Abstract
Familial hypercholesterolemia (FH) is an autosomal dominant condition that leads to significantly elevated low-density lipoprotein cholesterol (LDL-C) levels and an elevated risk for cardiovascular disease. Mipomersen is an antisense oligonucleotide inhibitor targeted to apolipoprotein B-100 (apoB-100) mRNA that is administered via subcutaneous injection. Once administered, mipomersen causes selective degradation of the apoB-100 mRNA and inhibition of protein translation. This ultimately results in substantial reductions in LDL-C and other lipoprotein levels. Mipomersen is approved for the treatment of homozygous FH. In this review, we discuss its mechanism, current evidence, limitations of use including adverse events, and impact on health-related quality of life.
Keywords: mipomersen, familial hypercholesterolemia, apolipoprotein B
Introduction
Familial hypercholesterolemia (FH) is a genetically inherited condition that leads to lifelong elevated levels of low-density lipoprotein cholesterol (LDL-C).1 The majority of FH is inherited in an autosomal co-dominant manner. Causal mutations arise from the LDL receptor (LDLR), apolipoprotein B (apoB), proprotein convertase subtilisin/kexin type 9 (PCSK9), and low-density lipoprotein receptor adaptor protein (LDLRAP) genes.2 FH exists in two states; heterozygous (more common), and homozygous.3 The prevalence of heterozygous FH is estimated at 1 in 200 to 1 in 500, while homozygous FH has an estimated prevalence of 1 in 160,000 to 1 in 1,000,000.1 Patients with FH, regardless of homozygous or heterozygous, are at a substantially increased risk of atherosclerotic cardiovascular disease (ASCVD), valvular heart disease including aortic stenosis, and cardiovascular mortality.1,4 FH is underrecognized and often remains undiagnosed until a cardiovascular event takes place. Early detection and intervention to reduce LDL-C levels is crucial to reduce the burden of ASCVD in individuals with FH.5
Patients with FH typically require aggressive lipid lowering therapy, often starting in childhood. While statins are the first line of medical therapy for patients with FH, multiple pharmacologic agents are often needed to adequately lower LDL-C in these patients. A growing number of additional pharmacologic agents can be used to lower LDL-C including ezetimibe, PCKS9 inhibitors, bempedoic acid, lomitapide, and mipomersen.6 In this review, we will discuss the use of mipomersen for the treatment of homozygous FH, current evidence, limitations, and impact on health-related quality of life.
Indication and Mechanism of Action
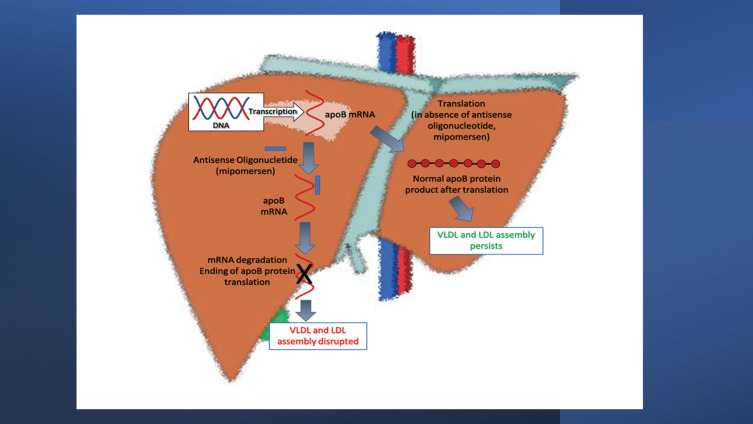
Mipomersen is a second-generation antisense oligonucleotide, a synthetically prepared strand of approximately 20 base pairs of deoxynucleotide sequences complementary to human apolipoprotein B (apoB)-100 mRNA, that is administered via subcutaneous injection.10 Once administered, mipomersen is transported to the liver where it binds to the apoB-100 mRNA causing its selective degradation and inhibition of protein translation. Clinically, the downstream effects of this result in decreased production of LDL-C, very low-density lipoprotein cholesterol (VLDL-C) and Lipoprotein(a) [Lp(a)].7 Figure 1 depicts the mechanism of action of mipomersen.
Figure 1.
Mipomersen mechanism of action.
Preclinical and Phase I Trials
Preclinical Studies
Preclinical studies were conducted on animal models and demonstrated reductions in apoB-100 mRNA in a dose- and time-dependent manner, as well as the total cholesterol (TC) and LDL-C.8 Additional studies on mouse models showed reductions in Lp(a) and atherosclerosis with the administration of mipomersen.9,10
Phase I Clinical Trials
A phase I randomized, double-blind, placebo-controlled dose-escalation study conducted by Kastelein et al studied the pharmacokinetic properties of mipomersen in 36 healthy volunteers with mild dyslipidemia.11 Participants were treated with an initial dose, ranging anywhere from 50 to 400 mg per week, and followed for a 4-week period. Dose-dependent reductions in plasma concentrations of apoB, LDL-C, and TC were observed, with maximal reductions observed in the 200 mg dose group (LDL-C reduction was 35% compared to baseline, apoB reduction was 50% from baseline). Overall, mipomersen was reasonably tolerated among the study participants with the most common adverse events being injection site reactions and asymptomatic elevations in liver transaminases. Injection site reactions, described as mild, painless erythema occurred in 21 of the 29 participants (72%) receiving the mipomersen. These typically occurred within 24 hours after administration of mipomersen and lasted for a median duration of 5 days. Elevations in serum alanine aminotransferase (ALT) levels occurred in 4 out of the 29 participants (14%) treated with mipomersen, with elevations exceeding 3 times the upper limit of normal occurring in 1 out of the 4 participants (3.4%).
Phase II and III Clinical Trials
Phase II Clinical Trials
Three randomized, double-blind, placebo-controlled phase II trials conducted by Akdim et al assessed the efficacy of mipomersen in patients with mild to moderate hypercholesterolemia as either monotherapy or on a background of other lipid lowering therapy including statin therapy. Across all three studies, significant dose-dependent reductions in LDL-C and apoB were observed in patients treated with mipomersen either alone or as an adjunct to stable statin or other lipid lowering therapy. Clinically significant reductions in LDL-C and apoB were noted at the 200 mg and 300 mg weekly dose.12–14 Across all three studies conducted by Akdim et al, 90% or more patients in the mipomersen arm developed injection site reactions, though these were described as mild to moderate in nature. Additionally, hepatotoxicity including elevations in transaminase levels ≥3 times the upper limit of normal occurred more frequently in patients treated with mipomersen as compared to placebo across all three trials [N = 10 (17%) vs N = 1 (7%); N = 4 (11%) vs N = 1 (13%); and N = 5 (13%) vs N = 0 (0%) in the mipomersen and placebo arms, respectively].
Another phase II clinical trial assessed the use of mipomersen in patients with hypercholesterolemia and atherosclerosis on lipid lowering therapy in addition to lipoprotein apheresis.15 In this prospective, randomized, controlled phase II trial, 15 patients with established atherosclerosis and an LDL-C ≥130 mg/dL on maximally tolerated lipid lowering therapy in addition to regular lipoprotein apheresis based on the German criteria were enrolled. In patients treated with mipomersen for >12 weeks pre-apheresis, LDL-C was reduced by 22.6% ± 17.0% compared to an increase of 1.6% ± 9.3% in the placebo arm (p = 0.006). A substantial number of patients in the mipomersen arm discontinued the drug prematurely; 3 discontinued the drug at <12 weeks due to side effects and an additional 4 patients discontinued it between 12 and 26 weeks due to severe injection site reactions and hepatotoxicity. While the effects of LDL-C reduction were promising, particularly across a varied background of treatments including lipoprotein apheresis, the tolerability of mipomersen was limited due to adverse effects limiting the scope of its use.
Phase III Clinical Trials
Three phase III trials were conducted in patients with moderate to severe hypercholesterolemia. In a randomized, double-blind, placebo-controlled, multiCenter trial conducted by McGowan et al assessed the use of mipomersen in adult patients (39 in the mipomersen arm vs 19 in the placebo arm) with severe hypercholesterolemia [LDL-C ≥7.8 mmol/L (301.16 mg/dL)] with or without the presence of coronary artery disease on a background of maximally tolerated lipid lowering therapy. Patients were randomized to the administration of 200 mg of mipomersen via weekly subcutaneous injection vs placebo and followed for 26 weeks. Findings in the mipomersen arm demonstrated reductions in LDL-C of 36% from baseline compared to a 13% increase in LDL-C levels in the placebo arm. Additionally, significant reductions were noted in apoB (36% reduction from baseline) and Lp(a) (33% reduction from baseline). No change was noted in high-density lipoprotein-cholesterol (HDL-C) levels. Reported adverse events were more frequent in the mipomersen arm compared with the placebo arm. Injection site reaction was the most common adverse event reported in both groups and occurred in 35 out of 39 patients in the mipomersen arm (90%) vs 6 out of 19 patients in the placebo arm (32%).16 Additionally, flu-like symptoms were more common in the mipomersen vs placebo arm (N = 18 (46%) vs N = 4 (21%)), respectively. Elevations in serum ALT and aspartate aminotransferase (AST) were noted in 21% and 13% of patients treated with mipomersen, respectively, vs 0% for both in the placebo arm. Furthermore, hepatic steatosis was noted in 5 patients treated with mipomersen (13%), but not noted in the placebo arm.
Another randomized, double-blind, placebo-controlled trial phase III study conducted by Stein et al studied the use of mipomersen in patients with heterozygous FH and coronary artery disease on a background of maximally tolerated lipid-lowering therapy including statins, ezetimibe, bile acid sequestrants, and niacin. Overall, 124 patients were enrolled in the study (83 in the mipomersen arm vs 41 in the placebo arm) and randomized to mipomersen 200 mg weekly administered via subcutaneous injections vs placebo. The primary endpoint was the percent change in LDL-C compared to baseline.17 The mean reduction in LDL-C at 26 weeks was 28%. Additional reductions were also noted in apoB, TC, and Lp(a) levels. Notable adverse events in this study included elevations in hepatic transaminases greater than 3 times the upper limit of normal that were more prevalent in the mipomersen arm (14.5% of patients). The greatest elevations in liver transaminases were associated with the greatest reductions in apoB levels. To further assess this, hepatic fat content at baseline and post treatment was measured. Hepatic fat content was increased compared to baseline in the mipomersen arm by 6.2% compared to decreased by 0.5% in the placebo arm, consistent with the hepatotoxic effects that were clinically observed with the use of mipomersen.
In another randomized, double-blind, placebo-controlled, multicenter trial, Thomas et al enrolled 157 patients (105 in the mipomersen arm vs 52 in the placebo arm) with LDL-C ≥100 mg/dl with, or at high risk for, coronary artery disease on background treatment with maximally tolerated lipid lowering therapy.18 Patients were randomized to treatment with 200 mg mipomersen via subcutaneous injection vs placebo for 26 weeks followed by a 24 week follow-up period. A significant reduction in LDL-C was noted in the mipomersen arm compared to the placebo arm (−36.9% vs −4.5% respectively). LDL-C <100 mg/dl was achieved in 76% of patients in the mipomersen arm (vs 38% in the placebo group). Reductions from baseline in apoB (38%) and Lp(a) (24%) in the mipomersen treatment arm. Once again, adverse events were more frequent in the mipomersen arm compared to the placebo arm (92.4% vs 80.8%). The most common adverse events in both groups were injection site reaction and flu-like symptoms. Elevation in transaminases and increased hepatic fat were also noted in this study and consistent with prior findings.18
Overall, clinical studies on mipomersen demonstrated its efficacy in reducing levels of apoB, LDL-C, triglycerides, and Lp(a) when compared with the placebo. However, adverse reactions, such as injection site reactions, elevations in liver transaminases and hepatic fat content were more frequently noted with mipomersen treatment.
Safety Concerns and Monitoring
Safety concerns specifically related to hepatotoxicity noted in the clinical trials led to the addition of a black box warning for serious risk of hepatotoxicity. Due to this, mipomersen is only available at specialty pharmacies through the Risk Evaluation and Mitigation Strategy (REMS) drug safety program in the United States. It is recommended that serum ALT, AST, alkaline phosphatase, and total bilirubin are measured prior to initiating treatment and be regularly monitored after its initiation. Mipomersen should be withheld if serum AST or ALT levels reach ≥3 times the upper limit of normal or if clinically significant liver toxicity is noted.19 A summary of the Phase I through III clinical trials and incidence of the adverse events related to the use of mipomersen vs placebo are detailed in Table 1.
Table 1.
Summary of Safety and Efficacy of Mipomersen Across Clinical Trials
| Study | Participant Characteristics | LDL-C Reduction from Baseline | Adverse Events |
|---|---|---|---|
| Phase I | |||
| Kastelein et al11 | 36 healthy volunteers with mild dyslipidemia (29 mipomersen arm, 7 placebo arm) | 35% |
ISRs: 72% mipomersen vs 0% placebo Transaminitis: 14% of patients treated with mipomersen |
| Flaim et al33 | 84 healthy volunteers (63 mipomersen arms, 21 placebo arm) | 9.5–21% |
ISR: 95–100% mipomersen vs 50% placebo FLS: <10% mipomersen |
| Phase II | |||
| Akdim et al12 | 74 patients with hypercholesterolemia on background statin therapy (59 mipomersen, 15 placebo arm) | 21–52% |
ISRs: 90% mipomersen vs 13% placebo Transaminitis: 17% mipomersen vs 7% placebo FLS: 25% mipomersen vs 7% placebo |
| Akdim et al13 | 44 patients with HeFH on background of lipid-lowering therapy (36 mipomersen arm, 8 placebo arm) | 21–34%** |
ISRs: 97% mipomersen vs 25% placebo Transaminitis: 11% mipomersen vs 13% placebo |
| Akdim et al14 | 50 patients with mild to moderate untreated hyperlipidemia (40 mipomersen arm, 10 placebo arm) | 7–71% |
ISRs: 100% mipomersen vs 60% placebo Transaminitis: 13% mipomersen vs 0% placebo FLS: 13% mipomersen vs 10% placebo |
| Waldmann et al.15 | 15 patients with atherosclerosis and LDL-C ≥130 mg/dL on maximally tolerated lipid lowering therapy and fulfilling the German criteria for lipoprotein apheresis. (11 mipomersen arm, 4 placebo arm) | 5.6–39.6% |
ISRs: 98% mipomersen arm* Transaminitis: 14% mipomersen arm* FLS: 65% mipomersen arm* |
| Visser et al34 | 33 subjects with hypercholesterolemia, statin intolerance and high risk for CVD (21 mipomersen arm, 12 placebo arm) | 47% |
ISR: 95% mipomersen vs 83% placebo Transaminitis: 81% mipomersen vs 25% placebo |
| Visser et al34 | 21 subjects with heterozygous FH and stable lipid lowering therapy (10 mipomersen arm, 11 placebo arm) | 22% |
ISR: 100% mipomersen vs 73% placebo Transaminitis (≥3x ULN): 0% mipomersen 0% placebo FLS: 70% mipomersen vs 18% placebo |
| Reeskamp et al.35 | 309 patients with severe or high risk HeFH on maximally tolerated LDL-lowering therapy (63 mipomersen arm, 21 placebo arm) | 18.8–21% |
Transaminitis (≥3x ULN): 21% mipomersen vs 1% placebo ISR or FLS leading to discontinuation: 17.6%-21.2% mipomersen vs 5.8% placebo |
| Phase III | |||
| Raal et al36 | 51 patients with HoFH on low fat diet and maximal medical therapy (34 mipomersen arm, 17 placebo arm) | 25% |
ISRs: 75% mipomersen vs 24% placebo, Transaminitis (≥3x ULN): 12% mipomersen vs 0% placebo FLS: 29% mipomersen vs 24% placebo |
| McGowan et al16 | 58 patients with severe hypercholesterolemia ± CHD on maximally tolerated lipid-lowering therapy (39 mipomersen arm, 19 placebo arm) | 36% |
ISRs: 90% mipomersen vs 32% placebo FLS: 46% mipomersen vs 21% placebo Transaminitis: ↑AST (13% mipomersen vs 0% placebo); ↑ALT (21% mipomersen vs 0% placebo) |
| Stein et al17 | 124 patients with HeFH and stable CAD on maximally tolerated statin (83 mipomersen arm, 41 placebo arm) | 28% |
ISRs: 93% mipomersen vs 42% placebo, Transaminitis (≥3x ULN): 14.5% mipomersen vs 2.4% placebo, FLSε: 49% mipomersen vs 32% placebo increased hepatic fat |
| Thomas et al18 | 157 individuals with baseline LDL-C ≥100 with or at high risk for CHD on maximally tolerated lipid- lowering therapy (105 mipomersen arm, 52 placebo arm) | 37% |
ISRs: 78% mipomersen vs 31% placebo Transaminitis: 31% mipomersen vs 14% placebo FLS: 34% mipomersen vs 21% placebo |
Abbreviations: ISRs, Injection site reactions; FLS, Flu-like symptoms; HeFH, Heterozygous Familial Hypercholesterolemia; HoFH, Homozygous Familial Hypercholesterolemia.
In December 2012, mipomersen was rejected for use by the European Medicines Agency due to concerns that a substantial proportion of patients had discontinued the medication within 2 years citing significant side effects. Furthermore, concerns regarding the long-term effects on liver transaminase elevation and hepatic steatosis were raised. In March 2013, a re-examination was conducted and due to concerns previously raised by the Committee for Medicinal Products for Human use not being addressed, it was not approved for use. However, mipomersen was approved for use in the United States by FDA in 2013 as an adjunct to lipid-lowering therapy for the treatment of homozygous FH.
Efficacy of Mipomersen and Related Adverse Events
A recent meta-analysis by Astaneh et al demonstrated that mipomersen significantly reduced LDL-C levels in patients with FH when compared with placebo [mean difference: −24.79, 95% CI (−30.15, −19.43), overall effect P value <0.00001].20 However, its use was associated with an incidence of injection site reactions of approximately 10% of patients. Patients receiving mipomersen were 2.56 (1.47–4.44) times more likely than those receiving the placebo to develop injection site reactions. Additional analyses from this study suggest the potential for hepatotoxicity via increased serum alanine transaminase levels >3 times upper limit of normal.20 These are important considerations when assessing tolerability of mipomersen.
Another meta-analysis by Fogacci et al evaluated the efficacy of mipomersen on LDL-C as well as additional lipid and lipoprotein parameters.21 Significant reductions were noted in LDL-C (WMD − 1.52, 95% CI − 1.85 to − 1.19; p < 0.001) and triglycerides (WMD –0.61, 95% CI − 0.76 to − 0.46, p < 0.001). While favorable effects of mipomersen were noted across lipid and lipoprotein parameters, this meta-analysis showed concerns with regard to adverse events that were consistently more prevalent in the treatment arm. Increased injection site reactions [odds ratio (OR) 11.41 95% CI 7.88 to 16.52, p < 0.001], hepatic steatosis (OR 4.96, 95% CI 1.99–12.39; p = 0.001), hepatic enzyme elevation (OR 3.61, 95% CI 2.09–6.24; p < 0.001) and flu-like symptoms (OR 2.02, 95% CI 1.45–2.81; p < 0.001) were noted in the mipomersen arm. Treatment with mipomersen resulted in increased discontinuation when compared to placebo (OR 3.02, 95% CI 1.96 to 4.65, p < 0.001) that was attributed to the adverse events associated with its administration. The favorable effects on the lipid profile must be weighed against the significant risk of adverse effects that have an impact on tolerability, adherence, and quality of life.
Potential strategies to mitigate the adverse events such as reduced dosing of mipomersen have also been explored. A double-blind trial compared three groups to assess efficacy and safety in heterozygous FH patients: mipomersen 200 mg once weekly (n = 104), mipomersen 70 mg thrice weekly (n = 102), and placebo (n = 103). Findings from the study demonstrated a reduction in the frequency of notable adverse effects with the 70 mg dose compared to the 200 mg dose including: flu-like symptoms (25.5% vs 42.3%), injection site pain (6.9% vs 12.5%), nausea (6.9% vs 8.7%), myalgias (4.9% vs 7.7%), pain in extremity (2.9% vs 4.8%), dizziness (2.9% vs 7.7%), and hepatic steatosis (8.8% vs 9.6%) in the reduced dose vs full dose arms, respectively. Importantly, the effect on apoB-containing lipoproteins in reduced dose arm compared with placebo was similar suggesting that the main benefit for the alternate dosing strategy of 70 mg thrice weekly would be to reduce adverse effects and improve tolerability and adherence.
Assessment of Quality of Life and Patient Reported Metrics
The diagnosis of FH alone can affect patient quality of life and overall wellbeing and several studies have looked at the impact of FH on quality of life. Mortensen et al conducted a study in which 10 patients with FH were interviewed via qualitative focus group interviews.22 Findings from the study demonstrated that the quality-of-life impact of FH appears to be related to the efficacy of treatment. Notably, individuals who were unable to reach treatment targets expressed more concern about the risk of ASCVD and premature cardiovascular death and this had a greater impact on their quality of life. Results from the Spanish FH cohort study reported that cardiovascular disease, female gender, older age, depression, obesity, lower educational level, xanthomas, and lower physical activity were associated with a worse quality of life.23
Findings from other studies suggest that FH treatment modalities can affect a patient’s social and mental wellbeing. Findings from a nationwide registry of homozygous FH in Turkey (A-HIT1) showed that surveyed patients with homozygous FH had higher rates of depression attributed to both the diagnosis of homozygous FH and due to drawbacks from the treatment.24 Patients undergoing the extracorporeal lipid removal procedure, apheresis, frequently reported physical, aesthetic, and psychological problems. Additionally, younger age at diagnosis was associated with better quality of life compared to older age.24 A study of patients who completed a trial with lovastatin, cholestyramine, probucol, or omega-3 fatty acids, reported that almost a quarter had abdominal and nervous system adverse events after 5.5 years, and approximately 25% reported diet and medication concerns.25 All of the events noted may alter the quality of life of patients.
While mortality benefit is a major criterion in assessing pharmacotherapy, selection of therapeutic agents needs to be made using shared decision-making with the patient. Adverse events, costs, and impact on quality of life are important parameters to consider when considering initiation of pharmacotherapy. Clinical trials have consistently demonstrated that injection site reactions, flu-like symptoms, and hepatotoxicity are the most common adverse events with mipomersen. A robust number of patients treated with mipomersen in clinical practice have reported the development of large erythematous injection site reactions that are cosmetically debilitating and have experienced flu-like symptoms after each injection lasting up to 24 hours in duration. Given the weekly dosing schedule of mipomersen, these flu-like symptoms can have a substantial impact on quality of life affecting patients social and emotional wellbeing in addition to their performance at work and other essential activities.
To put quality of life effects into perspective, mipomersen can be compared to another medication that is used in patients with homozygous FH, lomitapide. Lomitapide is an orally administered pharmacologic agent that is approved for use as an adjunct to a low-fat diet and other lipid lowering therapies in patients with homozygous FH. It is a microsomal triglyceride transfer protein inhibitor that prevents the assembly of apoB-containing lipoproteins in the liver and intestines. Clinical studies have demonstrated clinical efficacy of lomitapide with reductions in LDL-C levels ranging from 35% to 88%.26–29 Gastrointestinal adverse events including hepatic steatosis are most commonly reported with the use of lomitapide most of which were reportedly generally manageable but did require close monitoring of liver function. Notably, the oral formulation of this drug eliminates the injection site reactions that can be seen in over 70% of patients treated with mipomersen. While notable differences exist between mipomersen and lomitapide, the adverse effects of lomitapide are generally fewer and better tolerated than those of mipomersen.
Mipomersen faces the limitations of more frequent adverse events when compared to other lipid lowering agents and closer monitoring due to these adverse events, which add to the overall cost and inconvenience to patients thereby impacting quality of life.
Conclusion
While the clinical efficacy of mipomersen shows promise in theory, there are several notable limitations to its use. Mipomersen has a very limited scope of use and is indicated for use only in patients with homozygous FH and marketing authorization was rejected by the European Medicines Agency, further limiting its use in one of the largest international markets. Furthermore, the higher incidence of adverse events compared to other lipid lowering therapies have effects across several domains of wellbeing including physical health/limitations, psychological, social relationships, environment, emotional, treatment satisfaction, disease perception, among others.30–32 Beyond these limitations, frequent adverse events lead to the need for more intensive monitoring which are time, effort, and cost intensive. The clinical benefits must be judiciously weighed against the impact on quality of life when evaluating the use of mipomersen or any other pharmacologic agent.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Khera AV, Hegele RA. What is familial hypercholesterolemia, and why does it matter? Circulation. 2020;141(22):1760–1763. doi: 10.1161/CIRCULATIONAHA.120.046961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharifi M, Futema M, Nair D, Humphries SE. Genetic architecture of familial hypercholesterolaemia. Curr Cardiol Rep. 2017;19(5):44. doi: 10.1007/s11886-017-0848-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh S, Bittner V. Familial Hypercholesterolemia—Epidemiology, Diagnosis, and Screening. Curr Atheroscler Rep. 2015;17(2):3. doi: 10.1007/s11883-014-0482-5 [DOI] [PubMed] [Google Scholar]
- 4.Mundal L, Sarancic M, Ose L, et al. Mortality among patients with familial hypercholesterolemia: a registry based study in Norway, 19922010. J Am Heart Assoc. 2014;3(6):e001236. doi: 10.1161/JAHA.114.001236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alonso R, Mata P, Zambón D, Mata N, Fuentes-Jiménez F. Early diagnosis and treatment of familial hypercholesterolemia: improving patient outcomes. Expert Rev Cardiovasc Ther. 2013;11(3):327–342. doi: 10.1586/erc.13.7 [DOI] [PubMed] [Google Scholar]
- 6.Strilchuk L, Fogacci F, Cicero AF. Safety and tolerability of injectable lipid-lowering drugs: an update of clinical data. Expert Opin Drug Saf. 2019;18(7):611–621. doi: 10.1080/14740338.2019.1620730 [DOI] [PubMed] [Google Scholar]
- 7.Yu RZ, Gunawan R, Li Z, et al. No effect on QT intervals of mipomersen, a 2’-O-methoxyethyl modified antisense oligonucleotide targeting ApoB-100 mRNA, in a phase I dose escalation placebo-controlled study, and confirmed by a thorough QT (tQT) study, in healthy subjects. Eur J Clin Pharmacol. 2016;72(3):267–275. doi: 10.1007/s00228-015-1992-y [DOI] [PubMed] [Google Scholar]
- 8.Crooke RM, Graham MJ, Lemonidis KM, Whipple CP, Koo S, Perera RJ. An apolipoprotein B antisense oligonucleotide lowers LDL cholesterol in hyperlipidemic mice without causing hepatic steatosis. J Lipid Res. 2005;46(5):872–884. doi: 10.1194/jlr.M400492-JLR200 [DOI] [PubMed] [Google Scholar]
- 9.Merki E, Graham MJ, Mullick AE, et al. Antisense oligonucleotide directed to human apolipoprotein B-100 reduces lipoprotein(a) levels and oxidized phospholipids on human apolipoprotein B-100 particles in lipoprotein(a) transgenic mice. Circulation. 2008;118(7):743–753. doi: 10.1161/CIRCULATIONAHA.108.786822 [DOI] [PubMed] [Google Scholar]
- 10.Mullick AE, Fu W, Graham MJ, et al. Antisense oligonucleotide reduction of apoB-ameliorated atherosclerosis in LDL receptor-deficient mice. J Lipid Res. 2011;52(5):885–896. doi: 10.1194/jlr.M011791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastelein JJP, Wedel MK, Baker BF, et al. Potent reduction of apolipoprotein B and low-density lipoprotein cholesterol by short-term administration of an antisense inhibitor of apolipoprotein B. Circulation. 2006;114(16):1729–1735. doi: 10.1161/CIRCULATIONAHA.105.606442 [DOI] [PubMed] [Google Scholar]
- 12.Akdim F, Stroes ES, Sijbrands EJ, et al. Efficacy and safety of mipomersen, an antisense inhibitor of apolipoprotein B, in hypercholesterolemic subjects receiving stable statin therapy. J Am Coll Cardiol. 2010;55(15):1611–1618. doi: 10.1016/j.jacc.2009.11.069 [DOI] [PubMed] [Google Scholar]
- 13.Akdim F, Visser ME, Tribble DL, et al. Effect of mipomersen, an apolipoprotein B synthesis inhibitor, on low-density lipoprotein cholesterol in patients with familial hypercholesterolemia. Am J Cardiol. 2010;105(10):1413–1419. doi: 10.1016/j.amjcard.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 14.Akdim F, Tribble DL, Flaim JD, et al. Efficacy of apolipoprotein B synthesis inhibition in subjects with mild-to-moderate hyperlipidaemia. Eur Heart J. 2011;32(21):2650–2659. doi: 10.1093/eurheartj/ehr148 [DOI] [PubMed] [Google Scholar]
- 15.Waldmann E, Vogt A, Crispin A, Altenhofer J, Riks I, Parhofer KG. Effect of mipomersen on LDL-cholesterol in patients with severe LDL-hypercholesterolaemia and atherosclerosis treated by lipoprotein apheresis (The MICA-Study). Atherosclerosis. 2017;259:20–25. doi: 10.1016/j.atherosclerosis.2017.02.019 [DOI] [PubMed] [Google Scholar]
- 16.McGowan MP, Tardif JC, Ceska R, et al. Randomized, placebo-controlled trial of mipomersen in patients with severe hypercholesterolemia receiving maximally tolerated lipid-lowering therapy. PLoS One. 2012;7(11):e49006. doi: 10.1371/journal.pone.0049006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stein EA, Dufour R, Gagne C, et al. Apolipoprotein B synthesis inhibition with mipomersen in heterozygous familial hypercholesterolemia: results of a randomized, double-blind, placebo-controlled trial to assess efficacy and safety as add-on therapy in patients with coronary artery disease. Circulation. 2012;126(19):2283–2292. doi: 10.1161/CIRCULATIONAHA.112.104125 [DOI] [PubMed] [Google Scholar]
- 18.Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, Davidson M. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol. 2013;62(23):2178–2184. doi: 10.1016/j.jacc.2013.07.081 [DOI] [PubMed] [Google Scholar]
- 19.Genzyme. Highlights of Prescribing Information. 2020 [Google Scholar]
- 20.Astaneh B, Makhdami N, Astaneh V, Guyatt G. The effect of mipomersen in the management of patients with familial hypercholesterolemia: a systematic review and meta-analysis of clinical trials. J Cardiovascular Dev Dis. 2021;8(7):82. doi: 10.3390/jcdd8070082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fogacci F, Ferri N, Toth PP, Ruscica M, Corsini A, Cicero AFG. Efficacy and safety of mipomersen: a systematic review and meta-analysis of randomized clinical trials. Drugs. 2019;79(7):751–766. doi: 10.1007/s40265-019-01114-z [DOI] [PubMed] [Google Scholar]
- 22.Mortensen GL, Madsen I. Familial hypercholesterolemia reduces the quality of life of patients not reaching treatment targets. Dan Med J. 2016;1:543. [PubMed] [Google Scholar]
- 23.Mata N, Alonso R, Banegas JR, Zambón D, Brea A, Mata P. Quality of life in a cohort of familial hypercholesterolemia patients from the south of Europe. Eur J Public Health. 2014;24(2):221–225. doi: 10.1093/eurpub/cks174 [DOI] [PubMed] [Google Scholar]
- 24.Kayikcioglu M, Kuman-Tunçel O, Pirildar S, et al. Clinical management, psychosocial characteristics, and quality of life in patients with homozygous familial hypercholesterolemia undergoing LDL-apheresis in Turkey: results of a nationwide survey (A-HIT1 registry). J Clin Lipidol. 2019;13(3):455–467. doi: 10.1016/j.jacl.2019.02.001 [DOI] [PubMed] [Google Scholar]
- 25.Retterstøl K, Stugaard M, Gørbitz C, Ose L. Results of intensive long-term treatment of familial hypercholesterolemia. Am J Cardiol. 1996;78(12):1369–1374. doi: 10.1016/S0002-9149(96)00649-2 [DOI] [PubMed] [Google Scholar]
- 26.D’Erasmo L, Cefalù AB, Noto D, et al. Efficacy of lomitapide in the treatment of familial homozygous hypercholesterolemia: results of a real-world clinical experience in Italy. Adv Ther. 2017;34(5):1200–1210. doi: 10.1007/s12325-017-0531-x [DOI] [PubMed] [Google Scholar]
- 27.D’Erasmo L, Minicocci I, Nicolucci A, et al. Autosomal recessive hypercholesterolemia: long-term cardiovascular outcomes. J Am Coll Cardiol. 2018;71(3):279–288. doi: 10.1016/j.jacc.2017.11.028 [DOI] [PubMed] [Google Scholar]
- 28.Cuchel M, Meagher EA. du Toit Theron H, et al. Efficacy and safety of a microsomal triglyceride transfer protein inhibitor in patients with homozygous familial hypercholesterolaemia: a single-arm, open-label, Phase 3 study. Lancet. 2013;381(9860):40–46. doi: 10.1016/S0140-6736(12)61731-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roeters van Lennep J, Averna M, Alonso R. Treating homozygous familial hypercholesterolemia in a real-world setting: experiences with lomitapide. J Clin Lipidol. 2015;9(4):607–617. doi: 10.1016/j.jacl.2015.05.001 [DOI] [PubMed] [Google Scholar]
- 30.Komalasari R, Yoche MM. Quality of life of people with cardiovascular disease: a descriptive study. Asian Pac Isl Nurs J. 2019;4(2):92–96. doi: 10.31372/20190402.1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oldridge N, Cho C, Thomas R, Low M, Höfer S. Validation of the English Version of the HeartQoL Health-Related Quality of Life Questionnaire in Patients With Coronary Heart Disease. J Cardiopulm Rehabil Prev. 2018;38(2):92–99. doi: 10.1097/HCR.0000000000000248 [DOI] [PubMed] [Google Scholar]
- 32.Gierlaszyńska K, Pudlo R, Jaworska I, Byrczek-Godula K, Gąsior M. Tools for assessing quality of life in Cardiology and cardiac surgery. Kardiochir Torakochirurgia Pol. 2016;13(1):78–82. doi: 10.5114/kitp.2016.58974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flaim JD, Grundy JS, Baker BF, McGowan MP, Kastelein JJ. Changes in mipomersen dosing regimen provide similar exposure with improved tolerability in randomized placebo-controlled study of healthy volunteers. J Am Heart Assoc. 2014;3(2):e000560. doi: 10.1161/JAHA.113.000560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Visser ME, Wagener G, Baker BF, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, lowers low-density lipoprotein cholesterol in high-risk statin-intolerant patients: a randomized, double-blind, placebo-controlled trial. Eur Heart J. 2012;33(9):1142–1149. doi: 10.1093/eurheartj/ehs023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reeskamp LF, Kastelein JJP, Moriarty PM, et al. Safety and efficacy of mipomersen in patients with heterozygous familial hypercholesterolemia. Atherosclerosis. 2019;280:109–117. doi: 10.1016/j.atherosclerosis.2018.11.017 [DOI] [PubMed] [Google Scholar]
- 36.Raal FJ, Santos RD, Blom DJ, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, for lowering of LDL cholesterol concentrations in patients with homozygous familial hypercholesterolaemia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;375(9719):998–1006. doi: 10.1016/S0140-6736(10)60284-X [DOI] [PubMed] [Google Scholar]