Abstract
Wound infection is frequently reported following snakebite (SB). This study is retrospective. It was conducted in the emergency department and the Intensive Care Unit (ICU) of Cayenne General Hospital between 1 January 2016 and 31 July 2021. We included 172 consecutive patients hospitalized for SB envenoming. All patients were monitored for wound infection. Sixty-three patients received antibiotics at admission (36.6%). The main antibiotic used was amoxicillin–clavulanate (92.1%). Wound infection was recorded in 55 cases (32%). It was 19% in grade 1, 35% in grade 2, and 53% in grade 3. It included abscess (69.1%), necrotizing fasciitis (16.4%), and cellulitis (21.8%). The time from SB to wound infection was 6 days (IQR: 3–8). The main isolated microorganisms were A. hydrophila and M. morganii (37.5% and 18.8% of isolated organisms). Surgery was required in 48 patients (28.1%), and a necrosectomy was performed on 16 of them (33.3%). The independent factors associated with snakebite-associated infection were necrosis (p < 0.001, OR 13.15, 95% CI: 4.04–42.84), thrombocytopenia (p = 0.002, OR: 3.37, 95% CI: 1.59–7.16), and rhabdomyolysis (p = 0.046, OR: 2.29, 95% CI: 1.02–5.19). In conclusion, wound infection following SB is frequent, mainly in grade 2 and 3 envenomed patients, especially those with necrosis, thrombocytopenia, and rhabdomyolysis. The main involved bacteria are A. hydrophila and M. morganii.
Keywords: snakebite envenoming, clinical manifestations, French Guiana, Bothrops atrox, infection
1. Introduction
Snake envenoming is a public health problem in French Guiana [1,2]. It can be responsible for systemic and local manifestations. Local manifestations start within minutes after the snakebite (SB). They are associated with pain and edema and are followed, in severe cases, by local necrosis and blistering, which can turn into infection [3]. In French Guiana, the incidence of wound infection (WI) secondary to SB and the responsibility of microorganisms remains poorly investigated. Thus, local recommendations are only based on data from other regions and concerning other snakes [4,5,6,7].
Wound infection following snakebite occurs in 9–77% of the bitten patients [5,6,8,9,10,11]. The main responsible microorganisms are Aeromonas hydrophila, Morganella morganii, Klebsiella pneumoniae, Bacillus spp., and Enterococcus spp. [6,12]. Bacteria are inoculated into the wound from the snake’s oral cavity, along with the venom. Furthermore, local skin and muscle damages constitute a favorable field for bacterial growth. For this, some authors questioned the relevance of empiric antibiotic therapy in snake-bitten patients [7].
We conducted this retrospective study to assess the prevalence of wound infection after snake envenoming in French Guiana, to identify the involved bacteria, and to monitor the use of antibiotics in this context.
2. Results
From 1 January 2016 to 31 July 2021, 172 patients were admitted with a diagnosis of snakebite envenoming (an average of 31 cases per year). The median age of patients was 41 years (IQR: 28–52), and 69% were male. The median time from snakebite to hospital admission was 09:00 (IQR: 02:00–21:00), and the median time between snakebite and antivenom administration was 9:00 (IQR: 5:22–20:40). Snake identification was made in 45.3% of cases. It was Bothrops atrox in 66 patient (84.6% of identified snakes). During the follow-up, 55 cases (32%) developed wound infection.
2.1. Clinical and Biological Manifestations at Admission
At admission, the main clinical symptoms were edema (95.9%), pain (96.5%), systemic bleeding (14%), blister (12.8%), and local hemorrhage (12.8%). The elapsed time from snakebite to the development of systemic bleeding was 5 h (IQR: 0–24). The comparison of the two groups with and without wound infection showed a higher prevalence of necrosis (30.9% vs. 3.4%) and a higher cardiac rhythm (90 vs. 79 beats/min) in the wound infection group (p < 0.001 and 0.002, respectively). Table 1 summarizes the epidemiological and clinical parameters of our patients.
Table 1.
Comparison of baseline characteristics in patients with and without wound infection following snakebite.
| Total Population | Wound Infection | Without Wound Infection | p | ||||
|---|---|---|---|---|---|---|---|
| Nb | Result | Nb | Result | Nb | Result | ||
| Age (years) | 172 | 41 (28–52) | 55 | 46 (31.7–54.6) | 117 | 40 (25.4–50.8) | 0.340 |
| Gender, male | 172 | 119 (69.2%) | 55 | 39 (70.9%) | 117 | 80 (68.4%) | 0.737 |
| BMI | 119 | 23.8 (21–26.9) | 37 | 23.5 (20.3–26.9) | 82 | 23.8 (21.3–26.9) | 0.462 |
| Medical history | 172 | 42 (24.4%) | 55 | 12 (21.8%) | 117 | 30 (25.6%) | |
| Arterial hypertension | 172 | 13 (8%) | 55 | 2 (3.6%) | 117 | 11 (9.4%) | 0.182 |
| Alcohol abuse | 172 | 6 (3%) | 55 | 1 (1.8%) | 117 | 5 (4.3%) | 0.413 |
| Snake bite (SB) | |||||||
| Time from SB to hospital (hh:mm) | 171 | 9:00 (2:02–21:00) | 55 | 12:00 (3:30–22:58) | 116 | 7:07 (1:43–19:03) | 0.064 |
| Identification of the snake | 172 | 78 (45.3%) | 55 | 21 (38.2%) | 117 | 57 (48.7%) | 0.195 |
| Anatomic site of the bite | |||||||
| Upper limb | 172 | 34 (19.8%) | 55 | 10 (18.2%) | 117 | 24 (20.5%) | 0.328 |
| Lower limb | 172 | 137 (79.7%) | 55 | 44 (80%) | 117 | 93 (79.5%) | |
| Head | 172 | 1 (0.6%) | 55 | - | 117 | 1 (0.8%) | - |
| Grade of envenoming | |||||||
| Grade 1 | 172 | 74 (43%) | 55 | 14 (25.5%) | 117 | 60 (51.3%) | Reference |
| Grade 2 | 172 | 60 (34.9%) | 55 | 21 (38.2%) | 117 | 39 (33.3%) | 0.035 |
| Grade 3 | 172 | 38 (22.1%) | 55 | 20 (36.4%) | 117 | 18 (15.4%) | <0.001 |
| Clinical presentation at admission | |||||||
| Edema | 172 | 165 (95.9%) | 55 | 55 (100%) | 117 | 110 (94%) | 0.064 |
| Local hemorrhage | 172 | 22 (12.8%) | 55 | 8 (14.5%) | 117 | 14 (12%) | 0.637 |
| Necrosis | 172 | 21 (12.2%) | 55 | 17 (30.9%) | 117 | 4 (3.4%) | <0.001 |
| Blisters | 172 | 22 (12.8%) | 55 | 14 (25.5%) | 117 | 8 (6.8%) | 0.001 |
| Pain | 171 | 165 (96.5%) | 54 | 53 (98.1%) | 117 | 112 (95.7%) | 0.424 |
| Temperature (°C) | 165 | 36.9 (36.5–37.3) | 49 | 37 (36.6–37.4) | 116 | 36.9 (36.5–37.3) | 0.045 |
| Shock | 172 | 2 (1.2%) | 55 | 1 (1.8%) | 117 | 1 (0.9%) | 0.583 |
| Acute renal injury | 172 | 28 (16.3%) | 55 | 12 (21.8%) | 117 | 16 (13.7%) | 0.177 |
| Time to normal renal function (days) | 28 | 5 (28–10) | 12 | 4 (2–23) | 16 | 6 (2–10) | 0.958 |
| Systemic hemorrhage (SH) | 172 | 24 (14%) | 55 | 7 (12.7%) | 117 | 17 (14.5%) | 0.750 |
| Time from SB to SH (hours) | 24 | 5 (0–24) | 7 | 4 (1–8) | 17 | 7 (0–24) | 0.125 |
| Biological parameters at admission | |||||||
| Fibrinolysis | 172 | 151 (87.8%) | 55 | 45 (81.8%) | 117 | 106 (90.6%) | 0.101 |
| Thrombocytopenia | 172 | 49 (28.5%) | 55 | 25 (45.5%) | 117 | 24 (20.5%) | 0.001 |
| Hemolysis | 172 | 38 (22.1%) | 55 | 15 (27.3%) | 117 | 23 (19.7%) | 0.262 |
| Rhabdomyolysis | 172 | 54 (31.4%) | 55 | 26 (47.3%) | 117 | 28 (23.9%) | 0.002 |
| White blood count (/mm3) | 167 | 10.4 (8.3–13.6) | 53 | 12 (9.4–14.6) | 114 | 10.2 (8–13.2) | 0.016 |
| C-reactive protein (mg/L) | 153 | 8.7 (2.8–32.2) | 46 | 27.6 (5.6–83.2) | 107 | 6.4 (2.7–19.6) | 0.002 |
| Procalcitonin (µmol/L) | 10 | 0.1 (0–0.5) | 0 | - | 10 | 0.1 (0–0.5) | - |
Nb: number of patients for whom the data were recorded, SB: snakebite, BMI: body mass index, SH: systemic hemorrhage.
Biologic parameters at admission showed defibrinogenation in 151 cases (87.8%), thrombocytopenia in 49 cases (28.5%), hemolysis in 38 cases (22.1%), and rhabdomyolysis in 54 cases (31.4%). Thrombocytopenia and rhabdomyolysis were more frequent in the wound infection group (Table 1).
2.2. Initial Management
Initial management was based on analgesics (100%), fluid infusion (73.3%), blood components transfusion (9.9%), dialysis (5.2%), mechanical ventilation (1.7%), and norepinephrine infusion (1.2%). Sixty-three patients (36.6%) received antibiotics at admission. Amoxicillin–clavulanate was the main antibiotic used (92.1% of patients who received antibiotics at admission). The duration of initial amoxicillin–clavulanate administration was 1 day (IQR: 1–1 days). Antivenom was prescribed for 115 patients (66.9%), and 20 of them (17.2%) developed early adverse reactions. They were mild in 13 cases (11.3%) and severe in 7 cases (6.1%).
2.3. Wound Infection
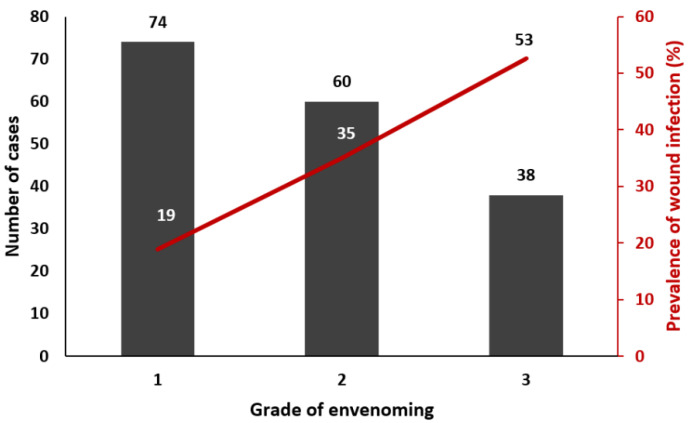
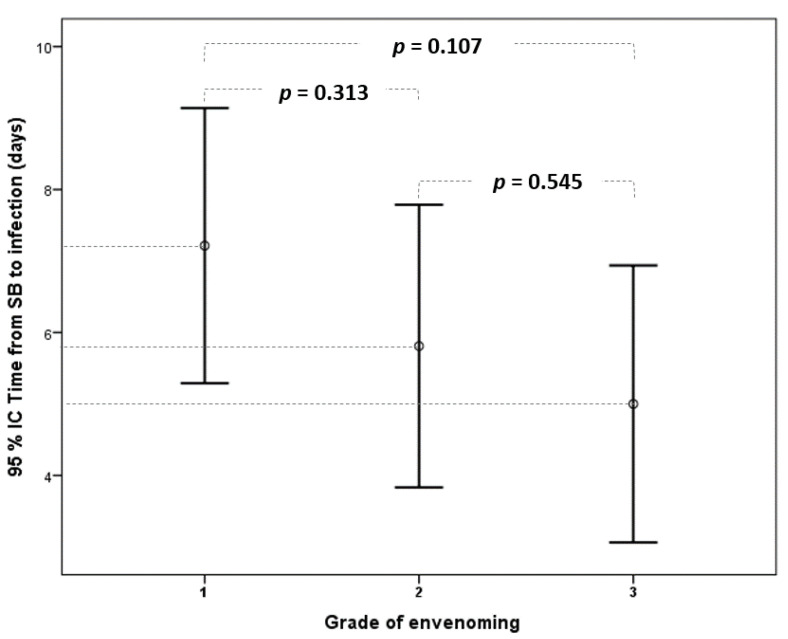
Wound infection was observed in 19% of cases in grade 1 (14/74), 35% in grade 2 (21/60), and 53% in grade 3 patients (20/38) (Figure 1). It included abscess (69.1%), necrotizing fasciitis (16.4%), and cellulitis (21.8%) (Table 2). The time from snakebite to infection was, on average, 6 days (IQR: 3–8). There was no statistical difference according to the grade of envenoming (Figure 2).
Figure 1.
Prevalence of wound infection following snakebite according to the grade of envenoming.
Table 2.
Clinical and therapeutic parameters recorded in patients with wound infection.
| Nb | Result | |
|---|---|---|
| Abscess | 55 | 38 (69.1%) |
| Necrotizing fasciitis | 55 | 9 (16.4%) |
| Cellulitis | 55 | 12 (21.8%) |
| Isolated microorganism | 55 | 32 (58.2%) |
| Time from SB to WI (days) | 55 | 6 (3–8) |
| Antibiotic duration for WI (days) | 36 | 7 (5–8) |
Nb: Number of patients for whom the data were recorded, WI: wound infection.
Figure 2.
Comparison of elapsed time from snakebite to the diagnosis of wound infection according to the grade of envenoming. (95% CI: 95% confidence interval).
2.4. Microbiological Analyses
Microbiological analysis was positive in 32 patients (58.2%). It was positive in 9.5%, 20%, and 34.2% of cases in grade 1, 2, and 3, respectively. It isolated one microorganism in 23 patients and two microorganisms in nine patients.
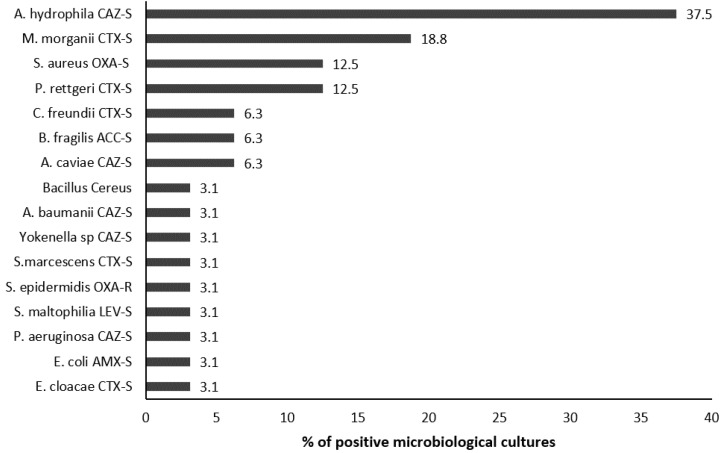
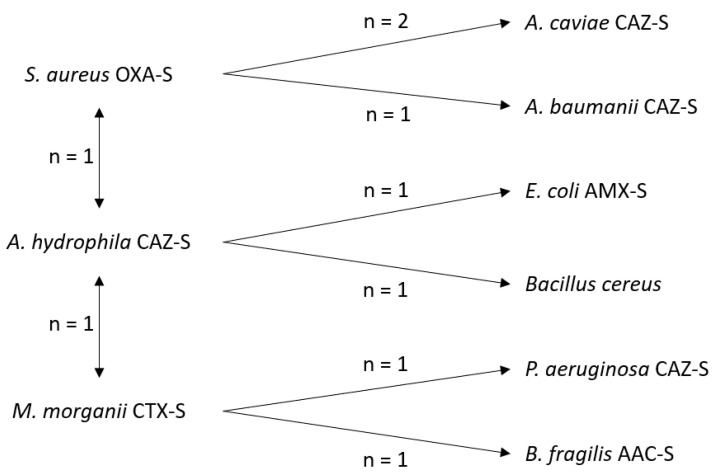
The isolated microorganisms were A. hydrophila susceptible to ceftazidime (CAZ-S) (37.5% of isolated microorganisms), M. morganii susceptible to cefotaxime (CTX-S) (18.8%), and S. aureus susceptible to oxacillin (OXA-S) and P. rettgeri CTX-S (12.5% each) (Figure 3). All microorganisms except one were wild type. However, they were resistant to amoxicillin–clavulanate in 82.9% of cases. The most isolated bacteria in patients with wound infection caused by two microorganisms were S. aureus OXA-S (4 cases), A. hydrophila CAZ-S (3 cases), and M. morganii CTX-S (3 cases) (Figure 4). Positive microbiological results were obtained from blood culture in two cases and local sampling in 30 cases. Antibiotic administration at admission was recorded in 11 cases with negative microbiological results (47.8%) and in 12 patients with positive microbiological results (37.5%) (p = 0.510).
Figure 3.
Isolated microorganisms from the local samples and blood cultures in patients with wound infection following snakebite. (The percentage is calculated based on the number of positive microbiological samples). CTX: cefotaxime, CAZ: ceftazidime, OXA: oxacillin, LEV: levofloxacin, AMX: amoxicillin, AAC: amoxicillin-clavulanate, S: susceptible.
Figure 4.
Coinfection patterns in patients with wound infection caused by microorganisms. CTX: cefotaxime, CAZ: ceftazidime, OXA: oxacillin, LEV: levofloxacin, AMX: amoxicillin, AAC: Amoxicillin-clavulanate, S: susceptible.
2.5. Management of Wound Infection
The treatment of wound infection was based on local disinfection (all cases), abscess drainage (38/55 patients; 69.1%), and antibiotics (36/55 patients; 65.5%). The main antibiotics used were amoxicillin–clavulanate, metronidazole, cefotaxime, piperacillin-tazobactam, and ciprofloxacin in 32.7%, 16.4%, 16.4%, 13.9%, and 13.9% of cases, respectively. The length of antibiotic therapy was 7 days (IQR: 5–8 days). The treatment regimen was based on one antibiotic in 23/55 patients (41.8%), two in 12/55 patients (21.8%), and four in one patient. Nineteen patients (34.5%) did not receive antibiotics, and their management was only based on local measures. Among patients with positive microbiological cultures (n = 32), 23 received antibiotics (71.9%). The prescribed antibiotic was adequate for the isolated microorganism in eight cases (35%). Among patients with negative microbiological cultures (n = 23), 13 received antibiotics (56.5%). A third-generation cephalosporin or piperacillin-tazobactam was prescribed in 6/13 cases (46.2%).
Surgery was required in 48 patients (27.9%), and a necrosectomy was performed on 16 of them (33.3%). The delay from snakebite to surgery was 7 days (IQR: 5–9). Overall, the median hospital length of stay was 9 days (IQR: 6–13). It was 14 days (IQR: 11–23) in patients with wound infection and 7 days (IQR: 5–11) in those without (p < 0.001). Table 3 summarizes the management and outcome of our patients.
Table 3.
Comparison of the management strategy and outcome of patients with and without wound infection following snakebite.
| Total Population | Wound Infection | Without Wound Infection | p | ||||
|---|---|---|---|---|---|---|---|
| Nb | Result | Nb | Result | Nb | Result | ||
| Renal replacement therapy | 172 | 9 (5.2%) | 55 | 4 (7.3%) | 117 | 5 (4.3%) | 0.410 |
| Noradrenaline | 172 | 2 (1.2%) | 55 | 1 (1.8%) | 117 | 1 (0.9%) | 0.583 |
| Mechanical ventilation | 172 | 3 (1.7%) | 55 | 2 (3.6%) | 117 | 1 (0.9%) | 0.194 |
| Antibiotics at admission | 172 | 63 (36.6%) | 55 | 22 (40%) | 117 | 41 (35%) | 0.391 |
| Antivenom therapy (AV) | 172 | 115 (66.9%) | 55 | 32 (58.2%) | 117 | 83 (70.9%) | 0.097 |
| Time from SB to AV | 83 | 9:00 (5:22–20:40) | 22 | 10:00 (6:00–19:45) | 61 | 9:00 (5:15–21:00) | 1 |
| Adverse reaction to AV | 116 | 20 (17.2%) | 33 | 7 (21.2%) | 83 | 13 (15.7%) | 0.284 |
| Transfusion | 172 | 17 (9.9%) | 55 | 9 (16.4%) | 117 | 8 (6.8%) | 0.51 |
| Surgery | 172 | 48 (27.9%) | 55 | 43 (78.2%) | 117 | 5 (4.3%) | <0.001 |
| Necrosectomy | 48 | 23 (47.9%) | 43 | 21 (48.8%) | 5 | 2 (40%) | 0.476 |
| Time from SB to surgery (days) | 48 | 7 (5–9) | 43 | 7 (5–9) | 5 | 5 (3–8) | 0.865 |
| Length of stay in ICU (days) | 138 | 3 (3–5) | 43 | 4 (3–8) | 95 | 3 (3–4) | 0.370 |
| Length of hospital stay (days) | 172 | 9 (6–13) | 55 | 14 (11–23) | 117 | 7 (5–11) | <0.001 |
Nb: Number of patients for whom the data were recorded, SB: snakebite, AV: antivenom.
2.6. Independent Factors Associated with Wound Infection
The logistic regression model selected patient-related variables that were significantly associated with snakebite-related infection, namely, the grade of envenoming, necrosis, blisters, rhabdomyolysis, and thrombocytopenia. The independent factors associated with snakebite-associated infection were necrosis (p < 0.001, OR 13.15, 95% CI: 4.04–42.84), thrombocytopenia (p = 0.002, OR: 3.37, 95% CI: 1.59–7.16), and rhabdomyolysis (p = 0.046, OR: 2.29, 95% CI: 1.02–5.19) (Table 4).
Table 4.
Factors associated with wound infection after snake envenoming (multivariate analysis).
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | Wound Infection (n = 55) |
Without Wound Infection (n = 117) |
p | OR | 95% CI | p |
| Blisters | 14 (25.5%) | 8 (6.8%) | 0.001 | 2.812 | 0.909–8.697 | 0.073 |
| Thrombocytopenia | 25 (45.5%) | 24 (20.5%) | 0.001 | 3.374 | 1.594–7.163 | 0.002 |
| Necrosis | 17 (30.9%) | 4 (3.4%) | <0.001 | 13.15 | 4.042–42.841 | <0.001 |
| Rhabdomyolysis | 26 (47.3%) | 28 (23.9%) | 0.002 | 2.294 | 1.015–5.187 | 0.046 |
| Grade 2 | 21 (38.2%) | 39 (33.3%) | 0.035 | 1.947 | 0.822–4.615 | 0.130 |
| Grade 3 | 20 (36.4%) | 18 (15.4%) | <0.001 | 0.875 | 0.263–2.916 | 0.828 |
OR: odd ratio, 95% CI: 95% confidence interval.
3. Discussion
In the present study, the infection following SB was frequent (32% in our case series), and the patients at highest risk were those presenting with severe envenoming (grades 2 and 3). The main bacteria responsible for wound infection were A. hydrophila CAZ-S, M. morganii CTX-S, and S. aureus OXA-S and P. rettgeri CTX-S.
In the literature, wound infection following snakebite occurs in 9–77% of patients [5,6,8,9,10,11]. The significant differences in the reported prevalence may be related to the case definitions used to characterize infection. A definite diagnosis can only be made when the responsible microorganism is isolated. In the remaining cases, infection is defined on a clinical basis, taking into account that clinical manifestations of local infection are quite similar to those induced by the venom toxins. Indeed, in clinical setting, it is difficult to differentiate local venom toxicity from wound infection, especially in severely envenomed patients. For this, we used the secondary appearance or worsening of local inflammatory symptoms as an indicator of the resolution or the stabilization of the toxic effect (related to envenoming) and the new appearance or worsening of local signs (related to infectious process). Overall, the secondary onset of signs evocative of wound infection suggest that the symptoms of snake envenoming are resolved and that local symptoms are related to a secondary event.
Documented wound infection combines local signs and positive microbiological cultures. However, in some cases, microbiological cultures remain sterile, and the diagnosis of infection is based solely on clinical evaluation. Moreover, initial empiric antibiotic therapy can result in negative microbiological cultures. Additionally, antibacterial activity in snake venoms have already been described in the literature [13,14,15,16]. Consequently, the prevalence of patients who developed wound infection secondary to snakebite could not be calculated except for those with positive microbiological cultures. Further studies should establish a more uniform set of criteria to define infection in snakebite envenoming and harmonize data that would allow for comparing studies.
In the present study, the main responsible bacteria were A. hydrophila CAZ-S, M. morganii CTX-S, and S. aureus OXA-S and P. rettgeri CTX-S. In the literature, the main involved bacteria in wound infection following snakebite are A. hydrophila, M. morganii, S. marcescens, Staphylococci, group D streptococci, Clostridium, E. coli, and E. faecalis. These bacteria have also been isolated from the mouth of viperid species [6,12]. Furthermore, S. aureus has rarely been isolated from the mouth of the snake, which suggests that these bacteria come from the patient’s skin instead of from the snake’s fangs. Therefore, strict disinfection of the bite site must be performed [17,18].
According to the Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections [19], amoxicillin–clavulanate is recommended in bitten patients. In the present study, patients received antibiotics at admission in 36.6% of cases, mainly amoxicillin–clavulanate (92.1%). However, systematic antibiotic administration is questionable after a snakebite. Indeed, several studies showed that isolated Enterobacteriaceae following snakebite-related infection showed 60–70% resistance to amoxicillin–clavulanate. In our study, 82.9% of isolated bacteria were resistant to amoxicillin–clavulanate. Moreover, bacteria were susceptible to third-generation cephalosporins in 97% and to ciprofloxacin in 100% of cases [6,12,18,20,21,22]. So, systematic amoxicillin–clavulanate administration should not be advised, and we support the empiric use of third-generation cephalosporins in severe snake-bitten patients.
In our study, 82.9% of isolated bacteria were resistant to amoxicillin–clavulanate. Consequently, amoxicillin–clavulanate is not the best choice as empiric therapy in the case of snakebite. Surprisingly, physicians prescribed antibiotics at admission in 36.6% of cases, mainly amoxicillin–clavulanate (92.1%). This result shows the need to promote medical teams’ training for better and optimal snake-envenoming care in French Guiana. More surprisingly, the main antibiotic used in patients with wound infection was amoxicillin–clavulanate, and no antibiotic was prescribed in 34.5% of patients. In patients with positive microbiological cultures, the prescribed antibiotic was adequate for the isolated microorganism in only 35% of cases. In patients with negative microbiological cultures, antibiotics were also prescribed because of the complex nature of the oral microbiota in snakes, and bite wounds can harbor potential pathogens, many of which are anaerobes, which are difficult to document. In our study, the prescribed antibiotics in case of negative microbiological cultures were adequate for recommendations in only 46.2% of cases. This questions the usefulness of antibiotics in case of wound infections following snakebite and whether local measures are sufficient in some cases.
The results of this study argue in favor of the promotion of a protocol relating to the proper use of antibiotics in the event of a snakebite.
Snake oral cavities and fangs contain many pathogenic bacteria [12,21,22]. However, only some envenomed patients developed wound infection following the snakebite (32% in our study). Most of these patients were severely envenomed (grades 2 and 3) and presented rhabdomyolysis and thrombocytopenia. These signs reflect the prominent tissue damage probably related to the high amount of injected venom. Therefore, it is suggested that venom-induced skin and muscle damage is favorable for bacterial colonization and constitutes the bed of infection [23].
Our study has limitations. First, this was a mono-centric observational study. However, the Cayenne General Hospital provides care for more than two-thirds of the Guianese population [24]. Second, the involved bacteria were only identified in a limited number of cases (58.2%), having little clinical evidence of infection, probably because of a low inoculum, the involvement of anaerobic bacteria, antibiotics exposure, or the lack of microbiological sampling in some cases. The comparison of patients with and without isolated bacteria did not show a difference in prior antibiotic administration. Third, in cases without microbiological documentation, the diagnosis of infection was assessed clinically. This approach is approved by many authors [9,25,26,27], but further studies are needed to evaluate the diagnostic value of clinical and biological parameters to assess the diagnosis of wound infection following snakebite. Fourth, the snake identification was not very precise because the snake was not seen in many cases and can be known by different common names according to the geographic region [28,29]. However, it is well known that, in French Guiana and in the Amazon region, more than 90% of SB envenomings are caused by B. atrox [3,17]. Finally, we did not have the ability to measure time to infection resolution.
4. Conclusions
Wound infection following snakebite in French Guiana is frequent in grade 2 and 3 envenomed patients, especially those with necrosis, thrombocytopenia, and rhabdomyolysis. The main involved bacteria are A. hydrophila and M. morganii. Empirical antibiotics should be adapted to the most common isolated bacteria in this context and for at-risk patients. Our data support that the most appropriate empirical antibiotics are third-generation cephalosporins and that empirical amoxicillin–clavulanate should no longer be used in this context. Local disinfection, necrosectomy, and abscess drainage remain the essential measures for treating wound infection following snakebite.
5. Materials and Methods
The study is retrospective. It was conducted in the emergency department (ED) and the intensive care unit (ICU) of Cayenne General Hospital between 1 January 2016 and 31 July 2021. We included all patients hospitalized for snake envenoming regardless of the severity grade. The grade of envenoming was assessed in accordance with the recommendations of the international symposium on snakebites in French Guiana (Table 5) [17]. We excluded all patients with a history of snakebite without signs of envenoming.
Table 5.
Severity grading scale of snake envenoming [17].
| Grade | ||||
|---|---|---|---|---|
| 1 (Mild) | 2 (Moderate) | 3 (Severe) | ||
| Coagulation disorder | present | present | present | |
| Local symptoms | Pain | present | present | present |
| Swelling | Not exceeding elbow or knee | Exceeding elbow or knee | Beyond the root of the limb | |
| Blister | absent | present | present | |
| Necrosis | absent | absent | present | |
| Local or systemic bleeding | absent | present | present | |
| Systemic manifestations (Hypotension, renal injury, coma, respiratory failure, …) |
absent | absent | present | |
Our hospital is a 510-bed general center that serves as a first-line medical center for an urban population of 100,000 inhabitants and as a referral center for a larger population coming from all the communities of French Guiana, accounting for almost 300,000 inhabitants [24].
5.1. Management of Snakebite Envenoming
The management of snake envenoming was based on the recommendations of the international symposium on snakebites in French Guiana [17]. All patients were checked for vaccination status and had a quick tetanus test. Anti-tetanus prophylaxis was administered accordingly. Some patients did not receive antivenom because there was no available antivenom in Cayenne, and snake-bitten patients were managed symptomatically until 2017 [2] or because of supply shortage. In 2017, the French Authority for Health recommended Antivipmyn Tri® for the treatment of snake-envenomed patients in French Guiana. Moreover, in September 2017, an international symposium was held at Cayenne under the aegis of the French Regional Health Agency and the Pan American Health Organization [17]. The conclusions of this symposium illustrated the urgent need to ensure the accessibility of effective and safe polyvalent viperid antivenom in French Guiana. In the symposium, experts advised against systematic antibiotic administration in snake-envenomed patients.
5.2. Diagnosis and Management of Snakebite-Related Wound Infection
Wound infection following snakebite was defined by a secondary increase in local inflammatory symptoms or the appearance of pain, erythema, local warmth, swelling, lymphangitis, or purulence, independent of the grade of envenoming. In grade 2 or 3 envenomings, the wound infection was suspected in the case of local inflammatory symptoms independent of the timing of occurrence and was confirmed in the case of a positive microbiological culture.
The microbiological documentation of wound infection was based on positive microbiological cultures obtained from blood, local skin samples, and by culturing surgical specimens obtained during surgical debridement.
Local samples were subjected to Gram staining and cultured for bacterial growth. They were plated on nonselective blood agar and chocolate agar and cultured at 37 °C for 2–7 days, and the color and shape of the colonies were observed. Species identification was performed with API-20E and API-20NE systems (BioMérieux, Marcy L’Etoile, France). Blood cultures were performed using aerobic (Bact/ALERT FA plus) and anaerobic (Bact/ALERT FN plus) blood culture vials which were incubated in a BacT/ALERT 3D (BioMérieux, Marcy L’Etoile, France). All isolates were then identified using MALDI-TOF mass spectrometry (MaldiBiotyper 3.0, Bruker Daltonique, Marnes la Vallée, France). Antimicrobial susceptibilities of all isolates were determined by the disk diffusion method based on the definition of the Antibiogram Committee of the French Microbiology Society [30]. Susceptibility patterns were expressed as susceptible (S) or resistant (R) to cefotaxime (CTX), ceftazidime (CAZ), oxacillin (OXA), levofloxacin (LEV), or amoxicillin (AMX), according to the studied bacteria.
Upon admission to the emergency department or intensive care unit, a complete blood sample was taken, including, among other things, hemostasis, renal function, and creatinine kinase.
In all patients, we collected epidemiological and clinical data, including age and sex, the date and time of the bite, the anatomical site of the bite, the snake description, the grade of envenoming, and the clinical manifestations at admission and during the hospital stay. The complete cure of infection was obtained when clinical symptoms resolved.
5.3. Ethical Statement
Our study is retrospective and did not require individual consent according to the French law regarding research conforming to the norm MR-003 (JORF No. 0160, 13 July 2018, text No. 109). The protocol of antivenom administration and blood test dosages were approved by the hospital’s institutional review board (ref: UF3700/17′, version “b”—November 2016, revised on 5 March 2020). All patients were informed about the hospital protocol on the management of snakebite envenoming and were informed that the data collected would be used in research programs. Verbal consent was obtained from all patients or relatives (when patients were <18 years or unable to consent) and was reported in the medical file of the patient by the doctor in charge. In patients receiving antivenom, a completed form (blank form reference: Q11ADOC025 v01), including the patient data, the dosage, and the route of administration used, was completed and returned to the French National Agency for Drug Safety (ANSM: Agence Nationale de Sécurité de Médicaments). On this form, the physician in charge certified that the patient was informed about the drug use and that he would undertake to inform the ANSM of any adverse reaction. Our database was registered at the Commission National de l’Informatique et des Libertés (registration No. 2217025v0—27 February 2020), in compliance with French law on electronic data sources.
5.4. Definitions
Thrombocytopenia is defined by a platelet count <150 G/L. Defibrinogenation is defined by a fibrinogen level <1 g/L (normal value: 2–4 g/L). Rhabdomyolysis is defined by a CK level >500 UI/L (normal value: 39–308 UI/L). Coagulation disorders are defined by international normalized ratio >2 (normal value: 0.8–1.2), partial thromboplastin time >1.5, prothrombin time, and coagulation factors <60%. Renal failure is defined according to the KDIGO definition [31]. Adverse reactions to antivenom were reported to the French Agency for the Safety of Health Products and were classified as ‘mild’ (only cutaneous urticaria, pruritus) or ‘severe’ (bronchospasm, angioedema, hypotension, colic) [32].
5.5. Statistical Analysis
We created a data file with the patient’s and snake’s information, and we performed a descriptive analysis using Excel (2007) and IBM SPSS Statistics for Windows, version 24 (IBM Corp., Armonk, NY, USA). Results were reported as the number of patients for whom the data were recorded (Nb), the median and interquartile range (IQR), or numbers with percentages. Time is expressed as hours and minutes (hh:mm). To compare qualitative variables, we used the Fisher exact test. Continuous variables were tested for normality using Kolmogorov–Smirnov test (KS) and Shapiro–Wilk (SW) test. Variables with normal distribution were compared using independent sample t-test. Variables with non-normal distribution were compared using the Mann–Whitney U test.
Variables associated with snakebite-related infection at the 0.05 level by univariate analysis were entered into the stepwise logistic regression model. We calculated the odd ratio (OR) and the 95% confidence interval (95% CI). All statistical tests were two-tailed, and p ≤ 0.05 was considered significant.
Author Contributions
Conceptualization, S.H., D.R., J.M.P., D.H. and H.K.; methodology, S.H., D.H. and H.K.; software, S.H., G.R.L. and P.L.; validation, S.H., D.R., M.D., S.M. and H.K.; formal analysis, S.H. and H.K.; data curation, S.H., and H.K.; writing—original draft preparation, S.H., J.M.P. and H.K.; writing—review and editing, D.R., J.M.P., S.M., F.C., M.D. and D.H.; supervision, H.K.; project administration, S.H. and H.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Cayenne General Hospital (protocol code UF3700/17’, version “b”; 12 September 2017). Our database is registered at the Commission Nationale de l’Informatique et des Libertés (registration No. 2217025v0), in compliance with French law on electronic data sources.
Informed Consent Statement
All patients were informed about the hospital protocol related to snakebite management and the use of collected data in research programs. Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting reported results can be found with the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Key Contribution
Wound infection following snakebite is frequent. It is caused mainly by A. hydrophila and M. morganii.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mutricy R., Heckmann X., Douine M., Marty C., Jolivet A., Lambert V., Perotti F., Boels D., Larréché S., Chippaux J.-P., et al. High Mortality Due to Snakebites in French Guiana: Time Has Come to Re-Evaluate Medical Management Protocols. PLoS Negl. Trop. Dis. 2018;12:e0006482. doi: 10.1371/journal.pntd.0006482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kallel H., Mayence C., Houcke S., Mathien C., Mehdaoui H., Gutiérrez J.M., Megarbane B., Hommel D., Resiere D. Severe Snakebite Envenomation in French Guiana: When Antivenom Is Not Available. Toxicon. 2018;146:87–90. doi: 10.1016/j.toxicon.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Resiere D., Monteiro W., Houcke S., Pujo J.M., Mathien C., Mayence C., Neviere R., Hommel D., de Almeida Gonçalves Sachett J., Mehdaoui H., et al. Bothrops Snakebite Envenomings in the Amazon Region. Curr. Trop. Med. Rep. 2020;7:48–60. doi: 10.1007/s40475-020-00203-4. [DOI] [Google Scholar]
- 4.Garg A., Sujatha S., Garg J., Acharya N.S., Chandra Parija S. Wound Infections Secondary to Snakebite. J. Infect. Dev. Ctries. 2009;3:221–223. doi: 10.3855/jidc.39. [DOI] [PubMed] [Google Scholar]
- 5.Wagener M., Naidoo M., Aldous C. Wound Infection Secondary to Snakebite. South Afr. Med. J. 2017;107:315–319. doi: 10.7196/SAMJ.2017.v107i4.12084. [DOI] [PubMed] [Google Scholar]
- 6.Resiere D., Mehdaoui H., Névière R., Olive C., Severyns M., Beaudoin A., Florentin J., Brouste Y., Banydeen R., Cabié A., et al. Infectious Complications Following Snakebite by Bothrops Lanceolatus in Martinique: A Case Series. Am. J. Trop. Med. Hyg. 2020;102:232–240. doi: 10.4269/ajtmh.19-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Resiere D., Gutiérrez J.M., Névière R., Cabié A., Hossein M., Kallel H. Antibiotic Therapy for Snakebite Envenoming. J. Venom. Anim. Toxins Incl. Trop. Dis. 2020;26:e20190098. doi: 10.1590/1678-9199-jvatitd-2019-0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen C.-M., Wu K.-G., Chen C.-J., Wang C.-M. Bacterial Infection in Association with Snakebite: A 10-Year Experience in a Northern Taiwan Medical Center. J. Microbiol. Immunol. Infect. 2011;44:456–460. doi: 10.1016/j.jmii.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 9.Mao Y.-C., Liu P.-Y., Hung D.-Z., Lai W.-C., Huang S.-T., Hung Y.-M., Yang C.-C. Bacteriology of Naja Atra Snakebite Wound and Its Implications for Antibiotic Therapy. Am. J. Trop. Med. Hyg. 2016;94:1129–1135. doi: 10.4269/ajtmh.15-0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsieh Y.-H., Hsueh J.-H., Liu W.-C., Yang K.-C., Hsu K.-C., Lin C.-T., Ho Y.-Y., Chen L.-W. Contributing Factors for Complications and Outcomes in Patients With Snakebite: Experience in a Medical Center in Southern Taiwan. Ann. Plast. Surg. 2017;78:S31–S36. doi: 10.1097/SAP.0000000000001002. [DOI] [PubMed] [Google Scholar]
- 11.Sachett J.A.G., da Silva I.M., Alves E.C., Oliveira S.S., Sampaio V.S., do Vale F.F., Romero G.A.S., dos Santos M.C., Marques H.O., Colombini M., et al. Poor Efficacy of Preemptive Amoxicillin Clavulanate for Preventing Secondary Infection from Bothrops Snakebites in the Brazilian Amazon: A Randomized Controlled Clinical Trial. PLoS Negl. Trop. Dis. 2017;11:e0005745. doi: 10.1371/journal.pntd.0005745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Résière D., Olive C., Kallel H., Cabié A., Névière R., Mégarbane B., Gutiérrez J.M., Mehdaoui H. Oral Microbiota of the Snake Bothrops Lanceolatus in Martinique. Int. J. Environ. Res. Public Health. 2018;15:2122. doi: 10.3390/ijerph15102122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glaser H.S.R. Bactericidal Activity of Crotalus Venom in Vitro. Copeia. 1948;1948:245–247. doi: 10.2307/1438710. [DOI] [Google Scholar]
- 14.Aloof-Hirsch S., de Vries A., Berger A. The Direct Lytic Factor of Cobra Venom: Purification and Chemical Characterization. Biochim. Biophys. Acta. 1968;154:53–60. doi: 10.1016/0005-2795(68)90257-2. [DOI] [PubMed] [Google Scholar]
- 15.Bustillo S., Leiva L.C., Acosta O., Bal de Kier Joffé E., Gorodner J.O. Antimicrobial Activity of Bothrops Alternatus Venom from the Northeast of Argentine. Rev. Latinoam. De Microbiol. 2008;50:79–82. [Google Scholar]
- 16.Blaylock R.S. Antibacterial Properties of KwaZulu Natal Snake Venoms. Toxicon. 2000;38:1529–1534. doi: 10.1016/S0041-0101(00)00085-4. [DOI] [PubMed] [Google Scholar]
- 17.Kallel H., Hommel D., Mehdaoui H., Megarbane B., Resiere D. Snakebites in French Guiana: Conclusions of an International Symposium. Toxicon. 2018;146:91–94. doi: 10.1016/j.toxicon.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Jorge M.T., Ribeiro L.A., Da Silva M.L.R., Kusano E.J.U., de Mendonça J.S. Microbiological Studies of Abscesses Complicating Bothrops Snakebite in Humans: A Prospective Study. Toxicon. 1994;32:743–748. doi: 10.1016/0041-0101(94)90343-3. [DOI] [PubMed] [Google Scholar]
- 19.Stevens D.L., Bisno A.L., Chambers H.F., Dellinger E.P., Goldstein E.J.C., Gorbach S.L., Hirschmann J.V., Kaplan S.L., Montoya J.G., Wade J.C. Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2014;59:147–159. doi: 10.1093/cid/ciu444. [DOI] [PubMed] [Google Scholar]
- 20.Lam K.K., Crow P., Ng K.H.L., Shek K.C., Fung H.T., Ades G., Grioni A., Tan K.S., Yip K.T., Lung D.C., et al. A Cross-Sectional Survey of Snake Oral Bacterial Flora from Hong Kong, SAR, China. Emerg. Med. J. 2011;28:107–114. doi: 10.1136/emj.2009.086694. [DOI] [PubMed] [Google Scholar]
- 21.Jorge M.T., de Mendonça J.S., Ribeiro L.A., da Silva M.L.R., Kusano E.J.U., Cordeiro C.L. Bacterial Flora of the Oral Cavity, Fangs and Venom of Bothrops Jararaca: Possible Source of Infection at the Local Bite. Rev. Do Inst. De Med. Trop. De São Paulo. 1990;32:6–10. doi: 10.1590/S0036-46651990000100002. [DOI] [PubMed] [Google Scholar]
- 22.Shaikh I.K., Dixit P.P., Pawade B.S., Potnis-Lele M., Kurhe B.P. Assessment of Cultivable Oral Bacterial Flora from Important Venomous Snakes of India and Their Antibiotic Susceptibilities. Curr. Microbiol. 2017;74:1278–1286. doi: 10.1007/s00284-017-1313-z. [DOI] [PubMed] [Google Scholar]
- 23.Saravia-Otten P., Gutierrez J.M., Arvidson S., Thelestam M., Flock J.-I. Increased Infectivity of Staphylococcus Aureus in an Experimental Model of Snake Venom-Induced Tissue Damage. J. Infect. Dis. 2007;196:748–754. doi: 10.1086/520537. [DOI] [PubMed] [Google Scholar]
- 24.Kallel H., Resiere D., Houcke S., Hommel D., Pujo J.M., Martino F., Carles M., Mehdaoui H. Critical Care Medicine in the French Territories in the Americas: Current Situation and Prospects. Rev. Panam. De Salud Pública. 2021;45:e46. doi: 10.26633/RPSP.2021.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang L.-W., Wang J.-D., Huang J.-A., Hu S.-Y., Wang L.-M., Tsan Y.-T. Wound Infections Secondary to Snakebite in Central Taiwan. J. Venom. Anim. Toxins Incl. Trop. Dis. 2012;18:272–276. doi: 10.1590/S1678-91992012000300004. [DOI] [Google Scholar]
- 26.Ki V., Rotstein C. Bacterial Skin and Soft Tissue Infections in Adults: A Review of Their Epidemiology, Pathogenesis, Diagnosis, Treatment and Site of Care. Can. J. Infect. Dis. Med. Microbiol. 2008;19:173–184. doi: 10.1155/2008/846453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cefalu J.E., Barrier K.M., Davis A.H. Wound Infections in Critical Care. Crit. Care Nurs. Clin. 2017;29:81–96. doi: 10.1016/j.cnc.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 28.da Siva A.M., Monteiro W.M., Bernarde P.S. Popular Names for Bushmaster (Lachesis Muta) and Lancehead (Bothrops Atrox) Snakes in the Alto Juruá Region: Repercussions for Clinical-Epidemiological Diagnosis and Surveillance. Rev. Soc. Bras. Med. Trop. 2019;52:e20180140. doi: 10.1590/0037-8682-0140-2018. [DOI] [PubMed] [Google Scholar]
- 29.da Silva J.L., da Siva A.M., do Amaral G.L.G., Ortega G., Monteiro W.M., Bernarde P.S. The Deadliest Snake According to Ethnobiological Perception of the Population of the Alto Juruá Region, Western Brazilian Amazonia. Rev. Soc. Bras. Med. Trop. 2019;53:e20190305. doi: 10.1590/0037-8682-0305-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soussy C.J., Carret G., Cavallo J.D., Chardon H., Chidiac C., Choutet P., Courvalin P., Dabernat H., Drugeon H., Dubreuil L., et al. Antibiogram Committee of the French Microbiology Society. Report 2000–2001. Pathol. Biol. 2000;48:832–871. [PubMed] [Google Scholar]
- 31.Khwaja A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin. Pract. 2012;120:c179–c184. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 32.Sampson H.A., Muñoz-Furlong A., Campbell R.L., Adkinson N.F., Bock S.A., Branum A., Brown S.G.A., Camargo C.A., Cydulka R., Galli S.J., et al. Second Symposium on the Definition and Management of Anaphylaxis: Summary Report—Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network Symposium. J. Allergy Clin. Immunol. 2006;117:391–397. doi: 10.1016/j.jaci.2005.12.1303. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting reported results can be found with the corresponding author.