Abstract
Background:
Osteoarthritis of the knee is one of the major disorders leading to social dysfunction, economic loss and social development. This study was conducted to systematically evaluate the efficacy and safety effectiveness of acupuncture inactivation of myofascial pain trigger points in the treatment of osteoarthritis of the knee.
Methods:
Randomized Controlled Trials (RCTs) on the treatment of knee pain were searched by computer from PubMed, The Cochrane Library, China journal full-text database (CNKI), Chinese biomedical literature database (CBM), China academic journal database (Wanfang Data) databases from the date of creation to December 2021, and the data were analyzed by Reman 5.3 software for data analysis.
Results:
A total of 724 patients from 9 RCTs were finally included, and the results of meta-analysis showed that the acupuncture myofascial pain trigger point group was better than the control group in terms of total effective rate, cure rate, VAS score, Lysholm score, and WOMAC score.
Conclusion:
The efficacy and safety of acupuncturing myofascial pain trigger points in the treatment of knee osteoarthritis is positive, but due to the limited number of literature included in this study and the low quality of the included literature, there is still a need for high-quality and large sample size RCTs for the analysis of this treatment option.
Keywords: acupuncture, knee osteoarthritis, meta-analysis, myofascial pain trigger points, systematic evaluation
1. Introduction
Knee osteoarthritis (KOA) is a chronic degenerative joint disease characterized by degeneration of articular cartilage.[1–3] Degenerative changes in articular cartilage often involve synovial membrane, ligaments, and other tissues leading to decreased stability of the knee joint, resulting in biomechanical imbalance of the knee joint thus causing pain and activity dysfunction around the knee joint clinical symptoms, which seriously affects the quality of life of middle-aged and elderly people, and is one of the main diseases that cause functional disability, economic loss and affect social development of the society.[4,5] Therefore, the search for a reliable and affordable treatment has become a focus of our attention.
In recent years, some scholars around the world have begun to pay attention to the relationship between injury and repair of soft tissues around the knee joint, and proposed that “muscle dysfunction” is the key to the development of knee osteoarthritis and the course of the disease.[6–9] The myofascial pain trigger point theory has become a hot topic of research for scholars, and numerous studies have shown that inactivation of myofascial pain trigger points around the knee joint can promote structural remodeling of the surrounding skeletal muscle to regulate the biomechanical balance, thus improving the clinical symptoms of knee osteoarthritis and providing a new direction for the conservative treatment of knee osteoarthritis,[10,11] therefore, this study used an evidence-based approach to evaluate the efficacy and safety of acupuncture myofascial pain trigger points for the treatment of KOA. In this study, the efficacy and safety of acupuncturing myofascial pain trigger points in the treatment of KOA were evaluated using an evidence-based approach to provide a scientific basis for the clinical efficacy of acupuncturing myofascial pain trigger points in the treatment of KOA.
2. Materials and methods
2.1. Search method
We searched a total of 5 databases through a comprehensive search of PubMed, The Cochrane Library, the China Journal Full Text Database (CNKI), the China Biomedical Literature Database (CBM), and the China Academic Journal Database (Wanfang Data), with self-built databases searched up to December 2021. We will use a combination of medical subject headings terms and free words to search the articles. Subject words include “acupuncture” or “acupuncture” and “myofascial pain trigger point” or “myofascial trigger point” or “myalgia” and “knee osteoarthritis” or “knee degenerative joint” or “patellofemoral joint pain” or “knee joint pain”. At the same time, references of included articles will be manually retrieved. We will adjust different search strategies for different databases.
2.2. Inclusion criteria
2.2.1. Study type
Clinical randomized controlled trials in Chinese or English only, whether take measures to use blinding and allocation concealment or not.
2.2.2. Intervention
The intervention of the experimental group use acupuncture to inactivate myofascial pain trigger points, The intervention of the control group was not limited
2.2.3. Participants
The included patients were diagnosed with osteoarthritis of the knee and patellofemoral osteoarthritis pain.
2.3. Exclusion criteria
Duplicate articles.
Unable to get data or data is incomplete.
Nonrandomized controlled trials, case report, review article, and animal experiment.
2.4. Outcomes
Clinical efficacy (including total effective rate and cure rate), visual analog score (VAS score), Lysholm score, WOMAC score, and adverse effects.
3. Results
3.1. Study selection
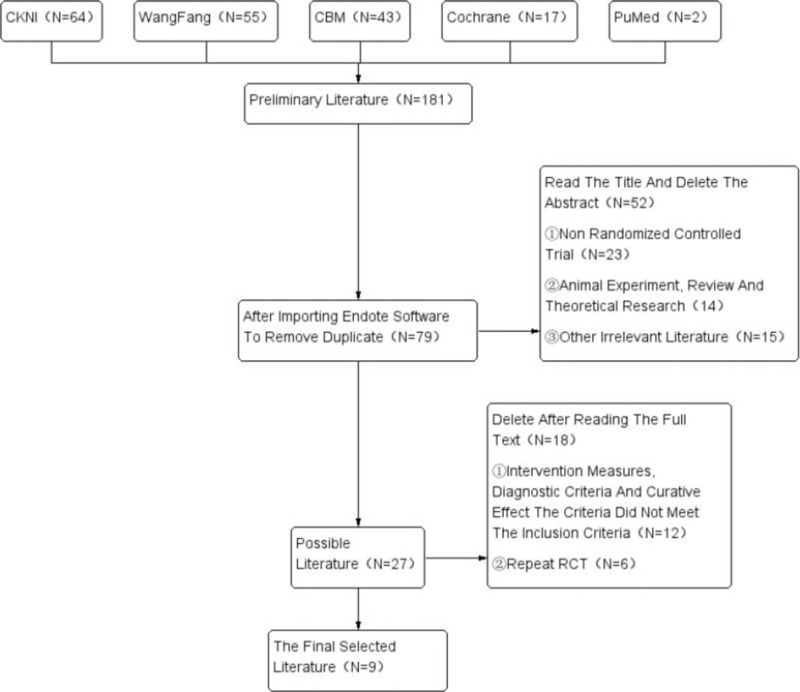
We will filter the studies level by level by eliminating duplicates, reading titles and abstracts, and reading the full text. The study screening will be completed independently by 2 researchers, and the third researcher will be responsible for the judgment in case of differences. The literature screening flow chart is shown in Figure 1.
Figure 1.
Flow chart of literature search. CBM = Chinese biomedical literature database, CKNI = China national knowledge infrastructure, RCT = randomized controlled trial.
3.2. Data extraction
We will use a homemade table to collect the following data included in the article (Table 1).
Table 1.
Basic characteristics of KOA studies with acupuncture myofascial pain trigger points for treatment.
| Included literature | Sample size | Interventions | |||||
| Author | Particular year | T/C | Treatment group | Control group | Observation index | Treatment cycle | Drop out |
| Wu Yanbin[14] | 2020 | 30/30 | A+B | Electrotherapy of pain points+B | VAS, Lysholm, Q angle, clinical effective rate | Twice a week, 6 times | Nothing |
| Zeng Wenbi[15] | 2019 | 30/32 | A+B | Oral loxoprofen | VAS, Lysholm, clinical effective rate | 6 times a week, 12 times | Nothing |
| Qin Weikai[16] | 2020 | 38/38 | A | Intra articular injection of sodium hyaluronate | VAS, tenderness value of the most obvious pain point in front of the knee, Lysholm, clinical effective rate | Treatment group: twice a week, 4 wks; control group: once a week, 5 times. | Nothing |
| Zhou You[17] | 2018 | 66/65 | A+B | Electroacupuncture+B | WHOQOL-BRIEF, WOMAC, VAS, Lysholm, clinical effective rate | Once a week, 3 times | Nothing |
| Zhang Wenjing[18] | 2015 | 50/50 | A | Acupuncture at traditional meridians | VAS, Lysholm, WOMAC, clinical effective rate | Once a day, 28 times, after 14 times, rest for 2 days | Nothing |
| Yin Jianhua[19] | 2019 | 54/54 | B+A | B+Computer medium frequency electricity | WOMAC, WHOQOL- BRIEF, VAS, Lysholm | Electrotherapy adjustment, once a week, 20 min" muscle stretching: 5 times a week, 3 wks | Nothing |
| Zhao Jiamin[20] | 2018 | 25/23 | A+B | Therapeutic instrument treatment | VAS, KOOS, WOMAC, clinical effective rate, 60°/s relative peak torque of extensor and flexor of knee joint, average power and total power | Acupuncture once a week for 6 wks Stretch 1 min/time, 3 times/d | 2 |
| Ma Yantao[21] | 2018 | 25/23 | A+B | False acupuncture at myalgia point+B | NPRS, knee joint ROM, Lysholm, isokinetic muscle strength test, surface electromyography test | Acupuncture once a week for 6 wks, Stretch 1 min/time, 3 times/d | 2 |
| Zhang Peng[22] | 2016 | 46/45 | A | Acupuncture at traditional meridians | VAS, WOMAC, efficacy evaluation | 30 min/time, once a day, 5 days as a course of treatment, continuous treatment for 4 courses; | Nothing |
| A = Acupuncture at myalgia points | B = Muscle drafting | ||||||
KOA = knee osteoarthritis, VAS = visual analog score.
First author and time of publication, publish journals, and so on.
Sample size, sex ratio, age, course of disease, course of treatment, country, etc of the experimental group, and the control group, among others.
Specific interventions for the experimental and control groups, among others.
Outcome indicators include primary outcome indicators and secondary outcome indicators
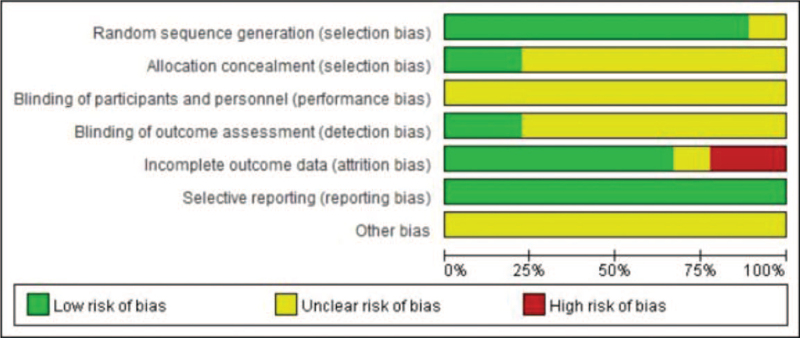
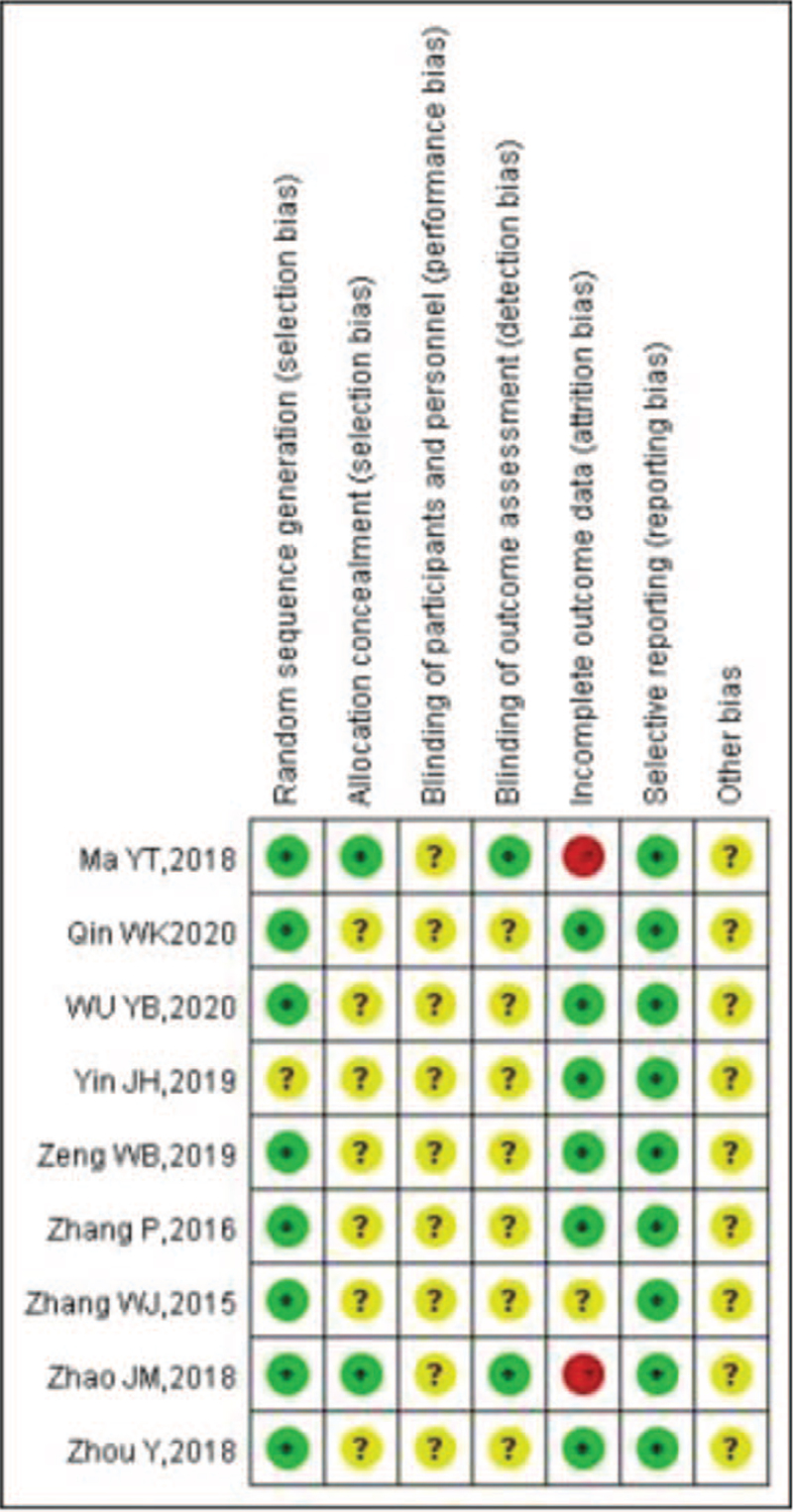
3.3. Risk of bias assessment
The 2 researchers will independently use Cochrane Risk of Bias Tool to assess risk bias in 7 areas: generation of random-allocation methods, allocation concealment, application of blind methods, completeness of outcomes, selective reporting, and other bias risks. The risk bias of included articles will be divided into 3 levels: high, unclear, or low. A third researcher will make the judgment if 2 researchers disagree on an assessment. Risk of bias assessment is shown in Figures 2 and 3.
Figure 2.
Risk bias analysis.
Figure 3.
Summary of bias analysis.
3.4. Evidence assessed
We will use the internationally accepted Grades of Recommendations Assessment, Development and Evaluation (GRADE) to assess the quality of evidence for the article, which is divided into 4 levels: high, medium, low, and very low.
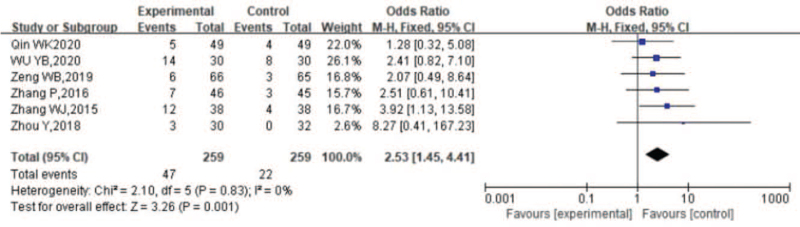
3.5. Total clinical efficiency
Figure 4 indicates that the 6 included RCTs reported the overall effectiveness of acupuncturing myofascial pain trigger points for KOA, with significant heterogeneity among the 6 RCTs (P = .83, I2 = 0%), and the random-effects model showed that the treatment group was superior to the control group in improving clinical outcomes in knee KOA (SMD = 2.53, 95% cl (1.45,4.41), Z = 3.26, P = .83).
Figure 4.
Meta-analysis of clinical efficacy of acupuncturing myofascial pain trigger points for KOA. KOA = knee osteoarthritis.
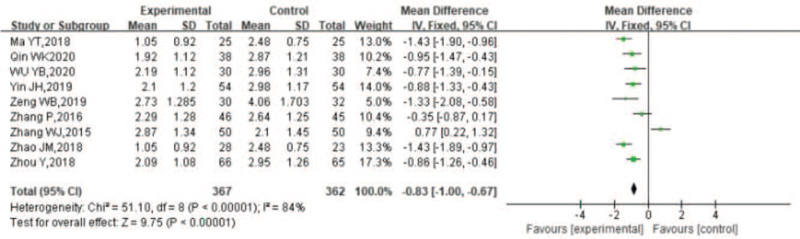
3.6. VAS scores
Figure 5 indicates that the 9 included RCTs reported VAS scores for KOA treated with acupuncture myofascial pain trigger points, with significant heterogeneity among the 9 RCTs (P < .00001, I2 = 84%), and a random-effects model showed that the treatment group was superior to the control group in improving VAS scores for knee KOA (SMD = –0.83, 95% cl (–1.00, –0.67), Z = 9.75, P < .00001).
Figure 5.
Meta-analysis of VAS scores for KOA treated with acupuncture inactivation of myofascial pain trigger points. KOA = knee osteoarthritis, VAS = visual analog score.
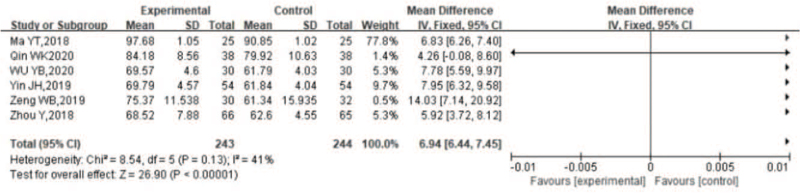
3.7. Lysholm scores
Figure 6 represents the 6 included RCTs reporting Lysholm scores for acupuncturing myofascial pain trigger points for KOA, with significant heterogeneity among the 6 RCTs (P = .13, I2 = 41%) and a random effects model showing that the treatment group was superior to the control group in improving Lysholm scores for knee KOA (SMD = 6.94, 95% cl (6.44, 7.45), Z = 26.90, P < .00001).
Figure 6.
Meta-analysis of Lysholm scores of myofascial pain trigger points treated with acupuncture inactivation for KOA. KOA = knee osteoarthritis.
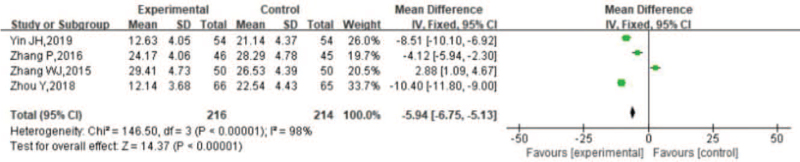
3.8. WOMAC scores
Figure 7 represents the 4 included RCTs reporting WOMAC score for KOA treated with acupuncture myofascial pain trigger points, with significant heterogeneity among the 4 RCTs (P < .00001, I2 = 98%), and a random effects model showing that the treatment group outperformed the control group in improving knee KOA WOMAC score scores (SMD = –5.94, 95% cl (–6.75, –5.13), Z = 14.37, P < .00001)
Figure 7.
Meta-analysis of WOMAC scores for KOA treated with acupuncture inactivation of myofascial pain trigger points. KOA = knee osteoarthritis.
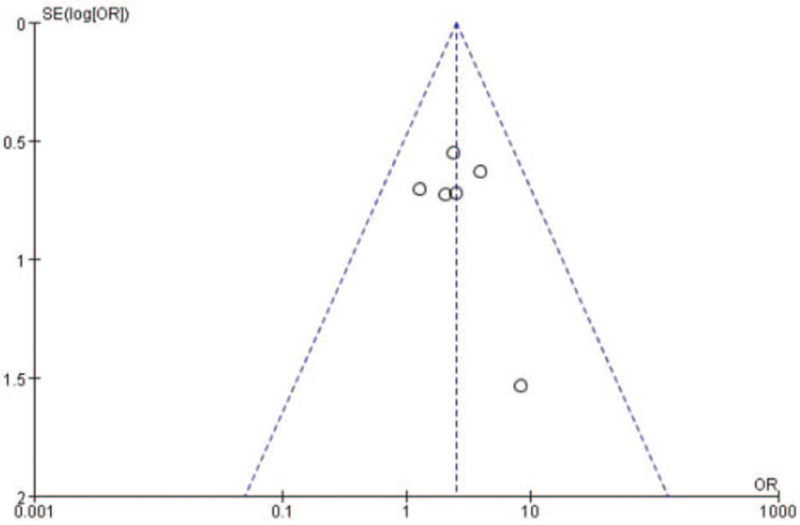
3.9. Risk of bias assessment
Figure 8 shows the funnel plot publication risk analysis based on the total effective rate, and the 6 RCTs show an asymmetric distribution on both sides of the center line of the funnel plot, indicating the existence of bias assessment.
Figure 8.
Funnel plot of publication bias based on total efficiency.
4. Data analysis
The article will be conduct with Revman5.3.0 (https://revman5.software.informer.com/) recommended by Cochrane Collaboration. χ2 test and I2 will be used to analyze the heterogeneity differences among the included articles. When P < .05, I2 > 50% the fixed-effect model is used; otherwise, the random-effect model is used. Dichotomous variables will be expressed as relative risk and their 95% confidence interval (95% CI), whereas continuous variables were expressed as mean difference or standardized mean difference and their 95% CI. We will conduct subgroup analysis or sensitivity analysis for studies with large heterogeneity to reduce the impact of heterogeneity differences.
4.1. Ethics
As the data source of this study is from the literature of major databases, it does not involve the recruitment of patients or the collection of personal information, so the sanction of the ethics committee is unnecessary.
5. Discussion
Osteoarthritis of the knee is a chronic degenerative osteoarthritic disease, which often brings about knee pain and limited joint movement, and in severe cases, the knee cannot be fully straightened; walking with a weak leg, which may be accompanied by knee inversion or knee valgus deformity, or in more severe cases, the inability to walk. In recent years, some scholars at home and abroad have begun to pay attention to the relationship between soft tissue injury and repair around the knee joint, and proposed that “muscle dysfunction” is the key to the development of knee osteoarthritis and its course,[5] in which myofascial pain trigger points are often generated by soft tissue injury, resulting in an imbalance of skeletal muscle mechanics around the knee joint. A large number of studies have shown that inactivation of myofascial pain trigger points around the knee is the key to conservative treatment of knee osteoarthritis, and Professor Huang Qiangmin et al[12,13] concluded that inactivation of myofascial pain trigger points around the knee can reduce intramuscular hypertension, relieve uneven skeletal muscle pull, and improve mechanical balance, thereby relieving Rahbar et al[11] divided KOA patients into 2 groups, the control group was treated with 16 conventional physiotherapy treatments and the intervention group was treated with the same physiotherapy treatments for the area around the knee joint where MTrPs were present, the results showed that the recovery of knee KOA in the intervention group was higher than that in the control group. recovery was higher than that of the control group.
In this study, a total of 181 publications were finally obtained by means of Chinese and English database searches as well as manual searches. The results of the Meta-analysis showed that the treatment group had better overall clinical efficiency, cure rate, VAS score, Lysholm score, and WOMAC score than the control group in the treatment of knee osteoarthritis. In terms of adverse events, there were only 2 cases of shedding for personal reasons in each control group in 2 RCTs, and no adverse reactions occurred in 7 RCTs, and the rest were not mentioned. This indicates that acupuncture inactivates periprosthetic myofascial pain trigger points for the clinical treatment of osteoarthritis of the knee with high safety. Based on this study, we concluded that acupuncture inactivation of myofascial pain trigger points is a clinically effective, rapid, precise, and safe treatment method for intervention of knee osteoarthritis. At the same time, this study has the shortcomings of low quality of included studies and small sample size, so high quality and large sample of RCTs are needed to validate it.
Author contributions
Conceptualization: TianZhong Peng, Xingzhen Lin.
Data curation: Fei Li, Hualong Lu, Manhua Zhu, TianZhong Peng
Formal analysis: TianZhong Peng, Fei Li, Hualong Lu
Investigation: Xingzhen Lin.
Resources: Xingzhen Lin.
Software: TianZhong Peng.
Supervision: Manhua Zhu, TianZhong Peng.
Writing – original draft: TianZhong Peng, Xingzhen Lin.
Writing – review & editing: TianZhong Peng, Xingzhen Lin
Footnotes
How to cite this article: Lin X, Li F, Lu H, Zhu M, Peng TZ. Acupuncturing of myofascial pain trigger points for the treatment of knee osteoarthritis: a systematic review and meta-analysis. Medicine. 2022;101:8(e28838).
The study was funded by Training Programme for Young and Middle-aged Talents in Chinese Medicine in Jiangxi Province (2021.2), Science and Technology Plan of Jiangxi Provincial Health and Family Planning Commission (20197057).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Lee MC, Saleh R, Achuthan A, et al. CCL17 blockade as a therapy for osteoarthritis pain and disease. Arthritis Res Ther 2018;20:62–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bastick An, Belo Jn, Runhaar J, et al. What are the prognostic factors for radiographic progression of knee osteo-arthritis a meta -analysis. Clin Orthop Relat Res 2015;473:2969–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Fan H, Zhang L, et al. Research progress of mechanisms of manipulation on knee osteoarthritis. J Trad Chin Orthop Trauma 2018;30:31–3. [Google Scholar]
- [4].Haser C, Stgglst T, Kriner M, et al. Effect of dry needling on thigh muscle strength and hip flexion in elite soccer players. Med Sci Sports Exerc 2017;49:378–83. [DOI] [PubMed] [Google Scholar]
- [5].Nunez-Corts R, Cruz-Montecinos C, Vsquez-Rosel A, et al. Dry needling combined with physical therapy in patients with chronic postsurgical pain following total knee arthroplasty: a case series. J Orthop Sports Phys Ther 2017;47:209–16. [DOI] [PubMed] [Google Scholar]
- [6].Yu Jiani. Effect of acupuncture “tendon adjustment and bone treatment” on the mechanical properties of FAK-PI3K-AKT pathway and quadriceps muscle in knee cartilage of KOA rabbits. Beijing University of Chinese Medicine, 2016. [Google Scholar]
- [7].Huan Yiran. Exploring the mechanism of action of acupuncture in the repair of cartilage and rectus femoris muscle in rabbits with KOA model based on the method of “tendon adjustment and bone treatment”. Beijing University of Chinese Medicine, 2014. [Google Scholar]
- [8].Guo C, Xie W. Study on the effect of electroacupuncture acupoint stimulation on the rectus femoris of rabbits with knee osteoarthritis. World J Integr Tradit West Med 2020;15:1456–60. [Google Scholar]
- [9].Huang QM, Zhuang XQ, Tan SS. The Diagnosis and Treatment of Myofascial Trigger Point. 2010;China: Guangxi Science and Technology Press, pp. 80–105. Chinese. [Google Scholar]
- [10].Mayoral O, Salvat I, Teresa Martn M, et al. Efficacy of myofascial trigger point dry needling in the prevention of pain after total knee arthroplasty: a randomized, double-blinded, placebo-controlled trial. Evid Based Complement Alternat Med 2013;23:694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bricca A, Roos EM, Juhl CB. Infographic. Therapeutic exercise relieves pain and does not harm knee cartilage nor trigger inflammation. Br J Sports Med 2019;54: bjsports-2019-100727. [DOI] [PubMed] [Google Scholar]
- [12].Huang QM, Zhuang XQ, Tan SS. The Diagnosis and Treatment of Myofascial Trigger. 2010;China: Guangxi Science and Technology Press, pp. 80–105. Chinese. [Google Scholar]
- [13].Ma Y, Huang Q, Li L, et al. Efficacy of acupuncture on myofascial trigger points of quadriceps femoris in the treatment of athletes with exercise-induced knee-joint pain. Pain Clin J 2018;14:25–30. [Google Scholar]
- [14].Wu Y-B, Bao W-L, Hu X-H. Therapeutic effect of myofascial trigger point combined with exercise therapy on femoral pain syndrome. J Kunming Med Univ 2020;41:147–50. [Google Scholar]
- [15].Zeng W-B, Luo L, LI W-C, Cai W. Clinical study on the treatment of knee osteoarthritis in early and middle stage with blade needle based on the theory of myofascial trigger point. Guiding J Tradit Chin Med Pharm 2019;25:117–9. [Google Scholar]
- [16].Qin W, Zhang K, et al. Clinical observation of acupuncture at tendon blockage point of quadriceps femoris muscle belly for patella femoral arthritis. Chin Acupunct Moxibustion 2020;40: 0810-0001. [DOI] [PubMed] [Google Scholar]
- [17].Zhou Y, Liao J, Zeng Z, et al. Acupuncture at myofascial trigger points combined with muscle stretching for treatment of early-middle knee osteoarthritis. J Trad Chin Orthop Trauma 2018;30:40–4. [Google Scholar]
- [18].Zhang W-J, Dong B-Q, Zhang H-P, Tan C-D, Song J, Zhang P. Observation of clinical efficacy on knee osteoarthritis treated with acupuncture at trigger points. World J Integr Tradit West Med 2015;10:40–4. [Google Scholar]
- [19].Yin J. Acupuncture myofascial pain trigger points combined with muscle stretching for early to mid-stage knee osteoarthritis. Shuang Zhu Yu Bao Jiang 2019;7:33–4. [Google Scholar]
- [20].Zhao J. Effects of Acupuncturing Quadriceps Trigger Points on Knee Mechanical Function and Pain in Patient with Patellofemoral Pain Syndrome. Shanghai: Shanghai University of Sport; 2018. [Google Scholar]
- [21].Ma Y. Efficacy of Acupuncture Myofascial Trigger Points on Quadriceps for Patellofemoral Pain Syndrome: A Randomized Controlled Trial. Shanghai: Shanghai University of Sport; 2018. [Google Scholar]
- [22].Zhang P. Evaluation Study on the Efficacy of Acupuncture of Knotted Tendon Lesion Points to Stimulate Painful Points and Traditional Meridian Points in the Treatment of KOA. Liaoning: Liaoning University of Traditional Chinese Medicine; 2016. [Google Scholar]