Abstract
Objective:
To test the manufacturer's recommendation for the application rubbing time of a self-etching primer (Transbond Plus, 3M Unitek) and to compare the resulting bond strength of a resin composite (Transbond XT, 3M Unitek) in the traditional laboratory tension on all four wings with a simulation of the clinical single-wing lift-off debonding instrument (LODI; 3M Unitek).
Materials and Methods:
Flattened stainless-steel maxillary incisor orthodontic brackets (Victory Series, 3M Unitek) were bonded to 108 flattened bovine incisors. The enamel was rubbed with the self-etching primer for 0, 5 (the manufacturer's recommendation), and 10 seconds during a 10-second application. Traditional four-wing and LODI simulated debonding forces and the adhesive remnant index (ARI) were recorded.
Results:
One-way analysis of variance testing among rubbing times and debonding methods indicated a significant difference in strength with 0 and 5 seconds of rubbing and between traditional and LODI simulated tension. The bond strengths were higher in the ARI = 1 subset compared to the ARI = 3–5 subsets.
Conclusions:
The manufacturer's recommendation for primer rubbing time produced the highest bond strength. Less force is required for debonding when tension is applied to one wing (LODI simulation) vs on all four wings.
Keywords: Self-etching primer, Debonding, Bond strength, LODI, ARI
INTRODUCTION
Orthodontic self-etching primers (SEPs) are increasingly popular1 because of improved efficiency2 and reduced technique sensitivity3 and because SEPs might cause fewer irreversible enamel changes than traditional etching priming as a result of decreased depths of penetration.4,5 While these advantages lead many clinicians to adopt SEPs, bond strengths comparable to those offered by traditional etching and priming are critical for clinical use,1,4–21 so the application method of SEPs warrants further investigation.14
The application technique, a combination of time and agitation (rubbing), has been studied for Transbond Plus (3M Unitek, Monrovia, Calif), a popular orthodontic self-etching system.5,22 Ostby et al.22 found that increasing the application time from 3 seconds to 15 seconds did not significantly increase the shear bond strength. Iijima et al.5 also found no significant difference in shear bond strengths for application times of 3, 10, and 30 seconds. However, when tested in tension, Perdigao et al.23 reported that doubling the manufacturer's suggested conditioning time might increase bond strengths for specific products. There is little information available concerning the effects of rubbing time on bond strength and debond mode (adhesive remnant index, ARI); therefore, the primary purpose of this study was to evaluate the effect of varying rubbing times on the tensile debonding characteristics of Transbond Plus.
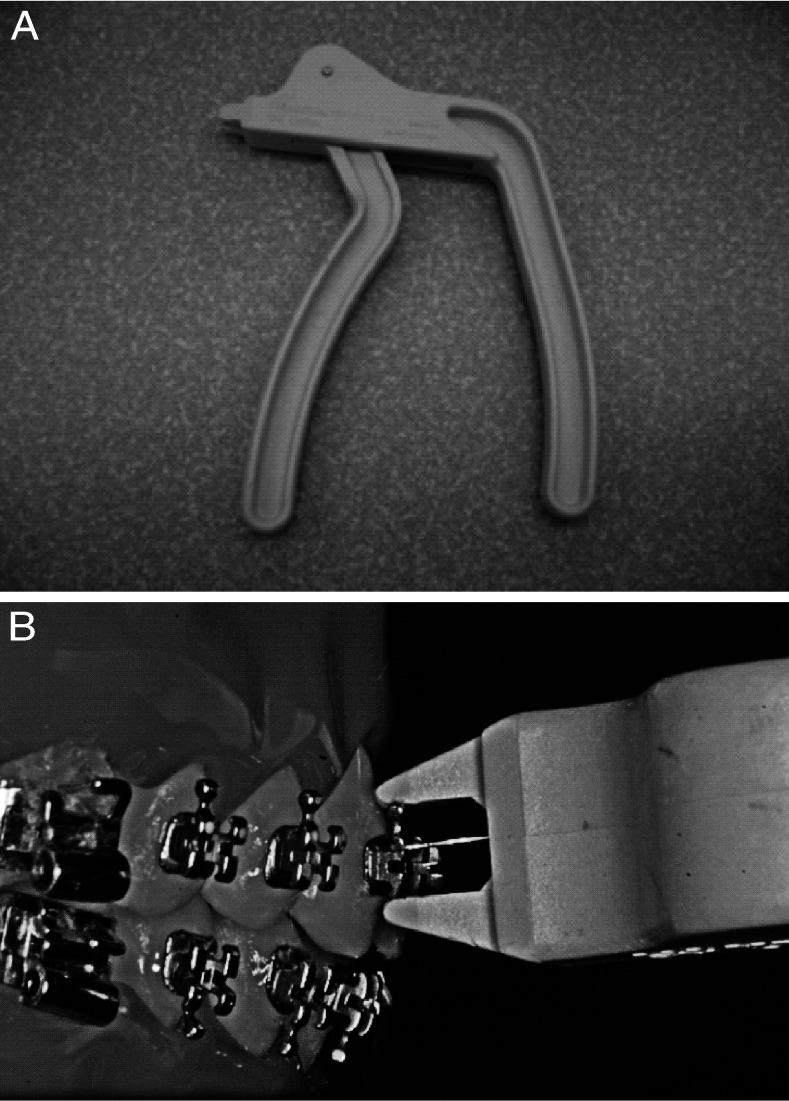
Although a tensile debonding test provides valuable information on relative bond strengths, it does not replicate clinical debonding procedures. Two common debonding tools are the traditional debonding pliers and the lift-off debonding instrument (LODI) (Figure 1). The pliers cause more bracket base and wing distortions than does the LODI.24 Since brackets are often reused in the same patient or commercially recycled, such deformations are undesirable. The LODI applies the tensile force onto one wing rather than distributing it among all four wings like the traditional tensile laboratory debonding test does. Hence, LODI produces a very different asymmetric stress distribution within the structures, with doubled peak stress magnitudes.25 Therefore, the secondary purpose of this study was to compare the traditional four-wing tensile test with tension on one wing of the bracket, a simulation of the clinically popular LODI. To determine if bracket asymmetry is a factor,9 there were two LODI groups—one was debonded using the distal-cervical wing, the other with the distal-incisal wing.
Figure 1.
(A) Lift-off debonding instrument (LODI; 3M Unitek, Monrovia, Calif) (B) pulling on the distal-cervical wing.
MATERIALS AND METHODS
Specimens
Bovine incisors, stored for 2–3 months in a 0.1% thymol solution to control bacterial growth, without obvious enamel defects, were obtained from the Oral Health Research Institute at the Indiana University School of Dentistry (IUSD). Institutional approval is not needed/obtainable for this type of research. The use of animal tissues (dead animal parts) is exempt under the Animal Welfare Act (US Department of Agriculture/APHIS, Animal and Plant Health Inspection Service). The IUSD Institutional Animal Care and Use Committee (IACUC) does not review or approve research proposals of this type.
After selection, the teeth were rinsed thoroughly and stored in distilled water for 3–4 months at room temperature. The teeth were then sectioned at their cementoenamel junctions. Each crown was partially embedded in self-curing acrylic resin (Coe tray plastic, GC America, Alsip, Ill) within a chlorinated polyvinyl chloride (CPVC) pipe (3/4-inch outside diameter, 5/64-inch wall thickness, approximately 1.0 inch long; Genova Products, Rensselaer, Ind) with the facial enamel surface parallel to, and approximately 1 mm beyond, the cylinder rim. The exposed enamel surface was initially flattened with a model trimmer and then smoothed with progressively finer grit (240SiC, 400SiC, and 600SiC) silicon carbide (SiC) sandpaper on a Leco Vari/Pol machine (Leco, Saint Joseph, Mich) to provide a uniform bonding area. Teeth with exposed dentin were discarded.
The curved (10.2-mm2) bases of maxillary incisor brackets (0.022-inch slot, Victory Series low profile, stainless-steel, UR central incisor; 3M Unitek) were flattened by a process in which approximately 200 N was applied by an MTS Bionix 858 (MTS, Minneapolis, Minn) testing machine. After flattening, approximately 10% of the brackets were randomly chosen and viewed at 10× magnification to verify the absence of damage.
Bonding
Prior to bonding, the flattened enamel surfaces were cleaned for 15 seconds with pumice in a rubber cup and then rinsed in distilled water. The enamel was dried with oil- and moisture-free compressed air. The teeth were randomly allocated to each of the five study groups, as follows: T0 = no rubbing of the SEP and traditional tension; T5 = 5 seconds of rubbing (the manufacturer's recommendation) and traditional tension; T10 = 10 seconds of rubbing and traditional tension; T5c = 5 seconds of rubbing and LODI simulated tension on the distal-cervical wing; and T5i = 5 seconds of rubbing and LODI simulated tension on the distal-incisal wing. Accepting a P value of ≤.05, the study required 20 specimens per group for 80% power. Thus, when including 10 spares that were distributed among the five groups, a total of 110 specimens were prepared (Table 1).
Table 1.
Summary Statisticsa
The SEP was on all enamel bonding surfaces for a total of 10 seconds, but it was rubbed for 0, 5, or 10 seconds depending on the group. T0, T5, and T10 groups were compared for the effect of application time, while T5, T5c, and T5i groups were compared for the effect of debonding method. T5 served as a control in both comparisons.
The Transbond Plus self-etching primer was applied to the enamel surfaces of the incisors according to the groups and then a gentle flow of air for 1–2 seconds was used to thin and dry the primer.26 Resin composite adhesive (Transbond XT, 3M Unitek) was applied to the bracket base and seated on the enamel with a bonding jig that was designed to align the bracket base parallel to the tooth surface while maintaining a shim-controlled uniform (0.15-mm) cement thickness.9,19 Excess resin was removed with an explorer. The incisal, gingival, mesial, and distal sides were light-cured (Ortholux XT, Visible Light Curing Unit, 3M Unitek) for 20 seconds each. The procedures were carried out in an environmentally controlled room at 23.3°C ± 1.1°C and 54% ± 5% relative humidity. The completed specimens were then placed in distilled water for 3–4 weeks prior to debonding.
Debonding
The brackets were debonded on the MTS Bionix 858 testing machine at a crosshead speed of 0.05 mm/s with loops of 50-pound test fishing line (Spiderwire, Johnson Worldwide Associates, Mankato, Minn). For the traditional tension test, one end of a loop (approximately 80-inch circumference) was hooked under two wings of the bracket, threaded over a smooth pin on the actuator, and hooked under the remaining two bracket wings (Figure 2). This resulted in the bracket being approximately 20 inches from the actuator pin. The sliding of the fishing line allowed for some self-leveling of forces on the wings. For the LODI simulated debonding, one end of the loop was hooked under the disto-cervical or disto-incisal wing and then looped over the actuator pin of the testing machine and back to the same wing (Figure 3). In all instances, failure was recorded and reported in Newtons.
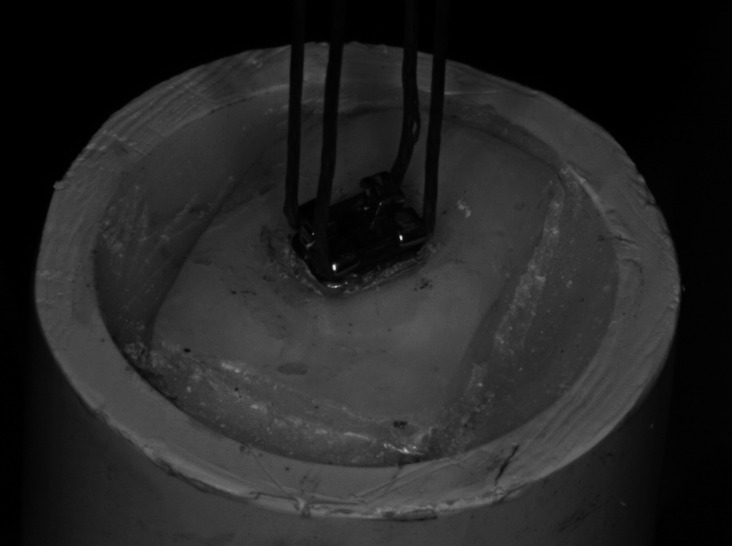
Figure 2.
Specimen under traditional tension. The flattened bracket was bonded to a flattened bovine incisor embedded in resin.
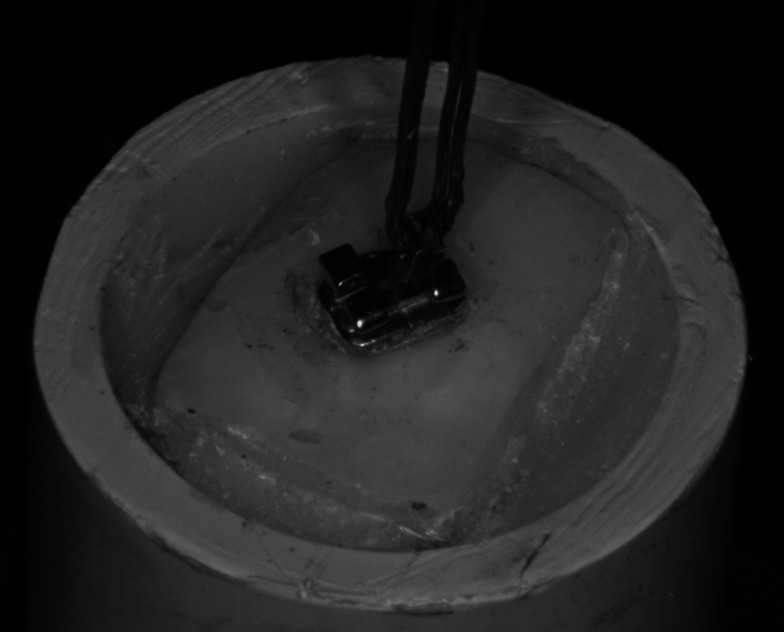
Figure 3.
Same as Figure 2, but for lift-off debonding instrument (LODI) simulation.
Adhesive Remnant Index
After debonding, the residual adhesive was assessed and scored according to the modified ARI27 as follows: 1 = all of the composite, with an impression of the bracket base, remains on the tooth; 2 = more than 90% of the composite remains on the tooth; 3 = more than 10% but less than 90% of the composite remains on the tooth; 4 = less than 10% of composite remains on the tooth; and 5 = no composite remains on the tooth.
Statistical Methods
The traditional tensile bond strengths were compared at 0, 5, and 10 seconds of rubbing. Comparisons between debonding methods were conducted at 5 seconds of rubbing. The mean bond strengths were evaluated using a one-way analysis of variance (ANOVA) to allow for comparisons between rubbing times as well as between debonding methods. ANOVA was also used to compare the ARI scores for differences in bond strength. Adjusted pairwise comparisons were made to determine the groups that were significantly different. P ≤ .05 was considered significant.
RESULTS
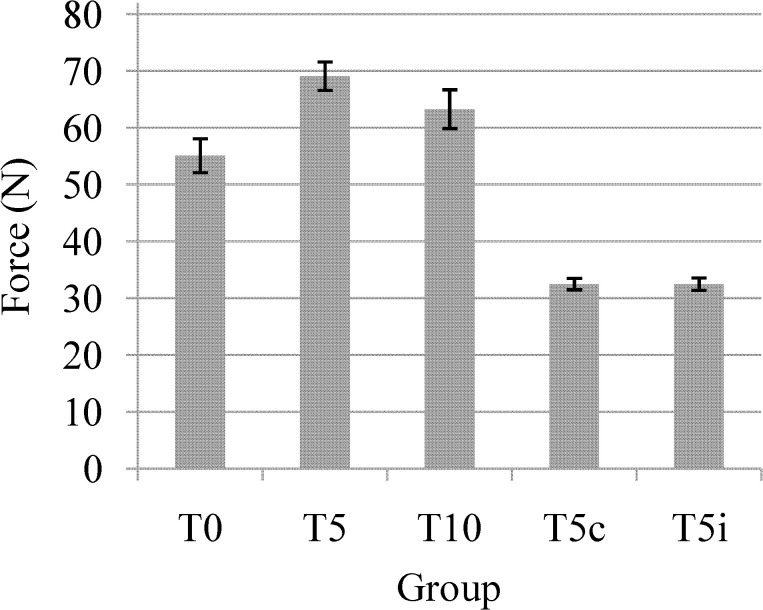
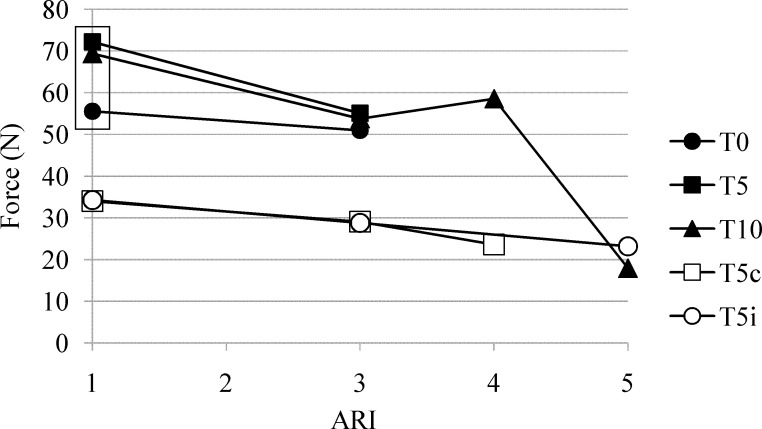
Bond strength summary statistics are presented in Table 1. The variation in time of rubbing of the self-etching primer had a significant effect on bond strength overall (P = .0064) and only between T5 and T0 (69.1 N vs 55.1 N; P = .0016; Figure 4).
Figure 4.
Mean (and standard error [SE]) tensile bond strengths.
The pairwise comparisons of debonding methods identified significant differences between T5 and T5c (69.1 N vs 32.5 N; P < .0001) and between T5 and T5i (69.1 N vs 32.5 N; P < .0001), but not between T5c and T5i (Figure 4).
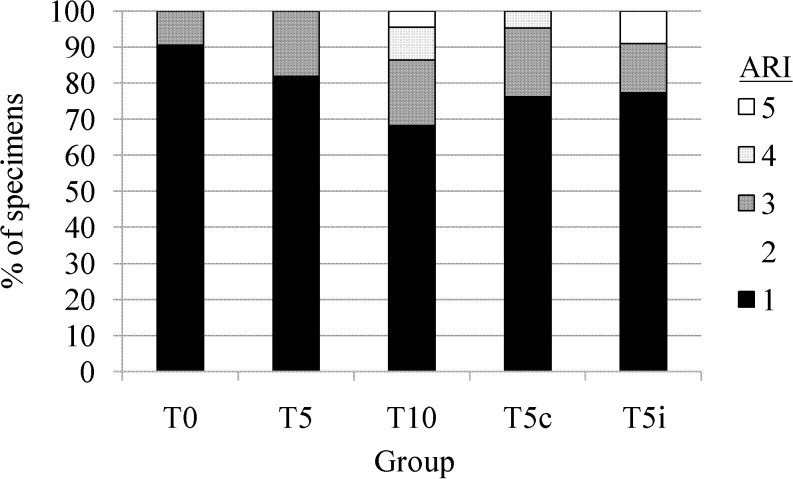
The ARI score and bond strength correlated for T5 (P = .0050), T10 (P = .0040), T5c (P = .0049), and T5i (P = .0007) but not for the T0 group (P = .67). The ARI score correlated with the bond strength for all rubbing time and debonding method groups combined (P = .0060). Bond strength was higher in the ARI = 1 subset compared to the ARI = 3–5 subsets (Figure 5). (There were no ARI = 2–type failures; Figure 6.)
Figure 5.
Mean strengths vs adhesive remnant index (ARI) scores.
Figure 6.
Adhesive remnant index (ARI) score distribution.
DISCUSSION
For cement thickness uniformity, brackets are manufactured with base curvatures to match the facial contours of specific generic human crowns. Unfortunately, this guarantees a mismatch with the broad, relatively flat surfaces of bovine teeth, the most widely used substitutes in orthodontic28–35 and other36–38 bonding studies. Our flattened bracket bases and crowns address this problem, and they also facilitate specimen alignment and bond thickness control.9,19
The results confirm the manufacturer's recommendations that Transbond Plus requires 5 seconds of rubbing during a 10-second application (T5) to produce the highest bond strengths among the times tested. The results also indicate that any rubbing increases the bond strength compared with no rubbing. This is concordant with the manufacturer's rationale that rubbing replenishes the depleted active ingredients of the Transbond Plus on the surface.39
All groups exhibited a general trend of decreasing bond strength with increasing ARI score (ie, as less and less of the cement remained on the tooth; Figure 5). Thus, within each group, the highest strengths occurred when all cement remained on the enamel (ARI = 1). Focusing on ARI = 1, there was a baffling statistical difference between the bond strengths of specimens that were rubbed (T5 and T10) and those that were not (T0). (This observation is based on 65%, 42/65, of all T0, T5, and T10 specimens [Figure 6], represented by the three data points within the box in Figure 5.) The question then becomes, why would the tensile strength be dependent on the preparation of the surface that remained intact?
We can only speculate that the ARI may reflect the end results of fracture propagation, not initiation. That is, there may be an initial enamel debond that is limited to a small area. Although not visually accessible, that detached region would allow a localized flexure of the cement layer. In turn, that may lead to concentrated stresses within the cement and/or at the bracket interface, ultimately resulting in the catastrophic failure. Thus, enamel surface preparation may exert its influence indirectly via that initial non-observed detachment from enamel. This, of course, requires further investigation, keeping in mind the complex stress fields within the structures.40
The secondary purpose of the study was to evaluate the forces needed to debond brackets using a simulated LODI. While the traditional laboratory tensile debonding test applies force to all four wings, in the LODI simulation, force was applied to one wing. The mean debonding forces on the disto-cervical and disto-incisal wings were not statistically different, demonstrating the irrelevance of this bracket's asymmetry in LODI debonding. The need for significantly lower (approximately half) debonding force verifies the higher stresses predicted by finite element analysis41 for such off-center loading.
CONCLUSIONS
This study supports the manufacturer's recommendations for the application of Transbond Plus.
LODI simulated tension requires significantly less debonding force, regardless of which wing is used.
Acknowledgments
We want to thank Robert W. Bandy, Dr James Baldwin, Dr James Shanks, and Dr Laura Parrish for their contributions and the 3M Unitek Company for the donation of brackets and adhesives. The study was partially supported by the Indiana University School of Dentistry Graduate Student Research Fund.
REFERENCES
- 1.Banks P, Thiruvenkatachari B. Long-term clinical evaluation of bracket failure with a self-etching primer: a randomized controlled trial. J Orthod. 2007;34:243–251. doi: 10.1179/146531207225022293. [DOI] [PubMed] [Google Scholar]
- 2.Bishara S. E, Oonsombat C, Soliman M. M, Warren J. J, Laffoon J. F, Ajlouni R. Comparison of bonding time and shear bond strength between a conventional and a new integrated bonding system. Angle Orthod. 2005;75:237–242. doi: 10.1043/0003-3219(2005)075<0233:COBTAS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Mao J, Qi J. Effect of saliva contamination on shear bond strength of orthodontic brackets when using a self-etch primer. J Huazhong Univ Sci Technol Med Sci. 2005;25:111–112. doi: 10.1007/BF02831404. [DOI] [PubMed] [Google Scholar]
- 4.Holzmeier M, Schaubmayr M, Dasch W, Hirschfelder U. A new generation of self-etching adhesives: comparison with traditional acid etch technique. J Orofac Orthop. 2008;69:78–93. doi: 10.1007/s00056-008-0709-6. [DOI] [PubMed] [Google Scholar]
- 5.Iijima M, Ito S, Yuasa T, Muguruma T, Saito T, Mizoguchi I. Bond strength comparison and scanning electron microscopic evaluation of three orthodontic bonding systems. Dent Mater J. 2008;27:392–399. doi: 10.4012/dmj.27.392. [DOI] [PubMed] [Google Scholar]
- 6.Bishara S. E, VonWald L, Laffoon J. F, Warren J. J. Effect of a self-etch primer/adhesive on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2001;119:621–624. doi: 10.1067/mod.2001.113269. [DOI] [PubMed] [Google Scholar]
- 7.Cal-Neto J. P, Carvalho F, Almeida R. C, Miguel J. A. Evaluation of a new self-etching primer on bracket bond strength in vitro. Angle Orthod. 2006;76:466–469. doi: 10.1043/0003-3219(2006)076[0466:EOANSP]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.da Costa C. C, Oshima H. M, Costa Filho L. C. Evaluation of shear bond strength and interfacial micromorphology of direct restorations in primary and permanent teeth—an in vitro study. Gen Dent. 2008;56:85–93; quiz 94–85, 111–112. [PubMed] [Google Scholar]
- 9.Gibb A. J, Katona T. R. A comparison of the shear-peel and third-order bond strengths of orthodontic brackets with 2 etch techniques and the role of bracket asymmetry. Am J Orthod Dentofacial Orthop. 2006;130:699.e1–699.e7. doi: 10.1016/j.ajodo.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 10.Huntley P. Long-term clinical evaluation of bracket failure with a self-etching primer: a randomized controlled trial. J Orthod. 2008;35:215–216; author reply 216. doi: 10.1179/jor.35.3.215b. [DOI] [PubMed] [Google Scholar]
- 11.Khalha A. No difference in the failure rates of orthodontic brackets bonded with self-etching primer. Evid Based Dent. 2008;9:79–80. doi: 10.1038/sj.ebd.6400598. [DOI] [PubMed] [Google Scholar]
- 12.Ostby A. W, Bishara S. E, Denehy G. E, Laffoon J. F, Warren J. J. Effect of self-etchant pH on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2008;134:203–208. doi: 10.1016/j.ajodo.2006.07.039. [DOI] [PubMed] [Google Scholar]
- 13.Sivakumar A, Gandhi S, Valiathan A. Long-term clinical evaluation of bracket failure with a self-etching primer: a randomized controlled trial. J Orthod. 2008;35:215; author reply 215. doi: 10.1179/146531207225022680. [DOI] [PubMed] [Google Scholar]
- 14.Reis A, dos Santos J. E, Loguercio A. D, de Oliveira Bauer J. R. Eighteen-month bracket survival rate: conventional versus self-etch adhesive. Eur J Orthod. 2008;30:94–99. doi: 10.1093/ejo/cjm089. [DOI] [PubMed] [Google Scholar]
- 15.Buyukyilmaz T, Usumez S, Karaman A. I. Effect of self-etching primers on bond strength—are they reliable? Angle Orthod. 2003;73:64–70. doi: 10.1043/0003-3219(2003)073<0064:EOSEPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Dorminey J. C, Dunn W. J, Taloumis L. J. Shear bond strength of orthodontic brackets bonded with a modified 1-step etchant-and-primer technique. Am J Orthod Dentofacial Orthop. 2003;124:410–413. doi: 10.1016/s0889-5406(03)00404-9. [DOI] [PubMed] [Google Scholar]
- 17.Ireland A. J, Knight H, Sherriff M. An in vivo investigation into bond failure rates with a new self-etching primer system. Am J Orthod Dentofacial Orthop. 2003;124:323–326. doi: 10.1016/s0889-5406(03)00403-7. [DOI] [PubMed] [Google Scholar]
- 18.Aljubouri Y. D, Millett D. T, Gilmour W. H. Six and 12 months' evaluation of a self-etching primer versus two-stage etch and prime for orthodontic bonding: a randomized clinical trial. Eur J Orthod. 2004;26:565–571. doi: 10.1093/ejo/26.6.565. [DOI] [PubMed] [Google Scholar]
- 19.Katona T. R, Long R. W. Effect of loading mode on bond strength of orthodontic brackets bonded with 2 systems. Am J Orthod Dentofacial Orthop. 2006;129:60–64. doi: 10.1016/j.ajodo.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 20.Lill D. J, Lindauer S. J, Tufekci E, Shroff B. Importance of pumice prophylaxis for bonding with self-etch primer. Am J Orthod Dentofacial Orthop. 2008;133:423–426, quiz 476 e422. doi: 10.1016/j.ajodo.2006.03.039. [DOI] [PubMed] [Google Scholar]
- 21.Montasser M. A, Drummond J. L, Evans C. A. Rebonding of orthodontic brackets. Part I, a laboratory and clinical study. Angle Orthod. 2008;78:531–536. doi: 10.2319/022307-90.1. [DOI] [PubMed] [Google Scholar]
- 22.Ostby A. W, Bishara S. E, Laffoon J, Warren J. J. Influence of self-etchant application time on bracket shear bond strength. Angle Orthod. 2007;77:885–889. doi: 10.2319/092006-383. [DOI] [PubMed] [Google Scholar]
- 23.Perdigao J, Gomes G, Lopes M. M. Influence of conditioning time on enamel adhesion. Quintessence Int. 2006;37:35–41. [PubMed] [Google Scholar]
- 24.Coley-Smith A, Rock W. P. Distortion of metallic orthodontic brackets after clinical use and debond by two methods. Br J Orthod. 1999;26:135–139. doi: 10.1093/ortho/26.2.135. [DOI] [PubMed] [Google Scholar]
- 25.Katona T. R, Moore B. K. The effects of load misalignment on tensile load testing of direct bonded orthodontic brackets—a finite element model. Am J Orthod Dentofacial Orthop. 1994;105:543–551. doi: 10.1016/s0889-5406(94)70138-5. [DOI] [PubMed] [Google Scholar]
- 26.UNITEK Instructions for Use—Transbond™ Plus Self Etching Primer. 2008 Available at: http://multimedia.3m.com/mws/mediawebserver?mwsId=66666UuZjcFSLXTtoxfan8z6EVuQEcuZgVs6EVs6E666666–&fn=011-581%20ML.pdf. [Google Scholar]
- 27.Bishara S. E, Olsen M, Von Wald L. Comparisons of shear bond strength of precoated and uncoated brackets. Am J Orthod Dentofacial Orthop. 1997;112:617–621. doi: 10.1016/s0889-5406(97)70226-9. [DOI] [PubMed] [Google Scholar]
- 28.Cehreli Z. C, Kecik D, Kocadereli I. Effect of self-etching primer and adhesive formulations on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 2005;127:573–579; quiz 625–576. doi: 10.1016/j.ajodo.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 29.Dall'Igna C. M, Marchioro E. M, Spohr A. M, Mota E. G. Effect of curing time on the bond strength of a bracket-bonding system cured with a light-emitting diode or plasma arc light. Eur J Orthod. 2011;33:55–59. doi: 10.1093/ejo/cjq027. [DOI] [PubMed] [Google Scholar]
- 30.Oesterle L. J, Shellhart W. C, Belanger G. K. The use of bovine enamel in bonding studies. Am J Orthod Dentofacial Orthop. 1998;114:514–519. doi: 10.1016/s0889-5406(98)70171-4. [DOI] [PubMed] [Google Scholar]
- 31.Sfondrini M. F, Cacciafesta V, Scribante A. Shear bond strength of fibre-reinforced composite nets using two different adhesive systems. Eur J Orthod. 2011;33:66–70. doi: 10.1093/ejo/cjq030. [DOI] [PubMed] [Google Scholar]
- 32.Fowler C. S, Swartz M. L, Moore B. K, Rhodes B. F. Influence of selected variables on adhesion testing. Dent Mater. 1992;8:265–269. doi: 10.1016/0109-5641(92)90097-v. [DOI] [PubMed] [Google Scholar]
- 33.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62:1076–1081. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 34.Reis A. F, Giannini M, Kavaguchi A, Soares C. J, Line S. R. Comparison of microtensile bond strength to enamel and dentin of human, bovine, and porcine teeth. J Adhes Dent. 2004;6:117–121. [PubMed] [Google Scholar]
- 35.Saleh F, Taymour N. Validity of using bovine teeth as a substitute for human counterparts in adhesive tests. East Mediterr Health J. 2003;9:201–207. [PubMed] [Google Scholar]
- 36.Cavalcanti A. N, Mitsui F. H, Ambrosano G. M, Marchi G. M. Influence of adhesive systems and flowable composite lining on bond strength of class II restorations submitted to thermal and mechanical stresses. J Biomed Mater Res B Appl Biomater. 2007;80:52–58. doi: 10.1002/jbm.b.30567. [DOI] [PubMed] [Google Scholar]
- 37.Muraguchi K, Shigenobu S, Suzuki S, Tanaka T. Improvement of bonding to bleached bovine tooth surfaces by ascorbic acid treatment. Dent Mater J. 2007;26:875–881. doi: 10.4012/dmj.26.875. [DOI] [PubMed] [Google Scholar]
- 38.Reeves G. W, Fitchie J. G, Hembree J. H, Jr, Puckett A. D. Microleakage of new dentin bonding systems using human and bovine teeth. Oper Dent. 1995;20:230–235. [PubMed] [Google Scholar]
- 39.UNITEK Transbond Plus Self-Etching Primer Frequently Asked Questions. 2003–2008 Available at: http://multimedia.3m.com/mws/mediawebserver?66666UuZjcFSLXTt4xTXMxT2EVuQEcuZgVs6EVs6E666666. [Google Scholar]
- 40.Katona T. R. A comparison of the stresses developed in tension, shear peel, and torsion strength testing of direct bonded orthodontic brackets. Am J Orthod Dentofacial Orthop. 1997;112:244–251. doi: 10.1016/S0889-5406(97)70251-8. [DOI] [PubMed] [Google Scholar]
- 41.Katona T. R. The effects of load location and misalignment on shear/peel testing of direct bonded orthodontic brackets—a finite element model. Am J Orthod Dentofacial Orthop. 1994;106:395–402. doi: 10.1016/S0889-5406(94)70061-3. [DOI] [PubMed] [Google Scholar]