Abstract
Context
The single-legged squat (SLS) is appropriate for targeting activation, strengthening, and neuromuscular retraining of the gluteus maximus, gluteus medius, and quadriceps. However, the effects of different nonstance-limb positions on muscle activity have not been fully evaluated.
Objective
To compare the muscle activity of selected stance-limb hip muscles during the SLS using 3 nonstance-limb positions: in front (SLS-Front), in the middle (SLS-Middle), and in back (SLS-Back).
Design
Controlled laboratory study.
Setting
Biomechanics laboratory.
Patients or Other Participants
A total of 17 healthy adults (8 men, 9 women; age = 22.6 ± 3.6 years, height = 173.3 ± 10.7 cm, mass = 71.2 ± 11.0 kg) participated.
Main Outcome Measure(s)
Surface electromyographic data of the gluteus maximus, gluteus medius, lateral hamstrings, medial hamstrings, rectus femoris, and tensor fascia lata (TFL) as well as kinetic data of the hip and knee were collected while participants performed the 3 SLS tasks. Mean muscle-activation levels during the descent and ascent phases for the selected hip muscles and hip and knee kinetics in all 3 planes were compared for the 3 tasks. Each variable of interest was analyzed using a separate linear regression model with a generalized estimating equations correction.
Results
Muscle-activation levels of the gluteus maximus, gluteus medius, medial hamstrings, rectus femoris, and TFL for the stance limb during descent (P ≤ .04) and the medial hamstrings and TFL during ascent (P ≤ .002) were different among the SLS tasks. The greatest number of differences occurred between SLS-Front and SLS-Back. During descent, gluteal muscle activity was greater in SLS-Front (P ≤ .03) and SLS-Middle (P = .03) than in SLS-Back. For both phases, TFL activity was greater during SLS-Front than during both SLS-Middle and SLS-Back (P ≤ .006). Kinetic differences at the hip and knee between SLS tasks were also observed (P values ≤ .02).
Conclusions
The 3 SLS tasks had different muscle-activation and kinetic profiles. Clinicians and researchers can vary nonstance-limb position during the SLS to manipulate muscle-activation levels and tailor the exercise to assist with goals at different stages of rehabilitation.
Keywords: muscle activity, movement analysis, therapeutic exercise, biomechanics
Key Points
Nonstance-limb position affected muscle activation during the single-legged squat.
Stance-limb gluteal muscle activity during the descent phase was lower with the nonstance limb behind than in the middle or in front.
Tensor fascia lata activity in the stance limb was higher with the nonstance limb held in front of the stance limb compared with the middle or back.
The nonstance-limb position can be modified to meet individual strengthening and rehabilitation goals.
The single-legged squat (SLS) is commonly used by clinicians as an assessment and treatment tool.1,2 As an assessment tool, the SLS is used to examine movement patterns of the trunk, pelvis, and lower extremity during dynamic single-legged weightbearing. Faults commonly observed during the SLS include increased ipsilateral trunk lean, contralateral pelvic drop, hip adduction, and knee abduction.3 As a treatment tool, the SLS is used for both strengthening and neuromuscular retraining to increase control of the hip and knee in the frontal and transverse planes.4 Most of this control is thought to come from appropriate activation of the hip abductors and external rotators.5,6
In several studies,3,7–15 researchers have used electromyography (EMG) to quantify muscle activity of the gluteus maximus, gluteus medius, hamstrings, quadriceps, and other lower extremity muscles during the SLS. Generally, they have found the SLS to be appropriate for targeting activation, strengthening, and neuromuscular retraining of the gluteus maximus, gluteus medius, and quadriceps. Muscle activity of the tensor fascia lata (TFL) during the SLS, however, has been less well examined. This is notable because the TFL is a hip abductor and internal rotator that may contribute to excessive hip internal rotation if gluteal muscle weakness is present.6,16 Therefore, it may be important to simultaneously quantify muscle activity of the gluteus maximus, gluteus medius, and TFL during the SLS to better understand the relationship among the muscles and whether the SLS can be used to strengthen the gluteal muscles while minimizing TFL activity.
There is no widely accepted way to perform the SLS, especially regarding the position of the nonstance limb. The 3 most common nonstance-limb positions during the SLS are with the nonstance limb in front of, in line with, or behind the stance limb. Different nonstance-limb positions may change the neuromuscular demands of the trunk, pelvis, and lower extremity and result in altered movement17–19 or muscle activation.19 Muscle activation during the SLS with different nonstance-limb positions has been evaluated in only 1 study. Olivier et al19 noted more rectus femoris activity and less biceps femoris activity with the nonstance limb behind the stance limb than with the nonstance limb in front. The greatest gluteus medius activity was with the nonstance limb in front and the hip flexed to 90°. However, they did not evaluate TFL activation19 and did not assess SLS with the nonstance knee extended in front, often called the pistol squat, a variation gaining popularity. Thus, the primary purpose of our study was to compare the muscle activity of selected hip muscles (ie, gluteus maximus, gluteus medius, lateral hamstrings, medial hamstrings, rectus femoris, and TFL) during the SLS via 3 commonly used nonstance-limb positions. A secondary purpose was to compare hip and knee kinetics among the 3 variations of the SLS task. We hypothesized that muscle activity of the selected hip muscles as well as hip and knee mechanics would be different among the SLS tasks.
METHODS
Participants
A convenience sample of 17 healthy adults (8 men, 9 women; age = 22.6 ± 3.6 years, height = 173.3 ± 10.7 cm, mass = 71.2 ± 11.0 kg) volunteered to participate in this study between January 2014 and March 2015; this was a subset of participants from previously published studies.17,18 To be included, individuals had to be between the ages of 18 and 50 years. Volunteers were excluded if they reported having any back or lower extremity pain lasting >2 weeks within the 2 months before the study. All participants provided written informed consent before testing. The study protocol was approved by the institutional review board of Boston University.
Instrumentation
Muscle activity of the gluteus maximus, posterior portion of the gluteus medius, lateral hamstrings, medial hamstrings, rectus femoris, and TFL was recorded using a surface EMG system (Bagnoli; Delsys Inc) sampling at 1000 Hz. Single differential surface EMG electrodes (DE-2.1; Delsys Inc), each with 2 parallel 10- × 1-mm silver bars spaced 10 mm apart, were placed bilaterally over the muscle bellies of the selected hip muscles according to the manufacturer's guidelines.20 In addition, a disposable ground electrode was placed on the bony prominence of the posterior right elbow. Before electrode placement, the skin was prepared by cleaning the area using a cotton ball soaked in rubbing alcohol. The electrodes were connected to a backpack-worn unit that transmitted the raw EMG data to the receiver unit through a shielded cable. The specifications of the 16-channel receiver unit included a response frequency of 20 to 450 Hz, input impedance of >1015 Ω, common-mode rejection ratio of >100 dB, and amplifier gain of 1000. The EMG signal amplitudes were visually inspected as participants contracted each muscle to verify electrode placement before data collection.
Trunk, pelvic, and lower extremity kinematic data were collected using a 10-camera motion-capture system (Vicon Motion Systems Ltd) sampling at 100 Hz. Retroreflective markers were placed bilaterally on the following bony landmarks: first and fifth metatarsal heads, calcanei, medial and lateral malleoli, medial and lateral femoral epicondyles, greater trochanters, anterior-superior iliac spines, iliac crests, sacrum between the posterior-superior iliac spines, xiphoid process, acromion processes, and spinous process of the C7 vertebra. In addition, plastic shells, each containing a cluster of 4 noncollinear markers, were placed on the lateral shanks and thighs.21 Ground reaction force data were collected using the force plates in an instrumented split-belt treadmill (Bertec Corp) sampling at 1000 Hz. Kinematic, kinetic, and EMG data were synchronized using Nexus (version 1.8.5; Vicon Motion Systems Ltd).
Procedures
Surface EMG electrodes were placed on the lower extremity before the placement of retroreflective markers on the trunk, pelvis, and lower extremity. After electrode and marker placement, a standing static trial was recorded and used to create a participant-specific model. The markers on the medial femoral epicondyles and medial malleoli were removed after the static trial to prevent any movement obstruction during testing.
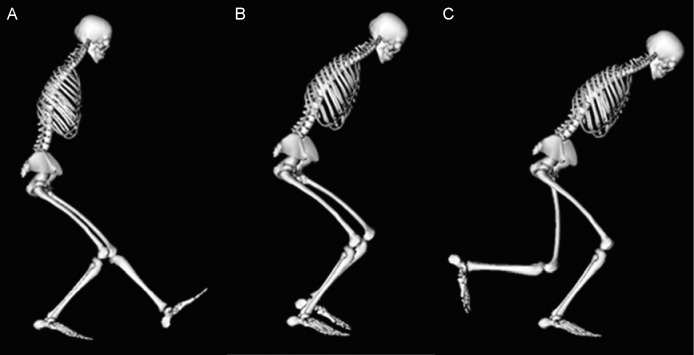
Next, participants performed 3 SLS tasks. The position of the nonstance limb differentiated the 3 SLS tasks: in front (SLS-Front), in the middle (SLS-Middle), and in back (SLS-Back). Five individual trials of each SLS task were collected for both limbs. The order of the 3 SLS tasks was block randomized. For each SLS task, participants started by standing on both limbs with each foot on a separate force plate. They were then instructed to stand on 1 limb, position their nonstance limb in 1 of 3 positions (Figure 1), squat as low as possible in a controlled manner while keeping their upper limbs at or out to their sides, and return to standing on both limbs. For SLS-Front, the nonstance limb was extended out to the front during the squat, similar to a pistol squat (Figure 1A). For SLS-Middle, the knee of the nonstance limb was slightly flexed with the nonstance foot held in line with the ankle of the stance limb during the squat (Figure 1B). For SLS-Back, the knee of the nonstance limb was flexed to 90° while the nonstance thigh maintained a vertical position during the squat (Figure 1C). Participants were allowed to practice each SLS task before the recorded trials. A trial was collected again if the participant lost his or her balance, did not position the nonstance limb correctly, or performed the motion in a jerky or noncontinuous manner. The speed of each squat was not strictly enforced using a metronome, but oral feedback was given when necessary to help participants maintain a consistent speed and a smooth, fluid motion during testing. We believed this better approximated what occurs in a clinical setting and was suitable for the repeated-measures design of this study.
Figure 1.
Each participant performed 3 single-legged squat (SLS) tasks that were differentiated by the position of the nonstance limb: A, SLS-Front, B, SLS-Middle, and C, SLS-Back.
Data Processing
The EMG processing and smoothing were completed using Visual3D (C-Motion). Raw EMG data were band-pass filtered between 10 and 390 Hz using a fourth-order Butterworth filter with zero phase lag and root mean square (RMS) smoothed using a 100-millisecond moving window. Average RMS data of the stance limb were extracted for 2 phases of the squat movement: descent (start of stance knee flexion to maximum knee flexion) and ascent (maximum knee flexion to return to standing on both limbs). For each phase, average RMS activations were averaged across the trials for each SLS task for each stance limb. Participant-based mean muscle activation of each muscle of each stance limb during each phase was exported for statistical analysis.
Marker data were labeled using Vicon Nexus and processed using Visual3D. Kinematic data were filtered using a low-pass, fourth-order Butterworth filter with a cutoff frequency of 6 Hz.22 Joint angles were calculated using a Visual3D hybrid model with a CODA pelvis23 and a right-handed Cardan X-Y-Z (mediolateral, anteroposterior, vertical) rotation sequence.24 Joint angles were calculated as the angle between the distal and proximal segments. Kinetic data were also processed using Visual3D and were filtered using a low-pass, fourth-order Butterworth filter with a cutoff frequency of 10 Hz.22 Kinematic and ground reaction force data were used to calculate internal joint moments. Custom code (MATLAB; The MathWorks, Inc) was used to extract hip and knee moments of the stance limb in the sagittal, frontal, and transverse planes at peak knee flexion for each trial. For each participant, mean joint moments were calculated by averaging across the trials for each SLS task for each stance limb.
Statistical Analysis
A repeated-measures analysis was performed for each variable of interest using a linear regression model with a generalized estimating equations (GEE) correction to determine differences among the 3 SLS tasks. For muscle activity, the variables of interest were the participant-based mean muscle activations of the selected lower extremity muscles (gluteus maximus, gluteus medius, lateral hamstrings, medial hamstrings, rectus femoris, and TFL) during each phase (descent and ascent) of each SLS task (SLS-Front, SLS-Middle, and SLS-Back). A separate linear regression model with a GEE correction was performed for each muscle during each phase. The kinetic variables of interest were mean hip and knee moments at peak knee flexion in the sagittal, frontal, and transverse planes as previously analyzed in an overlapping group of participants.17,18 Moments were normalized to each participant's mass before statistical analysis. A separate linear regression model with a GEE correction was calculated for each kinetic variable of interest. For all main effect analyses, 2 within-subject factors were included in each model: task (SLS-Front, SLS-Middle, and SLS-Back) and side of stance limb (left and right). Post hoc pairwise comparisons with a least significant difference correction were performed if we observed a task effect. All statistical analyses were performed using SPSS (version 24; IBM Corp). The α level was set at .05 for all tests.
RESULTS
Muscle Activity
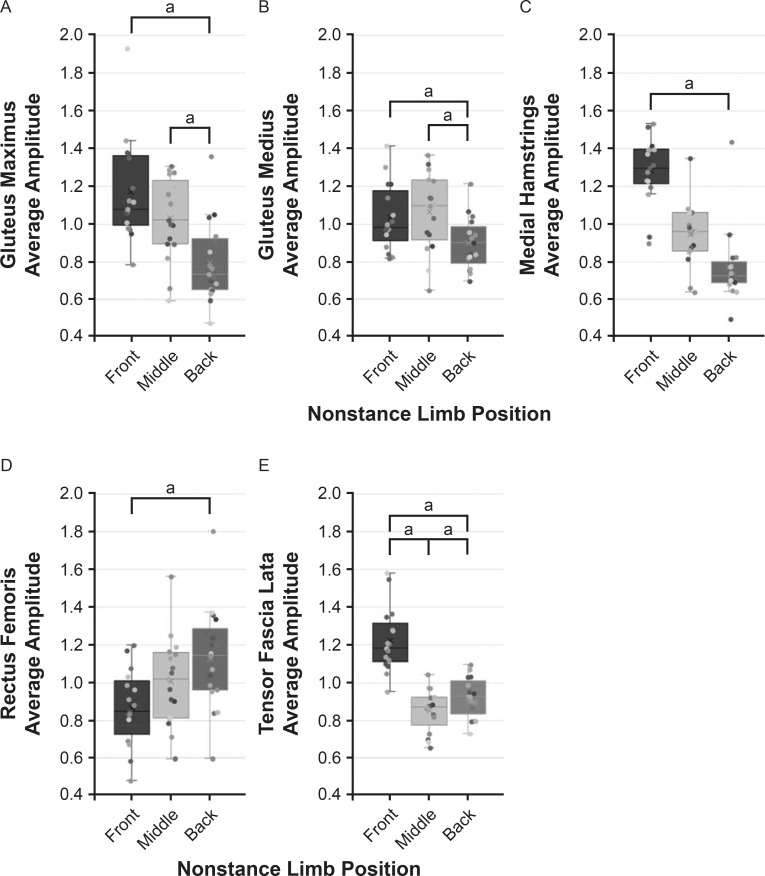
For the descent phase of the SLS tasks, we observed main effects of task for the gluteus maximus, gluteus medius, medial hamstrings, rectus femoris, and TFL (P ≤ .04; Figure 2), and post hoc pairwise comparisons were performed. The SLS-Front had higher average RMS amplitudes than the SLS-Back for the gluteus maximus (P = .006), gluteus medius (P = .03), medial hamstrings (P < .001), and TFL (P < .001) but lower amplitudes for the rectus femoris (P = .02). The SLS-Front also had higher average amplitudes for the TFL than the SLS-Middle (P < .001). The SLS-Middle had higher average amplitudes than the SLS-Back for the gluteus maximus and gluteus medius (both P = .03) but lower amplitude for the TLF (P = .04).
Figure 2.
Combined dot and box plots of average electromyographic amplitudes of the A, gluteus maximus; B, gluteus medius; C, medial hamstrings; D, rectus femoris; and E, tensor fascia lata during the descent phase of 3 single-legged squat tasks with different nonstance-limb positions. Values were normalized to each participant's average of the 3 tasks for display purposes only. The box represents the interquartile range (25th–75th percentile), and whiskers represent minimum and maximum values, excluding outliers (>1.5x interquartile range). Each dot represents an individual's data. A linear regression with a generalized estimating equations correction revealed a main effect for task for the muscles displayed (P < .05). a Paired comparison was different (P < .05).
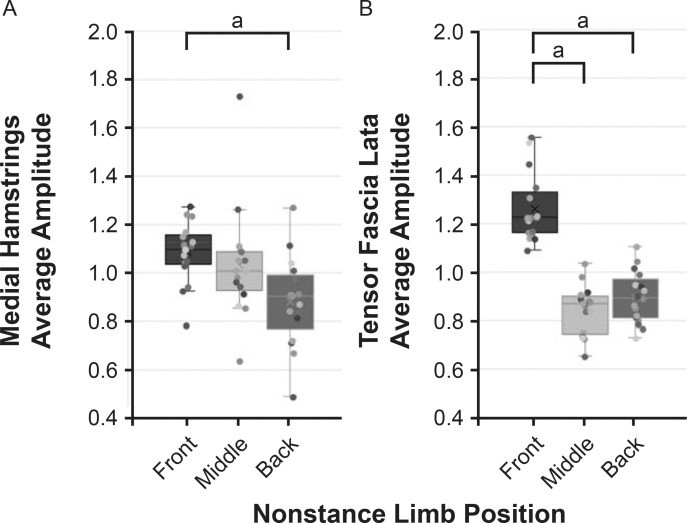
For the ascent phase, we observed main effects of task for the medial hamstrings and TFL (P = .002 and P < .001, respectively; Figure 3). Pairwise comparisons showed the SLS-Front had greater average RMS amplitudes for the medial hamstrings and the TFL than the SLS-Back (P = .006 and P = .001, respectively). The SLS-Front also had greater average amplitudes for the TFL than the SLS-Middle (P < .001).
Figure 3.
Combined dot and box plots of average electromyographic amplitudes of the A, medial hamstrings and B, tensor fascia lata during the ascent phase of 3 single-legged squat tasks with different nonstance-limb positions. Values were normalized to each participant's average of the 3 tasks for display purposes only. The box represents the interquartile range (25th–75th percentile), and whiskers represent minimum and maximum values, excluding outliers (>1.5x interquartile range). Each dot represents an individual's data. A linear regression with a generalized estimating equations correction revealed a main effect for task for the muscles displayed (P < .05). a Paired comparison was different (P < .05).
Kinetics
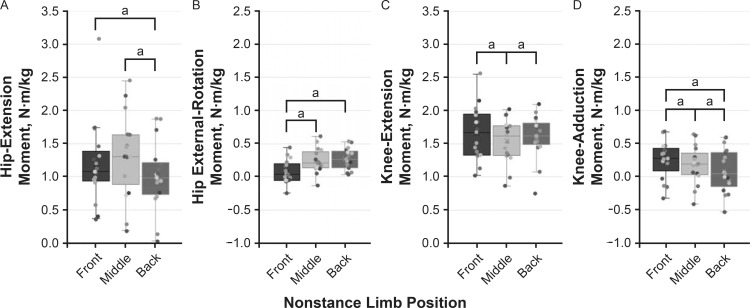
Hip-extension and external-rotation and knee-extension and -adduction moments at peak knee flexion exhibited main effects of task (P < .001), and post hoc pairwise comparisons were conducted (Figure 4). The SLS-Front had a greater hip-extension moment (P = .02) and knee-adduction moment (P < .001) but a smaller hip external-rotation moment (P < .001) than the SLS-Back. The SLS-Front also had a smaller hip external-rotation moment (P < .001) and greater knee-extension and knee-adduction moments (P = .02 and P = .002, respectively) than the SLS-Middle. The SLS-Middle had a greater hip-extension moment (P < .001) and knee-adduction moment (P < .001) than the SLS-Back but a smaller knee-extension moment (P = .008).
Figure 4.
Combined dot and box plots of hip and knee moments at peak knee flexion for 3 single-legged squat tasks with different nonstance-limb positions. A, Hip extension. B, Hip external rotation. C, Knee extension. D, Knee adduction. The box represents the interquartile range (25th–75th percentile), and whiskers represent minimum and maximum values, excluding outliers (>1.5x interquartile range). Each dot represents an individual's data. A linear regression with a generalized estimating equations correction revealed a main effect for task (P < .05) for the moments displayed. a Paired comparison was different (P < .05).
DISCUSSION
The position of the nonstance limb affected the muscle activity of the stance limb during the SLS. Among the 3 SLS tasks tested, the greatest number of differences in muscle-activation levels were between the SLS-Front and SLS-Back during both the descent and ascent phases. Hip and knee mechanics of the stance limb were also influenced by the nonstance-limb position during the SLS. Between the 2 joints, kinetics in all 3 planes differed among the SLS tasks, similar to previous findings from our laboratory.17,18 Our results confirmed that the position of the nonstance limb is a crucial factor to consider when using the SLS for assessment or rehabilitation. These findings can provide clinicians, researchers, and the general public with information to facilitate selection of the appropriate SLS variation for individual strengthening and rehabilitation goals.
We found that TFL activation increased during both the descent and ascent phases of the SLS when the nonstance limb was extended out in front of the stance limb versus being in line with or behind the stance limb. The TFL has been hypothesized to become a primary hip abductor in the presence of gluteus medius weakness and may contribute to further disuse of the gluteals.25,26 Increased muscle activation of the TFL during SLS-Front may suggest that it is being used to control hip adduction and contralateral pelvic drop during this task, but it may also increase a tendency to internally rotate the hip.6 Although it was not the focus of this study, we did note less hip external rotation in the SLS-Front than in the SLS-Back (mean difference ± SE: 2.3° ± 0.9°; P = .009), supporting this assertion. The hip external-rotation moment was also smaller during the SLS-Front than during the other 2 tasks and could have contributed to the increased TFL activation. In theory, increased activation of the TFL during SLS-Front without a change in the hip-abduction moment may suggest that less focus is being placed on the other hip abductor—the gluteus medius (a muscle often targeted during rehabilitation); we did not note a decrease in gluteus medius muscle activity in the SLS-Front versus the SLS-Middle. Therefore, the SLS-Front and SLS-Middle may be appropriate for targeting overall hip-abductor muscle activity. If the intention of the SLS is to minimize the use of the TFL while strengthening the gluteal muscles and focusing on producing a hip external-rotation moment (a common therapeutic goal), the SLS-Middle may be more appropriate than the SLS-Front.
Similar to Olivier et al,19 we noted a higher average RMS amplitude for the gluteus medius and lower amplitude for the rectus femoris during the SLS-Front than the SLS-Back. This finding may suggest that the SLS-Front is an appropriate variation for an individual with patellofemoral pain, a condition in which reducing patellofemoral joint loading via decreased rectus femoris activation may be beneficial. However, the SLS-Front also had a greater internal knee-adduction moment, which may increase the patellofemoral joint reaction force27 and therefore be less appropriate for an individual with patellofemoral pain.
Whereas Olivier et al19 observed changes in the lateral hamstrings (biceps femoris) with a nonstance-limb position, we detected changes only in the medial hamstrings. Differences in activation between the medial and the lateral hamstrings have been seen in clinical populations and with other movement modifications. For example, among individuals with symptomatic knee osteoarthritis involving the medial compartment, the ratio between lateral and medial hamstrings activation during gait was greater than that in an asymptomatic group of similar age.28 Modifying limb position also affects the ratio between the medial and lateral hamstrings. Positioning the limb with the foot externally rotated increases lateral hamstrings activity, whereas internally rotating the foot increases medial hamstrings activity.29 Furthermore, these ratios can be different during different phases of the activity.29,30 We identified more differences in muscle activity during the descent phase, wherein most muscles are working eccentrically, than during the ascent phase.
Although we often use muscle activity to infer moment and moments to infer muscle activity, our results highlight some of the inconsistencies. For example, although rectus femoris activity during descent was lower in the SLS-Front than in the SLS-Back, the knee-extension moment did not differ between those tasks. Instead, the knee-extension moment was smallest in the SLS-Middle compared with either of the other tasks. These disparate findings highlight both the complexity of human movement and the challenge of measuring it. The measure of muscle activity was the average over the phase of movement, while the moment was measured only at peak knee flexion.
Our results indicated that the 3 SLS tasks have different muscle-activation and kinetic profiles, suggesting that they can be used either individually or together as part of a rehabilitation program. Depending on the muscle activations or movement patterns being targeted or avoided, the position of the nonstance limb could be altered. In addition, the SLS tasks may be used in combination as part of a progressive program. For instance, it may be helpful to begin with the SLS-Middle and progress to the SLS-Front or SLS-Back because the SLS-Middle had the most intermediate characteristics of the 3 SLS tasks.
This study had limitations. First, our sample consisted of young, healthy adults without pain. This sample was chosen to understand how altering the position of the nonstance limb affected hip-muscle activations and lower extremity mechanics without pain confounding the results. As such, caution should be taken when generalizing our results to patient populations. Second, we did not use maximal voluntary isometric contraction measures to normalize muscles activity levels. We deemed this acceptable due to the repeated-measures design. Third, whereas we provided instructions on how to position the nonstance limb for each SLS, we did not instruct participants on how to position or move their trunk or lower extremity during the SLS. Therefore, we do not know whether the differences in muscle-activation levels and kinetics between the SLS tasks were due only to changing the nonstance-limb position or whether changes in other segments of the kinematic chain better explain the differences.
CONCLUSIONS
This study quantified the muscle-activity level of selected hip muscles as well as the hip and knee kinetics of 3 SLS tasks with different nonstance-limb positions. During the descent phase, all muscles except the lateral hamstrings exhibited different activation levels among the SLS tasks. The TFL activation levels during both the descent and ascent phases were greater for the SLS-Front than for either the SLS-Middle or SLS-Back. The kinetics of the hip and knee were also different among the 3 SLS tasks. These results indicated that the position of the nonstance limb during the SLS can substantially affect hip-muscle activity and hip and knee mechanics. As such, the nonstance-limb position should be considered when using the SLS for assessments or treatments. These findings can help guide the selection of the appropriate SLS variation for individual strengthening and rehabilitation needs.
ACKNOWLEDGMENTS
This work was supported by grants R21 AR061690 and K23 AR063235 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health. We thank the members of the Human Adaptation Laboratory for assistance with data collection and processing.
REFERENCES
- 1.Willy RW, Manal KT, Witvrouw EE, Davis IS. Are mechanics different between male and female runners with patellofemoral pain? Med Sci Sports Exerc . 2012;44(11):2165–2171. doi: 10.1249/MSS.0b013e3182629215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kivlan BR, Martin RL. Functional performance testing of the hip in athletes: a systematic review for reliability and validity. Int J Sports Phys Ther . 2012;7(4):402–412. [PMC free article] [PubMed] [Google Scholar]
- 3.Nakagawa TH, Moriya ET, Maciel CD, Serrao FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther . 2012;42(6):491–501. doi: 10.2519/jospt.2012.3987. [DOI] [PubMed] [Google Scholar]
- 4.Willy RW, Davis IS. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J Orthop Sports Phys Ther . 2011;41(9):625–632. doi: 10.2519/jospt.2011.3470. [DOI] [PubMed] [Google Scholar]
- 5.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther . 2010;40(2):42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 6.Selkowitz DM, Beneck GJ, Powers CM. Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lata? Electromyographic assessment using fine-wire electrodes. J Orthop Sports Phys Ther . 2013;43(2):54–64. doi: 10.2519/jospt.2013.4116. [DOI] [PubMed] [Google Scholar]
- 7.Distefano LJ, Blackburn JT, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther . 2009;39(7):532–540. doi: 10.2519/jospt.2009.2796. [DOI] [PubMed] [Google Scholar]
- 8.Krause DA, Jacobs RS, Pilger KE, Sather BR, Sibunka SP, Hollman JH. Electromyographic analysis of the gluteus medius in five weight-bearing exercises. J Strength Cond Res . 2009;23(9):2689–2694. doi: 10.1519/JSC.0b013e3181bbe861. [DOI] [PubMed] [Google Scholar]
- 9.Ayotte NW, Stetts DM, Keenan G, Greenway EH. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther . 2007;37(2):48–55. doi: 10.2519/jospt.2007.2354. [DOI] [PubMed] [Google Scholar]
- 10.Zeller BL, McCrory JL, Kibler WB, Uhl TL. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med . 2003;31(3):449–456. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]
- 11.Boudreau SN, Dwyer MK, Mattacola CG, Lattermann C, Uhl TL, McKeon JM. Hip-muscle activation during the lunge, single-leg squat, and step-up-and-over exercises. J Sport Rehabil . 2009;18(1):91–103. doi: 10.1123/jsr.18.1.91. [DOI] [PubMed] [Google Scholar]
- 12.Mauntel TC, Begalle RL, Cram TR, et al. The effects of lower extremity muscle activation and passive range of motion on single leg squat performance. J Strength Cond Res . 2013;27(7):1813–1823. doi: 10.1519/JSC.0b013e318276b886. [DOI] [PubMed] [Google Scholar]
- 13.Beutler AI, Cooper LW, Kirkendall DT, Garrett WE., II Electromyographic analysis of single-leg, closed chain exercises: implications for rehabilitation after anterior cruciate ligament reconstruction. J Athl Train . 2002;37(1):13–18. [PMC free article] [PubMed] [Google Scholar]
- 14.Bolgla L, Cook N, Hogarth K, Scott J, West C. Trunk and hip electromyographic activity during single leg squat exercises do sex differences exist? Int J Sports Phys Ther . 2014;9(6):756–764. [PMC free article] [PubMed] [Google Scholar]
- 15.Lubahn AJ, Kernozek TW, Tyson TL, Merkitch KW, Reutemann P, Chestnut JM. Hip muscle activation and knee frontal plane motion during weight bearing therapeutic exercises. Int J Sports Phys Ther . 2011;6(2):92–103. [PMC free article] [PubMed] [Google Scholar]
- 16.Berry JW, Lee TS, Foley HD, Lewis CL. Resisted side stepping: the effect of posture on hip abductor muscle activation. J Orthop Sports Phys Ther . 2015;45(9):675–682. doi: 10.2519/jospt.2015.5888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khuu A, Foch E, Lewis CL. Not all single leg squats are equal: a biomechanical comparison of three variations. Int J Sports Phys Ther . 2016;11(2):201–211. [PMC free article] [PubMed] [Google Scholar]
- 18.Khuu A, Lewis CL. Position of the non-stance leg during the single leg squat affects females and males differently. Hum Mov Sci . 2019;67:102506. doi: 10.1016/j.humov.2019.102506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Olivier B, Quinn SL, Benjamin N, Green AC, Chiu J, Wang W. Single-leg squat delicacies—the position of the nonstance limb is an important consideration. J Sport Rehabil . 2019;28(4):318–324. doi: 10.1123/jsr.2018-0181. [DOI] [PubMed] [Google Scholar]
- 20.Konrad P. The ABC of EMG a practical introduction to kinesiological electromyography. Noraxon; Published 2006. Accessed May 27, 2021. https://www.noraxon.com/wp-content/uploads/2014/12/ABC-EMG-ISBN.pdf . [Google Scholar]
- 21.Cappozzo A, Cappello A, Della Croce U, Pensalfini F. Surface-marker cluster design criteria for 3-D bone movement reconstruction. IEEE Trans Biomed Eng . 1997;44(12):1165–1174. doi: 10.1109/10.649988. [DOI] [PubMed] [Google Scholar]
- 22.Robertson DG, Dowling JJ. Design and responses of Butterworth and critically damped digital filters. J Electromyogr Kinesiol . 2003;13(6):569–573. doi: 10.1016/s1050-6411(03)00080-4. [DOI] [PubMed] [Google Scholar]
- 23.Bell AL, Brand RA, Pedersen DR. Prediction of hip joint centre location from external landmarks. Hum Mov Sci . 1989;8(1):3–16. doi: 10.1016/0167-9457(89)90020-1. [DOI] [Google Scholar]
- 24.Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng . 1993;115(4A):344–349. doi: 10.1115/1.2895496. [DOI] [PubMed] [Google Scholar]
- 25.Brody LT, Hall CM. Therapeutic Exercise Moving Toward Function 3rd ed. Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 26.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes . Mosby; 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waiteman MC, Briani RV, Pazzinatto MF, et al. Relationship between knee abduction moment with patellofemoral joint reaction force, stress and self-reported pain during stair descent in women with patellofemoral pain. Clin Biomech (Bristol Avon) . 2018;59:110–116. doi: 10.1016/j.clinbiomech.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Rutherford D, Baker M. Lateral to medial hamstring activation ratio: individuals with medial compartment knee osteoarthritis compared to asymptomatic controls during gait. Gait Posture . 2019;70:95–97. doi: 10.1016/j.gaitpost.2019.02.026. [DOI] [PubMed] [Google Scholar]
- 29.Lynn SK, Costigan PA. Changes in the medial-lateral hamstring activation ratio with foot rotation during lower limb exercise. J Electromyogr Kinesiol . 2009;19(3):e197–e205. doi: 10.1016/j.jelekin.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 30.Bourne MN, Williams MD, Opar DA, Al Najjar A, Kerr GK, Shield AJ. Impact of exercise selection on hamstring muscle activation. Br J Sports Med . 2017;51(13):1021–1028. doi: 10.1136/bjsports-2015-095739. [DOI] [PubMed] [Google Scholar]