Abstract
Introduction:
The impact of COVID-19 pandemics on cardiovascular diseases (CVD) may be caused by health system reorganization and/or collapse, or from changes in the behaviour of individuals. In Brazil, municipalities were empowered to define regulatory measures, potentially resulting in diverse effects on CVD morbimortality.
Objective:
To analyse the impact of COVID-19 pandemics on CVD outcomes in Belo Horizonte (BH), the sixth greater capital city in Brazil, including: mortality, mortality at home, hospitalizations, intensive care unit utilization, and in-hospital mortality; and the differential effect according to sex, age range, social vulnerability, and pandemic’s phase.
Methods:
Ecological study analysing data from the Mortality and Hospital Information System of BH residents aged ≥30 years. CVD was defined as in Chapter IX from ICD-10. Social vulnerability was classified by a composite socioeconomic index as high, medium and low. The observed age-standardized rates for epidemiological weeks 10–48, 2020, were compared to the expected rates (mean of 2015–2019). Risk ratios (RiR) were analysed and 95% confidence intervals were calculated for all estimates. Population projected to 2020 for BH and its census tracts were used to calculate rates.
Results:
We found no changes in CVD mortality rates (RiR 1.01, 95%CI 0.96–1.06). However, CVD deaths occurred more at homes (RiR 1.32, 95%CI 1.20–1.46) than in hospitals (RiR 0.89, 95%CI 0.79–0.99), as a result of a substantial decline in hospitalization rates, even though proportional in-hospital deaths increased. The rise in home deaths was greater in older adults and in had an increasing gradient in those more socially vulnerable (RiR 1.45); for high (RiR 1.45), medium (RiR 1.32) and low vulnerability (RiR 1.21).
Conclusion:
The greater occurrence of CVD deaths at home, in parallel with lower hospitalization rates, suggests that CVD care was disrupted during the COVID-19 pandemics, which more adversely affected older and more socially vulnerable individuals, exacerbating health inequities in BH.
Keywords: COVID-19, Cardiovascular Diseases, Mortality, Hospitalization, Social Vulnerability
Introduction
The COVID-19 pandemic had an indirect impact on cardiovascular diseases (CVD) care worldwide, resulting from reorganization of health systems, competing demands, and the change in populations’ behaviour that may have avoided contact with health facilities due to fear of contagion, or adherence to social distancing policies [1,2]. Previous studies have shown that excess mortality during the pandemic cannot be fully explained by COVID-19 deaths, and in some countries such as the US and the UK, CVD deaths increased in 2020 [3,4]. However, in other countries like Denmark, although more deaths at home were reported in individuals with CVD, overall mortality rates did not increase in the country during 2020 [5].
In Brazil, where nearly 200,000 excess deaths were reported in 2020 [6], CVD deaths also rose from March to June of 2020, in six capital cities, particularly in the least developed ones, in an analysis that evaluated preliminary mortality data [7]. However, due to the lack of national coordinated actions, the pandemic affected the country heterogeneously, leading to diverse death rates across the country, which peaked at different periods, and mostly affected socially vulnerable groups [6,8]. As a response to this lack of national coordination, each municipality had the power to implement local policies to mitigate the pandemic’s impact, including business and school closures, according to the pandemic course in their location [9].
Belo Horizonte is a city in Brazil with 2.5 million inhabitants, where local authorities daily monitored transmission rates and hospitalizations to guide regulatory measures, and although the city was able to delay the first pandemic wave in comparison to other capital cities – 1877 deaths due to COVID-19 occurred in 2020 [10,11], also mainly affecting the most vulnerable groups [9,12]. Moreover, during the 2020 pandemic period, CVD hospitalizations had a 16.3% decline, although the impact on CVD mortality has not been evaluated [13].
Because the effect of the pandemic on CVD depends on the pandemic course and behavioural changes in a location, a comprehensive analysis of the pandemic’s impact on CVD in a city is fundamental to guide future actions. As such, we aimed to analyse how the COVID-19 pandemic affected CVD deaths in a Brazilian city. To better understand the change in trends we investigated deaths, deaths at home, hospitalizations, ICU admissions and in-hospital mortality, and the differential impact of the pandemic on CVD according to sex, age group, social vulnerability, and the pandemic’s phase in the city.
Methods
Study design and Setting
This is an ecological, time-series study conducted in Belo Horizonte city, the 6th largest city in Brazil, with 2.5 million inhabitants, located in the Southeast region [14]. Brazil has a public universal health system (Unified Health System, Sistema Único de Saúde, SUS, in Portuguese), being consultations, hospitalizations, and most medications are free of charge to all Brazilian citizens [15], although 50% of Belo Horizonte residents have private health insurance [16]. During the COVID-19 pandemics, Belo Horizonte’s municipality composed a committee of specialists to address the pandemics issues and help local authorities to decide about the timely implementation of regulatory measures, following three daily indicators: transmission rate, and the proportion of occupied hospital and ICU beds [9]. Other actions taken by the municipality to confront the pandemic have been published [12]. We evaluated the effect of the pandemic from epidemiological weeks (EW) 10 to 48, 2020, on CVD outcomes in Belo Horizonte city following the STROBE guidelines for reporting observational studies [17].
Data Sources
We analyzed data on the number of deaths and deaths at home from the Mortality Information System (Sistema de Informação sobre Mortalidade, SIM, in portuguese). SIM is the official source of mortality data in the country and is qualified for causes of death. As such, good quality data can be analysed with a four-months delay from data extraction. SIM’s quality is rated four stars by the ‘The Global Burden of Disease’ study’s star rating system (0–5 stars) to assess the quality of cause of death data [18]. The numbers of hospital admissions, Intensive Care Unit (ICU) admissions and in-hospital deaths derive from the Hospital Information System (Sistema de Internações Hospitalares, SIH, in portuguese), which is also used for administrative purposes, including hospital payments, precluding underreporting. Over-reporting is also unlikely because hospitalizations data are audited for consistency. The SIH dataset included all public hospitalizations of the city, from which data for residents of Belo Horizonte were extracted. Previous SIH data quality checks revealed that, on average, after a three-months period of the hospitalization date, the completeness of data achieves 90% (Supplementary Material 1) [9]. Data from both systems were provided by the Belo Horizonte Health Department (Secretaria Municipal de Saúde, SMS, in portuguese). SIH data was extracted in March/2021 and SIM data in May/21. As such, the analysis was made including data until epidemiological week (EW) 48/2020. Datasets had census tract information that allowed analysis based on the Health Vulnerability Index (HVI), a social vulnerability index.
HVI is a census tract level health vulnerability index developed by Belo Horizonte Health Department based on sewage system and socioeconomic information [19]. The original HVI has four levels Low, Medium, High and Very High, but in the present work High and Very High categories were aggregated and further on named ‘High,’ to avoid small number of cases for specific cause’s analysis [19].
Because Brazil’s last available census was held in 2010, to estimate rates for 2020 at the municipal level and by HVI we used population estimates that applied growth rates estimated from a population projection developed by Freire et al. (2019) [20]. Population from census tracts with the same HVI was aggregated by age and sex, then age-specific growth rates for a ten-year period (2010 to 2020) estimated for Belo Horizonte was applied to each group of HVI population [14]. More detailed information has been previously published [9].
Definition of Causes and Measures
To have a comprehensive understanding of the pandemic’s impact on CVD, we examined outcomes for each of the following causes, by epidemiological week (EW), in adults ≥30 years: total CVD, defined as all records within Chapter IX (I00–I99) of the 10th International Classification of Diseases (ICD-10); Heart Failure (HF) (ICD-10 I50); Stroke (ICD-10 I60, I61, I62, I63, I64, I678); and Acute Coronary Syndrome (ACS) (ICD-10 I20, I21, I22, I23, I24) [21]. We additionally evaluated all records within Chapter XVIII (R00-R09) to better understand whether changes in the mortality patterns could be explained by changes in ill-defined codes, suggesting poorer quality of death certificates during the pandemics period.
For each CVD cause, seven measures were analyzed: death rates, death at home rates, hospitalization rates, Intensive Care Unit (ICU) admission rates, in-hospital death rates, and proportion of hospital admissions that resulted in ICU utilization or death. The cause of death was classified as the underlying cause, according to the World Health Organization protocols, and no analysis of multiple causes of death were performed [22]. Proportions of in-hospital deaths were defined as the ratio between the number registered for each variable and the total number of deaths during hospitalizations, considering each age group, sex and cause. All measures were age-standardized to the estimated population of Belo Horizonte in 2020, considering five-year age intervals. Measures for age groups (30–59; ≥60 years) were also standardized, considering the distribution of the population within these groups. In that sense, age specific rates (five years) were multiplied by the respective proportion of the population in the same age group and summed up. Data for total CVD was then analyzed stratified by sex, age groups (30–59 and ≥60 years), and according to vulnerability (high, medium and low HVI).
To investigate the effect of the pandemic course in the measures above described, we further analysed them according to the pandemic phase in the city, defined by the dates of the municipal decrees that regulated about social distancing measures, including business closures and reopening. The first phase comprises EW 10–21 and marks the beginning of the pandemic, when the city adopted its first distancing measures (EW 10) and the number of COVID-19 cases, hospitalizations and deaths were relatively low. In fact, the first confirmed COVID-19 case in the city occurred in EW 9. The second phase (EW 22–30) starts after the first gradual reopening of business facilities at EW 21, when the peak of COVID-19 occurred in Belo Horizonte in 2020, and the number of adverse events rose sharply. The third (EW 31–48) and last analyzed phase comprises the post-peak period, when the city gradually reopened at EW 31. This last phase ends at EW 48, when data of good quality was available, as previously stated [23].
Statistical Analysis
For each group (sex, age, cause, measure, vulnerability, and phase), the observed age-standardized rates and proportions for EW 10–48 in 2020 were compared to the expected measure, defined as the 2015 to 2019 corresponding mean. All rates were estimated considering the exposure time, allowing comparison between periods. The number of events in each period was divided by the fraction of the population of the corresponding number of weeks of exposure. Risk ratios (RiR) were calculated by dividing the observed by the expected values for each measure. We also calculated confidence intervals for all measures [24]. Confidence Intervals (CI) for rates and risk ratios were estimated from standard errors (SE) derived using the delta method, a technique that calculates SE from a logarithmic transformation that assures that the lower bond of the CI is positive, even in cases with high SE and low values for the rate or the RR. For proportions, CI were estimated based on the normal approximation to the binomial distribution.
For the time series analysis, the five-week moving averages of the studied variables from January to December 2020, were compared with the five-week moving averages of the previous period (January 2015 to December 2019). In the presented tables, the unsmoothed observed variables were compared to their unsmoothed mean for the same period from the 2015–2019 (EW 10–48). Analyses were performed using R, version 4.0.1 [25].
Ethical considerations
The study was approved by the Universidade Federal de Minas Gerais (UFMG) and SMS-BH Review Board (Protocol: CAAE 39778720.4.3001.5140). The data that support the findings of this study are publicly available at https://datasus.saude.gov.br/transferencia-de-arquivos/, and the steps to access the data described in a tutorial (Supplementary Material 2). However, the information on HVI, which is considered sensitive data, is not available and could only be provided after ethical approval.
Results
From EW 10–48, 2020, the all-cause age-standardized mortality rates rose from 911 to 1,075 per 100,000 inhabitants in Belo Horizonte. However, Table 1 reveals no excess mortality in the period for total CVD (RiR 1.0, CI 95% 0.96–1.06), even though there was a displacement in the place of death: while deaths at home increased (RiR 1.32, CI 95% 1.20–1.46), in-hospital mortality rates reduced (RiR 0.86, CI 95% 0.74–0.78), although the proportion of in-hospital mortality increased (RiR 1.16%, CI 95% 1.04–1.30). Looking at specific causes, for ACS and stroke there was no overall excess mortality, but ACS deaths occurred more at home, and were reduced in-hospital. For HF, mortality rates increased 32%, as a result of a significant 53% increase in deaths at home and no significant changes in in-hospital mortality. In parallel with these changes in mortality rates, total CVD hospitalizations rates decreased in the period, as did ICU admission rates, though the proportion of ICU utilization increased. For causes classified within the ICD Chapter XVIII, there was a reduction in mortality during the period, with non-significant changes in hospitalizations’ measures (Supplementary Material 3).
Table 1.
Age-standardized rates per 100,000 inhabitants or proportions and their 95% confidence intervals for cardiovascular disease outcomes observed in 2020 and expected (mean of 2015–2019) for epidemiological weeks 10–48, their absolute difference, and risk ratio with 95% confidence intervals. Belo Horizonte, MG, Brazil.
|
| ||||
|---|---|---|---|---|
| OBSERVED (95% CI) | EXPECTED(95% CI) | ABSOLUTE DIFFERENCE | RISK RATIO (95% CI) | |
|
| ||||
| Deaths | ||||
|
| ||||
| CVD | 247 (238;256) | 245 (236;254) | 2.0 | 1.01 (0.96;1.06) |
|
| ||||
| ACS | 41 (37;44) | 40 (37;44) | 0.2 | 1 (0.88;1.14) |
|
| ||||
| Stroke | 60 (56;65) | 61 (56;65) | –0.5 | 0.99 (0.89;1.1) |
|
| ||||
| HF | 24 (21;27) | 18 (15;20) | 5.9 | 1.32 (1.1;1.59)* |
|
| ||||
| Deaths at Home | ||||
|
| ||||
| CVD | 84 (78;89) | 63 (59;68) | 20.6 | 1.32 (1.2;1.46)* |
|
| ||||
| ACS | 10 (8;12) | 7 (6;9) | 2.8 | 1.38 (1.04;1.82)* |
|
| ||||
| Stroke | 9 (7;11) | 7 (6;9) | 1.7 | 1.22 (0.92;1.63) |
|
| ||||
| HF | 8 (7;10) | 5 (4;7) | 3.0 | 1.53 (1.12;2.1)* |
|
| ||||
| Hospital Admissions | ||||
|
| ||||
| CVD | 782 (766;799) | 1026 (1008;1045) | –244.0 | 0.76 (0.74;0.78)* |
|
| ||||
| ACS | 176 (169;184) | 222 (214;231) | –45.8 | 0.79 (0.75;0.84)* |
|
| ||||
| Stroke | 153 (146;160) | 148 (141;155) | 5.5 | 1.04 (0.97;1.11)* |
|
| ||||
| HF | 161 (154;169) | 168 (160;175) | –6.4 | 0.96 (0.9;1.02) |
|
| ||||
| ICU Admissions | ||||
|
| ||||
| CVD | 299 (289;309) | 341 (330;352) | –41.6 | 0.88 (0.84;0.92)* |
|
| ||||
| ACS | 127 (121;134) | 155 (148;163) | –28.4 | 0.82 (0.76;0.88)* |
|
| ||||
| Stroke | 48 (44;52) | 41 (37;45) | 7.4 | 1.18 (1.04;1.33)* |
|
| ||||
| HF | 45 (42;50) | 43 (39;47) | 2.8 | 1.06 (0.94;1.21) |
|
| ||||
| % ICU Admissions | ||||
|
| ||||
| CVD | 38 (37;39) | 33 (32;34) | 5.0 | 1.15 (1.1;1.21)* |
|
| ||||
| ACS | 72 (70;74) | 70 (68;71) | 2.1 | 1.03 (0.96;1.1) |
|
| ||||
| Stroke | 31 (29;33) | 27 (25;29) | 3.8 | 1.14 (1.01;1.29)* |
|
| ||||
| HF | 28 (26;30) | 25 (23;27) | 2.8 | 1.11 (0.98;1.25) |
|
| ||||
| In-Hospital Deaths | ||||
|
| ||||
| CVD | 49 (45;54) | 56 (51;60) | –6.3 | 0.89 (0.79;0.99) * |
|
| ||||
| ACS | 7 (5;8) | 9 (7;11) | –2.2 | 0.76 (0.57;1.01) |
|
| ||||
| Stroke | 16 (14;18) | 17 (14;19) | –0.7 | 0.96 (0.79;1.18) |
|
| ||||
| HF | 13 (11;15) | 12 (10;14) | 0.5 | 1.04 (0.83;1.31) |
|
| ||||
| % In-Hospital Deaths | ||||
|
| ||||
| CVD | 6 (5;6) | 5 (5;5) | 0.9 | 1.16 (1.04;1.3)* |
|
| ||||
| ACS | 4 (3;4) | 4 (3;5) | –0.2 | 0.96 (0.71;1.28) |
|
| ||||
| Stroke | 10 (9;12) | 11 (9;13) | –0.8 | 0.93 (0.76;1.13) |
|
| ||||
| HF | 8 (6;9) | 7 (6;8) | 0.6 | 1.08 (0.86;1.36) |
|
| ||||
ACS: acute coronary syndrome, CI: confidence intervals, CVD: cardiovascular disease, HF: heart failure, ICU: intensive care unit.
Table 2 shows the risk ratios and their 95% confidence intervals for total CVD in subgroup analysis. Regarding sex-stratified analysis, no differences between men and women were found, except that the increase in proportions of ICU utilization and in-hospital mortality were only significant for women. The analysis by age groups revealed that the increase in home deaths was only significant for older adults (≥60y). Of note, mortality rates were found to be at least ten times higher in the older age group, what may have precluded finding statistical significance in the younger group, for which the direction of changes were the same as for the older age group (Supplementary Material 4).
Table 2.
Risk ratios for total cardiovascular disease outcomes and their 95% confidence intervals in subgroup analysis, according to sex, age group, health vulnerability, and pandemic phase, in Belo Horizonte, Brazil, from epidemiological weeks 10–48, 2020, compared to the mean of epidemiological weeks 10–48, 2015–2019.
|
| ||||||||
|---|---|---|---|---|---|---|---|---|
| DEATHS | DEATHS AT HOME | % DEATHS AT HOME | HOSP. ADMISSIONS | ICU | % ICU | IN-HOSPITAL DEATHS | % IN-HOSPITAL DEATHS | |
|
| ||||||||
| Sex | ||||||||
|
| ||||||||
| Female | 0.98 (0.91;1.06) | 1.35 (1.17;1.56)* | 1.35 (1.17;1.56)* | 0.69 (0.66;0.72)* | 0.87 (0.81;0.94)* | 1.26 (1.17;1.35)* | 0.86 (0.73;1.02) | 1.2(1.02;1.42)* |
|
| ||||||||
| Male | 1.04 (0.97;1.11) | 1.29 (1.13;1.47)* | 1.27 (1.11;1.44)* | 0.84 (0.81;0.87)* | 0.88 (0.83;0.94)* | 1.05 (0.99;1.12) | 0.91 (0.78;1.06) | 1.14(0.98;1.32) |
|
| ||||||||
| Age Groups | ||||||||
|
| ||||||||
| 30–59 | 0.91 (0.79;1.04) | 1.09 (0.85;1.4) | 1.2 (0.93;1.54) | 0.66 (0.63;0.69)* | 0.86 (0.79;0.92)* | 1.29 (1.19;1.39)* | 0.8(0.63;1.01) | 1.2(0.95;1.53) |
|
| ||||||||
| 60+ | 1.03 (0.97;1.09) | 1.37 (1.23;1.52)* | 1.33 (1.2;1.48)* | 0.83 (0.8;0.86)* | 0.89 (0.84;0.94)* | 1.07 (1.01;1.14)* | 0.91(0.8;1.04) | 1.1(0.97;1.25) |
|
| ||||||||
| Vulnerability | ||||||||
|
| ||||||||
| Low | 0.95 (0.86;1.05) | 1.21 (1.01;1.45)* | 1.25 (1.04;1.49)* | 0.72 (0.67;0.78)* | 0.82 (0.73;0.92)* | 1.12 (0.99;1.26) | 1.02(0.76;1.38) | 1.32(0.98;1.79) |
|
| ||||||||
| Medium | 1.01 (0.93;1.09) | 1.32 (1.13;1.53)* | 1.32 (1.13;1.53)* | 0.76 (0.73;0.79)* | 0.89 (0.83;0.95)* | 1.18 (1.1;1.26)* | 0.88 (0.75;1.03) | 1.2(1.03;1.41)* |
|
| ||||||||
| High | 1.04 (0.94;1.14) | 1.45 (1.21;1.74)* | 1.41 (1.17;1.69)* | 0.81 (0.78;0.85)* | 0.9 (0.84;0.97)* | 1.13 (1.05;1.21)* | 0.82 (0.69;0.99)* | 1.13(0.95;1.36) |
|
| ||||||||
| Pandemic Phase | ||||||||
|
| ||||||||
| 1° Period | 1.01 (0.92;1.12) | 1.37 (1.15;1.63)* | 1.35 (1.13;1.6)* | 0.77 (0.73;0.81)* | 1.03 (0.95;1.12) | 1.34 (1.24;1.45)* | 0.87(0.7;1.06) | 1.12(0.91;1.38) |
|
| ||||||||
| 2° Period | 0.96 (0.86;1.06) | 1.35 (1.11;1.63)* | 1.4 (1.16;1.7)* | 0.75 (0.71;0.8)* | 0.8 (0.73;0.89)* | 1.07 (0.97;1.18) | 0.81 (0.64;1.02) | 1.07(0.85;1.36) |
|
| ||||||||
| 3° Period | 1.03 (0.95;1.12) | 1.28 (1.1;1.48)* | 1.24 (1.07;1.44)* | 0.76 (0.73;0.8)* | 0.82 (0.76;0.87)* | 1.07 (1;1.14) | 0.95(0.8;1.11) | 1.24(1.05;1.46)* |
|
| ||||||||
ICU: intensive care unit.
In the analysis according to social vulnerability groups, the rise in deaths at home during the 2020 pandemic period occurred in the three HVI groups, but with an increasing gradient from the low to medium, and high vulnerability groups, as also depicted in Figure 1.
Figure 1.
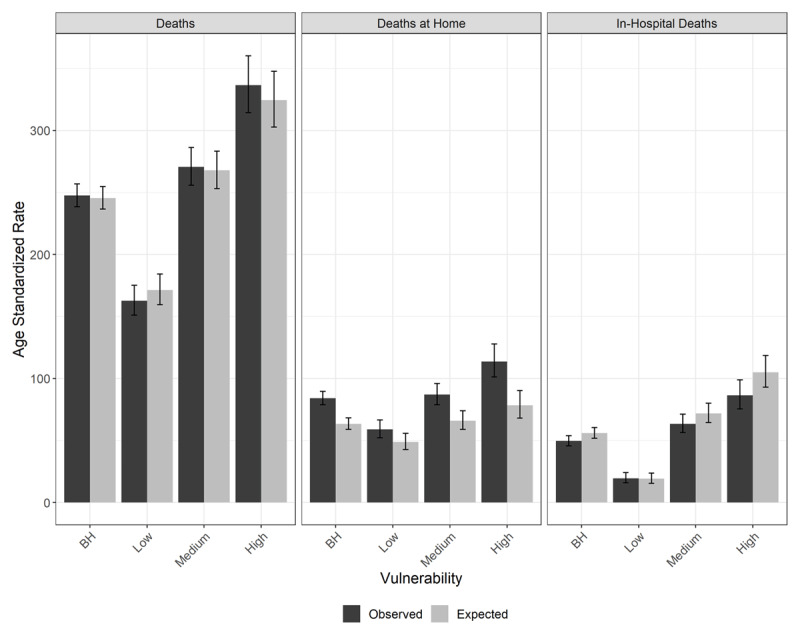
Age-standardized death, death at home, and in-hospital death rates per 100,000 inhabitants, for cardiovascular diseases, observed in 2020 and expected (mean of 2015–2019) for epidemiological weeks 10–48, with 95% confidence intervals. Belo Horizonte, MG, Brazil.
Lastly, Figure 2 and Table 2 reveals that there was in increase in deaths at home in all pandemic phases during the analysed period. However, the profile of hospitalizations suggests different drivers for the excess mortality at home: while there was a decrease for hospitalization in all phases, ICU admission rates only decreased in the second and third phases, possibly due to competing demands. In fact, the proportion of ICU utilization increased in the first period of the pandemic.
Figure 2.
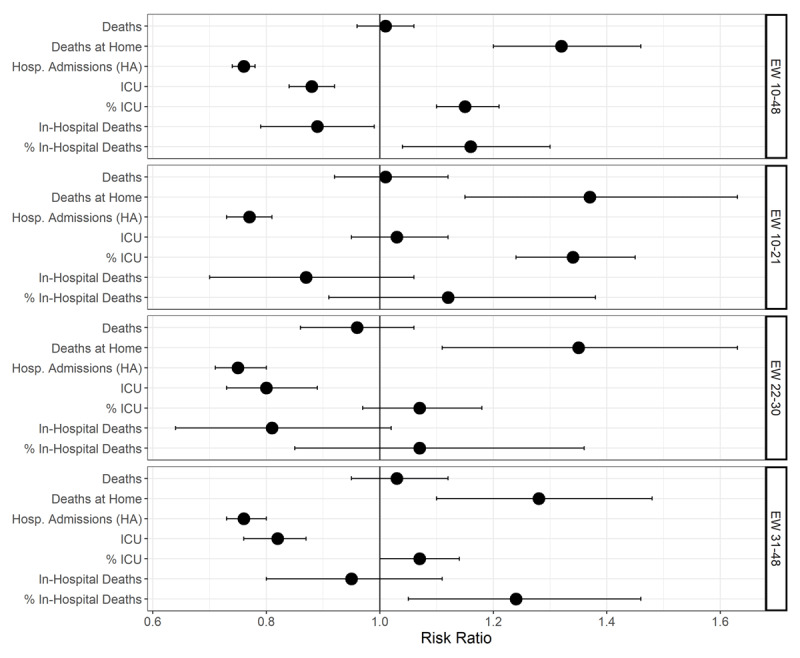
Risk ratios expected (mean of 2015–2019) and observed in 2020 for age-standardized rates per 100,000 inhabitants or proportions for cardiovascular disease outcomes for epidemiological weeks 10–48. Belo Horizonte, MG, Brazil.
Discussion
During the 2020 pandemic period, CVD deaths did not increase in Belo Horizonte, although there was a displacement of deaths, which occurred more at homes than at hospitals, even though the proportion of in-hospital deaths increased. These results suggest that there was a deferral of CVD care in hospitals, with higher in-hospital lethality, possibly due to greater clinical severity of hospitalized patients, or less adherence to evidence–based treatments because of disrupted pathways of care and overwhelmed hospitals. Importantly, this unfavorable impact on CVD care in the city was differential, mainly affecting older adults, and with an increasing trend in the more socially vulnerable groups, widening health gaps. Moreover, the changes in the location of deaths occurred during the whole 2020 pandemic period, although hospitalization and ICU utilization patterns suggest that these changes may have been led by different drivers: avoidance of hospitals at the first phase, and additional competition for beds in the second and third phases. Taken together, our study brings essential information for preparing the local health system for future waves of this or different pandemics, and to plan actions to mitigate the rebound effect resulting from the disrupted CVD care in the city.
Previous studies have shown an indirect effect of the COVID-19 pandemic in CVD care. First, studies revealed a reduction in hospitalizations, procedures, and/or consultations for CVD in high [26,27,28,29,30], and low-and middle income countries (LMIC) [31,32], then an increase in out-of-hospital deaths [33,34]. Moreover, a rise in the proportion of in-hospital mortality for CVD was reported, being this effect larger where greater decline in admission rates occurred, suggesting hospitalizations of sicker patients or delivery of worse quality of care, corroborating our findings [35,36]. In parallel, other studies revealed that excess mortality in the pandemic period could not be explained exclusively by COVID-19 deaths, and excess CVD deaths was found in some countries, including Brazil, which is not surprising, knowing the beneficial effect of in-hospital timely treatment for the most lethal cardiovascular conditions, such as ACS [37,38,39].
However, even though the effect of the pandemics in CVD deaths had already been investigated in six Brazilian capital cities, the findings could not be extended to Belo Horizonte due to the heterogeneity of the pandemics in Brazil. The cited study revealed that the cardiovascular mortality increase during the pandemics was of greater magnitude in the less developed cities, where a health system collapse occurred [7]. Moreover, the effect of mitigation policies or the differential impact according to individual-level factors, both fundamental to guide health policies, needed to be investigated.
In our analysis in Belo Horizonte, CVD death rates did not increase in the period. This finding could be attributed to Belo Horizonte having a smaller incidence of COVID-19 – and as a result, a lower overall impact of the pandemics compared to other Brazilian cities – or a better organization of the health system to cope with competing demands [11]. In fact, previous studies in the US and Brazil, showed that deaths from CVD increased more during the pandemics in areas of higher incidence of COVID-19 [2,7]. In addition, the health system collapse described in other Brazilian cities, such as Manaus, did not occur in Belo Horizonte in 2020 [11]. However, when we comprehensively analyze other cardiovascular outcomes in Belo Horizonte, we clearly found a disruption of CVD care in the city, with a rise in deaths at home – also seen in other countries [5,40], and significant declines in hospitalizations and in-hospital deaths, even though there was a rise in the proportion of in-hospital mortality for CVD. Looking at this overall pattern of CVD outcomes during the period in Belo Horizonte, an alternative for not finding an increase in CVD death rates may be lack of power to detect differences during the studied period. Importantly, individuals living with CVD are at increased risk of death due to COVID-19, and thus there may be an effect of competitive causes for this group in the pandemics period between COVID-19 and CVD deaths [41].
To further understand the effect on CVD care, we stratified the analysis by the main causes of cardiovascular death or hospitalization in the country, and interestingly we found more adverse effect on the mortality by HF, compared to ACS and stroke. Of note, not only deaths at home increased for HF in greater magnitude, but also the overall HF death rate rose. This finding contrasts with data from the US, where excess deaths for ischemic and hypertensive diseases were responsible for CVD excess mortality, and no increase in deaths by heart failure was observed, leading the authors to describe a potential bigger unfavorable effect on acute cardiovascular conditions [2]. However, this may differ in Brazil, where the care of chronic CVD may have been more adversely affected. During the early 2020 pandemic period, although the PHC centers designed protocols for attending the patient with CVD [42], any contact with the health system was, in fact, discouraged by national authorities, particularly for older individuals, what may have resulted in the decompensation of individuals living with HF [43]. A survey conducted in April and May, 2020, with 45,000 Brazilian adults, revealed a decrease in health services’ demand, and a reported difficulty in scheduling exams, consultations, elective hospitalization, and procedures, reflecting the ‘stay at home’ order from the first pandemics’ phase, as well as the fear of contracting COVID-19 [44]. Indeed, our study showed that hospitalizations for HF did not decline in the period, suggesting that HF decompensation were still highly demanding hospitals. Alternatively, HF may have been assigned as cause of death in the absence of a more specific diagnosis, harder to make at home or early after a hospital admission due to the lack of diagnostic tools.
Importantly, our study corroborates previous data from Brazil and other countries, which reveal that the pandemic exacerbated health inequities [6,9,45,46]. More excess mortality and COVID-19 confirmed deaths have been reported in the most vulnerable groups, according to race or neighbourhood [4,6,9]. Herein, we additionally describe that the adverse impact of the pandemic on CVD was also greater in the most vulnerable individuals: deaths at home presented an increasing trend from groups of low to high health vulnerability. This finding depicts the inequality chain in which the most vulnerable individuals live, with higher prevalence of unhealthy behaviours and cardiovascular risk factors, such as obesity and hypertension, which lead to higher prevalence of CVD [47,48]. Besides that, although Brazil has a universal healthcare system and the quality of PHC in Belo Horizonte has been rated as one of the best in the countries’ capital cities [11], PHC was not promptly adapted to deliver care for CVD in the pandemic context, as already described. Moreover, gaps in accessibility exist, such as having more public hospitals located in the less vulnerable areas of the city – a disadvantage for the treatment of time-dependent conditions, such as ACS, for those living in more vulnerable areas [39]. Additionally, other barriers to CVD care for more socially vulnerable groups may include impaired access to information, and to alternative pathways of care, such as telemedicine [49]. From a macro-level perspective, lower education, health literacy, and economic constraints may have also been determinants of lower access to health care to the most vulnerable, reinforcing disparities [50].
Our study has limitations. Because COVID-19 tests were not widely available in the community setting, out-of-hospital deaths may have been misdiagnosed, either over or underestimated deaths by CVD. Moreover, quality of death certificates may have worsen during the pandemic [51]. However, no changes in the pattern of deaths under ICD-10 Chapter XVIII, which includes ill-defined causes of deaths, was found in our analysis, suggesting that this was not a major issue. Importantly, because our aim was to understand the indirect impact of the pandemic on CVD, we did not include in the present analysis the cardiovascular deaths related to COVID-19. As such, if COVID-19 was considered the underlying cause of death according to the World Health Organization protocols, and there was an associated cardiovascular outcome in the death certificate, this outcome was not included in the present analysis [22,52], as it would require an analysis of multiple causes of death [52]. Another limitation refers to the fact that only public hospitalizations were analysed, due to availability of data. However, there was no substantial changes in the number of individuals with private health insurance in the city during the period [16]. While the definition of out-of-hospital cause of death was described as a potential limitation, the same does not occur for in-hospital mortality, as hospitalizations for COVID-19 had to be confirmed by laboratory tests (RT-PCR or serology) that, although not widely available at the community level, were available for in-hospital diagnosis in Belo Horizonte [53,54].
The strengths of our analysis include a thorough analysis of data quality that supported our decision to only include information until EW 48, to minimize the effect of reporting delays. Moreover, the age standardization of data was fundamental to reveal the difference among the HVI groups, since the higher the HVI, the greater is the proportion of younger individuals, masking the larger increase in mortality in the most vulnerable groups, if crude mortality rates were used [9]. Lastly, the comprehensive analysis of the pandemic’s impact on CVD with a focus in a city allowed us to understand the effect of the pandemic course, including that of mitigation policies.
Taken together, our analysis brings important messages for health professionals and stakeholders: tools to preclude disruption of CVD care must be developed and implemented during a health crisis. Alternative pathways of care, such as homecare, active search, telemedicine, digital health tools, or reorganization of PHC centres to partly devote them to chronic diseases management are options to keep track of chronic patients and stimulate the continuation of treatment [49,50,55]. Enhancement of educational campaigns to increase recognition of acute CVD symptoms, highlighting the importance of seeking emergency medical services in their presence are another essential strategy [5]. Additionally, health promotion should also be emphasized to counteract the increase of unhealthy behaviours that occurred during the pandemics, if we intend to mitigate the deleterious effect on cardiovascular health in the years to come. A Brazilian national survey found an increase in the prevalence of sedentary behaviour, smoking, consumption of alcohol, and ultra-processed foods during EW 18–22/2020, compared with the pre-pandemic period [56,57,58]. From the societal perspective, investments in social protection policies and education are essential to break the chain of inequalities. Presently, the health system will also have the challenge of adapting itself to the ‘rebound’ effect, prioritizing hospitalizations for cardiovascular elective procedures to catch up with the demand of procedures that were cancelled, and developing strategies to reassume care of patients with chronic CVD, particularly the most vulnerable.
Conclusion
During the 2020 COVID-19 pandemic period, CVD care was disrupted in Belo Horizonte city. CVD deaths were displaced to homes instead of hospitals during the period, concomitantly with a decrease in hospitalizations, suggesting that there was a deferral of hospital care for CVD. This unfavourable impact of COVID-19 pandemic was greater for older adults, and the most socially vulnerable group, exacerbating health inequalities in the city.
Additional Files
The additional files for this article can be found as follows:
Percent of hospital admissions processed in each month from the total of admissions in the respective month in 2019 and 2020, Hospital Information System, Belo Horizonte, MG, Brazil.
Tutorial to access data.
Age-standardized rates per 100,000 inhabitants and proportions for ICD Chapter XVIII outcomes observed in 2020, and expected (mean of 2015–2019), for epidemiological weeks 10–48, their absolute difference, and risk ratio. Belo Horizonte MG, Brazil.
Age-standardized rates per 100,00 inhabitants and proportions for cardiovascular disease outcomes observed in 2020, and expected (mean of 2015-2019) for epidemiological weeks 10–48, their absolute difference, and risk ratio, according to age range. Belo Horizonte, MG, Brazil.
Funding Statement
Dr Ribeiro is supported in part by CNPq (310679/2016-8 and 465518/2014-1), by FAPEMIG (PPM-00428-17 and RED-00081-16) and CAPES (88887.507149/2020-00). Deborah C Malta is partially financed by CNPq (CNPQ – 310177/2020-0). The project is financed by the Global Grants Program (GGP-30), Vital Strategies, São Paulo, SP, Brazil.
Funding Information
Dr Ribeiro is supported in part by CNPq (310679/2016-8 and 465518/2014-1), by FAPEMIG (PPM-00428-17 and RED-00081-16) and CAPES (88887.507149/2020-00). Deborah C Malta is partially financed by CNPq (CNPQ – 310177/2020-0). The project is financed by the Global Grants Program (GGP-30), Vital Strategies, São Paulo, SP, Brazil.
Competing interests
The authors have no competing interests to declare.
Author contributions
Brant, LC designed the work; supervised the data analysis and interpretation, and drafted the first version of the manuscript; Passos VMA designed the work; supervised the data analysis and interpretation, and critically revised the manuscript; Machado, IE; Correa PR; Santos MR; Malta DC; Ribeiro, ALP designed the work and collaborated in and data acquisition and interpretation, and critically revised the manuscript; Pinheiro, PC designed the work and did the statistical analysis, Souza MFM collaborated in the design of the work, in the interpretation of data, and critically revised the manuscript; and all authors approved this version of the manuscript.
References
- 1.Banerjee A, Chen S, Pasea L, et al. Excess Deaths in People with Cardiovascular Diseases during the COVID-19 Pandemic. Eur J Prev Cardiol. 2021; zwaa155. DOI: 10.1093/eurjpc/zwaa155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular Deaths During the COVID-19 Pandemic in the United States. J Am Coll Cardiol. 2021; 77(2): 159–69. DOI: 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmad FB, Anderson RN. The Leading Causes of Death in the US for 2020. JAMA. 2021; 325(18): 1829–30. DOI: 10.1001/jama.2021.5469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kontopantelis E, Mamas MA, Webb RT, et al. Excess Deaths from COVID-19 and Other Causes by Region, Neighbourhood Deprivation Level and Place of Death During the First 30 Weeks of the Pandemic in England and Wales: A Retrospective Registry Study. Lancet Reg Health Eur. 2021; 7: 100144. DOI: 10.1016/j.lanepe.2021.100144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butt JH, Fosbøl EL, Gerds TA, et al. All-Cause Mortality and Location of Death in Patients with Established Cardiovascular Disease Before, During, and After the COVID-19 Lockdown: A Danish Nationwide Cohort Study. Eur Heart J. 2021; 42(15): 1516–23. DOI: 10.1093/eurheartj/ehab028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marinho MF, Torrens A, Teixeira R, et al. Racial Disparity in Excess Mortality in Brazil During COVID-19 Times. Eur J Public Health. 2021; ckab097. DOI: 10.1093/eurpub/ckab097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brant LCC, Nascimento BR, Teixeira RA, et al. Excess of Cardiovascular Deaths During the COVID-19 Pandemic in Brazilian Capital Cities. Heart. 2020; 106(24): 1898–905. DOI: 10.1136/heartjnl-2020-317663 [DOI] [PubMed] [Google Scholar]
- 8.Baqui P, Bica I, Marra V, Ercole A, van der Schaar M. Ethnic and Regional Variations in Hospital Mortality from COVID-19 in Brazil: A Cross-Sectional Observational Study. Lancet Glob Health. 2020; 8(8): 1018–26. DOI: 10.1016/S2214-109X(20)30285-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Passos VMA, Brant LCC, Pinheiro PC, et al. Higher Mortality During the COVID-19 Pandemic in Socially Vulnerable Areas in Belo Horizonte: Implications for Vaccine Prioritization. Rev Bras Epidemiol. 2021; 24: e210025. DOI: 10.1590/1980-549720210025 [DOI] [PubMed] [Google Scholar]
- 10.Universidade Federal de Pelotas. EPICOVID19. Pelotas: UFPel; 2020. Retrieved from: http://epidemio-ufpel.org.br/uploads/downloads/19c528cc30e4e5a90d9f71e56f8808ec.pdf. (assessed 01 October 2021). [Google Scholar]
- 11.Guedes MBOG, Assis SJC, Sanchis GJB, Araujo DN, Oliveira AGRDC, Lopes JM. COVID-19 in Brazilian Cities: Impact of Social Determinants, Coverage and Quality of Primary Health Care. PLoS One. 2021; 16(9): e0257347. DOI: 10.1371/journal.pone.0257347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belo Horizonte (MG). Coronavírus [Internet]. Belo Horizonte: Prefeitura de Belo Horizonte; 2021. Retrieved from: https://prefeitura.pbh.gov.br/saude/coronavirus. (assessed 23 June 2021).
- 13.Dias RR, Santiago JAD, Madrini V, Jr., Mady C, Jatene FB. Impact of COVID-19 Pandemic in a Brazilian High-Volume Aortic Center. Braz J Cardiovasc Surg. 2021; 36(2): 145–19. DOI: 10.21470/1678-9741-2020-0567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Instituto Brasileiro de Geografia e Estatística. Belo Horizonte: Panorama [Internet]. Rio de Janeiro: IBGE; c2021. Retrieved from: https://cidades.ibge.gov.br/brasil/mg/belo-horizonte/panorama. (assessed 01 October 2021). [Google Scholar]
- 15.Ribeiro ALP, Duncan BB, Brant LC, Lotufo PA, Mill JG, Barreto SM. Cardiovascular health in Brazil: Trends and perspectives. Circulation. 2016; 133(4): 422–33. DOI: 10.1161/CIRCULATIONAHA.114.008727 [DOI] [PubMed] [Google Scholar]
- 16.Agência Nacional de Saúde Suplementar (Brazil) [Internet]. Brasília, DF: Agência Nacional de Saúde Suplementar; 2021. [cited 2021 Jun 23]. Retrieved from: https://www.gov.br/ans/pt-br. (assessed 23 June 2021). [Google Scholar]
- 17.Malta M, Cardoso LO, Bastos FI, Magnanini MM, Silva CM. STROBE Initiative: Guidelines on Reporting Observational Studies. Rev Saude Publica. 2010; 44(3): 559–65. DOI: 10.1590/S0034-89102010000300021 [DOI] [PubMed] [Google Scholar]
- 18.GBD 2016 Brazil Collaborators. Burden of Disease in Brazil, 1990–2016: A Systematic Subnational Analysis for the Global Burden of Disease Study 2016. Lancet. 2018; 392(10149): 760–75. DOI: 10.1016/S0140-6736(18)31221-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belo Horizonte (MG). Índice de Vulnerabilidade da Saúde (IVS-BH). Belo Horizonte: Prefeitura de Belo Horizonte; 2018. Retrieved from: https://prefeitura.pbh.gov.br/estatisticas-e-indicadores/indice-de-vulnerabilidade-da-saude. (assessed 02 October 2021). [Google Scholar]
- 20.Freire FHMA, Gonzaga MR, Queiroz BL. Projeção Populacional Municipal com Estimadores Bayesianos, Brasil 2010–2030. In: Sawyer DO (ed.), Seguridade Social Municipais: Projeto Brasil 3 Tempos. Brasília: Secretaria Especial de Assuntos Estratégicos da Presidência da República; 2019. [Google Scholar]
- 21.Centers for Disease Control and Prevention. International Classification of Diseases (ICD 10). Herndon: National Center for Health Statistics; 2020. [Google Scholar]
- 22.World Health Organization. International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. 2nd ed. Geneva: WHO Library; 2004. [Google Scholar]
- 23.Belo Horizonte (MG). Reabertura Gradual de Atividades e Protocolos de Funcionamento: Decretos [Internet]. Belo Horizonte: Prefeitura de Belo Horizonte; 2021. Retrieved from: https://prefeitura.pbh.gov.br/reabertura-de-atividades. (assessed 02 October 2021). [Google Scholar]
- 24.Kirkwood BR, Sterne J. Essential Medical Statistics. 2nd ed. Hoboken: Blackwell Publishers; 2003. [Google Scholar]
- 25.R Foundation. The R Project for Statistical Computing [Internet]. Vienna: R Development Core Team; 2014. Retrieved from: https://www.r-project.org/foundation/. (assessed 02 October 2021). [Google Scholar]
- 26.De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020; 383(1): 88–9. DOI: 10.1056/NEJMc2009166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew NWS, Ow ZGW, Teo VXY, et al. The Global Impact of the COVID-19 Pandemic on STEMI Care: A Systematic Review and Meta-Analysis. Can J Cardiol. 2021; 37: 1450–59. DOI: 10.1016/j.cjca.2021.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohamed MO, Banerjee A, Clarke S, et al. Impact of COVID-19 on Cardiac Procedure Activity in England and Associated 30-Day Mortality. Eur Heart J Qual Care Clin Outcomes. 2021; 7(3): 247–56. DOI: 10.1093/ehjqcco/qcaa079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhatt AS, Moscone A, McElrath EE, et al. Fewer Hospitalizations for Acute Cardiovascular Conditions During the COVID-19 Pandemic. J Am Coll Cardiol. 2020; 76(3): 280–8. DOI: 10.1016/j.jacc.2020.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wosik J, Clowse MEB, Overton R, et al. Impact of the COVID-19 Pandemic on Patterns of Outpatient Cardiovascular Care. Am Heart J. 2021; 231: 1–5. DOI: 10.1016/j.ahj.2020.10.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Normando PG, Araujo-Filho JA, Fonseca GA, et al. Reduction in Hospitalization and Increase in Mortality Due to Cardiovascular Diseases During the COVID-19 Pandemic in Brazil. Arq Bras Cardiol. 2021; 116(3): 371–80. DOI: 10.36660/abc.20200821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tam CF, Cheung KS, Lam S, et al. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak on ST-Segment-Elevation Myocardial Infarction Care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020; 13(4): e006631. DOI: 10.1161/CIRCOUTCOMES.120.006631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baldi E, Sechi GM, Mare C, et al. Out-of-Hospital Cardiac Arrest During the Covid-19 Outbreak in Italy. N Engl J Med. 2020; 383(5): 496–8. DOI: 10.1056/NEJMc2010418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guimarães NS, Carvalho TML, Machado-Pinto J, et al. Increased Home Death Due to Cardiopulmonary Arrest in Times of COVID-19 Pandemic. Arq Bras Cardiol. 2021; 116(2): 266–71. DOI: 10.36660/abc.20200547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cannata A, Watson SA, Daniel A, et al. Impact of the COVID-19 Pandemic on In-Hospital Mortality in Cardiovascular Disease: A Meta-Analysis. Eur J Prev Cardiol. 2021; zwab119. DOI: 10.1093/eurjpc/zwab119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rattka M, Dreyhaupt J, Winsauer C, et al. Effect of the COVID-19 Pandemic on Mortality of Patients with STEMI: A Systematic Review and Meta-Analysis. Heart. 2021; 107(6): 482–487. DOI: 10.1136/heartjnl-2020-318360 [DOI] [PubMed] [Google Scholar]
- 37.Sanmarchi F, Golinelli D, Lenzi J, et al. Exploring the Gap Between Excess Mortality and COVID-19 Deaths in 67 Countries. JAMA Netw Open. 2021; 4(7): e2117359. DOI: 10.1001/jamanetworkopen.2021.17359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L. Excess Deaths From COVID-19 and Other Causes, March–April 2020. JAMA. 2020; 324(5): 510–3. DOI: 10.1001/jama.2020.11787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cosentino N, Bartorelli AL, Marenzi G. Time to Treatment Still Matters in ST-Elevation Myocardial Infarction: A Call to Maintain Treatment Effectiveness during the COVID-19 Pandemic. Eur Heart J Cardiovasc Pharmacother. 2020; 6(6): 408–9. DOI: 10.1093/ehjcvp/pvaa054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu J, Mamas MA, Mohamed MO, et al. Place and Causes of Acute Cardiovascular Mortality During the COVID-19 Pandemic. Heart. 2021; 107(2): 113–119. DOI: 10.1136/heartjnl-2020-317912 [DOI] [PubMed] [Google Scholar]
- 41.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors Associated with COVID-19-Related Death Using OpenSAFELY. Nature. 2020; 584(7821): 430–6. DOI: 10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Belo Horizonte (MG). Proposta para Acompanhamento de Usuários com Condições Crônicas na APS, no Contexto da Pandemia pelo Vírus da SARS-CoV-2. Belo Horizonte: Prefeitura de Belo Horizonte; 2020. [Google Scholar]
- 43.Secretaria de Atenção Primária à Saúde. Nota Técnica N° 6/2020-COSAPI/CGCIVI/DAPES/SAPS/MS. Brasília: Ministério da Saúde; 2020. [Google Scholar]
- 44.Malta DC, Gomes CS, Silva AGD, et al. Use of Health Services and Adherence to Social Distancing by Adults with Noncommunicable Diseases During the COVID-19 Pandemic, Brazil, 2020. Cien Saude Colet. 2021; 26(7): 2833–42. DOI: 10.1590/1413-81232021267.00602021 [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization. Health Inequity and the Effects of COVID-19. Geneva: WHO; 2020. [Google Scholar]
- 46.Center for Disease Control and Prevent. Health Equity Considerations and Racial and Ethnic Minority Groups [Internet]. Atlanta: CDC; c2021. Retrieved from: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. (assessed 02 October 2021). [Google Scholar]
- 47.Malta DC, Campos MO, Oliveira MM, et al. Noncommunicable chronic disease risk and protective factor prevalence among adults in Brazilian state capital cities, 2013. Epidemiol Serv Saúde. 2015; 24(3): 373–87. DOI: 10.5123/S1679-49742015000200006 [DOI] [Google Scholar]
- 48.Nascimento BR, Brant LCC, Yadgir S, et al. Trends in Prevalence, Mortality, and Morbidity Associated with High Systolic Blood Pressure in Brazil from 1990 to 2017: Estimates from the ‘Global Burden of Disease 2017’ (GBD 2017) Study. Popul Health Metr. 2020; 18(Suppl 1): 17. DOI: 10.1186/s12963-020-00218-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic: Bridging or Opening the Digital Divide? Circulation. 2020; 142(5): 510–2. DOI: 10.1161/CIRCULATIONAHA.120.048185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.NCD Alliance. A Global NCD Agenda for Resilience and Recovery from COVID-19. Geneva: NCD Alliance; 2021. [Google Scholar]
- 51.Lopes R, Vargas M. Mortes por Causas Mal Definidas Saltam 30% na Pandemia de Covid. Folha de S.Paulo [Internet]. 25 September 2021. Retrieved from: https://www1.folha.uol.com.br/equilibrioesaude/2021/09/mortes-por-causas-mal-definidas-cresce. (assessed 01 October 2021).
- 52.Laurenti R, Jorge MHPM, Gotlieb SLD. Mortality information: the use of international rules for the selection of the underlying cause. Rev Bras Epidemiol. 2009; 12(2): 195–203. DOI: 10.1590/S1415-790X2009000200009 [DOI] [Google Scholar]
- 53.Minas Gerais (Brazil). Secretaria de Estado de Saúde. Plano Estadual de Contingência para Emergência em Saúde: Infecção Humana pelo SARS-CoV-2 (doença pelo coronavirus – COVID-2019). Belo Horizonte: Secretaria de Estado de Saúde; 2020. Retrieved from: https://coronavirus.saude.mg.gov.br/images/2021/09/Plano_de_Contingencia_-_Revisao_3_-_03_09_2021.pdf. (assessed 23 June 2021). [Google Scholar]
- 54.Brazil. Ministério da Saúde. Portaria no 245, de 24 de março de 2020. Inclui procedimento na Tabela de Procedimentos, Medicamentos, Órteses, Próteses e Materiais Especiais (OPM) do Sistema Único de Saúde (SUS), para Atendimento Exclusivo de Pacientes com Diagnóstico de Infecção pelo COVID-19 […]. Brasília, DF, Diário Oficial da União. 30 April 2020. Retrieved from: https://www.in.gov.br/en/web/dou/-/portaria-n-245-de-24-de-marco-de-2020-*-254675204. (assessed 23 June 2021). [Google Scholar]
- 55.Pinto FJ, Piñeiro D, Banerjee A, Perel P, Pervan B, Eiselé JL. World Heart Day 2021: COVID-19, Digital Health, and Tackling Cardiovascular Disease. Lancet; 2021. DOI: 10.1016/S0140-6736(21)02144-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Malta DC, Gomes CS, Souza PRB, Jr., et al. Factors Associated with Increased Cigarette Consumption in the Brazilian Population During the COVID-19 Pandemic. Cad Saude Publica. 2021; 37(3): e00252220. DOI: 10.1590/0102-311x00252220 [DOI] [PubMed] [Google Scholar]
- 57.Malta DC, Szwarcwald CL, Barros MBA, et al. The COVID-19 Pandemic and Changes in Adult Brazilian Lifestyles: A Cross-Sectional Study, 2020. Epidemiol Serv Saude. 2020; 29(4): e2020407. DOI: 10.1590/s1679-49742020000400026 [DOI] [PubMed] [Google Scholar]
- 58.Werneck AO, Silva DR, Malta DC, et al. Associations of Sedentary Behaviours and Incidence of Unhealthy Diet During the COVID-19 Quarantine in Brazil. Public Health Nutr. 2021; 24(3): 422–426. DOI: 10.1017/S1368980020004188 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Percent of hospital admissions processed in each month from the total of admissions in the respective month in 2019 and 2020, Hospital Information System, Belo Horizonte, MG, Brazil.
Tutorial to access data.
Age-standardized rates per 100,000 inhabitants and proportions for ICD Chapter XVIII outcomes observed in 2020, and expected (mean of 2015–2019), for epidemiological weeks 10–48, their absolute difference, and risk ratio. Belo Horizonte MG, Brazil.
Age-standardized rates per 100,00 inhabitants and proportions for cardiovascular disease outcomes observed in 2020, and expected (mean of 2015-2019) for epidemiological weeks 10–48, their absolute difference, and risk ratio, according to age range. Belo Horizonte, MG, Brazil.


