Abstract
Objective:
The present study tested the hypothesis that the effect of self-paced exercise on adherence to exercise programs is more pronounced with increasing age.
Method:
Fifty-nine low-active overweight adults (18-65 years) were encouraged to walk 30 to 60 min/day and randomized to either self-paced (n = 30) or prescribed moderate-intensity (n = 29) conditions.
Results:
The effect of study condition was moderated by age (main effect: b = 6.14, SE = 2.54, p = .02; Condition × Age: b = −11.55, SE = 3.77, p < .01), such that among participants >50 years, those in the self-paced condition exercised 6 more min/day than participants in the prescribed moderate-intensity condition (p = .02), whereas among participants <50 years, those in the self-paced condition exercised 5.4 fewer min/day compared with those in the moderate-intensity condition (p = .05). Affective response to physical activity did not mediate the moderating effect of age.
Discussion:
As age increases, adults may be more likely to adhere to self-paced versus prescribed moderate-intensity exercise.
Keywords: exercise, affective response, age, self-paced, weight
Introduction
In the United States, approximately 70% of adults are overweight or obese (Hales, Carroll, Fryar, & Ogden, 2017). Regular physical activity (PA) plays an important role in preventing weight gain and in weight maintenance after weight loss (Donnelly et al., 2009; Donnelly et al., 2003; Donnelly, Jacobsen, Heelan, Seip, & Smith, 2000; Garber et al., 2011; Jakicic et al., 2001). Moreover, independent of any effects it may have on weight, regular PA has been shown to decrease risk of heart disease (Barry et al., 2014), type 2 diabetes (Ross, 2003), and cancers of the breast and colon (Boyle, Keegel, Bull, Heyworth, & Fritschi, 2012; Monninkhof et al., 2007), morbidities for which those who are overweight or obese are at increased risk. The benefits of regular PA may become more pertinent as people age, with mounting evidence demonstrating the protective effects of regular PA on age-related weight gain (Waller, Kaprio, & Kujala, 2008) as well as cardiovascular disease, certain cancers, dementia, sarcopenia, osteoporosis, and Alzheimer’s disease (Nelson et al., 2007; Warburton, Nicol, & Bredin, 2006).
The current U.S. Department of Health and Human Services guidelines recommend that adults expend at least 1,000 kcal per week in PA (Royall, Troiano, Johnson, Kohl, & Fulton, 2008), which can be obtained through 150 min per week of moderate-intensity PA, 75 min of vigorous-intensity PA, or some combination. However, current estimates suggest that only 3.5% to 43.5% of U.S. adults, and 28% of overweight or obese adults adhere to these recommendations, with estimates varying according to measurement methods (Adabonyan, Loustalot, Kruger, Carlson, & Fulton, 2010; Carlson, Fulton, Schoenborn, & Loustalot, 2010; Donnelly et al., 2009; Troiano et al., 2008; Young, Jerome, Chen, Laferriere, & Vollmer, 2009). Moreover, people across all World Health Organization regions become less active as they age (Hallal et al., 2012). Among U.S. adults, a more progressive decline in PA is seen after age 45 to 50 (Luke, Dugas, Durazo-Arvizu, Cao, & Cooper, 2011; Troiano et al., 2008). In essence, PA rates tend to decrease as people age and gain weight while the health benefits of PA become more pronounced.
Until recently, research on psychological contributors to PA adherence has been focused primarily on cognitive determinants, such as self-efficacy, outcome expectancies, attitudes, social support, social norms, and behavioral intentions (Marcus et al., 2006; Williams & Marcus, 2012). However, in the past two decades, there has been a gradual increase in attention to affective determinants of health behaviors in general (Williams, Rhodes, & Conner, 2018) and PA adherence in particular (Baldwin, Baldwin, Loehr, Kangas, & Frierson, 2013; Conner, Rhodes, Morris, McEachan, & Lawton, 2011; Ekkekakis, 2003; Ekkekakis, Hall, & Petruzzello, 2005b; Kiviniemi, Voss-Humke, & Seifert, 2007; Kwan & Bryan, 2010; Rhodes, Courneya, Blanchard, & Plotnikoff, 2007; Rhodes, Fiala, & Conner, 2009; Rose & Parfitt, 2012; Schneider, Dunn, & Cooper, 2009; Williams et al., 2008; Williams, Dunsiger, Jennings, & Marcus, 2012). One of the major challenges to increasing PA among unfit and/or sedentary populations is that many people within these populations experience a negative shift in affective valence (feeling good versus bad; Russell, 1980) from prior to PA to during PA (Ekkekakis, Parfitt, & Petruzzello, 2011). These findings appear to conflict with the popular notion that “exercise feels good”; however, positive shifts in affective valence tend to occur after PA rather than during PA (Ekkekakis et al., 2011). Thus, it is more accurate to say: Being done with exercise feels good, whereas exercise itself often feels bad.
Affective responses to PA may be important for understanding the low rates of PA. For example, previous theorists have posited that humans have a universal tendency to pursue behaviors that feel good and avoid behaviors that feel bad, a phenomenon known as the hedonic principle or psychological hedonism (Bentham, 1789/2007; Cabanac, 1971; Kahneman, Wakker, & Sarin, 1997; Williams, 2018). Indeed, a recent systematic review indicates that those who experience more negative (or less positive) affective responses to PA are less likely to repeat PA in the future, and thus more likely to drop out of PA promotion programs (Rhodes & Kates, 2015). Given that many people have an immediate negative affective response to PA, and a more negative response predicts lower PA behavior, it is unsurprising that there is a public health problem of physical inactivity (Lee, Emerson, & Williams, 2016).
One possible strategy to increase PA adherence is to circumvent the negative affective response to PA by recommending self-paced PA—that is, engaging in PA of a self-selected intensity (Williams, 2008). By self-selecting intensity rather than attempting to engage in PA of a prescribed intensity (e.g., moderate intensity), it is possible that one can optimize affective response to PA, thus making an aversive response less likely and, in turn, increasing the likelihood of continuing to engage in regular PA (Kwan & Bryan, 2010; Schneider et al., 2009; Williams et al., 2008; Williams et al., 2012).
Some recent evidence has accumulated to suggest that self-paced PA may lead to a more positive affective response and thus better adherence to PA programs. Several laboratory studies comparing the psychological response to self-paced versus prescribed intensity PA have shown that self-paced PA results in a more positive affective response (Ekkekakis & Lind, 2006; Parfitt, Rose, & Burgess, 2006; Rose & Parfitt, 2007). Moreover, in a recent randomized pilot study, adults assigned to a self-paced walking condition engaged in more minutes of PA than adults who were prescribed moderate-intensity walking, with a trend toward greater PA-based energy expenditure for the self-paced condition (Williams et al., 2015). In the latter study, better adherence to the self-paced condition was a function of a more positive affective response to self-paced versus prescribed moderate-intensity PA (Williams et al., 2016).
Few studies, however, have examined age differences in affective response to self-paced or prescribed intensity PA and the implications for PA adherence. In two laboratory studies, Barnett (2012) found that compared with younger adults, older adults showed higher positive engagement (e.g., enthusiastic, happy, upbeat) during 20 min of stationary cycling at 60% VO2max, whereas Focht, Knapp, Gavin, Raedeke, and Hickner (2007) found no difference between age groups in affective response during 20 min of stationary cycling at 65% of VO2peak. In a third study, DaSilva and colleagues (2010) found no age-related differences in affective responses to self-paced PA. However, to our knowledge, no study has examined age-related differences in affective response and adherence to self-paced versus moderate-intensity PA.
Thus, the goal of the present study was to test age as a moderator of the effects of self-selected versus prescribed moderate-intensity PA on PA adherence. We hypothesized (Hypothesis 1) that the recommendation for self-paced PA (as compared with prescribed moderate-intensity PA) would have a more positive effect on adherence to PA among older versus younger adults (Figure 1). We further hypothesized (Hypothesis 2) that any age-related differences seen in the positive effect of self-paced (compared with prescribed moderate intensity) PA on PA behavior would be explained by more positive affective responses to PA.
Figure 1.
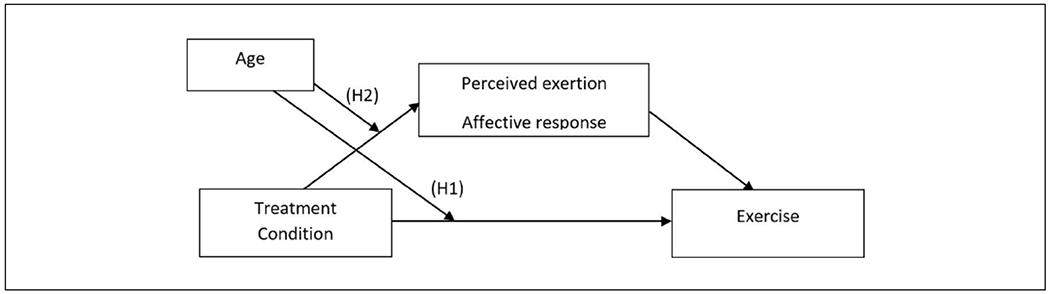
Conceptual model.
Method
The present study was a secondary analysis of data from a previous randomized pilot study comparing self-selected with prescribed moderate-intensity PA among low-active overweight adults (Williams et al., 2015). Moderate intensity (64%-76% of age-adjusted maximal heart rate) was used as a comparison to self-paced intensity because it is recommended as an appropriate intensity for the general population by the American College of Sports Medicine (Thompson, Pescatello, & Gordon, 2010), the Center for Disease Control and Prevention (2008), and the World Health Organization (2010). The local institutional review board approved the study protocol.
Participants
Participants were community-dwelling adults (n = 59), ages 18 to 65, who were low-active (<60 min/week of structured exercise) and overweight or obese (body mass index [BMI] = 25.0-39.9 kg/m2), but otherwise healthy (i.e., no chronic disease) (Table 1). The participants had a mean age of 47.71 years (SD = 11.06), and a mean BMI of 31.93 kg/m2 (SD = 3.99). Most participants were female (88%), employed (85%), reported household income ⩾ US$50,000/year (54%), and self-identified as non-Hispanic White (76%). There were no significant differences in baseline demographics between groups (p > .05).
Table 1.
Demographic Characteristics of Subjects by Total Sample and by Age 50.
| Total (n = 59) | Moderate intensity (n = 14) | Self-paced (n = 15) | Moderate intensity (n = 15) | Self-paced (n = 15) | |
|---|---|---|---|---|---|
| Age (SD) | 47.71 (11.06) years | Age < 50 years | Age ⩾ 50 years | ||
| Gender, % female | 88% | 92.9% | 85.7% | 80.0% | 92.8% |
| BMI (SD) | 31.93 (3.99) | 31.83 (3.20) | 32.52 (5.89) | 31.36 (2.88) | 32.04 (3.77) |
| Race/ethnicity, % non-Hispanic White | 88% | 85.7% | 78.6% | 93.3% | 93.8% |
| Household income, % over 50,000 | 54% | 64.3% | 57.1% | 46.7% | 50.0% |
| Employment, % employed | 85% | 92.9% | 71.4% | 86.7% | 87.5% |
Note. BMI = body mass index.
Procedures
Participant recruitment included distribution of brochures throughout the community, and advertising in newspapers, on the Internet, and the radio. Participants were blinded to the true purpose of this study (i.e., the efficacy of self-paced versus prescribed moderate-intensity exercise prescriptions) and were instead told that the purpose of the study was to test an exercise promotion program.
All participants received a 6-month exercise promotion program consisting of mailed print-based materials designed to help them overcome barriers to regular exercise (Marcus, Lewis, et al., 2007; Marcus, Napolitano et al., 2007; Williams et al., 2011). The intervention focused on structured and planned exercise, with a particular focus on walking-for-exercise. This was done to isolate the effects of intensity of PA (self-paced vs. prescribed moderate intensity) by minimizing potential variability in PA modality (e.g., lifestyle PA, cycling, jogging, hiking, and swimming). Specifically, all participants were instructed to engage in one 30- to 60-min walking session at least 5 days per week, with a total goal of 150 to 300 min of walking per week, to meet national PA guidelines (Donnelly et al., 2009; Royall et al., 2008).
Participants were randomized to either the prescribed moderate intensity or self-selected (self-paced) intensity condition. Participants were randomized surreptitiously at the randomization/enrollment session, with research staff opening sealed envelopes in which assigned groups were written in advance. Participants randomized to the moderate-intensity condition (n = 29) were told to walk at an intensity corresponding to 64% to 76% of their predicted maximal heart rate. Participants in the self-selected intensity condition (n = 30) were told to select their own pace when walking for exercise. All participants were given a heart rate monitor and asked not to walk at a pace that elevated their heart rate beyond 76% of their predicted maximal heart rate.
Measures
Exercise.
Structured and planned walking for purposes of exercise was measured through ecological momentary assessment (EMA) throughout the course of the 6-mon intervention. Participants used handheld electronic diaries (e-diaries; HP iPAC 111) to provide real-time self-reports of their exercise behavior. Participants were instructed to indicate the start of an exercise session when they began walking and to indicate when the session ended. The real-time reports of exercise were used to calculate the number of minutes participants walked for exercise. Each morning participants were also asked whether they had (a) exercised the previous day, and (b) if they had reported this exercise session in real time using their e-diaries. Participants completed 87% of these daily morning reports over the 6-month study period, with no differences between conditions (p > .05). For 81% of the exercise sessions that participants reported on the daily morning report (i.e., participant indicated that they had walked for exercise the previous day), participants reported completing real-time exercise reports on the previous day at the time of the exercise session (and, in all cases, they had done so), and thus, the number of minutes of exercise was computed based on the real-time data. However, for the remaining 19% of exercise sessions reported on the morning report, participants reported that they did not record the exercise in real time (and, in all cases, they had not done so). In these situations, participants were asked to retrospectively report the number of minutes of exercise completed the previous day.
Affective response to exercise.
Participants were asked to report their affective response to exercise at every exercise session during the 6-month study. After indicating the start of an exercise session, participants were asked to report their affect in response to the question, “right now, how are you feeling?” and responded on a scale from −5 (very bad) to +5 (very good) (Hardy & Rejeski, 1989). Participants were asked to report their affect during exercise in 5-min increments after the initial affect report when the exercise session started. To reduce burden, after 35 min of walking, participants were asked to report their affect in 10-min increments; after 55 min of walking, participants were asked to report their affect in 15-min increments. There was at least one during-exercise affect report for 90.2% of exercise sessions that were reported in real time.
Statistical Analyses
A mixed effects regression model was used to test the hypothesis that age at baseline was a moderator of the effect of condition on minutes of exercise over the course of the 6-month intervention. The clustered nature of the data was taken into account by nesting daily minutes of exercise both within week and within participant. The distribution of daily minutes of exercise was skewed toward zero, and a log-transformation used to normalize the data. Missing data were accounted for through a likelihood-based approach to estimation which makes use of all available data.
To test the moderation hypothesis, exercise behavior was regressed on condition, age, time, the interaction between Condition × Age, and a subject-specific random intercept. To test whether the interaction effect of Condition × Age was mediated by affective response to exercise, a series of three regression models were conducted simultaneously, to estimate overall path coefficients, as well as indirect effects. A median split was used to divide participants into those who were ⩾50 versus <50. Age 50 is also a clinically meaningful cut point regarding declines in PA (Luke et al., 2011; Troiano et al., 2008). First, affective response to exercise was regressed on the Condition × Age interaction, main effects of condition and age, time, and a subject-specific random intercept (a path). Next, exercise behavior was regressed on affective response to exercise, time, and a subject-specific random intercept (b path). Finally, exercise behavior was regressed on the Condition × Age interaction, main effects of condition and age, affective response to exercise, time, and a subject-specific random intercept (indirect path). All standard errors were adjusted for clustering effects over time. Analyses were conducted using SPSS 18.0 and SAS 9.3.
Results
We tested for a moderation effect of age on the impact of self-paced versus prescribed moderate-intensity exercise on number of minutes of structured walking for exercise. We found significant moderating effects of age such that differences between self-paced and moderate-intensity conditions were more pronounced among older participants (main effect of condition: 6.14, SE = 2.54, p = .02; Condition × Age: −11.55, SE = 3.77, p < .01; Figure 2). As hypothesized, simple effects analysis showed that among participants ⩾50 years, those in the self-paced condition exercised 6 more min/day (p = .02) compared with those in the moderate-intensity condition. Alternatively, among participants <50 years, those in the moderate-intensity condition exercised 5.4 more min/day compared with those in the self-paced condition, with the latter difference of borderline significance (p = .05).
Figure 2.
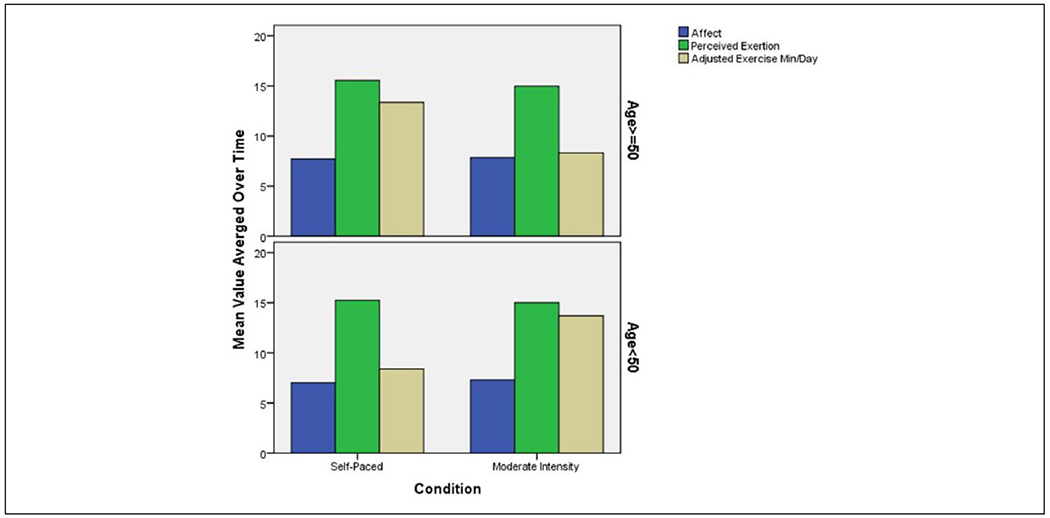
Affective response to exercise, perceived exertion, and exercise minutes per day by age and intervention group.
We also examined affective response to exercise as a putative mediator of the moderating effects of age to determine whether effects of study condition on walking minutes by age were due to age-based differences in affective response to exercise. Contrary to our hypothesis, the effect of study condition on affective response to exercise was not moderated by age (p = .13) (Figure 2). The effect of study condition on perceived exertion also was not moderated by age (Figure 2).
Discussion
Empirical evidence regarding the benefits of self-paced walking for increasing PA is accumulating (Schneider et al., 2009; Williams et al., 2015; for review see Ekkekakis, 2009). Self-paced PA, in contrast to prescribed intensity PA, may influence affective response to PA, which may vary by age (Barnett, 2012; but see DaSilva et al., 2010; Focht et al., 2007). To our knowledge, the present study is the first to examine the moderating role of age on the effect of a self-selected versus prescribed moderate-intensity exercise on exercise adherence (Figure 1).
Consistent with our hypothesis, age moderated the effect of condition on minutes spent walking for exercise over a 6-month exercise promotion program. Participants who were older and told to self-select their exercise intensity exercised more minutes per week compared with older participants who were told to exercise at moderate intensity. In contrast, and unexpectedly, participants who were younger and told to exercise at a moderate intensity trended toward exercising more minutes per week compared with younger participants told to self-select their exercise intensity.
In an attempt to understand why the self-paced recommendation worked better among adults who were older, we investigated affective response to exercise as a putative mediator of the hypothesized moderating effect of age. A prior study using the present data showed that, among the full sample of participants, those in the self-paced condition has a more positive affective response to exercise than those in the prescribed moderate-intensity condition (Williams et al., 2016). However, the present analysis showed that the effect of condition on affective response to exercise was not moderated by age. That is, there was no differential effect of condition (self-paced vs. moderate intensity) on affective response to exercise as a function of age.
Taken together, the present findings show that adults who were older were more likely to exercise if they were given a recommendation to exercise at their own pace rather than specifically told to exercise at moderate intensity. The positive effect of self-paced exercise among older versus younger adults was not explained by affective response to exercise. Other possible reasons for this finding are that older adults, compared with younger adults, may have experienced more uncomfortable symptoms, such as shortness of breath, due to a longer span of de-conditioning, and therefore were more likely to exercise at a self-paced versus a moderate intensity. Although one might expect that such physical symptoms would impact affective response, it is possible that they instead had a direct effect on exercise behavior. In addition, there may have been other unmeasured variables that led to the differential effects of self-selected versus moderate intensity on exercise behavior among older versus younger adults, such as differences in expected benefits of exercising at a self-paced intensity, greater ability to engage in communal walking at a self-paced intensity, or the challenge of determining moderate-intensity levels. Additional research is needed to understand the role of these and other potential mediators of the differential effects of self-selected versus moderate intensities among older versus younger adults.
A strength of the present study is the use of EMA in a field-based experimental context, which, compared with the previous laboratory studies in this area, is likely to be more ecologically valid. The present sample also intentionally included only participants who were overweight and obese. This population was chosen because previous research shows that affective response to PA may be more negative among overweight and obese adults (Ekkekakis & Lind, 2006).
On the contrary, the relatively small sample size in the present study provided limited statistical power, particularly when testing effects of moderated mediation. Thus, the null findings for our second hypothesis could be the result of a type II error. In addition, the present study included a predominantly affluent female sample and thus the findings may not generalize to other populations.
Conclusion
While the health benefits of PA become more pronounced as people age and gain weight, PA rates tend to decrease. The present study provides preliminary evidence that recommending self-paced exercise may be a particularly effective strategy to promote exercise among overweight adults who are older (i.e., ⩾50), as compared with the prescription of moderate-intensity exercise as recommended in national guidelines. More research is needed to explore the potential mechanisms of this effect.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by National Cancer Institute (R21 CA137211; Williams, PI). Harold Lee was supported by National Heart Lung and Blood Institute (F31 HL140817). Jessica Emerson was supported by National Cancer Institute (F31 CA206245).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adabonyan I, Loustalot F, Kruger J, Carlson SA, & Fulton JE (2010). Prevalence of highly active adults—Behavioral risk factor surveillance system, 2007. Preventive Medicine, 51, 139–143. doi: 10.1016/j.ypmed.2010.05.014 [DOI] [PubMed] [Google Scholar]
- Baldwin AS, Baldwin SA, Loehr VG, Kangas JL, & Frierson GM (2013). Elucidating satisfaction with physical activity: An examination of the day-to-day associations between experiences with physical activity and satisfaction during physical activity initiation. Psychology & Health, 28, 1424–1441. [DOI] [PubMed] [Google Scholar]
- Barnett F (2012). The effect of exercise on affective and self-efficacy responses in older and younger women. Journal of Physical Activity and Health, 10, 97–105. doi: 10.1123/jpah.10.1.97 [DOI] [PubMed] [Google Scholar]
- Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, & Blair SN (2014). Fitness vs. fatness on all-cause mortality: A meta-analysis. Progress in Cardiovascular Diseases, 56, 382–390. [DOI] [PubMed] [Google Scholar]
- Bentham J (2007). An introduction to the principles of morals and legislation. New York, NY: Dover Publications. (Original work published 1789) [Google Scholar]
- Boyle T, Keegel T, Bull F, Heyworth J, & Fritschi L (2012). Physical activity and risks of proximal and distal colon cancers: A systematic review and meta-analysis. Journal of the National Cancer Institute, 104, 1548–1561. [DOI] [PubMed] [Google Scholar]
- Cabanac M (1971). Physiological role of pleasure. Science, 173, 1103–1107. doi: 10.1126/science.173.4002.1103 [DOI] [PubMed] [Google Scholar]
- Carlson SA, Fulton JE, Schoenborn CA, & Loustalot F (2010). Trend and prevalence estimates based on the 2008 Physical Activity Guidelines for Americans. American Journal of Preventive Medicine, 39, 305–313. doi: 10.1016/j.amepre.2010.06.006 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2008). Physical activity guidelines advisory committee report, 2008. Washington, DC: U.S. Department of Health and Human Services. Retrieved from https://www.cdc.gov/cancer/dcpc/prevention/policies_practices/physical_activity/guidelines.htm [Google Scholar]
- Conner M, Rhodes RE, Morris B, McEachan R, & Lawton R (2011). Changing exercise through targeting affective or cognitive attitudes. Psychology & Health, 26, 133–149. [DOI] [PubMed] [Google Scholar]
- DaSilva SG, Guidetti L, Buzzachera CF, Elsangedy HM, Krinski K, Krause MP, … Baldari C (2010). Age and physiological, perceptual, and affective responses during walking at a self-selected pace. Perceptual and Motor Skills, 111, 963–978. doi: 10.2466/06.10.13.PMS.111.6.963-978 [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK & American College of Sports Medicine. (2009). American College of Sports Medicine position stand: Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise, 41, 459–471. doi: 10.1249/MSS.0b013e3181949333 [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Hill JO, Jacobsen DJ, Potteiger J, Sullivan DK, Johnson SL, … Washburn RA (2003). Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: The Midwest Exercise Trial. Archives of Internal Medicine, 163, 1343–1350. doi: 10.1001/archinte.163.11.1343 [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Jacobsen DJ, Heelan KS, Seip R, & Smith S (2000). The effects of 18 months of intermittent vs. continuous exercise on aerobic capacity, body weight and composition, and metabolic fitness in previously sedentary, moderately obese females. International Journal of Obesity and Related Metabolic Disorders, 24, 566–572. [DOI] [PubMed] [Google Scholar]
- Ekkekakis P (2003). Pleasure and displeasure from the body: Perspectives from exercise. Cognition and Emotion, 17, 213–239. [DOI] [PubMed] [Google Scholar]
- Ekkekakis P (2009). Let them roam free? Physiological and psychological evidence for the potential of self-selected exercise intensity in public health. Sports Medicine, 39, 857–888. doi: 10.2165/11315210-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Ekkekakis P, Hall EE, & Petruzzello SJ (2005a). Some like it vigorous: Measuring individual differences in the preference for and tolerance of exercise intensity. Journal of Sport and Exercise Psychology, 27, 350–374. doi: 10.1123/jsep.27.3.350 [DOI] [Google Scholar]
- Ekkekakis P, Hall EE, & Petruzzello SJ (2005b). Variation and homogeneity in affective responses to physical activity of varying intensities: An alternative perspective on dose-response based on evolutionary considerations. Journal of Sports Sciences, 23, 477–500. [DOI] [PubMed] [Google Scholar]
- Ekkekakis P, & Lind E (2006). Exercise does not feel the same when you are overweight: The impact of self-selected and imposed intensity on affect and exertion. International Journal of Obesity, 30, 652–660. doi: 10.1038/sj.ijo.0803052 [DOI] [PubMed] [Google Scholar]
- Ekkekakis P, Parfitt G, & Petruzzello SJ (2011). The pleasure and displeasure people feel when they exercise at different intensities. Sports Medicine, 41, 641–671. doi: 10.2165/11590680-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Focht BC, Knapp DJ, Gavin TP, Raedeke TD, & Hickner RC (2007). Affective and self-efficacy responses to acute aerobic exercise in sedentary older and younger adults. Journal of Aging and Physical Activity, 15, 123–138. doi: 10.1123/japa.15.2.123 [DOI] [PubMed] [Google Scholar]
- Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, & Lee IM, … American College of Sports Medicine. (2011). American College of Sports Medicine position stand: Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Medicine & Science in Sports & Exercise, 43, 1334–1359. doi: 10.1249/MSS.0b013e318213fefb [DOI] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, & Ogden CL (2017). Prevalence of obesity among adults and youth: United States, 2015-2016. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. [Google Scholar]
- Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U & Lancet Physical Activity Series Working Group. (2012). Global physical activity levels: Surveillance progress, pitfalls, and prospects. The Lancet, 380, 247–257. doi: 10.1016/S0140-6736(12)60646-1 [DOI] [PubMed] [Google Scholar]
- Hardy CJ, & Rejeski WJ (1989). Not what, but how one feels: The measurement of affect during exercise. Journal of Sport and Exercise Psychology, 11, 304–317. doi: 10.1123/jsep.11.3.304 [DOI] [Google Scholar]
- Jakicic JM, Clark K, Coleman E, Donnelly JE, Foreyt J, Melanson E, … American College of Sports Medicine. (2001). American College of Sports Medicine position stand: Appropriate intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise, 33, 2145–2156. [DOI] [PubMed] [Google Scholar]
- Kahneman D, Wakker PP, & Sarin R (1997). Back to Bentham? Explorations of experienced utility. Quarterly Journal of Economics, 112, 375–405. doi: 10.1162/003355397555235 [DOI] [Google Scholar]
- Kiviniemi MT, Voss-Humke AM, & Seifert AL (2007). How do I feel about the behavior? The interplay of affective associations with behaviors and cognitive beliefs as influences on physical activity behavior. Health Psychology, 26, 152–158. [DOI] [PubMed] [Google Scholar]
- Kwan BM, & Bryan AD (2010). Affective response to exercise as a component of exercise motivation: Attitudes, norms, self-efficacy, and temporal stability of intentions. Psychology of Sport and Exercise, 11, 71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HH, Emerson JA, & Williams DM (2016). The exercise-affect-adherence pathway: An evolutionary perspective. Frontiers in Psychology, 7, 1285. doi: 10.3389/fpsyg.2016.01285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus BH, Lewis BA, Williams DM, Dunsiger S, Jakicic JM, Whiteley JA, … Parisi AF (2007). A comparison of Internet and print-based physical activity interventions. Archives of Internal Medicine, 167, 944–949. doi: 10.1001/archinte.167.9.944 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Napolitano MA, King AC, Lewis BA, Whiteley JA, Albrecht A, … Papandonatos GD (2007). Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychology, 26, 401–409. doi: 10.1037/0278-6133.26.4.401 [DOI] [PubMed] [Google Scholar]
- Marcus BH, Williams DM, Dubbert PM, Sallis JF, King AC, Yancey AK, … Interdisciplinary Working Group on Quality of Care and Outcomes Research. (2006). Physical activity intervention studies: What we know and what we need to know: A scientific statement from the American Heart Association Council on nutrition, physical activity, and metabolism (subcommittee on physical activity); council on cardiovascular disease in the young; and the interdisciplinary working group on quality of care and outcomes research. Circulation, 114, 2739–2752. doi: 10.1161/CIRCULATIONAHA.106.179683 [DOI] [PubMed] [Google Scholar]
- Monninkhof EM, Elias SG, Vlems FA, van der Tweel I, Schuit AJ, Voskuil DW, … van Leeuwen FE (2007). Physical activity and breast cancer: A systematic review. Epidemiology, 18, 137–157. [DOI] [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, … Castaneda-Sceppa C (2007). Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation, 116, 1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650 [DOI] [PubMed] [Google Scholar]
- Parfitt G, Rose EA, & Burgess WM (2006). The psychological and physiological responses of sedentary individuals to prescribed and preferred intensity exercise. British Journal of Health Psychology, 11, 39–53. doi: 10.1348/135910705X43606 [DOI] [PubMed] [Google Scholar]
- Rhodes RE, Courneya KS, Blanchard CM, & Plotnikoff RC (2007). Prediction of leisure-time walking: An integration of social cognitive, perceived environmental, and personality factors. International Journal of Behavioral Nutrition and Physical Activity, 4(1), Article 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, Fiala B, & Conner M (2009). A review and meta-analysis of affective judgments and physical activity in adult populations. Annals of Behavioral Medicine, 38, 180–204. [DOI] [PubMed] [Google Scholar]
- Rhodes RE, & Kates A (2015). Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Annals of Behavioral Medicine, 49, 715–731. doi: 10.1007/s12160-015-9704-5 [DOI] [PubMed] [Google Scholar]
- Rose EA, & Parfitt G (2007). A quantitative analysis and qualitative explanation of the individual differences in affective responses to prescribed and self-selected exercise intensities. Journal of Sport & Exercise Psychology, 29, 281–309. [DOI] [PubMed] [Google Scholar]
- Rose E, & Parfitt G (2012). Exercise experience influences affective and motivational outcomes of prescribed and self-selected intensity exercise. Scandinavian Journal of Medicine & Science in Sports, 22, 265–277. [DOI] [PubMed] [Google Scholar]
- Ross R (2003). Does exercise without weight loss improve insulin sensitivity? Diabetes Care, 26, 944–945. [DOI] [PubMed] [Google Scholar]
- Royall PS, Troiano RP, Johnson MA, Kohl HW III., & Fulton JE (2008). Physical activity guidelines for Americans. Washington, DC. [Google Scholar]
- Russell JA (1980). A circumplex model of affect. Journal of Personality and Social Psychology, 39, 1161–1178. doi: 10.1037/h0077714 [DOI] [PubMed] [Google Scholar]
- Schneider M, Dunn A, & Cooper D (2009). Affect, exercise, and physical activity among healthy adolescents. Journal of Sport and Exercise Psychology, 31, 706–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson WR, Pescatello LS, & Gordon NF (2010). ACSM’s guidelines for exercise testing and prescription (Vol. 8). Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise, 40, 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Waller K, Kaprio J, & Kujala U (2008). Associations between long-term physical activity, waist circumference and weight gain: A 30-year longitudinal twin study. International Journal of Obesity, 32, 353–361. doi: 10.1038/sj.ijo.0803692 [DOI] [PubMed] [Google Scholar]
- Warburton DE, Nicol CW, & Bredin SS (2006). Health benefits of physical activity: The evidence. Canadian Medical Association Journal, 174, 801–809. doi: 10.1503/cmaj.051351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM (2008). Exercise, affect, and adherence: An integrated model and a case for self-paced exercise. Journal of Sport and Exercise Psychology, 30, 471–496. doi: 10.1123/jsep.30.5.471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM (2018). Psychological hedonism, hedonic motivation, and health-related behavior. In Williams DM, Rhodes RE, & Conner MT (Eds.), Affective determinants of health behavior (pp. 204–234). New York, NY: Oxford University Press. [Google Scholar]
- Williams DM, Dunsiger S, Ciccolo JT, Lewis BA, Albrecht AE, & Marcus BH (2008). Acute affective response to a moderate-intensity exercise stimulus predicts physical activity participation 6 and 12 months later. Psychology of Sport and Exercise, 9, 231–245. doi: 10.1016/j.psychsport.2007.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM, Dunsiger S, Emerson JA, Gwaltney CJ, Monti PM, & Miranda R Jr. (2016). Self-paced exercise, affective response, and exercise adherence: A preliminary investigation using ecological momentary assessment. Journal of Sport and Exercise Psychology, 38, 282–291. doi: 10.1123/jsep.2015-0232 [DOI] [PubMed] [Google Scholar]
- Williams DM, Dunsiger S, Jennings EG, & Marcus BH (2012). Does affective valence during and immediately following a 10-min walk predict concurrent and future physical activity? Annals of Behavioral Medicine, 44, 43–51. doi: 10.1007/s12160-012-9362-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM, Dunsiger S, Miranda R Jr., Gwaltney CJ, Emerson JA, Monti PM, & Parisi AF (2015). Recommending self-paced exercise among overweight and obese adults: A randomized pilot study. Annals of Behavioral Medicine, 49, 280–285. doi: 10.1007/s12160-014-9642-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM, & Marcus BH (2012). Theorecital Approaces to Exercise Promotion. The Oxford Handbook of Exercise Psychology, 241–241. [Google Scholar]
- Williams DM, Papandonatos GD, Jennings EG, Napolitano MA, Lewis BA, Whiteley JA, … Marcus BH (2011). Does tailoring on additional theoretical constructs enhance the efficacy of a print-based physical activity promotion intervention? Health Psychology, 30, 432–441. doi: 10.1037/a0023084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DM, Rhodes RE, & Conner MT (2018). Affective Determinants of Health Behavior. New York, NY: Oxford University Press. [Google Scholar]
- World Health Organization. (2010). Global recommendations on physical activity for health. Author. Retrieved from http://www.who.int/dietphysicalactivity/factsheet_adults/en/ [PubMed] [Google Scholar]
- Young DR, Jerome GJ, Chen C, Laferriere D, & Vollmer WM (2009). Peer reviewed: Patterns of physical activity among overweight and obese adults. Preventing Chronic Disease, 6(3), A90. [PMC free article] [PubMed] [Google Scholar]


