Abstract
Objectives:
To test the hypothesis that the sagittal position of the anterior teeth has no effect on pharyngeal airway dimension or hyoid bone position and to investigate the influence of orthodontic retraction of the anterior teeth on each section of pharynx and hyoid position.
Materials and Methods:
Forty-four Class I bimaxillary protrusion adults, treated with preadjusted appliances and maximum anchorage after extraction of four premolars, were divided into two groups according to their vertical craniofacial skeletal patterns. Pretreatment and posttreatment variables were compared using paired t-test, and the relationship between pharyngeal airway size and dentofacial variables was analyzed using Pearson correlation coefficient. The changes of pharyngeal airway size and hyoid position after treatment were compared between two groups using independent t-test.
Results:
Upon retraction of the incisors, the upper and lower lips were retracted by 2.60 mm and 3.87 mm, respectively. The tip of upper incisor was retracted by 6.84 mm and lower incisor retracted by 4.95 mm. There was significant decrease in SPP-SPPW, U-MPW, TB-TPPW, V-LPW, VAL, C3H, and SH (P < .05). No statistically significant different changes were observed in the dentofacial structures, pharyngeal airway, and hyoid position between the two groups after the treatment. There was a significant correlation between the retraction distance of lower incisor and the airway behind the soft palate, uvula, and tongue.
Conclusions:
The pharyngeal airway size became narrower after the treatment. Extraction of four premolars with retraction of incisors did affect velopharyngeal, glossopharyngeal, hypopharyngeal, and hyoid position in bimaxillary protrusive adult patients.
Keywords: Pharyngeal airway, Hyoid bone, Bimaxillary protrusion, Cephalometrics
INTRODUCTION
Bimaxillary protrusion is a condition characterized by protrusive and proclined upper and lower incisors and a disharmonious profile. Cephalometric analysis generally shows an increased UL-E line, LL-E line, U1/FH, and L1/MP value.1
The negative perception of protruding lips and protrusive dentitions often leads such patients to seek orthodontic care to decrease protrusion and improve profile. For this objective, four premolars are often extracted to create room for retraction of anterior teeth,2 which changes not only tooth position but also hard and soft tissue components.3 Previous studies have shown a possible relationship between pharyngeal airway and skeletal structures, soft tissues, and musculature. For example, tongue position changed in the oral environment after mandibular setback surgery.4 Nasopharyngeal airway was increased with maxillary protraction in skeletal Class III children.5 Changes in the size of nasopharyngeal airway dimension have been reported following rapid maxillary expansion.6 In addition, controversial findings on the relationship between vertical craniofacial pattern and pharyngeal airway were also demonstrated.7,8
However, the effects of orthodontic treatment, specifically the effects of anterior tooth retraction on pharyngeal airway after extraction of four premolars in the bimaxillary protrusive patients, have seldom been discussed. A recent study indicated that orthodontic treatment with extraction of four premolars did not influence oropharyngeal airway volume in adolescents.9 The authors attributed the negative finding mainly to the pharynx growth. However, specific changes of the pharyngeal airway and hyoid bone position were not investigated. Another study by Germec-Cakan et al.10 reported a decrease of airway space behind the tip of soft palate and tongue in 13 subjects with extraction orthodontic treatment. Other sections of the pharynx, such as nasopharynx, hypopharynx, and airway length were not evaluated. It is well documented that significant dentofacial changes exist after such orthodontic treatment, including soft profile and incisor angulation. An alteration of incisors and soft tissue position could potentially affect tongue position and pharyngeal airway.9 Given the fact that the research is now increasingly defined by an evidence-based approach, it is worthwhile to investigate the influence of extraction orthodontic treatment on the pharyngeal airway.
The aim of this retrospective study was to investigate the influence of maximal retraction of anterior teeth on each section of pharyngeal airway dimension and hyoid position after extraction of four premolars in adults with bimaxillary protrusion. The differences in pharyngeal airway between various vertical craniofacial skeletal groups were also evaluated.
MATERIALS AND METHODS
Eighty-two patients who were clinically diagnosed with bimaxillary protrusion were chosen from the files of patients previously treated at the Department of Orthodontics, Peking University School and Hospital of Stomatology. From this patient sample, 44 patients (36 female and 8 male) who met the following selection criteria were included in this study:
Minimum age 16 years;
Skeletal Class I, Class I first molar, canine, and premolar relationship;
Well aligned arches with no or minimal crowding;
Increased UL-E line, LL-E line, U1/SN, and L1/MP value greater than two standard deviation above the mean;
Orthodontic treatment consisting of extraction of four first premolars;
Maximum anchorage and maximal retraction of anterior teeth;
No obvious hyperplasia of tonsils or adenoids on cephalograms;
Pre and post radiographs with good hard and soft tissue outlines and teeth in full occlusion, lips resting in natural position.
The mean preoperative age was 21.19 years with an overall range of 16–34 years. Informed consent forms were signed by each patient or their parents. The study proceeded with the approval of both the Institutional Review Board and the participants. No subjects had a history of previous orthodontic/orthopedic treatment or any cleft lip/palate. The patients and their parents were questioned about the medical history to exclude any patients with chronic mouth breathing, permanent snoring and tonsillectomy, or adenoidectomy.
All patients were treated with 0.022 × 0.028 inch preadjusted appliances after extraction of four first premolars. Anchorage was reinforced with maximum anchorage mechanics using headgears or mini-implants, depending upon the patients' compliance. All pretreatment and posttreatment cephalograms were taken from the same machine by the same operator and the linear magnification of the machine was 11%. The subjects were divided into two groups according to the FH/MP angle before treatment:
Group 1: Nonhyperdivergent, ie, FH/MP angle smaller than 30.5° (16 subjects)
Group 2: Hyperdivergent, ie, FH/MP angle larger than 30.5° (28 subjects)
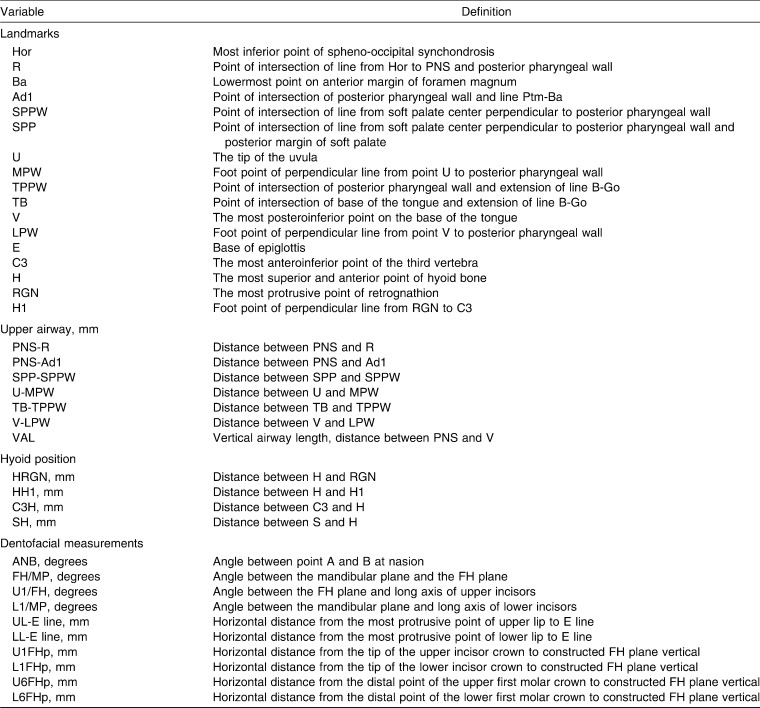
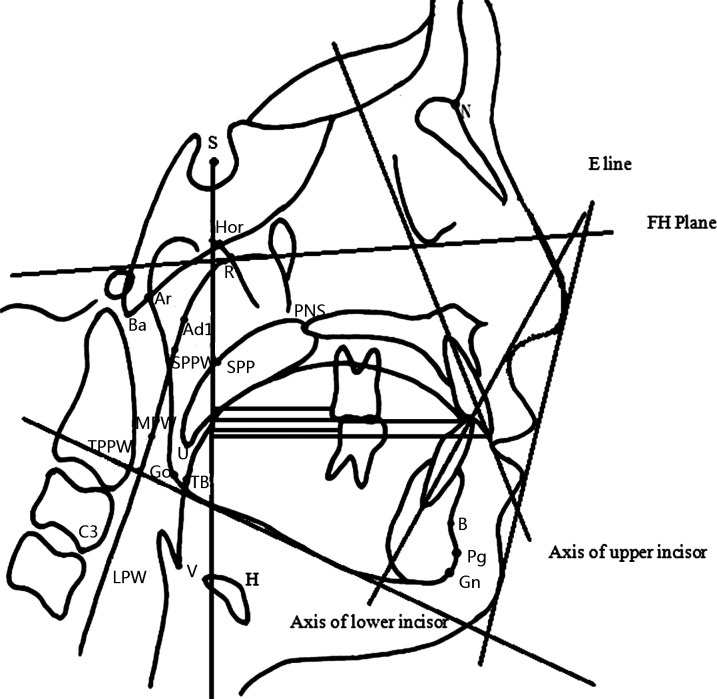
The pharynx consists of four different sections, nasopharynx, velopharynx, glossopharynx, and hypopharynx, each of which has it own components and surrounding structures. These four sections and hyoid position were evaluated, respectively. Correspondingly, 11 variables were selected, each with a specific clinical implication and answering a slightly different clinical question. The cephalometric landmarks and analyses (Table 1, Figures 1 and 2) were based on the methods described previously by Lowe et al.,11 Liu et al.,12 and Zhong et al.13 Two serial cephalograms from each subject were traced by the same investigator.
Table 1.
Cephalometric Landmarks and Measurements
Figure 1.
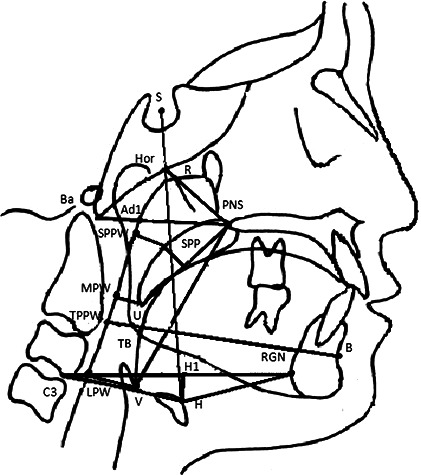
The cephalometric landmarks and analyses of pharyngeal airway.
Figure 2.
The cephalometric landmarks and analyses of dentofacial complex.
Evaluation of Error at Measuring and Calculation
To assess measurement error, the records of 44 subjects were reevaluated 8 weeks later. The mean differences were less than 1.0 mm and 1.0°, respectively. The standard error of a single measurement was calculated for each variable. The systematic error was determined using paired t-tests,14 and no statistically significant difference was found. Pearson correlation coefficients were calculated to evaluate the reliability of observations and showed a statistically significant range of 0.94 to 0.99.
Statistical Analysis
All statistical analyses were performed with software package SPSS (for Windows 7, version 16.0, SPSS, Chicago, Ill). Data were expressed as the mean and standard deviation (SD). Shapiro-Wilk test was applied to preoperative and postoperative measurements and showed a normally distributed population. Therefore, pretreatment vs posttreatment values were analyzed with paired t-test. The changes of pharyngeal airway and hyoid position after treatment were compared between two groups using independent t-test. Simple linear correlation analysis was performed to determine whether there was an association between the changes of pharyngeal airway measurements and those of dentofacial structures.
RESULTS
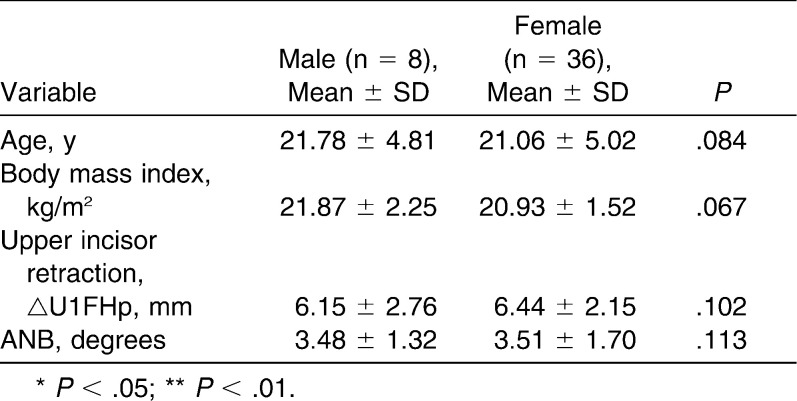
Demographic data showed no significant difference between the male and female groups (Table 2). The body mass index (BMI) was within normal limits (18.5 to 23.9 kg/m2).15
Table 2.
Data Between Male and Female Groups
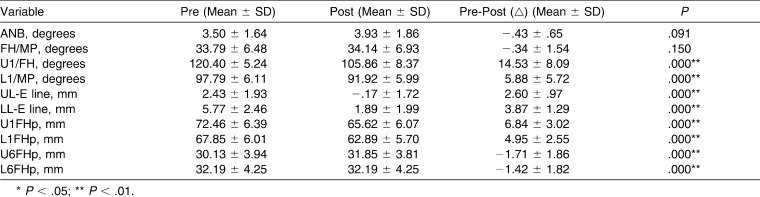
Upon retraction of the incisors (Table 3), the upper and lower lips were retracted by 2.60 mm (P < .0001) and by 3.87 mm (P < .0001), respectively. The mean decrease was 14.53° (P < .001) in the U1/FH angle and 5.88° (P < .001) in the L1/MP angle. The tip of the upper incisor was retracted by 6.84 mm (P < .001) and the tip of lower incisor was retracted by 4.95 mm (P < .001). However, the ANB angle and the mandibular plane angle (FH/MP) did not show any significant changes (P > .05).
Table 3.
Changes in Dentofacial Parameters Preoperatively and Postoperatively (n = 44)
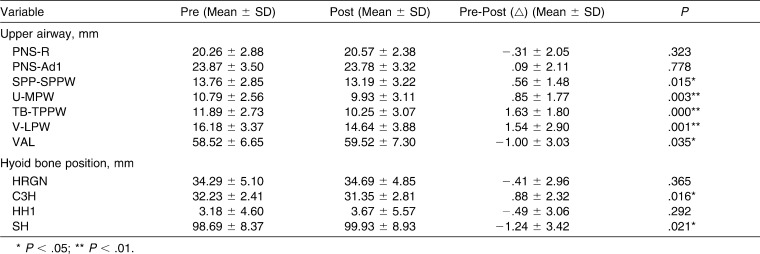
Table 4 shows the changes of pharyngeal airway and the hyoid bone position after the treatment. The results displayed a significant decrease in SPP-SPPW (P < .05), U-MPW (P < .01), TB-TPPW (P < .001), V-LPW (P < .01), VAL (P < .05), C3H (P < .05), and SH (P < .05), whereas changes in PNS-R, PNS-Ad1, HRGN, and HH1 showed no significant differences (P > .05). Velopharynx, glossopharynx, and hypopharynx were significantly reduced after treatment with the hyoid bone tending to move in a posterior and inferior direction.
Table 4.
Changes in Nasopharynx, Velopharynx, Glossopharynx, Hypopharynx, and Hyoid Bone Position (n = 44)
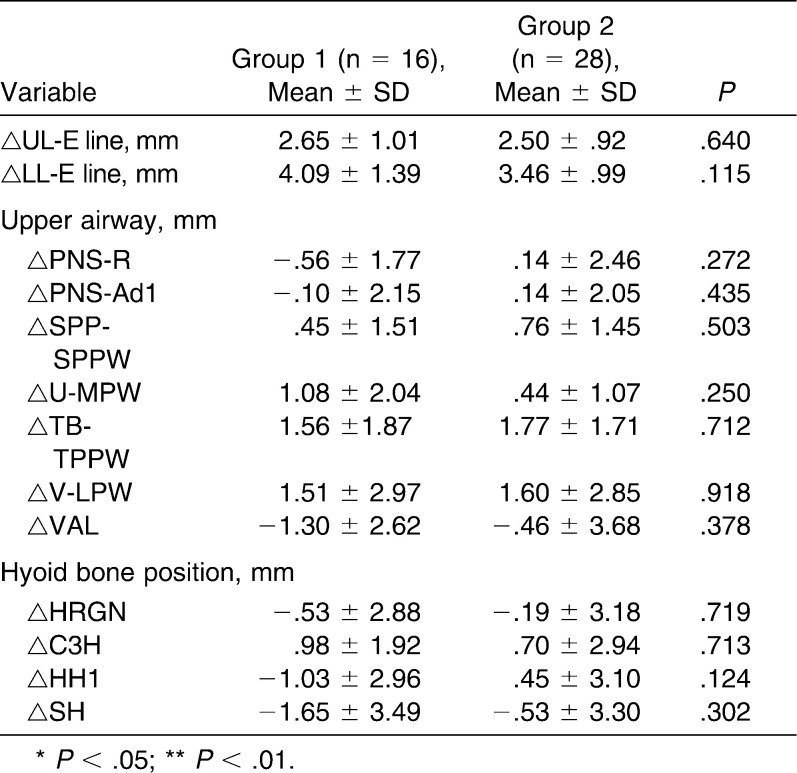
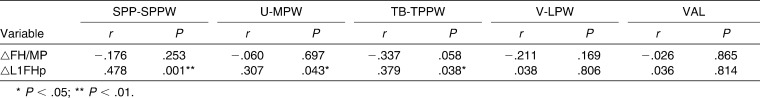
No statistically significant differences were observed in the retraction distance of the upper and lower lips and the tip of upper and lower incisor, ANB angle, FH/MP angle, pharyngeal airway, and the hyoid bone position between the hyperdivergent and nonhyperdivergent groups after the treatment as shown in Table 5. There was a significant correlation present between the retraction of the lower incisor and the airway behind the soft palate (SPP-SPPW), uvula (U-MPW), and the tongue (TB-TPPW) (Table 6).
Table 5.
Comparison of Changes in Nasopharynx, Velopharynx, Oropharynx, Hypopharynx, and Hyoid Bone Position Between Two Groups
Table 6.
Linear Correlation Analysis Between the Changes of Upper Airway and Those of Dentofacial Parameters (n = 44)
DISCUSSION
In the present study, the dimension of the velopharynx, glossopharynx, and hypopharynx were decreased after maximal retraction of anterior teeth with extraction of four premolars in bimaxillary protrusive patients, similar to the findings by Germec-Cakan et al.10 Both studies confirmed that maximal traction of the anterior teeth did influence pharyngeal airway dimension in adults. In addition, we also found a backward and downward movement of the hyoid bone.
However, our results differed from the result of a recent study by Valiathan et al.,9 who demonstrated oropharyngeal volumes did not show significant change after orthodontic treatment with extraction of four premolars in adolescents. The authors attributed this negative finding to mandibular growth and the high variability of oropharyngeal volume. Valiathan et al.9 did not specify the anchorage system used and tooth movement, while in our study, mini-implants or headgears were applied to ensure the maximal retraction of anterior teeth, which may partially explain the different results.
For the present study, although the mean reduction of pharyngeal airway size was around 15%, a significantly decreased reduction was found in a typical case of a 23-year-old man on velopharynx, glossopharynx, and hypopharynx. The size of SPP-SPPW was reduced by 9.2%, U-MPW by 10.1%, TB-TPPW by 33.3%, and V-LPW by 21.7% (Figure 3). Since all 44 patients were over 16 years of age, there is no growth potential in this population. In addition, all subjects suffered from bimaxillary protrusive malocclusion and the strategy of maximum anchorage was maintained, which inevitably improved the homogeneity of subjects. Dental outcomes exhibited statistically significant changes for anterior teeth after orthodontic treatment but extraction of four premolars did not cause significant bony changes. In conclusion, there is a relationship between the position of anterior teeth and the pharyngeal airway in adults.
Figure 3.
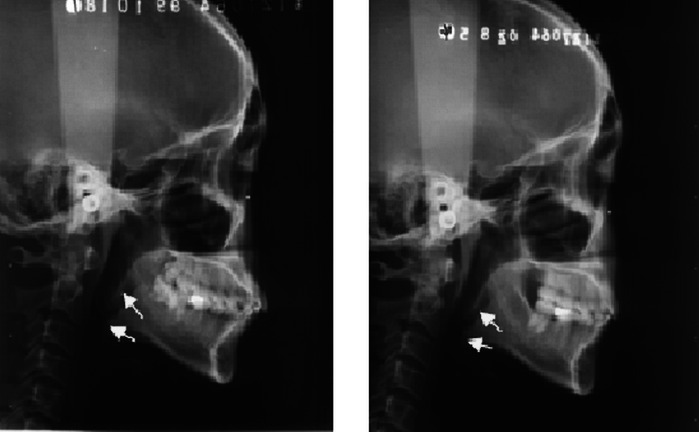
The pretreatment and posttreatment cephalograms of a typical case (left, pre; right, post).
Since patients with bimaxillary protrusion generally have perfectly good occlusion, orthodontic treatment is often solely sought to correct the protrusive profile and improve the facial esthetics. The clinical relevance of this study was that the clinicians must put the incisors in the most esthetic position to meet these patient demands. In this study, the tips of the incisors were measured, and the relationship between the changes of teeth and upper airway size was investigated. It is known that the arch width (intercanine distance and intermolar distance) does not change much after orthodontic treatment with extraction. The most change occurred in the sagittal plane of space, ie, arch length. Retraction of incisors contributes most to the decrease in arch length and change in the anterior boundary of the oral cavity.
Our study indicated that the pharyngeal airway size was decreased after retraction. Specifically, the nasopharynx did not change much. However, the velopharynx and glossopharynx were located between the soft palate, tongue, and bony cervical vertebrae. Any factors that can influence the posture and position of tongue and soft palate may displace them backward and encroach upon these two sections. Moreover, the significant correlation between retraction of lower incisors and the changes of the velopharynx and glossopharynx suggested the more the incisors were retracted, the more the pharyngeal airway was reduced. Therefore, it is safe to speculate that the retraction of anterior teeth decreases the arch length, causing dorsal movement of the anterior boundary of oral cavity. The soft palate and tongue muscle may exert a further influence on the velopharynx, glossopharynx, and hypopharynx behind them in an adaptation to this change.16 Thus, the respiratory form and size of the pharyngeal airway should be taken into consideration, especially when extraction of four premolars and maximal retraction of anterior teeth are planned.
Our findings confirmed that the horizontal spaces around the tongue were decreased with the downward movement of the hyoid bone caused by the retraction of incisors. The hyoid position depends on the relative balance of muscle attachment from the base of the cranium bilaterally and the region of the mandibular symphysis.17 The inferior movement of the hyoid bone seen in the present study is consistent with the findings of other studies, showing that this movement is an adaptation preventing an encroachment of the tongue into the pharyngeal airway.18
It has been found there is a positive correlation between the pharyngeal airway and the length and position of the mandible.19 Previous studies have also explored the relationship between pharyngeal airway dimension and mandibular plane angle. Ucara and Uysalb7 identified significant differences in orofacial airway dimensions of Class I subjects with different growth patterns, while Grauer et al.8 did not find the relationship between pharyngeal volume and facial morphology. In order to control this potential confounding factor, we divided the subjects into two groups according to vertical skeletal pattern. The present study showed no statistically significant differences in the changes of pharyngeal airway and the hyoid position between the two groups. The vertical craniofacial skeletal pattern may not be a contributory factor in the pharyngeal airway narrowing. Pharyngeal airway narrowing occurred in both of the two groups.
Nevertheless, it is unclear whether the decrease of pharyngeal airway and displacement of the tongue after more than 2 years of orthodontic treatment are a long-term stable adaptation or some radical changes as those after orthognathic surgical setback of the mandible in Class III malocclusion, in which decreased pharynx shows a trend to its original dimension. That is the limitation of the current pilot study, in which long-term changes are not determined. In addition, two-dimensional imaging was used to evaluate three-dimensional pharyngeal structure. However, there is a high correlation between lateral radiographs and three-dimensional magnetic resonance imaging scans when assessing the pharyngeal airway.20 Moreover, Miles et al.21 reported a high reliability of cephalometric landmarks and measurements. Thus, cephalograms are still widely used to evaluate the pharyngeal airway.5,7,13 Further studies may be aimed at long-term effects of orthodontic treatment on pharyngeal airway with three-dimensional imaging.
CONCLUSIONS
Following retraction of incisors, the velopharyngeal, glossopharyngeal, and hypopharyngeal airway became narrower.
The changes of the pharyngeal airway size were no different between the hyperdivergent and nonhyperdivergent groups.
The hyoid bone tends to move in a posterior and inferior direction.
A significant relationship has been demonstrated between the reduction of the velopharynx, glossopharynx, and the retraction distance of lower incisors in this study.
Acknowledgments
This study was supported by National Natural Science Foundation of China, 30500571, and Beijing Nova Program 2006A08.
REFERENCES
- 1.Ma J, Wang L, Zhang W, Chen W, Zhao C, Smales R. J. Comparative evaluation of micro-implant and headgear anchorage used with a pre-adjusted appliance system. Eur J Orthod. 2008;30:283–287. doi: 10.1093/ejo/cjm128. [DOI] [PubMed] [Google Scholar]
- 2.Kusnoto J, Kusnoto H. The effect of anterior tooth retraction on lip position of orthodontically treated adult Indonesians. Am J Orthod Dentofacial Orthop. 2001;120:304–307. doi: 10.1067/mod.2001.116089. [DOI] [PubMed] [Google Scholar]
- 3.Sharma J. N. Skeletal and soft tissue point A and B changes following orthodontic treatment of Nepalese Class I bimaxillary protrusive patients. Angle Orthod. 2010;80:91–96. doi: 10.2319/010409-6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawakami M, Yamamoto K, Fujimoto M, Ohgi K, Inoue M, Kirita T. Changes in tongue and hyoid positions, and posterior airway space following mandibular setback surgery. J Craniomaxillofac Surg. 2005;33:107–110. doi: 10.1016/j.jcms.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Lee J. W, Park K. H, Kim S. H, Park Y. G, Kim S. J. Correlation between skeletal changes by maxillary protraction and upper airway dimensions. Angle Orthod. 2011;81:426–432. doi: 10.2319/082610-499.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tecco S, Caputi S, Festa F. Evaluation of cervical posture following palatal expansion: a 12-month follow-up controlled study. Eur J Orthod. 2007;29:45–51. doi: 10.1093/ejo/cjl021. [DOI] [PubMed] [Google Scholar]
- 7.Ucara F. I, Uysal T. Orofacial airway dimensions in subjects with Class I malocclusion and different growth patterns. Angle Orthod. 2011;81:460–468. doi: 10.2319/091910-545.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grauer D, Cevidanes J. S. H, Styner M. A, Ackerman J. L, Proffit W. R. Pharyngeal airway volume and shape from cone-beam computed tomography: relationship to facial morphology. Am J Orthod Dentofacial Orthop. 2009;136:805–814. doi: 10.1016/j.ajodo.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valiathan M, El H, Hans M. G, Palomo M. J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–1074. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Germec-Cakan D, Taner T, Akan S. Uvulo-glossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. Eur J Orthod. 2010 Nov 30 doi: 10.1093/ejo/cjq109. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Lowe A. A, Ono T, Ferguson K. A, Pae E. K, Ryan C. F, Fleetham J. A. Cephalometric comparisons of craniofacial and upper airway structure by skeletal subtype and gender in patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 1996;110:653–664. doi: 10.1016/s0889-5406(96)80043-6. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Zeng X, Fu M, Huang X, Lowe A. A. Effects of a mandibular repositioner on obstructive sleep apnea. Am J Orthod Dentofacial Orthop. 2000;118:248–256. doi: 10.1067/mod.2000.104831. [DOI] [PubMed] [Google Scholar]
- 13.Zhong Z, Tang Z, Gao X, Zeng X. L. A comparison study of upper airway among different skeletal craniofacial patterns in nonsnoring Chinese children. Angle Orthod. 2010;80:267–274. doi: 10.2319/030809-130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Houston W. J. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 15.Chinese Medical Association Subsection of Cardiovascular Disease Chinese Journal of Cardiology Editorial Board. Highlights of the Second National Conference on Dyslipidemia. Chin J Cardiol. 2002;30:643–646. [Google Scholar]
- 16.Marsan G, Vasfi Kuvat S, Oztas E, Cura N, Susal Z, Emekli U. Oropharyngeal airway changes following bimaxillary surgery in Class III female adults. J Craniomaxillofac Surg. 2009;37:69–73. doi: 10.1016/j.jcms.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 17.Durzo C. A, Brodie A. G. Growth behavior of the hyoid bone. Angle Orthod. 1962;32:193–204. [Google Scholar]
- 18.Tselnik M, Pogrel M. A. Assessment of the pharyngeal airway space after mandibular setback surgery. J Oral Maxillofac Surg. 2000;58:282–285. doi: 10.1016/s0278-2391(00)90053-3. [DOI] [PubMed] [Google Scholar]
- 19.Muto T, Yamazaki A, Takeda S. A cephalometric evaluation of the pharyngeal airway space in patients with mandibular retrognathia and prognathia, and normal subjects. Int J Oral Maxillofac Surg. 2008;37:228–231. doi: 10.1016/j.ijom.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 20.Pirilä-Parkkinen K, Löppönen H, Nieminen P, Tolonen U, Pääkkö E, Pirttiniemi P. Validity of upper airway assessment in children: a clinical, cephalometric, and MRI study. Angle Orthod. 2011;81:433–439. doi: 10.2319/063010-362.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miles P. G, O'Reilly M, Close J. The reliability of upper airway landmark identification. Aust Orthod J. 1995;14:3–6. [PubMed] [Google Scholar]