Abstract
Background
Patients undergoing bariatric surgery have high rates of psychiatric comorbidity, which may increase their vulnerability to COVID-19-related mental health distress. Exacerbation of mental health distress and disordered eating could have significant negative effects on long-term weight management and quality of life for these patients if untreated.
Objective
To determine the efficacy of a telephone-based cognitive behavioral therapy (Tele-CBT) intervention in improving depressive, anxiety, and disordered eating symptoms during COVID-19.
Methods
Participants were recruited as part of a larger randomized controlled trial study (clinicaltrials.gov ID: NCT03315247) between March 2020 and March 2021 and randomized 1:1 to receive Tele-CBT or standard bariatric care. Outcomes of Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), Emotional Eating Scale (EES), and Binge Eating Scale (BES) were measured at baseline, immediately post-intervention, and 3 months post-intervention. Linear mixed models were used to test the effect of intervention group, time, and group-by-time interaction for each outcome.
Results
Eighty-one patients were included in the intention-to-treat analysis. Mean (SD) age of participants was 47.68 (9.36) years and 80.2% were female. There were significant group-by-time interactions for all outcomes and significant differences between groups across time. There were significant decreases in mean GAD-7 (p = 0.001), PHQ-9 (p < 0.001), EES-Total (p = 0.001), EES-Anger (p = 0.003), EES-Anxiety (p < 0.001), EES-Depression (p < 0.001), and BES (p = 0.002) scores for the Tele-CBT group at post-intervention and follow-up when compared to baseline and the control group.
Conclusion
Tele-CBT is a feasible and effective treatment for improving psychological distress and disordered eating among post-operative bariatric surgery patients during the COVID-19 pandemic.
Graphical abstract
Keywords: Discipline and resistance, Online compulsory education, Foucault, Covid-19, China
Introduction
The SARS-CoV-2 coronavirus disease (COVID-19) pandemic has caused over 4 million deaths globally and resulted in significant distress, social disruption, and economic burden worldwide [1, 2]. Although studies comparing general population mental health outcomes before and during the COVID-19 pandemic have not conclusively shown a significant difference to date, studies have identified high-risk patient populations experiencing COVID-19 mental health distress, such as patients with chronic or pre-existing medical conditions, including obesity [3, 4]. COVID-19 lockdowns have further resulted in worsening mental health, distress, and eating behaviors for patients living with obesity [5]. In addition, the high rates of COVID-19 mental health distress and eating-related difficulties have also been associated with worse weight loss outcomes in patients with obesity, including patients who underwent bariatric surgery [6–8]. As a result, patients with obesity have experienced profound psychosocial burden secondary to COVID-19 which has compromised obesity management and weight loss outcomes [6, 9].
Patients undergoing bariatric surgery have high rates of psychiatric comorbidity, which may increase patients’ vulnerability to COVID-19-related psychological distress and its negative impact on coping and behavior change after bariatric surgery. Approximately 55 to 70% of bariatric surgery patients have a lifetime history of psychiatric illness consisting mainly of depressive, anxiety, and binge eating disorders, which could increase patients’ vulnerability to mental health complications during COVID-19 [10–12]. Moreover, patients experiencing disordered eating (e.g., binge eating symptoms) beyond the first year after bariatric surgery are at increased risk of poorer weight loss and mental quality of life outcomes [13–15]. Beyond the second year following bariatric surgery, patients may be at increased risk of developing depression, which has been associated with weight recidivism and impaired quality of life [15, 16]. During COVID-19, post-operative bariatric surgery patients reported challenges with eating behaviors, specifically difficulty following their recommended diet, increased hunger, increased impulse to eat, and increased snacking behavior [17]. Studies suggest that poor dietary adherence and disordered eating are associated with anxiety, depressive, and stress symptoms secondary to the pandemic [17–19]. Data from a qualitative study of post-operative bariatric surgery patients also identified increasing anxiety with rising COVID-19 case numbers and dysregulated eating patterns in response to increased emotional distress [20]. Therefore, COVID-19 mental health distress and disordered eating could have significant negative effects on long-term weight management and quality of life for bariatric surgery patients if untreated.
The literature on psychosocial interventions to support patients living with obesity during COVID-19 remains limited, despite emerging rapid and systematic reviews. Soklaridis and colleagues conducted a rapid review of mental health interventions and supports during COVID-19 and identified some preliminary evidence from past pandemics for cognitive behavioral therapy (CBT), progressive muscle relaxation, and an internet-based self-help intervention [21]. A recent living systematic review of randomized controlled trials identified well-designed trials providing evidence for self-guided internet-based CBT and a lay-person supportive phone intervention to improve mental health distress [22]. These reviews underscore the importance of accessible and scalable interventions to support patients’ self-management and mental health in the context of physical distancing, self-isolation, and travel restrictions during the COVID-19 pandemic. Despite this preliminary evidence for COVID-19 mental health interventions, these reviews did not identify any mental health interventions that specifically addressed pandemic-related psychological distress or disordered eating in patients with obesity.
The COVID-19 pandemic offers a unique opportunity to redefine psychosocial care and treatment delivery for bariatric surgery patients mainly through virtual care [23]. Qualitative interviews of post-operative bariatric surgery patients during COVID-19 have underscored the importance of having access to psychosocial support via virtual care (including telemedicine and telephone) during the COVID-19 pandemic [20]. Moreover, Messiah et al. conducted a systematic review of eHealth strategies for metabolic and bariatric surgery and identified several studies describing mobile, virtual (remote), and online-based treatments for patients; however, well-designed studies examining the effectiveness of these interventions are lacking [24]. Although COVID-19 has provided an opportunity to accelerate implementation of virtually delivered psychosocial treatments in bariatric surgery care, we could not identify any research examining the effectiveness of virtually delivered psychosocial interventions to treat COVID-19 mental health distress or eating psychopathology.
Given the lack of research on the efficacy of COVID-19 mental health interventions to support patients after bariatric surgery, this randomized controlled trial aimed to evaluate the efficacy of a telephone-based cognitive behavioral therapy (Tele-CBT) intervention in improving depressive, anxiety, and disordered eating symptoms during COVID-19 in patients who were 1-year post-bariatric surgery, a period that has been recommended as an optimal time for psychosocial intervention [25, 26]. This Tele-CBT intervention has previously demonstrated efficacy in improving psychological distress and disordered eating symptoms before and after surgery [27–30]. Based on these initial studies, we hypothesized that patients in the Tele-CBT group would report significant reductions in anxiety, depressive, emotional eating, and binge eating symptoms immediately following the intervention compared to the control group, and would remain significantly lower at 3-month follow-up.
Methods
Study Setting
Patients were recruited from the University Health Network Bariatric Surgery Program (UHN-BSP), the Humber River Hospital Bariatric Surgery Program (HRH-BSP), and The Ottawa Hospital Weight Management Clinic (TOH-WMC) between March 2020 and March 2021 as part of a larger multisite randomized controlled trial (NCT03315247). We included patients recruited from the larger RCT until March 2021 given the 2-month duration of the intervention and significant changes to public health restrictions in June 2021 as a result of COVID-19 re-opening.
This study was approved by the University Health Network Research Ethics Board in Toronto, Canada. All patients provided their informed consent for inclusion before they participated in the study. To be accepted into the UHN-BSP, HRH-BSP, or TOH-WMC, patients are required to be 18 years or older with a pre-operative body mass index (BMI) of ≥ 40 kg/m2 or ≥ 35 kg/m2 with at least one obesity-related comorbidity. Eligibility criteria to participate in the study included receiving bariatric surgery 1 year ago, being fluent in English, and having access to a telephone and to a computer with Internet connection for questionnaire completion. Exclusion criteria included poorly controlled psychiatric illness that would impede a patient’s ability to engage in the Tele-CBT sessions (e.g., psychosis) or active suicidal ideation. Patients received a Roux-en-Y gastric bypass unless a sleeve gastrectomy was surgically indicated (e.g., if there was a history of previous abdominal surgeries resulting in extensive adhesions and/or distorted anatomy).
Study Procedures
All patients who were invited to participate following screening completed a series of questionnaires at baseline using Qualtrics survey software (Provo, UT). All patients were between 12 and 14 months post-surgery when completing the baseline questionnaires. Upon completion, participants were randomized 1:1 to either the Tele-CBT group or the control group using Randi, an in-house built randomization program. Randomization was stratified by site. Those randomized to the control group received standard bariatric care which included symptom monitoring and care navigation (i.e., if patients were flagged to have scored above clinical cutoff for any of the questionnaire measures, or if they requested additional support, they were directed back to the clinical care team or relevant community resources for further care), whereas those randomized to the Tele-CBT group received the intervention described below. All participants were asked to complete questionnaires at post-intervention and follow-up. The total time interval between the baseline and post-intervention questionnaire was 10 weeks, and the total time interval between the baseline and follow-up questionnaire was 24 weeks.
The full Tele-CBT protocol has been detailed previously [28, 30, 31]. In brief, the intervention consisted of six weekly 1-h sessions that were scheduled at a time convenient for the participant, and a seventh 1-h “booster” session was delivered 1 month after the sixth session. These sessions were conducted by three doctoral students in clinical psychology with experience in the assessment and treatment of bariatric surgery patients and they received clinical supervision from the last author. The Tele-CBT intervention is tailored to the needs of post-operative bariatric surgery patients and is informed by a personalized cognitive behavioral model of overeating and obesity. Themes and topics discussed during the sessions include scheduling healthy meals and snacks at regular time intervals, planning pleasurable activities as an alternative to overeating, identifying and planning for difficult eating scenarios, and reducing vulnerability to overeating by challenging negative thoughts and solving problems. Given that the province in which this research study took place either had stay-at-home orders or severe restrictions in place to reduce the spread of COVID-19 for the duration of the study, the sessions were tailored to address COVID-related concerns that patients raised during the sessions. For example, patients who were having difficulty maintaining a consistent schedule when they shifted to working from home could be encouraged to adopt a normalized eating schedule, schedule regular activities, and set boundaries between their work and personal time. Patients experiencing low mood and/or social isolation could be encouraged to maintain a consistent schedule, plan pleasurable and mastery activities, and reach out to others. Patients experiencing anxiety could be encouraged to engage in self-care activities and the clinician would help them to challenge their negative thoughts (e.g., changing catastrophic thoughts into more adaptive ones) and use problem-solving if a problem within their control was contributing to their anxiety. The clinician also highlighted how each of the strategies could be applied to various issues a patient may be experiencing. For example, scheduling pleasurable activities can help to improve mood and social connection, and distract from urges to binge eat. Challenging negative thoughts can help reduce vulnerability to overeating and improve mood and anxiety. Participants completed homework between sessions (e.g., worksheets such as food records, thought records, problem-solving skills), and implemented skills that were taught during the sessions (e.g., engaging in self-care and pleasurable activities). The final “booster” session allowed for participants to check-in with their therapist to review the skills they learned, troubleshoot any issues that arose during the month prior, and develop a relapse prevention plan to help maintain the improvements made following surgery.
Study Measures
Psychological distress was assessed using the Generalized Anxiety Disorder 7-item scale (GAD-7) [32, 33] and the Patient Health Questionnaire 9-item scale (PHQ-9) [34]. The GAD-7 is a 7-item self-report questionnaire assessing anxiety symptoms on a scale ranging from 0 (not at all) to 3 (nearly every day). Scores on the GAD-7 range from 0 to 21 with mild, moderate, and severe levels of anxiety symptoms corresponding to cutoff scores of 5, 10, and 15, respectively. The PHQ-9 consists of 9 items assessing depressive symptoms on a scale ranging from 0 (not at all) to 3 (nearly every day). Scores on the PHQ-9 range from 0 to 27 with mild, moderate, moderately severe, and severe levels of depressive symptoms corresponding to cutoff scores of 5, 10, 15, and 20, respectively. Both measures have been used to assess treatment outcomes in bariatric surgery patient populations [15, 35, 36].
Eating psychopathology was assessed using the Emotional Eating Scale (EES) [37] and Binge Eating Scale (BES) [38, 39]. The EES is a 25-item self-report measure that assesses a person’s tendency to cope with negative affect through eating. The scale ranges from 0 (no desire) to 4 (overwhelming urge) and consists of questions that ask participants to rate the intensity of their urge to eat in response to 25 emotions. The EES is comprised of 3 subscales that reflect eating in response to anger/frustration, anxiety, and depression. The BES is a 16-item self-report measure designed specifically for use with individuals with obesity and assesses the presence of binge eating characteristics indicative of an eating disorder. Scores on the BES range from 0 to 46 with moderate and severe levels of binge eating corresponding to cutoff scores of 18 and 27, respectively.
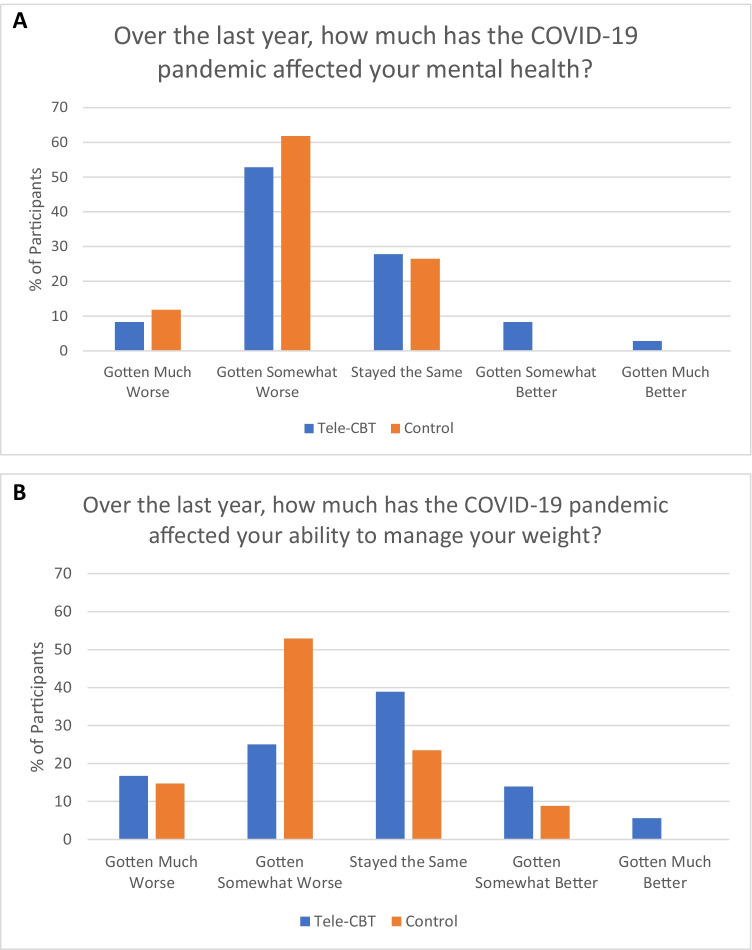
Impact of the COVID-19 pandemic on participants’ mental health and weight management ability was assessed using two 5-point Likert scales that ranged from 1 (my mental health/weight management ability has gotten much worse) to 5 (my mental health/weight management ability has gotten much better).
Statistical Analysis
All statistical analyses were performed using SPSS Statistics for Windows (Version 24.0; SPSS, IBM Corp., Armonk, NY) adhering to the “intention-to-treat” principle. Participant characteristics were summarized using descriptive statistics including means, standard deviations, frequencies, and proportions. The Shapiro–Wilk test was used to determine whether continuous outcomes were normally distributed. Non-normally distributed outcomes were log(x + 1) transformed for analysis. Linear mixed models with random intercepts were generated for each outcome variable with fixed effects of time (baseline, post-intervention, and follow-up), group (control and Tele-CBT), and time-by-group interaction. For reporting, the estimated means and standard errors from the mixed models were retransformed to the original units as exp(mean log) − 1 ± exp(mean log) × (exp(SE log) × 1). Mann–Whitney U tests were used to compare the effects of the COVID-19 pandemic on patients’ mental health and weight management ability between groups. A post hoc power analysis performed using G*Power (Version 3.1.9.2; Franz Faul, Universität Kiel, Germany) determined that our sample of 76 patients achieved 76% power to detect an effect size of 0.35 (two-sided test at α = 5%). Two-sided p values < 0.05 were considered statistically significant.
Results
Participant Flow and Characteristics
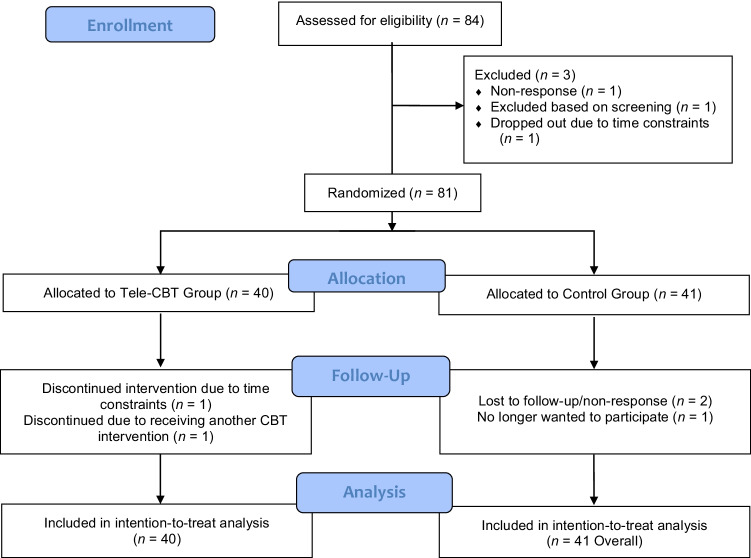
Participant flow for this study is detailed in the CONSORT diagram outlined in Fig. 1. Of the 84 patients who consented to participate in the study, 81 (96%) completed the baseline questionnaires and were randomized to either the Tele-CBT group (n = 40) or the control group (n = 41). Of the remaining participants, one did not respond to phone calls or emails, one dropped out due to time constraints, and one was excluded due to their screening results. One participant from the Tele-CBT group discontinued treatment due to time constraints and one participant discontinued due to starting CBT for eating and mood difficulties outside of this study. Two participants from the control group were lost to follow-up due to non-response and one participant was withdrawn as they no longer wanted to participate. Out of 81 randomized patients, a total of 76 (94%) patients completed all study procedures at 1.25 years post-surgery (henceforth referred to as “post-intervention”) and 67 (83%) patients completed all study procedures at 1.5 years post-surgery (henceforth referred to as “follow-up”). In the primary intention-to-treat analyses, all 81 randomized patients were included in the analyses. The mean (SD) age at baseline of participants was 47.68 (9.36) years and the majority were female (80.2%), Caucasian (77.8%), in a relationship (63%), completed college or university (61.7%), and employed full-time (65.4%) (Table 1). Majority of patients reported mild to no symptoms on the GAD-7, PHQ-9, and BES at baseline (Table 2).
Fig. 1.
CONSORT diagram of participant flow
Table 1.
Participant characteristics (n = 81)
| Characteristic | Mean (SD) or n (%) |
|---|---|
| Study site | |
| University Health Network Bariatric Surgery Program | 69 (85.2) |
| Humber River Hospital Bariatric Surgery Program | 2 (2.5) |
| The Ottawa Hospital Weight Management Clinic | 10 (12.3) |
| Age at baseline (years) | 47.68 (9.36) |
| Gender (female) | 65 (80.2%) |
| Race/Ethnicity | |
| Arab/West Asian | 3 (3.7%) |
| Black | 5 (6.2%) |
| Latin American | 1 (1.2%) |
| South Asian | 1 (1.2%) |
| South East Asian | 1 (1.2%) |
| White (Caucasian) | 63 (77.8%) |
| Other | 6 (8.6%) |
| Relationship status | |
| Married/Common-Law | 51 (63.0%) |
| Divorced/Separated | 13 (16.0%) |
| Single | 17 (21.0%) |
| Occupational status | |
| Full-time | 53 (65.4%) |
| Part-time | 8 (9.9%) |
| Retired | 8 (9.9%) |
| Disability | 5 (6.2%) |
| Unemployed | 6 (7.4%) |
| Education | |
| Some high school | 2 (2.5%) |
| High school graduate | 11 (13.6%) |
| Some college/university | 18 (22.2%) |
| College or university graduate | 50 (61.7%) |
Table 2.
Patient symptom severity scores at baseline for GAD-7, PHQ-9, and BES
| Baseline Symptom Severity Scores | n (%) |
|---|---|
| GAD-7 | |
| None (< 5) | 36 (44.4%) |
| Mild (5–9) | 28 (34.6%) |
| Moderate (10–14) | 16 (19.8%) |
| Severe (> 15) | 1 (1.2%) |
| PHQ-9 | |
| None (< 5) | 31 (38.3%) |
| Mild (5–9) | 30 (37.0%) |
| Moderate (10–14) | 13 (16.1%) |
| Moderately severe (15–19) | 7 (8.6%) |
| Severe (> 20) | 0 (0%) |
| BES | |
| Mild to none (0–17) | 47 (58.8) |
| Moderate (18–26) | 24 (30.0%) |
| Severe (> 27) | 9 (11.2%) |
Of the 70 patients who reported on the impact of COVID-19, a majority reported that their mental health had either gotten much worse (10%) or worse (57.1%) over the last year (Fig. 2A). Similarly, a slight majority reported that their ability to manage their weight had gotten much worse (15.7%) or worse (38.6%) over the last year, while a minority reported that their ability to manage their weight stayed the same (31.4%) or improved (14.3%) (Fig. 2B). There were no significant differences between treatment groups when comparing participants’ mental health and weight management ability scores (p = 0.19 and p = 0.09, respectively).
Fig. 2.
A Impact of the COVID-19 pandemic on participants’ mental health. B Impact of the COVID-19 pandemic on participants’ weight management
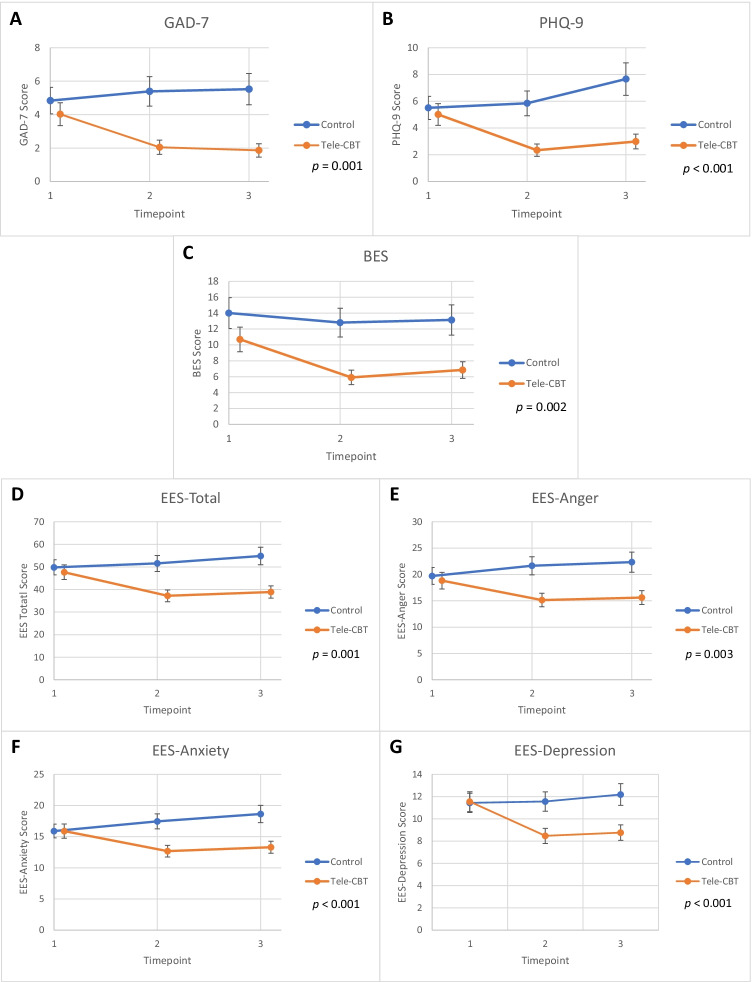
Comparison of Tele-CBT and Control Groups on Outcomes Across Time
Estimated mean scores and standard errors from linear mixed models for each clinical outcome by group at baseline, post-intervention, and follow-up are presented in Table 3 and Fig. 3. When examining whether there were significant group-by-time interactions for the outcomes, it was found that all outcomes showed a significant difference between groups across time. There was a significant decrease in mean GAD-7 (p = 0.001), PHQ-9 (p < 0.001), EES-Total (p = 0.001), EES-Anger (p = 0.003), EES-Anxiety (p < 0.001), EES-Depression (p < 0.001), and BES (p = 0.002) scores for the Tele-CBT group at post-intervention and follow-up when compared to baseline, whereas there was an increase in mean scores at post-intervention and follow-up when compared to baseline for these outcomes in the control group (Fig. 3). As a sensitivity analysis, we included site as a variable in all of our models, and site was not found to be significant. The group-by-time interaction for all models remained significant after controlling for site (data not shown).
Table 3.
Estimated means ± standard errors for clinical variables between Tele-CBT and Control groups at baseline, post-intervention, and 3-month follow-up
| Measure | Baseline | Post-intervention | Follow-up | |||
|---|---|---|---|---|---|---|
| Tele-CBT mean (SE) | Control mean (SE) | Tele-CBT mean (SE) | Control mean (SE) | Tele-CBT mean (SE) | Control mean (SE) | |
| N = 40 | N = 41 | N = 38 | N = 38 | N = 37 | N = 30 | |
| GAD-7 | 4.02 (0.69) | 4.84 (0.79) | 2.05 (0.43) | 5.39 (0.88) | 1.86 (0.40) | 5.52 (0.94) |
| PHQ-9 | 5.01 (0.81) | 5.50 (0.87) | 2.34 (0.46) | 5.84 (0.93) | 2.99 (0.55) | 7.65 (1.21) |
| BES | 10.69 (1.54) | 14.01 (1.95) | 5.91 (0.92) | 12.80 (1.81) | 6.85 (1.04) | 13.14 (1.90) |
| EES-Total | 47.67 (3.22) | 49.81 (3.36) | 37.521 (2.61) | 51.56 (3.53) | 38.88 (2.72) | 54.86 (3.87) |
| EES-Anger | 18.67 (1.47) | 20.714 (1.56) | 15.01 (1.21) | 21.92 (1.74) | 15.43 (1.24) | 22.381 (1.78) |
| EES-Anxiety | 15.83 (1.04) | 15.93 (1.05) | 12.59 (0.85) | 17.49 (1.16) | 13.25 (0.90) | 19.17 (1.31) |
| EES-Depression | 11.17 (0.82) | 11.74 (0.84) | 8.30 (0.63) | 11.74 (0.86) | 8.59 (0.65) | 12.57 (0.94) |
GAD-7, Generalized Anxiety Disorders 7-item scale; PHQ-9, Patient Health Questionnaire 9-item scale; EES-Total, Emotional Eating Scale total score; EES-Anger, Emotional Eating Scale – Anger subscale; EES-Anxiety, Emotional Eating Scale – Anxiety subscale; EES-Depression, Emotional Eating Scale – Depression subscale; BES, Binge Eating Scale
All outcomes were non-normally distributed and log(x + 1) transformed for analysis. For reporting, the estimated means and standard errors from the mixed models were retransformed to the original units as exp(mean log) − 1 ± exp(mean log) × (exp(SE log) − 1)
Fig. 3.
Estimated mean outcomes (± standard errors) between the Tele-CBT and control groups over time. Timepoints 1, 2, and 3 refer to baseline, post-intervention, and 3-month follow-up, respectively. p values refer to the time-by-group interaction. A GAD-7: Generalized Anxiety Disorders 7-item scale; B PHQ-9: Patient Health Questionnaire 9-item scale; C BES: Binge Eating Scale; D EES-Total: Emotional Eating Scale total score; E EES-Anger: Emotional Eating Scale – Anger subscale; F EES-Anxiety: Emotional Eating Scale – Anxiety subscale; G EES-Depression: Emotional Eating Scale – Depression subscale
Discussion
The current study sought to examine whether a brief and accessible telephone-based CBT intervention would improve psychological distress and eating psychopathology among post-operative bariatric surgery patients during the COVID-19 pandemic. Over half of our participants indicated that they experienced distress and difficulties managing their weight over the last year. This finding aligns with the results of a survey of 800 bariatric patients in which 75% of patients reported feeling anxious about their health during the pandemic, 60% reduced their exercise, 35% changed their eating habits, and 30% gained weight. [40].
One year post-surgery has been identified as a critical period when weight trajectories diverge, and initial improvements in health-related quality of life particularly within the mental health domain begin to decline within 2 years following surgery [41–43]; thus, psychosocial interventions are recommended early in the post-operative period to support the development of coping skills to maintain long-term improvements following surgery [25, 26]. The COVID-19 pandemic resulted in the closure or reduced capacity of many bariatric surgery programs as staff were redeployed and resources were reallocated to other departments with urgent need, and as a result, most bariatric patients had limited access to bariatric care and psychosocial supports during a period of increased vulnerability to psychosocial distress, disordered eating, and weight regain. 44% of post-operative bariatric patients in the aforementioned survey reported that reduced access to bariatric care caused them health problems, and all participants reported that remote support is needed from a dietician and a psychologist [40].
The results of the current study suggest that Tele-CBT is efficacious in improving psychological distress and eating psychopathology among post-operative bariatric surgery patients during the COVID-19 pandemic. The group receiving Tele-CBT reported significant improvements in binge eating symptoms (44% reduction), emotional eating (22% reduction), depression (49% reduction), and anxiety (47% reduction) from pre- to post-intervention, and these improvements were sustained over the 3-month follow-up period. In contrast, the control group that received standard bariatric care did not report significant improvements in any of these variables over the same period. Whereas the mean scores on the BES, PHQ-9, and GAD-7 all fell within the non-clinical range at post-treatment in the Tele-CBT group, the control group reported mild depression and anxiety symptoms at post-treatment according to PHQ-9 and GAD-7 cutoffs. These findings further support the growing body of literature on the efficacy of Tele-CBT for bariatric surgery patients [27, 28, 30]. The treatment completion rate of 95% in the current study was higher than in previous Tele-CBT studies (ranging from 73.7 to 74.5%), suggesting that bariatric patients may have found the intervention to be especially useful when they otherwise had limited access to bariatric care and other psychosocial resources during COVID-19 restrictions.
The Tele-CBT treatment protocol contained several elements that may have been helpful in managing common challenges that arose during the pandemic. A survey examining the impact of COVID-19 stay-at-home orders among patients in an obesity program indicated that 84% felt depressed, 50% stockpiled food, 61% engaged in stress eating, and 48% reduced their exercise time [5]. The disruption in daily routines also resulted in erratic dietary patterns and frequent snacking for many people. The Tele-CBT protocol directly targets many of these issues by helping patients develop a normalized eating schedule consisting of 3 nutritious meals and 2–3 snacks consumed at consistent times in designated eating areas without other distractions such as work or television. Patients are also taught goal setting and problem-solving skills which could be used to brainstorm creative ways to engage in physical activity or to purchase and prepare nutritious food during COVID-restrictions. Additionally, patients are encouraged to engage in self-care and pleasurable activities to reduce their vulnerability to low mood and binge eating and are taught strategies to challenge maladaptive thoughts that may trigger stress eating episodes. Aside from the treatment-specific factors, it is also important to acknowledge that the social support provided during the telephone calls may have been impactful especially during COVID stay-at-home orders.
Given the potential for mental health distress to persist despite re-opening and improvement in COVID-19 pandemic cases, as well as the possibility of additional restrictions in response to COVID-19 variants of concern in the future, this study is highly relevant as it provides data on an efficacious virtual treatment for bariatric surgery patients. There is a paucity of data on psychosocial interventions to address mental health distress during COVID-19. A living systematic review identified 9 randomized controlled trials, 3 of which were designed specifically to address COVID-related mental health distress and were found to improve depression and anxiety among individuals with dysfunctional COVID-related worry, patients with an autoimmune condition, and homebound older adults, and the remainder of which examined standard interventions that were somewhat adapted for COVID-19 [22]. To our knowledge, the current study is the first to examine a psychosocial treatment for individuals living with obesity during the pandemic.
Some of the benefits of virtual care include increased convenience, increased access to treatment, less disruptive (e.g., require less time off from work), and less costly (e.g., no travel expenses) [44, 45]. There is also no risk of COVID-19 transmission between the patient and therapist, and no treatment disruptions if COVID restrictions require clinic closures or if the patient or therapist is required to self-isolate. Given some of the unique benefits of virtual psychosocial care, it will likely continue in some capacity post-COVID to extend the reach of treatment. For example, a hybrid model may be beneficial where the therapist meets the patient in person to develop a therapeutic alliance, orient them to treatment, and provide them with treatment resources (e.g., informational handouts and treatment worksheets), and then offer the option of virtual therapy to reduce patient burden and increase treatment retention. Such an approach may mitigate some of the challenges of virtual care while retaining the benefits.
Limitations and Future Directions
Strengths of the current study include the RCT design, virtual intervention, high treatment retention rate, and use of psychometrically sound outcome measures. Limitations include the short follow-up period and the modest sample size given that recruitment was limited to a 1-year period (March 2020 to March 2021) of strict public health measures prior to a phased approach to COVID-19 re-opening. It is noteworthy that although over half of patients reported that they experienced greater distress and difficulties managing their weight over the last year, the severity of anxiety, depression, and binge eating symptoms they reported on the GAD-7, PHQ-9, and BES was quite mild on average, even at baseline. It will be important to examine the efficacy of Tele-CBT in a sample of patients who score above clinical cutoffs on these measures given that the limited psychosocial resources available within bariatric programs are typically directed to those currently experiencing clinically significant distress. It would also be informative to examine whether the treatment is effective among patients in non-bariatric obesity programs. Finally, given the advances that have been made in videoconferencing platforms and the likelihood of virtual care continuing in some capacity post-pandemic, future research should compare the efficacy of a telephone vs. video intervention and explore patient experiences and preferences, as telephone-based interventions may lack potentially critical clinical information (e.g., assessing the patient via sight) and abilities (e.g., sharing material on the screen) when compared to a video intervention. It is important to note, however, that although it would be beneficial to study the impact of video visits, the greatest increase in virtual care visits in Canada during the COVID-19 pandemic was accounted for by the increase in telephone-based visits [46]. Development of an evidence-based hybrid approach of combining in-person and virtual sessions that optimizes the benefits of each modality while reducing the barriers to implementation is warranted [47, 48].
Conclusion
Given the increase in distress and obesogenic behaviors related to the COVID-19 pandemic, it is critical that patients have consistent access to psychosocial care. The rapid expansion of virtual care across bariatric programs provides opportunities to extend the reach of psychosocial care beyond the pandemic.23,47 The results of the current study suggest that Tele-CBT is a feasible and efficacious treatment for improving psychological distress and eating psychopathology among post-operative bariatric surgery patients.
Acknowledgements
We would like to thank our patients who engaged in this study during the COVID-19 pandemic and our University Health Network, Humber River Hospital and Ottawa Hospital Bariatric Surgery Teams who supported patient recruitment.
Funding
This study was funded by the Canadian Institutes of Health Research (Grant #317877).
Declarations
Ethics Approval and Consent to Participate
All procedures performed in this study were in accordance with the University Health Network Research Ethics Board in Toronto, Canada. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Key points
• The Tele-CBT group had a significant decrease in depressive and anxiety symptoms.
• The Tele-CBT group had a significant reduction in disordered eating symptoms.
• Improvements in the Tele-CBT group were sustained at 3-month follow-up.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
3/18/2022
A Correction to this paper has been published: 10.1007/s11695-022-06015-x
References
- 1.World Health Organization. WHO coronavirus disease (COVID-19) Dashboard. https://covid19.who.int/. Accessed July 20, 2021
- 2.World Health Organization. Impact of COVID-19 on people’s livelihoods, their health and our food systems: joint statement by ILO, FAO, IFAD and WHO. https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people%27s-livelihoodstheir-health-and-our-food-systems. Accessed July 20, 2021.
- 3.Sun Y, Wu Y, Bonardi O, et al. Effects of COVID-19 mental health interventions among community-based children, adolescents, and adults: a living systematic review of randomised controlled trials. medRxiv. 2021.
- 4.Messiah SE, Uppuluri M, Xie L, et al. Substance use, mental health, and weight-related behaviors during the COVID-19 pandemic among metabolic and bariatric surgery patients. Obes Surg. 2021;31(8):3738–3748. doi: 10.1007/s11695-021-05488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Almandoz JP, Xie L, Schellinger JN, et al. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin Obes. 2020;10(5):e12386. [DOI] [PMC free article] [PubMed]
- 6.Conceicao E, de Lourdes M, Ramalho S, Felix S, Pinto-Bastos A, Vaz AR. Eating behaviors and weight outcomes in bariatric surgery patients amidst COVID-19. Surg Obes Relat Dis. 2021;17(6):1165–1174. doi: 10.1016/j.soard.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borgatti AC, Schneider-Worthington CR, Stager LM, et al. The COVID-19 pandemic and weight management: effective behaviors and pandemic-specific risk factors. Obes Res Clin Pract. 2021. [DOI] [PMC free article] [PubMed]
- 8.Pellegrini M, Ponzo V, Rosato R, et al. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12(7). [DOI] [PMC free article] [PubMed]
- 9.Youssef A, Mylopoulos M, Maunder R, et al. Understanding bariatric patients’ experiences of self-management post-surgery: a qualitative study. Clin Obes. 2021:e12473. [DOI] [PubMed]
- 10.Mitchell JE, Selzer F, Kalarchian MA, et al. Psychopathology before surgery in the Longitudinal Assessment of Bariatric Surgery-3 (LABS-3) Psychosocial Study. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2012;8(5):533–541. doi: 10.1016/j.soard.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sockalingam S, Hawa R, Wnuk S, Strimas R, Kennedy S. Weight loss following roux-en-y gastric bypass surgery: a systematic review of psychosocial predictors. Curr Psych Rev. 2011;7(3):226–233. doi: 10.2174/157340011797183139. [DOI] [Google Scholar]
- 12.Heinberg LJ, Mitchell JE, Peat C, Steffen K. DSM 5 lifetime psychiatric diagnoses in two bariatric surgery programs. Obes Surg. 2021;31(6):2812–2816. doi: 10.1007/s11695-021-05236-w. [DOI] [PubMed] [Google Scholar]
- 13.Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016;49(12):1058–1067. doi: 10.1002/eat.22578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nasirzadeh Y, Kantarovich K, Wnuk S, et al. Binge eating, loss of control over eating, emotional eating, and night eating after bariatric surgery: results from the Toronto Bari-PSYCH cohort study. Obes Surg. 2018;28(7):2032–2039. doi: 10.1007/s11695-018-3137-8. [DOI] [PubMed] [Google Scholar]
- 15.Youssef A, Keown-Stoneman C, Maunder R, et al. Differences in physical and mental health-related quality of life outcomes 3 years after bariatric surgery: a group-based trajectory analysis. Surg Obes Relat Dis. 2020;16(11):1837–1849. doi: 10.1016/j.soard.2020.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell JE, King WC, Chen JY, et al. Course of depressive symptoms and treatment in the longitudinal assessment of bariatric surgery (LABS-2) study. Obesity (Silver Spring) 2014;22(8):1799–1806. doi: 10.1002/oby.20738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sisto A, Vicinanza F, Tuccinardi D, et al. The psychological impact of COVID-19 pandemic on patients included in a bariatric surgery program. Eat Weight Disord. 2020. [DOI] [PMC free article] [PubMed]
- 18.Ramalho SM, Trovisqueira A, de Lourdes M, et al. The impact of COVID-19 lockdown on disordered eating behaviors: the mediation role of psychological distress. Eat Weight Disord. 2021. [DOI] [PMC free article] [PubMed]
- 19.Felix S, de Lourdes M, Ribeiro I, et al. A preliminary study on the psychosocial impact of COVID-19 lockdown in post-bariatric surgery women: the importance of eating behavior, health care access, and social support. Curr Psychol. 2021:1–7. [DOI] [PMC free article] [PubMed]
- 20.Youssef A, Cassin SE, Wnuk S, Leung S, Jackson T, Sockalingam S. The impact of COVID-19 pandemic on bariatric patients’ self-management post-surgery. Appetite. 2021;162:105166. [DOI] [PMC free article] [PubMed]
- 21.Soklaridis S, Lin E, Lalani Y, Rodak T, Sockalingam S. Mental health interventions and supports during COVID- 19 and other medical pandemics: A rapid systematic review of the evidence. Gen Hosp Psychiatry. 2020;66:133–146. doi: 10.1016/j.genhosppsych.2020.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonardi O, Wang Y, Li K, et al. Effects of COVID-19 mental health interventions among community-based children, adolescents, and adults: a living systematic review of randomised controlled trials. medRxiv. 2021.
- 23.Sockalingam S, Leung SE, Cassin SE. The impact of coronavirus disease 2019 on bariatric surgery: redefining psychosocial care. Obesity (Silver Spring) 2020;28(6):1010–1012. doi: 10.1002/oby.22836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Messiah SE, Sacher PM, Yudkin J, et al. Application and effectiveness of eHealth strategies for metabolic and bariatric surgery patients: a systematic review. Digit Health. 2020;6:2055207619898987. doi: 10.1177/2055207619898987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalarchian MA, Marcus MD. Psychosocial interventions pre and post bariatric surgery. Eur Eat Disord Rev. 2015;23(6):457–462. doi: 10.1002/erv.2392. [DOI] [PubMed] [Google Scholar]
- 26.David LA, Sijercic I, Cassin SE. Preoperative and post-operative psychosocial interventions for bariatric surgery patients: a systematic review. Obes Rev. 2020;21(4):e12926. [DOI] [PubMed]
- 27.Sockalingam S, Cassin SE, Wnuk S, et al. A pilot study on telephone cognitive behavioral therapy for patients six-months post-bariatric surgery. Obes Surg. 2017;27(3):670–675. doi: 10.1007/s11695-016-2322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sockalingam S, Leung SE, Hawa R, et al. Telephone-based cognitive behavioural therapy for female patients 1-year post-bariatric surgery: a pilot study. Obes Res Clin Pract. 2019;13(5):499–504. doi: 10.1016/j.orcp.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Costa-Dookhan KA, Leung SE, Cassin SE, Sockalingam S. Psychosocial predictors of response to telephone-based cognitive behavioural therapy in bariatric surgery patients. Can J Diabetes. 2020;44(3):236–240. doi: 10.1016/j.jcjd.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 30.Cassin SE, Sockalingam S, Du C, Wnuk S, Hawa R, Parikh SV. A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav Res Ther. 2016;80:17–22. doi: 10.1016/j.brat.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cassin SE, Sockalingam S, Wnuk S, et al. Cognitive behavioral therapy for bariatric surgery patients: preliminary evidence for feasibility, acceptability, and effectiveness. Cogn Behav Pract. 2013;20(4):529–543. doi: 10.1016/j.cbpra.2012.10.002. [DOI] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cassin S, Sockalingam S, Hawa R, et al. Psychometric properties of the Patient Health Questionnaire (PHQ-9) as a depression screening tool for bariatric surgery candidates. Psychosomatics. 2013;54(4):352–358. doi: 10.1016/j.psym.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Sockalingam S, Hawa R, Wnuk S, et al. Psychosocial predictors of quality of life and weight loss two years after bariatric surgery: results from the Toronto Bari-PSYCH study. Gen Hosp Psychiatry. 2017;47:7–13. doi: 10.1016/j.genhosppsych.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 37.Arnow B, Kenardy J, Agras WS. The Emotional Eating Scale: the development of a measure to assess coping with negative affect by eating. Int J Eat Disord. 1995;18(1):79–90. doi: 10.1002/1098-108X(199507)18:1<79::AID-EAT2260180109>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 38.Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 39.Hood MM, Grupski AE, Hall BJ, Ivan I, Corsica J. Factor structure and predictive utility of the Binge Eating Scale in bariatric surgery candidates. Surg Obes Relat Dis. 2013;9(6):942–948. doi: 10.1016/j.soard.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Waledziak M, Rozanska-Waledziak A, Pedziwiatr M, et al. Bariatric surgery during COVID-19 pandemic from patients’ point of view-the results of a national survey. J Clin Med. 2020;9(6). [DOI] [PMC free article] [PubMed]
- 41.Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA. 2013;310(22):2416–2425. doi: 10.1001/jama.2013.280928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA Surg. 2018;153(5):427–434. doi: 10.1001/jamasurg.2017.5025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coulman KD, Blazeby JM. Health-related quality of life in bariatric and metabolic surgery. Curr Obes Rep. 2020;9:307–314. doi: 10.1007/s13679-020-00392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murphy R, Calugi S, Cooper Z, Dalle Grave R. Challenges and opportunities for enhanced cognitive behaviour therapy (CBT-E) in light of COVID-19. Cogn Behav Therap. 2020;13:e14. [DOI] [PMC free article] [PubMed]
- 45.Santiago VA, Cassin SE, Wnuk S, et al. “If you’re offered help, take it”: a qualitative study examining bariatric patients’ experience of telephone-based cognitive behavioural therapy. Clin Obes. 2021;11(2):e12431. [DOI] [PubMed]
- 46.Bhatia RS, Chu C, Pang A, Tadrous M, Stamenova V, Cram P. Virtual care use before and during the COVID-19 pandemic: a repeated cross-sectional study. CMAJ Open. 2021;9(1):E107–E114. doi: 10.9778/cmajo.20200311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strudwick G, Sockalingam S, Kassam I, et al. Digital interventions to support population mental health in Canada during the COVID-19 pandemic: rapid review. JMIR Ment Health. 2021;8(3):e26550. [DOI] [PMC free article] [PubMed]
- 48.Yeo C, Ahmed S, Oo AM, Koura A, Sanghvi K, Yeo D. COVID-19 and obesity-the management of pre- and post-bariatric patients amidst the COVID-19 pandemic. Obes Surg. 2020;30(9):3607–3609. doi: 10.1007/s11695-020-04670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]