Abstract
Gender impacts substance use initiation, substance use disorder development, engagement with treatment, and harms related to drug and alcohol use. Using the biopsychosocial model of addiction, this review provides a broad summary of barriers and facilitators to addiction services among women. It also reviews substance use among pregnant and parenting women and approaches to care. Given the increasing rates of substance use among women, there is a need to implement and scale-up gender-responsive addiction programming and pursue advocacy at the policy level that addresses the root drivers of substance use inequities among women.
Keywords: Women, Substance use disorders, Gender, Treatment
INTRODUCTION
Gender differences exist in the origins, development, course, and treatment of substance use disorders (SUD). Men have historically used alcohol and other substances more than women, and therefore, addiction services, research, and policies have primarily been either tailored to men or designed using a gender-neutral approach.1 Gender-neutral approaches tend to benefit men over women, as they fail to consider the specific needs of women. This is problematic, as the gender gap in SUD is narrowing.2,3 Over the past decade in the United States, metrics, such as rates of high-risk drinking and alcohol use disorder,4 opioid misuse and opioid overdoses rates,5,6,7 and methamphetamine-involved overdose rates,8 have all increased more rapidly in women than men. Given the narrowing gender gap, there have been increasing calls for clinical, public health, and research approaches that comprehensively address women-specific needs.1,9,10
Gender-based differences in SUD development, trajectories, health and psychosocial consequences, and treatment outcomes are well documented in the literature.11,12,13 Compared with men, women initiate drug and alcohol use at an older age and may exhibit a telescoping effect, that is, they more rapidly progress from initiation of substance use to the development of an SUD.14,15 Research has consistently demonstrated greater physical, psychological, and social harms of drug and alcohol use in women.16,17,18 For example, compared with men, women who inject drugs experience higher rates of injection drug use–associated infections, including HIV and hepatitis C.17,19 Worldwide, women account for approximately one-third of people with SUD but only one-fifth in SUD treatment, highlighting a treatment disparity.20
Here, the authors provide a broad overview of critical issues in SUD in women using the biopsychosocial model of addiction.21 From the wide range of issues relevant to women and SUD, they prioritize the following topics: (1) barriers and facilitators to addiction treatment and harm reduction services; (2) substance use while pregnant and parenting; and (3) gender-responsive addiction care.
Sex, Gender, And The Intersectionality Of Race
Understanding gender-based differences in substance use requires a comprehensive framework that recognizes the difference between sex and gender and encompasses the full spectrum of gender identity. “Sex” is the biological classification of a human as male or female based on their physical and physiologic attributes.22 “Gender” refers to socially constructed roles and behaviors that vary across societies and change over time.22 Gender identity refers to one’s internal sense of being a woman, man, or anywhere along the gender spectrum, including transgender, nonbinary, and genderqueer identities.23 In this article, “women” refers to all individuals who identify as a woman, regardless of their sex. However, it is recognized that compared with cisgender women, transgender and genderqueer individuals experience enhanced marginalization and discrimination based on their gender identity.18 Transgender and genderqueer women are twice as likely to misuse alcohol and other drugs compared with cisgender women.24 They also experience heightened risk for other SUD-related comorbidities, gender-based violence, suicide, and murder compared with cisgender women.25
There is also a need for a comprehensive and intersectional perspective that recognizes that women’s experiences with substance use are not homogeneous. Intersectionality affirms that sex and gender interact with race/ethnicity, class, sexual orientation, and other social categories to shape human experiences (Fig. 1).26 In particular, structural racism enhances stigma, discrimination, gender-based violence, and treatment barriers for Black, Indigenous, and other Women of Color compared with White women with SUD.27,28 Racism is a primary driver of drug law enforcement and public conceptions of drug use, and in the United States, Black Women are disproportionately targeted by laws and policies that reinforce racial inequities in the consequences of substance use.29,30
Figure 1.
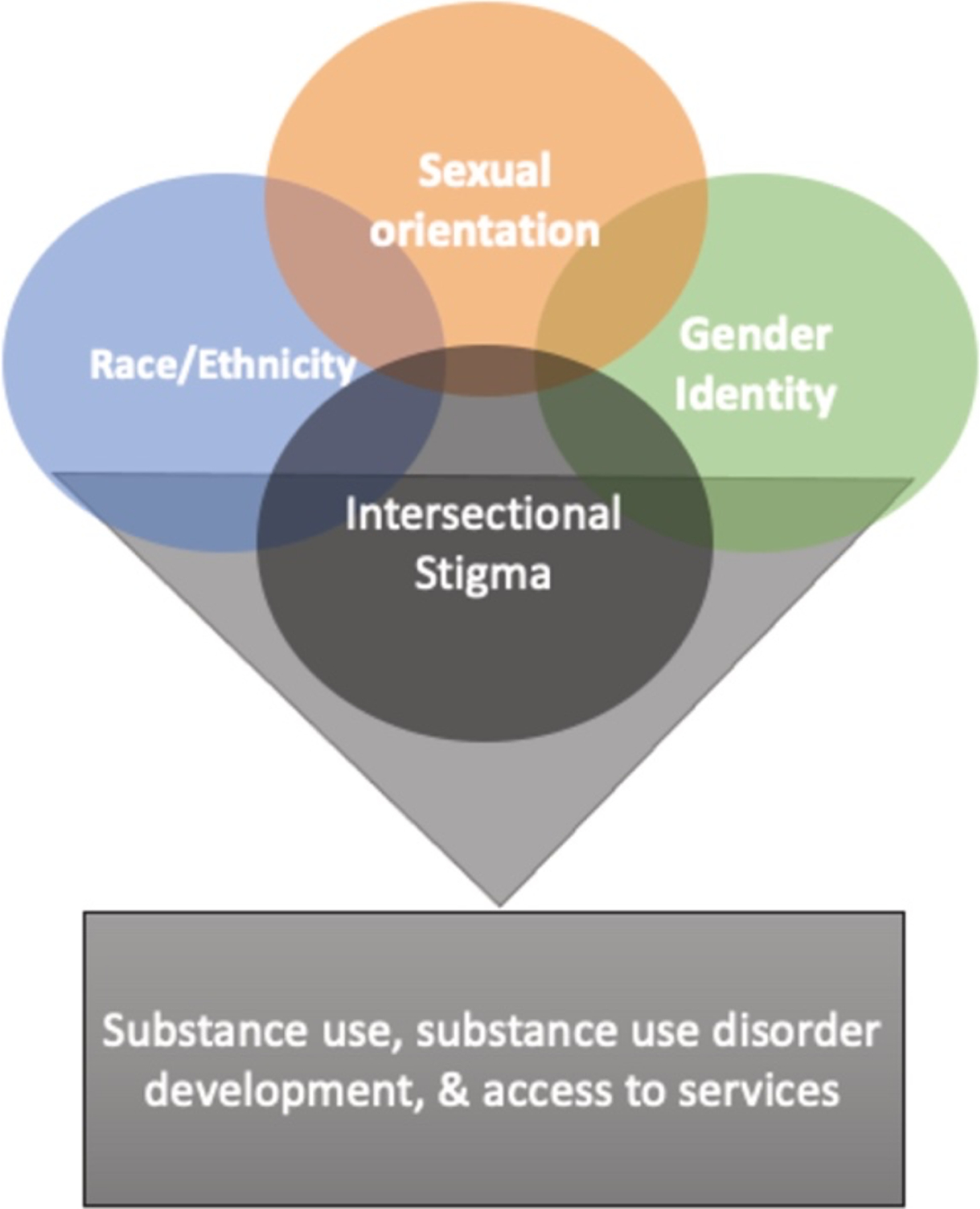
Intersectionality of sex, gender, race/ethnicity, and substance use
The Biopsychosocial Model Of Addiction
The authors use the biopsychosocial model of addiction that roots SUD as a product of the genetic, neurobiological, and social environment.21 This framework orients women’s experiences with substance use and addiction treatment across 4 dimensions: biological, psychological, social, and system structures (Fig. 2). The authors provide a high-level overview of each dimension. It is beyond the scope of the article to explore each dimension fully.
Figure 2.
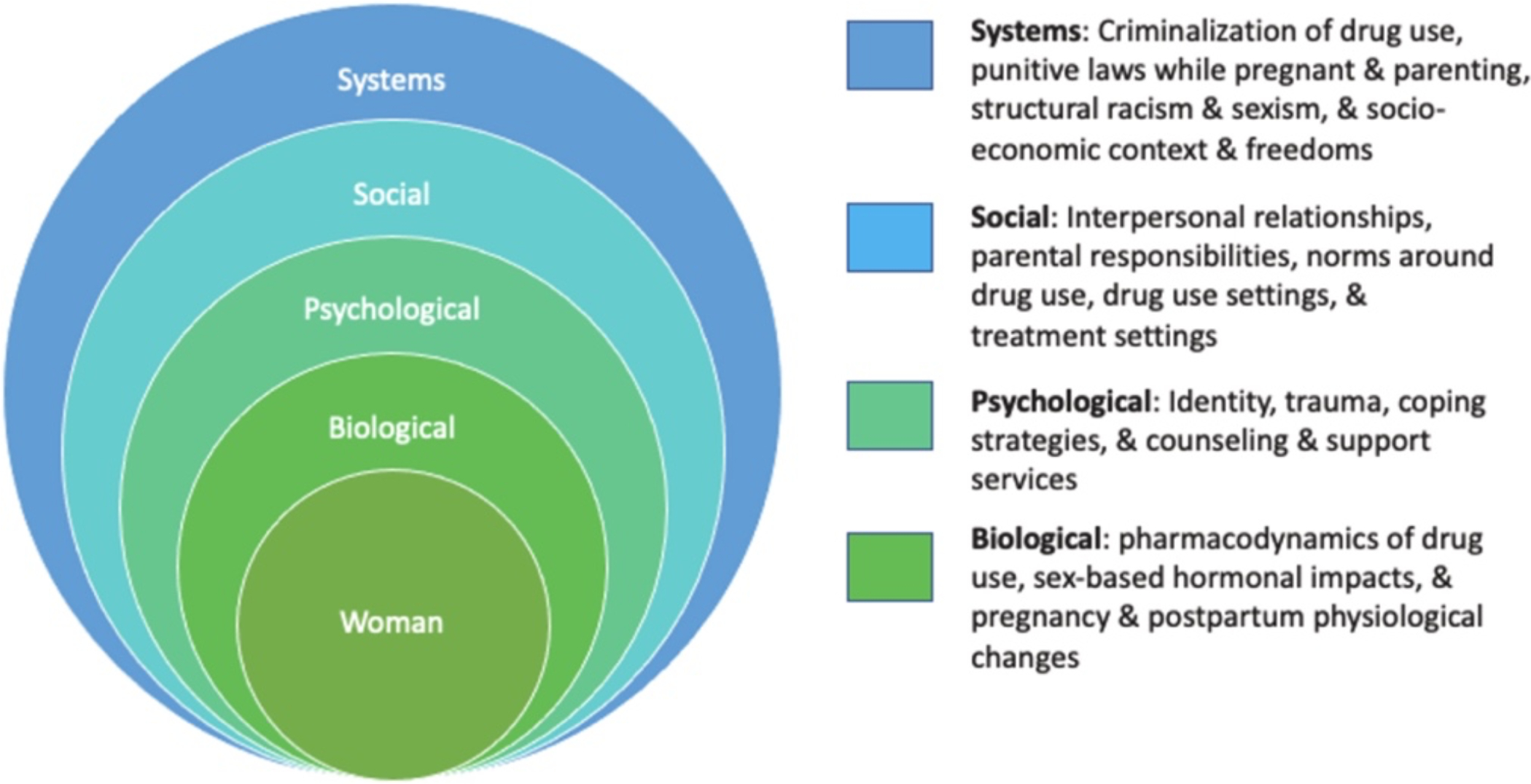
Biopsychosocial model of addiction and gender.
Biological
Sex differences exist in how men versus women respond biologically to alcohol and drugs in both the short and the long term.11 Different alcohol metabolism in men compared with women is the most consistent and well-understood finding. Women develop higher blood alcohol levels after drinking equivalent amounts of alcohol compared with men and are at higher risk of cirrhosis than men.31,32,33 The evidence on effects of sex hormones on subjective drug experiences is equivocal with no consistent differences found.11 In addition, associations between sex and neural responses to substances are not well studied, as most structural brain studies on addiction and substance use do not evaluate sex differences.34 Ongoing research to better understand the intersection of sex, genetics, and risks of substance use and addiction is needed.1
Psychological
In the psychological realm, women with SUD have higher rates of cooccurring psychiatric disorders, including mood disorders, posttraumatic stress disorder, and eating disorders.35,36 Women are also disproportionately affected by trauma and abuse.37,38 These experiences drive substance use initiation and persistent use.13,39
Social
Interpersonal relationships and communities substantially influence women’s substance use patterns. For example, women are more likely to start using substances if their intimate partner does so.40 Male-dominated street cultures influence women’s drug injection practices, whereby women are more likely than men to use assisted injection methods.41 Women who use drugs are also more likely than men to engage in sex work.42 Because of structural factors, such as the criminalization of sex work, sex work environments increase the risk of violence, trauma, and sexually transmitted infections.16
Systems
The criminalization of some substance use and sex work, and stigma surrounding these while pregnant and parenting disproportionately impact women.43,44 Women face increased policing and police violence while using illegal drugs and doing sex work that limits harm reduction behaviors and service utilization.45,46 Current punitive legal and child welfare approaches to substance use while pregnant and parenting reinforce stigma, discourage health care access, and perpetuate substance use among women.47,48
Barriers To Addiction And Harm Reduction Services
Women are less likely to enter substance use treatment compared with men relative to the prevalence of SUD in the general population.12 However, once in treatment, gender has not consistently been associated with differences in retention or substance use, suggesting women can and do benefit from treatment.12,49 Therefore, examining psychological, social, and systems barriers to treatment is critical to reducing disparities for women.
Psychological Barriers
Psychological factors, such as high rates of cooccurring trauma and severe mental illness, among women with SUDs can influence engagement with care.49,50 At least half of the women seeking treatment for SUD have experienced trauma and have a cooccurring mental illness.49 Women who use drugs and have experienced abuse are reluctant to seek care and have more unmet and complex health care needs when they present to care compared with those who have not experienced abuse.51,52 Nevertheless, SUD treatment services do not universally address trauma or have mental health services. The US 2019 National Survey of Substance Abuse Treatment Services found that only 70% of SUD treatment facilities offered some degree of mental health treatment services (Table 1).53 As defined in this survey, mental health services could be counseling alone and did not necessarily include access to psychiatric evaluation and vice versa. Unaddressed trauma and untreated mental illness reduce attendance and retention in SUD care.12
Table 1.
Availability of gender-responsive services among substance use disorder treatment programs, United States 2019a
| Ancillary Services | Percent of Facilities Offering Services |
|---|---|
| Case management | 96 |
| Mental health | 75 |
| Transportation assistance | 46 |
| Domestic violence | 38 |
| Childcare for client’s children | 6 |
| Residential bed for client’s children | 3 |
Data derived from the Substance Abuse and Mental Health Services Administration 2019 National Survey of Substance Abuse Treatment Services.53
Social Barriers
Harm reduction and other low-barrier treatment programs can become male-dominated, reproducing street-gendered relations and inequalities that limit women’s access to services.54 Women who use drugs are also more likely than their male counterparts to enter dependent and/or violent relationships dominated by their partner, hindering their economic freedom and autonomy to seek treatment.11,40 Substance use services often fail to take sufficient steps to counteract these gendered barriers. For example, despite evidence that gender-concordant providers improve entry into and continuation in treatment,55,56 1 national study of 108 methadone programs found that only 9% offered and matched clients to gender-concordant clinicians,51 and another study showed only 38% provided domestic violence services.53 Work force challenges, namely fewer women practicing addiction medicine, likely limit programs’ abilities to offer gender-concordant clinicians.
Systems Barriers
Enhanced surveillance and punitive policies for pregnant and parenting women increase stigma and disincentivize women from accessing treatment.48,57 Women also cite limited treatment options while pregnant, difficulty accessing childcare, and difficulty balancing rigid treatment schedules while fulfilling caretaking obligations as barriers to SUD treatment.48 The same 2019 US survey of SUD programs found that 24% offered treatment for pregnant or postpartum women, 6% provided child care for clients’ children, and 3% had residential beds for families (see Table 1).53 In addition, other structural determinants of health, such as housing instability, legal issues, and lack of transportation, disproportionately reduce women’s access to services compared with men.58 SUD services do not universally prioritize addressing these social determinants, for example, by paying for transportation to and from treatment, thereby reducing access for women.53,59
Facilitators To Addiction Treatment And Harm Reduction Services
Although there is robust literature documenting the gendered barriers to SUD treatment that women encounter, less research has focused on facilitators to treatment among women compared with men. The strengths-based approach, most notably used by social workers, highlights competencies, motivations, and social/environmental supports that facilitate engagement with care.60 A strengths-based approach recognizes that gender also positively influences women’s treatment engagement and outcomes.
Biological Facilitators
From a biological standpoint, women are more likely than men to engage in the health care system when they are young and healthy for preventive, sexual, and reproductive health needs.61 Women are more likely to have a regular clinician from whom they seek routine care and medical advice, which improves trust in the health care system.61 Regular engagement in medical services could facilitate screening for high-risk substance use, SUD diagnosis, and linkage to treatment for both SUD and psychiatric disorders.
Psychological Facilitators
Concerning psychological differences, the higher prevalence of cooccurring mood and anxiety disorders in women with SUD can present challenges, but also opportunities for engagement in mental health therapies that simultaneously improve SUD outcomes (eg, cognitive-behavioral therapy).62 Studies show women are more likely to seek and receive medical treatment for underlying psychiatric disorders than men, in part because of conventional gender norms that make it more acceptable for women to express strong emotions and engage in counseling.63,64 Use of antidepressants is more common in women than men.65 Engagement with mental health services and openness to treatment present opportunities to address substance use in women.
Social Facilitators
Socially, women’s recreational and community activities are less likely to center on alcohol or drug use, thus reducing their exposure to habitual substance use early in life.11 Women tend to form more intimate, supportive relationships with both friends and romantic partners.66 The ability to sustain relationships and mobilize social support is positively associated with individuals’ psychological well-being and capacity to cope with adverse events.67 In addition, although women’s role as caregivers can serve as a barrier to seeking SUD treatment, it can also be a facilitator; research has consistently demonstrated that the desire to maintain or regain child custody is a strong motivator for SUD treatment in women.12,68 Engaging and leveraging women’s community support networks provides an opportunity to increase treatment success.
System Facilitators
Finally, system-level factors can also facilitate SUD treatment among women. Women-led policy and community efforts that seek to reduce substance use harm inequities have a long and strong history in many communities. Women-led community organizations designed for women who use drugs and women engaged in sex work improve health outcomes and engagement in care, as they are perceived as safe and welcoming spaces for women.69,70 Thoughtful policies and programs that prioritize the well-being of the fetus and parent-infant dyad provide investment opportunities to expand women-only and family-based treatment programming.71
Substance Use Among Pregnant And Parenting Women
Pregnancy
The 2019 National Survey of Drug Use and Health data found, in the last month, 5.8% of pregnant women reported illicit substance use, 9.6% reported tobacco product use, and 9.5% reported alcohol use.72 Although pregnant women report less substance use than nonpregnant women, the medical risks are greater. For example, women who use illicit drugs, alcohol, and tobacco are at greater risk of miscarriage and preterm delivery.73,74 Stimulant and alcohol use are associated with medical complications of pregnancy, such as gestational hypertension and preeclampsia.74 The consequences of cannabis use during pregnancy are less understood, but a large 2019 retrospective study found cannabis use was associated with an increased risk of preterm labor and placental abruption.75 Substance use during pregnancy also impacts the health of the developing fetus, which is well described elsewhere.74
Although pregnancy can be a strong motivator for treatment among women with SUD, punitive laws and practices regulating substance use during pregnancy are major barriers to accessing care. Thirty-six states recognize fetuses as potential victims of crime, and, in 2014, Tennessee became the first state to explicitly criminalize drug use during pregnancy.76 Data from 2021 show that 23 states and the District of Columbia classify drug use during pregnancy as child abuse; 3 states find drug use during pregnancy as grounds for civil commitment, and 25 states and the District of Columbia mandate reporting of prenatal drug use to child welfare services.77 Many of the mandated reporting laws include medications prescribed during pregnancy to treat opioid use disorder as a reason to file a report to child welfare.77 Such mandates alienate pregnant women from seeking care, and among those that do, discourage them from accepting lifesaving pharmacologic treatment for SUD.78,79 For Black, Indigenous, and pregnant Women of Color, the punitive nature of these mandates is compounded by institutional racism resulting in significantly more report filings and custody disruptions.80,81
Despite these barriers, pregnancy is a powerful catalyst for change and engagement with SUD treatment among women with SUD. A 2016 survey found 88% of pregnant women self-disclosed their substance use to their obstetric provider.82 SUD treatment that is individualized, responsive to the women’s context, and integrated with mental health and postpartum care is critical. However, many SUD treatment programs for pregnant women are not integrated with postpartum or pediatric care.68 The postpartum period can be particularly challenging for women with SUD given high rates of postpartum depression, fragmented transitions of care, lapses in insurance after delivery, physiologic changes impacting SUD treatment, and stress and shame related to neonatal withdrawal syndromes or loss of child custody.83,84 A 2019 study found that overdose risk was greatest 7 to 12 months following delivery compared with all other prenatal and postpartum periods.85
Breastfeeding
Breastfeeding is an important aspect of the postpartum period for women with SUD. There are specific advantages of breastfeeding for substance-exposed mother-infant dyads; for example, breastfeeding reduces the severity of neonatal-opioid withdrawal syndrome and decreases the need for pharmacologic treatment.86 Despite this, breastfeeding rates among women with SUD vary widely, in part because of restrictive breastfeeding guidelines.87 Current recommendations from the American Academy of Breastfeeding Medicine stipulate that in addition to women being engaged in prenatal care and stable in recovery, they should also have no record of substance use (by urine drug testing) 90 to 30 days before delivery.88 Such policies reduce the number of women who are supported in breastfeeding initiation.89
Although there are clear harms to breastfeeding by women with active substance use, substance use in the third trimester should not disqualify women who are not using substances at delivery and are motivated from initiating breastfeeding. A retrospective cohort study from 2020 showed that the predictive value for postpartum substance use based on urine drug testing from the third trimester was only 36%.90 Most substances are eliminated in hours to days rather than days to weeks from the maternal system.91 Therefore, women who discontinue substance use before delivery or during the delivery hospitalization could be supported to initiate breastfeeding. Women-centered recommendations paired with ongoing screening, home lactation visiting programs, and SUD treatment support could facilitate successful breastfeeding among substance-exposed mother-infant dyads.
Parenting
In the United States, between 55% and 70% of women in substance use treatment programs have children.72 The same stressors leading to drug and alcohol use and SUD development among women can be exacerbated when parenting. Namely, parents experience increases in stress, sleep deprivation, and economic responsibilities and often need to prioritize their children’s needs over their own SUD treatment and other health care needs.92
Integrated treatment programs are critical to supporting parenting women with SUD. Different models exist, but dyadic models, or programs that provide care to both parents and children, offer several advantages. Examples of such programs include the FOCUS program at the University of New Mexico and the FIR Square and Sheway programs in Vancouver, Canada.93,94 Both programs are medical homes for families that provide wrap-around services to women and their children up to ages 3 to 5. These programs focus on interdisciplinary care delivery, case management, community outreach, housing, and legal services.93 Integrated programs have been shown to increase treatment retention, reduce parenting stress, decrease substance use and relapse, increase self-esteem, and improve parenting knowledge.95
Gender-Responsive Addiction Care
Given the differences in the impact and patterns of substance use between women and men, it follows that clinical programs providing care for women who use drugs should reflect those differences. This can be called “gender-responsive care,” and for this review, is defined as patient-centered care that considers how gender has affected a woman’s experience with drug and alcohol use and treatment (Fig. 3). Even when clinical programs are not exclusively focused on women, any addiction treatment provider or program can ensure women receive care tailored to their needs by adopting specific approaches described in later discussion.
Figure 3.
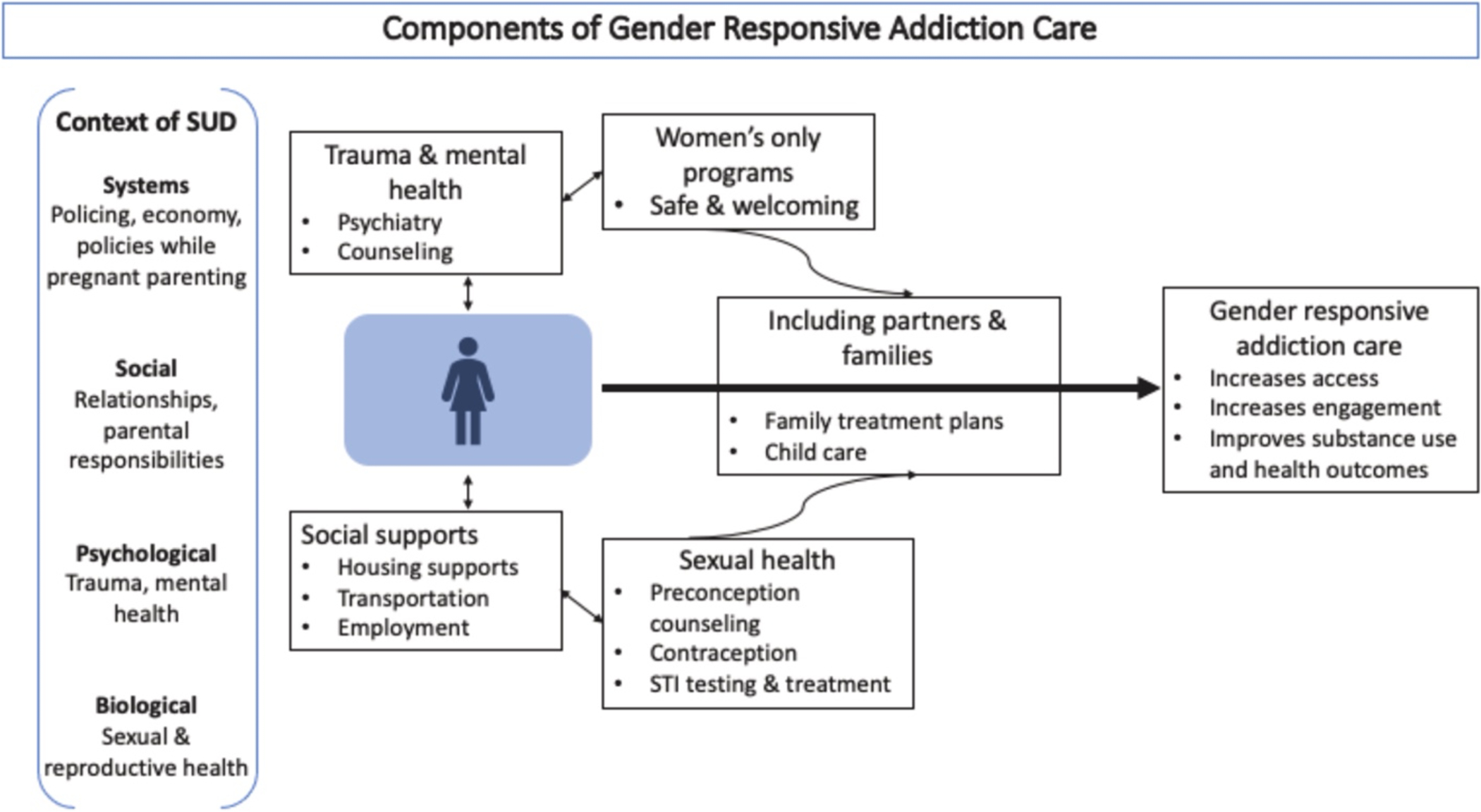
Gender-responsive care
Specific Components of Gender-Responsive Care
Trauma and mental health
As discussed earlier, cooccurring mental health disorders and trauma are high among women with SUDs. Programs should offer trauma-informed integrated treatment for cooccurring mental health disorders, including considering single-gender group therapy, which some women report creates a safer environment.
Sexual health
If available, programs should offer comprehensive reproductive and sexual health care. In addition to routine screening for sexually transmitted infections, age-appropriate cervical cancer screening, assessing pregnancy timing goals, and providing appropriate counseling for contraception or preconception should be offered. Addressing the sexual and reproductive health needs of women increases engagement with addiction treatment.96
Social needs
Different clinical programs will have varying capacities to respond to social needs affecting women. However, having the capacity to refer to clinical and community supports, such as housing services, life skills programs, and recovery management, is necessary. Wherever possible, providing childcare, transportation, and cell phones for those who need them can concretely increase access to care for women.
Women’s only programs
Women’s only treatment offers a safe environment that women may be more comfortable accessing. Programs unable to offer women’s only spaces all the time could alternatively offer select women’s only groups, days, or times for treatment or harm reduction services.97
Including partners and families
Data demonstrate the importance of including families and partners in treatment.98 Families can provide critical support for women outside of the clinical setting at home and in the community. When possible, this includes providing childcare services for parenting women.
Overall, gender-responsive care can mitigate many of the barriers to care described earlier. By acknowledging gender-based differences and tailoring care, treatment programs can provide care that meets women’s unique needs and improves their outcomes.
Summary
Women have unique, currently unmet, needs that impact their substance use initiation, SUD development trajectories, and harms related to drug and alcohol use. Implementing and scaling up gender-responsive addiction programming is critical given the evolving epidemiology of substance use among women, and evidence that shows gender-responsive services improve treatment outcomes.99 Additional investments in research to maintain and build multidisciplinary research programs that seek to address all aspects of the consequences of substance among women are needed.100 In addition, advocacy at the policy level to expand postpartum Medicaid coverage, expand funded parental leave, expand childcare benefits, and dismantle punitive policies that target pregnant and parenting women are needed to address the root drivers of substance use inequities and barriers to care among women.
Key points:
The substance use disorder gap between men and women is narrowing.
Gender-based differences in substance use disorder development, trajectories, health, and psychosocial consequences exist.
Gender-responsive care is patient-centered care that considers how gender has affected a woman’s experience with drug and alcohol use and treatment.
There is a need to implement and scale-up gender-responsive addiction programming.
Advocacy at the policy level to address the root drivers of substance use inequities among women is needed.
Acknowledgments
The authors acknowledge that the land where we work, live, teach, learn, and gather is the traditional territory of Massachusetts and their neighbors, the Wampanoag and Nipmuc Peoples, who have stewarded this land for hundreds of generations and continue to do so today.
Funding:
M.T.H. Harris is supported by the Research in Addiction Medicine Fellowship NIDA (R25DA033211-Samet) and the International Collaborative Addiction Medicine Research Fellowship (NIDA R25-DA037756-Fairburn).
Footnotes
Conflict of interest
None to declare.
REFERENCES
- 1.Meyer JP, Isaacs K, El-Shahawy O, et al. : Research on women with substance use disorders: reviewing progress and developing a research and implementation roadmap. Drug Alcohol Depend 2019; 197: pp. 158–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Keyes KM, Grant BF, Hasin DS: Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend 2008; 93: pp. 21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seedat S, Scott KM, Angermeyer MC, et al. : Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 2009; 66: pp. 785–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grant BF, Chou SP, Saha TD, et al. : Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 2017; 74: pp. 911–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones C, Logan J, Gladden M, et al. : Vital signs: demographic and substance use trends among heroin users — United States, 2002–2013. MMWR Morb Mortal Wkly Rep 2015; 64: pp. 719–725. [PMC free article] [PubMed] [Google Scholar]
- 6.VanHouten JP: Drug overdose deaths among women aged 30–64 years — United States, 1999–2017. MMWR Morb Mortal Wkly Rep 2019; 68: pp. 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vital signs: overdoses of prescription opioid pain relievers --- United States, 1999--2008. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm Accessed February 28, 2021 [PubMed]
- 8.Han B, Cotto J, Etz K, et al. : Methamphetamine overdose deaths in the US by sex and race and ethnicity. JAMA Psychiatry 2021; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyers SA, Smith LR, Werb D: Preventing transitions into injection drug use: a call for gender-responsive upstream prevention. Int J Drug Policy 2020; 83: pp. 102836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collins AB, Bardwell G, McNeil R, et al. : Gender and the overdose crisis in North America: moving past gender-neutral approaches in the public health response. Int J Drug Policy 2019; 69: pp. 43–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McHugh RK, Votaw VR, Sugarman DE, et al. : Sex and gender differences in substance use disorders. Clin Psychol Rev 2018; 66: pp. 12–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenfield SF, Brooks AJ, Gordon SM, et al. : Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug Alcohol Depend 2007; 86: pp. 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ait-Daoud N, Blevins D, Khanna S, et al. : Women and addiction: an update. Med Clin North Am 2019; 103: pp. 699–711. [DOI] [PubMed] [Google Scholar]
- 14.Hernandez-Avila CA, Rounsaville BJ, Kranzler HR: Opioid-, cannabis- and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug Alcohol Depend 2004; 74: pp. 265–272. [DOI] [PubMed] [Google Scholar]
- 15.Lewis B, Hoffman LA, Nixon SJ: Sex differences in drug use among polysubstance users. Drug Alcohol Depend 2014; 145: pp. 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park JN, Footer KHA, Decker MR, et al. : Interpersonal and structural factors associated with receptive syringe-sharing among a prospective cohort of female sex workers who inject drugs. Addiction 2019; 114: pp. 1204–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Bassel N, Strathdee SA: Women who use or inject drugs: an action agenda for women-specific, multilevel and combination HIV prevention and research. J Acquir Immune Defic Syndr 2015; 69: pp. S182–S190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinkham S, Malinowska-Sempruch K: Women, harm reduction and HIV. Reprod Health Matters 2008; 16: pp. 168–181. [DOI] [PubMed] [Google Scholar]
- 19.Degenhardt L, Peacock A, Colledge S, et al. : Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health 2017; 5: pp. e1192–e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United Nations Office on Drugs and Labor: World drug report 2020 (Set of 6 booklets). 2021. United Nations Geneva, Switzerland [Google Scholar]
- 21.Buchman DZ, Skinner W, Illes J: Negotiating the relationship between addiction, ethics, and brain science. AJOB Neurosci 2010; 1: pp. 36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Government of Canada CI of HR: What is gender? What is sex? - CIHR. Available at: https://cihr-irsc.gc.ca/e/48642.html Accessed March 5, 2021
- 23.General definitions. LGBT resource center. Available at: https://lgbt.ucsf.edu/glossaryterms Accessed March 5, 2021
- 24.Connolly D, Gilchrist G: Prevalence and correlates of substance use among transgender adults: a systematic review. Addict Behav 2020; 111: pp. 106544. [DOI] [PubMed] [Google Scholar]
- 25.Boyer TL, Youk AO, Haas AP, et al. : Suicide, homicide, and all-cause mortality among transgender and cisgender patients in the Veterans Health Administration. LGBT Health 2021; [DOI] [PubMed] [Google Scholar]
- 26.Hankivsky O: Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med 2012; 74: pp. 1712–1720. [DOI] [PubMed] [Google Scholar]
- 27.Waltermaurer E, Watson C-A, McNutt L-A: Black women’s health: the effect of perceived racism and intimate partner violence. Violence Women 2006; 12: pp. 1214–1222. [DOI] [PubMed] [Google Scholar]
- 28.Center for Substance Abuse Treatment: Substance abuse treatment: addressing the specific needs of women. 2009. Substance Abuse and Mental Health Services Administration (US) Available at: http://www.ncbi.nlm.nih.gov/books/NBK83252/ Accessed November 16, 2020 [PubMed] [Google Scholar]
- 29.Race & the war on drugs. American civil liberties union. Available at: https://www.aclu.org/other/race-war-drugs Accessed March 5, 2021
- 30.Knight KR: Structural factors that affect life contexts of pregnant people with opioid use disorders: the role of structural racism and the need for structural competency. Womens Reprod Health 2020; 7: pp. 164–171. [Google Scholar]
- 31.Chrostek L, Jelski W, Szmitkowski M, et al. : Gender-related differences in hepatic activity of alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in humans. J Clin Lab Anal 2003; 17: pp. 93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rehm J, Taylor B, Mohapatra S, et al. : Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev 2010; 29: pp. 437–445. [DOI] [PubMed] [Google Scholar]
- 33.Tapper EB, Parikh ND: Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ 2018; 362: pp. k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lind KE, Gutierrez EJ, Yamamoto DJ, et al. : Sex disparities in substance abuse research: evaluating 23 years of structural neuroimaging studies. Drug Alcohol Depend 2017; 173: pp. 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Conway KP, Compton W, Stinson FS, et al. : Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2006; 67: pp. 247–257. [DOI] [PubMed] [Google Scholar]
- 36.Mergler M, Driessen M, Havemann-Reinecke U, et al. : Differential relationships of PTSD and childhood trauma with the course of substance use disorders. J Subst Abuse Treat 2018; 93: pp. 57–63. [DOI] [PubMed] [Google Scholar]
- 37.Hien D, Cohen L, Campbell A: Is traumatic stress a vulnerability factor for women with substance use disorders?. Clin Psychol Rev 2005; 25: pp. 813–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Back SE, Payne RL, Wahlquist AH, et al. : Comparative profiles of men and women with opioid dependence: results from a national multisite effectiveness trial. Am J Drug Alcohol Abuse 2011; 37: pp. 313–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mburu G, Ayon S, Mahinda S, et al. : Determinants of women’s drug use during pregnancy: perspectives from a qualitative study. Matern Child Health J 2020; 24: pp. 11701178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mburu G, Limmer M, Holland P: Role of boyfriends and intimate sexual partners in the initiation and maintenance of injecting drug use among women in coastal Kenya. Addict Behav 2019; 93: pp. 20–28. [DOI] [PubMed] [Google Scholar]
- 41.Boyd J, Collins AB, Mayer S, et al. : Gendered violence and overdose prevention sites: a rapid ethnographic study during an overdose epidemic in Vancouver, Canada. Addict Abingdon Engl 2018; 113: pp. 2261–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chettiar J, Shannon K, Wood E, et al. : Survival sex work involvement among streetinvolved youth who use drugs in a Canadian setting. J Public Health 2010; 32: pp. 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldenberg S, Watt S, Braschel M, et al. : Police-related barriers to harm reduction linked to non-fatal overdose amongst sex workers who use drugs: results of a community-based cohort in Metro Vancouver, Canada. Int J Drug Policy 2020; 76: pp. 102618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duff P, Shoveller J, Chettiar J, et al. : Sex work and motherhood: social and structural barriers to health and social services for pregnant and parenting street and off-street sex workers. Health Care Women Int 2015; 36: pp. 1039–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Goldenberg S, Liyanage R, Braschel M, et al. : Structural barriers to condom access in a community-based cohort of sex workers in Vancouver, Canada: influence of policing, violence and end-demand criminalisation. BMJ Sex Reprod Health 2020; 46: pp. 301–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Odinokova V, Rusakova M, Urada LA, et al. : Police sexual coercion and its association with risky sex work and substance use behaviors among female sex workers in St. Petersburg and Orenburg, Russia. Int J Drug Policy 2014; 25: pp. 96–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Patrick SW, Schiff DM, Prevention C on SUA: A public health response to opioid use in pregnancy. Pediatrics 2017; 139: pp. e20164070. [DOI] [PubMed] [Google Scholar]
- 48.Stone R: Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice 2015; 3: pp. 1–15. [Google Scholar]
- 49.Greenfield SF, Pettinati HM, O’Malley S, et al. : Gender differences in alcohol treatment: an analysis of outcome from the COMBINE Study. Alcohol Clin Exp Res 2010; 34: pp. 1803–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huhn AS, Berry MS, Dunn KE: Review: sex-based differences in treatment outcomes for persons with opioid use disorder. Am J Addict 2019; 28: pp. 246–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zule WA, Lam WKK, Wechsberg WM: Treatment readiness among out-of-treatment African-American crack users. J Psychoactive Drugs 2003; 35: pp. 503–510. [DOI] [PubMed] [Google Scholar]
- 52.Substance Abuse and Mental Health Services Administration: Trauma-informed care in behavioral health services. 2014. Substance Abuse and Mental Health Services Administration; Rockville, MD: [PubMed] [Google Scholar]
- 53.Substance Abuse and Mental Health Services Administration: National survey of substance abuse treatment services (N-SSATS): 2019. Data on substance abuse treatment facilities. 2020. Substance Abuse and Mental Health Services Administration; Rockville, MD: Available at: https://www.samhsa.gov/data/data-we-collect/n-ssats-national-surveysubstance-abuse-treatment-services [Google Scholar]
- 54.Fairbairn N, Small W, Shannon K, et al. : Seeking refuge from violence in street-based drug scenes: women’s experiences in North America’s first supervised injection facility. Soc Sci Med 2008; 67: pp. 817–823. [DOI] [PubMed] [Google Scholar]
- 55.Marsh JC, Miller NA: Female clients in substance abuse treatment. Int J Addict 1985; 20: pp. 995–1019. [DOI] [PubMed] [Google Scholar]
- 56.Wechsberg W, Suerken C, Crum L, et al. : Availability of special services for women in methadone treatment: results from a national study 2001. 2001. The 129th Annual Meeting of the American Public Health Association Atlanta, GA [Google Scholar]
- 57.Roberts SC, Pies C: Complex calculations: how drug use during pregnancy becomes a barrier to prenatal care. Matern Child Health J 2011; 15: pp. 333–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Miguel AQC, Jordan A, Kiluk BD, et al. : Sociodemographic and clinical outcome differences among individuals seeking treatment for cocaine use disorders. The intersection of gender and race. J Subst Abuse Treat 2019; 106: pp. 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Grella CE, Greenwell L: Substance abuse treatment for women: changes in the settings where women received treatment and types of services provided, 1987–1998. J Behav Health Serv Res 2004; 31: pp. 367–383. [DOI] [PubMed] [Google Scholar]
- 60.Shaima N, Narayanan G: A glass half full not empty: strength-based practice in persons with substance use disorders. Psychol Stud 2018; 63: pp. 19–24. [Google Scholar]
- 61.Women and health care in the early years of the ACA: key findings from the 2013 Kaiser Women’s Health Survey. KFF. Available at: https://www.kff.org/womens-healthpolicy/report/women-and-health-care-in-the-early-years-of-the-aca-key-findings-fromthe-2013-kaiser-womens-health-survey/ Accessed March 5, 2021 [Google Scholar]
- 62.Horsfall J, Cleary M, Hunt GE, et al. : Psychosocial treatments for people with cooccurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry 2009; 17: pp. 24–34. [DOI] [PubMed] [Google Scholar]
- 63.Wendt D, Shafer K: Gender and attitudes about mental health help seeking: results from national data. Health Soc Work 2016; 41: pp. e20–e28. [Google Scholar]
- 64.Pattyn E, Verhaeghe M, Bracke P: The gender gap in mental health service use. Soc Psychiatry Psychiatr Epidemiol 2015; 50: pp. 1089–1095. [DOI] [PubMed] [Google Scholar]
- 65.Brody DJ: Antidepressant use among adults: United States, 2015–2018. NCHS Data Brief 2020; pp. 8. [PubMed] [Google Scholar]
- 66.Umberson D, Chen MD, House JS, et al. : The effect of social relationships on psychological well-being: are men and women really so different?. Am Sociol Rev 1996; 61: pp. 837–857. [Google Scholar]
- 67.Southwick SM, Sippel L, Krystal J, et al. : Why are some individuals more resilient than others: the role of social support. World Psychiatry 2016; 15: pp. 77–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sword W, Jack S, Niccols A, et al. : Integrated programs for women with substance use issues and their children: a qualitative meta-synthesis of processes and outcomes. Harm Reduct J 2009; 6: pp. 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Deering KN, Kerr T, Tyndall MW, et al. : A peer-led mobile outreach program and increased utilization of detoxification and residential drug treatment among female sex workers who use drugs in a Canadian setting. Drug Alcohol Depend 2011; 113: pp. 46–54. [DOI] [PubMed] [Google Scholar]
- 70.Kim SR, Goldenberg SM, Duff P, et al. : Uptake of a women-only, sex-work-specific drop-in center and links with sexual and reproductive health care for sex workers. Int J Gynaecol Obstet 2015; 128: pp. 201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Niv N, Hser Y-I: Women-only and mixed-gender drug abuse treatment programs: service needs, utilization and outcomes. Drug Alcohol Depend 2007; 87: pp. 194–201. [DOI] [PubMed] [Google Scholar]
- 72.Substance Abuse and Mental Health Services Administration: Key substance use and mental health indicators in the United States: results from the 2019 national survey on drug use and health. 2020. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Rockville, MD: Available at: https://www.samhsa.gov/data/ [Google Scholar]
- 73.Pineles BL, Park E, Samet JM: Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol 2014; 179: pp. 807–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Louw K-A: Substance use in pregnancy: the medical challenge. Obstet Med 2018; 11: pp. 54–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Corsi DJ, Walsh L, Weiss D, et al. : Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA 2019; 322: pp. 145152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murphy AS: A survey of state fetal homicide laws and their potential applicability to pregnant women who harm their own fetuses. Indiana Law J 2014; 89: pp. 847. [Google Scholar]
- 77.Guttmacher Institute: New York, NY: Substance use during pregnancy. 2021. Guttmacher Institute; Available at: https://www.guttmacher.org/print/statepolicy/explore/substance-use-during-pregnancy Accessed April 1, 2021 [Google Scholar]
- 78.Kozhimannil KB, Dowd WN, Ali MM, et al. : Substance use disorder treatment admissions and state-level prenatal substance use policies: evidence from a national treatment database. Addict Behav 2019; 90: pp. 272–277. [DOI] [PubMed] [Google Scholar]
- 79.Hui K, Angelotta C, Fisher CE: Criminalizing substance use in pregnancy: misplaced priorities. Addiction 2017; 112: pp. 1123–1125. [DOI] [PubMed] [Google Scholar]
- 80.Harp KLH, Bunting AM: The racialized nature of child welfare policies and the social control of black bodies. Soc Polit 2020; 27: pp. 258–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Harp KLH, Oser CB: A longitudinal analysis of the impact of child custody loss on drug use and crime among a sample of African American mothers. Child Abuse Negl 2018; 77: pp. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.McCarthy JJ, Leamon MH, Finnegan LP, et al. : Opioid dependence and pregnancy: minimizing stress on the fetal brain. Am J Obstet Gynecol 2017; 216: pp. 226–231. [DOI] [PubMed] [Google Scholar]
- 83.Chapman SLC, Wu L-T: Postpartum substance use and depressive symptoms: a review. Women Health 2013; 53: pp. 479–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pace CA, Kaminetzky LB, Winter M, et al. : Postpartum changes in methadone maintenance dose. J Subst Abuse Treat 2014; 47: pp. 229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schiff DM, Nielsen T, Terplan M, et al. : Fatal and nonfatal overdose among pregnant and postpartum women in Massachusetts. Obstet Gynecol 2018; 132: pp. 466–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Welle-Strand GK, Skurtveit S, Jansson LM, et al. : Breastfeeding reduces the need for withdrawal treatment in opioid-exposed infants. Acta Paediatr 2013; 102: pp. 1060–1066. [DOI] [PubMed] [Google Scholar]
- 87.Tsai LC, Doan TJ: Breastfeeding among mothers on opioid maintenance treatment: a literature review. J Hum Lact 2016; 32: pp. 521–529. [DOI] [PubMed] [Google Scholar]
- 88.Reece-Stremtan S, Marinelli KA: ABM clinical protocol #21: guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med 2015; 10: pp. 135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wachman EM, Saia K, Humphreys R, et al. : Revision of breastfeeding guidelines in the setting of maternal opioid use disorder: one institution’s experience. J Hum Lact 2016; 32: pp. 382–387. [DOI] [PubMed] [Google Scholar]
- 90.Harris M, Joseph K, Hoeppner B, et al. : A retrospective cohort study examining the utility of perinatal urine toxicology testing to guide breastfeeding initiation. J Addict Med 2020; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.D’Apolito K: Breastfeeding and substance abuse. Clin Obstet Gynecol 2013; 56: pp. 202211. [DOI] [PubMed] [Google Scholar]
- 92.Barlow J, Sembi S, Parsons H, et al. : A randomized controlled trial and economic evaluation of the parents under pressure program for parents in substance abuse treatment. Drug Alcohol Depend 2019; 194: pp. 184–194. [DOI] [PubMed] [Google Scholar]
- 93.Stulac S, Bair-Merritt M, Wachman EM, et al. : Children and families of the opioid epidemic: under the radar. Curr Probl Pediatr Adolesc Health Care 2019; 49: pp. 100637. [DOI] [PubMed] [Google Scholar]
- 94.Marshall SK, Charles G, Hare J, et al. : Sheway’s services for substance using pregnant and parenting women: evaluating the outcomes for infants. Can J Commun Ment Health 2005; 24: pp. 19–34. [DOI] [PubMed] [Google Scholar]
- 95.Moreland AD, McRae-Clark A: Parenting outcomes of parenting interventions in integrated substance-use treatment programs: a systematic review. J Subst Abuse Treat 2018; 89: pp. 52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wright TE: Integrating reproductive health services into opioid treatment facilities: a missed opportunity to prevent opioid-exposed pregnancies and improve the health of women who use drugs. J Addict Med 2019; 13: pp. 420–421. [DOI] [PubMed] [Google Scholar]
- 97.Greenfield SF, Sugarman DE, Freid CM, et al. : Group therapy for women with substance use disorders: results from the Women’s Recovery Group Study. Drug Alcohol Depend 2014; 142: pp. 245–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bagley SM, Ventura AS, Lasser KE, et al. : Engaging the family in the care of young adults with substance use disorders. Pediatrics 2021; 147: pp. S215–S219. [DOI] [PubMed] [Google Scholar]
- 99.Ashley OS, Marsden ME, Brady TM: Effectiveness of substance abuse treatment programming for women: a review. Am J Drug Alcohol Abuse 2003; 29: pp. 19–53. [DOI] [PubMed] [Google Scholar]
- 100.Wechsberg WM: Promising international interventions and treatment for women who use and abuse drugs: focusing on the issues through the InWomen’s Group. Subst Abuse Rehabil 2012; 3: pp. 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


