Abstract
Background:
Pneumatic tourniquets are widely used in total knee arthroplasty (TKA). Some surgeons prefer a uniform tourniquet inflation pressure (UTIP) for all patients; others use personalized tourniquet inflation pressures (PTIP) based on systolic blood pressure and limb occlusion pressure. However, no consensus exists regarding the optimal mode of inflation pressure during TKA. This review aimed to appraise if personalized tourniquet inflation pressures are better than uniform tourniquet inflation.
Methods:
The databases (Web of Science, Embase, PubMed, Cochrane Controlled Trials Register, Cochrane Library, Highwire, CBM, CNKI, VIP, Wanfang) were searched on March 2021 to systematically identify and screen the literature for randomized controlled trials involving PTIP and UTIP during total knee arthroplasty.
Results:
Thirteen randomized controlled trials, involving 1204 TKAs (1201 patients) were included in the systematic review. The meta-analysis identified a trend toward less visual analogue scale (VAS) score at rest with PTIP group at 1 day (P = .002), 2 to 3 days (P = .01), and less VAS score at activity 1 day (P < .0001), 2 to 3 days after the operation (P < .00001), and discharge (P < .0001). No significant difference was found between the groups in terms of VAS score at rest when discharge (P = 1.0). We also found no significant difference in terms of intraoperative blood loss (P = .48), total blood loss (P = .15), lower limb vein thrombosis (P = .42), and thigh bullae (P = .17). However, in the PTIP group, we found a significant higher hospital for special surgery (HSS) score (P = .007), broader knee Range of motion (P = .02), less rate of thigh ecchymosis (P = .00001), and shorter thigh circumference at 1 day (P = .006), 2 to 3 days (P = .0005), and discharge (P = .02).
Conclusion:
PTIP provides a similar bloodless surgical field compared with the conventional UTIP. Furthermore, PTIP provides less pain intensity, thigh circumference, rate of thigh ecchymosis, higher hospital for special surgery, and better initial recovery of knee flexion in total knee arthroplasty. Therefore, we recommend using a PTIP method during TKA. More adequately powered and better-designed randomized controlled trials studies with long-term follow-up are required to produce evidence-based guidelines regarding the PTIP method.
Keywords: limb occlusion pressure, personalized tourniquet inflation pressure, systolic blood pressure, total knee arthroplasty
1. Introduction
Pneumatic tourniquets that are used in total knee arthroplasty (TKA) may lead to soft tissue damage, including the skin, vessels, muscles, nerves, and fibrinolytic activity due to unnecessarily excessive inflation pressure.[1–4] However, many orthopedic surgeons use it. A study of the American Association of Hip and Knee Surgeons found that approximately 95% of surgeons used tourniquets during TKA.[5]
The tourniquet can provide a clear bloodless field, which potentially reduces intraoperative blood loss, operative time, and better prepares the cement–bone interface, despite the possible adverse effects associated with its use during TKA.[6] The tourniquet use is almost indispensable in orthopedic practice. Although a lot of procedures employ the use of a tourniquet, there is still a lack of evidence-based guidelines of standard practice regarding optimal inflation pressures.[7–9] While some prefer a uniform tourniquet inflation pressure (UTIP) for all patients,[10–12] others use personalized tourniquet inflation pressures (PTIP), which based on systolic blood pressure (SBP)[3,13,14] or limb occlusion pressure (LOP). This study aimed to compare the effects of the PTIP with conventional UTIP on rehabilitation outcomes in TKA patients.
2. Methods
Our meta-analysis was registered on PROSPERO (International prospective register of systematic reviews), and the registration number was CRD42020168432. We assessed the quality of the included studies according to the items recommended in Cochrane Collaboration (Revman 5.3; http://handbook.cochrane.org/), and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.
2.1. Search strategy
We identified relevant randomized controlled trials involving PTIP or conventional UTIP in total knee arthroplasty in electronic databases, including PubMed, Web of Science, Embase, Cochrane Controlled Trials Register, Cochrane Library, Highwire, CBM, CNKI, VIP, Wanfang database, up to March 2021. The keywords included “total knee arthroplasty,” “total knee replacement,” “tourniquet,” “pressure,” in conjunction with Boolean operators “AND” or “OR.” Review Manager Software was used to perform our meta-analysis.
2.2. Inclusion criteria
The inclusion criteria were: the intervention was PTIP, based on SBP or LOP in TKA; the comparator was the UTIP based on surgeon experience; randomized controlled trial studies; the outcomes are intraoperative blood loss, total blood loss, visual analogue scale (VAS) score, hospital for special surgery (HSS) score, knee range of motion (ROM), thigh circumference, complication rates including lower limb vein thrombosis, thigh bullae, and thigh ecchymosis; the follow-up rate was at least 80%. At least one outcome was included in the study.
The exclusion criteria were as follows: observational studies; non-randomized controlled trials (RCTs); the included studies have insufficient outcome data.
2.3. Data extraction process
Two reviewers independently extracted the available data from each study. The primary data were based on the following: first author, year of publication, country, number of TKAs and participants, age, gender, body mass index, the primary indication for TKA, prosthesis, anesthesia, operation time, mean tourniquet time, mean inflation pressure, practices of tourniquet pressure, the time for loosening the tourniquet. The primary outcome consisted of intraoperative blood loss, total blood loss, VAS score, HSS score, complications such as lower limb vein thrombosis, thigh bullae, and thigh ecchymosis. Secondary outcomes included knee ROM and thigh circumference. We resolved the disagreements by discussion to reach a consensus.
2.4. Quality assessment
We used the Cochrane risk of bias tool to assess the risk of bias in the RCTs and determine whether biases might have affected the results.
2.5. Ethical consideration
Ethical approval is not required, because this study is based on existed literature. The findings of this systematic review will be disseminated through a peer-reviewed journal.
2.6. Statistical analysis
Review Manager 5.3 software (The Nordic Cochrane Collaboration, Copenhagen) was used to perform the meta-analysis. The Q test and I2 were used to evaluate the heterogeneity between studies. The random-effects model was in the place of the fixed effects model for heterogeneity test, P values ≤.1 or I2 ≥ 50%. The mean difference (MD) or standard mean difference (SMD) was used to assess continuous outcomes such as VAS, blood loss, HSS, knee ROM, and thigh circumference with a 95% confidence interval (CI). We used relative risks with a 95% CI to assess dichotomous outcomes such as rate of lower limb vein thrombosis, thigh bullae, and thigh ecchymosis. We considered the results as a statistically significant difference when P values were <.05.
3. Results
3.1. Search results
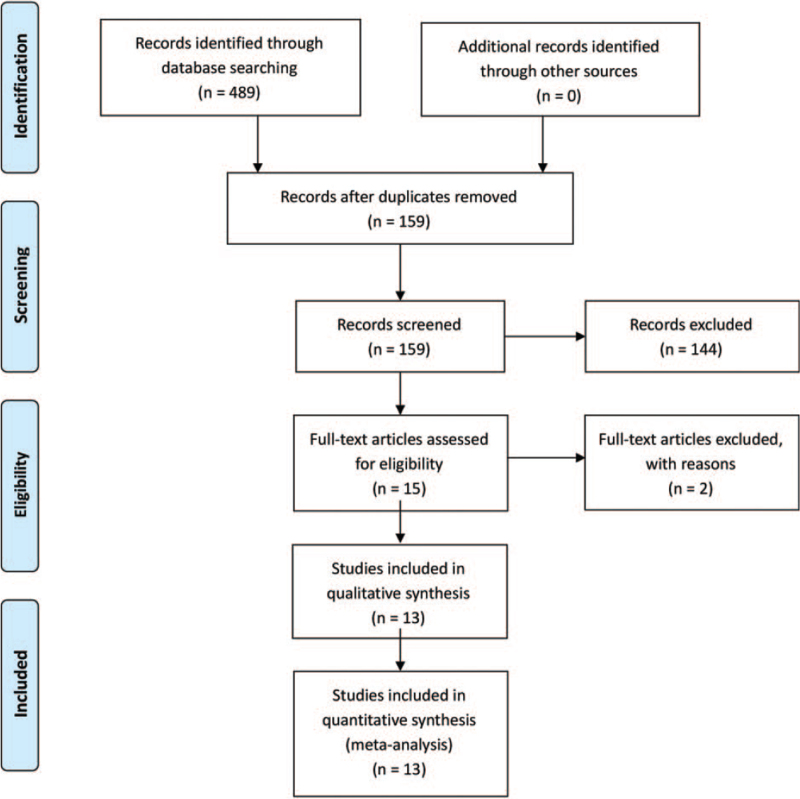
The detailed literature screening process is shown as the PRISMA flow diagram in Fig. 1. The literature search identified 489 citations. Of these, we removed 330 duplicates. Upon reviewing the titles and abstracts of the 159 remaining articles, we excluded 144 papers according to the inclusion criteria and retrieved the full text of 13 articles. Finally, we identified 1204 TKAs (1201 patients) assessed in 13 randomized controlled trials.[15–27] We presented the detailed baseline characteristics in Table 1, detailed information in Table 2, and tourniquet intervention information in Table 3. All the studies were double-arm RCTs and were published in English and Chinese between the years 2005 and 2021.
Figure 1.
The search results and selection procedure. The literature search identified 489 citations. Of these, we removed 330 duplicates. Upon reviewing the titles and abstracts of the 159 remaining articles, we excluded 144 papers according to the inclusion criteria and retrieved the full text of 13 articles. Finally, we identified 1204 TKAs (1201 patients) assessed in 13 randomized controlled trials. TKA = total knee arthroplasty.
Table 1.
The detailed baseline characteristics information.
| Author/yr | Patients | Knees | Mean age, y | Female gender (%) | BMI | Outcome |
| Ishii 2005 | 29/28 | 30/30 | 71/68 | 93.1/85.7 | 25.5/26.6 | 1 (1.1; 1.2); 3 (3.1) |
| Unver 2013 | 17/21 | 17/21 | 68/67.3 | 82.4/85.7 | 30.8/32 | 2 (2.1; 2.2; 2.3; 2.4; 2.5; 2.6); 3.1 |
| De Souza Leão 2016 | 30/30 | 30/30 | 66/65.4 | 73.3/76.7 | NA | 2 (2.2; 2.3); 5 |
| Geng 2014 | 61/60 | 61/60 | NA | NA | NA | 3 (3.2; 3.3) |
| Lei 2019 | 36/35 | 36/35 | 67.42/68.86 | 80.6/80 | 24.67/24.84 | 1 (1.1; 1.2); 2 (2.1; 2.2; 2.3); 3 (3.2; 3.3); 4; 6 (6.1;6.2) |
| Si 2018 | 88/82 | 88/82 | NA | NA | NA | 3 (3.1;3.2) |
| Wu 2014 | 30/30 | 30/30 | 65.97/65.67 | NA | 23.26/23.74 | 6.1 |
| Zhang 2016 | 80/80 | 80/80 | NA | NA | NA | 3.2 |
| Zhou 2019 | 50/50 | 50/50 | 67/65.8 | 52/54 | 22.9/23 | 1 (1.1; 1.2); 2 (2.1; 2.2; 2.3; 2.4; 2.5; 2.6); 3.1 |
| Pan 2019 | 50/50 | 50/50 | 66.35/65.43 | 64/58 | NA | 3.2 |
| Yang 2020 | 50/50 | 50/50 | 69.44/70.35 | 40/30 | NA | 2.1; 3 (3.2; 3.3) |
| Zhang 2021 | 42/42 | 42/42 | 58.91/59.89 | 40.5/38.1 | NA | 1 (1.1; 1.2); 3.2; 4 |
| Tao 2018 | 40/40 | 40/40 | 63.5/64.3 | 62.5/60 | NA | 3.2 |
1. Blood loss (1.1 intraoperative blood loss; 1.2 total blood loss); 2. VAS (2.1 VAS at rest 1 day; 2.2 VAS at rest 2–3 day; 2.3 VAS at rest discharge; 2.4 VAS at activity 1 day; 2.5 VAS at activity 2–3 days; 2.6 VAS at activity discharge); 3. Complications (3.1 lower limb vein thrombosis; 3.2 thigh ecchymosis; 3.3 thigh bullae); 4. Hospital for Special Surgery score; 5. Range of motion; 6. Thigh circumference (6.1 thigh circumference at 1 day; 6.2 thigh ecchymosis at 3 days; 6.2 thigh ecchymosis at 5 days).
The detailed baseline characteristics information, including the number of TKAs, age, gender, BMI, and outcomes of 2 groups.
Table 2.
The detailed information of surgery.
| Author/yr | Diagnosis | Prothesis | Anesthesia | Operation time, min |
| Ishii 2005 | 29OA,1RA/27OA,3RA | Cementless TKA with New Jersey LCS | Spinal | 71/72 |
| Unver 2013 | 17OA/21OA | (Nexgen; Zimmer, Warsaw, IN). | General | NA |
| De Souza Leão 2016 | 30OA/30OA | Modular III (MDT, Rio Claro, SP, Brazil), | Spinal | NA |
| Geng 2014 | 61OA/60OA | NA | NA | NA |
| Lei 2019 | 36OA/35OA | CR Gemi MK (LINK, Germany) | General | NA |
| Si 2018 | 88 OA/82 OA | NA | General | |
| Wu 2014 | 30 OA/30OA | NA | Spinal | NA |
| Zhang 2016 | 80 OA/80OA | NA | General | NA |
| Zhou 2019 | 50 OA/50OA | A3 (AKMEDICAL) | General | NA |
| Pan 2019 | 50 OA/50OA | NA | Spinal | NA |
| Yang 2020 | NA | NA | NA | NA |
| Zhang 2021 | 42 OA/42OA | NA | Spinal | NA |
| Tao 2018 | 40 OA/40OA | NA | Spinal | NA |
The detailed information of surgery including diagnosis, prothesis, anesthesia, and operation time of 2 groups. OA = osteoarthritis.
Table 3.
The tourniquet intervention information.
| Personalized tourniquet pressurel/Conventional tourniquet pressure | ||||
| Author/yr | Mean tourniquet time, min | Mean inflation pressure, mm Hg | Practices of tourniquet pressure | The time for loosening the tourniquet |
| Ishii 2005 | 48/50 | 238/350 | 100 mm Hg above SBP/350 mm Hg | Before the incision was closed |
| Unver 2013 | 60/58.3 | 169.7/304.7 | AOP /300 mm Hg | After the application of a wool and crepe bandage to the limb. |
| De Souza Leão 2016 | 118/110 | NA | 100 mm Hg above SBP/350 mm Hg | After Robert Jones dressing was made |
| Geng 2014 | NA | 245/250 | LOP /250 mm Hg | NA |
| Lei 2019 | 55.79/57.23 | 181.72/270 | LOP /270 mm Hg | After the application of a bandage to the limb. |
| Si 2018 | 59/59 | 340.425/487.5 | LOP/ 487.5 mm Hg | After the application of a bandage to the limb. |
| Wu 2014 | 81.77/81.23 | 360.28/500 | LOP/500 mm Hg | NA |
| Zhang 2016 | 59.61/59.84 | 333/487.5 | LOP/487.5 mm Hg | After the application of a bandage to the limb. |
| Zhou 2019 | NA | NA | LOP/525 mm Hg | After the application of a bandage to the limb. |
| Pan 2019 | NA | NA | 112.5 mm Hg above SBP /450 mm Hg | NA |
| Yang 2020 | NA | 413.83/450 | LOP/450 mm Hg | NA |
| Zhang 2021 | NA | NA | 112.5 mm Hg above SBP /450 mm Hg | After the application of a bandage to the limb. |
| Tao 2018 | NA | NA | 150 mm Hg above SBP /450 mm Hg | After the application of a bandage to the limb |
The tourniquet intervention information including the mean tourniquet time, mean inflation pressure, practices of tourniquet pressure, the time for loosening the tourniquet of 2 groups. LOP = limb occlusion pressure, SBP = systolic blood pressure.
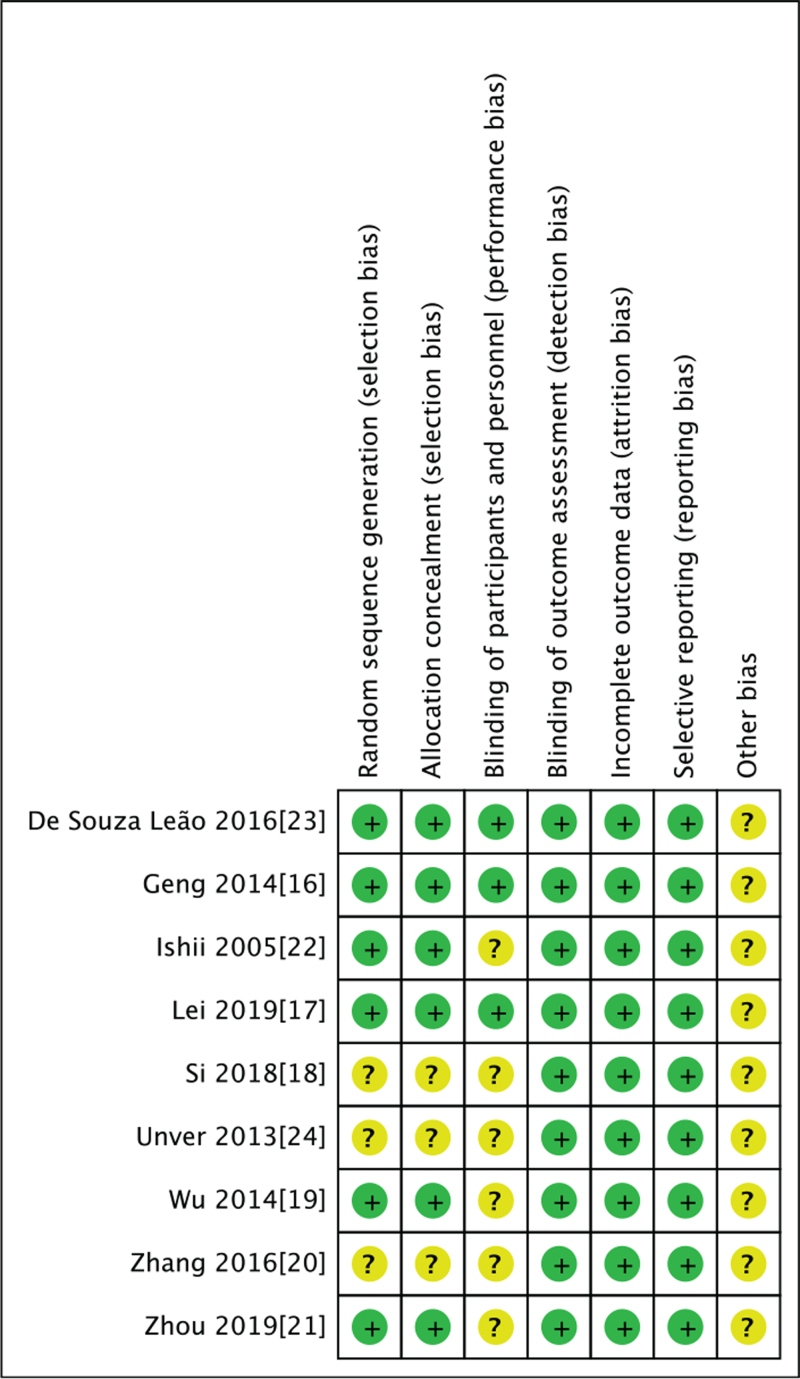
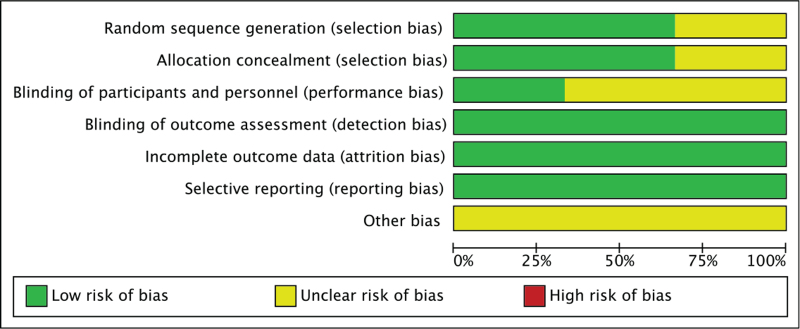
3.2. Risk of bias assessment
The risk of bias summary and bias graph for RCTs is shown in Figs. 2 and 3. The correct randomization and sufficient allocation concealment were adequately described in 10 studies. The blinding of outcome assessment was described in 13 studies, and the blinding of participants and personnel was described in 3 studies. Each study retained complete outcome data and avoided selective reporting. Other potential biases of all studies cannot be ignored. Therefore, we rated them as having an unclear risk of other bias. As a result, the included studies’ overall quality was considered adequate (Figs. 2 and 3).
Figure 2.
The risk of bias summary for RCTs. +: no bias; –: bias; ?: bias unknown. The correct randomization and sufficient allocation concealment were adequately described in 10 studies. The blinding of outcome assessment was described in 13 studies, and the blinding of participants and personnel was described in 3 studies. Each study retained complete outcome data and avoided selective reporting. Other potential biases of all studies cannot be ignored. Therefore, we rated them as having an unclear risk of other bias. As a result, the included studies’ overall quality was considered adequate.
Figure 3.
The risk of bias graph. The overall quality of the studies was considered adequate.
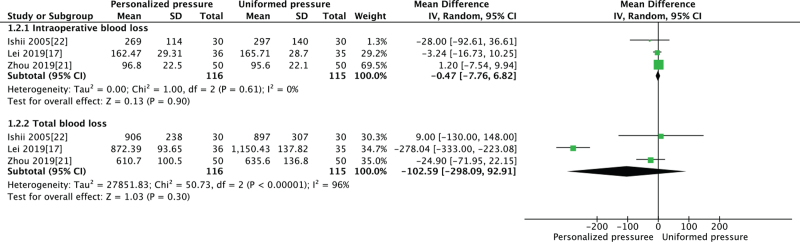
3.3. Pooled analysis of blood loss between the PTIP group and UTIP group
Patients in both groups experienced similar intraoperative blood loss (MD = –1.41, 95% CI [–5.36, 2.54], P = .48, Fig. 4) and total blood loss (MD = –87.23, 95% CI [–206.86, 32.40], P = .15, Fig. 4).
Figure 4.
Pooled analysis of blood loss between the PTIP group and the UTIP group. Patients in both groups experienced similar intraoperative blood loss (MD = –1.41, 95% CI [–5.36, 2.54], P = .48) and total blood loss (MD = –87.23, 95% CI [–206.86, 32.40], P = .15). CI = confidence interval, MD = mean difference, PTIP = personalized tourniquet inflation pressures, UTIP = uniform tourniquet inflation pressure.
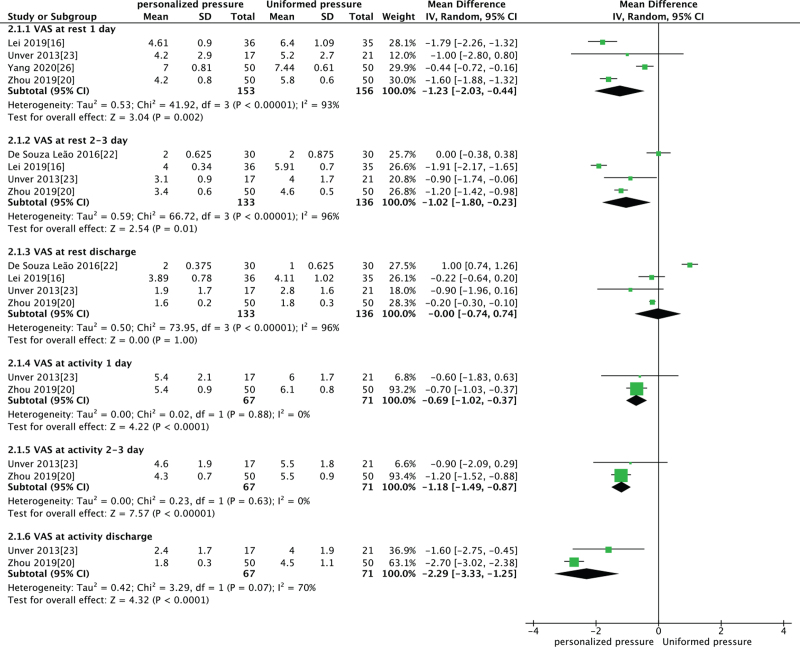
3.4. Pooled analysis of VAS between PTIP group and UTIP group
We were able to detect a significantly lower VAS at rest 1 day after operation (MD = –1.23, 95% CI [–2.03, –0.44], P = .002 Fig. 5), 2 to 3 days after operation (MD = –1.02, 95% CI [–1.8, –0.23], P = .01 Fig. 5) and lower VAS at activity 1 day after operation (MD = –0.69, 95% CI [–1.02, –0.37], P < .0001, Fig. 5), 2 to 3 days after operation (MD = –1.18, 95% CI [–1.49, –0.87], P < .00001, Fig. 5), and discharge (MD = –2.29, 95% CI [–3.33, –1.25], P < .0001, Fig. 5) in patients with personalized pressure group. The results of the meta-analysis showed that patients in both groups experienced similar VAS at rest when discharge from hospital (MD = –0.00, 95% CI [–0.74, 0.74], P = 1.0, Fig. 5).
Figure 5.
Pooled analysis of VAS between PTIP group and UTIP group. In personalized pressure group, there is a significantly lower VAS at rest 1 day after operation (MD = –1.23, 95% CI [–2.03, –0.44], P = .002), 2 to 3 days after operation (MD = –1.02, 95% CI [–1.8, –0.23], P = .01), and lower VAS at activity 1 day after operation (MD = –0.69, 95% CI [–1.02, –0.37], P < .0001), 2 to 3 days after operation (MD = –1.18, 95% CI [–1.49, –0.87], P < .00001) and discharge (MD = –2.29, 95% CI [–3.33, –1.25], P < .0001). Patients in both groups experienced similar VAS at rest when discharge from hospital (MD = –0.00, 95% CI [–0.74, 0.74], P = 1.0). CI = confidence interval, MD = mean difference, PTIP = personalized tourniquet inflation pressures, UTIP = uniform tourniquet inflation pressure, VAS = visual analogue scale.
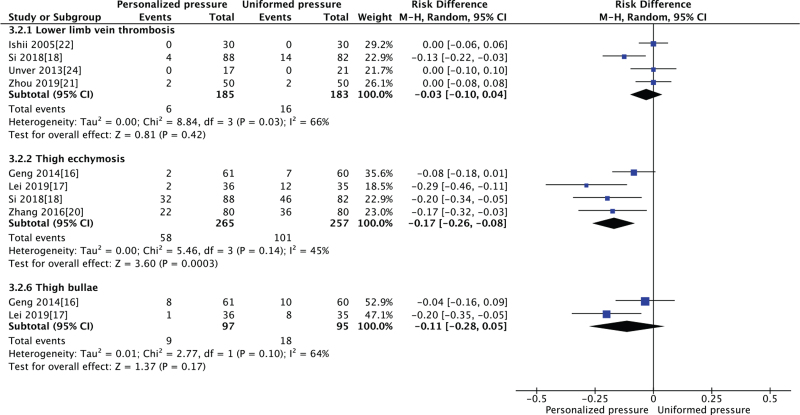
3.5. Pooled analysis of complication rates between PTIP group and UTIP group
Our results showed that patients in both groups experienced similar rates of lower limb vein thrombosis (MD = –0.03, 95% CI [–0.1, 0.04], P = .42, Fig. 6) and thigh bullae (MD = –0.08, 95% CI [–0.17, 0.02], P = .1, Fig. 6), however we also detect a significantly lower rate of thigh ecchymosis (MD = –0.19, 95% CI [–0.24, –0.13], P < .00001; Fig. 6) in patients with personalized pressure group.
Figure 6.
Pooled analysis of complication rates between PTIP group and UTIP group. Both groups experienced similar rates of lower limb vein thrombosis (MD = –0.03, 95% CI [–0.1, 0.04], P = .42) and thigh bullae (MD = –0.08, 95% CI [–0.17, 0.02], P = .1). There is a significantly lower rate of thigh ecchymosis (MD = –0.19, 95% CI [–0.24, –0.13], P < .00001) in patients with personalized pressure group. CI = confidence interval, MD = mean difference, PTIP = personalized tourniquet inflation pressures, UTIP = uniform tourniquet inflation pressure.
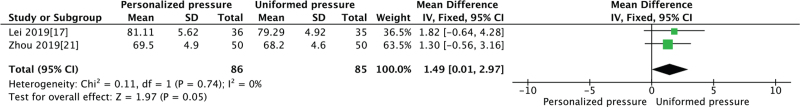
3.6. Pooled analysis of HSS between PTIP group and UTIP group
Our results showed that patients in personalized pressure group experienced higher HSS scores (MD = 1.90, 95% CI [0.51, 3.29], P = .007 Fig. 7).
Figure 7.
Pooled analysis of HSS between PTIP group and UTIP group. In personalized pressure group, there is a significantly higher HSS (MD = 1.90, 95% CI [0.51,3.29], P = .007). CI = confidence interval, HSS = hospital for special surgery, MD = mean difference, PTIP = personalized tourniquet inflation pressures, UTIP = uniform tourniquet inflation pressure.
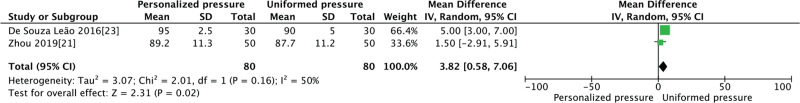
3.7. Pooled analysis of ROM between PTIP group and UTIP group
We detected a significantly better knee ROM (MD = 3.82, 95% CI [0.58, 7.06], P = .02; Fig. 8) in patients with personalized pressure group.
Figure 8.
Pooled analysis of ROM between PTIP group and UTIP group. There is significantly better knee ROM (MD = 3.82, 95% CI [0.58, 7.06], P = .02) in patients with personalized pressure group. CI = confidence interval, MD = mean difference, PTIP = personalized tourniquet inflation pressures, ROM = range of motion, UTIP = uniform tourniquet inflation pressure.
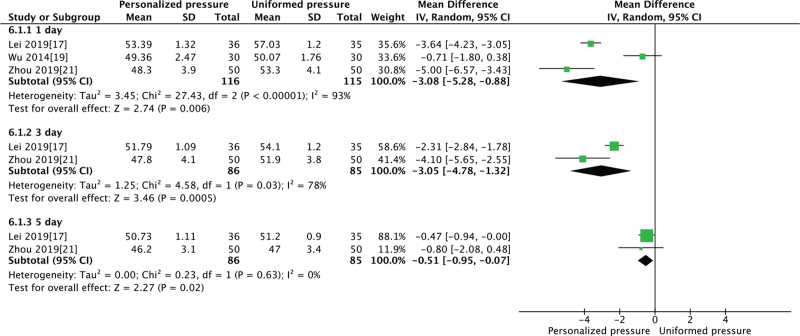
3.8. Pooled analysis of thigh circumference between PTIP group and UTIP group
We detected a significantly shorter thigh circumference 1 day after operation (MD = –3.08, 95% CI [–5.28, –0.88], P = 0.006; Fig. 9), 3 days after operation (MD = –3.05, 95% CI [–4.78, –1.32], P = .0005; Fig. 9) and 5 days after operation (MD = –0.51, 95% CI [–0.95, –0.07], P = .02; Fig. 9) in patients with personalized pressure group.
Figure 9.
Pooled analysis of thigh circumference between PTIP group and UTIP group. Thigh circumference is significantly shorter 1 day after operation (MD = –3.08, 95% CI [–5.28, –0.88], P = .006), 3 days after operation (MD = –3.05, 95% CI [–4.78, –1.32], P = .0005) and 5 days after operation (MD = –0.51, 95% CI [–0.95, –0.07], P = .02) in patients with personalized pressure group. CI = confidence interval, MD = mean difference, PTIP = personalized tourniquet inflation pressures, UTIP = uniform tourniquet inflation pressure.
4. Discussion
Although clinical efforts and advances in tourniquet technology have resulted in the use of lower inflation pressures, there was no meta-analysis comparing the effects of PTIP with UTIP on rehabilitation outcomes and postoperative complications. Our meta-analysis is the first meta-analysis to compare the impact of PTIP with conventional UTIP during TKA. The current meta-analysis's main finding was that both PTIP and conventional UTIP ensure equal blood loss in total knee arthroplasty. No significant difference was observed between the groups in terms of rate of lower limb vein thrombosis, and thigh bullae. However, in patients using a tourniquet with PTIP, we found a significant reduction in postoperative pain, thigh circumference, rate of thigh ecchymosis, higher HSS, and a better initial recovery of knee flexion.
The present work analysis was not able to identify any differences between the 2 groups in the case of intraoperative blood loss and total blood loss. These findings mean PTIP would provide a bloodless surgical field comparable to conventional UTIP.
Immediate postoperative pain relief following TKA is crucial in facilitating early recovery. We were able to detect a significantly lower pain intensity within 3 days after operation both at rest and during mobilization in patients with PTIP group. We also identified a significantly lower pain intensity at the activity when patients were at discharge; however, we could not identify any difference of pain intensity at rest when patients left the hospital. An explanation for the increased pain in the early postoperative period with conventional uniform pressure group could be direct higher pressure on the surrounding soft tissues due to the tourniquet. In our study, the pressure of the PTIP is lower than the conventional UTIP group. Worland et al[28] showed an essential correlation between tourniquet pressure and thigh pain in the immediate postoperative period. We thought that the PTIP lowers pain levels while increasing patients’ adherence to rehabilitation, which resulted in earlier restoration in functions.
In patients using a tourniquet with PTIP, we found a significant reduction in thigh circumference. We think the reason may be due to less stress on the thigh muscles in the PTIP group.
Knee flexion ROM is often used to evaluate short-term effectiveness. Besides, discharge from the hospital is dependent on the mobility of patients following TKA. The PTIP group documented a significantly higher postoperative ROM. It may be related to using a conventional UTIP with higher tourniquet pressure that causes some temporary loss of flexibility in the tight thigh muscles. The PTIP group also reveal a higher HSS score. The reason may be less pain, more knee ROM in the PTIP group.
As for complications, all studies did not experience major significant complications such as symptomatic PE, thigh necrosis, nerve palsy, or delayed rehabilitation. We found no significant difference between groups regarding the rate of lower limb vein thrombosis and thigh bullae. However, in patients using a tourniquet with personalized tourniquet inflation, we found a significant reduction in the quality of thigh ecchymosis. It is possible to achieve functional benefits with decreasing some complications related to the tourniquet and to have the advantages as with the personalized tourniquet application.
The pressure for safe tourniquet use remains controversial, and no strict guidelines have been established. Most of the orthopedic surgeons routinely apply fixed tourniquet pressure in TKA based on individual experiences. It was very convenient to choose the fixed pressure value. However, it did not take patients’ actual individual situation into account, so the selected pressure values were mostly on the high side. Some researchers suggested that upper limb pressure in an adult is 250 to 300 mm Hg, and lower limb pressure is 350 to 500 mm Hg.[29] A higher tourniquet pressure ensures the reliable function of the tourniquet; however, it may lead to a higher incidence of complications. The pressures higher than 350 mm Hg on the lower limbs increase neuropraxia and compression.[8,13] While a lower tourniquet pressure is safer than higher pressure, it may not provide a bloodless operative field. Optimal tourniquet pressure should be determined to balance safety and efficacy. In recent years, some investigators proposed that the tourniquet pressure setting should be personalized. Compression pressure on a pneumatic tourniquet's limb artery wall is different due to different physiological functions, such as systolic blood pressure, age, weight, limb circumference size, and muscle tissue thickness.
Setting the tourniquet pressure based on SBP or LOP allows us to use a personalized tourniquet pressure in each patient and is useful in optimizing tourniquet cuff pressures. The tourniquet beyond the SBP, allowed a certain amount of safety margin, which added to the SBP ranges widely, from 100 to 150 mm Hg in total knee arthroplasty.[21,28,30–35] LOP is the term that mean the lowest tourniquet pressure is required to cease the arterial blood flow into the extremity distal to the cuff. LOP can be determined automatically or manually by slow cuff inflation to pulse cessation with diagnostic equipment such as Doppler flowmeter or pulse oximeter.[36–39] Now, modern tourniquet systems permit an automated LOP estimation through a probe incorporated in the tourniquet system itself.[4] One cuff pressure setting method that has been used successfully in clinical studies is LOP + 40 mm Hg for LOP levels <130 mm Hg, LOP + 60 mm Hg for LOP levels between 131 and 190 mm Hg, and LOP + 80 mm Hg for LOP levels >190 mm Hg.[4,40]
Following an analysis of the current literature, this work demonstrated a relative predominance of the advantages when a tourniquet is used with the personalized application. However, the present meta-analysis has several limitations: first, there are 2 methods for personalized tourniquets, including SBP and LOP. Because of the limited data, we were not able to evaluate one of them separately. We performed a sensitivity analysis on them and found that the conclusion is stable when removing one method. Second, the studies’ comparability was complicated through the different measurement methods and follow-up examination time points; however, we have tried our best to evaluate results based on time points. Third, the tourniquet time, the time for loosening the tourniquet, and the cuff pressure used were also not uniform (see Table 1). Fourth, there are no worldwide uniform guidelines for performing total knee arthroplasty. Different surgical techniques (such as the selection of approach, methods of anesthesia, drainage patterns hemostasis, and anticoagulation regimens) were used in the individual studies. Fifth, some of the RCTs were not registered in the Trial registration which may cause bias.
5. Conclusion
In conclusion, personalized tourniquet inflation pressure provides a bloodless surgical field comparable to that of a conventional uniformed method with less pain intensity, thigh circumference, rate of thigh ecchymosis, higher HSS, and better initial recovery knee flexion in total knee arthroplasty. Therefore, we recommend using personalized tourniquet inflation pressure during TKA. When use the tourniquet inflation pressure based on SBP, we can select the pressure 100 to 150 mm Hg beyond SBP. When we use the tourniquet inflation pressure based on LOP, the cuff pressure is LOP + 40 mm Hg for LOP levels <130 mm Hg, LOP + 60 mm Hg for LOP levels between 131 and 190 mm Hg, and LOP + 80 mm Hg for LOP levels >190 mm Hg. Due to the limited comparability of the studies available, more longer follow-up period and overall higher quality RCTs are needed to confirm the present meta-analysis results.
Author contributions
Conceptualization: Xu Cai, Yonggang Zhou.
Data curation: Changjiao Sun, Xin Yang, Xiaofei Zhang, Qi Ma.
Formal analysis: Changjiao Sun, Xiaofei Zhang.
Investigation: Changjiao Sun, Xin Yang, Qi Ma, Peng Yu.
Methodology: Peng Yu.
Project administration: Qi Ma, Peng Yu.
Resources: Xiaofei Zhang, Qi Ma.
Software: Changjiao Sun, Xiaofei Zhang, Peng Yu.
Supervision: Changjiao Sun, Xiaofei Zhang, Xu Cai, Yonggang Zhou.
Validation: Changjiao Sun.
Writing – original draft: Changjiao Sun.
Writing – review & editing: Changjiao Sun, Xu Cai, Yonggang Zhou.
Footnotes
Abbreviations: CIs = confidence intervals, HSS = hospital for special surgery, LOP = limb occlusion pressure, PTIP = personalized tourniquet inflation pressures, RCTs = randomized controlled trials, ROM = range of motion, SBP = systolic blood pressure, TKA = total knee arthroplasty, UTIP = uniform tourniquet inflation pressure.
How to cite this article: Sun C, Yang X, Zhang X, Ma Q, Yu P, Cai X, Zhou Y. Personalized tourniquet pressure may be a better choice than uniform tourniquet pressure during total knee arthroplasty: a PRISMA-compliant systematic review and meta-analysis of randomized-controlled trials. Medicine. 2022;101:8(e28981).
XC and YZ contributed equally to this work.
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Availability of data and materials: The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
The authors declare that they have no competing interests.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Noordin S, McEwen JA, Kragh JF, Jr, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am 2009;91:2958–67. [DOI] [PubMed] [Google Scholar]
- [2].Odinsson A, Finsen V. Tourniquet use and its complications in Norway. J Bone Joint Surg Br 2006;88:1090–2. [DOI] [PubMed] [Google Scholar]
- [3].Olivecrona C, Blomfeldt R, Ponzer S, Stanford BR, Nilsson BY. Tourniquet cuff pressure and nerve injury in knee arthroplasty in a bloodless field: a neurophysiological study. Acta Orthop 2013;84:159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Olivecrona C, Ponzer S, Hamberg P, Blomfeldt R. Lower tourniquet cuff pressure reduces postoperative wound complications after total knee arthroplasty: a randomized controlled study of 164 patients. J Bone Joint Surg Am 2012;94:2216–21. [DOI] [PubMed] [Google Scholar]
- [5].Berry DJ, Bozic KJ. Current practice patterns in primary hip and knee arthroplasty among members of the American Association of Hip and Knee Surgeons. J Arthroplasty 2010;25: (6 suppl): 02–4. [DOI] [PubMed] [Google Scholar]
- [6].Parvizi J, Diaz-Ledezma C. Total knee replacement with the use of a tourniquet: more pros than cons. Bone Joint J 2013;95-B: (11 suppl A): 133–4. [DOI] [PubMed] [Google Scholar]
- [7].Sadri A, Braithwaite IJ, Abdul-Jabar HB, Sarraf KM. Understanding of intra-operative tourniquets amongst orthopaedic surgeons and theatre staff--a questionnaire study. Ann R Coll Surg Engl 2010;92:243–5. quiz 1p following 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sharma JP, Salhotra R. Tourniquets in orthopedic surgery. Indian J Orthop 2012;46:377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Yalcinkaya M, Sokucu S, Erdogan S, Kabukcuoglu YS. Tourniquet use in orthopedic surgery: a descriptive survey study among Turkish orthopedic surgeons and residents in Istanbul. Acta Orthop Traumatol Turc 2014;48:483–90. [DOI] [PubMed] [Google Scholar]
- [10].Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop 2002;26:306–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mittal R, Ko V, Adie S, et al. Tourniquet application only during cement fixation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg 2012;82:428–33. [DOI] [PubMed] [Google Scholar]
- [12].Bould M, Freeman BJ, Pullyblank A, Newman JH. Blood loss in sequential bilateral total knee arthroplasty. J Arthroplasty 1998;13:77–9. [DOI] [PubMed] [Google Scholar]
- [13].Wakankar HM, Nicholl JE, Koka R, D’Arcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br 1999;81:30–3. [DOI] [PubMed] [Google Scholar]
- [14].Barwell J, Anderson G, Hassan A, Rawlings I. The effects of early tourniquet release during total knee arthroplasty: a prospective randomized double-blind study. J Bone Joint Surg Br 1997;79:265–8. [DOI] [PubMed] [Google Scholar]
- [15].Geng J, Zhao P, Cheng J, et al. Effect of lower tourniquet cuff pressure on reducing incision complications after total knee arthroplasty. Chin J Bone Joint Inj 2014;29:605–6. [Google Scholar]
- [16].Lei Y, Li H, Zhang J, Mei B, Tao H. Personalized tourniquet pressure setting for total knee arthroplasty. Orthop J China 2019;27:1385–9. [Google Scholar]
- [17].Si F. Application of individualized pressure value of inflatable tourniquet in knee arthroplasty. Shanghai Nurs J 2018;18:45–7. [Google Scholar]
- [18].Wu Z, Yang P, Guo Y, Feng Q, Jin L. Study on individualized pressure nursing of pneumatic tourniquet during knee surface replacement. Jilin Med J 2014;35:7461–3. [Google Scholar]
- [19].Zhang H, Chen M, Tai C. Application effect of individualized pressure value of inflatable tourniquet in total knee arthroplasty. Anhui Med J 2016;37:1292–3. [Google Scholar]
- [20].Zhou J, Hu W, Hu S, et al. Application of personalized tourniquet pressure in primary total knee arthroplasty. J Clin Rehabil Tis Eng Res 2019;23:3136–42. [Google Scholar]
- [21].Ishii Y, Matsuda Y. Effect of tourniquet pressure on perioperative blood loss associated with cementless total knee arthroplasty: a prospective, randomized study. J Arthroplasty 2005;20:325–30. [DOI] [PubMed] [Google Scholar]
- [22].de Souza Leao MG, Neta GP, Coutinho LI, da Silva TM, Ferreira YM, Dias WR. Comparative analysis of pain in patients who underwent total knee replacement regarding the tourniquet pressure. Rev Bras Ortop 2016;51:672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Unver B, Karatosun V, Tuncali B. Effects of tourniquet pressure on rehabilitation outcomes in patients undergoing total knee arthroplasty. Orthop Nurs 2013;32:217–22. [DOI] [PubMed] [Google Scholar]
- [24].Anna P, Jinfu H, Yanling L. Influence of personalized electric pneumatic tourniquet pressure setting on total knee arthroplasty. Chin J Mod Drug Appl 2019;13:80–1. [Google Scholar]
- [25].Tao J, Yao H, Peng H, Xu H. Application of individualized electric pneumatic tourniquet pressure in total knee arthroplasty. Mod Nurs 2018;25:134–5. [Google Scholar]
- [26].Yang Y, Gao X, Yu L, Liu H, Wu H, Yao C. Research of the pressure value setting of tourniquet based on blood oxygen monitor in elderly patients with total knee arthroplasty. China Med Equip 2020;17:132–5. [Google Scholar]
- [27].Zhang L, Ju R. Influence of different pressure parameters of pneumatic tourniquet on patients undergoing knee arthroplasty. Pract J Med Pharm 2021;38:57–9. [Google Scholar]
- [28].Worland RL, Arredondo J, Angles F, Lopez-Jimenez F, Jessup DE. Thigh pain following tourniquet application in simultaneous bilateral total knee replacement arthroplasty. J Arthroplasty 1997;12:848–52. [DOI] [PubMed] [Google Scholar]
- [29].Recommended practices for use of the pneumatic tourniquet. Aorn j 2002;75:379–82. 84–86. [DOI] [PubMed] [Google Scholar]
- [30].Clarke MT, Longstaff L, Edwards D, Rushton N. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br 2001;83:40–4. [DOI] [PubMed] [Google Scholar]
- [31].Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg 2001;44:33–8. [PMC free article] [PubMed] [Google Scholar]
- [32].Mu J, Liu D, Ji D, et al. Determination of pneumatic tourniquet pressure of lower limb by ultrasonic Doppler. Ann Plast Surg 2018;80:290–2. [DOI] [PubMed] [Google Scholar]
- [33].Kim TK, Bamne AB, Sim JA, Park JH, Na YG. Is lower tourniquet pressure during total knee arthroplasty effective? A prospective randomized controlled trial. BMC Musculoskelet Disord 2019;20:275.1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Manén Berga F, Novellas Canosa M, Anglès Crespo F, Bernal Dzekonski J. [Effect of ischemic tourniquet pressure on the intensity of postoperative pain]. Rev Esp Anestesiol Reanim 2002;49:131–5. [PubMed] [Google Scholar]
- [35].Ishii Y, Noguchi H, Matsuda Y, Takeda M, Higashihara T. A new tourniquet system that determines pressures in synchrony with systolic blood pressure in total knee arthroplasty. J Arthroplasty 2008;23:1050–6. [DOI] [PubMed] [Google Scholar]
- [36].Masri BA, Day B, Younger AS, Jeyasurya J. Technique for measuring limb occlusion pressure that facilitates personalized tourniquet systems: a randomized trial. J Med Biol Eng 2016;36:644–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].McLaren AC, Rorabeck CH. The pressure distribution under tourniquets. J Bone Joint Surg Am 1985;67:433–8. [PubMed] [Google Scholar]
- [38].Reid HS, Camp RA, Jacob WH. Tourniquet hemostasis. A clinical study. Clin Orthop Relat Res 1983;(177):230–4. [PubMed] [Google Scholar]
- [39].Younger AS, Manzary M, Wing KJ, Stothers K. Automated cuff occlusion pressure effect on quality of operative fields in foot and ankle surgery: a randomized prospective study. Foot Ankle Int 2011;32:239–43. [DOI] [PubMed] [Google Scholar]
- [40].Younger AS, McEwen JA, Inkpen K. Wide contoured thigh cuffs and automated limb occlusion measurement allow lower tourniquet pressures. Clin Orthop Relat Res 2004;(428):286–93. [DOI] [PubMed] [Google Scholar]