Abstract
This study aimed to analyze the dietary patterns of adolescent students during the COVID-19 pandemic lockdown. To achieve the research´s aim 127 adolescent students, 60 men (18.88±4.18 years) and 67 women (17.61±7.43 years) completed an online questionnaire that analyzed variables regarding their nutritional profile. Adolescent students presented a dietary pattern during the COVID-19 pandemic lockdown characterized by different associations of food consumption, On one hand, the consumption of healthier foods such as meat, fish, vegetables, legumes, rice, or pasta, and on the other hand non-healthier foods as food, alcohol, or pastries. Further investigations are needed to implement multidisciplinary interventions to develop healthier habits in schools and to encourage the adoption of healthy diets among adolescents.
Keywords: Nutrition, Covid-19, Students, Lockdown, Questionnaire, Dietary patterns
1. Introduction
In December 2019 a new coronavirus (SARS-Cov2) emerged in Wuhan, China, spreading a pandemic of acute respiratory syndrome in humans (COVID-19). This pathology has infected and killed thousands of people throughout the world [1], generating a global health and economic crisis. Since this emergence, governments around the world have taken extraordinary actions to respond and contain the virus. One of the containment measures was the total confinement of the population in their homes, also known as lockdown. This led to the disruption of most daily activities, separation from loved ones, and the loss of freedom. Many companies were forced to implement teleworking quickly so that their employees could continue to carry out their duties from home. In consequence, although most people are not expected to suffer mental disorders, a significant percentage of the population has experienced intense emotional adjustment reactions [2]. In addition, it has been demonstrated that the death of relatives and increased social adversity, may lead to psychological adverse effects, increasing the risk of emotional disturbance, depression, low mood, irritability, insomnia, and post-traumatic stress symptoms [3]. In general, authors emphasize that the COVID-19 pandemic has impacted the mental health of citizens worldwide, leading to “psychological distress” [4]
This critical situation and confinement changed lifestyle, especially diet and physical activity patterns. In Spain, it has been reported that the diet conducted during the lockdown had a larger energy intake and lower nutritional quality than the pre-COVID-19 eating patterns [5]. As isolation is often perceived as a stressful situation [6], this increase in energy ingestion and the craving for comfort food could be due to boredom and stress [7]. It is known how in times of uncertainty people are most vulnerable to different groups of mental disorders that may constitute comorbid disorders [8]. The threatening context, uncertainty, and low predictability of this pandemic situation along with the protective measures to prevent the transmission of the COVID-19, potentially affect the well-being of different age groups [9]. Particularly in adolescence, a period where human encompasses elements of biological growth and major social role transitions, it has been reported that psychological health problems, especially emotional disorders, are common during stressful events as pandemic circumstances [10]. In this line, there is a connection between negative emotions as boredom and stress promoted during the lockdown and unhealthy eating habits to draw attention away [11,12]. Additionally, it has been demonstrated that anxiety and fear of COVID-19 were associated with higher body shape and weight concerns [13]. Concerning this, studies highlight the fact that mood disorders likely influence both hedonic and homeostatic aspects of food intake, making a clear definition of food addiction difficult [14]. Food addiction is evoked by the taste and consumption of palatable foods which activate the brain's reward system leading to compulsive overeating [15]. Therefore, stressful situations and exposure to a traumatic event seem to be associated with alcohol dependence [16] and a greater preference for energy- and nutrient-dense foods, namely those that are high in sugar and fat [17].
Regarding alcohol consumption, in Europe students and workers have declared that they consumed more alcohol during the lockdown [18,19]. Furthermore, in line with our study, previous authors showed that the mean age of initiation to alcohol use was 15.1 years [20,21]. In fact, during out-of-lockdown, drinking was the leading cause of incident disability-adjusted life years for people aged 10 to 24 years [22], thus, our results could indicate the same trend. For these reasons, further research is needed to provide recommendations regarding appropriate lifestyle habits in post-COVID-19 times.
In this line, adolescents showed the unhealthiest diet of all age groups [23,24]. The prolonged stay at home with often unlimited food access provokes more disruptive eating behaviors, including food consumption without hunger feeling and as we mentioned before, frequent overeating [25]. Thus, BMI was increased and it was associated with less frequent consumption of vegetables, fruit, and legumes during quarantine, and higher adherence to meat, dairy, and fast-foods [26] However, in Italy, Spain, Chile, Colombia, and Brazil the lockdown also increased the possibility of cooking at home and the number of adolescents who consume the recommended weekly servings of legumes and fruits during confinement increased by 8% and 7.7%, respectively, in comparison to before confinement moment [27]. Studies suggested that Mediterranean Diet adherence slightly increases during confinement, although consumption of 'unhealthy' food also increases [28]. Moreover, the number of subjects that practice physical activity, as well as the time spent on it weekly, decreases [28]. The lockdown and the inability of people to do any physical activity made the situation worse, resulting in developing diseases such as obesity, diabetes, cardiovascular disease, and cancer, and these diseases are mortality risk factors for COVID-19 [28].. In this varying context, educational institutions may try to implement multidisciplinary strategies to face stressful situations without losing healthy habits. Then, the objective of the present research was to analyze the dietary patterns of adolescent students during the COVID-19 pandemic lockdown.
2. Material and methods
2.1. Participants
We studied 127 high school students. Among them, 60 were men (18.88±4.18 years) and the rest of them were women (17.61±7.43 years). They were interviewed via an online questionnaire in a period of 3 months, from October 2020 to December 2020. Our inclusion criteria were: Enrolment in the current academic year and currently living in Spain to prevent double responses from the same person, students had to include their Student ID, their school´s name, and the name of their class. Furthermore, data were considered strictly confidential. This research complied with the Helsinki declarations (revised in Brazil,2013), on human research and was approved by the University Ethics Committee (CIPI/18/074). All the participants digitally signed a consented participation where the aims and procedure of the study was explained.
2.2. Design and procedure
The week before data collection, researchers visited each school to introduce themselves to the adolescents and to familiarize them with every procedure. The call to participate in the study was made through a link sent by researchers.
Students were interviewed via an online questionnaire in the first trimester of their academic year. Due to social isolation measures adopted by citizens who have contact with confirmed COVID-19 cases, these questionnaires could be answered at home or school. To reach the aim of the present research, a cross-sectional study was developed.
2.3. Measures
To achieve the research aims students completed a nutrition questionnaire. Students completed it by an online service, at one time, in their homes or school, in lecture time (09:00 to 14:00) using their personal computers or devices. The questionnaire was the following.
Nutritional habits were analyzed using an adapted previously used questionnaire. It includes the following 23 items which were related to the consumption frequency per week of different food groups:
-
1
Fruit juices and nectars (250 ml)
-
2
Alcohol (Whiskey, rum, gin…) (50 ml approx.)
-
3
Beer (250 ml approx.)
-
4
Wine (50 ml approx.)
-
5
Soft drinks (coke, soda…) (250 ml approx.)
-
6
Energy drinks (250 ml approx)
-
7
Milk (250 ml approx.)
-
8
Fermented products (125 gr)
-
9
Pastries (1 portion)
-
10
Cheese (50 gr)
-
11
Eggs (1 piece)
-
12
Meat (150 gr)
-
13
Fish (150 gr)
-
14
Sausage/cold meat (150 gr)
-
15
Legumes (200 gr)
-
16
Rice (150 gr)
-
17
Pasta (150 gr)
-
18
Fruit (1 portion)
-
19
Raw vegetables (salad) (200 gr approx.)
-
20
Cooked vegetables (200 gr approx.)
-
21
Bread (50 gr approx.)
-
22
Whole-grain cereal (bread, rice, oat…)
-
23
Fast food (1 serving)
Each item was ranged from 1 to 6, where 1= “I do not consume”, 2= “less than three times per week”,3=“three times or more per week”, 4= “seven or more times per week”, 5“ten or more times per week”,6=“more than thirteen times”
2.4. Statistical analysis
Statistical analyses were analyzed using the Statistical Package for the Social Sciences (SPSS) version 24.0 (SPSS Inc., Chicago, IL., USA). Descriptive statistics (mean and standard deviation) were calculated for each variable. Kolmogorov–Smirnov tests were performed to analyze the normality and homogeneity of each variable. A bivariate correlational analysis was conducted with the Pearson test. The level of significance for all the comparisons was set at p ≤ 0.05.
3. Results
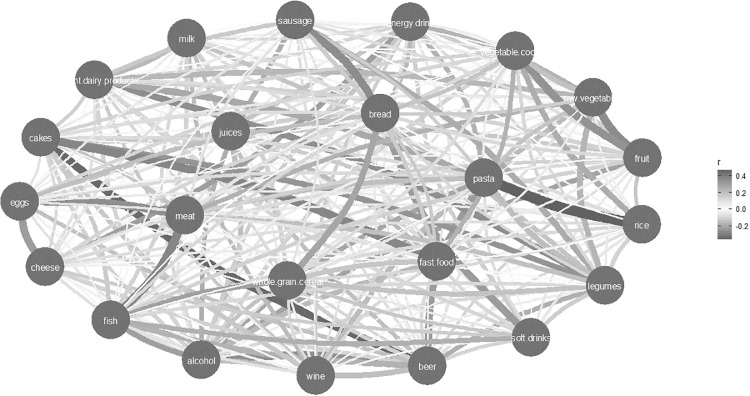
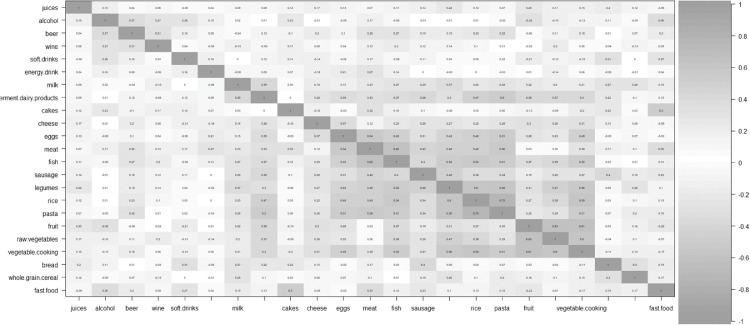
This study presented two well-defined profiles of nutrition patterns. All positive significant correlations are included in (Fig. 1 ) and (Fig. 2 ). Results are also presented as mean± standard deviation (Table 1 ), it presents students’ responses to the frequency of consumption of preferred food types. Results indicate that the majority of students reported high consumption of milk, bread, and fruit (three or more than three times per week). Furthermore, wine, beer, and alcohol consumption presents the lowest values (less than two times per week).
Fig. 1.
Correlation diagram analysis between food patterns.
Fig. 2.
Correlation analysis between food patterns.
Table 1.
Food intake frequencies to compare dietary patterns during COVID-19 confinement.
| Food items | Mean±SD |
|---|---|
| Juices | 2.2 ± 1.1 |
| Alcohol | 1.2 ± 0.4 |
| Beer | 1.2 ± 0.6 |
| Wine | 1 ± 0.2 |
| Soft drinks | 2.1 ± 1.1 |
| Energy drink | 1.3 ± 0.7 |
| Milk | 3.4 ± 1.4 |
| Fermented products | 2.8 ± 1.1 |
| Cakes/pastries | 2.3 ± 1 |
| Cheese | 2.4 ± 1.1 |
| Eggs | 2.5 ± 0.8 |
| Meat | 2.9 ± 1.1 |
| Fish | 2.3 ± 0.9 |
| Sausages | 2.7 ± 1.1 |
| Legumes | 2.4 ± 0.8 |
| Rice | 2.3 ± 0.8 |
| Pasta | 2.4 ± 0.8 |
| Fruit | 3 ± 1.2 |
| Raw vegetable | 2.4 ± 1.1 |
| Cooked vegetables | 2.5 ± 1.2 |
| Bread | 3.2 ± 1.3 |
| Whole-grain cereal | 2.4 ± 1.2 |
| Fast food | 1.9 ± 0.7 |
According to the healthiest nutritional profile promoted (Fig. 1), significant correlation was found between healthy food as milk and legumes (r:0.36, p:0.007) fermented milk and different types of food as fish (r:0.35, p:0.012), sausages (r:0.40, p:0.001), rice (r:0.39,p:0.002), pasta(r:0.49,p:0.001), fruit (r:0.33,p:0.048) or cooked vegetables (r:0.39,p:0.002). Additionally, a higher eggs consumption was found when students showed a higher consumption of meat (r:0.39, p:0.002), fish (r:0.42, p: 0,001) legume (r:0.39, p:0.002), rice (r:0.53, p:0.001), pasta (r:0.046, p:0.001) or cooked vegetables (r:0.45, p:0.001). Moreover, results revealed also a healthy profile in adolescents by finding a significant correlation between meat consumption and some foods as fish (r:0.049, p:0.001), sausages (r:0.37, p:0.005), legumes (r:0.38, p:0.003), rice (r:0.38, p:0.004) and pasta (r:0.5, p:0.001).
Previous results correlates with the following data showing a relationship between healthy meals. Their frequency of fish intake was higher when cold meat (r:0.41, p:0.001), legumes (r:0.49, p:0.001), rice (r:0.47, p:0.001), pasta (r:0.52, p:0.001) and raw (r:0.36, p:0.007) and cooked vegetables (r:0.048, p:0.001) were higher. Significant correlation was found between legumes and rice or pasta (r:0.55, p:0.001) or cooked vegetables (r:0.55, p:0.001) and moreover significant correlation appeared between rice and raw (r:0.37, p:0.006) and cooked vegetables (r:0.52, p:0.001). To conclude, higher values of fruit consumption were found when values of raw (r:0.63, p:0.001) and cooked vegetables (r:0.59, p:0.001) consumption were higher (Fig. 2).
Regarding the unhealthiest profile (Fig. 2) a significant correlation was found between alcohol and beer (r:0.39, p:0.002) and fast food (r:0.36, p:0.008). Moreover, higher consumption of soft drinks was found when bread consumption was higher (r:0.34, p:0.019). Furthermore, a significant correlation was found between pastries intake and fast food (r:0.50, p:0.001). A significant correlation was found between cold meat consumption and bread intake (r:0.43, p:0.001).
4. Discussion
The purpose of this study was to analyze the dietary patterns of adolescent students during the COVID-19 pandemic lockdown. It has been found a significant correlation between different types of unhealthy foods such as alcohol and beer, alcohol and fast food, and pastries and fast food. In comparison, a significant correlation was demonstrated too among healthier food such as legumes and meat or fish, fish, and rice or pasta and fruit and vegetables. This fact revealed two well-distinguished dietary patterns. Firstly, this is consistent with the high prevalence of fast-food consumption among young adolescents in low- and middle-income countries in pre-COVID 19 times (LMICs) [29,30]. The increased fast-food and alcohol consumption observed could be alarming because long-term health problems could arise in cases of repeated lockdowns in the future [31,32]. Regarding alcohol consumption, Students have previously reported that they had consumed at least one glass of alcohol at the age of 13 or younger [33]. In this line, there is previous evidence that showed the deeply interconnected nature of food and alcohol consumption [34]. Consequently, over the past few years, adolescence is associated with high rates of alcohol consumption [34] and overweight and obesity [35]. This implies multiple immediate and long-term risks, including raised cholesterol, triglycerides, and glucose; type 2 diabetes; high blood pressure; and an elevated risk of developing adult obesity and its associated consequences [36]. As collateral effects of the coronavirus 2019 pandemic lockdown, the prevalence of overweight/obesity and obesity has significantly increased in overall youths, specifically in high school and undergraduate students [37]. In this line, studies revealed that boredom may induce overeating and increase screen time too [38]. Furthermore, social isolation might worse lifestyle behaviors with enhanced sedentarism, as well as decreased outdoor time and increased weight gain [38]. However, as mentioned above, this study showed a bidirectional influence. A healthier diet was promoted too during COVID 19 lockdown. Inconsistent with this, adults reported changing their diets to be healthier during the lockdown, and 30% reported consuming more vegetables, fruits, and milk products than before home-isolation [39] youths reported an increase in their frequency of intake of wheat products, other staple foods, fish, eggs, fresh vegetables, preserved vegetables, fresh fruit, and dairy products [40].
Regarding the energy requirement and knowing that it is estimated between 1800 and 2500 calories in girls and 2500–3500 calories in boys [41]. In this research, adolescents reported high consumption of food rich in energy as rice, pasta, cheese, or legumes, almost three times per week. Although these energy needs depend on sex, age, body size, pubertal development, and physical activity, results showed an increased energy intake because of adolescents’ tendency for fat- and sugar-rich foods such as fast food or bakery products. However, previous studies also revealed that the consumption of carbonated or sugary drinks, fast food, and commercial pastries decreased in western Europe [42], this last research may be consistent with our data which showed also healthier dietary habits. Above all, energy intake should be taken into account and controlled when sports activities decrease, sleep time increases, and screen time increased [43]. Concerning carbohydrates ‘consumption, results also revealed that adolescents’ carbohydrates (basic and complex) are consumed more than dietary guidelines’ recommendation [44]. Even though basic carbohydrates such as sugar should be reduced, pastries, soft drinks, and energy drinks intake are common in students’ diets. As mentioned above, it is important to mention that unhealthy eating behaviors may cause significant morbidities, the European Society for Clinical Nutrition and Metabolism guidelines suggest using low carbohydrate diets to avoid insulin resistance and hyperglycemia [45].. Governments should take into consideration and create new policies to create adherence and promote healthy diets among youth.
Concerning food composition, COVID-19 has modified the frequency of intake of some products and the amount of consumption of others [46]. Concerning protein requirements (0.8 g/kg/day for girls and 1.0 g/kg/day for boys) [47], based on this research adolescent could have consumed a lower supply of it since they reported a lower consumption of protein than three servings per week. Overeating may be justified by this fact, studies suggested that a diet low in protein increases an attempt to obtain a higher amount of protein from food, leading to overeating and an increased risk of obesity [48]. It is demonstrated that a high protein consumption (>15%) may be a top priority during pandemic since it induces immunoglobulin production and potential antiviral activity [49]. Although our data revealed that consumption of nutrients with high animal protein quality such as egg and milk or vegetative sources rich in protein such as dry legumes and cereal products seems to be regular choices in adolescents’ dietary patterns, its intake is lower than recommendations [50]. It is important to highlight that when an adequate amount of protein is not acquired, retardation of linear growth and sexual maturation may happen, thus it is necessary to encourage children and adolescents to eat two to three servings of meat, fish, poultry, or other protein-rich food each day [51].
In relation to the vitamins and minerals that could be obtained in the intake, results may reveal a deficiency in adolescents’ diet. Its necessity is increased during the adolescent years above that required for growing infants and children [52]. Previous findings suggested that vitamins A, B related vitamins (folic acid, vitamins B6 and B12), vitamin D, vitamin C, and the minerals Se, Fe, Cu, and Zn, are important for proper immune function [53]. Although studies showed that dietary changes towards a healthier diet had taken place during the COVID-19 confinement in Spain, insufficient concentrations were identified in other European researches [54]. Data on vitamin status showed the need for public health authorities to find ways of enhancing particularly vitamin D and folic acid status in identified risk groups [55]. Authors suggested that the requirement for vitamin D, and vitamins A, C, and E are needed in increased amounts for the preservation of the structural and functional properties of the new cells attained during growth [56].
The prevalence of healthy food or unhealthy food among students during uncertain times as a pandemic could be affected by many other factors. It would be necessary to keep in mind the influence of every region, place of residence, educational level, or socioeconomic status [57].. Additionally, it is known that a lower socioeconomic status could be related to a worse diet quality [58]. Findings also may highlight the role of social engagement and encouragement of relatives and peers in adolescents' diet quality. Moreover, previous studies have consistently demonstrated the importance of parents to healthy eating habits during adolescence, specifically vegetable and fruit consumption [59]. Overall, healthy-diet promotion programs and policies targeted at young adolescents should be implemented in LMICs, and their effectiveness should be evaluated.
Although questionnaires provided significant information to be collected in a short period, severe lockdown measures did not allow us to get further methods of evaluation. In addition, self-reported answers may evoke an information bias. Moreover, economic status and place of residence were not included in the questionnaires, and it could be an important issue to take into consideration to improve the complete understanding of nutritional patterns of the different educational levels analyzed.
4.1. Limitation of the study and future research lines
The main limitation of the present research was the low number of participants. The difficulty to recruit voluntary participants in the stressful context of the COVID-19 pandemic and lockdown precluded a large sample. Although the data collection process was completed quickly, questionnaires should be improved in order to get further information about adolescents’ nutrient intake. Future studies must seek this issue. For future research lines, it would be interesting to analyze the effect of pandemic stressors on psychological profile, fact that previous authors highlighted as an important factor to modified behaviors of people [60,61], and the relation with their nutritional habits of them.
4.2. Practical applications
Nutrition habits analysis may be considered as a useful tool to prevent immediate and long-term risks as obesity or diabetes in adolescents. Knowledge of dietary factors could be used by educational institutions to implement multidisciplinary interventions to reduce bad eating habits among students. Additionally, economic status was not included in questionnaires and could be considered an important issue to consider in future research as previous authors highlighted [62], as well as other contextual and behaviors factors as nutritional, odontological, physical activity, social and psychological patterns that could modulate the contextual profile of adolescents [63], [64], [65], [66], [67], [68], [69], [70].
5. Conclusion
Adolescent students presented a dietary pattern during the COVID-19 pandemic lockdown characterized by different associations of food consumption. The study revealed two well-defined profiles of nutrition. On one hand, the consumption of healthier foods such as meat, fish, vegetables, legumes, rice, or pasta, and on the other hand non-healthier foods such as food, alcohol, or pastries. Further investigations are needed to implement multidisciplinary interventions to develop healthier habits in schools and to encourage the adoption of healthy diets among adolescents.
Data Availability
Data will be made available on request.
References
- 1.W.H.O. Coronavirus Disease (COVID-19) pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 24 May 2021).
- 2.Li S., Wan Y., Xue J., Zhao N., Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active web users. Int. J. Environ. Res. Public Health. 2020;17:2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X. An investigation of the mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immunity. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clemente-Suárez V.J., Ramos-Campo D.J., Mielgo-Ayuso J., Dalamitros A.A., Nikolaidis P.A., Hormeño-Holgado A., Tornero-Aguilera J.F. Nutrition in the actual COVID-19 pandemic. A narrative review. Nutrients. 2021;13:1924. doi: 10.3390/nu13061924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Odriozola-González P., Planchuelo-Gómez Á., Irurtia M.J., de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Muscogiuri G., Barrea L., Savastano S., Colao A. Nutritional recommendations for CoVID-19 quarantine. Eur. J. Clin. Nutr. 2020;74:850–851. doi: 10.1038/s41430-020-0635-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andrews G. Comorbidity and the general neurotic syndrome. Br JPsychiatry. 1996;168:76–84. https://pubmed.ncbi.nlm.nih.gov/8864152/ [PubMed] [Google Scholar]
- 9.Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med. Sci. Monitor. 2020:26. doi: 10.12659/MSM.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moynihan A.B., Van Tilburg W.A., Igou E.R., Wisman A., Donnelly A.E., Mulcaire J.B. Eaten up by boredom: consuming food to escape awareness of the bored self. Front. Psychol. 2015;6 doi: 10.3389/fpsyg.2015.00369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gasmi A., Noor S., Tippairote T., Dadar M., Menzel A., Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haddad C., Zakhour M., Bou Kheir M., Haddad R., Al Hachach M., Sacre H., Salameh P. Association between eating behavior and quarantine/confinement stressors during the coronavirus disease 2019 outbreak. J. Eat Disord. 2020;8:40. doi: 10.1186/s40337-020-00317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lutter M., Nestler E.J. Homeostatic and hedonic signals interact in the regulation of food intake. J. Nutr. 2009;139:629–632. doi: 10.3945/jn.108.097618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butler M.J., Eckel L.A. Eating as a motivated behavior: modulatory effect of high-fat diets on energy homeostasis, reward processing, and neuroinflammation. Integr Zool. 2018;13:673–686. doi: 10.1111/1749-4877.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subbie-Saenz de Viteri S., Pandey A., Pandey G., Kamarajan C., Smith R., Anokhin A., Bauer L., Bender A., Chan G., Dick D., Edenberg H., Kinreich S., Kramer J., Schuckit M., Zang Y., McCutcheon V., Bucholz K., Porjesz B., Meyers J.L. Pathways to post-traumatic stress disorder and alcohol dependence: trauma, executive functioning, and family history of alcoholism in adolescents and young adults. Brain Behav. 2020:10. doi: 10.1002/brb3.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torres S.J., Nowson C.A. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23:887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., Crunelle C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: results from a web-based survey. Eur. Addict. Res. 2020;26:309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martín-Rodríguez A., Tornero-Aguilera J.F., López-Pérez P.J., Clemente-Suárez V.J. Gender differences in nutritional, odontological and psychological patterns of adolescent students during COVID-19 pandemic. Appl. Sci. 2021;11:8499. doi: 10.3390/app11188499. [DOI] [Google Scholar]
- 20.Aiken A., Clare P.J., Wadolowski M., Hutchinson D., Najman J.M., Slade T., Bruno R., McBride N., Kypri K., Mattick R.P. Age of alcohol initiation and progression to binge drinking in adolescence: a prospective cohort study. Alcohol Clin. Exp. Res. 2018;42:100–110. doi: 10.1111/acer.13525. [DOI] [PubMed] [Google Scholar]
- 21.Leal-López E., Sánchez-Queija I., Rivera F., Moreno C. Trends in alcohol consumption among school-aged adolescents in Spain (2010-2018) Gac. Sanit. 2021;35:35–41. doi: 10.1016/j.gaceta.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 22.Gore F.M., Bloem P.J.M., Patton G.C., Ferguson J., Joseph V., Coffey C., Sawyer S.M., Mathers C.D. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet. 2011;377:2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- 23.Rose T., Barker M., Jacob C., Morrison L., Lawrence W., Strömmer S., Vogel C., Woods-Townsend K., Farrell D., Inskip H., Baird J.A. Systematic review of digital interventions for improving the diet and physical activity behaviors of adolescents. J. Adolesc. Health. 2017;61:669–677. doi: 10.1016/j.jadohealth.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cutler G.J., Flood A., Hannan P., Neumark-Sztainer D. Major patterns of dietary intake in adolescents and their stability over time. J. Nutr. 2009;139:323–328. doi: 10.3945/jn.108.090928. [DOI] [PubMed] [Google Scholar]
- 25.Opichka K., Smith C., Levine A.S. Problematic eating behaviors are more prevalent in African American women who are overweight or obese than African American women who are lean or normal weight. Fam. Commun. Health. 2019;42:81–89. doi: 10.1097/FCH.0000000000000222. [DOI] [PubMed] [Google Scholar]
- 26.Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. 2020;12:1657. doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ruiz-Roso M.B., de Carvalho Padilha P., Mantilla-Escalante D.C., Ulloa N., Brun P., Acevedo-Correa D., Arantes Ferreira Peres W., Martorell M., Aires M.T., de Oliveira Cardoso L. Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12:1807. doi: 10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sánchez-Sánchez E., Ramírez-Vargas G., Avellaneda-López Y., Orellana-Pecino J.I., García-Marín E., Díaz-Jimenez J. Eating habits and physical activity of the spanish population during the COVID-19 pandemic period. Nutrients. 2020;12:2826. doi: 10.3389/fnut.2021.683261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li L., Sun N., Zhang L., Xu G., Liu J., Hu J., Zhang Z., Lou J., Deng H., Shen Z., Han L. Fast-food consumption among young adolescents aged 12-15 years in 54 low- and middle-income countries. Glob Health Action. 2020;13 doi: 10.1080/16549716.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O., Paineiras-Domingos L.L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C.S., Mataruna L., Taheri M., Irandoust K., Khacharem A., Bragazzi N.L., Chamari K., Glenn J.M., Bott N.T., Gargouri F., Chaari L., Batatia H., Ali G.M., Abdelkarim O., Jarraya M., Abed K.E., Souissi N., Van Gemert-Pijnen L., Riemann B.L., Riemann L., Moalla W., Gómez-Raja J., Epstein M., Sanderman R., Schulz S.V., Jerg A., Al-Horani R., Mansi T., Jmail M., Barbosa F., Ferreira-Santos F., Šimunič B., Pišot R., Gaggioli A., Bailey S.J., Steinacker J.M., Driss T., Hoekelmann A. Effects of COVID-19 home confinement on eating behaviour and physical activity: results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bakaloudi D., Dhanushya T., Jeyakumar D., Jayawardena R., Chourdakis M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: a systematic review of the evidence. Clin. Nutr. 2021:S0261–S5614. doi: 10.1016/j.clnu.2021.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malta D.C., Szwarcwald C.L., Barros M.B.A., Gomes C.S., Machado Í.E., Souza Júnior P.R.B., Romero D.E., Lima M.G., Damacena G.N., Pina M.F., Freitas M.I.F., Werneck A.O., Silva D.R.P.D., Azevedo L.O., Gracie R. The COVID-19 Pandemic and changes in adult Brazilian lifestyles: a cross-sectional study. Epidemiol Serv Saude. 2020;29 doi: 10.12998/wjcc.v10.i3.882. [DOI] [PubMed] [Google Scholar]
- 33.Sturua L., Baramidze L., Gamkrelidze A., Galdava G. Alcohol use in Georgian students; pilot study rigorously following criteria of a European school project on alcohol and another drug. Georgian Med News. 2010;179:52–61. https://pubmed.ncbi.nlm.nih.gov/20234066/ [PubMed] [Google Scholar]
- 34.Scott S., Muir C., Stead M., Fitzgerald N., Kaner E., Bradley J., Wrieden W., Power C., Adamson A. Exploring the links between unhealthy eating behavior and heavy alcohol use in the social, emotional and cultural lives of young adults (aged 18–25): a qualitative research study. Appetite. 2020;144 doi: 10.1016/j.appet.2019.104449. [DOI] [PubMed] [Google Scholar]
- 35.Das J.K., Salam R.A., Thornburg K.L., Prentice A.M., Campisi S., Lassi Z.S., Koletzko B., Bhutta Z.A. Nutrition in adolescents: physiology, metabolism, and nutritional needs. Ann N Y Acad Sci. 2017;1393:21–33. doi: 10.1111/nyas.13330. [DOI] [PubMed] [Google Scholar]
- 36.Lloyd L.J., Langley-Evans S.C., McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int. J. Obes. 2012;36:1–11. doi: 10.1038/ijo.2011.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang S., Guo B., Ao L., Yang C., Zhang L., Zhou J., Jia P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. 2020;10:12416. doi: 10.1111/cob.12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Balanzá-Martínez V., Atienza-Carbonell B., Kapczinski F., De Boni R.B. Lifestyle behaviors during the COVID-19 - time to connect. Acta Psychiatr. Scand. 2020;141:399–400. doi: 10.1111/acps.13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X., Lei S.M., Le S., Yang Y., Zhang B., Yao W., Gao Z., Cheng S. Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among chinese adults. Int. J. Environ. Res. Public Health. 2020;17:5575. doi: 10.3390/ijerph17155575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yu B., Zhang D., Yu W., Luo M., Yang S., Jia P. Impacts of lockdown on dietary patterns among youths in China: the COVID-19 impact on lifestyle change survey. Public Health Nutr. 2021;24:3221–3232. doi: 10.1017/S1368980020005170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kuzgun Y. Nobel Publishing; Ankara: 2002. Counseling in Primary Education. [Google Scholar]
- 42.Kriaucioniene V., Bagdonaviciene L., Rodríguez-Pérez C., Petkeviciene J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: the Lithuanian COVIDiet Study. Nutrients. 2020;12:3119. doi: 10.3390/nu12103119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jia P., Zhang L., Yu W., Yu B., Liu M., Zhang D., Yang S. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 impact on lifestyle change survey (COINLICS) Int J Obes (Lond) 2021;45:695–699. doi: 10.1038/s41366-020-00710-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.T. Erkan. Nutrition in adolescents. In Adolescent Health II, (2008) p. 73.
- 45.Barazzoni R., Bischoff S.C., Breda J., Wickramasinghe K., Krznaric Z., Nitzan D., Singer P. ESPEN expert statements and practical guidance for the nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020;39:1631–1638. doi: 10.1016/j.clnu.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang Y.C. COVID-19–related school closings and risk of weight gain among children. Obesity. 2020;28:1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ozdemil A. Vitamins minerals and fibres in adolescence diet. Int. Journal Caring Science. 2012;9:364. [Google Scholar]
- 48.Gosby A.K., Conigrave A.D., Raubenheimer D., Simpson S.J. Protein leverage and energy intake. Obes. Rev. 2014;15:183–191. doi: 10.1016/j.cmet.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 49.Ng T.B., Cheung R.C.F., Wong J.H., Wang Y., Ip D.T.M., Wan D.C.C., Xia J. Antiviral activities of whey proteins. Appl. Microbiol. Biotechnol. 2015;99:6997–7008. doi: 10.1007/s00253-015-6818-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karakoyun M., Yagci R.V. Healthy nutrition and obesity in adolescence. Turkey Clinical J Fam Med-Special Topics. 2013;4:31–35. [Google Scholar]
- 51.Richardson D.P., Lovegrove J.A. Nutritional status of micronutrients as a possible and modifiable risk factor for COVID-19: a UK perspective. Br. J. Nutr. 2021;125:678–684. doi: 10.1017/S000711452000330X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marino D.D., King J.C. Nutritional concerns during adolescence. Pediatr. Clin. North Am. 1980;27:123–139. doi: 10.1016/s0031-3955(16)33824-x. [DOI] [PubMed] [Google Scholar]
- 53.Richter M., Baerlocher K., Bauer J.M., Elmadfa I., Heseker H., Leschik-Bonnet E., Stangl G., Volkert D., Stehle P. Revised reference values for the intake of protein. Ann. Nutr. Metab. 2019;74:242–250. doi: 10.1159/000499374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rodríguez-Pérez C., Molina-Montes E., Verardo V., Artacho R., García-Villanova B., Guerra-Hernández E.J., Ruíz-López M.D. Changes in dietary behaviours during the COVID-19 outbreak confinement in the spanish COVIDiet study. Nutrients. 2020;12:1730. doi: 10.3390/nu12061730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moreno L.A., Gottrand F., Huybrechts I., Ruiz J.R., González-Gross M., DeHenauw S. HELENA study group. nutrition and lifestyle in european adolescents: the HELENA (healthy lifestyle in europe by nutrition in adolescence) study. Adv. Nutr. 2014;5:615S–623S. doi: 10.3945/an.113.005678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Diab L., Krebs N.F. Vitamin excess and deficiency. Pediatr. Rev. 2018;39:161–179. doi: 10.1542/pir.2016-0068. [DOI] [PubMed] [Google Scholar]
- 57.Alemán J.A., Rentero M.P.Z., Montoro-García S., Mulero J., Garrido A.P., Leal M., Guerrero L., Ramos E., Ruilope L.M. Adherence to the “Mediterranean diet” in Spain and its relationship with cardiovascular risk (DIMERICA study) Nutrients. 2016;8:680. doi: 10.3390/nu8110680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Darmon N., Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr. Rev. 2015;73:643–660. doi: 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.J. Vanhelst, L. Beghin, E. Drumez, A. Duhamel, E. de Henauw. Adolescents'' diet quality in relation to their relatives'' and peers'' diet engagement and encouragement: the healthy lifestyle in europe by nutrition in adolescence (HELENA) study. Public health nutrition, (2018)17, 3192–3201. doi: 10.1017/S1368980018001787. [DOI] [PMC free article] [PubMed]
- 60.Rodriguez-Besteiro S., Tornero-Aguilera J.F., Fernández-Lucas J., Clemente-Suárez V.J. Gender differences in the COVID-19 pandemic risk perception, psychology, and behaviors of spanish university students. Int. J. Environ. Res. Public Health. 2021;18:3908. doi: 10.3390/ijerph18083908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Clemente-Suárez V.J., Navarro-Jiménez E., Jimenez M., Hormeño-Holgado A., Martinez-Gonzalez M.B., Benitez-Agudelo J.C., Perez-Palencia N., Laborde-Cárdenas C.C., Tornero-Aguilera J.F. Impact of COVID-19 pandemic in public mental health: an extensive narrative review. Sustainability. 2021;13:3221. doi: 10.3390/su13063221. [DOI] [Google Scholar]
- 62.Martínez-González M.B., Pérez-Pedraza D.C., Alfaro-Álvarez J., Reyes-Cervantes C., González-Malabet M., Clemente-Suárez V.J. Women facing psychological abuse: how do they respond to maternal identity humiliation and body shaming? Int. J. Environ. Res. Public Health. 2021;18:6627. doi: 10.3390/ijerph18126627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Clemente-Suárez V.J., Beltrán-Velasco A.I., Ramos-Campo D.J., Mielgo-Ayuso J., Nikolaidis P.A., Belando N., Tornero-Aguilera J.F. Physical activity and COVID-19. The basis for an efficient intervention in times of COVID-19 pandemic. Physiol. Behav. 2022;244 doi: 10.1016/j.physbeh.2021.113667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rodriguez-Besteiro S., Valencia-Zapata G., Beltrán de la Rosa E., Clemente-Suárez V.J. Food consumption and COVID-19 risk perception of university students. Sustainability. 2022;14(3):1625. [Google Scholar]
- 65.Clemente-Suárez V.J., Ruisoto P., Isorna-Folgar M., Cancelo-Martínez J., Beltrán-Velasco A.I., Tornero-Aguilera J.F. Psychophysiological and psychosocial profile of patients attending drug addiction centers. Appl. Psychophysiol. Biofeedback. 2021:1–8. doi: 10.1007/s10484-021-09531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.López-Varas F., García-López O., Icarán-Francisco E.M., Burgos-Postigo S., Clemente-Suárez V.J. Modifications of academic competences and intelligence in a university grade. Physiol. Behav. 2021;241 doi: 10.1016/j.physbeh.2021.113564. [DOI] [PubMed] [Google Scholar]
- 67.Tornero-Aguilera J.F., Rubio-Zarapuz A., Clemente-Suárez V.J. Implications of surgical mask use in physical education lessons. Physiol. Behav. 2021;239 doi: 10.1016/j.physbeh.2021.113513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Beltrán-Velasco A.I., Donoso-González M., Clemente-Suárez V.J. Analysis of perceptual, psychological, and behavioral factors that affect the academic performance of education university students. Physiol. Behav. 2021;238 doi: 10.1016/j.physbeh.2021.113497. [DOI] [PubMed] [Google Scholar]
- 69.Conde P.S., Clemente-Suárez V.J. Differences between students and professors in difficulty, stress and performance in a nursing objective structured clinical examination (OSCE) Physiol. Behav. 2021;239 doi: 10.1016/j.physbeh.2021.113502. [DOI] [PubMed] [Google Scholar]
- 70.Martín-Rodríguez A., Tornero-Aguilera J.F., López-Pérez P.J., Clemente-Suárez V.J. The effect of loneliness in psychological and behavioral profile among high school students in Spain. Sustainability. 2022;14(1):168. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.