Abstract
The venomous sting of honeybees causes a variety of medical problems. The severity and duration of a honeybee sting reaction can vary between patients and at different occasions in the same person. Clinical manifestations range from local and systemic allergic reactions to serious manifestations. The systemic manifestations include, among others, encephalitis, polyneuritis, bleeding manifestations, rhabdomyolysis and renal failure. Despite the high incidence of insect stings, very few reports of stroke have been described in the literature; however, serious complications should always be suspected. Here, we report the case of a previously healthy 13-year-old boy who presented to Wad Medani Children Hospital, Sudan, with an altered mental state and severe anaphylaxis, following numerous stings of honeybees. He also had intracranial haemorrhages, renal failure, petechial rash and shock.
Keywords: Honeybee stings, Anaphylaxis, Intracranial haemorrhage, Stroke, Coagulopathy, Child, Sudan
INTRODUCTION
Stings of honeybees and wasps of the Hymenoptera order are encountered on a daily basis throughout the world [1]. Bee venom by virtue of containing enzymes, biogenic amines, lipids and amino acids may cause local and systemic reactions and sudden deaths, largely resulting from renal failure secondary to extensive haemolysis and myolysis. Bee venom is composed of four major proteins: hyaluronidase, phospholipase A, melittin and apamin. Individuals who are honeybee-sensitive are also very sensitive to phospholipase A. The allergen named Apim6 causes strong IgE and T-cell reactions [1].
Although most stings cause only minor problems, high venom loads resulting from 450 stings or more to a victim during a single encounter can produce a toxic reaction, with potentially life-threatening complications [2]. Clinical manifestations range from local and systemic allergic reactions to serious manifestations. Infrequent mild complications, like vomiting, diarrhoea, dyspnoea, and generalised oedema, are also reported [3,4]. Neurological complications may include aphasia, dysarthria, seizures, ataxia, apraxia and coma [5]. Stroke due to hypotension produced by anaphylaxis may cause cerebral ischaemia. However, stroke after a massive attack of bees is a rare complication [6].
CASE REPORT
A 13-year-old boy without any past medical history for significant disease, particularly allergy, was admitted to our unit at Wad Medani Children Hospital with severe anaphylactic immense body angioedema, following multiple uncountable honeybee stings with hives on his head, face and limbs (Figure 1). His parents reported a fall from a tree without clear evidence of head injury or bleeding. On the same day, he developed diarrhoea and vomiting.
Figure 1.

Severe anaphylactic massive body angioedema, conjunctival chemosis and a dead insect’s part removed from the eye.
On admission to the intensive care unit, his blood pressure was 110/60 mmHg at the 50th percentile. He was deeply comatose with the Glasgow Coma Scale (GCS) <8, without lateralising signs or abnormal movement. The following day his condition was progressively worsening and he went into a deep coma and acute renal failure. Besides the severe orbital oedema, he developed conjunctivitis with conjunctival chemosis, pus and bloody discharges. On examination, there was a pseudo-membrane and corneal ulcers with an imbedded dead insect’s part (Figure 1). He developed purpuric skin lesions on both the upper and lower limbs (Figure 2).
Figure 2.

Purpuric skin lesions on the upper (A) and lower limbs (B).
The child developed acute renal injury with impaired renal functions. Urinalysis showed traces of albumin and sugar with microscopic haematuria. Renal function tests (RFTs) initially showed blood urea nitrogen (BUN) of 222 mg/dl (reference range [RR] = 7-20 mg/dl) with serum creatinine of 5.8 mg/dl (RR= 0.7-1.2 mg/dl). Electrolytes were as follow: serum Na 124 mEq/l (RR = 135-145 mEq/l) and serum potassium 7.5 mEq/l (RR = 3.5-5.0 mEq/l). He developed oliguria with urine output less than 100 ml over 24 hours. Muscle creatine kinase (CK) enzyme was also elevated to 398 U/l (RR = 38-174 U/l), suggesting muscle injury (rhabdomyolysis). All these tests worsened over the following few days, necessitating sessions of haemodialysis at Wad Medani Nephrology Hospital. Coagulation tests on initial work up were prothrombin time (PT) of 14.2 seconds (RR = 12.7-16.1 seconds) and the activated partial thromboplastin time of 33 seconds (RR = 30-40 seconds). The platelet count was 114 × 103/l (RR = 150-450 × 103/l) and white blood cell count was 27.4 × 109/l (RR = 4.5-11.0 × 109/l), mainly neutrophils (58%) and haemoglobin level was 13.1 g/dl (RR= 12.7-17.7 g/dl).
The child’s condition improved following the dialysis sessions. His GCS rose to 12 and he became fully conscious after the fourth session. His urine output increased to 150 ml/day and then returned to normal. Reinvestigations thereafter were as follow: BUN = 103 mg/dl (RR = 7-20 mg/dl), serum creatinine dropped to 2.4 mg/dl (RR = 0.7-1.2 mg/dl), serum sodium increased to 133 mEq/l (RR = 135-145 mEq/l) and serum potassium dropped to 4 mEq/L (RR = 3.5-5.0 mEq/l). Cranial computed tomography (CT) scan (Figure 3) revealed multiple areas of intracerebral haemorrhage mainly on the left hemisphere involving the anterior and posterior centrum semiovale and occipital lobe, associated with multiple bifrontal acute haemorrhage. Haemorrhage was also seen on the left cerebellar hemisphere (Figure 3B). No skull or cervical vertebral fractures were detected.
Figure 3.
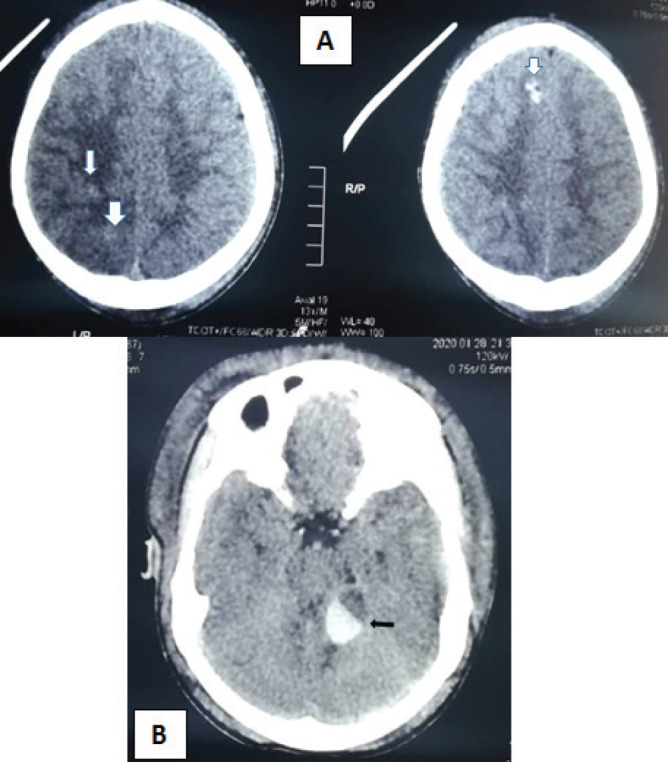
Cranial CT scan revealing (A) multiple areas of intracerebral haemorrhage (arrows). (B) Haemorrhage was also seen in the left cerebellar hemisphere (arrow).
Three months later after frequent follow-up visits to the clinic, his neurological examination was unremarkable with no residual complications. His renal functions returned to normal with clear urine. RFTs showed BUN of 23 mg/dl (RR = 7-20 mg/dl) with serum creatinine of 1.5 mg/dl (RR = 0.7-1.2 mg/dl). The electrolytes were serum sodium of 141 mEq/l (RR = 135-145 mEq/l) and serum potassium of 3.0 mEq/l (RR= 3.5-5.0 mEq/l). His last CK level dropped to 88 U/l (RR = 38-174 U/l).
Management
As an emergency, the child was treated with intravenous antihistamine (chlorpheniramine hydrogen maleate), subcutaneous adrenaline to reduce the allergic response and intravenous methylprednisolone (30 mg/kg daily for 3 days).
For acute renal failure, the child was treated for hyperkalaemia with intravenous (IV) calcium gluconate and salbutamol inhaler without a remarkable effect. He was then started on a total of five haemodialysis sessions. The sessions ran as three consecutive daily sessions for 3 days. They lasted 2, 3 and 4 hours, respectively. The last two sessions were given every other day, each lasting for 4 hours. The dialysate constituted a 500-ml ultra-filtrate heparin free blood (due to the haemorrhagic insults) at a flow rate of 150 ml/hour.
He was followed closely by an ophthalmologist. The conjunctivitis, pseudo-membrane and corneal ulcers were treated with topical antibiotic eye drops; including Optiflox eye drops, Fucithalmic eye ointment and acyclovir eye ointment. Few days later, the oedema subsided and the fundus was normal on the right eye, whereas the left eye showed a hazy view because of an ulcer, which hindered the fundal examination. On follow-up 3 months later, the child had fully recovered.
DISCUSSION
Anaphylactic shock is the most prominent immediate risk following bee stings. A toxic reaction can follow massive envenomation that is directly related to the dose. Anaphylaxis manifestations are variable and include difficulty breathing such as wheezing, facial swelling, gastrointestinal disturbances, cramps and itchy rash elsewhere. A small percentage of people who are stung by bees or other insects quickly develop anaphylaxis, a severe allergic reaction to honeybee stings. This is hypothetically considered to be life-threatening and requires emergency action. Following a second attack, people who have anaphylaxis to a bee sting have a 25%-65% chance of a severe allergic reaction. Immunotherapy (“allergy shots”) has to be considered as one of the prevention measures [7]. The uncomplicated stings which subside within few hours mainly cause pain, erythema, pallor, urticarial rash, numbness, tingling, sweating and weakness. Our patient presented with almost all these features suggesting the emergency situation on admission. Some anaphylaxis manifestations prove to result in significant morbidity and mortality [8]. Insect saliva, excretions or secretions and body parts can cause hypersensitivity and systemic responses in some people. In this case, a dead insect’s part was removed from the child’s eye (Figure 1).Variable neurological complications due to bee stings were reported including dizziness or fainting, loss of consciousness, seizures, ataxia, apraxia, aphasia, dysarthria and coma secondary to haemorrhagic infarcts [8,9]. These neurologic manifestations, mainly haemorrhagic stroke, are extremely rare following bee venom poisoning [2,10]. In this case, the patient had multiple haemorrhagic strokes. After regaining his conscious, he was able to speak very well with good speech articulation.
The pathophysiology explaining stroke due to honeybee sting is still unknown. Theories include venom vasoactive and inflammatory mediators causing vasoconstriction and cerebral ischaemia. Disseminated intravascular coagulation due to tissue damage results in the release of tissue thromboplastins secondary to exposure of the blood to the phospholipids from damaged tissues leading to vessel occlusion due to widespread fibrin thrombi deposition [11]. Hymenoptera svenom contains an enzyme that can splits phospholipids causing significant coagulation abnormalities [12]. Similarly it contains a variety of amines, peptides and enzymes that cause various clinical manifestations. A polypeptide toxin (mellitin) causes the direct toxic effects and damages cell membranes and hyaluronidase, phospholipase enzymes and other compounds such as histamine, serotonin, thromboxane and leukotrienes. Vasoactive and inflammatory mediators, principally thromboxane and leukotrienes, have been shown to cause vasoconstriction; resulting in cerebral infarction [13]. Endothelial damage and haemolysis cause vessel occlusion due to widespread fibrin thrombi deposition [14-16].
Rhabdomyolysis is a serious complication following bee venom which may cause acute renal failure. This may be the case in our patient who had increased CK levels. Another explanation is the direct nephrotoxic action and renal ischemia due to bee venom [3]. In addition, a neuropharmacological factor mainly sympathetic mechanism of endothelial permeability with a concurrent systemic thrombogenic or immune response has also been postulated [14].
Various therapeutic interventions if started early after diagnosis reduces the expected complications. Treatment strategies must include rapid recognition and collaboration with experienced clinicians to facilitate specialised treatment protocols. Diagnosing the early phases of a systemic allergic reaction preceding anaphylactic shock is of paramount importance in managing any patient in whom insect exposure is suspected. Severe anaphylaxis can be fatal in as little as 10 minutes.
Epinephrine is the drug of choice for shock, angioedema, airway obstruction, bronchospasm and urticaria in severe anaphylactic reactions. It relaxes the blood vessels and muscles, helping the body to deal with the reaction while emergency medical help is required. Epinephrine can be administered using different routes, e.g., intramuscular and IV. Continuous infusion may be given in cases of refractory shock. A ‘bee sting kit’ containing an EpiPen and an epinephrine shot has been used. This is recommended to be adopted in Sudan particularly for those who are frequently exposed to bees or other venomous wasps. Prednisone is believed to ameliorate delayed effects of anaphylactic reactions and may limit biphasic anaphylaxis. Methylprednisolone is useful for treating inflammatory and allergic reactions [10].
Further studies are needed to reveal the pathophysiology involved and to prevent organ damage, as there is no complete cure for stroke. As central nervous system involvement is known to have a delayed onset, it is important to anticipate and treat these patients to avoid a fatal outcome. To ensure that practitioners are competent enough in treating anaphylactic reactions, continuous training and provision of the risk medications are highly recommended at primary healthcare levels in Sudan. We plan to follow-up this boy for a longer time, for possible expected complications such as nephrotic syndrome and other immune-mediated complications.
Acknowledgements
The authors would like to thank the parents for their patience, understanding and agreement to publish this case. Acknowledgements are also extended to the teams from the nephrology and ophthalmology hospitals for their indispensable help.
Conflicts of interest
The authors declare no conflicts of interest.
Funding
None.
Ethical approval
Ethical clearance was obtained from the ethics committees of the University of Gezira and Gezira State Ministry of Health. Informed consent for participation and publication of medical details were obtained from the parents of the child.
REFERENCES
- 1.Kozak HH, Uca AU, Altaş M, Elbeyli AB. Subarachnoid hemorrhage occurring after bee sting (Letter to the Editor) Science Direct. 2016;50:139–40. doi: 10.1016/j.pjnns.2016.01.005. https://doi.org/10.1016/j.pjnns.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Murat G, Handan A, Ali KE, Baydin A, Kayabas A. Acute ischemic stroke and severe multiorgan dysfunction due to multiple bee stings. Turk J Emerg Med. 2016;16(3):126–8. doi: 10.1016/j.tjem.2015.02.002. https://doi.org/10.1016/j.tjem.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Temizoz O, Celik Y, Asil T, Balci K, Unlu E, Yilmaz A. Stroke due to bee sting. Neurologist. 2009;15(1):42–3. doi: 10.1097/NRL.0b013e31818c7251. https://doi.org/10.1097/NRL.0b013e31818c7251. [DOI] [PubMed] [Google Scholar]
- 4.Michael L S. Honey bee sting pain index by body location. PeerJ. 2014;2:1–15. doi: 10.7717/peerj.338. https://doi.org/10.7717/peerj.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahale R, Mehta A, Shankar AK, Buddaraju K, John AA, Javali M, et al. Isolated posterior circulation stroke following honey-bee sting. Neurol India. 2016;64(7):116–8. doi: 10.4103/0028-3886.178053. https://doi.org/10.4103/0028-3886.178053. [DOI] [PubMed] [Google Scholar]
- 6.Stack K, Pryor L. Significant traumatic intracranial hemorrhage in the setting of massive bee venom-induced coagulopathy: a case report. Wilderness Environ Med. 2016;27(3):405–8. doi: 10.1016/j.wem.2016.05.005. https://doi.org/10.1016/j.wem.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 7.Rosen P, Marx JA, Hockberger RS, Walls RM, Adams J. Philadelphia, PA: Elsevier/Saunders; 2014. Rosen’s emergency medicine: concepts and clinical practice. [Google Scholar]
- 8.Aleman RM, Martinez MG, Herrera H, Herrera HP. Floor of the nose mucosa lysis and labial abscess caused by a bee sting. Braz Dent J. 2009;20(3):249–53. doi: 10.1590/s0103-64402009000300014. https://doi.org/10.1590/S0103-64402009000300014. [DOI] [PubMed] [Google Scholar]
- 9.Yoder J, Lloyd A, Tilney PV, McKenna DP. Intracerebral hemorrhage following multiple bee stings. JAAPA. 2013;26(7):1. doi: 10.1097/01.JAA.0000431513.20819.4b. https://doi.org/10.1097/01.JAA.0000431513.20819.4b. [DOI] [PubMed] [Google Scholar]
- 10.Mahale R, Mehta A, Shankar AK, Buddaraju K, John AA, Javali M, et al. Isolated posterior circulation stroke following honey-bee sting. Neurol India. 2016;64(7):1–4. doi: 10.4103/0028-3886.178053. https://doi.org/10.4103/0028-3886.178053. [DOI] [PubMed] [Google Scholar]
- 11.Wani M, Saleem S, Verma S, Yousuf I, Wani M, Asimi R, et al. Multiple cerebral infarctions with severe multi-organ dysfunction following multiple wasp stings. Ann Indian Acad Neurol. 2014;17(1):125–7. doi: 10.4103/0972-2327.128581. https://doi.org/10.4103/0972-2327.128581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bilir O, Ersunan G, Kalkan A, Ozmen T, Yigit Y. A different reason for cerebrovascular disease. Am J Emerg Med. 2013;31(5):5–6. doi: 10.1016/j.ajem.2012.12.040. https://doi.org/10.1016/j.ajem.2012.12.040. [DOI] [PubMed] [Google Scholar]
- 13.Jain J, Banait S, Srivastava AK, Lodhe R. Stroke intracerebral multiple infarcts: Rare neurological presentation of honey bee bite. Ann Indian Acad Neurol. 2012;15(2):163–6. doi: 10.4103/0972-2327.95008. https://doi.org/10.4103/0972-2327.95008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Narang SK, Paleti S, Azeez Asad MA, Samina T. Acute ischemic infarct in the middle cerebral artery territory following a Russell’s viper bite. Neurol India. 2009;57(4):479–80. doi: 10.4103/0028-3886.55594. https://doi.org/10.4103/0028-3886.55594. [DOI] [PubMed] [Google Scholar]


