada S, Kato TS, Thomas SS, Conwell SD, Russo C, Di Tullio MR, et al. Pre-operative echocardiographic features associated with persistent mitral regurgitation after left ventricular assist device implantation. J Heart Lung Transplant. 2013;32(9):897–904. doi: 10.1016/j.healun.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stulak JM, Tchantchaleishvili V, Haglund NA, Davis ME, Schirger JA, Cowger JA, et al. Uncorrected pre-operative mitral valve regurgitation is not associated with adverse outcomes after continuous-flow left ventricular assist device implantation. J Heart Lung Transplant. 2015;34(5):718–723. doi: 10.1016/j.healun.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 19.Potapov EV, Antonides C, Crespo-Leiro MG, Combes A, Farber G, Hannan MM, et al. 2019 EACTS Expert Consensus on long-term mechanical circulatory support. Eur J Cardiothorac Surg. 2019;56(2):230–270. doi: 10.1093/ejcts/ezz098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirklin JK, Pagani FD, Goldstein DJ, John R, Rogers JG, et al. American Association for Thoracic Surgery/International Society for Heart and Lung Transplantation guidelines on selected topics in mechanical circulatory support. J Heart Lung Transplant. 2020;39(3):187–219. doi: 10.1016/j.healun.2020.01.1329. [DOI] [PubMed] [Google Scholar]
- 21.Kassis H, Cherukuri K, Agarwal R, Kanwar M, Elapavaluru S, Sokos GG, et al. Significance of residual mitral regurgitation after continuous flow left ventricular assist device implantation. JACC Heart Fail. 2017;5(2):81–88. doi: 10.1016/j.jchf.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 23.Shah NR, Cevik C, Hernandez A, Gregoric ID, Frazier OH, Stainback RF. Transthoracic echocardiography of the HeartWare left ventricular assist device. J Card Fail. 2012;18(9):745–748. doi: 10.1016/j.cardfail.2012.06.529. [DOI] [PubMed] [Google Scholar]
- 24.Estep JD, Stainback RF, Little SH, Torre G, Zoghbi WA. The role of echocardiography and other imaging modalities in patients with left ventricular assist devices. JACC Cardiovasc Imaging. 2010;3(10):1049–1064. doi: 10.1016/j.jcmg.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 25.Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2003;16(7):777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 26.Wagner T, Bernhardt AM, Magnussen C, Reichenspurner H, Blankenberg S, Grahn H. Right heart failure before LVAD implantation predicts right heart failure after LVAD implantation—is it that easy? J Cardiothorac Surg. 2020;15(1):113. doi: 10.1186/s13019-020-01150-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robertson JO, Naftel DC, Myers SL, Tedford RJ, Joseph SM, Kirklin JK, et al. Concomitant mitral valve procedures in patients undergoing implantation of continuous-flow left ventricular assist devices: an INTERMACS database analysis. J Heart Lung Transplant. 2018;37(1):79–88. doi: 10.1016/j.healun.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Shiran A, Sagie A. Tricuspid regurgitation in mitral valve disease incidence, prognostic implications, mechanism, and management. J Am Coll Cardiol. 2009;53(5):401–408. doi: 10.1016/j.jacc.2008.09.048. [DOI] [PubMed] [Google Scholar]
- 29.Patel H, Desai M, Tuzcu EM, Griffin B, Kapadia S. Pulmonary hypertension in mitral regurgitation. J Am Heart Assoc. 2014;3(4):e000748. doi: 10.1161/JAHA.113.000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider M, Dannenberg V, Konig A, Geller W, Binder T, Hengstenberg C, et al. Prognostic value of echocardiographic right ventricular function parameters in the presence of severe tricuspid regurgitation. J Clin Med. 2021;10(11):2266. doi: 10.3390/jcm10112266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Numan L, Ramjankhan FZ, Oberski DL, Oerlemans M, Aarts E, Gianoli M, et al. Propensity score-based analysis of long-term outcome of patients on HeartWare and HeartMate 3 left ventricular assist device support. ESC Heart Fail. 2021;8(2):1596–1603. doi: 10.1002/ehf2.13267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tang PC, Haft JW, Romano MA, Bitar A, Hasan R, Palardy M, et al. Right ventricular function and residual mitral regurgitation after left ventricular assist device implantation determines the incidence of right heart failure. J Thorac Cardiovasc Surg. 2020;159(3):897–905.e4. doi: 10.1016/j.jtcvs.2019.03.089. [DOI] [PubMed] [Google Scholar]
- 33.Agricola E, Stella S, Gullace M, Ingallina G, D'Amato R, Slavich M, et al. Impact of functional tricuspid regurgitation on heart failure and death in patients with functional mitral regurgitation and left ventricular dysfunction. Eur J Heart Fail. 2012;14(8):902–908. doi: 10.1093/eurjhf/hfs063. [DOI] [PubMed] [Google Scholar]
- 34.Pausch J, Harmel E, Sinning C, Reichenspurner H, Girdauskas E. Standardized subannular repair for type IIIb functional mitral regurgitation in a minimally invasive mitral valve surgery settingdagger. Eur J Cardiothorac Surg. 2019;56(5):968–975. doi: 10.1093/ejcts/ezz114. [DOI] [PubMed] [Google Scholar]
- 35.Pawale A, Itagaki S, Parikh A, Pinney SP, Adams DH, Anyanwu AC. Mitral valve repair for severe mitral valve regurgitation during left ventricular assist device implantation. J Thorac Cardiovasc Surg. 2019;157(5):1841–8.e1. doi: 10.1016/j.jtcvs.2018.12.071. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used for this study are available from the corresponding authors on reasonable request.