Abstract
Recent studies have investigated dietary patterns to assess the overall dietary habits of specific populations. However, limited epidemiological research has been conducted to explore the unique dietary intakes in low and middle-income countries. This study aims to examine the dietary patterns of Filipino adults and their association with sociodemographic and lifestyle factors. A total of 10,025 adults (≥20 years old) who participated in the 2013 Philippine National Nutrition Survey were included in the analysis. Dietary patterns were derived using factor analysis of 18 food groups from the dietary survey component. Six dietary patterns were identified, namely (1) rice; (2) cereal, milk, sugar, and oil; (3) fruits and miscellaneous food; (4) fish; (5) vegetables and corn; and (6) meat and beverage. Generalized ordered logistic regression analysis indicated that the dietary patterns were associated with different factors, specifically sex, age, educational attainment, marital status, employment status, household size, wealth quintile, smoking status, alcohol consumption, and physical activity. Our findings showed distinct dietary patterns among Filipino adults that were influenced by various sociodemographic and lifestyle parameters. The results of this study have valuable public health implications and the dietary patterns generated can further be used to analyze the link between diet and health outcomes.
Keywords: dietary patterns, factor analysis, adults, Philippines
1. Introduction
Dietary risk is an important driver in most deaths and disabilities due to non-communicable diseases. It pertains to the “aggregated effect of diet quality components consisting of low whole grains, fruits, fiber, legumes, nuts and seeds, omega-3 fatty acids, polyunsaturated fatty acids, vegetables, milk, and calcium; and high sodium, trans fat, red or processed meat, and sugar-sweetened beverages” [1]. Globally, an estimated 7.94 million deaths among adults ≥25 years old were attributable to dietary risks in 2019. It also accounts for more than 10% of disability-adjusted life years in many Asian countries, including the Philippines [1].
Investigating patterns of dietary intake is an alternative approach to determine the complex interaction among food components [2]. Dietary patterns may be generated based on prior knowledge of diets known to be healthy (a priori method) or through the application of statistical techniques (a posteriori method). The most common methodologies employed in the latter approach are factor analysis and principal component analysis [3,4,5].
Numerous research studies on a posteriori-derived dietary patterns of adults have been conducted in Asia [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. However, the literature mostly focuses on diet–disease relationships. To the best of our knowledge, only one study on food patterns and non-communicable disease risk factors was implemented in the Philippines [6]. Therefore, it is critical to advance research on dietary patterns to improve nutrition programs in low and middle-income countries as well as in specific vulnerable groups. Hence, this study was undertaken to identify the dietary patterns among Filipino adults using a nationwide dataset from the 2013 National Nutrition Survey. We also examined the association between dietary patterns and sociodemographic and lifestyle factors.
2. Materials and Methods
2.1. Study Population
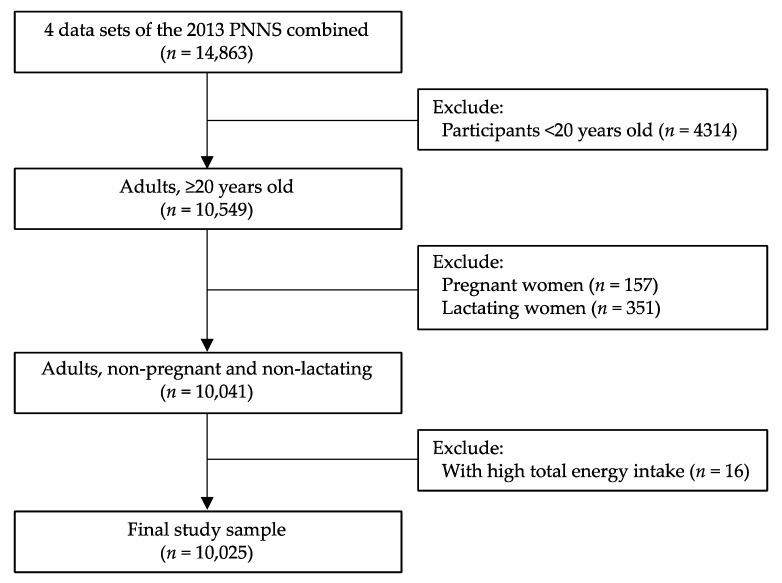
We analyzed data from the Philippine National Nutrition Survey (PNNS) carried out by the Food and Nutrition Research Institute, Department of Science and Technology (FNRI-DOST), in 2013 [28]. The PNNS used a stratified multistage sampling design [29,30]. The study samples were selected from participants aged 20 years or older with complete identification data in the four survey components, i.e., dietary, clinical, socioeconomic individual, and socioeconomic household. Pregnant women and lactating mothers were excluded. Participants with high total energy intake or those with greater than 5 SD of the mean energy intake were further excluded, as applied in past studies [31]. A total of 10,025 adults were eligible for the analysis (Figure 1).
Figure 1.
Study participant selection.
2.2. Dietary Intake Assessment
Dietary intake was assessed with the 24 h food recall method on two non-consecutive days in the 2013 PNNS. Trained registered nutritionist-dietitians interviewed the participants on their food and beverage consumption from the previous day, starting from the time they woke up until bedtime, using structured questionnaires. The food items recalled were estimated utilizing household measurements or through food sample weighing. Calibrated kitchen utensils (spoons, cups, and plates), rulers, and a photo catalog of foods were shown to the participants as visual aids. Successively, the weights of foods were converted to as purchased values using the list of common foods compiled by the FNRI-DOST. Energy and nutrient intakes were calculated using the Philippine Food Composition Table. The dietary data were aggregated into food groups based on the major functions and state of food [30].
2.3. Dietary Pattern Analysis
Dietary patterns were identified using the factor analysis (principal axis factoring procedure in R software) of 18 non-overlapping food groups (Table 1). As suggested in published studies, we excluded the food groups consumed by less than 10% of the population to avoid too many zero values in the data that may lead to extraneous results [32,33,34]. The Bartlett’s test of sphericity (p < 0.000) and Kaiser–Meyer–Olkin measure of sampling adequacy (>0.50) were also evaluated prior to factor analysis to verify data suitability. In the identification of the number of factors to be retained, components with an eigenvalue >1.0, the scree plot results, and factor interpretability were considered (Supplementary Table S1 and Supplementary Figure S1). The factors extracted were rotated using varimax rotation to achieve a simpler structure [35]. Food groups with factor loading values of ≥|0.25| were regarded as significantly contributing to a pattern [6,36]. A six-factor solution was finally selected considering to the aforementioned empirical criteria in conjunction with the substantive meaning of the factor loadings.
Table 1.
Food groups used in the dietary pattern analysis 1.
| Food Groups | Food Items Included |
|---|---|
| Rice and rice products | Rice and other rice products, such as rice noodles and rice cakes |
| Corn and corn products | Milled corn, corn on a cob, and other corn products like cornstarch, corn pudding, popcorn, and corn chips |
| Other cereal products |
Pandesal, bread, cookies/biscuits, cakes/pastries, noodles, flour, and others |
| Starchy roots and tubers | Sweet potatoes and products, potatoes and products, cassava and products, and other roots and tubers such as yam, taro, and arrowroot |
| Sugar and syrups | Sugars, jams, candies, honey, sweetened soda, sherbet, ice drop, ice candy, sugary foods like chocolates, and others |
| Dried beans, nuts, and seeds | Mungbean and products, soybeans and products, nuts and products, and other dried beans/seeds and products like almond, peas, sesame seed, green peas, tofu, and others |
| Green leafy and yellow vegetables | Green leafy vegetables, squash fruit, carrot, and other yellow vegetables |
| Other vegetables | Eggplant, string beans, bitter gourd, other wild vegetables, and other canned/processed vegetables |
| Fruits | Mango, citrus fruits, strawberry, guava, banana, watermelon, melon, jackfruit, pineapple, young coconut, and others |
| Fish and fish products | Fresh fish, dried fish, processed fish, crustaceans, and mollusks |
| Meat and meat products | Fresh meat, organ meat, and processed meat |
| Poultry | Chicken and other fowls like duck, goose, pigeon, turkey |
| Eggs | Hen’s egg, duck’s egg, and other eggs like quail egg and turkey egg |
| Milk and milk products | Fresh whole milk, evaporated milk, recombined milk, powdered milk, condensed milk, cheese, and other milk products like ice cream, yogurt, and cultured milk |
| Fats and oils | Cooking oil, coconut meat, coconut cream, pork drippings and lard, butter, margarine, peanut butter, and others |
| Beverages | Coffee, tea, alcoholic beverages, chocolate-based beverages, fruit-flavored drink, and others |
| Condiments and spices | Salt, vinegar, catsup, and other seasonings |
| Other miscellaneous food | Lemongrass, bay leaves, oregano, turmeric, food coloring, and others |
1 The food groups and food items were pre-identified in the 2013 Philippine National Nutrition Survey.
Factor scores were then estimated for each participant using the regression method. Moreover, because of skewness, the factor scores were divided into tertile intervals to categorize the participant’s adherence to the patterns. The upper tertile (T3) denoted high adherence to a specific dietary pattern and the bottom tertile (T1) denoted low adherence. Labeling of the dietary patterns was carried out according to data interpretation and previous literature. Additionally, a sensitivity analysis was performed to test the stability of the generated factor solution using principal component analysis (PCA). PCA was conducted for the whole sample (dudi.pca function in R software). We compared the number of components to be retained based on eigenvalues, the scree plot analysis, and the variance explained, in which it was consistent (Supplementary Table S2 and Supplementary Figure S2).
2.4. Sociodemographic and Lifestyle Factors
The sociodemographic characteristics of the participants included sex (male or female), age (20–39, 40–59, and ≥60 years), education (highest level completed), marital status (single, married/with partner, and others), employment (employed or unemployed), household size (1–3, 4–6, and ≥7), and wealth quintile (poorest, poor, middle, rich, and richest). Household size was created from the socioeconomic datasets [30]. Wealth status was derived using the PCA of household assets, household characteristics, access to utilities, and infrastructure variables. The scores from the analysis were equally divided into five groups to define the wealth quintile as poorest, poor, middle, rich, and richest [30].
The lifestyle factors were comprised of smoking (current smoker or not), alcohol consumption (current drinker or not), and physical activity (low or high). Current smoking was characterized as either: (a) smoking at least one cigarette per day or on a regular/occasional basis, or (b) smoking at least weekly or less often than weekly [30,37]. Current alcohol drinkers referred to the consumption of any alcoholic beverage during the survey period [30,38]. An individual not engaged in (a) 3 or more days of vigorous-intensity activity of at least 20 min daily, or (b) 5 or more days of moderate-intensity activity or walking for at least 30 min per day was classified as having low physical activity [30,37]. All the sociodemographic and lifestyle information were obtained through face-to-face interviews [30].
2.5. Statistical Analysis
Descriptive statistics were generated for the sociodemographic and lifestyle characteristics of the participants. Data are presented as weighted percentages and 95% confidence intervals. To assess the association between tertiles of dietary pattern scores and sociodemographic and lifestyle factors, we used the generalized ordered logistic regression analysis. The Brant test was utilized for proportionality assumptions and indicated that the parallel lines assumption was violated for eight variables. Explanatory variables included in the generalized ordered logistic regression model were sex, age, educational attainment, marital status, employment status, household size, wealth quintile, smoking, alcohol consumption, and physical activity. Sampling weights were incorporated in the regression analysis to account for the complex survey sampling design. The significance level was set at p < 0.05. All the data analyses were done in R software version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
3. Results
3.1. Characteristics of Study Participants
The descriptive characteristics of the participants are shown in Table 2. A total of 10,025 adults (4976 men and 5049 non-pregnant and non-lactating women) were included in this study. The sample was predominantly of young adults (47.5%), those who finished high school (37.8%), married individuals (65.5%), employed workers (60.1%), and those who belonged to 4–6 membered families (46.2%). Approximately 23% resided in the richest households or the last wealth quintile. In terms of lifestyle factors, 27.0% were smokers, 51.6% were alcohol drinkers, and 44.7% had low physical activity.
Table 2.
Characteristics of the participants by sex (n = 10,025).
| Variables 1 | % | 95% CI |
|---|---|---|
| Sex | ||
| Male | 49.5 | 48.3, 50.6 |
| Female | 50.5 | 49.4, 51.7 |
| Age group | ||
| 20–39 years | 47.5 | 46.0, 49.0 |
| 40–59 years | 37.6 | 36.3, 39.0 |
| ≥60 years | 14.9 | 13.9, 15.9 |
| Educational attainment | ||
| Elementary and lower | 30.8 | 28.6, 33.0 |
| High school | 37.8 | 36.1, 39.6 |
| College and higher | 31.4 | 29.2, 33.6 |
| Marital status | ||
| Single | 24.5 | 22.9, 26.1 |
| Married | 65.5 | 63.8, 67.2 |
| Others | 10.0 | 9.2, 10.9 |
| Employment status | ||
| Employed | 60.1 | 58.6, 61.5 |
| Unemployed | 39.9 | 38.5, 41.4 |
| Household size | ||
| 1–3 | 31.5 | 29.3, 33.9 |
| 4–6 | 46.2 | 43.4, 49.1 |
| ≥7 | 22.2 | 19.8, 24.8 |
| Wealth quintile | ||
| Poorest | 17.1 | 14.9, 19.7 |
| Poor | 18.6 | 16.6, 20.7 |
| Middle | 20.5 | 18.5, 22.7 |
| Rich | 20.7 | 18.7, 22.9 |
| Richest | 23.1 | 20.5, 26.0 |
| Current smoker | ||
| Yes | 27.0 | 25.5, 28.5 |
| No | 73.0 | 71.5, 74.5 |
| Current alcohol drinker | ||
| Yes | 51.6 | 49.6, 53.7 |
| No | 48.4 | 46.3, 50.4 |
| Physical activity | ||
| Low | 44.7 | 42.0, 47.3 |
| High | 55.3 | 52.7, 58.0 |
Table displays weighted percentages. 1 Variables with missing observations: educational attainment (n = 53), smoking and drinking status (n = 581), and physical activity classification (n = 701).
3.2. Dietary Patterns and Their Correlates
We identified six dietary patterns through factor analysis (Table 3). Factor 1, named the rice pattern, was characterized by positive loading in the rice and rice products food group, and negative loading in the corn and corn products food group. Factor 2 or the cereal, milk, sugar, and oil pattern was composed of other cereal products, sugar and syrups, milk and milk products, and fats and oils. Factor 3, labeled as the fruits and miscellaneous food pattern, was comprised of fruits and other miscellaneous foods. Factor 4, referred to as the fish pattern, had high loading in the fish and fish products food group. Factor 5 or the vegetables and corn pattern consisted of green leafy and yellow vegetables, other vegetables, and corn and corn products. Factor 6, called the meat and beverage pattern, was constituted of meat and meat products and beverages. Overall, these six dietary patterns explained 21.7% of the variance in the food intake (5.8%, 3.7%, 3.4%, 3.5%, 2.6%, and 2.7% for factors 1–6, respectively).
Table 3.
Factor loadings for the six identified dietary patterns.
| Food Groups | Dietary Patterns 1 | |||||
|---|---|---|---|---|---|---|
| Rice | Cereal, Milk, Sugar, and Oil | Fruits and Miscellaneous Food | Fish | Vegetables and Corn | Meat and Beverage | |
| Rice and rice products | 0.936 | −0.009 | −0.001 | 0.142 | 0.064 | 0.069 |
| Corn and corn products | −0.331 | −0.099 | −0.045 | 0.046 | 0.294 | 0.004 |
| Other cereal products | −0.024 | 0.475 | −0.005 | −0.040 | −0.071 | 0.092 |
| Starchy roots and tubers | −0.046 | −0.003 | 0.037 | 0.007 | 0.145 | 0.017 |
| Sugar and syrups | 0.049 | 0.327 | 0.029 | 0.004 | −0.011 | 0.198 |
| Dried beans, nuts, and seeds | 0.051 | 0.081 | −0.027 | −0.070 | 0.049 | 0.023 |
| Green leafy and yellow vegetables | 0.007 | −0.105 | 0.003 | −0.002 | 0.491 | −0.073 |
| Other vegetables | 0.119 | 0.038 | 0.042 | −0.118 | 0.295 | −0.049 |
| Fruits | −0.007 | 0.077 | 0.570 | 0.023 | 0.065 | 0.000 |
| Fish and fish products | 0.113 | −0.031 | 0.018 | 0.741 | −0.054 | −0.050 |
| Meat and meat products | 0.072 | 0.205 | 0.016 | −0.133 | −0.073 | 0.525 |
| Poultry | 0.077 | 0.208 | 0.028 | −0.079 | −0.038 | 0.153 |
| Eggs | 0.103 | 0.185 | 0.026 | −0.088 | −0.042 | 0.016 |
| Milk and milk products | −0.055 | 0.281 | 0.089 | −0.008 | −0.003 | 0.057 |
| Fats and oils | 0.028 | 0.266 | 0.024 | 0.024 | 0.005 | 0.003 |
| Beverages | −0.009 | 0.054 | −0.008 | 0.018 | 0.004 | 0.312 |
| Condiments and spices | −0.039 | 0.173 | −0.007 | 0.109 | −0.024 | 0.145 |
| Other miscellaneous | 0.030 | 0.058 | 0.514 | −0.001 | 0.050 | 0.004 |
| Proportion variance, % | 5.8 | 3.7 | 3.4 | 3.5 | 2.6 | 2.7 |
| Cumulative variance, % | 5.8 | 9.5 | 12.9 | 16.4 | 19.0 | 21.7 |
1 Dietary patterns are labeled based on the factor loadings with the absolute value of 0.25 or greater. Bold values represent food groups kept in their related dietary pattern.
The results of the generalized ordered logistic regression analysis revealed that the dietary patterns were associated with different sociodemographic and lifestyle factors (Table 4). Males, young adults (20–39 years old), those who were married, those who were living in 4–6 membered households, and adults engaged in high physical activity were more likely to be in the low or medium tertiles of the rice pattern (the first pattern). Furthermore, the odds of adhering to this pattern were found to be significant among individuals with elementary or high school levels of education, unemployed, from the poorest or middle-quintile households, and who were not current smokers. Regarding the cereal, milk, sugar, and oil pattern, which is the second pattern, adults who attained high school and college education or higher, who were employed, who were current alcohol drinkers, and with low physical activity had higher odds of following the pattern. The likelihood of adhering to this pattern increased with the improvement in wealth status. The third dietary pattern or the fruits and miscellaneous food pattern was favored by females, middle-aged (40–59 years old) and older adults (≥60 years old), those who finished college or higher education, and those dwelling in small-sized (1–3 members) households, and the rich or richest-quintile households. Similarly, adults with high school education and non-current smokers had low adherence to this pattern. The odds of adhering to the fourth pattern (the fish pattern) were higher among males and married adults. Males, married individuals, non-current smokers, and adults with high physical activity were more likely to follow the fifth dietary pattern or the vegetables and corn pattern. In addition, this pattern was commonly observed by those belonging to the poorest households, with a significant dose–response relationship. Finally, for the sixth pattern, the meat and beverage pattern, males, adults aged 20–39 years, those with high school and college education attainment, employed workers, those from the richest households or the wealthiest quintile, current smokers, and current alcohol drinkers had a higher likelihood to have low or medium adherence.
Table 4.
Sociodemographic and lifestyle factors associated with dietary patterns analyzed by generalized ordered logistic regression 1.
| Variables | Rice Pattern | Cereal, Milk, Sugar, and Oil Pattern | Fruits and Miscellaneous Food Pattern | Fish Pattern | Vegetables and Corn Pattern | Meat and Beverage Pattern | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T2 and T3 vs. T1 | T3 vs. T1 or T2 | T2 and T3 vs. T1 | T3 vs. T1 or T2 | T2 and T3 vs. T1 | T3 vs. T1 or T2 | T2 and T3 vs. T1 | T3 vs. T1 or T2 | T2 and T3 vs. T1 | T3 vs. T1 or T2 | T2 and T3 vs. T1 | T3 vs. T1 or T2 | |
| Sex (ref. = male) | ||||||||||||
| Female |
0.18
(0.16, 0.21) |
0.29
(0.25, 0.33) |
0.96 (0.85, 1.09) |
1.18
(1.05, 1.33) |
1.35
(1.19, 1.53) |
1.83
(1.59, 2.11) |
0.64
(0.57, 0.72) |
0.76
(0.67, 0.86) |
0.63
(0.56, 0.70) |
0. 60
(0.53, 0.67) |
0.73
(0.64, 0.82) |
0.82
(0.72, 0.93) |
| Age group (ref. = 20–39 years) | ||||||||||||
| 40–59 years |
0.75
(0.67, 0.85) |
0.80
(0.71, 0.92) |
0.84
(0.74, 0.96) |
0.87
(0.76, 1.00) |
1.20
(1.07, 1.36) |
1.15
(1.02, 1.31) |
1.04 (0.93, 1.17) |
1.10 (0.97, 1.24) |
1.20
(1.06, 1.36) |
1.07 (0.95, 1.20) |
0.75
(0.66, 0.86) |
0.78
(0.68, 0.89) |
| ≥60 years |
0.36
(0.30, 0.43) |
0.45
(0.38, 0.54) |
0.81
(0.67, 0.97) |
0.87 (0.72, 1.04) |
1.65
(1.40, 1.94) |
1.88
(1.58, 2.25) |
1.04 (0.88, 1.22) |
1.16 (0.97, 1.39) |
1.05 (0.88, 1.26) |
0.95 (0.80, 1.13) |
0.51
(0.42, 0.61) |
0.58
(0.48, 0.70) |
| Educational attainment (ref. = ≤ elementary) | ||||||||||||
| High school | 1.07 (0.94, 1.21) |
1.29
(1.12, 1.48) |
1.77
(1.51, 2.07) |
1.73
(1.52, 1.97) |
1.29
(1.13, 1.47) |
1.03 (0.89, 1.20) |
0.90 (0.79, 1.03) |
0.91 (0.79, 1.05) |
0.94 (0.82, 1.07) |
0.97 (0.85, 1.10) |
1.47
(1.28, 1.68) |
1.28
(1.13, 1.46) |
| ≥College |
0.83
(0.70, 0.97) |
0.93 (0.76, 1.13) |
2.52
(2.05, 3.09) |
2.37
(1.94, 2.90) |
1.58
(1.33, 1.89) |
1.22
(1.04, 1.44) |
0.92 (0.77, 1.09) |
0.85
(0.72, 0.99) |
0.95 (0.81, 1.12) |
0.89 (0.74, 1.08) |
2.01
(1.70, 2.38) |
1.69
(1.42, 2.02) |
| Marital status (ref. = single) | ||||||||||||
| Married |
1.21
(1.05, 1.38) |
1.23
(1.06, 1.43) |
0.95 (0.82, 1.09) |
0.92 (0.79, 1.07) |
1.08 (0.94, 1.23) |
1.01 (0.88, 1.17) |
1.30
(1.13, 1.49) |
1.36
(1.18, 1.57) |
1.19
(1.03, 1.38) |
1.19
(1.04, 1.35) |
0.89 (0.77, 1.03) |
0.96 (0.81, 1.13) |
| Others | 0.84 (0.65, 1.07) |
0.88 (0.72, 1.09) |
1.03 (0.83, 1.28) |
1.02 (0.82, 1.26) |
0.90 (0.73, 1.10) |
0.93 (0.75, 1.15) |
1.07 (0.87, 1.33) |
1.03 (0.84, 1.26) |
0.89 (0.71, 1.11) |
0.82 (0.65, 1.03) |
0.86 (0.68, 1.08) |
0.90 (0.73, 1.12) |
| Employment status (ref. = employed) | ||||||||||||
| Unemployed |
1.15
(1.02, 1.29) |
1.08 (0.97, 1.20) |
0.87
(0.78, 0.97) |
0.81
(0.72, 0.92) |
0.94 (0.83, 1.05) |
1.08 (0.95, 1.24) |
0.95 (0.85, 1.06) |
1.02 (0.91, 1.13) |
0.98 (0.88, 1.10) |
0.90 (0.80, 1.00) |
0.71
(0.63, 0.80) |
0.74
(0.67, 0.83) |
| Household size (ref. = 1–3) | ||||||||||||
| 4–6 |
1.14
(1.01, 1.30) |
1.18
(1.04, 1.36) |
0.92 (0.80, 1.06) |
0.96 (0.83, 1.11) |
0.86
(0.75, 0.98) |
0.87
(0.77, 0.99) |
1.09 (0.95, 1.25) |
1.03 (0.90, 1.18) |
0.98 (0.86, 1.12) |
0.98 (0.86, 1.13) |
0.98 (0.84, 1.14) |
0.92 (0.80, 1.06) |
| ≥7 | 0.96 (0.81, 1.14) |
0.99 (0.83, 1.19) |
0.99 (0.82, 1.20) |
0.92 (0.77, 1.10) |
0.85 (0.71, 1.01) |
0.92 (0.78, 1.09) |
0.96 (0.80, 1.14) |
0.93 (0.78, 1.11) |
1.00 (0.84, 1.21) |
1.00 (0.84, 1.20) |
0.92 (0.77, 1.11) |
1.02 (0.85, 1.21) |
| Wealth quintile (ref. = poorest) | ||||||||||||
| Poor | 0.98 (0.82, 1.18) |
1.24 (0.99, 1.54) |
1.26 (1.00, 1.59) |
1.47
(1.24, 1.75) |
1.09 (0.89, 1.32) |
1.05 (0.88, 1.26) |
0.99 (0.81, 1.21) |
1.03 (0.84, 1.27) |
0.77
(0.64, 0.94) |
0.90 (0.73, 1.12) |
1.39
(1.12, 1.72) |
1.22
(1.01, 1.46) |
| Middle | 1.06 (0.87, 1.29) |
1.40
(1.12, 1.77) |
1.84
(1.44, 2.34) |
2.48
(2.06, 3.00) |
1.21 (0.98, 1.50) |
1.16 (0.96, 1.39) |
0.99 (0.81, 1.21) |
1.02 (0.83, 1.26) |
0.53
(0.43, 0.66) |
0.76
(0.61, 0.94) |
1.72
(1.37, 2.16) |
1.62
(1.32, 1.99) |
| Rich | 0.88 (0.72, 1.08) |
1.18 (0.93, 1.49) |
2.68
(2.08, 3.45) |
3.66
(2.92, 4.59) |
1.68
(1.37, 2.05) |
1.55
(1.27, 1.89) |
0.94 (0.75, 1.17) |
0.92 (0.75, 1.13) |
0.45
(0.37, 0.56) |
0.71
(0.57, 0.90) |
3.30
(2.61, 4.18) |
3.19
(2.57, 3.96) |
| Richest |
0.62
(0.49, 0.79) |
0.78 (0.60, 1.03) |
3.71
(2.83, 4.85) |
5.63
(4.35, 7.30) |
2.21
(1.78, 2.74) |
1.87
(1.50, 2.33) |
0.90 (0.71, 1.15) |
0.84 (0.67, 1.06) |
0.40
(0.32, 0.50) |
0.58
(0.44, 0.75) |
4.41
(3.43, 5.68) |
3.79
(2.95, 4.87) |
| Current smoker (ref. = yes) | ||||||||||||
| No |
1.17
(1.02, 1.33) |
0.95 (0.82, 1.09) |
1.05 (0.91, 1.20) |
0.96 (0.83, 1.11) |
1.25
(1.09, 1.42) |
0.99 (0.87, 1.11) |
1.09 (0.95, 1.25) |
1.10 (0.95, 1.28) |
1.21
(1.07, 1.36) |
1.19
(1.04, 1.37) |
0.83
(0.72, 0.96) |
0.80
(0.70, 0.92) |
| Current alcohol drinker (ref. = yes) | ||||||||||||
| No | 0.90 (0.80, 1.02) |
0.93 (0.82, 1.05) |
0.83
(0.73, 0.93) |
0.86
(0.76, 0.97) |
1.06 (0.94, 1.18) |
1.06 (0.94, 1.20) |
0.93 (0.82, 1.05) |
0.95 (0.83, 1.08) |
0.92 (0.81, 1.04) |
1.06 (0.93, 1.19) |
0.66
(0.58, 0.75) |
0.74
(0.65, 0.83) |
| Physical activity (ref. = high) | ||||||||||||
| Low |
0.81
(0.72, 0.92) |
0.87
(0.77, 0.99) |
1.17
(1.04, 1.31) |
1.23
(1.09, 1.39) |
1.00 (0.89, 1.13) |
1.00 (0.89, 1.13) |
0.96 (0.86, 1.08) |
0.98 (0.88, 1.09) |
0.80
(0.71, 0.89) |
0.83
(0.74, 0.92) |
1.07 (0.95, 1.21) |
1.01 (0.89, 1.14) |
1 The values shown are odds ratio (OR) and 95% confidence intervals (CI). Values in bold are significantly different at a level of p < 0.05. T1, T2, and T3 indicate the tertiles of dietary pattern scores.
In general, females had higher odds of adhering to two dietary patterns (i.e., the cereal, milk, sugar, and oil pattern, and the fruits and miscellaneous food pattern), while the inverse was found in the other dietary patterns. Older adults were more likely to follow the fruits and miscellaneous food pattern. Marital status was significantly associated with three patterns, including the rice, fish, and vegetables and corn patterns. Likewise, the cereal, milk, sugar, and oil dietary pattern, and the meat and beverage dietary pattern were most often observed by current alcohol drinkers. The correlations for wealth status were interesting, as those residing in the poorest quintile had a higher likelihood of adhering to the vegetables and corn pattern, whereas those from the richest quintile favored the cereal, milk, sugar, and oil pattern, and the meat and beverage pattern. The variables of educational attainment, employment status, household size, smoking, and physical activity showed varying associations with different dietary patterns.
4. Discussion
This large-scale, population-based study investigated the sociodemographic and lifestyle determinants of the major dietary patterns among Filipino adults. Six distinct dietary patterns were generated, namely (1) rice; (2) cereal, milk, sugar, and oil; (3) fruits and miscellaneous food; (4) fish; (5) vegetables and corn; and (6) meat and beverage. Results of the generalized ordered logistic regression analysis demonstrated that the dietary patterns were differently associated with sex, age, educational attainment, marital status, employment status, household size, wealth quintile, smoking, alcohol consumption, and physical activity.
The dietary patterns derived in our study were in line with previous literature. For example, the rice and fish patterns were comparable to those reported among the Korean [39,40] and Canadian [41] adult populations. The cereal, milk, sugar, and oil pattern contained core food groups similar to the high-energy [26] as well as high-bread and low-rice [17] patterns described in earlier studies. The fruits and miscellaneous food pattern, and vegetables and corn pattern have also been noted in other research [17,42]. Remarkably, the meat and beverage pattern was consistent with the Philippines study [6].
We found significant sociodemographic and lifestyle differences across the six dietary patterns. Men were more likely to adhere to the rice pattern, fish pattern, vegetables and corn pattern, and meat and beverage pattern. This result is in agreement with the national dietary survey results wherein Filipino adult men had a higher mean consumption of rice and rice products, meat, fish, and beverages than women [30]. The influences of age, educational attainment, and marital status on dietary patterns were diverse. Older adults and those with a high school level of education or higher commonly followed the fruits and miscellaneous food pattern, while younger adults and those with at least an elementary education favored the rice pattern; cereal, milk, sugar, and oil pattern; and meat and beverage pattern. In accordance with the literature, age was positively associated with the fruit-based patterns [21,43,44] and was negatively correlated with diets consisting of energy-dense, refined, and processed-food components [21,45]. Our results demonstrated that older adults make positive decisions with respect to their nutrition and health. As for the level of education, most studies documented that healthier dietary patterns or diets containing fruits and vegetables were observed more frequently in highly educated individuals [21,46,47]. Nevertheless, our findings indicate that educational attainment was related to the rice, cereal, milk, sugar and oil; fish; and meat and beverage patterns. This may be ascribed to other factors of healthy eating apart from the number of years in school [48]. With regard to marital status, the relationship found in this study concurs with earlier works wherein dietary patterns may be affected by the state of social relationships [41,49].
The determinants of socioeconomic status, including employment, household size, and wealth quintile, had mixed effects on the dietary patterns. Employed adults had higher adherence to the cereal, milk, sugar, and oil pattern, and the meat and beverage pattern, but had a lower likelihood of following the rice pattern. Moreover, those who lived in small and medium-sized households usually followed the fruits and miscellaneous food pattern, and rice pattern, respectively. The odds of adhering to the cereal, milk, sugar, and oil, and the meat and beverage patterns were 3 to 5 times higher among adults in the richest quintile than the poorest quintile. Socioeconomic position could modify dietary patterns through economic capacity. According to FNRI-DOST, the daily per capita food cost of a typical Filipino household was estimated at PhP 60.39 (USD 1.20) in 2013, with nearly 38% spent on fish, meat, and poultry. The unexpended amount was allocated for cereal and cereal products (30.5%); vegetables (8.3%); miscellaneous food (6.7%); milk and milk products (4.7%); eggs (2.7%); fruits (2.6%); fats and oils (2.4%); sugars and syrup (2.1%); dried beans, nuts, and seeds (1.1%); and starchy roots and tubers (1.0%). In addition, family size altered diet diversity as more food groups were eaten by households with less members. An increasing intake of less expensive food items was also reported among the poorest households [30].
Adults who were current alcohol drinkers and with low physical activity were more likely to adhere to the cereal, milk, sugar, and oil pattern, and those who were both current smokers and alcohol drinkers mostly observed the meat and beverage pattern. Conversely, non-current smokers and those engaged in high physical activity favored the vegetables and corn pattern and rice pattern. Existing evidence relates the clustering of unhealthy diets with unhealthy behaviors such as smoking, alcohol consumption, and physical inactivity [45,50].
A number of limitations should be taken into account in the interpretation of our study results. First, dietary intake was assessed using two non-consecutive 24 h food recalls. Measurement errors and recall bias are inevitable in this method. In order to standardize data collection and minimize errors, the nutritionist-dietitians received trainings before the conducting of PNNS [30]. Furthermore, Denova-Gutiérrez and colleagues [51] conveyed a reasonable validity between the 24 h food recall and food frequency questionnaire in generating dietary patterns using factor analysis, rationalizing the usefulness of food recall. The variability of seasonal food intake was also captured since the survey was carried out for over a year [30]. Second, the factor analysis approach involved several subjective decisions that could influence the constitution of dietary patterns [2,3,4,52]. Nonetheless, this statistical method provides an estimate of the relationship between the food groups consumed by individuals and allows for the determination of dietary patterns that represent the eating habits of a study population [2,52,53,54]. It is encouraging that dietary patterns in our current study were also ascertained in other investigations, which could imply reproducibility among different populations. Third, the dietary patterns explained the low variability of the total food intake (ranging from 2.6 to 5.8%). Past literature elucidates that the amount of variance explained by factors or components determined through a posteriori techniques is relatively low and affected by the number of food groups incorporated in the analysis [55,56]. Lastly, the cross-sectional design did not allow for the exploration of lifetime dietary intake and inference of causal relationships. It will be necessary to conduct prospective studies to verify our findings.
Notwithstanding the aforesaid limitations, this study contributes to the current body of knowledge on food patterns mainly because the data was from a national survey that is representative of the consumption behavior of Filipino adults. Another important strength is the sensitivity analysis performed to evaluate the stability of the derived dietary patterns. The results of the factor solution cross-validation through PCA revealed adequate stability.
5. Conclusions
This study offers a novel approach in characterizing the consumption patterns of a nationally representative sample of adults in the Philippines. Findings indicate six major dietary patterns among community-dwelling adults, including (1) rice; (2) cereal, milk, sugar, and oil; (3) fruits and miscellaneous food; (4) fish; (5) vegetables and corn; and (6) meat and beverage patterns. These patterns were associated with sociodemographic and lifestyle factors, and would have valuable implications for public health interventions. For instance, it is crucial to tailor nutrition and health promotion programs for adults who are younger, employed, from the richest households, and with unhealthy lifestyles to include fish, fruits, and vegetables in their daily diets. This study also puts forward the concept that healthy dietary patterns in conjunction with food-based dietary guidelines are necessary for improving the nutritional state of adults. Future research is warranted to examine the link between the Filipino diet and the health outcomes using these dietary patterns.
Acknowledgments
We would like to thank the Food and Nutrition Research Institute, Department of Science and Technology, Philippines, for granting us access to the 2013 National Nutrition Survey data. This study was supported by the Veritas et Conscientia Scholarship at the College of Medicine, National Cheng Kung University, Tainan City, Taiwan.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14040886/s1, Figure S1: Scree plot showing variances of the factors extracted using factor analysis; Figure S2. Scree plot showing the percentage of explained variances of the dimensions or components extracted using principal component analysis; Table S1: Eigenvalues of the factors or components extracted using factor analysis; Table S2. Eigenvalues of the dimensions or components extracted using principal component analysis.
Author Contributions
Conceptualization, A.R.d.J., W.-C.H. and S.C.H.; writing—original draft preparation, A.R.d.J.; data analysis, W.-C.H. and A.R.d.J.; supervision, S.C.H.; writing—review and editing, A.R.d.J., W.-C.H. and S.C.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research study received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and certified for exemption from the Human Research Ethics Committee of National Cheng Kung University (HREC no. 110-280, date of approval: 27 May 2021).
Informed Consent Statement
The 2013 National Nutrition Survey obtained ethical clearance from the Institutional Ethics Review Committee of the Department of Science and Technology, Food and Nutrition Research Institute, Manila, Philippines, before the survey was conducted. Written informed consent was obtained from all the subjects involved in the study.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://enutrition.fnri.dost.gov.ph/site/home.php (accessed on 14 February 2020).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murray C.J.L., Aravkin Y., Zheng P., Abbafati C., Abbas K.M., Abbasi-Kangevari M., Abd-Allah F., Abdelalim A., Abdollahi M., Abdollapour I., et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hu F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Moeller S.M., Reedy J., Millen A.E., Dixon L.B., Newby P.K., Tucker K.L., Krebs-Smith S.M., Guenther P.M. Dietary patterns: Challenges and opportunities in dietary patterns research an experimental biology workshop, April 1, 2006. J. Am. Diet. Assoc. 2007;107:1233–1239. doi: 10.1016/j.jada.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Tucker K.L. Dietary patterns, approaches, and multicultural perspective. Appl. Physiol. Nutr. Metab. 2010;35:211–218. doi: 10.1139/H10-010. [DOI] [PubMed] [Google Scholar]
- 5.Ocké M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013;72:191–199. doi: 10.1017/S0029665113000013. [DOI] [PubMed] [Google Scholar]
- 6.Angeles-Agdeppa I., Sun Y., Tanda K.V. Dietary pattern and nutrient intakes in association with non-communicable disease risk factors among Filipino adults: A cross-sectional study. Nutr. J. 2020;19:1–13. doi: 10.1186/s12937-020-00597-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai J.X., Nuli R., Zhang Y., Zhang Y.Y., Abudusemaiti M., Kadeer A., Tian X., Xiao H. Association of dietary patterns with type 2 diabetes mellitus among middle-aged adults in Uygur population of Xinjiang region. J. Nutr. Sci. Vitaminol. 2019;65:362–374. doi: 10.3177/jnsv.65.362. [DOI] [PubMed] [Google Scholar]
- 8.Chan R., Yau F., Yu B., Woo J. The role of dietary patterns in the contribution of cardiorespiratory fitness in community-dwelling older Chinese adults in Hong Kong. J. Am. Med. Dir. Assoc. 2019;20:558–563. doi: 10.1016/j.jamda.2018.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Doostvandi T., Bahadoran Z., Mozaffari-Khosravi H., Tahmasebinejad Z., Mirmiran P., Azizi F. The association of dietary patterns and the incidence of insulin resistance after a 3-year follow-up: Tehran Lipid and Glucose Study. Asia Pac. J. Clin. Nutr. 2017;26:531–538. doi: 10.6133/apjcn.032016.12. [DOI] [PubMed] [Google Scholar]
- 10.Haidari F., Shirbeigi E., Cheraghpour M., Mohammadshahi M. Association of dietary patterns with body mass index, waist circumference, and blood pressure in an adult population in Ahvaz, Iran. Saudi Med. J. 2014;35:967–974. [PubMed] [Google Scholar]
- 11.Hong X., Xu F., Wang Z.Y., Liang Y.Q., Li J.Q. Dietary patterns and the incidence of hyperglycemia in China. Public Health Nutr. 2015;19:131–141. doi: 10.1017/S1368980015000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ito T., Kawakami R., Tanisawa K., Miyawaki R., Ishii K., Torii S., Suzuki K., Sakamoto S., Torii S., Suzuki K., et al. Dietary patterns and abdominal obesity in middle-aged and elderly Japanese adults: Waseda Alumni’s Sports, Exercise, Daily Activity, Sedentariness and Health Study (WASEDA’S Health Study) Nutrition. 2019;58:149–155. doi: 10.1016/j.nut.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 13.Kim J., Jo I., Joung H. A rice-based traditional dietary pattern is associated with obesity in Korean adults. J. Acad. Nutr. Diet. 2012;112:246–253. doi: 10.1016/j.jada.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Lee J.Y., Jun N.R., Yoon D., Shin C., Baik I. Association between dietary patterns in the remote past and telomere length. Eur. J. Clin. Nutr. 2015;69:1048–1052. doi: 10.1038/ejcn.2015.58. [DOI] [PubMed] [Google Scholar]
- 15.Muga M.A., Owili P.O., Hsu C.Y., Rau H.H., Chao J.C.J. Dietary patterns, gender, and weight status among middle-aged and older adults in Taiwan: A cross-sectional study. BMC Geriatr. 2017;17:1–10. doi: 10.1186/s12877-017-0664-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naja F., Itani L., Hwalla N., Sibai A.M., Kharroubi S.A. Identification of dietary patterns associated with elevated blood pressure among Lebanese men: A comparison of principal component analysis with reduced rank regression and partial least square methods. PLoS ONE. 2019;14:e0220942. doi: 10.1371/journal.pone.0220942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okada E., Takahashi K., Takimoto H., Takabayashi S., Kishi T., Kobayashi T., Nakamura K., Ukawa S., Nakamura M., Sasaki S., et al. Dietary patterns among Japanese adults: Findings from the National Health and Nutrition Survey, 2012. Asia Pac. J. Clin. Nutr. 2018;27:1120–1130. doi: 10.6133/apjcn.042018.06. [DOI] [PubMed] [Google Scholar]
- 18.Park J.E., Jung H., Lee J.E. Dietary pattern and hypertension in Korean adults. Public Health Nutr. 2013;17:597–606. doi: 10.1017/S1368980013000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rashidkhani B., Gargari B.P., Ranjbar F., Zareiy S., Kargarnovin Z. Dietary patterns and anthropometric indices among Iranian women with major depressive disorder. Psychiatry Res. 2013;210:115–120. doi: 10.1016/j.psychres.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 20.Rezazadeh A., Rashidkhani B. The association of general and central obesity with major dietary patterns of adult women living in Tehran, Iran. J. Nutr. Sci. Vitaminol. 2010;56:132–138. doi: 10.3177/jnsv.56.132. [DOI] [PubMed] [Google Scholar]
- 21.Rezazadeh A., Rashidkhani B., Omidvar N. Association of major dietary patterns with socio-economic and lifestyle factors of adult women living in Tehran, Iran. Nutrition. 2010;26:337–341. doi: 10.1016/j.nut.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 22.Safdar N.F., Bertone-Johnson E.R., Cordeiro L., Jafar T.H., Cohen N.L. Dietary patterns and their association with hypertension among Pakistani urban adults. Asia Pac. J. Clin. Nutr. 2015;24:710–719. doi: 10.6133/apjcn.2015.24.4.27. [DOI] [PubMed] [Google Scholar]
- 23.Shin D., Lee K.W., Kim M.H., Kim H.J., An Y.S., Chung H.K. Identifying dietary patterns associated with mild cognitive impairment in older Korean adults using reduced rank regression. Int. J. Environ. Res. Public Health. 2018;15:100. doi: 10.3390/ijerph15010100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vajdi M., Nikniaz L., Asl A.M.P., Farhangi M.A. Lifestyle patterns and their nutritional, socio-demographic and psychological determinants in a community-based study: A mixed approach of latent class and factor analyses. PLoS ONE. 2020;15:e0236242. doi: 10.1371/journal.pone.0236242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Venkaiah K., Brahmam G.N.V., Vijayaraghavan K. Application of factor analysis to identify dietary patterns and use of factor scores to study their relationship with nutritional status of adult rural populations. J. Health Popul. Nutr. 2011;29:327–338. doi: 10.3329/jhpn.v29i4.8448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei Z.Y., Liu J.J., Zhan X.M., Feng H.M., Zhang Y.Y. Dietary patterns and the risk of metabolic syndrome in Chinese adults: A population-based cross-sectional study. Public Health Nutr. 2018;21:2409–2416. doi: 10.1017/S1368980018001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang M.Y., Li Z.J., Yang S.M., Sun Y.Y., Jin M.D., Chen X., Yu Q. The association between dietary patterns and depressive symptoms in Chinese adults. Biomed Res. Int. 2020;2020:8380151. doi: 10.1155/2020/8380151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Department of Science and Technology-Food and Nutrition Research Institute Public Use File. [(accessed on 14 February 2020)]; Available online: http://enutrition.fnri.dost.gov.ph/site/home.php.
- 29.Patalen C.F., Ikeda N., Angeles-Agdeppa I., Vargas M.B., Nishi N., Duante C.A., Capanzana M.V. Data Resource Profile: The Philippine National Nutrition Survey (NNS) Int. J. Epidemiol. 2020;49:742–743f. doi: 10.1093/ije/dyaa045. [DOI] [PubMed] [Google Scholar]
- 30.Department of Science and Technology-Food Nutrition Research Institute eNutrition, Facts and Figure 2013 National Nutrition Survey. [(accessed on 3 September 2020)]; Available online: https://www.fnri.dost.gov.ph/index.php/19-nutrition-statistic/175-national-nutrition-survey#facts-and-figures.
- 31.Flores M., Macias N., Rivera M., Lozada A., Barquera S., Rivera-Dommarco J., Tucker K.L. Dietary patterns in Mexican adults are associated with risk of being overweight or obese. J. Nutr. 2010;140:1869–1873. doi: 10.3945/jn.110.121533. [DOI] [PubMed] [Google Scholar]
- 32.Gazan R., Béchaux C., Crépet A., Sirot V., Drouillet-Pinard P., Dubuisson C., Harvard S. Dietary patterns in the French adult population: A study from the second French national cross-sectional dietary survey (INCA2) (2006–2007) Br. J. Nutr. 2016;116:300–315. doi: 10.1017/S0007114516001549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Gavelle E., Huneau J.F., Mariotti F. Patterns of protein food intake are associated with nutrient adequacy in the general French adult population. Nutrients. 2018;10:226. doi: 10.3390/nu10020226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zárate-Ortiz A.G., Melse-Boonstra A., Rodríguez-Ramírez S., Hernández-Cordero S., Feskens E.J. Dietary patterns and the double burden of malnutrition in Mexican adolescents: Results from ENSANUT-2006. Nutrients. 2019;11:2753. doi: 10.3390/nu11112753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smyth R., Johnson A. Factor Analysis. [(accessed on 8 January 2022)]. Available online: https://www.uwo.ca/fhs/tc/labs/10.FactorAnalysis.pdf.
- 36.Bell L.K., Edwards S., Grieger J.A. The relationship between dietary patterns and metabolic health in a representative sample of adult Australians. Nutrients. 2015;7:6491–6505. doi: 10.3390/nu7085295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization . WHO STEPS Surveillance Manual: The WHO STEPwise Approach to Chronic Disease Risk Factor Surveillance. WHO; Geneva, Switzerland: 2005. [Google Scholar]
- 38.World Health Organization . Global Status Report on Alcohol and Health 2018. WHO; Geneva, Switzerland: 2019. [Google Scholar]
- 39.Park S., Bae J.-H. Fermented food intake is associated with a reduced likelihood of atopic dermatitis in an adult population (Korean National Health and Nutrition Examination Survey 2012–2013) Nutr. Res. 2016;36:125–133. doi: 10.1016/j.nutres.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 40.Lee W.L., Woo H.D., Cho M.J., Park J.K., Kim S.S. Identification of dietary patterns associated with incidence of hyperglycemia in middle-aged and older Korean adults. Nutrients. 2019;11:1801. doi: 10.3390/nu11081801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Z., Liu L., Roebothan B., Ryan A., Colbourne J., Baker N., Yan J., Wang P.P. Four major dietary patterns identified for a target-population of adults residing in Newfoundland and Labrador, Canada. BMC Public Health. 2015;15:1–12. doi: 10.1186/s12889-015-1433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mishra G., Ball K., Arbuckle J., Crawford D. Dietary patterns of Australian adults and their association with socioeconomic status: Results from the 1995 National Nutrition Survey. Eur. J. Clin. Nutr. 2002;56:687–693. doi: 10.1038/sj.ejcn.1601391. [DOI] [PubMed] [Google Scholar]
- 43.Knudsen V.K., Matthiessen J., Biltoft-Jensen A., Sørensen M.R., Groth M.V., Christensen T., Fagt S. Identifying dietary patterns and associated health-related lifestyle factors in the adult Danish population. Eur. J. Clin. Nutr. 2014;68:736–740. doi: 10.1038/ejcn.2014.38. [DOI] [PubMed] [Google Scholar]
- 44.Park S., Murphy S., Wilkens L.R. Dietary patterns using the Food Guide Pyramid groups are associated with socioeconomic and lifestyle factors: The multi-ethnic cohort study. J. Nutr. 2005;135:843–849. doi: 10.1093/jn/135.4.843. [DOI] [PubMed] [Google Scholar]
- 45.Sánchez-Villegas A., Delgado-Rodríguez M., Martínez-González M.Á., de Irala-Estévez J. Gender, age, socio-demographic and lifestyle factors associated with major dietary patterns in the Spanish Project SUN (Seguimineto Universidad de Navarra) Eur. J. Clin. Nutr. 2003;57:285–292. doi: 10.1038/sj.ejcn.1601528. [DOI] [PubMed] [Google Scholar]
- 46.Kesse-Guyot E., Bertrais S., Peneau S., Estaquio C., Dauchet L., Vergnaud A.C., Czemichow P., Galan S., Hercberg S., Bellisle F. Dietary patterns and their sociodemographic and behavioral correlates in French middle-aged adults from the SU. VI. MAX cohort. Eur. J. Clin. Nutr. 2009;63:521–528. doi: 10.1038/sj.ejcn.1602978. [DOI] [PubMed] [Google Scholar]
- 47.Kriaučionienė V., Petkevičienė J., Klumbienė J. Dietary patterns and their association with lifestyle factors in Lithuanian adult population. Medicina. 2009;44:799–804. doi: 10.3390/medicina44100100. [DOI] [PubMed] [Google Scholar]
- 48.World Health Organization . Global Strategy on Diet, Physical Activity and Health. WHO; Geneva, Switzerland: 2004. [Google Scholar]
- 49.Vinther J.L., Conklin A.I., Wareham N.J., Monsivais P. Marital transitions and associated changes in fruit and vegetable intake: Findings from the population-based [rospective EPIC-Norfolk cohort, UK. Soc. Sci. Med. 2016;157:120–126. doi: 10.1016/j.socscimed.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ax E., Lemming E.W., Becker W., Andersson A., Lindroos A.K., Cederholm T., Sjörgren P., Fung T.T. Dietary patterns in Swedish adults: Results from a national dietary survey. Br. J. Clin. Nutr. 2015;115:95–104. doi: 10.1017/S0007114515004110. [DOI] [PubMed] [Google Scholar]
- 51.Denova-Gutiérrez E., Tucker K.L., Salmerón J., Flores M., Barquera S. Relative validity of a food frequency questionnaire to identify dietary patterns in Mexican adult population. Salud Publica Mex. 2016;58:608–616. doi: 10.21149/spm.v58i6.7842. [DOI] [PubMed] [Google Scholar]
- 52.Martinez M.E., Marshall J.R., Sechrest L. Invited commentary: Factor analysis and the search for objectivity. Am. J. Epidemiol. 1998;148:17–19. doi: 10.1093/oxfordjournals.aje.a009552. [DOI] [PubMed] [Google Scholar]
- 53.Skrondal A., Rabe-Hesketh S. Generalized Latent Variable Modeling: Multilevel, Longitudinal and Structural Equation Models. Chapman and Hall/CRC; London, UK: 2004. [Google Scholar]
- 54.Hair J.F., Black W.C., Babin B.J., Anderson R.E. Multivariate Data Analysis. 7th ed. Pearson Prentice Hall; Hoboken, NJ, USA: 2009. [Google Scholar]
- 55.Hawrysz I., Wadolowska L., Slowinska M.A., Czerwinska A., Golota J.J. Adherence to Prudent and Mediterranean dietary patterns is inversely associated with lung cancer in moderate but not heavy male Polish smokers: A case-control study. Nutrients. 2020;12:3788. doi: 10.3390/nu12123788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Borges C.A., Rinaldi A.E., Conde W.L., Mainardi G.M., Behar D., Slater B. Dietary patterns: A literature review of methodological characteristics of the main step in multivariate analyzes. Rev. Bras. Epidemiol. 2015;18:837–857. doi: 10.1590/1980-5497201500040013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: http://enutrition.fnri.dost.gov.ph/site/home.php (accessed on 14 February 2020).