Abstract
Fever is a natural and almost universal mammalian response to infection. There exists a fear amongst general public and healthcare providers regarding fever being harmful leading to its overzealous management with antipyretics. Although the National Institute for Health and Care Excellence (NICE) guidelines suggest the use of single antipyretic agent for management of fever, combination therapy with paracetamol, and ibuprofen is common in paediatric practice in the United Kingdom. These antipyretics at times can cause significant adverse events even when administered at regular therapeutic doses.
We describe a young boy who presented with significant hypothermia (34.1°C) and was initially treated as cold sepsis. Once the boy got warmed up and as blood results became subsequently available, it became clearer that the hypothermia was secondary to therapeutic doses of antipyretics. In conclusion, we hope to improve awareness regarding this condition in clinical practice and educate health care professionals and caregivers with recommended NICE guidelines.
Keywords: Fever, hypothermia, antipyretics, therapeutic doses, sepsis
INTRODUCTION
Fever is defined as ‘an elevation of body temperature above the normal daily variation’ (NICE) [1]. It is a natural and almost universal mammalian response to infection but is one of the commonest reasons for parents to seek medical care for children. A fear of raised body temperature exists amongst the general public and healthcare providers alike [2]; this stem largely from the connection with febrile convulsions, and the historical observation that fever was often associated with serious infectious illnesses and hence the belief that it should be treated as a pathological entity in itself. The National Institute for Health and Care Excellence (NICE) (2017) guidelines recommend the use of a single antipyretic for treating febrile children but advises against using combination therapy simultaneously though suggests consideration for using alternating antipyretic agents if distress persists [1]. Healthcare professionals often prescribe combination antipyretic therapy for treating fever despite the contradictive scientific evidence of the benefit of elevated temperature in the presence of infection [2,3]. A hospital-based study in the United Kingdom involving 53 children aged 0-17 years who had febrile illnesses showed that 29/53 (55%) had been prescribed both paracetamol and ibuprofen on their drug chart and 17/53 (32%) had been administered both the drugs together [3].
This paper describes a case of hypothermia in a young boy that was caused by therapeutic doses of combination antipyretic therapy and resulted in a diagnostic dilemma that was initially managed as cold sepsis.
CASE REPORT
A previously fit and healthy 2-year-old boy attended the emergency department brought by ambulance. His parents had found him difficult to rouse; his temperature was 34.1°C using an Avent digital ear thermometer.
He had a 4-day history of coryzal symptoms with cough and pyrexia up to 40°C. Parents had measured his temperature at 30 minutes intervals prior to admission. He had not been reviewed by his general practitioner but parents had been advised by the triage nurse practitioner based in the primary care that a viral illness was likely and to administer children’s paracetamol and ibuprofen solutions according to the manufacturers’ instructions.
Initial observations in the Emergency Department were: heart rate 158/minute, respiratory rate 21/minute, saturations 98% in air and temperature of 35.2°C. Clinical examination was unremarkable. In view of the unexplained hypothermia, a provisional diagnosis of cold sepsis was made and blood tests including blood cultures were sent. Blood gas analysis showed normal parameters; lactate was 1.6 mmol/l. Intravenous ceftriaxone at 50 mg/kg once daily was started and he was admitted for close monitoring.
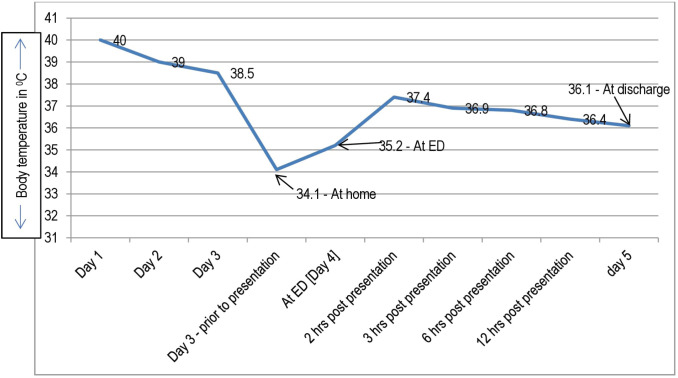
His clinical condition gradually improved once he had rewarmed to a temperature of 36.8°C. Observations remained within normal limits and no further doses of antipyretics were given. Figure 1 shows the temperature recorded during the illness. Blood investigations were unremarkable (C-reactive protein 9 mg/l, white cell count 9 × 109/l). The ceftriaxone was stopped after the second dose following a negative blood culture result.
Figure 1.
Temperature recorded during the course of the illness
The review of the history revealed that parents had called for an ambulance as the child had not been improving, felt cold to touch, and was difficult to rouse. They had continued to administer regular doses of combination of antipyretics (100 mg of ibuprofen 8 hourly and paracetamol 120 mg 6 hourly) in accordance with advice received from the primary care, and following the manufacturers’ dosage guidance on the bottles. In view of the history, normal clinical findings, normal blood tests and a negative blood culture result, the most likely diagnosis was hypothermia induced by regular therapeutic doses of (combination) antipyretics.
DISCUSSION
This case highlights the need to consider administration of regular antipyretic therapy as a possible cause for hypothermia in an otherwise well child; even when the correct recommended dose of medication has been given. Identifying the association between regular antipyretic dosing and presenting hypothermia in this case prevented further unnecessary interventions.
Little is known on the mechanism of toxicity regarding the association between antipyretics and hypothermia. Van Tittelboom et al. [4] postulated that in some children for reasons yet unknown, a temporary state of increased sensitivity to therapeutic doses of paracetamol results in an abnormal formation of endogenous antipyretics. Richardson et al. [5] suggested that combination antipyretic therapy may have a ‘summative effect’ leading to hypothermia.
Regardless of mechanism, the association of hypothermia with antipyretic use is being increasingly reported in young children and can lead to false positive diagnostic conundrums and needless invasive investigations and medication. Table 1 highlights relevant paediatric literature reporting hypothermia induced by therapeutic doses of antipyretics.
Table 1.
Literature review of cases of hypothermia induced by therapeutic doses of antipyretics.
| Name of author and year of publication | Drug used | Number of cases | Age | Lowest temperature recorded | Outcome |
|---|---|---|---|---|---|
| Van Tittelboom and Govaerts-Lepicard [4] | Paracetamol | 4 | 4.5 years | All presented with temperature of 35°C | All survived |
| 21 months | |||||
| 4 months | |||||
| 3 months | |||||
| Desai and Sriskandan [6] | Ibuprofen | 1 | 7 years | 33.5°C | Survived |
| Richardson and Sills [5] | Paracetamol and ibuprofen | 1 | 15 months | 33.6°C | Survived |
| Paul & Whibley, [7] | Paracetamol | 1 | 15 months | 35°C | Survived |
| Lo, et al., [8] | Ibuprofen | 1 | 3.3 years | 34°C | Survived |
| Current case | Paracetamol and ibuprofen | 1 | 2 years | 34.1°C | Survived |
A large Italian study by using two databases (Rete Nazionale di Farmacovigilanza & VigiBase), 3,386 reports of adverse drug reactions due to ibuprofen were retrieved and 26% (n = 886) were children [9]. One hundred and fifteen cases of hypothermia were reported of which 56 were children; suspected drugs were ibuprofen (n = 19) paracetamol (n = 13), and 3 children had received combination therapy [9]. The same paper also highlights the physiological and anatomical differences that make the paediatric population at greater risk for hypothermia [9].
CONCLUSION
Fever is a natural, and presumably physiologically beneficial response to infection, though antipyretics are often prescribed with the intention to reduce body temperature, rather than alleviating distress. The use of combination antipyretic therapy in therapeutic doses in this case highlights the possibility of causing hypothermia in young patients. Raising awareness amongst health care professionals and caregivers to exercise restraint in the use of antipyretics as recommended by the NICE guideline is suggested. We hope this case report heightens the awareness of this rare but unusual side-effect of very common medications amongst new paediatricians and other health professionals looking after children and to exercise caution while providing advice regarding regular use of antipyretics.
ACKNOWLEDGEMENTS
The authors would like to thank the parents for providing consent to publish the case of their child.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
FUNDING
None available for this case study.
ETHICAL APPROVAL
Signed informed consent for participation and publication of medical details was obtained from the parents of this child. Confidentiality of patient’s data was ensured at all stages. The authors declare that ethics committee approval was not required for this case report.
REFERENCES
- 1.National Institute for Health and Care Excellence Guidelines Updates Team. London, UK: NICE; 2019. [2020 Sep 17]. Fever in under 5s: assessment and initial management. NICE guideline [NG143] Available from: https://www.nice.org.uk/guidance/ng143. [PubMed] [Google Scholar]
- 2.Clericetti CM, Milani GP, Bianchetti MG, Simonetti GD, Fossali EF, Balestra AM, et al. Systematic review finds that fever phobia is a worldwide issue among caregivers and healthcare providers. Acta Paediatr. 2019;108:1393–7. doi: 10.1111/apa.14739. https://doi.org/10.1111/apa.14739. [DOI] [PubMed] [Google Scholar]
- 3.Banks T, Paul SP, Wall M. Managing fever in children with a single antipyretic. Nurs Times. 2013;109:24–5. [PubMed] [Google Scholar]
- 4.Van Tittelboom T, Govaerts-Lepicard M. Hypothermia: an unusual side effect of paracetamol. Vet Hum Toxicol. 1989;31:575–9. [PubMed] [Google Scholar]
- 5.Richardson J, Sills J. Hypothermia following fever. Arch Dis Child. 2004;89:1177. doi: 10.1136/adc.2004.055376. https://doi.org/10.1136/adc.2004.055376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Desai PR, Sriskandan S. Hypothermia in a child secondary to ibuprofen. Arch Dis Child. 2003;88:87–8. doi: 10.1136/adc.88.1.87-a. https://doi.org/10.1136/adc.88.1.87-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paul SP, Whibley J. Paracetamol may cause hypothermia in children. Nurse Prescribing. 2010;8:519. https://doi.org/10.12968/npre.2010.8.11.79784. [Google Scholar]
- 8.Lo M, Yan L, Marques JS. Unexpected hypothermia following ibuprofen. BAOJ Pediatr. 2016;2:007. [Google Scholar]
- 9.Donati M, Monaco L, Melis M, Sottosanti L, Biagi C, Vaccheri A, et al. Ibuprofen-associated hypothermia in children: analysis of the Italian spontaneous reporting database. Eur J Clin Pharmacol. 2016;72:1239–43. doi: 10.1007/s00228-016-2088-z. https://doi.org/10.1007/s00228-016-2088-z. [DOI] [PubMed] [Google Scholar]