Abstract
Background: Frailty has been associated with increased mortality among hepatobiliary pancreatic (HBP) cancer patients. Nevertheless, estimates of frailty prevalence in HBP cancers and the precise average effect regarding mortality remains uncertain. The present systematic review and meta-analysis aimed to quantify: (1) the prevalence of frailty in patients with liver and pancreatic cancers and (2) the impact of frailty on mortality in patients affected by liver and pancreatic cancers. Methods: MEDLINE/PubMed database search was conducted from inception until 1 November 2021, the pooled prevalence and relative risk (RR) estimate were calculated. Results: A total of 34,276 patients were identified and the weighted prevalence of frailty was 39%; (95% [C.I.] 23–56; I2 = 99.9%, p < 0.0001). Frailty was significantly associated with increased mortality RR 1.98 (95% [C.I.] 1.49–2.63; I2 = 75.9%, p = 0.006). Conclusions: Frailty prevalence is common among HBP cancer patients and exerts a significant negative impact on survival. These findings are characterized by significant heterogeneity and caution is warranted on their interpretation. However, stratification of patients with HBP cancer by frailty status may provide prognostic information and may inform priorities for decision-making strategy.
Keywords: frailty, elderly, mortality, hepatic cancer, biliary cancer, pancreatic cancer
1. Introduction
Frailty is a clinical syndrome characterized by multiple reductions in physiological reserves and vulnerability to stressors [1]. New drugs, infections, surgery, and hospitalizations are common stressors which may trigger significant changes in health status of frail patients, leading to several negative health outcomes and mortality.
Even though a standardized frailty measurement tool is still lacking, different frailty models have been developed, with the Fried phenotype model and cumulative deficit model, based on comprehensive geriatric assessments (CGA), being the most common [2,3]. Frailty is associated with advanced age, physical and cognitive decline, multiple chronic conditions and polypharmacotherapy.
Oncologic patients are characterized by several features of frailty syndrome, such as reduction in physiological reserves, low physical performance, malnutrition, cachexia. Moreover, chemotherapy and surgical treatment may induce adverse outcomes [4]. Almost one-third of cancers are diagnosed in patients aged 70 years or over, making the therapeutic approach and the prognosis in this population particularly challenging [5].
According to recent epidemiological data, liver and pancreatic cancers counted, respectively, 905, 677, and 495,773 new cancer cases in 2020 worldwide, and estimation of cancer death was 830,180 for liver and 466,003 for pancreas malignances [6]. Recent data have shown that surgery procedures for the elderly with hepatic and liver cancers may be well tolerated, but frailty concurs to influence the decision-making strategies [7,8]. A recent consensus statement suggested that frailty may be associated with negative short- and long-term outcomes in patients with hepatobiliary and pancreatic malignancies [9]. Frailty assessment in this population may contribute to disease management; accordingly, detection of other systems and organ deficits before treatment strategy reduces the risk of complications. Indeed, CGA has shown a predictive role in treatment toxicity and complications. However, epidemiological data regarding the prevalence and the impact of frailty in this population are lacking. Therefore, in this study, we aimed to quantitatively synthesize, through a systematic review and meta-analysis, (1) the prevalence of frailty in patients with liver and pancreatic cancers and (2) the impact of frailty on mortality in patients affected by liver and pancreatic cancers.
2. Materials and Methods
This systematic review and meta-analysis were performed according to the Preferred Reporting Items for Statistic Reviews and Meta-Analyses (PRISMA) statement and Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [10,11]. This study followed a pre-determined unpublished protocol available upon request.
2.1. Search Strategy
Studies were identified and evaluated independently by two authors in the MEDLINE/PubMed database, until 1 November 2021. Free text terms and or MeSH terms were used as keywords for the search strategy referred to frailty, geriatric assessments, pancreatic cancer, biliary cancer, and liver cancer. In detail, we used the combination of the following search terms: geriatric assessment AND (biliary cancer OR liver cancer OR pancreatic cancer) and frailty AND (biliary cancer OR liver cancer OR pancreatic cancer). Each of these combinations provided the following complete search items. The complete search items which result from the above-mentioned combinations are: ((“geriatric assessment”[MeSH Terms] OR (“geriatric”[All Fields] AND “assessment”[All Fields]) OR “geriatric assessment”[All Fields]) AND (“biliary tract neoplasms”[MeSH Terms] OR (“biliary”[All Fields] AND “tract”[All Fields] AND “neoplasms”[All Fields]) OR “biliary tract neoplasms”[All Fields] OR (“biliary”[All Fields] AND “cancer”[All Fields]) OR “biliary cancer”[All Fields] OR (“liver neoplasms”[MeSH Terms] OR (“liver”[All Fields] AND “neoplasms”[All Fields]) OR “liver neoplasms”[All Fields] OR (“liver”[All Fields] AND “cancer”[All Fields]) OR “liver cancer”[All Fields]) OR (“pancreatic neoplasms”[MeSH Terms] OR (“pancreatic”[All Fields] AND “neoplasms”[All Fields]) OR “pancreatic neoplasms”[All Fields] OR (“pancreatic”[All Fields] AND “cancer”[All Fields]) OR “pancreatic cancer”[All Fields]))) AND (1000/1/1:2021/11/1[pdat]); and ((“frailty”[MeSH Terms] OR “frailty”[All Fields] OR “frailties”[All Fields]) AND (“biliary tract neoplasms”[MeSH Terms] OR (“biliary”[All Fields] AND “tract”[All Fields] AND “neoplasms”[All Fields]) OR “biliary tract neoplasms”[All Fields] OR (“biliary”[All Fields] AND “cancer”[All Fields]) OR “biliary cancer”[All Fields] OR (“liver neoplasms”[MeSH Terms] OR (“liver”[All Fields] AND “neoplasms”[All Fields]) OR “liver neoplasms”[All Fields] OR (“liver”[All Fields] AND “cancer”[All Fields]) OR “liver cancer”[All Fields]) OR (“pancreatic neoplasms”[MeSH Terms] OR (“pancreatic”[All Fields] AND “neoplasms”[All Fields]) OR “pancreatic neoplasms”[All Fields] OR (“pancreatic”[All Fields] AND “cancer”[All Fields]) OR “pancreatic cancer”[All Fields])) AND 1000/01/01:2021/11/01[Date—Publication]) AND (1000/1/1:2021/11/1[pdat]).
2.2. Selection Criteria
All selected titles and abstracts were reviewed by two authors independently. Studies were considered eligible if they fulfilled the following criteria: aim 1: (a) they reported the prevalence of frailty in patients with pancreatic cancer; (b) they reported the prevalence of frailty in patients with liver or biliary cancer; aim 2: (a) studies which reported relevant analysis regarding liver and or pancreatic cancer mortality in patients with and without frailty. Only articles published in English language were considered. Articles reporting data on pancreatic and periampullary cancers were also considered for this study. Exclusion criteria were (a) abstracts, editorials, comments, unpublished data; (b) unclear frailty definition; (c) frailty assessment only based on single measure such as gait speed, grip strength, or muscle mass; and (d) studies where data regarding the number of death events were not stratified on frailty status, and where calculation of relative risk (RR) was not possible.
2.3. Quality and Risk of Bias Assessment
Quality of the included studies was assessed using the guidelines in the Newcastle–Ottawa Scale (NOS) [12], based on selection, comparability, exposure, or endpoint. These items were categorized into three major components containing eight items. Presence of publication bias was explored visually performing the test for asymmetry of the funnel plot by Egger test [13].
2.4. Data Extraction
Two reviewers, independently using a standardized form, completed data extraction. Disagreement was resolved by consensus and by the opinion of a third reviewer when necessary. Information on study year, author first name, data regarding sample size, prevalence, setting, outcome, and characteristics of pancreatic or liver cancers was recorded.
2.5. Statistical Analysis
The prevalence of frailty was summarized using descriptive statistics. Pooled prevalence rates accounting for inter-study variation were analyzed using a non-linear random effects model and statistical uncertainties were expressed in 95% Confidence Intervals (CI). RR estimates together with CI were extracted from each study and a pooled overall average effect size was calculated using random effect models. Heterogeneity was assessed using I2 statistic. Heterogeneity has been considered substantial if I2 value was greater than 25% [14]. To explore the reasons for heterogeneity subgroup analysis was conducted for: (a) studies identifying frailty with Fried Frailty Phenotype; (b) studies identifying frailty with Modified Frailty Index; (c) data regarding pancreas cancer; and (d) data regarding liver cancer. In addition, to explore the influence of potential effect modifiers on endpoints, a meta-regression analysis was performed to test age and sex (male%). For all meta-regression analyses, a random effects model was used to take into account the mean of a distribution of effects across studies. All reported test results were two-tailed and a p value ≤ 0.05 was considered significant. Data analyses were performed with STATA version 16 (StataCorp LLC, College Station, TX, USA).
3. Results
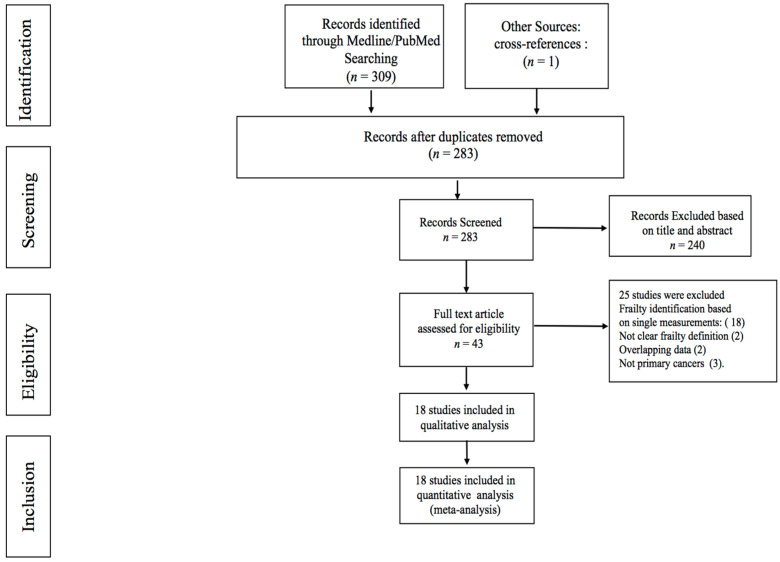
A total of 310 articles were identified by the initial search (Figure 1), 43 manuscripts were retrieved for more detailed evaluation, and 18 studies [7,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30] were finally included in the systematic review qualitative and quantitative analysis. Relevant data regarding mortality were reported in four studies. Detailed characteristics of the included studies are reported in Table 1.
Figure 1.
Flowchart of search strategy and included studies.
Table 1.
Characteristics of included studies.
| First Author and Year | Study Design | Total Population | Mean Age | Male (%) | Frail | Non-Frail | Frailty Tool | Cancer Type | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Al Abbas et al., 2020 | Retrospective Cohort Study | 9867 | 64.5 | 53.2 | 5996 | 3871 | Modified Frailty Index | Pancreatic Cancers (Adenocarcinoma 50%) | Surgery, Chemotherapy, Radiotherapy |
| Augustin et al., 2016 | Retrospective Cohort Study | 13,020 | N/R | 48.3 | 8024 | 4996 | Modified Frailty Index | Pancreatic Cancer, not specified | Surgery, Chemotherapy, Radiation |
| Baimas-George et al., 2021 | Prospective Cohort Study | 19 | 62 | 47 | 14 | 5 | Fried Phenotype Model | Pancreatic Adenocarcinoma (90%); Colangiocarcinoma (10%) | Chemotherapy, Surgery |
| Benjamin et al., 2017 | Prospective Cohort Study | 134 | 65.4 | 52 | 29 | 105 | SPPB | Pancreatic Ductal Adenocarcinoma | Surgery |
| Dale et al., 2014 | Prospective Cohort Study | 76 | 67.3 | 56.3 | 11 | 65 | VES-13, Fried and SPPB | Pancreatic Endocrine, Exocrine, Biliary | Surgery |
| DeMaria et al., 2019 | Prospective Cohort Study | 50 | 64 | 68 | 15 | 35 | Fried Phenotype Model | Hepatocellular Carcinoma | Surgery, liver transplantation |
| Gebbia et al., 2020 | Prospective Cohort Study | 40 | 74.7 | 65 | 34 | 6 | G8 | Advanced/metastatic Pancreatic Carcinoma | Chemotherapy |
| Kaibori et al., 2021 | Retrospective Cohort Study | 100 | 79 | N/R | 50 | 50 | G8, VES-13 | Hepatocellular Carcinoma | Surgery |
| Limpawattana et al., 2019 | Retrospective Cohort Study | 75 | N/R | 77.3 | 9 | 66 | Frail Scale | Biliary Cancer | Chemotherapy |
| Loi et al., 2021 | Retrospective Cohort Study | 42 | 85.3 | N/R | 11 | 31 | G8 | Hepatocellular Carcinoma | SBRT |
| Mima et al., 2021 | Retrospective Cohort Study | 142 | 56 | 16 | 126 | Clinical Frailty Scale | Pancreatic Cancer: Adenocarcinoma (98%) | Surgery | |
| Mogal et al., 2017 | Retrospective Cohort Study | 9986 | 64.1 | 51.2 | 637 | 9349 | Modified Frailty Index | Pancreatic Cancer, not specified | Surgery |
| Ngo-Huang et al., 2019 | Prospective Cohort Study | 142 | 65 | 65.5 | 36 | 106 | Fried Phenotype Model | Pancreatic Ductal Adenocarcinoma | Surgery, Chemotherapy, Radiation, Palliative |
| Reiser et al., 2021 | Retrospective Cohort Study | 158 | N/R | 37 | 68 | 90 | Modified Frailty Index | Pancreatic Ductal Adenocarcinoma | Surgery, Neoadjuvant therapy |
| Rittberg et al., 2020 | Retrospective Cohort Study | 87 | 73.7 | 54 | 67 | 20 | Modified Frailty Index | Advanced Pancreatic Cancer | Chemotherapy |
| van Wijk et al., 2021 | Prospective Cohort Study | 100 | 74 | 51 | 22 | 78 | Groningen frailty indicator | Hepatobiliary pancreatic cancers (Mixed population) | Scheduled for surgery |
| Yamada et al., 2021 | Retrospective Cohort Study | 120 | N/R | N/R | 29 | 91 | Clinical Frailty Scale | Pancreatic Ductal Adenocarcinoma | Surgery |
| Paolini et al., 2021 | Retrospective Cohort Study | 118 | 52.5 | 81 | 37 | Modified Frailty Index | Pancreatic, periampullary cancers, common bile duct cancers | Surgery (open or robotic) |
3.1. Prevalence of Frailty in Patients with Pancreatic and Liver Cancer
A total of 34,276 patients were identified with an average age ranging from 62 to 85.3 years and a rate of male population ranging from 37.9% to 76%. Characteristics of studies included in the meta-analysis are reported in Table 1. The weighted prevalence of frailty in patients with pancreas and liver cancer was 39%, (95% [C.I.] 23–56; I2 = 99.9%, p < 0.0001) (Figure 2). Meta-regression analysis revealed that age (beta coefficient 0.004 95% CI −0.0202–0.030 p = 0.697) and male population: beta coefficient −0.006 (95% [C.I.] −0.022–0.009 p = 0.408) were not significant moderators.
Figure 2.
Overall prevalence of frailty in patients with HBP cancer. Forest plot of cumulative prevalence of frailty from all included studies. Squares are study-specific prevalence. Diamond is the pooled prevalence. Horizontal lines represent 95% Confidence Interval (CI).
3.2. Subgroup Analysis
Estimated prevalence of frailty in patients with pancreas cancer was 42% (95% [C.I.] 19–64; I2 = 100%, p < 0.0001) (Supplementary Material Figure S1), and in patients with liver cancer was 29% (95% [C.I.] 11–48; I2 = 92%, p < 0.0001) (Supplementary Material Figure S2).
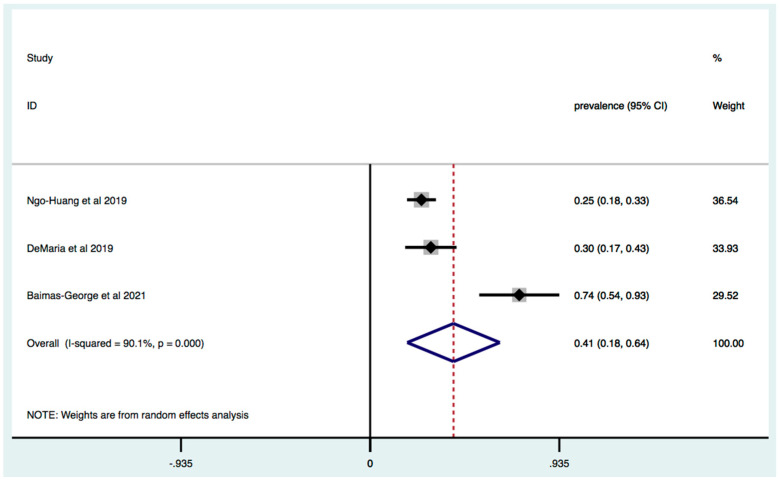
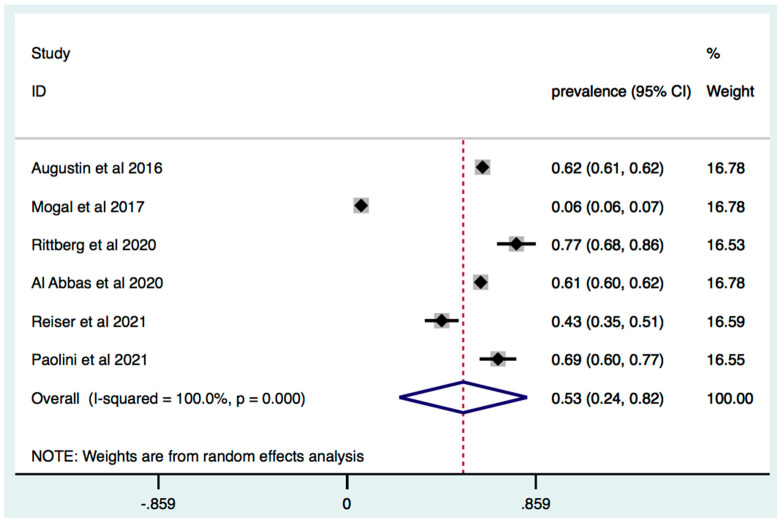
The Fried Frailty Model was used for the detection of frailty in three studies and the overall prevalence was 41% (95% [C.I.] 18–64; I2 = 90.1%, p < 0.0001) (Figure 3). The Modified Frailty Index was performed in six studies and estimated prevalence of frailty across these studies was 53% (95% [C.I.] 24–82; I2 = 100%, p < 0.0001) (Figure 4).
Figure 3.
Prevalence of frailty in patients with HPB cancer: identification of frailty based on Fried Frailty Criteria. Forest plot of cumulative prevalence of frailty from all studies applying Fried Phenotype Model. Squares are study-specific prevalence. Diamond is the pooled prevalence. Horizontal lines represent 95% Confidence Interval (CI).
Figure 4.
Prevalence of frailty in patients with HPB cancer: identification of frailty based on Modified Frailty Index. Forest plot of cumulative prevalence of frailty from all studies applying Modified Frailty Index. Squares are study-specific prevalence. Diamond is the pooled prevalence. Horizontal lines represent 95% Confidence Interval (CI).
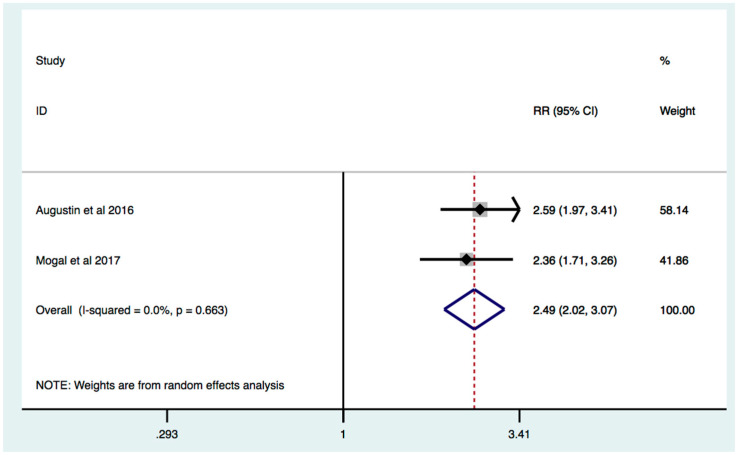
3.3. Frailty Is Associated with Increased Mortality in Patients with HPB Cancer
On the basis of data from four studies, frailty was significantly associated with increased mortality RR 1.98 (95% [C.I.] 1.49–2.63; I2 = 75.9%, p = 0.006) (Figure 5). In studies where frailty detection was performed by the Modified Frailty Index, effect estimate was increased by 25.8%: RR 2.49 (95% [C.I.] 2.02–3.07; I2 = 0%, p = 0.663) (Figure 6). Subgroup analysis of studies where only surgery treatment was performed also revealed that frail HBP patients, compared to non-frail HPB patients, are characterized by increased mortality: RR: 1.79 [C.I.] 1.35–2.39; I2 = 67.4%, p = 0.046 (Supplementary Material Figure S3).
Figure 5.
Effect of frailty on mortality in patients with HPB cancer. Forest plot of mortality risk comparing frailty hepatobiliary pancreatic cancers vs. non-frail hepatobiliary pancreatic cancer patients. Squares are study-specific Relative Risk (RR). Diamond is the estimated overall RR. Horizontal lines represent 95% Confidence Interval (CI).
Figure 6.
Effect of frailty on mortality in patients with HPB cancer: identification of frailty based on Modified Frailty Index. Forest plot of mortality risk comparing frailty hepatobiliary pancreatic cancers vs. non-frail hepatobiliary pancreatic cancer patients when frailty was identified by Modified Frailty Index. Squares are study-specific Relative Risk (RR). Diamond is the estimated overall RR. Horizontal lines represent 95% Confidence Interval (CI).
3.4. Study Quality
The quality of the included studies evaluated by NOS criteria was moderate or good, ranging from 5 to 8 points. NOS quality assessment of the included studies are reported in Supplementary Table S1.
3.5. Publication Bias
Asymmetry was assessed by visual inspection of funnel plots. However, Egger’s regression test did not indicate significant publication bias among the included studies. For aim 1, overall prevalence p = 0.291; subgroup analysis frailty prevalence in pancreas cancer p = 0.421; liver cancer p = 0.735; and aim 2, p = 0.334 (funnel plots in Supplementary Materials Figures S4–S7).
4. Discussion
The present systematic review and meta-analysis summarize for the first time the prevalence of frailty among patients affected by HPB cancers. The evaluation of data regarding 34,276 patients revealed that frailty prevalence accounts to about 39% in this population. Furthermore, frailty exerts an adverse role in overall mortality, as demonstrated by RR 1.98 95% C.I. 1.49–2.63. However, the interpretation of our findings is limited by the different definitions and criteria used to identify frailty.
Frailty is a wide-range metric of general health status and multiple physiological reserves, which strongly correlates with patient prognosis [31,32]. The prevalence of frailty in community dwelling population ranges from 4 to 59%, based on the criteria used for the definition and identification of frailty [33]. Frailty evaluation in single diseases is also reported to range widely, for instance from 9–28% in chronic obstructive pulmonary disease, 52.2–85.9% in hypertension, and 15–52% in heart failure [34,35]. Furthermore, frailty prevalence in patients with advanced liver disease awaiting liver transplantation ranges from 17–43% [36].
In our study, the overall estimates of frailty prevalence were 39% (95% [C.I.] 23–56%) considering all patients affected by pancreas and liver cancers. A previous meta-analysis study focused on frailty prevalence in all oncologic patients revealed that the median prevalence of frailty is about 42% ranging from 6 to 86% [4]. Our finding regarding overall prevalence is in line with this study, even if most of the articles were on breast, prostate, and colon-rectal cancers [4]. Considering that breast and prostate cancers are characterized by high incidence in ageing population, it is intuitive to expect a high prevalence of frailty in these populations. Pancreas and liver cancer are not as frequent as breast, prostate, or colon-rectal cancers world-wide; nevertheless, the high prevalence of frailty that we find in this study may be explained by the increased incidence, proportional to chronological age. Indeed, cholangiocarcinoma’s incidence increases with age, peaking at 59–75 years for males and 80–84 years for females [37], while median age for hepatocellular carcinoma onset in Europe, Japan, and North America is over 62 years [38]. In most of the evidence, the incidence of pancreatic cancer increases with age, occurring mostly after the age of 70 and only 32% of patients are diagnosed under 64 years in the U.S.A. [39]. However, in our findings, definition and screening of frailty was performed by a huge variety of assessment scales, such as the Modified Frailty Index, Fried Frailty index, short physical performance battery, clinical frailty scale, G8 score, and VES-13 scale. It should be mentioned that not all the above-mentioned assessment tools focus on the same aspects of frailty and heterogeneity which have been detected in the methods used to identify frailty. Indeed, Kojima et al, reported that quantification of frailty is performed by dissimilar tools even in the same clinical setting and, surprisingly, application of the same method still produced a wide range of frailty prevalence [40]. Of note, a study focused on the prevalence and feasibility of different frailty screening tools in nursing homes concluded that conceptualization of frailty leads to a significant heterogeneity in the prevalence of frailty, which significantly affects the interrelation between multimorbidity and disability [41]. Despite this, some studies report that different frailty tools have shown a similar capacity to detect frailty and similar prognostic potentialities [42].
Pathophysiology of frailty is characterized by reduced reserves of different inter-related systems and organs such as: brain, endocrine, immune, musculoskeletal, cardiovascular, respiratory, and renal. Frailty syndrome is often characterized by extreme fatigue, un-explained weight loss, and fluctuating disability [1]. Delirium and falls are further consequences, commonly associated with hospitalization which leads to the development of severely impaired mobility [43,44]. Significant weight loss and fatigue are frequent symptoms in oncologic patient. Moreover, pain, dysphagia, and reduced absorption of nutrients, which characterize clinical presentation of pancreas and liver cancer [45], may lead to malnutrition [46] and the development of muscle mass impairment. Typical biological substrate of physical frailty is represented by fatigue, malnutrition, reduced muscle mass, impairment of physical performance, and mobility. Limited functional reserve, impairment of liver function, and chemotherapy may contribute to the development of muscle mass reduction and sarcopenia [47,48,49,50].
In addition, chronic inflammation and immune system modulation are closely related to liver and pancreatic cancers progression [51,52].
Frail HBP cancer patients, compared to non-frail HPB cancer patients, suffer from an increased risk of mortality, revealing that frailty is a significant predictor of mortality in this population. Accumulation of health deficits related to functional status, mobility, malnutrition, and comorbidities are all elements of frailty, apart from the chronological age, which may influence the overall survival [53]. Poor physical performance is strongly associated with disability and adverse surgical outcomes [54,55]. A meta-analysis study revealed that sarcopenia was associated with an increased risk of complications after gastrointestinal tumor resection and suggested that combination of physical performance and muscle mass measurements may increase the prognostic value and accuracy in preoperative risk stratification [47].
Sub-group analysis of studies whose frailty assessment was based on the Modified Frailty Index, which takes into account comorbidities and functional status, increased the effect estimates: RR 2.49 (95% [C.I.] 2.07–3.11). Furthermore, analysis of data in HPB patients who had undergone surgery also revealed that frailty is significantly associated with increased mortality: RR: 1.79 (95% [C.I.] 1.35–2.39).
The advances made in medical care have provided an important rise of elderly population needing oncologic and surgical management. Despite substantial improvements in perioperative management and surgical techniques, pancreatic and hepatobiliary surgery carries a high risk of morbidity and mortality [56,57]. As matter of the fact, frailty screening it is not routinely performed among HBP cancer patients, however findings from our meta-analysis strongly encourage clinicians to perform CGA in this population, as it represents the only method to evaluate the complexity which characterizes elderly patients with malignancies. Furthermore, frailty evaluations may provide relevant information about multiple accumulated deficits as malnutrition, physical mobility impairment and reduced cognitive performance; furthermore, it may also exert preventive role, as pre-rehabilitation procedures and new developing strategies may be applied in selected patients [58,59,60,61,62]. The oncological outcomes of laparoscopic liver resection in elderly patients with colorectal metastasis were comparable to those observed with open resection, and a reduction in both minor and major postoperative morbidity was observed [63,64].
In addition, some perioperative parameters such as drain removal and refeeding seem to favor robotic pancreaticoduodenectomy compared to open surgery in frail patients [30] and, in selective cases, robotic surgery may be considered for colorectal cancer liver metastases [65,66,67].
Limitations
Our data are characterized by increased heterogeneity, as demonstrated by I2 evaluation of above 45%. It should be mentioned that different frailty detection tools used in different studies may, in part, explain the high heterogeneity. In addition, our analysis is based on observational studies, which may be characterized by increased heterogeneity. Another limitation of our results is that data from the included studies were not sufficient to provide subgroup analysis based on pancreas or liver cancer subtypes. Furthermore, it was not possible to compare different treatment strategies.
5. Conclusions
The present systematic review and meta-analysis study summarizes the prevalence and the effects of frailty on overall mortality among patients with HBP cancers. Frailty prevalence is high and exerts a negative role on survival of HBP cancer patients. These findings are characterized by significant heterogeneity, and lack of a standard definition of frailty hampers their interpretation. However, stratification of patients with HBP cancer based on comprehensive geriatric assessment tools may provide prognostic information and may critically contribute to decision-making strategy.
Acknowledgments
Leonardo Bencivenga has been supported by the research grant provided by the Cardiopath PhD program, the research grant provided by the FDIME, and the STAR PLUS research Grant provided by University of Naples Federico II.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11041116/s1, Figure S1. Overall prevalence of frailty in patients with pancreas cancer; Figure S2. Overall prevalence of frailty in patients with liver cancer; Figure S3: Mortality risk in frail vs non frail patients with HPB cancer where surgery treatment was performed; Figure S4: funnel plot of all prevalence studies; Figure S5: funnel plot of prevalence studies including only pancreas cancer; Figure S6: funnel plot of prevalence studies including only liver cancers; Figure S7: funnel plot of mortality risk; Table S1. Study Quality.
Author Contributions
Conceptualization, K.K. and L.B.; methodology, M.C.; software, R.V.; validation, G.R. and G.G.; formal analysis, K.K.; investigation, L.B., G.D.C. and M.C.B.; resources, K.K.; data curation, A.S., V.P., G.D.C. and M.C.; P.A.; writing—original draft preparation, K.K.; writing—review and editing, L.B.; visualization, G.G.; and supervision, G.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting the results of the study will be available on request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Clegg A., Young J., Iliffe S., Rikkert M.O., Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fried L.P., Tangen C.M., Walston J., Newman A.B., Hirsch C., Gottdiener J., Seeman T., Tracy R., Kop W.J., Burke G., et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001;56:M146–M157. doi: 10.1093/gerona/56.3.M146. [DOI] [PubMed] [Google Scholar]
- 3.Rockwood K., Song X.W., MacKnight C., Bergman H., Hogan D.B., McDowell I., Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Handforth C., Clegg A., Young C., Simpkins S., Seymour M.T., Selby P.J., Young J. The prevalence and outcomes of frailty in older cancer patients: A systematic review. Ann. Oncol. 2014;26:1091–1101. doi: 10.1093/annonc/mdu540. [DOI] [PubMed] [Google Scholar]
- 5.Venuta F., Diso D., Onorati I., Anile M., Mantovani S., Rendina E.A. Lung cancer in elderly patients. J. Thorac. Dis. 2016;8((Suppl. 11)):S908–S914. doi: 10.21037/jtd.2016.05.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 7.Dale W., Hemmerich J., Kamm A., Posner M.C., Matthews J.B., Rothman R., Palakodeti A., Roggin K.K. Geriatric assessment improves prediction of surgical outcomes in older adults undergoing pancreaticoduodenectomy: A prospective cohort study. Ann. Surg. 2014;259:960–965. doi: 10.1097/SLA.0000000000000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de la Fuente S.G., Bennett K.M., Pappas T.N., Scarborough J.E. Pre- and intraoperative variables affecting early outcomes in elderly patients undergoing pancreaticoduodenectomy. HPB. 2011;13:887–892. doi: 10.1111/j.1477-2574.2011.00390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rostoft S., van Leeuwen B. Frailty assessment tools and geriatric assessment in older patients with hepatobiliary and pancreatic malignancies. Eur. J. Surg. Oncol. 2021;47:514–518. doi: 10.1016/j.ejso.2020.08.024. [DOI] [PubMed] [Google Scholar]
- 10.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 11.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009;3:e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 12.Lo C.K., Mertz D., Loeb M. Newcastle-Ottawa Scale: Comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson S.G., Sharp S.J. Explaining heterogeneity in meta-analysis: A comparison of methods. Stat. Med. 1999;18:2693–2708. doi: 10.1002/(SICI)1097-0258(19991030)18:20<2693::AID-SIM235>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 15.Al Abbas A.I., Borrebach J.D., Pitt H.A., Bellon J., Hogg M.E., Zeh H.J., Zureikat A.H. Development of a Novel Pancreatoduodenectomy-Specific Risk Calculator: An Analysis of 10,000 Patients. J. Gastrointest. Surg. 2020;25:1503–1511. doi: 10.1007/s11605-020-04725-0. [DOI] [PubMed] [Google Scholar]
- 16.Augustin T., Burstein M.D., Schneider E.B., Morris-Stiff G., Wey J., Chalikonda S., Walsh R.M. Frailty predicts risk of life-threatening complications and mortality after pancreatic resections. Surgery. 2016;160:987–996. doi: 10.1016/j.surg.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Baimas-George M., Watson M., Thompson K., Shastry V., Iannitti D., Martinie J.B., Baker E., Parala-Metz A., Vrochides D. Prehabilitation for Hepatopancreatobiliary Surgical Patients: Interim Analysis Demonstrates a Protective Effect From Neoadjuvant Chemotherapy and Improvement in the Frailty Phenotype. Am. Surg. 2020;87:714–724. doi: 10.1177/0003134820952378. [DOI] [PubMed] [Google Scholar]
- 18.DeMaria S.D., Jr., Khromava M., Schiano T.D., Lin H.M., Kim S. Standardized measures of frailty predict hospital length of stay following orthotopic liver transplantation for hepatocellular carcinoma. Clin. Transplant. 2019;33:e13746. doi: 10.1111/ctr.13746. [DOI] [PubMed] [Google Scholar]
- 19.Gebbia V., Mare M., Cordio S., Valerio M.R., Piazza D., Bordonaro R., Firenze A., Giuffrida D. Is G8 geriatric assessment tool useful in managing elderly patients with metastatic pancreatic carcinoma? J. Geriatr. Oncol. 2021;12:163–167. doi: 10.1016/j.jgo.2020.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Kaibori M., Matsushima H., Ishizaki M., Kosaka H., Matsui K., Ogawa A., Yoshii K., Sekimoto M. Perioperative Geriatric Assessment as A Predictor of Long-Term Hepatectomy Outcomes in Elderly Patients with Hepatocellular Carcinoma. Cancers. 2021;13:842. doi: 10.3390/cancers13040842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Limpawattana P., Wirasorn K., Sookprasert A., Sawanyawisuth K., Titapun A., Luvira V., Khuntikeo N., Chindaprasirt J. Frailty Syndrome in Biliary Tract Cancer Patients: Prevalence and Associated Factors. Asian Pac. J. Cancer Prev. 2019;20:1497–1501. doi: 10.31557/APJCP.2019.20.5.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loi M., Comito T., Franzese C., Desideri I., Dominici L., Faro L.L., Clerici E., Franceschini D., Baldaccini D., Badalamenti M., et al. Charlson comorbidity index and G8 in older old adult (≥80 years) hepatocellular carcinoma patients treated with stereotactic body radiotherapy. J. Geriatr. Oncol. 2021;12:1100–1103. doi: 10.1016/j.jgo.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Mima K., Hayashi H., Nakagawa S., Matsumoto T., Kinoshita S., Matsumura K., Kitamura F., Uemura N., Nakao Y., Itoyama R., et al. Frailty is associated with poor prognosis after resection for pancreatic cancer. Int. J. Clin. Oncol. 2021;26:1938–1946. doi: 10.1007/s10147-021-01983-z. [DOI] [PubMed] [Google Scholar]
- 24.Mogal H., Bs S.A.V., Dodson R., Hsu F.-C., Howerton R., Shen P., Clark C.J. Modified Frailty Index Predicts Morbidity and Mortality After Pancreaticoduodenectomy. Ann. Surg. Oncol. 2017;24:1714–1721. doi: 10.1245/s10434-016-5715-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngo-Huang A., Holmes H.M., Bordes J.K.A.D., Parker N.H., Fogelman D., Petzel M.Q.B., Song J., Bruera E., Katz M.H.G. Association between frailty syndrome and survival in patients with pancreatic adenocarcinoma. Cancer Med. 2019;8:2867–2876. doi: 10.1002/cam4.2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rieser C.J., Zenati M., Narayanan S., Bahary N., Lee K.K., Paniccia A., Bartlett D.L., Zureikat A.H. Optimal Management of Resectable Pancreatic Head Cancer in the Elderly Patient: Does Neoadjuvant Therapy Offer a Survival Benefit? Ann. Surg. Oncol. 2021;28:6264–6272. doi: 10.1245/s10434-021-09822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rittberg R., Zhang H., Lambert P., Kudlovich R., Kim C.A., Dawe D.E. Utility of the modified frailty index in predicting toxicity and cancer outcomes for older adults with advanced pancreatic cancer receiving first-line palliative chemotherapy. J. Geriatr. Oncol. 2020;12:112–117. doi: 10.1016/j.jgo.2020.07.004. [DOI] [PubMed] [Google Scholar]
- 28.van Wijk L., van der Snee L., Buis C.I., Hentzen J.E.K.R., Haveman M.E., Klaase J.M. A prospective cohort study evaluating screening and assessment of six modifiable risk factors in HPB cancer patients and compliance to recommended prehabilitation interventions. Perioper. Med. 2021;10:1–12. doi: 10.1186/s13741-020-00175-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamada S., Shimada M., Morine Y., Imura S., Ikemoto T., Saito Y., Miyazaki K., Tokunaga T., Nishi M. Significance of frailty in prognosis after surgery in patients with pancreatic ductal adenocarcinoma. World J. Surg. Oncol. 2021;19:1–8. doi: 10.1186/s12957-021-02205-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paolini C., Bencini L., Gabellini L., Urciuoli I., Pacciani S., Tribuzi A., Moraldi L., Calistri M., Coratti A. Robotic versus open pancreaticoduodenectomy: Is there any difference for frail patients? Surg. Oncol. 2021;37:101515. doi: 10.1016/j.suronc.2020.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Morley J.E., Vellas B., van Kan G.A., Anker S.D., Bauer J.M., Bernabei R., Cesari M., Chumlea W., Doehner W., Evans J., et al. Frailty Consensus: A Call to Action. J. Am. Med. Dir. Assoc. 2013;14:392–397. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corbi G., Cacciatore F., Komici K., Rengo G., Vitale D.F., Furgi G., Pagano G., Bencivenga L., Davinelli S., Ferrara N. Inter-relationships between Gender, Frailty and 10-Year Survival in Older Italian Adults: An observational longitudinal study. Sci. Rep. 2019;9:18416. doi: 10.1038/s41598-019-54897-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collard R.M., Boter H., Schoevers R.A., Voshaar R.O. Prevalence of Frailty in Community-Dwelling Older Persons: A Systematic Review. J. Am. Geriatr. Soc. 2012;60:1487–1492. doi: 10.1111/j.1532-5415.2012.04054.x. [DOI] [PubMed] [Google Scholar]
- 34.Marengoni A., Vetrano D.L., Manes-Gravina E., Bernabei R., Onder G., Palmer K. The Relationship between COPD and Frailty: A Systematic Review and Meta-Analysis of Observational Studies. Chest. 2018;154:21–40. doi: 10.1016/j.chest.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 35.Pandey A., Kitzman D., Whellan D.J., Duncan P.W., Mentz R.J., Pastva A.M., Nelson M.B., Upadhya B., Chen H., Reeves G.R. Frailty Among Older Decompensated Heart Failure Patients: Prevalence, Association With Patient-Centered Outcomes, and Efficient Detection Methods. JACC Heart Fail. 2019;7:1079–1088. doi: 10.1016/j.jchf.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laube R., Wang H., Park L., Heyman J.K., Vidot H., Majumdar A., Strasser S.I., Mccaughan G., Liu K. Frailty in advanced liver disease. Liver Int. 2018;38:2117–2128. doi: 10.1111/liv.13917. [DOI] [PubMed] [Google Scholar]
- 37.Pericleous M., Khan S.A. Epidemiology of HPB malignancy in the elderly. Eur. J. Surg. Oncol. 2021;47:503–513. doi: 10.1016/j.ejso.2020.03.222. [DOI] [PubMed] [Google Scholar]
- 38.Park J., Chen M., Colombo M., Roberts L., Schwartz M., Chen P.-J., Kudo M., Johnson P., Wagner S., Orsini L.S., et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: The BRIDGE Study. Liver Int. 2015;35:2155–2166. doi: 10.1111/liv.12818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bosetti C., Bertuccio P., Negri E., La Vecchia C., Zeegers M., Boffetta P. Pancreatic cancer: Overview of descriptive epidemiology. Mol. Carcinog. 2011;51:3–13. doi: 10.1002/mc.20785. [DOI] [PubMed] [Google Scholar]
- 40.Kojima G. Frailty as a Predictor of Nursing Home Placement Among Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. J. Geriatr. Phys. Ther. 2018;41:42–48. doi: 10.1519/JPT.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 41.Martínez-Velilla N., Herce P.A., Herrero C., Gutiérrez-Valencia M., de Asteasu M.L.S., Mateos A.S., Zubillaga A.C., Beroiz B.I., Jiménez A.G., Izquierdo M. Heterogeneity of Different Tools for Detecting the Prevalence of Frailty in Nursing Homes: Feasibility and Meaning of Different Approaches. J. Am. Med. Dir. Assoc. 2017;18:898.e1–898.e8. doi: 10.1016/j.jamda.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 42.Woo J., Leung J., Morley J.E. Comparison of Frailty Indicators Based on Clinical Phenotype and the Multiple Deficit Approach in Predicting Mortality and Physical Limitation. J. Am. Geriatr. Soc. 2012;60:1478–1486. doi: 10.1111/j.1532-5415.2012.04074.x. [DOI] [PubMed] [Google Scholar]
- 43.Eeles E.M.P., White S.V., O’Mahony S.M., Bayer A.J., Hubbard R.E. The impact of frailty and delirium on mortality in older inpatients. Age Ageing. 2012;41:412–416. doi: 10.1093/ageing/afs021. [DOI] [PubMed] [Google Scholar]
- 44.Balestroni G., Panzeri A., Omarini P., Cerutti P., Sacco D., Giordano A., Pistono M., Komici K., Ferrario S.R. Psychophysical health of elderly inpatients in cardiac rehabilitation: A retrospective cohort study. Eur. J. Phys. Rehabilit. Med. 2020;56:197–205. doi: 10.23736/S1973-9087.20.05970-5. [DOI] [PubMed] [Google Scholar]
- 45.Calise F., Giuliani A., Sodano L., Crolla E., Bianco P., Rocca A., Ceriello A. Segmentectomy: Is minimally invasive surgery going to change a liver dogma? Updates Surg. 2015;67:111–115. doi: 10.1007/s13304-015-0318-z. [DOI] [PubMed] [Google Scholar]
- 46.Rovesti G., Valoriani F., Rimini M., Bardasi C., Ballarin R., Di Benedetto F., Menozzi R., Dominici M., Spallanzani A. Clinical Implications of Malnutrition in the Management of Patients with Pancreatic Cancer: Introducing the Concept of the Nutritional Oncology Board. Nutrients. 2021;13:3522. doi: 10.3390/nu13103522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Simonsen C., de Heer P., Bjerre E.D., Suetta C., Hojman P., Pedersen B.K., Svendsen L.B., Christensen J.F. Sarcopenia and Postoperative Complication Risk in Gastrointestinal Surgical Oncology: A meta-analysis. Ann. Surg. 2018;268:58–69. doi: 10.1097/SLA.0000000000002679. [DOI] [PubMed] [Google Scholar]
- 48.Martin L., Birdsell L., MacDonald N., Reiman T., Clandinin M.T., McCargar L.J., Murphy R., Ghosh S., Sawyer M.B., Baracos V.E. Cancer Cachexia in the Age of Obesity: Skeletal Muscle Depletion Is a Powerful Prognostic Factor, Independent of Body Mass Index. J. Clin. Oncol. 2013;31:1539–1547. doi: 10.1200/JCO.2012.45.2722. [DOI] [PubMed] [Google Scholar]
- 49.Zhang G., Meng S., Li R., Ye J., Zhao L. Clinical significance of sarcopenia in the treatment of patients with primary hepatic malignancies, a systematic review and meta-analysis. Oncotarget. 2017;8:102474–102485. doi: 10.18632/oncotarget.19687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.EuroSurg Collaborative Body mass index and complications following major gastrointestinal surgery: A prospective, international cohort study and meta-analysis. Color. Dis. 2018;20:O215–O225. doi: 10.1111/codi.14292. [DOI] [PubMed] [Google Scholar]
- 51.Roderburg C., Wree A., Demir M., Schmelzle M., Tacke F. The role of the innate immune system in the development and treatment of hepatocellular carcinoma. Hepatic Oncol. 2020;7:HEP17. doi: 10.2217/hep-2019-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Padoan A., Plebani M., Basso D. Inflammation and Pancreatic Cancer: Focus on Metabolism, Cytokines, and Immunity. Int. J. Mol. Sci. 2019;20:676. doi: 10.3390/ijms20030676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Panzeri A., Komici K., Cerutti P., Sacco D., Pistono M., Ferrario S.R. Gender differences and long term outcome of over 75 elderlies in cardiac rehabilitation: Highlighting the role of psychological and physical factors through a secondary analysis of a cohort study. Eur. J. Phys. Rehabil. Med. 2021;57:288–297. doi: 10.23736/S1973-9087.21.06484-4. [DOI] [PubMed] [Google Scholar]
- 54.Souwer E.T., Moos S.I., van Rooden C.J., Bijlsma A.Y., Bastiaannet E., Steup W.H., Dekker J.W.T., Fiocco M., Bos F.V.D., Portielje J.E. Physical performance has a strong association with poor surgical outcome in older patients with colorectal cancer. Eur. J. Surg. Oncol. 2020;46:462–469. doi: 10.1016/j.ejso.2019.11.512. [DOI] [PubMed] [Google Scholar]
- 55.Rocca A., Brunese M., Cappuccio M., Scacchi A., Martucci G., Buondonno A., Perrotta F., Quarto G., Avella P., Amato B. Impact of Physical Activity on Disability Risk in Elderly Patients Hospitalized for Mild Acute Diverticulitis and Diverticular Bleeding Undergone Conservative Management. Medicina. 2021;57:360. doi: 10.3390/medicina57040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Virani S., Michaelson J.S., Hutter M.M., Lancaster R.T., Warshaw A.L., Henderson W.G., Khuri S.F., Tanabe K.K. Morbidity and Mortality after Liver Resection: Results of the Patient Safety in Surgery Study. J. Am. Coll. Surg. 2007;204:1284–1292. doi: 10.1016/j.jamcollsurg.2007.02.067. [DOI] [PubMed] [Google Scholar]
- 57.Kamiyama T., Nakanishi K., Yokoo H., Kamachi H., Tahara M., Yamashita K., Taniguchi M., Shimamura T., Matsushita M., Todo S. Perioperative Management of Hepatic Resection Toward Zero Mortality and Morbidity: Analysis of 793 Consecutive Cases in a Single Institution. J. Am. Coll. Surg. 2010;211:443–449. doi: 10.1016/j.jamcollsurg.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 58.Ceccarelli G., Costa G., De Rosa M., Pisanelli M.C., Frezza B., De Prizio M., Bravi I., Scacchi A., Gallo G., Amato B., et al. Minimally Invasive Approach to Gastric GISTs: Analysis of a Multicenter Robotic and Laparoscopic Experience with Literature Review. Cancers. 2021;13:4351. doi: 10.3390/cancers13174351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Malot C., Durand-Bouteau A., Barizien N., Bizard A., Kennel T., Fischler M., Minnella E., Le Guen M. Prehabilitation Program in Elderly Patients: A Prospective Cohort Study of Patients Followed Up Postoperatively for Up to 6 Months. J. Clin. Med. 2021;10:4500. doi: 10.3390/jcm10194500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ceccarelli G., Andolfi E., Biancafarina A., Rocca A., Amato M., Milone M., Scricciolo M., Frezza B., Miranda E., De Prizio M., et al. Robot-assisted surgery in elderly and very elderly population: Our experience in oncologic and general surgery with literature review. Aging Clin. Exp. Res. 2016;29:55–63. doi: 10.1007/s40520-016-0676-5. [DOI] [PubMed] [Google Scholar]
- 61.Giuliani A., Ceccarelli G., Rocca A. The role of laparoscopic distal pancreatectomy in elderly patients. Minerva Chir. 2018;73:179–187. doi: 10.23736/S0026-4733.18.07594-6. [DOI] [PubMed] [Google Scholar]
- 62.Montroni I., Rostoft S., Spinelli A., Van Leeuwen B.L., Ercolani G., Saur N.M., Jaklitsch M.T., Somasundar P.S., Carino N.D.L., Ghignone F., et al. GOSAFE—Geriatric Oncology Surgical Assessment and Functional rEcovery after Surgery: Early analysis on 977 patients. J. Geriatr. Oncol. 2019;11:244–255. doi: 10.1016/j.jgo.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 63.Martínez-Cecilia D., Cipriani F., Vishal S., Ratti F., Tranchart H., Barkhatov L., Tomassini F., Montalti R., Halls M., Troisi R.I., et al. Laparoscopic Versus Open Liver Resection for Colorectal Metastases in Elderly and Octogenarian Patients: A Multicenter Propensity Score Based Analysis of Short- and Long-term Outcomes. Ann. Surg. 2017;265:1192–1200. doi: 10.1097/SLA.0000000000002147. [DOI] [PubMed] [Google Scholar]
- 64.Loffredo D., Marvaso A., Ceraso S., Cinelli N.A., Rocca A., Vitale M., Rossi M., Genovese E.A., Amato B., Cinelli M. Minimal invasive surgery in treatment of liver metastases from colorectal carcinomas: Case studies and survival rates. BMC Surg. 2013;13:S45. doi: 10.1186/1471-2482-13-S2-S45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rocca A., Scacchi A., Cappuccio M., Avella P., Bugiantella W., De Rosa M., Costa G., Polistena A., Codacci-Pisanelli M., Amato B., et al. Robotic surgery for colorectal liver metastases resection: A systematic review. Int. J. Med. Robot. Comput. Assist. Surg. 2021;17:e2330. doi: 10.1002/rcs.2330. [DOI] [PubMed] [Google Scholar]
- 66.Rocca A., Cipriani F., Belli G., Berti S., Boggi U., Bottino V., Cillo U., Cescon M., Cimino M., Corcione F., et al. The Italian Consensus on minimally invasive simultaneous resections for synchronous liver metastasis and primary colorectal cancer: A Delphi methodology. Updat. Surg. 2021;73:1247–1265. doi: 10.1007/s13304-021-01100-9. [DOI] [PubMed] [Google Scholar]
- 67.Sena G., Picciariello A., Marino F., Goglia M., Rocca A., Meniconi R.L., Gallo G. One-Stage Total Laparoscopic Treatment for Colorectal Cancer with Synchronous Metastasis. Is It Safe and Feasible? Front. Surg. 2021;8:752135. doi: 10.3389/fsurg.2021.752135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data supporting the results of the study will be available on request.