Abstract
Objective:
To test the null hypothesis that the presence of dehiscence and fenestration was not different among patients with skeletal Class I, II, and III malocclusions.
Materials and Methods:
In this retrospective study, a total of 123 cone-beam computed tomography (CBCT) images were obtained with an iCAT scanner (Imaging Sciences International, Hatfield, Pa). Patients with normal vertical patterns were classified according to dental malocclusion and ANB angle. Class I comprised 41 patients—21 girls and 20 boys (mean age, 22.4 ± 4.5 years); Class II comprised 42 patients—22 girls and 20 boys (mean age, 21.5 ± 4.2 years); and Class III comprised 40 subjects—22 girls and 18 boys (mean age, 22.1 ± 4.5 years). A total of 3444 teeth were evaluated. Analysis of variance and Tukey's test were used for statistical comparisons at the P < .05 level.
Results:
Statistical analysis indicated that the Class II group had a greater prevalence of fenestration than the other groups (P < .001). No difference was found in the prevalence of dehiscence among the three groups. Although fenestration had greater prevalence in the maxilla, more dehiscence was found in the mandible for all groups. In Class I, alveolar defects (dehiscence, fenestration) were matched relatively in both jaws. Furthermore, Class II and Class III subjects had more alveolar defects (41.11% and 45.02%, respectively) in the mandible. Dehiscences were seen with greater frequency in the mandibular incisors of all groups.
Conclusion:
The null hypothesis was rejected. Significant differences in the presence of fenestration were found among subjects with skeletal Class I, Class II, and Class III malocclusions. Fenestrations had greater prevalence in the maxilla, but more dehiscences were found in the mandible.
Keywords: Fenestration, Dehiscence, Tomography, Orthodontic malocclusion
INTRODUCTION
“Bone traces tooth movement” is a basic axiom in orthodontics; it suggests that whenever orthodontic tooth movement occurs, bone around the alveolar socket will remodel to the same extent.1 Because bone resorption occurs in the direction of tooth movement, the reduced volume of the alveolar bone, sometimes with minimal thickness and sometimes nonexistent, is a complicating factor for orthodontic treatment.2 The biologic and biomechanical factors are closely related and determine the potential side effects of orthodontic treatment, such as external root resorption, dehiscence, fenestration, and gingival recession.3
Gingival recession is described as exposure of the root surface by an apical shift in the position of the gingiva.4 Many factors may contribute to the development of recessions, including difficulty in plaque control due to fixed orthodontic appliances, coronally attached frenal and muscle attachments, abnormal tooth position, overhanging restorations or crowns, transverse expansion, proclination of teeth, fenestration, and dehiscence.5 These predisposing factors contribute to the establishment and/or progression of gingival inflammation and the formation of dehiscence.6
Clinically, gingival recession is always accompanied by alveolar bone dehiscences.7 Whether underlying bone dehiscence is developed before or parallel with gingival recession has not been clarified.8 Alveolar dehiscence is a defect that results in lowering of the crestal bone margin to expose the root surface.9 Fenestrations are isolated areas in which the root is denuded of bone, and the root surface is covered only by periosteum and overlying gingiva.5 The occurrence of dehiscence and fenestration during orthodontic treatment depends on several factors, such as the direction of movement, the frequency and magnitude of orthodontic forces, and the volume and anatomic integrity of periodontal tissues.10 To avoid these problems, the alveolar morphology must be determined before orthodontic treatment through imaging, which shows bone topography and anatomy.11
Until the introduction of computed tomography (CT), visualization of labial/buccal and lingual bone plates was not possible because of image superimposition associated with conventional radiographs, and because the gingival covering interfered with clinical analysis.12 Cone-beam computed tomography (CBCT) has provided the means to visualize these defects three-dimensionally.13 CT images can show bone dehiscence and fenestration by means of high definition and sensitivity.14 CBCT yields high-definition images of teeth and bone at a far lower dosage of radiation than is used with medical imaging and closer to the range of standard dental film series.15
Various animal experiments have shown that loss of thin bone plates may be induced by orthodontic tooth movement.16 Therefore, the choice of treatment plan should be greatly influenced by bone morphology and the position of the teeth.17,18 Visualization of anatomic details of our patients and comprehension of tooth movement collateral effects permit us to recognize our limits and to practice safe orthodontics.12
Only a few studies have evaluated the presence of alveolar defects with CT. Garib et al.12 evaluated alveolar bone morphology visualized by means of CT. Leung et al.19 investigated the accuracy and reliability of CBCT in the diagnosis of fenestration and dehiscence on dry human skulls. Recently, Evangelista et al.11 compared the presence of dehiscence and fenestration between patients with Class I and Class II division 1 malocclusions.
To date, no study has been undertaken to compare the presence of alveolar defects in subjects with Class I, Class II, and Class III malocclusions, with CBCT. Thus, the aim of this study was to evaluate the null hypothesis that the presence of dehiscence and fenestration was not different among patients with skeletal Class I, Class II, and Class III malocclusions.
MATERIALS AND METHODS
A power analysis established by G*Power, version 3.0.10 (Franz Faul, Universität Kiel, Kiel, Germany) software, based on 1∶1 ratio between groups, with sample size of 40 patients, would give more than 70% power to detect significant differences with 0.40 effect size and at the α = .05 significance level.
The present study was carried out on the CBCT scans of three groups selected from the archives of the Oral and Maxillofacial Radiology Department of Dicle University. By January 2011, 1520 sets of images were in the database of the department. Because this study was an archive study, no ethical approval was gained.
CBCT images of 142 patients (mean age, 18 to 30 years) were analyzed, and the criteria presented in Table 1 were followed for sample selection. Of 142 images, 123 tomographs were included in the present study. These tomographs were obtained by using CBCT (iCAT, Model 17–19, Imaging Sciences International, Hatfield, Pa) with a single 360-degree rotation and a voxel size of 0.3 mm at the following settings: exposures were made with 5.0 mA, 120 kV, and exposure time of 9.6 seconds, and axial slice thickness was 0.3 mm.
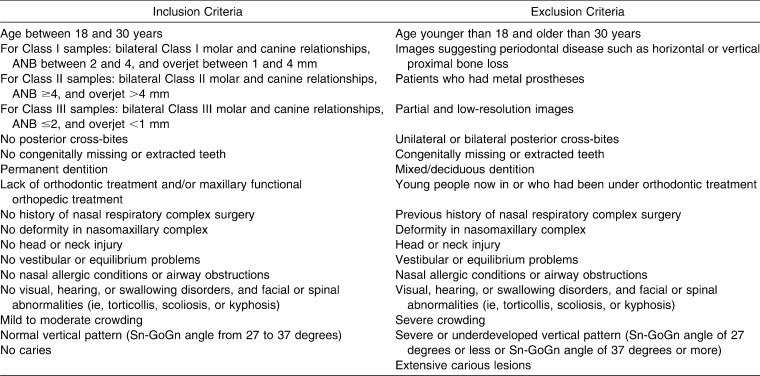
Table 1.
Adopted Criteria for Sample Selection
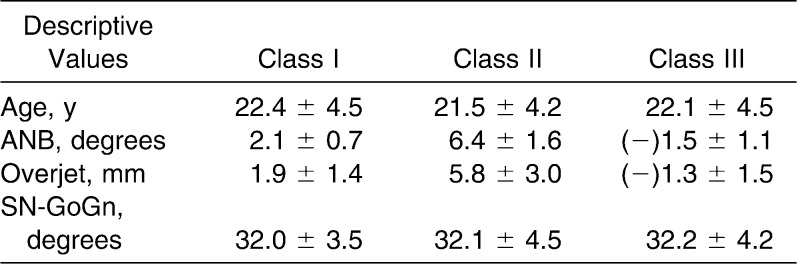
The tomographs were classified into three groups on the basis of dental malocclusion. The Class I malocclusion group (ANB = 0 to 4 degrees) comprised 41 patients—21 girls and 20 boys (mean age, 22.4 ± 4.5 years), the Class II malocclusion group (ANB > 4 degrees) comprised 42 patients—22 girls and 20 boys (mean age, 21.5 ± 4.2 years), and the Class III malocclusion group (ANB < 0 degrees) comprised 40 subjects—22 girls and 18 boys (mean age, 22.1 ± 4.5 years). All teeth except the third molars were included, and a total of 3444 teeth were evaluated. Table 2 shows sample characteristics according to malocclusion.
Table 2.
Mean Values (±Standard Deviations) for Age, ANB, Overjet, and SN-GoGn in Patients With Class I, Class II, and Class III Malocclusions
Primary and secondary reconstructions of the data were performed with iCAT software. This secondary reconstruction allowed us to create three-dimensional projections of images with maximum intensity for making linear measurements. Each tooth root was evaluated in axial and cross-sectional slices at buccal and lingual surfaces. The situation showing no cortical bone around the root in at least three sequential views was accepted as an alveolar defect. If the alveolar bone height was more than 2 mm from the cementoenamel junction,20 it was classified as dehiscence (Figure 1). When the defect did not involve the alveolar crest, this case was classified as fenestration (Figure 2).
Figure 1.
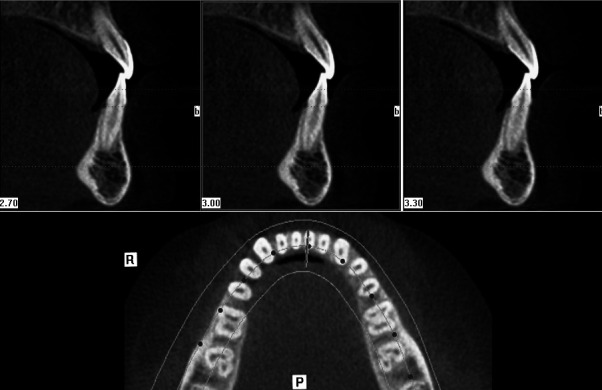
Dehiscence in at least three sequential views.
Figure 2.
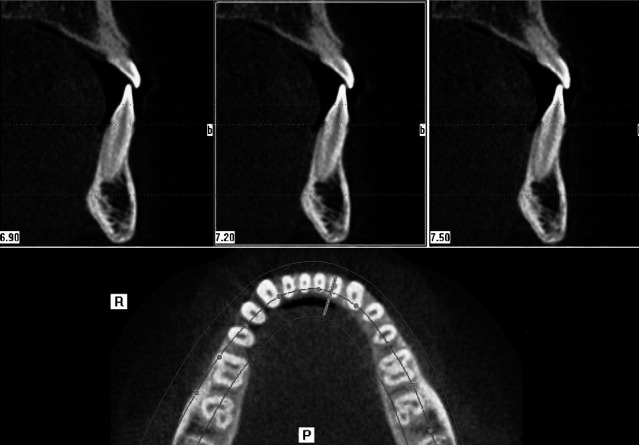
Fenestration in at least three sequential views.
Statistical Analysis
All statistical analyses were performed with the Statistical Package for the Social Sciences (SPSS), version 13.0 (SPSS Inc, Chicago, Ill). The normality test of Shapiro-Wilks and Levene's variance homogeneity test were applied to the data, which were found to be normally distributed with homogeneity of variance among groups. Thus, statistical evaluation was performed using parametric tests.
Arithmetic mean and standard deviation values were calculated for each measurement.
Statistical comparisons of alveolar defects in subjects in different malocclusion groups were undertaken by one-way analysis of variance (ANOVA) and Tukey's Honestly Significant Differences (HSD) test. When the P value was less than .05, the statistical test was determined to be significant.
RESULTS
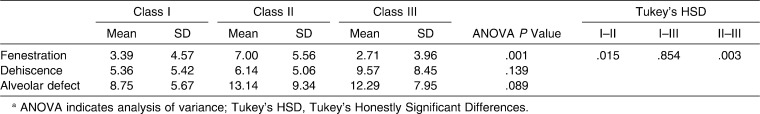
According to ANOVA, statistically significant differences were found in fenestration measurements among patients with different Angle malocclusion groups (P = .001) (Table 3). Tukey's HSD test indicated that Class II patients had a greater prevalence of fenestration than patients in the other groups (P = .001). No significant difference was noted in the incidence of dehiscence among the three groups (P = .139).
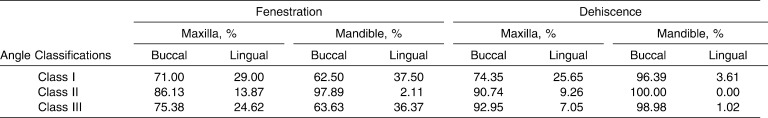
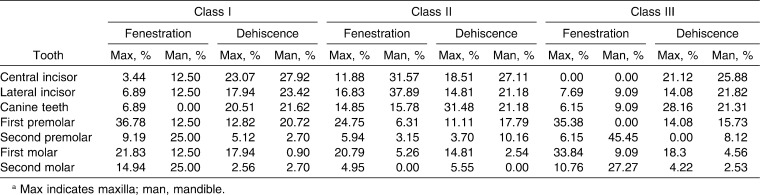
Table 3.
Mean Values (mm) (±Standard Deviations) for Alveolar Defects in Patients With Class I, Class II, and Class III Malocclusions
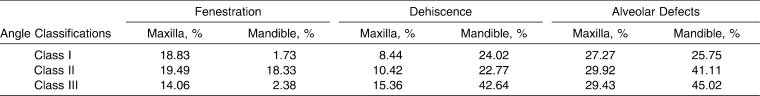
Tables 4 to 6 show the distributions and incidences of alveolar defects. Although fenestrations had greater prevalence in the maxilla, a greater number of dehiscences were found in the mandible for all groups. In the Class I group, alveolar defects were found to be relatively similar in both jaws (Table 4). Furthermore, Class II and Class III groups had more alveolar defects in the mandible (41.11% and 45.02%, respectively).
Table 4.
Distribution of Alveolar Defects in Maxilla and Mandible for Different Malocclusions
Table 5.
Incidence of Fenestration and Dehiscence for Different Malocclusions
Table 6.
Incidence of Alveolar Defects in Tooth for Different Malocclusions
Alveolar defects were more predominant in the buccal root surfaces (Table 5). Most cases of fenestration in the maxilla were seen at the first premolars (Class I group, 36.78%; Class II group, 24.75%; Class III group, 35.38%) and at the first molars (Class I, 21.83%; Class II, 20.79%; Class III, 33.84%) in all groups. Dehiscences were seen with greater frequency in the mandibular incisor region for all groups (Table 6).
DISCUSSION
Because underestimated or misdiagnosed buccal alveolar bone defects can cause treatment relapse21 or gingival recession,22 identification of alveolar bone defects before orthodontic treatment is critical in treatment planning. Also, orthodontic mechanics can decentralize teeth from the alveolar bone envelope, causing bone dehiscences and fenestrations, depending on the initial morphology of alveolar bone and the amount of tooth movement.12
Before the introduction of CT, visualization of labial/buccal and lingual bone plates was not possible because of image superimposition associated with conventional radiographs, and because the gingival covering interfered with clinical analysis.12 Use of high-resolution CT enables us to examine the shape and size of alveolar bones without the disadvantages of conventional radiographs.23 These images are not subjected to distortion or superimposition and facilitate quantitative and qualitative evaluation of bone surfaces and quantitative evaluation of the relationship between teeth and bone.24 Because they have high resolution and sensitivity, helical CT14 and CBCT images can demonstrate bone dehiscences and fenestrations.15 Spiral CT and helical CT use more radiation and have higher costs than CBCT, and their use is limited for routine dental radiography.25 Because of these advantageous properties, CBCT scans obtained from the archive were used to determine alveolar defects in the current study.
Facial types of subjects may have an effect on the morphology of buccal and lingual bone plates. Although hypodivergent subjects present thicker alveolar ridges,26 hyperdivergent subjects have thinner alveolar ridges, especially in the mandibular anterior region.2 Therefore, orthodontic treatment planning presents less restriction for moving the lower incisors in the labiolingual direction in hypodivergent subjects.12 On the other hand, Evangelista et al.11 reported that facial types do not affect the prevalence of alveolar defects. In the current study, only normodivergent subjects were evaluated. Further investigation is useful to determine whether a facial growth pattern has an influence on the morphology of alveolar bone.
Investigation on human skulls by Rupprecht et al.27 showed that African American males and white females are significantly more likely to have dehiscences, and African American females are significantly more likely to have fenestrations.27 In the current study for the present population, all samples showed a higher prevalence of dehiscences than fenestrations. Dehiscences could be determined easily and more accurately than fenestrations with CBCT. Although the densities of cementum and bone are similar because of their similar hydroxyapatite content,4 enamel has more hydroxyapatite content. Therefore, drawing the attention of the investigator to this density difference may lead to overdetermination of dehiscence. Additionally, the bone margin has a certain thickness, which can cause difficulty in selecting the point accurately for measurement.19
A large number of studies have associated the protrusion of maxillary anterior teeth with the majority of Class II patients. Riedel28 noted that the maxillary incisors in Class II malocclusions are twice as far anterior to the facial plane as those in normal occlusion. Besides, mandibular incisors are strongly inclined buccally and are protruded in relation to the apical base.29 In the current study, Class II samples had significant fenestration prevalence (18.33%) compared with Class I (1.73%) and Class III (2.38%) samples at the mandibular region (P < .001). On the other hand, alveolar defects of the maxillary teeth had similar prevalence to Class I samples. Among Class II subjects, the teeth most affected were the mandibular central (31.57%) and lateral incisors (37.89%). This result may be attributed to the thinner bone structure in the lower anterior region. Another explanation for the increased prevalence of dehiscence could be the dentoalveolar compensation seen in Class II patients. Therefore, for labiolingual movement of the mandibular incisors, tooth tipping should be preferred over bodily tooth movement in Class II patients.
When the groups were evaluated, Class III samples showed the least fenestration and the greatest dehiscence prevalence (fenestration: maxilla, 14.06%, mandible, 2.38%; dehiscence: maxilla, 15.36%, mandible, 42.64%). Studies on the components of Class III malocclusions revealed that Class III patients have protrusive maxillary incisors and retrusive mandibular incisors.30 Moreover, Class III patients present a thinner mandibular symphysis even than Class I and Class II patients.31 The type of tooth movement depends on the line of action of force related to the center of resistance of teeth.32 Labiolingual movement of the incisors should be carefully planned in Class III treatments.
The presence of dehiscences and fenestrations is positively correlated with thin alveolar bone and is negatively correlated with occlusal attrition.27 In the mandible, the thickness of the alveolar ridge is remarkably decreased from the posterior to the anterior region.33 Before orthodontic treatment, bone dehiscences are common in the mandibular symphysis region, especially among adults.16 In accordance with the literature, dehiscence was more frequently found in the mandible, whereas fenestration was more frequent in the maxilla.11,27 According to present findings, the most frequent dehiscence was seen in the mandibular anterior segment for all samples. The most frequent fenestration in the maxilla was seen at the first premolars for all groups (Class I, 36.78%; Class II, 24.75%; Class III, 35.38%). One possible explanation for this distribution was the anatomic characteristics of the maxilla.12 The maxillary first premolars are located in an area that becomes narrower upward.12 The buccal-lingual movement of the maxillary first molars can have detrimental effects on the health of the teeth and the periodontium. For this reason, a CBCT investigation would be useful for assessment of premolar inclination to put the teeth in the center of the alveolus.
Crowded and misaligned teeth are possible risk factors for bone dehiscences and fenestrations.16 Inadequate bone support during orthodontic movement may have deleterious effects on teeth and the periodontium.34 Therefore, buccal-lingual movements present greater risk for breaking the limits of the alveolar bone, causing buccal and lingual bone plate resorption. Studies have shown greater prevalence of alveolar defects on the buccal surface than on the lingual surface.11,27 This may be attributed to narrower bone at the buccal surface, where the amount of marrow bone is less dense than in the lingual region.11 Dehiscence and fenestration of the buccal cortical plate have been reported in rapid maxillary expansion, suggesting that root movement of the buccal dental segment exceeds lateral bone remodeling.35 Even a single tooth movement in a buccolingual direction can produce the same effect.36 Further investigation is needed to determine whether maxillary expansion creates alveolar defects.
CONCLUSIONS
The Class II malocclusion group had greater prevalence of fenestrations than the Class III and Class I groups. However, no significant difference was found for the incidence of dehiscence.
Although fenestrations had greater prevalence in the maxilla, a greater number of dehiscences were found in the mandible for all groups.
Alveolar defects were predominant in the buccal root surfaces.
Most fenestrations in the maxilla were seen at the first premolars and the first molars in all investigated groups. However, dehiscences were seen with greater frequency in the mandibular incisors.
REFERENCES
- 1.Reitan K. Effects of force magnitude and direction of tooth movement on different alveolar bone types. Angle Orthod. 1964;34:244–255. [Google Scholar]
- 2.Handelman C. S. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:95–109. doi: 10.1043/0003-3219(1996)066<0095:TAAIII>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Thilander B. L. Complications of orthodontic treatment. Curr Opin Dent. 1992;2:28–37. [PubMed] [Google Scholar]
- 4.Glickman I, Carranza F. A. Clinical Periodontology 5th ed. Philadelphia, Pa: WB Saunders; 1979. pp. 100–101. [Google Scholar]
- 5.Koke U, Sander C, Heinecke A, Muller H. P. A possible influence of gingival dimensions on attachment loss and gingival recession following placement of artificial crowns. Int J Periodontics Restorative Dent. 2003;23:439–445. [PubMed] [Google Scholar]
- 6.Genco R. J. Current view of risk factors for periodontal diseases. J Periodontol. 1996;67:1041–1049. doi: 10.1902/jop.1996.67.10.1041. [DOI] [PubMed] [Google Scholar]
- 7.Richman C. Is gingival recession a consequence of an orthodontic tooth size and/or tooth position discrepancy? “A paradigm shift.”. Compend Contin Educ Dent. 2011;32:62–69. [PubMed] [Google Scholar]
- 8.Engelking G, Zachrisson B. U. Effects of incisor repositioning on monkey periodontium after expansion through the cortical plate. Am J Orthod. 1982;2:23–32. doi: 10.1016/0002-9416(82)90542-5. [DOI] [PubMed] [Google Scholar]
- 9.Watson W. G. Expansion and fenestration or dehiscence. Am J Orthod. 1980;77:330–332. doi: 10.1016/0002-9416(80)90086-x. [DOI] [PubMed] [Google Scholar]
- 10.Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone and symphysis after orthodontic treatment: a retrospective study. Am J Orthod Dentofacial Orthop. 1996;110:239–246. doi: 10.1016/s0889-5406(96)80006-0. [DOI] [PubMed] [Google Scholar]
- 11.Evangelista K, Vasconcelos K. F, Bumann A, Hirsch E, Nitka M, Silva M. A. G. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138:133.e1–133.e7. doi: 10.1016/j.ajodo.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Garib D. G, Yatabe M. S, Ozawa T. O, Filho O. G. S. Alveolar bone morphology under the perspective of the computed tomography: defining the biological limits of tooth movement. Dental Press J Orthod. 2010;15:192–205. [Google Scholar]
- 13.Mengel R, Candir M, Shiratori K, Flores-de-Jacoby L. Digital volume tomography in the diagnosis of periodontal defects: an in vitro study on native pig and human mandibles. J Periodontol. 2005;76:665–673. doi: 10.1902/jop.2005.76.5.665. [DOI] [PubMed] [Google Scholar]
- 14.Fuhrmann R. A, Bücker A, Diedrich P. R. Assessment of alveolar bone loss with high resolution computed tomography. J Periodontal Res. 1995;30:258–263. doi: 10.1111/j.1600-0765.1995.tb02131.x. [DOI] [PubMed] [Google Scholar]
- 15.Huang J, Bumann A, Mah J. Three-dimensional radiographic analysis in orthodontics. J Clin Orthod. 2005;39:421–428. [PubMed] [Google Scholar]
- 16.Fuhrmann R. Three-dimensional evaluation of periodontal remodeling during orthodontic treatment. Semin Orthod. 2002;8:23–28. [Google Scholar]
- 17.Gracco A, Luca L, Bongiorno M. C, Siciliani G. Computed tomography evaluation of mandibular incisor bony support in untreated patients. Am J Orthod Dentofacial Orthop. 2010;138:179–187. doi: 10.1016/j.ajodo.2008.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Kilic C, Kamburoglu K, Yuksel S. P, Ozen T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 2010;4:462–467. [PMC free article] [PubMed] [Google Scholar]
- 19.Leung C. C, Palomo L, Griffith R, Hans M. G. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;37:109–119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Persson R. E, Hollender L. G, Laurell L, Persson G. R. Horizontal alveolar bone loss and vertical bone defects in an adult patient population. J Periodontol. 1998;69:348–356. doi: 10.1902/jop.1998.69.3.348. [DOI] [PubMed] [Google Scholar]
- 21.Rothe L. E, Bollen A. M, Little R. M, Herring S. W, Chaison J. B, Chen C. S, Hollender L. G. Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod Dentofacial Orthop. 2006;130:476–484. doi: 10.1016/j.ajodo.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 22.Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 2005;127:552–561. doi: 10.1016/j.ajodo.2003.12.026. [DOI] [PubMed] [Google Scholar]
- 23.Fuhrmann R. Three-dimensional interpretation of periodontal lesions and remodeling during orthodontic treatment. Part III. J Orofac Orthop. 1996;57:224–237. doi: 10.1007/BF02190235. [DOI] [PubMed] [Google Scholar]
- 24.Fuhrmann R, Wehrbein H, Langen H. J, Diedrich P. Assessment of the dentate alveolar process with high resolution computer tomography. Dentomaxillofac Radiol. 1995;24:50–54. doi: 10.1259/dmfr.24.1.8593909. [DOI] [PubMed] [Google Scholar]
- 25.Mah J. K, Danforth R. A, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:508–513. doi: 10.1016/s1079-2104(03)00350-0. [DOI] [PubMed] [Google Scholar]
- 26.Gracco A, Lombardo L, Mancuso G, Gravina V, Siciliani G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009;79:692–702. doi: 10.2319/081908-437.1. [DOI] [PubMed] [Google Scholar]
- 27.Rupprecht R. D, Horning G. M, Nicoll B. K, Cohen M. E. Prevalence of dehiscences and fenestrations in modern American skulls. J Periodontol. 2001;72:722–729. doi: 10.1902/jop.2001.72.6.722. [DOI] [PubMed] [Google Scholar]
- 28.Riedel R. A. The relation of maxillary structures to cranium in malocclusion and normal occlusion. Angle Orthod. 1952;22:142–145. [Google Scholar]
- 29.Freitas M. R, Santos M. A, Freitas K. M, Janson G, Freitas D. S, Henriques J. F. Cephalometric characterization of skeletal Class II, division 1 malocclusion in white Brazilian subjects. J Appl Oral Sci. 2005;13:198–203. doi: 10.1590/s1678-77572005000200020. [DOI] [PubMed] [Google Scholar]
- 30.Ellis E, 3rd, McNamara J. A., Jr Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984;42:295–305. doi: 10.1016/0278-2391(84)90109-5. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y, Park J. U, Kook Y. A. Alveolar bone loss around incisors in surgical skeletal Class III patients. Angle Orthod. 2009;79:676–682. doi: 10.2319/070308-341.1. [DOI] [PubMed] [Google Scholar]
- 32.Smith R. J, Burstone C. J. Mechanics of tooth movement. Am J Orthod. 1984;85:294–307. doi: 10.1016/0002-9416(84)90187-8. [DOI] [PubMed] [Google Scholar]
- 33.Swasty D, Lee J. S, Huang J. C, Maki K, Gansky S. A, Hatcher D, Miller A. J. Anthropometric analysis of the human mandibular cortical bone as assessed by cone-beam computed tomography. J Oral Maxillofac Surg. 2009;67:491–500. doi: 10.1016/j.joms.2008.06.089. [DOI] [PubMed] [Google Scholar]
- 34.Wennstrom J. L, Stokland B. L, Nyman S, Thilander B. Periodontal tissue response to orthodontic movement of teeth with infrabony pockets. Am J Orthod Dentofacial Orthop. 1993;103:313–319. doi: 10.1016/0889-5406(93)70011-C. [DOI] [PubMed] [Google Scholar]
- 35.Vardimon A. D, Graber T. M, Voss L. R, Lemke J. Determinants controlling iatrogenic external root resorption and repair during and after palatal expansion. Angle Orthod. 1991;61:113–124. doi: 10.1043/0003-3219(1991)061<0113:DCIERR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 36.Wainwright W. M. Faciolingual tooth movement: its influence on the root and cortical plate. Am J Orthod. 1973;64:278–302. doi: 10.1016/0002-9416(73)90021-3. [DOI] [PubMed] [Google Scholar]