Abstract
Normal embryogenesis requires complex regulation and precision, which depends on multiple mechanistic details. Defective embryogenesis can occur by various mechanisms. Maintaining redox homeostasis is of importance during embryogenesis. NADPH, as produced from the action of glucose-6-phosphate dehydrogenase (G6PD), has an important role in redox homeostasis, serving as a cofactor for glutathione reductase in the recycling of glutathione from oxidized glutathione and for NADPH oxidases and nitric oxide synthases in the generation of reactive oxygen (ROS) and nitrogen species (RNS). Oxidative stress differentially influences cell fate and embryogenesis. While low levels of stress (eustress) by ROS and RNS promote cell growth and differentiation, supra-physiological concentrations of ROS and RNS can lead to cell demise and embryonic lethality. G6PD-deficient cells and organisms have been used as models in embryogenesis for determining the role of redox signaling in regulating cell proliferation, differentiation and migration. Embryogenesis is also modulated by anti-oxidant enzymes, transcription factors, microRNAs, growth factors and signaling pathways, which are dependent on redox regulation. Crosstalk among transcription factors, microRNAs and redox signaling is essential for embryogenesis.
Keywords: G6PD, G6PD deficiency, embryonic lethal, ROS, animal models
1. Introduction
The quality of an embryo and its growth warrant the existence and perpetuation of a species. Signaling events regulating cell proliferation, migration and differentiation with temporal and spatial precision are critical for healthy embryos. Defective embryos are subjected to destruction by various mechanisms [1]. Reduction-oxidation (Redox) status modulated by an imbalance of reactive species and anti-oxidants sensitizes signaling pathways, leading to altered cellular fates and embryonic defects [2]. Classic studies of embryogenesis have focused on the deleterious effects of oxidants on lipids, proteins and nucleic acids. Oxidants can serve as signaling molecules by initiating and promoting cell proliferation during embryonic development [3].
Glucose-6-phosphate dehydrogenase (G6PD) is the rate-limiting enzyme in the pentose phosphate pathway (PPP). G6PD is ubiquitously expressed in living organisms. The biochemical functions of G6PD include the oxidation of glucose-6-phosphate to 6-phosphogluconolactone and the production of the reduced form of nicotinamide adenine dinucleotide phosphate (NADPH). As a powerful biological reducing equivalent, NADPH supports reductive biosynthesis and maintains redox homeostasis. G6PD status is critical for life. Sufficient G6PD is necessary for normal cell growth and organismal survival. G6PD deficiency causes a wide range of pathophysiological effects, including growth arrest, senescence, cell death and embryonic defects [4].
NADPH can serve as a pro-oxidant for generating reactive oxygen species (ROS) via NADPH oxidase (NOX) and reactive nitrogen species (RNS) via nitric oxide synthase (NOS). Both ROS and RNS promote cell growth and differentiation [5]. G6PD is an important source of NADPH for the activity of NOX and NOS. The production of superoxide and nitric oxide is positively associated with G6PD status [6,7,8]. Because embryogenesis is coupled with metabolic alterations and energy consumption, ROS and RNS can be generated at supra-physiological concentrations. Anti-oxidant compounds and enzymatic systems can negate the harmful consequences of ROS and RNS. Among them, NADPH-dependent anti-oxidant enzymes, including thioredoxin reductase, aldo-keto reductase and glutathione reductase, are essential for reproduction and embryonic survival.
Thioredoxin (Trx), a group of small redox proteins, reduces the formation of disulfide bonds in sulfhydryl residues. Oxidized Trx is then reduced by thioredoxin reductase (TrxR) using NADPH as an electron donor [9]. The importance of Trx in reproduction and fetal development is demonstrated by the embryonic lethality in Trx-knockout mice [10,11,12,13]. Carbonyl compounds, derived from oxidative modification of organic compounds, can react with thiols and amino acids leading to carbonyl stress [9]. The aldo-keto reductases catalyze the reduction of carbonyl groups to alcohols in an NADPH-dependent manner. This is associated with the protection of the male reproductive system [14].
NADPH is utilized by glutathione (GSH) reductase to regenerate the reduced form of GSH. Besides its role in anti-oxidative defense, GSH mediates various cellular processes by undergoing reversible oxidation with cysteine in protein targets, including kinases, phosphatases and transcription factors [15]. Glutathione peroxidase (GPx) utilizes GSH to detoxify peroxides. The expression of GPx4 in the testis and embryos suggests that it plays an essential role in male reproduction [16] and early embryonic development [13]. GSH is also linked with oxygen sensing through epigenetic regulation during development [17].
Oxygen has many roles in a biological system, including supporting metabolism and bioenergetics, maintaining redox homeostasis and supplying oxygen-based radicals as signaling molecules [18,19]. The evolution of metazoans is associated with increased levels of oxygen [20]. To adapt to the oxygen-rich environment, living organisms develop regulatory mechanisms to promote growth and survival, such as a cysteine-rich proteome. Approximately 3% of amino acids in proteins found in organisms are cysteines [21]. The complete development of the respiratory system is critical in an embryo and is, in part, redox sensitive [22]. The PPP functions as a key regulator for mediating hyperoxia-induced lung vascular dysgenesis at the late stages of embryogenesis. Hyperoxia-induced enhancement of the PPP causes abnormal proliferation of lung endothelial cells, dysmorphic vascular development and alveolar simplification in neonatal mice [23].
2. The Role of Redox in Humans and Other Species
Different animal models have been used in different redox studies because redox systems in all species are somewhat similar. In mammalian cells, the main source of intracellular ROS production are the NOX family (NOX 1-5, DUOX 1/2) [24] and the mitochondrial electron transport chain (ETC complexes I–IV, electron transporters ubiquinone and cytochrome c) [25,26,27]. Sequence comparisons and phylogenetic analysis indicate that C. elegans possesses twenty proteins closely related in sequence and length to TRX in S. cerevisiae, H. sapiens, and D. melanogaster [28]. Human mitochondrial TRXN2 (an ortholog with C. elegans TRX-2) is oxidized by mitochondrial-dependent superoxide, leading to the activation of the apoptosis signal-regulating kinase 1 (ASK-1) signaling pathway [29]. In humans, there are two thioredoxin genes, TXN and TXN2. In S. cerevisiae, thioredoxins are encoded by TRX1, TRX2 and TRX3 [30]. In addition, a family of anti-oxidant proteins, peroxiredoxins (Prx), are conserved in all types of organisms, including bacteria, plants, nematodes, and mammals. C. elegans peroxiredoxins-2 (CePrx2), a homolog of human PRDX2, is essential for normal growth and egg production [31].
In bacteria, fungi, worms and mammals, the disulfide reducing enzymes, GSH reductase and TrxR, are conserved. However, D. melanogaster does not have GSH reductase. It is replaced by TrxR, which results in the maintenance of a high GSH concentration [32]. Glutaredoxins (GLRX) are redox enzymes that use glutathione as a cofactor for reducing protein disulfides. The mammalian GLRX3/PICOT (ortholog of C. elegans GLRX-3) is involved in immune cell activation, development of cardiac hypertrophy, embryonic development and post-embryonic growth. GLRX3 also functions as an iron-sulfur protein [28]. Another redox compound, protein disulfide isomerase (PDI), which is found in the endoplasmic reticulum (ER), catalyzes the formation (oxidation), breakage (reduction) and rearrangement (isomerization) of disulfide bonds between cysteine residues within proteins. PDI-1, PDI-2 and PDI-3 are important for embryogenesis, viability and formation of the extracellular matrix in C. elegans [33].
3. G6PD Studies in Embryonic Stem Cells and Animal Models
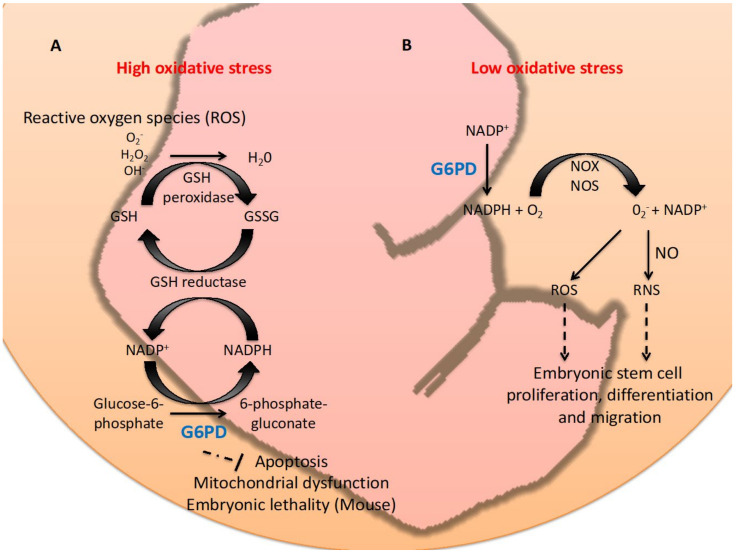
G6PD has a pro-survival role in cells and organisms [5]. How an enzyme involved in carbohydrate metabolism and redox homeostasis regulates cell survival and reproduction is largely unknown due to the biological complexity (Figure 1).
Figure 1.
Graphic summary of the dual role, anti-oxidant or pro-oxidant, of G6PD in embryogenesis. Panel A: Under high oxidative stress conditions (supra-physiological), G6PD acts as a key anti-oxidative enzyme by eliminating ROS (O2-, H2O2 or OH-) via production of NADPH and regeneration of GSH. This mechanism prevents embryonic cells in animal models from undergoing apoptosis, mitochondria dysfunction and embryonic lethality in animal models. Panel B: G6PD can act as a pro-oxidant in low oxidative stress conditions (eustress) by providing NADPH for NOX/NOS in producing ROS or RNS, which are required for ESCs proliferation, differentiation and migration.
3.1. Embryonic Stem Cells
Upon targeted inactivation of G6PD by homologous recombination, male mice embryonic stem (ES) cells are viable; however, they are very sensitive to oxidative stress [34]. Despite normal proliferation in vitro, G6PD-depleted ES cells are prone to apoptosis and mitochondrial dysfunction when challenged with oxidants. This can be ascribed to intracellular GSH levels [35]. G6PD-deficient ES cells can differentiate into many cell types, while G6PD-deficient erythroid cells undergo apoptosis upon hemoglobin switching [36]. This is caused by elevated oxidative stress due to enhanced release of oxygen from hemoglobin. Despite delaying apoptosis by the reducing agent, NAC, or a pan-caspase inhibitor zVAD-fmk, complementation of the G6PD gene into G6PD-deficient ES cells prevents cellular demise [36].
Cre-lox recombination-derived G6PD-deficient mouse ES cells are sensitive to oxidative stress [37]. Diamide, a potent thiol scavenger, depletes NADPH and GSH by oxidation and decreases survival in G6PD-deficient ES cells. While wild type ES cells rapidly restore the NADPH/NADP+ ratio and PPP activity upon diamide challenge, G6PD-deficient ES cells fail to do so. This indicates that the activation of G6PD is the major NADPH source in response to oxidative stress.
3.2. Mouse
The importance of G6PD in embryogenesis has been shown in mouse studies [38]. G6PD(-) ES cells are used to inject into mouse blastocysts to produce chimeric mice. The first generation (F1) G6PD(+/-) heterozygotes obtained from the cross between normal females and chimeric males are healthy and fertile. Only normal G6PD males can survive when F1 G6PD(+/-) females are bred with normal males. Hemizygous G6PD(-) male embryos fail to grow at E.7.5, a critical stage for the development of the blood circulation. These embryos eventually die at E10.5. Likewise, heterozygous G6PD(+/-) females display tissue abnormalities and increased apoptotic cells. At later stages, necrotic cells appear and the embryos die between E11.5 and E12.5. Both G6PD(-) and F2 G6PD(+/-) embryos show apoptotic cells in the allantois, indicating a disturbance of placenta differentiation. The lethality of G6PD-deficient mouse embryos is ascribed to oxidative damage after the establishment of the blood circulation, thereby affecting placental function. Hence, G6PD plays a protective role against oxidative stress in the placenta to support the growth of trophoblast during embryogenesis. A comparative study shows that female mouse embryos contain less H2O2 and survive better than male embryos under heat stress [39]. The slow-growing female embryos display a higher level of G6PD transcripts. Upon G6PD inhibition, the differences caused by ROS between male and female embryos are absent, suggesting a protective role of G6PD in differential sensitivity of heat-induced oxidative stress during embryogenesis.
3.3. Zebrafish
A transparent embryo and ex utero development make zebrafish an ideal model organism for studying embryogenesis. A G6PD morpholino knockdown zebrafish has been established due to the lack of significant hemolysis in G6PD-deficient mice upon oxidant challenge [40]. G6PD morpholino reduces G6PD activity in zebrafish leading to rapid hemolysis and pericardial edema. Titration of G6PD morpholino in zebrafish embryos does not cause edema and hemolysis until challenged with pro-oxidant compounds, including menthol, 1-naphthol and primaquine [40]. In addition to the edema and reduced hemoglobin in G6PD morphants, 1-naphthol increases ROS generation and erythrocyte apoptosis. Zebrafish embryonic defects caused by G6PD deficiency, including the decreased epiboly rate and elevated cell shedding at the embryo surface, are mediated by the epithelial-mesenchymal transition (EMT) pathway [41]. E-cadherin, encoded by CDH-1, regulates cell movement and tissue formation during early embryogenesis in zebrafish [42]. Reduction of E-cadherin decreases cell adhesion and the epiboly rate. Complementation of human G6PD or CDH-1 cRNA reduces embryonic defects and the expression of epithelial surface markers, E-cadherin and β-catenin, in G6PD-deficient zebrafish embryos [41]. G6PD deficiency in zebrafish impairs redox signaling mediated by NADPH oxidase-4 (NOX4) and down-regulates Smad3 and miR-200b, which are involved in embryonic stem cell differentiation and stability [43,44]. These findings indicate that G6PD plays a cytoregulatory role in appropriating redox homeostasis for modulating embryogenesis.
3.4. Nematode
In order to decipher the common mechanism underlying early embryogenesis, a simple invertebrate animal model may be suitable for large-scale analyses using cell biology, molecular biology and genetic approaches. A pilot research program led by Sydney Brenner sought an organism with the potential to identify each gene involved in development and to trace the lineage of every cell. Caenorhabditis elegans, a free-living soil nematode, has been chosen because of several advantages [45]. C. elegans has become a favorite model of embryologists because its embryo and cuticle are transparent, thereby benefiting microscopic examination. C. elegans, approximately 1 mm in size, has a short duration of embryogenesis (16 h) and lifecycle (3 days) as well as a life span (3–4 weeks), which is ideal for investigation of the gene regulatory network in embryogenesis, development and aging.
The high degree of conservation of G6PD between the nematode and vertebrate counterparts indicates that G6PD in C. elegans is a functional homologue of vertebrate G6PD. A G6PD-deficient C. elegans established by RNA interference knockdown displays enhanced apoptotic germ cells and less embryo production, indicating impairment of oogenesis [46]. Similar to mouse and zebrafish models, G6PD-deficient C. elegans shows a dramatic reduction of hatched embryos. Such embryonic defects are possibly due to increased ROS and DNA oxidative damage, leading to altered MAPK signaling [46].
Further characterization of G6PD-deficient C. elegans embryos reveals that their membrane function is impaired. These membrane abnormalities in C. elegans embryos, including enhanced permeability to fluorescent dyes and loss of barrier structural integrity, as well as abnormal polarity and cytokinesis, are associated with altered lipid metabolism [47]. A significant increase of lysoglycerophospholipids is associated with the activation of calcium-independent phospholipase A2 (iPLA), possibly mediated by the imbalanced redox status, including decreased NADP levels and increased lipid peroxidation. Suppression of multiple iPLA alleviates defective permeability and polarity.
Transient treatment of tert-butyl hydroperoxide (tBHP), an inducer of lipid peroxidation decreases brood size and increases germ cell apoptosis [48]. tBHP stimulates malondialdehyde (MDA) generation and up-regulates iPLA activity, thereby interfering with oogenesis and embryogenesis. These findings indicate that G6PD deficiency-derived lipid peroxidation enhances germ cell demise, leading to embryonic lethality, and demonstrates that G6PD is required for maintaining membrane stability and lipid homeostasis through redox balance during early embryonic stages.
4. The Redox Role of G6PD in Cellular Migration and Differentiation during Embryogenesis
Oxidative stress differentially influences cell fate and embryogenesis. Physiological levels (eustress) of ROS generated during embryogenesis promote proliferation and differentiation of cells and are required for normal development in the blastocyst stage and neuronal differentiation of embryogenesis [49]. ROS is involved in crucial processes, such as embryonic blood stem cell development [50,51] and differentiation of embryonic cardiomyocytes [52,53,54]. ROS can affect stem cell fate and generate stem cells, as seen with the differentiation of mesenchymal stem cells (MSC) to adipocytes caused by the enhancement of intracellular ROS through NOX4-mediated H2O2 signaling [55]. Increased ROS beyond physiological levels (oxidative stress) causes apoptosis, whereas even higher ROS levels lead to necrosis [56]. This suggests that redox-dependent signaling plays a critical role in cell migration and cell differentiation during embryogenesis (Figure 1).
4.1. Involvement of G6PD in Cell Migration
Cell migration occurs during embryogenesis. In gastrulation, groups of cells inside blastocysts migrate collectively to form the three layers of the embryo (ectoderm, mesoderm and endoderm) that eventually migrate to target locations, where they differentiate and form various tissues and organs [57]. The collective cell migration requires coordination and teamwork between migrating cells, which interact with the extracellular matrix of other tissues and respond to chemotactic signals generated in the surrounding environment [58].
One of the signals that influence cell migration during embryogenesis is redox signaling, which can alter cell fate, leading to structural and functional changes in the developmental processes. Disruption of redox signaling during organogenesis induces adverse outcomes, such as defective cell migration, premature cell differentiation, apoptosis, alterations in cell proliferation and cellular polarity [2].
Redox signaling influences cell migration during embryogenesis through different mechanisms in different animals. Up-regulation of ROS induced by ethanol decreases hemangioblast migration from the posterior primitive streak to the area of opaca in the early chick embryo via the FGF/VEGF/PDGF signaling pathway [59]. In zebrafish, glutaredoxin 2, the vertebrate oxidoreductase protein modulating the intracellular thiol pool, is required for heart development. Knockdown of glutaredoxin 2 disturbs migration of the cardiac neural crest cells, leading to apoptosis [60]. Upon knockdown of superoxide dismutase 1, elevated ROS impairs embryonic primordial germ cell migration and adhesion in cellular blastoderm embryos of Drosophila melanogaster [61].
4.2. Contribution of G6PD to Cell Differentiation
Cell differentiation is closely associated with cell proliferation in a developing embryo. Embryonic differentiation occurs after zygote cleavage. The pluripotent ES cells differentiate into many cell types followed by organizing into tissues and organs [62,63]. Cell differentiation in the developmental process is influenced by redox signaling. ROS generated by osteoclasts is important for differentiation and the resorption of bone tissue [64]. Undifferentiated pre-adipocytes have a high level of GSH, whereas the GSH level drops and GSSG increases upon differentiation [65].
NOX4-dependent ROS production regulates cardiac differentiation through the p38 MAPK signaling pathway [66]. Increased ROS by NOX4 is involved in adipocyte differentiation via CREB (cAMP response element-binding protein) in mesenchymal stem cells [55]. Enhanced ROS production occurs during carbon monoxide-induced neuronal differentiation in SH-SY5Y cells. This event stimulates the PPP to increase NADPH production and affect cell differentiation [49].
5. Embryogenesis Regulated by Other Redox-Related Genes, Transcription Factors, MicroRNAs, Growth Factors and Signaling Pathways
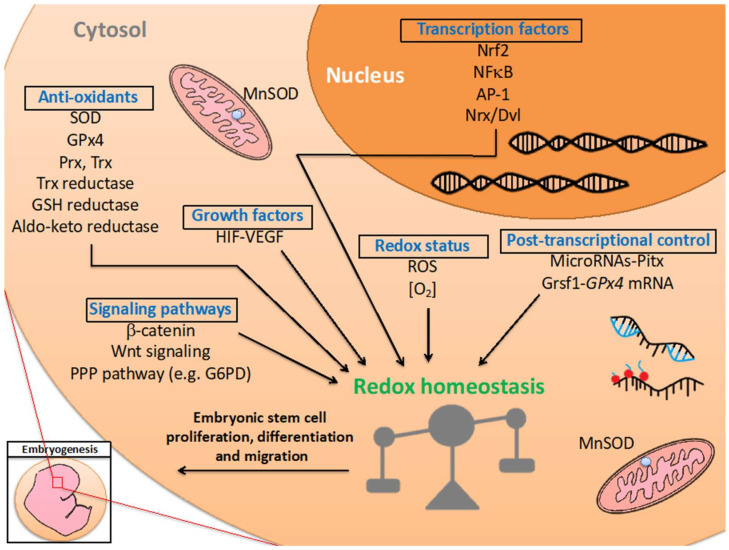
Embryogenesis is a precisely controlled biological process for reprogramming the metabolic state of the cell and driving a single cell to a mature organism [67,68]. Embryogenesis is closely associated with activation and/or repression of genes within a developmental timeline [69,70]. This process is tightly and precisely regulated by various factors, such as transcription factors, microRNAs, growth factors and signaling pathways [71,72,73,74,75] (Table 1) (Figure 2). Redox reactions are essential for providing energy production and for regulating oxidative stress. Sufficient energy production and an appropriate redox environment are required for establishing a proper milieu for the embryo. Metabolically generated oxidants and associated anti-oxidant defenses participate in the initiation of certain outcomes during embryogenesis [76].
Table 1.
Summary of redox-related factors and pathways in embryonic development.
| Type | Name | Model | Functions | Experimental Protocols | References |
|---|---|---|---|---|---|
| Enzymatic/anti-oxidant enzyme | SODs | Human | The SOD activity in placenta protects embryos from lipid peroxidation. | Biochemical analysis | [77,78] |
| Enzymatic/anti-oxidant enzyme | MnSOD | Mouse Drosophila |
Maintains cardiac function and neonatal survival. Prevents abnormal brain morphology and axonal aberrations during neurodevelopment. |
Mouse: biochemical analysis. Drosophila: lifespan analysis, brain/neuron morphology | [73,79] |
| Enzymatic/anti-oxidant enzyme | GPx4 | Mouse | Male reproduction and early embryonic development. Initiates gastrulation and develops embryonic cavities |
siRNA knockdown. Molecular biology/morphology analysis. |
[13,16,80] |
| Enzymatic/anti-oxidant enzyme | Prx | Human Cow Drosophila C. elegans |
Stimulates blastocyst development and increases embryonic mitochondrial activity. Support embryogenesis. |
Molecular biology/biochemical/life span analysis. | [31,81,82,83,84] |
| Enzymatic/anti-oxidant enzyme | Trx/TrxR | Mouse | Support embryonic viability and embryogenesis. | Knockout mice. Molecular biology/morphology analysis. |
[10,11,12,13] |
| Enzymatic/pro-oxidant enzyme | NOX | Mouse | Promotes cardiac differentiation, cardiomyogenesis, and neonatal cardiac cell growth. | shRNA/siRNA knockdown. Biochemical/molecular biology/morphology analysis. |
[66,85] |
| Non-enzymatic/transcription factor | Nrf2 | Human Mouse |
Enhances oxidative stress resistance. Controls self-renewal and pluripotency of ES cells. Supports embryo cleavage and blastocyst formation. Maintains stemness and survival under oxidative stress. | siRNA knockdown and CRISPR-mediated ectopic gene expression | [86,87,88,89] |
| Non-enzymatic/transcription factor | NF-κB | Mouse | Embryonic and liver parenchymal cell survival | Knockout mice coupled with histological/molecular biology analysis. | [90] |
| Non-enzymatic/transcription factor | AP-1 | Mouse | Embryonic survival, liver erythropoiesis, hepatogenesis, development of the placenta and yolk sac, chondrocytes and extraembryonic tissues | Knockout mice coupled with biochemical/molecular biology/morphology analyses. | [91,92,93,94,95] |
| Non-enzymatic/transcription factor | HIF-1 | Human mouse |
Modulates vascular development (VEGF) in hypoxia. Trophoblast proliferation and differentiation, morphogenesis of the developing heart, chondrogenesis and myocardial development. | Knockout mice. Molecular biology/morphology analysis. |
[96,97,98,99] |
| Non-enzymatic/transcription factor | Pitx2, Pitx3 | Mouse | Anti-oxidant defense in fetal myogenesis | Knockout/knockdown and ectopic gene expression. Metabolomics/molecular biology analysis. |
[100] |
| Non-enzymatic/post-transcriptional control | Pitx-miRNA (mir-15b, mir -23b, mir-106b and mir-503) pathway | Mouse | Modulates cell proliferation and cell fate of skeletal-muscle stem cells (satellite cells) | Knockout/knockdown and ectopic gene expression. Bioinformatics/molecular biology analysis. | [101] |
| Non-enzymatic/post-transcriptional control | Grsf-1 | Mouse | Modulates brain development by recruiting GPx4 mRNA to translationally active polysome fractions by targeting 5′ untranslated region (UTR) of GPx4 mRNAs. | Bioinformatics/biochemical analysis | [102] |
| Signaling pathway | Wnt signaling (Nrx and Dvl) | Human C. aethiops Mouse Xenopus |
Senses ROS levels to activate or inactivate Wnt signaling for directing embryo gastrulation. | siRNA knockdown and microinjection-mediated ectopic gene expression research. Biochemical/molecular biology/morphology analysis. | [103,104,105] |
| Signaling pathway | PPP pathway (including G6PD) | Mouse Zebrafish C. elegans |
Maintains redox homeostasis during embryogenesis. Mediates abnormal lung development in hyperoxia in the neonatal mice. |
Knockout/siRNA or morpholino knockdown. Metabolomics/biochemical/molecular biology/morphology analysis. |
[23,34,35,36,37,38,39,40,41,42,43,44,46,47,48] |
Figure 2.
Regulation of redox homeostasis in embryogenesis. Redox-related factors, including anti-oxidant enzymes, transcription factors, post-transcriptional control, growth factors, signaling pathways and redox status, support embryogenesis and the developmental timeline through maintaining redox homeostasis. The biological function of these factors are discussed in the main text and summarized in Table 1.
5.1. Anti-Oxidant Enzymes
Several anti-oxidant enzymes are involved in embryogenesis, such as superoxide dismutase (SOD), GPx, Prx and catalase (CAT). These anti-oxidant enzymes catalyze the decomposition of hydrogen peroxide into water and oxygen [28].
SOD controls ROS levels by converting superoxide to hydrogen peroxide, which can be detoxified to water by catalase and glutathione peroxidase [106]. Protein and mRNA of SOD are expressed during bovine embryogenesis [107]. The good quality of oocytes and embryos exhibits high SOD activity [108]. SOD also prevents the motility loss in mouse sperm and protects embryos from oxidative stress [109]. Newborn mice with sod-2-/- deficiency show neonatal lethality after 4–5 days. Lacking SOD activity can be fatal in newborns [73]. These findings reveal the importance of ROS levels being regulated by an antioxidative enzyme in embryogenesis.
GPx reduces H2O2 to H2O using GSH as the electron donor. One of the GPx isozymes, GPx4/PHGPx (phospholipid hydroperoxide glutathione peroxidase), reduces lipid hydroperoxide in cell membranes and is involved in gastrulation. GPx4 expression is up-regulated by G-rich RNA Sequence Binding Factor 1 (Grsf1) through a post-transcription mechanism. Grsf1 recruits GPX4 mRNA to translationally activate polysome fractions by targeting the 5′ untranslated region (UTR) of GPx4 mRNAs. Overexpression of GPX4 mRNA rescues Grsf1 deficiency-induced developmental retardation of embryos. This post-transcriptional regulation links the anti-oxidant enzyme, GPx4, to embryogenesis [102]. Homozygous GPx4-deficient mice die in utero at midgestation between 7.5 and 8.5 days post coitum because of retardation in brain development and abnormal heart formation [13,80]. However, the heterozygotes GPx4-deficient mice are viable, fertile and appear normal, in spite of having decreased levels of cytosolic, mitochondrial and nuclear GPx4 mRNA and proteins. These heterozygote GPx4-deficient mice are more susceptible to various oxidative stressors [13]. Another GPX isozyme, GPx3, is required for posterior embryogenesis in Xenopus laevis. GPx3 knockdown enhances cell death and decreased cell proliferation in the tail region through the Wnt/Notch/FGF signaling pathway [110].
Within the embryo, the nervous system is not completely developed [111]. Redox signaling contributes to the development of the nervous system, such as axonal growth and neuronal differentiation [112]. Redox imbalance can negatively affect embryonic neural development. Silencing GPx4 expression by RNA interference leads to a hindbrain developmental defect in mice (rhombomeres 5 and 6 impairment) [80]. SOD2 deficiency results in increased ROS levels, abnormal brain morphology and axonal aberration in Drosophila [79]. This suggests that embryonic development of the nervous system is redox sensitive.
Prx removes ROS through conserved reactive cysteines residues by which H2O2 is reduced. The mammalian Prxs affect gamete maturation, fertilization and embryogenesis. The deficiency of Prx does not have lethal consequences for embryogenesis. Among the six members of Prxs, Prx2, Prx3 and Prx5 influence embryogenesis [81]. Prx2 stimulates the development of the blastocyst by reducing intracellular ROS and increasing embryonic mitochondrial activity [82]. Prx3 is one of the candidate genes that predict embryo quality. Lower expression of Prx3 is associated with high-quality embryos [83]. Drosophila peroxiredoxin 5 (dPrx5) is essential in the early stages of embryogenesis [84]. C. elegans with Prx-2 deficiency have a reduced brood size and retarded development. The CePrx2 only affects two types of pharyngeal neurons, which are single pharyngeal interneuron 14 and the sensory interneuron 12 [31].
Catalase is found in all living organisms. One catalase molecule can reduce millions of H2O2 molecules to yield H2O and O2. The peroxisomal CTL-2-deficient C. elegans has a lower egg-laying capacity and shorter life span [113]. Embryonic catalase protects the embryo from excessive ROS production. The lack of catalase promotes structural embryopathies in C57BL/6 mice [114,115,116,117].
5.2. Transcription Factors
As key regulators of various cellular processes, transcription factors activate downstream target genes by enhancing transcription activity [118]. Transcription factors can sense cellular redox status, including NF-E2-related factor 2 (Nrf2), Nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), Activator Protein-1 (AP-1) and hypoxia-inducible factor (HIF), thereby contributing to the regulation of cell proliferation, differentiation and apoptosis in embryos [76].
Nrf2 regulates the adaptive response to oxidative stress [119]. The evolution of Nrf2 is correlated with increasing atmospheric oxygen [120]. Nrf2 binds with genes containing the anti-oxidant response element (ARE) [121]. Nrf2 also serves as a master regulator for self-renewal, pluripotency and differentiation in ES cells [122]. In mesodermal development, multipotent stromal cells (MSCs) differentiate to osteoblasts, chondrocytes, myocytes and adipocytes [123]. Overexpression of Nrf2 in MSCs enhances oxidative stress resistance, cell survival and osteoblastic differentiation [87,88]. In early embryogenesis in mice, the Nrf2-associated cell cycle transition from the G2 to the M phase is inhibited by brusatol (a quassinoid isolated from Bruceajavanica), and this inhibition is dependent on the cyclin B-CDK1 (cyclin-dependent kinase I) complex [89]. This indicates that a dual role exists for Nrf2 in maintaining redox homeostasis and modulating embryogenesis.
NF-κB regulates gene expressions, including that related to pro-inflammatory cytokines (IL1, IL2, IL6, IL8 and TNFα), adhesion molecules (VCAM-1, ICAM and E- and P-selectin), apoptotic regulators (Bcl-XL and c-IAPs), growth factors (G-CSF) and redox-related enzymes (COX2, iNOS, SOD, 12-LOX and GSH-synthase) [76]. Activation of NF-κB in response to stress, such as hypoxia or oxidative and nitrosative stress, results in the modulation of downstream gene expression [124]. During embryogenesis, loss-of-function of NF-κB leads to embryonic lethality at E15 and apoptosis of liver parenchymal cells in mice [90].
AP-1 regulates various gene expressions and controls proliferation, differentiation and apoptosis in response to cellular stress [125]. AP-1 is activated by the upstream MAP-kinase (p38, ERK and JNK) signaling pathways [126]. While NF-κB modulates the postnatal stage, AP-1 regulates embryogenesis in the prenatal stage. Knockout of AP-1 results in embryogenic defects in mice, including embryonic lethality, abnormal liver erythropoiesis, hepatogenesis and the development of the placenta and yolk sac, chondrocytes and extra-embryonic tissues [91,92,93,94,95].
5.3. Redox-Related Post-Transcriptional Controls
Post-transcriptional regulation plays a crucial role in redox-dependent developmental processes. Myogenesis is an important biological process for forming skeletal muscular tissue during embryogenesis [127]. Loss of function of two transcription factors, Paired-like homeodomain transcription factor 2 gene (Pitx2) and Pitx3, leads to abnormal accumulation of ROS in mouse myogenesis [100]. The Pitx-MicroRNA (mir-15b, mir-23b, mir-106b and mir-503) pathway regulates myoblast proliferation, demonstrating that the crosstalk of transcription factors, microRNAs and redox signaling is essential for embryogenesis [101].
The basic helix loop helix (bHLH) and Per-ARNT-SIM (PAS) transcription factor superfamily proteins of HIF are essential in developmental programs, such as trophoblast proliferation and differentiation, morphogenesis of the developing heart, chondrogenesis and myocardium development [96,97,98,99]. They activate various downstream target genes via the hypoxia response element in the enhancer region. Among three HIF-α subunits, HIF-1α is ubiquitously localized in developing tissues and is regulated by the oxygen gradient [128]. HIF-1α is regulated by post-transcriptional control. The 3′ or 5′ UTR of HIF-1α mRNA contains AU-rich elements attracting the RNA binding protein, such as Human antigen R (HuR) or polypyrimidine tract-binding protein (PBP), for stabilizing HIF-1α mRNA and stimulating HIF-1α protein synthesis [129,130]. Similarly, the 3′ UTR of Trx mRNA is protected from degradation by the cold-inducible RNA-binding protein (CIRP) hnRNPA18, which enhances Trx expression [131]. Such post-transcriptional regulation is found in the mRNA of redox-embryogenesis related enzymes, including Cox-2, GPx1 and MnSOD (manganese-dependent superoxide dismutase or mitochondrial SOD2) [76].
5.4. Growth Factors and Redox Modulation
Growth factors contribute to cell proliferation and differentiation in embryogenesis [132]. The signaling of the epidermal growth factor receptor (EGFR) shows a redox-regulated linkage to tyrosine kinase signaling, which is redox-sensitive [133]. Fibroblast growth factor (FGF) and vascular endothelial growth factor (VEGF) are inhibited in hyperoxia, leading to bronchopulmonary dysplasia in humans, demonstrating a linkage between ROS, growth factors and lung development [75]. H2O2-induced pulmonary hypertension in rats, which is modulated by EGFR signaling through redox regulation [134].
Vasculogenesis is an important event during early mammalian embryogenesis. In order to supply nutrients for embryos, blood vessels are stimulated for growing, branching and invading developing tissues and organs [135]. Crosstalk between growth factors and redox-related transcription factors promotes vascular development. HIF-1 responds to systemic oxygen changes, activates vascular endothelial growth factor (VEGF) transcription and modulates vascular development for adaption to hypoxia. HIF-1 is protective during embryogenesis, as demonstrated by preventing the lethality of mice at the embryonic 10.5 stage (E10.5) [56,136].
5.5. Redox Status and Signaling Pathways
The redox status plays a critical role in regulating differentiation, proliferation, apoptosis and cell division asymmetry during embryogenesis [2]. Therefore, redox signaling is required for building a healthy embryo at the correct time point and place. The evolutionally conserved regulation of the O2 concentration controls cell metabolic processes by producing, sensing and responding to its metabolites (ROS). This regulation contributes to redox cellular signaling. This network of redox cellular signaling not only involves cell metabolism but also embryogenesis [137]. ES cells undergo cell cycle arrest of the G2/M cell cycle phase transiently by increasing ROS levels, which indicates the oxidative stress resistance of the ESCs [138]. ES cells at an O2 concentration of 2–5% maintain their clonal regression and genetic integrity [139,140]. Lower O2 concentrations or oxidative stress induced by H2O2 leads to ES cell death by activating apoptotic signal transduction [138,140], indicating the importance of maintaining a physiological O2 concentration for regulating redox signaling for directing ES cells into the correct timeline of the cell cycle.
The Wingless and int-1 (Wnt) signaling pathway regulates embryonic cell differentiation, proliferation, cell fate determination and apoptosis, especially at the gastrulation stage [141,142]. Wnt signaling is activated by sensing the ROS level. Nucleoredoxin (Nrx) acts as a key regulator for Wnt signaling regulation by targeting dishevelled (Dvl) activity directly [105]. Hydrogen peroxide oxidizes Nrx, leading to Dvl release from the Nrx/Dvl complex, and promotes β-catenin accumulation to activate Wnt signaling [104]. Differential levels of Nrx regulate Wnt signaling during Xenopus gastrulation [103].
6. Conclusions
Maintaining redox homeostasis is critical for the normal development of an embryo. NADPH produced from the action of G6PD is important in maintaining redox homeostasis by serving as a cofactor for NADPH-dependent redox enzymes, including GSH reductase, TrxR, aldo-keto reductase, as well as NOX and NOS. GSH and TRX function as anti-oxidants that contribute to the maintenance of redox homeostasis, while ROS and RNS at physiologic concentrations (eustress) contribute to cellular growth and differentiation. G6PD is involved in oogenesis, embryogenesis and post-embryonic development. This is substantiated from studies in which G6PD is inactive or knocked-down. G6PD-deficient cells and organisms have been used as models for determining the role of redox signaling in regulating cell proliferation, differentiation and migration during embryogenesis. Embryogenesis is also modulated by anti-oxidant enzymes, transcription factors, microRNAs, growth factors and signaling pathways, which are dependent on redox regulation. Novel technologies, including multi-omics sequencing [143] and single-cell sequencing [144], are promising for comprehensively uncovering the molecular actions of how redox homeostasis regulates embryogenesis. Recent development of genetic engineering tools, such as CRISPR knock-in, can further establish new G6PD models in stem cells and model organisms [145,146,147]. It is anticipated that other redox-sensitive pathways governing embryogenesis will be reported following the development of novel and advanced technologies.
Author Contributions
Conceptualization, H.-C.Y., P.-H.C., W.-Y.T., A.S. and D.T.-Y.C.; Resources, H.-C.Y. and D.T.-Y.C.; Writing—Original Draft Preparation, H.-C.Y., P.-H.C., and W.-Y.T.; Writing—Review and Editing, P.-H.C., W.-Y.T. and, A.S.; Supervision, A.S. and D.T.-Y.C.; Project Administration, H.-Y.L.; Funding Acquisition, H.-C.Y. and D.T.-Y.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by grants from the Ministry of Science and Technology of Taiwan (MOST-109-2320-B-264-001-MY2 to HCY, MOST-109-2320-B-255-009, MOST-110-2320-B-255-007, MOST-110-2811-B-255-002 to DTYC), Chang Gung Memorial Hospital (BMRP098 to DTYC) and Chang Gung University of Science and Technology (NMRPF3K0211, ZURPF3L0021 to DTYC).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Menezo Y., Dale B., Cohen M. DNA damage and repair in human oocytes and embryos: A review. Zygote. 2010;18:357–365. doi: 10.1017/S0967199410000286. [DOI] [PubMed] [Google Scholar]
- 2.Timme-Laragy A.R., Hahn M.E., Hansen J.M., Rastogi A., Roy M.A. Redox stress and signaling during vertebrate embryonic development: Regulation and responses. Semin. Cell Dev. Biol. 2018;80:17–28. doi: 10.1016/j.semcdb.2017.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hansen J.M., Jones D.P., Harris C. The Redox Theory of Development. Antioxid. Redox Signal. 2020;32:715–740. doi: 10.1089/ars.2019.7976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang H.C., Wu Y.H., Liu H.Y., Stern A., Chiu D.T. What has passed is prolog: New cellular and physiological roles of G6PD. Free Radic. Res. 2016;50:1047–1064. doi: 10.1080/10715762.2016.1223296. [DOI] [PubMed] [Google Scholar]
- 5.Yang H.C., Wu Y.H., Yen W.C., Liu H.Y., Hwang T.L., Stern A., Chiu D.T. The Redox Role of G6PD in Cell Growth, Cell Death, and Cancer. Cells. 2019;8:1055. doi: 10.3390/cells8091055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serpillon S., Floyd B.C., Gupte R.S., George S., Kozicky M., Neito V., Recchia F., Stanley W., Wolin M.S., Gupte S.A. Superoxide production by NAD(P)H oxidase and mitochondria is increased in genetically obese and hyperglycemic rat heart and aorta before the development of cardiac dysfunction. The role of glucose-6-phosphate dehydrogenase-derived NADPH. Am. J. Physiol. Heart Circ. Physiol. 2009;297:H153–H162. doi: 10.1152/ajpheart.01142.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leopold J.A., Cap A., Scribner A.W., Stanton R.C., Loscalzo J. Glucose-6-phosphate dehydrogenase deficiency promotes endothelial oxidant stress and decreases endothelial nitric oxide bioavailability. FASEB J. 2001;15:1771–1773. doi: 10.1096/fj.00-0893fje. [DOI] [PubMed] [Google Scholar]
- 8.Tsai K.J., Hung I.J., Chow C.K., Stern A., Chao S.S., Chiu D.T. Impaired production of nitric oxide, superoxide, and hydrogen peroxide in glucose 6-phosphate-dehydrogenase-deficient granulocytes. FEBS Lett. 1998;436:411–414. doi: 10.1016/S0014-5793(98)01174-0. [DOI] [PubMed] [Google Scholar]
- 9.Fujii J., Iuchi Y., Okada F. Fundamental roles of reactive oxygen species and protective mechanisms in the female reproductive system. Reprod. Biol. Endocrinol. 2005;3:43. doi: 10.1186/1477-7827-3-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsui M., Oshima M., Oshima H., Takaku K., Maruyama T., Yodoi J., Taketo M.M. Early embryonic lethality caused by targeted disruption of the mouse thioredoxin gene. Dev. Biol. 1996;178:179–185. doi: 10.1006/dbio.1996.0208. [DOI] [PubMed] [Google Scholar]
- 11.Nonn L., Williams R.R., Erickson R.P., Powis G. The absence of mitochondrial thioredoxin 2 causes massive apoptosis, exencephaly, and early embryonic lethality in homozygous mice. Mol. Cell. Biol. 2003;23:916–922. doi: 10.1128/MCB.23.3.916-922.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jakupoglu C., Przemeck G.K., Schneider M., Moreno S.G., Mayr N., Hatzopoulos A.K., de Angelis M.H., Wurst W., Bornkamm G.W., Brielmeier M., et al. Cytoplasmic thioredoxin reductase is essential for embryogenesis but dispensable for cardiac development. Mol. Cell. Biol. 2005;25:1980–1988. doi: 10.1128/MCB.25.5.1980-1988.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Imai H., Hirao F., Sakamoto T., Sekine K., Mizukura Y., Saito M., Kitamoto T., Hayasaka M., Hanaoka K., Nakagawa Y. Early embryonic lethality caused by targeted disruption of the mouse PHGPx gene. Biochem. Biophys. Res. Commun. 2003;305:278–286. doi: 10.1016/S0006-291X(03)00734-4. [DOI] [PubMed] [Google Scholar]
- 14.Iuchi Y., Kaneko T., Matsuki S., Ishii T., Ikeda Y., Uchida K., Fujii J. Carbonyl stress and detoxification ability in the male genital tract and testis of rats. Histochem. Cell Biol. 2004;121:123–130. doi: 10.1007/s00418-003-0607-3. [DOI] [PubMed] [Google Scholar]
- 15.Hansen J.M., Harris C. Glutathione during emb.bryonic development. Biochim. Biophys. Acta. 2015;1850:1527–1542. doi: 10.1016/j.bbagen.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Imai H., Matsuoka M., Kumagai T., Sakamoto T., Koumura T. Lipid Peroxidation-Dependent Cell Death Regulated by GPx4 and Ferroptosis. Curr. Top. Microbiol. Immunol. 2017;403:143–170. doi: 10.1007/82_2016_508. [DOI] [PubMed] [Google Scholar]
- 17.Hitchler M.J., Domann F.E. An epigenetic perspective on the free radical theory of development. Free Radic. Biol. Med. 2007;43:1023–1036. doi: 10.1016/j.freeradbiomed.2007.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radi R. Oxygen radicals, nitric oxide, and peroxynitrite: Redox pathways in molecular medicine. Proc. Natl. Acad. Sci. USA. 2018;115:5839–5848. doi: 10.1073/pnas.1804932115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coffman J.A., Su Y.H. Redox regulation of development and regeneration. Curr. Opin. Genet. Dev. 2019;57:9–15. doi: 10.1016/j.gde.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Knoll A.H., Sperling E.A. Oxygen and animals in Earth history. Proc. Natl. Acad. Sci. USA. 2014;111:3907–3908. doi: 10.1073/pnas.1401745111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miseta A., Csutora P. Relationship between the occurrence of cysteine in proteins and the complexity of organisms. Mol. Biol. Evol. 2000;17:1232–1239. doi: 10.1093/oxfordjournals.molbev.a026406. [DOI] [PubMed] [Google Scholar]
- 22.Ofman G., Tipple T.E. Thiol-Redox Regulation in Lung Development and Vascular Remodeling. Antioxid Redox Signal. 2019;31:858–873. doi: 10.1089/ars.2018.7712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gong J., Feng Z., Peterson A.L., Carr J.F., Lu X., Zhao H., Ji X., Zhao Y.Y., De Paepe M.E., Dennery P.A., et al. The pentose phosphate pathway mediates hyperoxia-induced lung vascular dysgenesis and alveolar simplification in neonates. JCI Insight. 2021;6:e137594. doi: 10.1172/jci.insight.137594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang H.C., Cheng M.L., Ho H.Y., Chiu D.T. The microbicidal and cytoregulatory roles of NADPH oxidases. Microbes Infect. 2011;13:109–120. doi: 10.1016/j.micinf.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 25.Lambeth J.D. NOX enzymes and the biology of reactive oxygen. Nat. Rev. Immunol. 2004;4:181–189. doi: 10.1038/nri1312. [DOI] [PubMed] [Google Scholar]
- 26.Pervaiz S., Bellot G.L., Lemoine A., Brenner C. Redox signaling in the pathogenesis of human disease and the regulatory role of autophagy. Int. Rev. Cell. Mol. Biol. 2020;352:189–214. doi: 10.1016/bs.ircmb.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Zhao R.Z., Jiang S., Zhang L., Yu Z.B. Mitochondrial electron transport chain, ROS generation and uncoupling (Review) Int. J. Mol. Med. 2019;44:3–15. doi: 10.3892/ijmm.2019.4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnston A.D., Ebert P.R. The Redox System in C. elegans, a Phylogenetic Approach. J. Toxicol. 2012;2012:546915. doi: 10.1155/2012/546915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim P.L., Liu J., Go M.L., Boelsterli U.A. The mitochondrial superoxide/thioredoxin-2/Ask1 signaling pathway is critically involved in troglitazone-induced cell injury to human hepatocytes. Toxicol. Sci. 2008;101:341–349. doi: 10.1093/toxsci/kfm273. [DOI] [PubMed] [Google Scholar]
- 30.Pedrajas J.R., Kosmidou E., Miranda-Vizuete A., Gustafsson J.A., Wright A.P., Spyrou G. Identification and functional characterization of a novel mitochondrial thioredoxin system in Saccharomyces cerevisiae. J. Biol. Chem. 1999;274:6366–6373. doi: 10.1074/jbc.274.10.6366. [DOI] [PubMed] [Google Scholar]
- 31.Isermann K., Liebau E., Roeder T., Bruchhaus I. A peroxiredoxin specifically expressed in two types of pharyngeal neurons is required for normal growth and egg production in Caenorhabditis elegans. J. Mol. Biol. 2004;338:745–755. doi: 10.1016/j.jmb.2004.03.021. [DOI] [PubMed] [Google Scholar]
- 32.Kanzok S.M., Fechner A., Bauer H., Ulschmid J.K., Muller H.M., Botella-Munoz J., Schneuwly S., Schirmer R., Becker K. Substitution of the thioredoxin system for glutathione reductase in Drosophila melanogaster. Science. 2001;291:643–646. doi: 10.1126/science.291.5504.643. [DOI] [PubMed] [Google Scholar]
- 33.Winter A.D., McCormack G., Page A.P. Protein disulfide isomerase activity is essential for viability and extracellular matrix formation in the nematode Caenorhabditis elegans. Dev. Biol. 2007;308:449–461. doi: 10.1016/j.ydbio.2007.05.041. [DOI] [PubMed] [Google Scholar]
- 34.Pandolfi P.P., Sonati F., Rivi R., Mason P., Grosveld F., Luzzatto L. Targeted disruption of the housekeeping gene encoding glucose 6-phosphate dehydrogenase (G6PD): G6PD is dispensable for pentose synthesis but essential for defense against oxidative stress. EMBO J. 1995;14:5209–5215. doi: 10.1002/j.1460-2075.1995.tb00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fico A., Paglialunga F., Cigliano L., Abrescia P., Verde P., Martini G., Iaccarino I., Filosa S. Glucose-6-phosphate dehydrogenase plays a crucial role in protection from redox-stress-induced apoptosis. Cell Death Differ. 2004;11:823–831. doi: 10.1038/sj.cdd.4401420. [DOI] [PubMed] [Google Scholar]
- 36.Paglialunga F., Fico A., Iaccarino I., Notaro R., Luzzatto L., Martini G., Filosa S. G6PD is indispensable for erythropoiesis after the embryonic-adult hemoglobin switch. Blood. 2004;104:3148–3152. doi: 10.1182/blood-2004-03-0835. [DOI] [PubMed] [Google Scholar]
- 37.Filosa S., Fico A., Paglialunga F., Balestrieri M., Crooke A., Verde P., Abrescia P., Bautista J.M., Martini G. Failure to increase glucose consumption through the pentose-phosphate pathway results in the death of glucose-6-phosphate dehydrogenase gene-deleted mouse embryonic stem cells subjected to oxidative stress. Biochem. J. 2003;370:935–943. doi: 10.1042/bj20021614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Longo L., Vanegas O.C., Patel M., Rosti V., Li H., Waka J., Merghoub T., Pandolfi P.P., Notaro R., Manova K., et al. Maternally transmitted severe glucose 6-phosphate dehydrogenase deficiency is an embryonic lethal. EMBO J. 2002;21:4229–4239. doi: 10.1093/emboj/cdf426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perez-Crespo M., Ramirez M.A., Fernandez-Gonzalez R., Rizos D., Lonergan P., Pintado B., Gutierrez-Adan A. Differential sensitivity of male and female mouse embryos to oxidative induced heat-stress is mediated by glucose-6-phosphate dehydrogenase gene expression. Mol. Reprod. Dev. 2005;72:502–510. doi: 10.1002/mrd.20366. [DOI] [PubMed] [Google Scholar]
- 40.Patrinostro X., Carter M.L., Kramer A.C., Lund T.C. A model of glucose-6-phosphate dehydrogenase deficiency in the zebrafish. Exp. Hematol. 2013;41:697–710.e692. doi: 10.1016/j.exphem.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu Y.H., Lee Y.H., Shih H.Y., Chen S.H., Cheng Y.C., Tsun-Yee Chiu D. Glucose-6-phosphate dehydrogenase is indispensable in embryonic development by modulation of epithelial-mesenchymal transition via the NOX/Smad3/miR-200b axis. Cell Death Dis. 2018;9:10. doi: 10.1038/s41419-017-0005-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Babb S.G., Marrs J.A. E-cadherin regulates cell movements and tissue formation in early zebrafish embryos. Dev. Dyn. 2004;230:263–277. doi: 10.1002/dvdy.20057. [DOI] [PubMed] [Google Scholar]
- 43.Li P., Ma X., Adams I.R., Yuan P. A tight control of Rif1 by Oct4 and Smad3 is critical for mouse embryonic stem cell stability. Cell Death Dis. 2015;6:e1588. doi: 10.1038/cddis.2014.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J., Gao Y., Yu M., Wu H., Ai Z., Wu Y., Liu H., Du J., Guo Z., Zhang Y. Retinoic Acid Induces Embryonic Stem Cell Differentiation by Altering Both Encoding RNA and microRNA Expression. PLoS ONE. 2015;10:e0132566. doi: 10.1371/journal.pone.0132566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brenner S. The genetics of Caenorhabditis elegans. Genetics. 1974;77:71–94. doi: 10.1093/genetics/77.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yang H.C., Chen T.L., Wu Y.H., Cheng K.P., Lin Y.H., Cheng M.L., Ho H.Y., Lo S.J., Chiu D.T. Glucose 6-phosphate dehydrogenase deficiency enhances germ cell apoptosis and causes defective embryogenesis in Caenorhabditis elegans. Cell Death Dis. 2013;4:e616. doi: 10.1038/cddis.2013.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen T.L., Yang H.C., Hung C.Y., Ou M.H., Pan Y.Y., Cheng M.L., Stern A., Lo S.J., Chiu D.T. Impaired embryonic development in glucose-6-phosphate dehydrogenase-deficient Caenorhabditis elegans due to abnormal redox homeostasis induced activation of calcium-independent phospholipase and alteration of glycerophospholipid metabolism. Cell Death Dis. 2017;8:e2545. doi: 10.1038/cddis.2016.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang H.C., Yu H., Ma T.H., Tjong W.Y., Stern A., Chiu D.T. tert-Butyl Hydroperoxide (tBHP)-Induced Lipid Peroxidation and Embryonic Defects Resemble Glucose-6-Phosphate Dehydrogenase (G6PD) Deficiency in C. elegans. Int. J. Mol. Sci. 2020;21:8688. doi: 10.3390/ijms21228688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Almeida A.S., Soares N.L., Sequeira C.O., Pereira S.A., Sonnewald U., Vieira H.L.A. Improvement of neuronal differentiation by carbon monoxide: Role of pentose phosphate pathway. Redox Biol. 2018;17:338–347. doi: 10.1016/j.redox.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harris J.M., Esain V., Frechette G.M., Harris L.J., Cox A.G., Cortes M., Garnaas M.K., Carroll K.J., Cutting C.C., Khan T., et al. Glucose metabolism impacts the spatiotemporal onset and magnitude of HSC induction in vivo. Blood. 2013;121:2483–2493. doi: 10.1182/blood-2012-12-471201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hernandez-Garcia D., Wood C.D., Castro-Obregon S., Covarrubias L. Reactive oxygen species: A radical role in development? Free Radic Biol Med. 2010;49:130–143. doi: 10.1016/j.freeradbiomed.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 52.Hom J.R., Quintanilla R.A., Hoffman D.L., de Mesy Bentley K.L., Molkentin J.D., Sheu S.S., Porter G.A., Jr. The permeability transition pore controls cardiac mitochondrial maturation and myocyte differentiation. Dev. Cell. 2011;21:469–478. doi: 10.1016/j.devcel.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liang J., Wu M., Chen C., Mai M., Huang J., Zhu P. Roles of Reactive Oxygen Species in Cardiac Differentiation, Reprogramming, and Regenerative Therapies. Oxid. Med. Cell Longev. 2020;2020:2102841. doi: 10.1155/2020/2102841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang D., Li Y., Heims-Waldron D., Bezzerides V., Guatimosim S., Guo Y., Gu F., Zhou P., Lin Z., Ma Q., et al. Mitochondrial Cardiomyopathy Caused by Elevated Reactive Oxygen Species and Impaired Cardiomyocyte Proliferation. Circ. Res. 2018;122:74–87. doi: 10.1161/CIRCRESAHA.117.311349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kanda Y., Hinata T., Kang S.W., Watanabe Y. Reactive oxygen species mediate adipocyte differentiation in mesenchymal stem cells. Life Sci. 2011;89:250–258. doi: 10.1016/j.lfs.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 56.Dennery P.A. Effects of oxidative stress on embryonic development. Birth Defects Res. C Embryo Today. 2007;81:155–162. doi: 10.1002/bdrc.20098. [DOI] [PubMed] [Google Scholar]
- 57.Horwitz R., Webb D. Cell migration. Curr. Biol. 2003;13:R756–R759. doi: 10.1016/j.cub.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 58.Scarpa E., Mayor R. Collective cell migration in development. J. Cell Biol. 2016;212:143–155. doi: 10.1083/jcb.201508047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang G., Chen B.Z., Wang C.J., Zhang J., Gao L.R., Chuai M., Bao Y., Yang X. Ethanol exposure leads to disorder of blood island formation in early chick embryo. Reprod. Toxicol. 2017;73:96–104. doi: 10.1016/j.reprotox.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 60.Berndt C., Poschmann G., Stuhler K., Holmgren A., Brautigam L. Zebrafish heart development is regulated via glutaredoxin 2 dependent migration and survival of neural crest cells. Redox Biol. 2014;2:673–678. doi: 10.1016/j.redox.2014.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Syal S., Ng C., Kim Y., Janbieh J., Govind S., Deshpande G. Reactive oxygen species signaling in primordial germ cell development in Drosophila embryos. Genesis. 2020;58:e23362. doi: 10.1002/dvg.23362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Keller G. Embryonic stem cell differentiation: Emergence of a new era in biology and medicine. Genes Dev. 2005;19:1129–1155. doi: 10.1101/gad.1303605. [DOI] [PubMed] [Google Scholar]
- 63.Murry C.E., Keller G. Differentiation of embryonic stem cells to clinically relevant populations: Lessons from embryonic development. Cell. 2008;132:661–680. doi: 10.1016/j.cell.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 64.Agidigbi T.S., Kim C. Reactive Oxygen Species in Osteoclast Differentiation and Possible Pharmaceutical Targets of ROS-Mediated Osteoclast Diseases. Int. J. Mol. Sci. 2019;20:3576. doi: 10.3390/ijms20143576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Takahashi S., Zeydel M. gamma-Glutamyl transpeptidase and glutathione in aging IMR-90 fibroblasts and in differentiating 3T3 L1 preadipocytes. Arch. Biochem. Biophys. 1982;214:260–267. doi: 10.1016/0003-9861(82)90029-7. [DOI] [PubMed] [Google Scholar]
- 66.Li J., Stouffs M., Serrander L., Banfi B., Bettiol E., Charnay Y., Steger K., Krause K.H., Jaconi M.E. The NADPH oxidase NOX4 drives cardiac differentiation: Role in regulating cardiac transcription factors and MAP kinase activation. Mol. Biol. Cell. 2006;17:3978–3988. doi: 10.1091/mbc.e05-06-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhai J., Xiao Z., Wang Y., Wang H. Human embryonic development: From peri-implantation to gastrulation. Trends Cell Biol. 2022;32:18–29. doi: 10.1016/j.tcb.2021.07.008. [DOI] [PubMed] [Google Scholar]
- 68.Gerri C., Menchero S., Mahadevaiah S.K., Turner J.M.A., Niakan K.K. Human Embryogenesis: A Comparative Perspective. Annu. Rev. Cell Dev. Biol. 2020;36:411–440. doi: 10.1146/annurev-cellbio-022020-024900. [DOI] [PubMed] [Google Scholar]
- 69.Pera M.F., Rossant J. The exploration of pluripotency space: Charting cell state transitions in peri-implantation development. Cell Stem Cell. 2021;28:1896–1906. doi: 10.1016/j.stem.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 70.Reynolds L.P., McLean K.J., McCarthy K.L., Diniz W.J.S., Menezes A.C.B., Forcherio J.C., Scott R.R., Borowicz P.P., Ward A.K., Dahlen C.R., et al. Nutritional Regulation of Embryonic Survival, Growth, and Development. Adv. Exp. Med. Biol. 2022;1354:63–76. doi: 10.1007/978-3-030-85686-1_4. [DOI] [PubMed] [Google Scholar]
- 71.Laurent L.C. MicroRNAs in embryonic stem cells and early embryonic development. J. Cell. Mol. Med. 2008;12:2181–2188. doi: 10.1111/j.1582-4934.2008.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Allen R.G., Balin A.K. Oxidative influence on development and differentiation: An overview of a free radical theory of development. Free Radic. Biol. Med. 1989;6:631–661. doi: 10.1016/0891-5849(89)90071-3. [DOI] [PubMed] [Google Scholar]
- 73.Li Y., Huang T.T., Carlson E.J., Melov S., Ursell P.C., Olson J.L., Noble L.J., Yoshimura M.P., Berger C., Chan P.H., et al. Dilated cardiomyopathy and neonatal lethality in mutant mice lacking manganese superoxide dismutase. Nat. Genet. 1995;11:376–381. doi: 10.1038/ng1295-376. [DOI] [PubMed] [Google Scholar]
- 74.Allu A.D., Soja A.M., Wu A., Szymanski J., Balazadeh S. Salt stress and senescence: Identification of cross-talk regulatory components. J. Exp. Bot. 2014;65:3993–4008. doi: 10.1093/jxb/eru173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grant M.M., Koo H.C., Rosenfeld W. Oxygen affects human endothelial cell proliferation by inactivation of fibroblast growth factors. Am. J. Physiol. 1992;263:L370–L375. doi: 10.1152/ajplung.1992.263.3.L370. [DOI] [PubMed] [Google Scholar]
- 76.Ufer C., Wang C.C., Borchert A., Heydeck D., Kuhn H. Redox control in mammalian embryo development. Antioxid. Redox Signal. 2010;13:833–875. doi: 10.1089/ars.2009.3044. [DOI] [PubMed] [Google Scholar]
- 77.Sekiba K., Yoshioka T. Changes of lipid peroxidation and superoxide dismutase activity in the human placenta. Am. J. Obstet. Gynecol. 1979;135:368–371. doi: 10.1016/0002-9378(79)90707-5. [DOI] [PubMed] [Google Scholar]
- 78.Takehara Y., Yoshioka T., Sasaki J. Changes in the levels of lipoperoxide and antioxidant factors in human placenta during gestation. Acta Med. Okayama. 1990;44:103–111. doi: 10.18926/AMO/30438. [DOI] [PubMed] [Google Scholar]
- 79.Celotto A.M., Liu Z., Vandemark A.P., Palladino M.J. A novel Drosophila SOD2 mutant demonstrates a role for mitochondrial ROS in neurodevelopment and disease. Brain Behav. 2012;2:424–434. doi: 10.1002/brb3.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Borchert A., Wang C.C., Ufer C., Schiebel H., Savaskan N.E., Kuhn H. The role of phospholipid hydroperoxide glutathione peroxidase isoforms in murine embryogenesis. J. Biol. Chem. 2006;281:19655–19664. doi: 10.1074/jbc.M601195200. [DOI] [PubMed] [Google Scholar]
- 81.Li L. The Relevance of Mammalian Peroxiredoxins to the Gametogenesis, Embryogenesis, and Pregnancy Outcomes. Reprod. Sci. 2017;24:812–817. doi: 10.1177/1933719116667217. [DOI] [PubMed] [Google Scholar]
- 82.Fakruzzaman M., Ghanem N., Bang J.I., Ha A.N., Lee K.L., Sohn S.H., Wang Z., Lee D.S., Kong I.K. Effect of peroxiredoxin II on the quality and mitochondrial activity of pre-implantation bovine embryos. Anim. Reprod. Sci. 2015;159:172–183. doi: 10.1016/j.anireprosci.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 83.Hammond E.R., Stewart B., Peek J.C., Shelling A.N., Cree L.M. Assessing embryo quality by combining non-invasive markers: Early time-lapse parameters reflect gene expression in associated cumulus cells. Hum. Reprod. 2015;30:1850–1860. doi: 10.1093/humrep/dev121. [DOI] [PubMed] [Google Scholar]
- 84.Radyuk S.N., Michalak K., Klichko V.I., Benes J., Rebrin I., Sohal R.S., Orr W.C. Peroxiredoxin 5 confers protection against oxidative stress and apoptosis and also promotes longevity in Drosophila. Biochem. J. 2009;419:437–445. doi: 10.1042/BJ20082003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Buggisch M., Ateghang B., Ruhe C., Strobel C., Lange S., Wartenberg M., Sauer H. Stimulation of ES-cell-derived cardiomyogenesis and neonatal cardiac cell proliferation by reactive oxygen species and NADPH oxidase. J. Cell Sci. 2007;120:885–894. doi: 10.1242/jcs.03386. [DOI] [PubMed] [Google Scholar]
- 86.Jang J., Wang Y., Kim H.S., Lalli M.A., Kosik K.S. Nrf2, a regulator of the proteasome, controls self-renewal and pluripotency in human embryonic stem cells. Stem Cells. 2014;32:2616–2625. doi: 10.1002/stem.1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mohammadzadeh M., Halabian R., Gharehbaghian A., Amirizadeh N., Jahanian-Najafabadi A., Roushandeh A.M., Roudkenar M.H. Nrf-2 overexpression in mesenchymal stem cells reduces oxidative stress-induced apoptosis and cytotoxicity. Cell Stress Chaperones. 2012;17:553–565. doi: 10.1007/s12192-012-0331-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yuan Z., Zhang J., Huang Y., Zhang Y., Liu W., Wang G., Zhang Q., Wang G., Yang Y., Li H., et al. NRF2 overexpression in mesenchymal stem cells induces stem-cell marker expression and enhances osteoblastic differentiation. Biochem. Biophys. Res. Commun. 2017;491:228–235. doi: 10.1016/j.bbrc.2017.07.083. [DOI] [PubMed] [Google Scholar]
- 89.Lin Y., Sui L.C., Wu R.H., Ma R.J., Fu H.Y., Xu J.J., Qiu X.H., Chen L. Nrf2 inhibition affects cell cycle progression during early mouse embryo development. J. Reprod. Dev. 2018;64:49–55. doi: 10.1262/jrd.2017-042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Beg A.A., Sha W.C., Bronson R.T., Ghosh S., Baltimore D. Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-kappa B. Nature. 1995;376:167–170. doi: 10.1038/376167a0. [DOI] [PubMed] [Google Scholar]
- 91.Hilberg F., Aguzzi A., Howells N., Wagner E.F. c-jun is essential for normal mouse development and hepatogenesis. Nature. 1993;365:179–181. doi: 10.1038/365179a0. [DOI] [PubMed] [Google Scholar]
- 92.Johnson R.S., van Lingen B., Papaioannou V.E., Spiegelman B.M. A null mutation at the c-jun locus causes embryonic lethality and retarded cell growth in culture. Genes Dev. 1993;7:1309–1317. doi: 10.1101/gad.7.7b.1309. [DOI] [PubMed] [Google Scholar]
- 93.Schreiber M., Wang Z.Q., Jochum W., Fetka I., Elliott C., Wagner E.F. Placental vascularisation requires the AP-1 component fra1. Development. 2000;127:4937–4948. doi: 10.1242/dev.127.22.4937. [DOI] [PubMed] [Google Scholar]
- 94.Karreth F., Hoebertz A., Scheuch H., Eferl R., Wagner E.F. The AP1 transcription factor Fra2 is required for efficient cartilage development. Development. 2004;131:5717–5725. doi: 10.1242/dev.01414. [DOI] [PubMed] [Google Scholar]
- 95.Schorpp-Kistner M., Wang Z.Q., Angel P., Wagner E.F. JunB is essential for mammalian placentation. EMBO J. 1999;18:934–948. doi: 10.1093/emboj/18.4.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dunwoodie S.L. The role of hypoxia in development of the Mammalian embryo. Dev. Cell. 2009;17:755–773. doi: 10.1016/j.devcel.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 97.Compernolle V., Brusselmans K., Franco D., Moorman A., Dewerchin M., Collen D., Carmeliet P. Cardia bifida, defective heart development and abnormal neural crest migration in embryos lacking hypoxia-inducible factor-1alpha. Cardiovasc. Res. 2003;60:569–579. doi: 10.1016/j.cardiores.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 98.Amarilio R., Viukov S.V., Sharir A., Eshkar-Oren I., Johnson R.S., Zelzer E. HIF1alpha regulation of Sox9 is necessary to maintain differentiation of hypoxic prechondrogenic cells during early skeletogenesis. Development. 2007;134:3917–3928. doi: 10.1242/dev.008441. [DOI] [PubMed] [Google Scholar]
- 99.Ream M., Ray A.M., Chandra R., Chikaraishi D.M. Early fetal hypoxia leads to growth restriction and myocardial thinning. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;295:R583–R595. doi: 10.1152/ajpregu.00771.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.L’Honore A., Commere P.H., Ouimette J.F., Montarras D., Drouin J., Buckingham M. Redox regulation by Pitx2 and Pitx3 is critical for fetal myogenesis. Dev. Cell. 2014;29:392–405. doi: 10.1016/j.devcel.2014.04.006. [DOI] [PubMed] [Google Scholar]
- 101.Lozano-Velasco E., Vallejo D., Esteban F.J., Doherty C., Hernandez-Torres F., Franco D., Aranega A.E. A Pitx2-MicroRNA Pathway Modulates Cell Proliferation in Myoblasts and Skeletal-Muscle Satellite Cells and Promotes Their Commitment to a Myogenic Cell Fate. Mol. Cell. Biol. 2015;35:2892–2909. doi: 10.1128/MCB.00536-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ufer C., Wang C.C., Fahling M., Schiebel H., Thiele B.J., Billett E.E., Kuhn H., Borchert A. Translational regulation of glutathione peroxidase 4 expression through guanine-rich sequence-binding factor 1 is essential for embryonic brain development. Genes Dev. 2008;22:1838–1850. doi: 10.1101/gad.466308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Funato Y., Michiue T., Terabayashi T., Yukita A., Danno H., Asashima M., Miki H. Nucleoredoxin regulates the Wnt/planar cell polarity pathway in Xenopus. Genes Cells. 2008;13:965–975. doi: 10.1111/j.1365-2443.2008.01220.x. [DOI] [PubMed] [Google Scholar]
- 104.Funato Y., Michiue T., Asashima M., Miki H. The thioredoxin-related redox-regulating protein nucleoredoxin inhibits Wnt-beta-catenin signalling through dishevelled. Nat. Cell Biol. 2006;8:501–508. doi: 10.1038/ncb1405. [DOI] [PubMed] [Google Scholar]
- 105.Funato Y., Miki H. Redox regulation of Wnt signalling via nucleoredoxin. Free Radic. Res. 2010;44:379–388. doi: 10.3109/10715761003610745. [DOI] [PubMed] [Google Scholar]
- 106.Gwozdzinski K., Pieniazek A., Gwozdzinski L. Reactive Oxygen Species and Their Involvement in Red Blood Cell Damage in Chronic Kidney Disease. Oxid. Med. Cell. Longev. 2021;2021:6639199. doi: 10.1155/2021/6639199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lequarre A.S., Feugang J.M., Malhomme O., Donnay I., Massip A., Dessy F., Van Langendonckt A. Expression of Cu/Zn and Mn superoxide dismutases during bovine embryo development: Influence of in vitro culture. Mol. Reprod. Dev. 2001;58:45–53. doi: 10.1002/1098-2795(200101)58:1<45::AID-MRD7>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 108.Kably Ambe A., Ruiz Anguas J., Carballo Mondragon E., Corona de Lau C., Karchmer Krivitsky S. Correlation between follicle levels of superoxide dismutase and oocyte quality, fertilization rates and embryo development. Ginecol. Obstet. Mex. 2004;72:335–344. [PubMed] [Google Scholar]
- 109.Nonogaki T., Noda Y., Narimoto K., Umaoka Y., Mori T. Effects of superoxide dismutase on mouse in vitro fertilization and embryo culture system. J. Assist. Reprod. Genet. 1992;9:274–280. doi: 10.1007/BF01203828. [DOI] [PubMed] [Google Scholar]
- 110.Lee H., Ismail T., Kim Y., Chae S., Ryu H.Y., Lee D.S., Kwon T.K., Park T.J., Kwon T., Lee H.S. Xenopus gpx3 Mediates Posterior Development by Regulating Cell Death during Embryogenesis. Antioxidants. 2020;9:1265. doi: 10.3390/antiox9121265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Elshazzly M., Lopez M.J., Reddy V., Caban O. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. Embryology, Central Nervous System. [PubMed] [Google Scholar]
- 112.Olguin-Albuerne M., Moran J. Redox Signaling Mechanisms in Nervous System Development. Antioxid. Redox Signal. 2018;28:1603–1625. doi: 10.1089/ars.2017.7284. [DOI] [PubMed] [Google Scholar]
- 113.Petriv O.I., Rachubinski R.A. Lack of peroxisomal catalase causes a progeric phenotype in Caenorhabditis elegans. J. Biol. Chem. 2004;279:19996–20001. doi: 10.1074/jbc.M400207200. [DOI] [PubMed] [Google Scholar]
- 114.Miller-Pinsler L., Wells P.G. Embryonic catalase prot.tects against ethanol embryopathies in acatalasemic mice and transgenic human catalase-expressing mice in embryo culture. Toxicol. Appl. Pharmacol. 2015;287:232–239. doi: 10.1016/j.taap.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 115.Miller L., Wells P.G. Altered methanol embryopathies in embryo culture with mutant catalase-deficient mice and transgenic mice expressing human catalase. Toxicol. Appl. Pharmacol. 2011;252:55–61. doi: 10.1016/j.taap.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 116.Abramov J.P., Wells P.G. Embryonic catalase protects against endogenous and phenytoin-enhanced DNA oxidation and embryopathies in acatalasemic and human catalase-expressing mice. FASEB J. 2011;25:2188–2200. doi: 10.1096/fj.11-182444. [DOI] [PubMed] [Google Scholar]
- 117.Abramov J.P., Wells P.G. Embryoprotective role of endogenous catalase in acatalasemic and human catalase-expressing mouse embryos exposed in culture to developmental and phenytoin-enhanced oxidative stress. Toxicol. Sci. 2011;120:428–438. doi: 10.1093/toxsci/kfr007. [DOI] [PubMed] [Google Scholar]
- 118.Elhiti M., Stasolla C. Transduction of Signals during Somatic Embryogenesis. Plants. 2022;11:178. doi: 10.3390/plants11020178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Seminotti B., Grings M., Tucci P., Leipnitz G., Saso L. Nuclear Factor Erythroid-2-Related Factor 2 Signaling in the Neuropathophysiology of Inherited Metabolic Disorders. Front. Cell Neurosci. 2021;15:785057. doi: 10.3389/fncel.2021.785057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gacesa R., Dunlap W.C., Barlow D.J., Laskowski R.A., Long P.F. Rising levels of atmospheric oxygen and evolution of Nrf2. Sci. Rep. 2016;6:27740. doi: 10.1038/srep27740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Reddy N.M., Kleeberger S.R., Yamamoto M., Kensler T.W., Scollick C., Biswal S., Reddy S.P. Genetic dissection of the Nrf2-dependent redox signaling-regulated transcriptional programs of cell proliferation and cytoprotection. Physiol. Genom. 2007;32:74–81. doi: 10.1152/physiolgenomics.00126.2007. [DOI] [PubMed] [Google Scholar]
- 122.Dai X., Yan X., Wintergerst K.A., Cai L., Keller B.B., Tan Y. Nrf2: Redox and Metabolic Regulator of Stem Cell State and Function. Trends Mol. Med. 2020;26:185–200. doi: 10.1016/j.molmed.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 123.Ankrum J.A., Ong J.F., Karp J.M. Mesenchymal stem cells: Immune evasive, not immune privileged. Nat. Biotechnol. 2014;32:252–260. doi: 10.1038/nbt.2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bouyahya A., El Menyiy N., Oumeslakht L., El Allam A., Balahbib A., Rauf A., Muhammad N., Kuznetsova E., Derkho M., Thiruvengadam M., et al. Preclinical and Clinical Antioxidant Effects of Natural Compounds against Oxidative Stress-Induced Epigenetic Instability in Tumor Cells. Antioxidants. 2021;10:1553. doi: 10.3390/antiox10101553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yoshitomi Y., Ikeda T., Saito-Takatsuji H., Yonekura H. Emerging Role of AP-1 Transcription Factor JunB in Angiogenesis and Vascular Development. Int. J. Mol. Sci. 2021;22:2804. doi: 10.3390/ijms22062804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Checa J., Aran J.M. Reactive Oxygen Species: Drivers of Physiological and Pathological Processes. J. Inflamm. Res. 2020;13:1057–1073. doi: 10.2147/JIR.S275595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bentzinger C.F., Wang Y.X., Rudnicki M.A. Building muscle: Molecular regulation of myogenesis. Cold Spring Harb. Perspect. Biol. 2012;4:a008342. doi: 10.1101/cshperspect.a008342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cerychova R., Pavlinkova G. HIF-1, Metabolism, and Diabetes in the Embryonic and Adult Heart. Front. Endocrinol. 2018;9:460. doi: 10.3389/fendo.2018.00460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sheflin L.G., Zou A.P., Spaulding S.W. Androgens regulate the binding of endogenous HuR to the AU-rich 3′UTRs of HIF-1alpha and EGF mRNA. Biochem. Biophys. Res. Commun. 2004;322:644–651. doi: 10.1016/j.bbrc.2004.07.173. [DOI] [PubMed] [Google Scholar]
- 130.Galban S., Kuwano Y., Pullmann R., Jr., Martindale J.L., Kim H.H., Lal A., Abdelmohsen K., Yang X., Dang Y., Liu J.O., et al. RNA-binding proteins HuR and PTB promote the translation of hypoxia-inducible factor 1alpha. Mol. Cell. Biol. 2008;28:93–107. doi: 10.1128/MCB.00973-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yang R., Weber D.J., Carrier F. Post-transcriptional regulation of thioredoxin by the stress inducible heterogenous ribonucleoprotein A18. Nucleic Acids Res. 2006;34:1224–1236. doi: 10.1093/nar/gkj519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Miricescu D., Badoiu S.C., Stanescu S., II, Totan A.R., Stefani C., Greabu M. Growth Factors, Reactive Oxygen Species, and Metformin-Promoters of the Wound Healing Process in Burns? Int. J. Mol. Sci. 2021;22:9512. doi: 10.3390/ijms22179512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Heppner D.E., van der Vliet A. Redox-dependent regulation of epidermal growth factor receptor signaling. Redox Biol. 2016;8:24–27. doi: 10.1016/j.redox.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Rafikova O., Rafikov R., Kangath A., Qu N., Aggarwal S., Sharma S., Desai J., Fields T., Ludewig B., Yuan J.X., et al. Redox regulation of epidermal growth factor receptor signaling during the development of pulmonary hypertension. Free Radic. Biol. Med. 2016;95:96–111. doi: 10.1016/j.freeradbiomed.2016.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Azevedo Portilho N., Pelajo-Machado M. Mechanism of hematopoiesis and vasculogenesis in mouse placenta. Placenta. 2018;69:140–145. doi: 10.1016/j.placenta.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 136.Forsythe J.A., Jiang B.H., Iyer N.V., Agani F., Leung S.W., Koos R.D., Semenza G.L. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol. Cell Biol. 1996;16:4604–4613. doi: 10.1128/MCB.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Vriz S. Redox signalling in development and regeneration. Semin. Cell Dev. Biol. 2018;80:1–2. doi: 10.1016/j.semcdb.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 138.Guo Y.L., Chakraborty S., Rajan S.S., Wang R., Huang F. Effects of oxidative stress on mouse embryonic stem cell proliferation, apoptosis, senescence, and self-renewal. Stem Cells Dev. 2010;19:1321–1331. doi: 10.1089/scd.2009.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Forsyth N.R., Musio A., Vezzoni P., Simpson A.H., Noble B.S., McWhir J. Physiologic oxygen enhances human embryonic stem cell clonal recovery and reduces chromosomal abnormalities. Cloning Stem Cells. 2006;8:16–23. doi: 10.1089/clo.2006.8.16. [DOI] [PubMed] [Google Scholar]
- 140.Harvey A.J., Rathjen J., Yu L.J., Gardner D.K. Oxygen modulates human embryonic stem cell metabolism in the absence of changes in self-renewal. Reprod. Fertil. Dev. 2016;28:446–458. doi: 10.1071/RD14013. [DOI] [PubMed] [Google Scholar]
- 141.Tepekoy F., Akkoyunlu G., Demir R. The role of Wnt signaling members in the uterus and embryo during pre-implantation and implantation. J. Assist. Reprod. Genet. 2015;32:337–346. doi: 10.1007/s10815-014-0409-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Covarrubias L., Hernandez-Garcia D., Schnabel D., Salas-Vidal E., Castro-Obregon S. Function of reactive oxygen species during animal development: Passive or active? Dev. Biol. 2008;320:1–11. doi: 10.1016/j.ydbio.2008.04.041. [DOI] [PubMed] [Google Scholar]
- 143.Liu Y., Yang M., Deng Y., Su G., Enninful A., Guo C.C., Tebaldi T., Zhang D., Kim D., Bai Z., et al. High-Spatial-Resolution Multi-Omics Sequencing via Deterministic Barcoding in Tissue. Cell. 2020;183:1665–1681.e1618. doi: 10.1016/j.cell.2020.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Satoh N., Hisata K., Foster S., Morita S., Nishitsuji K., Oulhen N., Tominaga H., Wessel G. A single-cell RNA-seq analysis of Brachyury-expressing cell clusters suggests a morphogenesis-associated signal center of oral ectoderm in sea urchin embryos. Dev. Biol. 2022;483:128–142. doi: 10.1016/j.ydbio.2022.01.005. [DOI] [PubMed] [Google Scholar]
- 145.Palinkas H.L., Racz G.A., Gal Z., Hoffmann O.I., Tihanyi G., Rona G., Gocza E., Hiripi L., Vertessy B.G. CRISPR/Cas9-Mediated Knock-Out of dUTPase in Mice Leads to Early Embryonic Lethality. Biomolecules. 2019;9:136. doi: 10.3390/biom9040136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Piergentili R., Del Rio A., Signore F., Umani Ronchi F., Marinelli E., Zaami S. CRISPR-Cas and Its Wide-Ranging Applications: From Human Genome Editing to Environmental Implications, Technical Limitations, Hazards and Bioethical Issues. Cells. 2021;10:969. doi: 10.3390/cells10050969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Erwood S., Gu B. Embryo-Based Large Fragment Knock-in in Mammals: Why, How and What’s Next. Genes. 2020;11:140. doi: 10.3390/genes11020140. [DOI] [PMC free article] [PubMed] [Google Scholar]