Abstract
Objective:
To verify whether bone mineral density (BMD) of cortical bone, trabecular bone, and total bone influence the primary stability of orthodontic miniscrews and to verify whether there is a correlation between the measurement of BMD by cone-beam computed tomography (CBCT) and central dual-energy x-ray absorptiometry (DEXA).
Materials and Methods:
Twenty bovine bone sections were extracted from the pubic and iliac bones from regions with cortical thicknesses of approximately 1 mm. The BMD of the total bone block was evaluated using two methods: CBCT and DEXA. The BMD of cortical, trabecular, and total bone in the region of interest (ROI) were also evaluated by CBCT. After scanning the bone blocks, 20 self-drilling miniscrews (INP®) 1.4 mm in diameter and 6 mm long were inserted into them. The peak implant insertion torque (IT) was registered. After this, the pull-out test (PS) was performed and the maximum force registered. The Pearson correlation test was applied to verify the correlations between variables.
Results:
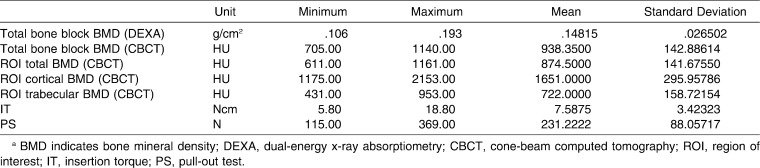
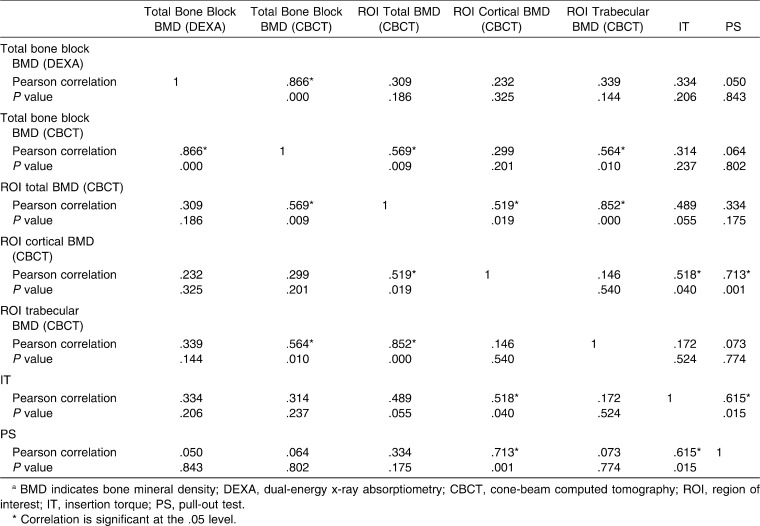
The BMD of the total bone block verified by CBCT and DEXA showed a positive and strong correlation (r = 0.866, P = .000). The BMD of the ROI for cortical bone influenced the IT (r = 0.518, P = .40) and the PS of miniscrews (r = 0.713, P = .001, Table 2). However, the total bone BMD (verified by CBCT and DEXA) and trabecular bone BMD presented weak and not statistically significant correlations with primary stability.
Conclusions:
There was a positive correlation between total bone block BMD measured by DEXA and CBCT. The cortical BMD influenced the IT and PS.
Keywords: Bone density, Cone-beam computed tomography, Dual-energy x-ray absorptiometry, Miniscrew
INTRODUCTION
The primary stability of miniscrews depends on the characteristics of the device, the insertion technique, and the bone quality and quantity of the receptor site.1 The bone quality classification most accepted in implant dentistry has been that proposed by Lekholm and Zarb,2 based on the amount of cortical and trabecular bone shown in preoperative radiographs. However, this classification depends on the operator's subjective evaluation of the radiograph. A less subjective method for evaluating the quality of cortical and trabecular bone involves verifying the bone mineral density (BMD).3
The quantification of BMD taken as the gold standard in endocrinology and traumatology is bone densitometry by means of central dual-energy x-ray absorptiometry (DEXA).4 In implant dentistry, however, cone-beam computed tomography (CBCT) has been used for this purpose because it offers a three-dimensional analysis that allows the quantification of the mineral density of jaw bones in specific sites in Hounsfield units (HU). When evaluating the BMD of the receptor site by CBCT, it is possible to verify the cortical BMD and trabecular BMD separately or the total bone BMD, which is the measurement of mineral density of trabecular bone and cortical bone together.
The aims of this study were to verify how these parameters influence the primary stability of orthodontic miniscrews and to verify whether there is a correlation between the measurement of BMD by CBCT and that by DEXA.
MATERIALS AND METHODS
The sample consisted of 20 bone sections extracted from bovine pelvic bone (Bos taurus, Angus lineage). The bones were obtained from a slaughterhouse (registered with ANVISA—the Brazilian Health Surveillance Agency) immediately after slaughter. The bone sections were extracted from the caudal portion of the pubic bone and from the gluteal wing of iliac bone with the use of a trephine bur (8 mm in diameter × 20 mm long; Sin Implantes, São Paulo, Brazil) adapted to a low-speed motor (Beltec LB100, Araraquara, Brazil) under irrigation. The bone sections (8 mm in diameter × 12 mm long) were taken from regions in which there was a mean cortical thickness of 1 mm (measured with an orthodontic caliper; Odin, Ortho-pli, Philadelphia, Pa). The extracted material was immersed in sterile physiological solution and stored by freezing (−20°C).
BMD Evaluation
The BMD was evaluated using two methods: DEXA and CBCT. First, the bone mineral content of specimens was measured and divided by the area to obtain the BMD by means of central DEXA Prodigy (GE/LUNAR, Madison, Wisc), calibrated for small animals. To perform the exam, the bone blocks were thawed at room temperature and placed in plastic boxes (6 cm × 11 cm × 4 cm) containing raw rice to simulate soft tissue.5 Following this step, the samples were irradiated by DEXA for 30 seconds.5 This analysis comprised the entire bone block (cortical and trabecular bones).
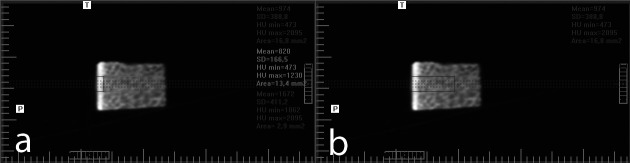
After this, CBCT (I-CAT 3D Dental Imaging System, Hatsfield, Pa) was used to obtain tomographs in accordance with a standard protocol (120 KV, 47 mA, FOV of 22 cm, voxel of 0.4 mm, and scan time of 30 seconds). All of the samples were arranged identically in a styrofoam box with the cortical bone perpendicular to the floor for the purpose of scanning. Data were imported in Digital Imaging and Communications in Medicine (DICOM) format and handled by I-CAT Vision (Dental Imaging System). Once imported, CT data were reconstructed into 1-mm–thick transaxial images. The BMD was obtained using the multiplanar reconstruction screen and measuring the HU of the selected area. First, a sagittal section was obtained in the center of the bone block. To verify whether the data for CBCT measurement of BMD were correlated with the data acquired from DEXA, the total area of the bone block in this section was evaluated (total bone block BMD). After this, the region of interest (ROI) was isolated. The ROI was considered the area in the center of the block that would surround the miniscrew after its placement (2.4 mm × 7 mm). The BMD of cortical bone, trabecular bone, and total bone were measured separately in the ROI (Figure 1).
Figure 1.
Region of interest (ROI) delimitation in the sagittal section. (a) Smaller rectangle on the left indicates the cortical ROI. Larger rectangle on the right indicates the trabecular ROI; (b) total bone ROI.
Primary Stability Evaluation
The primary stability was evaluated by means of insertion torque (IT) measurement and pull-out strength (PS). Twenty miniscrews (INP®, São Paulo, Brazil) 1.4 mm in diameter and 6 mm long were inserted into the bone blocks with the use of a manual placement key connected to a digital torque meter (Lutron TQ-8800, Taipei, Taiwan) to allow measurement of the peak implant placement torque. The values were recorded in Newton centimeters (Ncm). After this, the pull-out test, which consists of extracting the miniscrew from the bone at a constant speed, was performed to evaluate the maximum force required to remove it.6 The mechanical test was performed in a universal test machine (Emic DL 2000, São José dos Pinhais, Brazil) using a 500-Kgf load cell at a crosshead speed of 0.05 mm per second6 to remove the miniscrew. The maximum PS was recorded.
Statistical Analysis
The variables total bone BMD (evaluated by DEXA and CBCT), cortical BMD, trabecular BMD, and total BMD in ROI (evaluated by CBCT), IT, and PS were evaluated using the Statistical Package for the Social Sciences (version 17, SPSS Inc, Chicago, Ill). The values obtained were tabulated and submitted to normality and homogeneity tests (Shapiro-Wilk and Levene). The Pearson correlation test was applied to verify the correlations between variables. The level of significance was 5%.
RESULTS
Descriptive statistics are presented in Table 1. The result of the Pearson correlation test is shown in Table 2. The cortical bone BMD in the ROI (CBCT) influenced the IT (r = 0.866, P = .000, positive and strong correlation) and the PS of miniscrews (r = 0.713, P = .001, positive and strong correlation). However, the total bone block BMD, measured by means of DEXA and CBCT, the total BMD in the ROI, and the trabecular BMD in the ROI presented weak and non–statistically significant correlations with primary stability. The two variables that measured the primary stability, IT and PS, presented a positive and substantial correlation (r = 0.615, P = .015).
Table 1.
Descriptive Statisticsa
Table 2.
Pearson Correlation Testa
DISCUSSION
Although DEXA4 is used as the gold-standard method for measuring BMD in traumatology and endocrinology, CBCT is often used in implant dentistry. CT was introduced as a preparatory exam for prosthodontic implant placement by Schwarz7 in 1987 and became popular in dentistry. The CT three-dimensional analysis allows the quantification of the mineral density of jaw bones in specific sites in cross sections. The BMD is measured in HU by the difference in grayscale. The CBCT also allows bone dimensions to be measured before miniscrew placement. The results of this study showed that the BMD of the total bone block, verified by CBCT and DEXA, had a positive and strong correlation (r = 0.866, P = .000).
The results of this study showed that the BMD of the ROI of cortical bone influences the primary stability of miniscrews measured by the IT and PS tests. The total bone block BMD and the total BMD ROI did not influence the IT and PS of miniscrews. A similar result was previously described by Cha et al.8 They evaluated the primary stability of miniscrews inserted in the jaws of beagle dogs. As in the present study, the bone density was assessed by CBCT and the primary stability was verified by means of IT and also by the Periotest value (Periotest, Medizintechnik Gulden, Modautal, Germany). They found a positive association between cortical BMD and miniscrew primary stability, but the BMD for the total bone was weak and non–statistically significant.
The importance of the cortical bone in miniscrew stability has previously been established by assessing the cortical thickness, and a positive association was verified between cortical thickness and the primary stability of miniscrews.1,6,8–11 The evaluation of cortical BMD corroborates its importance in terms of initial stability.
The ROI of total BMD has previously been related to the primary stability of prosthodontic implants,12–14 but it was not verified for miniscrews in the present study or in the study of Cha et al.8 The ROI of trabecular BMD also plays an important role in the primary stability of prosthodontic implants, as verified by Bergkvist et al.3 and Merheb et al.15 However, in this study, with a cortical thickness of 1 mm, there was no association between the ROI of trabecular BMD and the primary stability of mini-implants.
Despite the limitations of our laboratory study, the CBCT proved to be a useful exam for noninvasive assessment of bone density at the preoperative stage of mini-implant placement. Moreover, the cortical thickness and the cortical BMD can be measured to estimate the primary stability of miniscrews.
We suggest that future research should investigate the influence of total BMD and trabecular BMD on primary stability when there is a cortical thickness of less than 1 mm.
CONCLUSIONS
The total bone block BMD measured by DEXA and CBCT presented a positive and strong correlation.
The ROI of cortical BMD presented a positive and substantial correlation with IT and PS; however, the ROIs of trabecular BMD, total BMD, and total bone block BMD were not correlated with the primary stability of miniscrews.
Acknowledgments
The authors would like to express their grateful appreciation to the following entities: Cordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) for the financial support provided; Sistema de Implantes Nacionais e de Próteses (INP) for the donation of the miniscrews; Frigorífico Silva for the donation of the bones and Doctors Maria Lucia Fleiuss Farias and Laura Maria Carvalho Mendonça for their assistance in the DEXA examination of the bones.
REFERENCES
- 1.Wilmes B, Rademacher C, Olthoff G, Drescher D. Parameters affecting primary stability of orthodontic mini-implants. J Orofac Orthop. 2006;67:162–174. doi: 10.1007/s00056-006-0611-z. [DOI] [PubMed] [Google Scholar]
- 2.Lekholm U, Zarb G. Patient selection and preparation. In: Branemark P. I, Zarb G, Albrektsson T, editors. TissueIntegrated Prostheses Osseointegration in Clinical Dentistry. Chicago, Ill: Quintessence; 1985. pp. 199–209. [Google Scholar]
- 3.Bergkvist G, Koh K. J, Sahlholm S, Klintstrom E, Lindh C. Bone density at implant sites and its relationship to assessment of bone quality and treatment outcome. Int J Oral Maxillofac Implants. 2010;25:321–328. [PubMed] [Google Scholar]
- 4.Carey J. J, Delaney M. F, Love T. E, et al. DXA-generated Z-scores and T-scores may differ substantially and significantly in young adults. J Clin Densitom. 2007;10:351–358. doi: 10.1016/j.jocd.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Pithon M. M, Andrade A. C. D. V, Rodrigues V. B, Santos R. L. Influence of the immunosuppressant tracolimus (FK-506) on the flexural strength of femur: a study in rats. Rev Bras Ortopedia. 2010;45:286–289. doi: 10.1016/S2255-4971(15)30370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huja S. S, Litsky A. S, Beck F. M, Johnson K. A, Larsen P. E. Pull-out strength of monocortical screws placed in the maxillae and mandibles of dogs. Am J Orthod Dentofacial Orthop. 2005;127:307–313. doi: 10.1016/j.ajodo.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 7.Schwarz M. S, Rothman S. L, Rhodes M. L, Chafetz N. Computed tomography: part I. Preoperative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants. 1987;2:5. [PubMed] [Google Scholar]
- 8.Cha J. Y, Kil J. K, Yoon T. M, Hwang C. J. Miniscrew stability evaluated with computerized tomography scanning. Am J Orthod Dentofacial Orthop. 2010;137:73–79. doi: 10.1016/j.ajodo.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Motoyoshi M, Yoshida T, Ono A, Shimizu N. Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implants. Int J Oral Maxillofac Implants. 2007;22:779–784. [PubMed] [Google Scholar]
- 10.Motoyoshi M, Inaba M, Ono A, Ueno S, Shimizu N. The effect of cortical bone thickness on the stability of orthodontic mini-implants and on the stress distribution in surrounding bone. Int J Oral Maxillofac Surg. 2009;38:13–18. doi: 10.1016/j.ijom.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Su Y. Y, Wilmes B, Honscheid R, Drescher D. Application of a wireless resonance frequency transducer to assess primary stability of orthodontic mini-implants: an in vitro study in pig ilia. Int J Oral Maxillofac Implants. 2009;24:647–654. [PubMed] [Google Scholar]
- 12.Aksoy U, Eratalay K, Tozum T. F. The possible association among bone density values, resonance frequency measurements, tactile sense, and histomorphometric evaluations of dental implant osteotomy sites: a preliminary study. Implant Dent. 2009;18:316–325. doi: 10.1097/ID.0b013e31819ecc12. [DOI] [PubMed] [Google Scholar]
- 13.Pagliani L, Motroni A, Nappo A, Sennerby L. Short communication: use of a diagnostic software to predict bone density and implant stability in preoperative CTs. Clin Implant Dent Relat Res. doi: 10.1111/j.1708-8208.2010.00291.x. In press. [DOI] [PubMed] [Google Scholar]
- 14.Turkyilmaz I, McGlumphy E. A. Influence of bone density on implant stability parameters and implant success: a retrospective clinical study. BMC Oral Health. 2008;8:32. doi: 10.1186/1472-6831-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merheb J, Van Assche N, Coucke W, Jacobs R, Naert I, Quirynen M. Relationship between cortical bone thickness or computerized tomography-derived bone density values and implant stability. Clin Oral Implants Res. 2010;21:61261–61267. doi: 10.1111/j.1600-0501.2009.01880.x. [DOI] [PubMed] [Google Scholar]