Abstract
Objective
To explore how COVID-19 influenced the provision of high-quality maternity care in Indonesia.
Design and methods
A qualitative descriptive study using in-depth interviews was undertaken. Thematic analysis was used to analyse data, and behaviour change frameworks (Theoretical Domain Framework (TDF) and Capability, Opportunity, and Motivation (COM-B)) were used to identify and map facilitators and barriers influencing maternity care provision during the COVID-19 pandemic.
Setting and participants
Fifteen midwives working in community maternity care facilities in Surabaya and Mataram, Indonesia were included. Surabaya is in western Indonesia, with around 56,000 births per year and a population of around 3 million. Mataram is in eastern Indonesia, with around 7,000 births per year and a population of around 500,000.
Findings
The main changes to maternity care provision during the COVID-19 pandemic were reduced frequency of antenatal and postpartum care visits, reduced support for women, including unavailability of maternity care and reduced number of antenatal care and labour companions, changes in location of provision of care, and public health changes related to COVID-19. The main factors influencing the provision of high-quality maternity care during the COVID-19 pandemic were behavioural regulation, professional role and identity, and environmental context and resources.
Key conclusions and implications for practice
Maternity care provision underwent substantial changes during the COVID-19 pandemic in Indonesia. Findings from this study can contribute to better understanding of how maternity care provision changed during the pandemic, and how positive changes can be reinforced, and negative changes can be addressed.
Keywords: Maternity care, Quality of care, COVID-19 pandemic, Midwives, Indonesia
Introduction
Women have the right to receive high quality maternity care – including during the COVID-19 pandemic – in order to have a positive pregnancy experience and healthy outcomes for themselves and their babies (WHO, 2016a; WHO and UNFPA, 2020). However, the pandemic has resulted in changes in how maternity care is provided in many places across the world. This includes moving in-person to online consultations and reducing timing and frequency of antenatal and postpartum care visits (Coxon et al., 2020; Sweet et al., 2021b). Although COVID-19 public health control and prevention measures justify some changes to care provision, many have significantly impacted women's experiences of care, and the outcomes for themselves and their babies. Many women are having pregnancy care (Panda et al., 2021; Sweet et al., 2021a) and going through labour and birth alone (Asefa et al., 2021) which can have profound impacts on feelings of isolation for women, potential for mistreatment during birth, and negative childbirth experience and outcomes. Ensuring quality of maternity care during the COVID-19 pandemic is crucial to maintain women's rights, and more work is needed to assess how COVID-19 has impacted on the provision of care.
Indonesia experienced two devastating waves of COVID-19 infections between January-February and June-September 2021 (Indonesia's COVID-19 task force, 2021), and as of December 2021, has recorded over four million cumulative COVID-19 cases (WHO, 2021). However, there has been limited exploration of the impact of COVID-19 on maternal and newborn health in Indonesia. Few studies investigating maternity care provision during the pandemic in Indonesia observed some changes, including a limitations in the number of women who could receive antenatal care per day, reductions in opening hours for primary health centres, limitations on companions during in-person antenatal care, and COVID-19 screening for pregnant women (Helmyati et al., 2022; Johariyah et al., 2020; Widiasih et al., 2021). In addition, Hazfiarini et al. (2021) documented the impacts of COVID-19 on midwives’ perspectives and experiences in providing maternity care. Johariyah et al. (2020) also reported just over half of midwives provided reduced number of antenatal care visits, but no information was provided on the number of recommended visits during the pandemic or how midwives monitored pregnant women given the reduced visits. To address these gaps, our study aimed to provide a more detailed understanding of how COVID-19 influenced maternity care provision in Indonesia, and map these factors influencing care using behaviour change frameworks.
Methods
Study design
We conducted a qualitative study adopting a constructivist paradigm (Broom and Willis, 2007). Constructivist paradigms focus on subjective meanings and interpretations which enabled our study participants to articulate their experiences and allow us to gain in-depth understanding. This study is reported according to the consolidated criteria for reporting qualitative research [COREQ] (Tong et al., 2007) (Appendix 1). The detailed methods of this study are reported elsewhere (Hazfiarini et al., 2021) and summarised below. This study received formal ethics approval in Australia and Indonesia.
Study sites
In Indonesia, primary maternity care is provided at community maternity health facilities, which are puskesmas (primary health centre), puskesmas pembantu (auxiliary puskesmas), mobile puskesmas, poskesdes/poskeskel (village health post) or polindes (village-level birth facility), and posyandu (integrated service posts) (Mahendradhata et al., 2017). Midwives working at the primary health centre are responsible for providing care at auxiliary puskesmas and mobile puskesmas, while midwives employed at village health post or village-level birth facility provide care both at village health post and integrated service posts (Mahendradhata et al., 2017).
Our study was conducted in two regions, Surabaya and Mataram, in order to understand the difference in maternity care provision during the COVID-19 pandemic in a higher and relatively lower burden settings. Surabaya is the capital city of East Java province, which at the time of study planning in August 2020, had the highest number of cases in the province, and East Java had the second-highest number of confirmed COVID-19 cases in Indonesia (The Government of East Java, 2020; The Government of Indonesia, 2020). Mataram is the capital of West Nusa Tenggara province. In August 2020, this province ranked 12th of 34 provinces in the number of confirmed COVID-19 in the country, with Mataram having the highest number of cases (The Government of Indonesia, 2020; The Government of West Nusa Tenggara, 2020).
Recruitment and sampling
We used a stratified purposive sampling to select registered midwives, who were 18 years or older, worked as a midwife for at least three years, provided maternity care during the pandemic and worked in different maternity care settings (primary health centres and village health post). As a basis of the stratification, we used the ratio of the primary health centres and village health post availability in the two regions, which approximately two to one (District Health Office of Mataram, 2012; Provincial Health Office of East Java, 2018).
Participants were recruited through an advertisement posted in WhatsApp groups of primary health centres in Surabaya and Mataram, with help from the first author's personal and professional contacts, and public Facebook groups of the Indonesian Midwives Association. The personal and professional contacts only helped to distribute the advertisement and did not influence the potential study participants' decisions to participate. A snowballing method was also used to recruit midwives in different levels of maternity care facilities (Sadler et al., 2010).
Each potential participant received Plain Language Statement and consent form through WhatsApp chat after receiving explanation about the study' objectives, confidentiality, potential risks and data collection process through a short phone call. They were contacted 48-hours after reviewing the Plain Language Statement and consent form to confirm participation. If they agreed to participate, we sent a link to sign the consent form digitally through Zoho (www.zoho.com), and an instructional guide to sign the consent form was sent through WhatsApp. No authors had a prior relationship with any of the participants before the study commenced.
Study instruments
The semi-structured interview guide consisted of three broad sections: 1) how midwives provided antenatal, childbirth and postpartum care before the COVID-19 pandemic, 2) how midwives provided antenatal, childbirth, and postpartum care during the COVID-19 pandemic, and 3) midwives' experiences in providing maternity care during the pandemic. Two midwives working in different regions of study sites were interviewed to pilot the guide, and no changes were made to the interview guide after piloting.
Data collection and management
The first author conducted all interviews in Bahasa Indonesia through WhatsApp calls between December 2020 and February 2021. Interviews were carried out at a convenient time for participants and they confirmed no one else was present at the beginning of the interviews. The interviews lasted for 45-60 minutes. After interview completion, participants received 50,000 rupiahs (approximately £2.6) mobile credits to compensate for mobile data used for the interview.
All interviews were audio-recorded and transcribed verbatim in Bahasa Indonesia by the first author. The second author reviewed a subset of transcriptions for accuracy and completeness. Quotations used in this paper were translated to English at the time of writing. If participants provided ambiguous responses, they were contacted through WhatsApp chat to confirm their responses. Data collection stopped when data saturation was reached, determined by no new themes identified from the preliminary analysis (Guest et al., 2020).
Data analysis
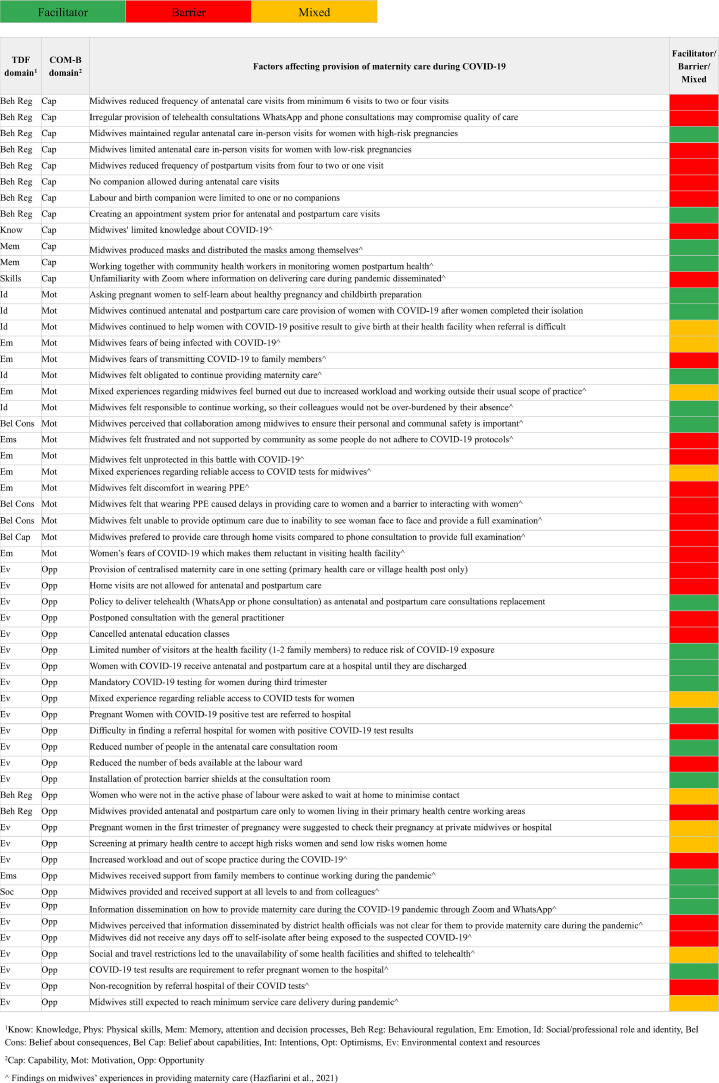
We used an inductive thematic analysis by Braun and Clarke (2006), to analyse the interview transcripts. The first and second authors conducted a line-by-line coding independently of a sample of interview transcripts. The codes were collated into potential themes and sub-themes and discussed with the research team. Next, the first and second authors mapped the final themes and sub-themes to the Theoretical Domains Framework (TDF) and Capability, Opportunity, and Motivation (COM-B) models of behaviour change. TDF and COM-B are interrelated frameworks, where TDF provides a more granular understanding of the capability and motivation in the simplified COM-B model (Atkins et al., 2017). We mapped to TDF and COM-B to understand barriers and facilitators of high-quality provision of maternity care during the COVID-19 pandemic, and how the interplay across these domains affects the care provision (Michie et al., 2011). Since findings from this study were mostly facilitators and barriers to Opportunity domain, findings from a related study on midwives’ experiences in providing maternity care (Hazfiarini et al., 2021) were also mapped to COM-B model to have a comprehensive understanding of factors influencing the high-quality of maternity care provision during the pandemic. We used NVivo 12 (Edhlund and McDougall, 2019) to manage and review coded data and themes. Pseudonyms are used for midwives to protect participants’ confidentiality.
Results
Eighteen midwives were approached to participate; 15 agreed to participate; three declined due to timing constraints. All participants were female and there were seven village and eight primary health care-based midwives (Table 1 ). Participants’ ages ranged from the late 20s to late 40s, and most had 10-20 years of work experience as midwives. Most midwives had a diploma of midwifery, and one had a Bachelor's of midwifery.
Table 1.
Characteristics of participants
| Pseudonyms* | Region | Type of facility† | Age (years) | Midwifery experience (years) |
|---|---|---|---|---|
| Indah | Surabaya | PHC | 31-40 | 10-20 |
| Rani | Mataram | VHP | 31-40 | 10-20 |
| Dina | Surabaya | VHP | 31-40 | 10-20 |
| Anisa | Surabaya | VHP | ≥ 41 | 10-20 |
| Wulan | Surabaya | PHC | 20-30 | <10 |
| Rizka | Mataram | PHC | 31-40 | 10-20 |
| Kartika | Surabaya | VHP | ≥ 41 | 20-30 |
| Siti | Surabaya | PHC | ≥ 41 | 10-20 |
| Ayu | Mataram | PHC | ≥ 41 | 20-30 |
| Intan | Mataram | PHC | 31-40 | 10-20 |
| Tuti | Mataram | PHC | ≥ 41 | 20-30 |
| Nurul | Surabaya | PHC | 31-40 | 10-20 |
| Putri | Mataram | VHP | ≥ 41 | 20-30 |
| Dinda | Surabaya | VHP | 31-40 | 10-20 |
| Citra | Mataram | VHP | 31-40 | 10-20 |
VHP = Village Health Post.
PHC = Primary Health Centre.
All participants were female midwives.
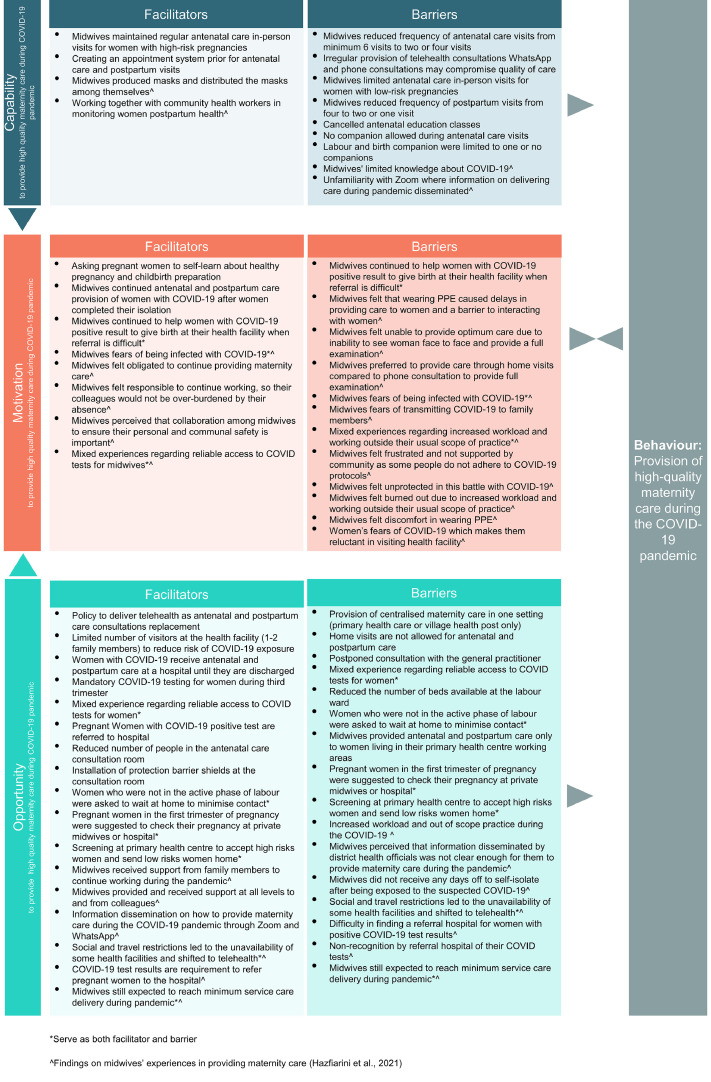
Findings are presented based on the COM-B domains: 1) Capability, 2) Motivation, and 3) Opportunity Fig. 1. depicts changes in the provision of maternity care during the COVID-19 pandemic in Surabaya and Mataram, which highlights the facilitators and barriers of each COM-B domain. The link between the TDF and COM-B domains and research findings is illustrated in Fig. 2 .
Fig. 1.
Mapping the changes in the provision of maternity care during the COVID-19 pandemic to the COM-B model of behaviour change.
Fig. 2.
Links between TDF and COM-B identified factors affecting provision of maternity care during the COVID-19 pandemic.
Capability
In our study, Capability refers to a midwife's psychological and physical capacity to provide maternity care, including their knowledge, skills, behavioural regulation, and memory, attention and decision-making (Michie et al., 2011). In our study, midwives built on their own capacity to provide care during the COVID-19 period including reduced frequency of antenatal and postpartum care visits, continuation of regular antenatal care visits for women with high-risk pregnancies, introduction of telehealth consultations, reduced number of companions during care provision and use of an appointment system. Almost all of these changes provided barriers to enabling women to access maternity care, limited their access to adequate quality maternity care and impacted their positive experiences of care. The appointment system prior to in-person visits was one positive change, as this assisted the provision of safe maternity care by preventing overcrowding and long waiting time at the facilities.
Reduced frequency of antenatal and postpartum care visits
All participants discussed a reduction in the frequency of antenatal care visits during the COVID-19 pandemic, with variation in the revised number of recommended visits. Six midwives reported reducing antenatal care visits from a minimum of six visits, to between two and four visits in total. For example:
“We used to conduct monthly check-up for pregnant women in the first and second trimester of pregnancy and fortnightly check-up during the third trimester. Now, women only have four antenatal care visits throughout the pregnancy. One visit in their first and second trimester, and two visits in the third trimester.” (Dinda, Surabaya, village midwife)
Similarly, some midwives reported reducing the frequency of postpartum care visits from a minimum of four visits to between one and two visits, saying:
“During the pandemic, in-person postpartum visits were reduced to a maximum two times throughout postpartum period, but we continuously monitor women's health by phone.” (Rizka, Mataram, primary health centre midwife)
Other midwives did not suggest a fixed number of antenatal care visits, but they requested that women only visit maternity health facilities if they experienced issues with their pregnancy as explained here:
“During the [COVID-19] pandemic, we suggest women check their pregnancy at primary health centre only if they experience pregnancy issues.” (Tuti, Mataram, primary health centre midwife)
Despite reduced in-person visits, midwives in both regions maintained regular antenatal care visits for women with high-risk pregnancies during the pandemic. One midwife explained:
“For women with a high-risk pregnancy, we continue to suggest them to check their pregnancy at [the] primary health centre routinely. We do not reduce antenatal care visits for high-risk pregnant women.” (Putri, Mataram, village midwife)
Telehealth consultations
WhatsApp or phone consultations replaced some of the previously in-person visits although this was more common in the postpartum period. Only two midwives reported providing phone or WhatsApp consultation for antenatal care. One said:
“Many pregnant women have my phone number so that they can consult with me about their pregnancy by phone or WhatsApp. For example, if they feel something wrong, they can contact me.” (Dinda, Surabaya, village midwife)
Reduced number of companions
Some midwives in Mataram prohibited women having a companion present during antenatal care visits to maintain physical distancing in a consultation room, as evidenced here:
“[the] husband used to be able to be present during antenatal care consultation. Now, women should attend antenatal care consultation alone.” (Intan, Mataram, primary health centre midwife).
Labour and birth companions were limited to one or no companions. This was different to before the pandemic, where some midwives in Surabaya and Mataram had allowed women's husbands and mothers to be present in the labour room. This shift was explained here:
“Only one person allowed to accompany pregnant women in the labour room. They must wear a mask and face shield. However, during delivery, we ask them to wait outside the delivery room to prevent [having an] overcrowded room.” (Wulan, Surabaya, primary health centre midwife)
Availability of an appointment system
Some midwives in Mataram implemented an appointment system that women used before they visited the health facility. This was so they could prepare themselves, for example:
“For pregnant women who want to visit village health post, I ask them to make an appointment first by phone so that I can prepare myself, wearing personal protective equipment (PPE) and cleaning and disinfecting the consultation room.” (Rani, Mataram, village midwife)
Opportunity
In our study, Opportunity refers to the physical and social factors outside of an individual that influence their ability to provide maternity care (Michie et al., 2011). In our study, opportunity comprises of policies implemented in maternity care facilities. Changes in the location of maternity care and postponed or cancelled services were barriers to physical opportunity since they limited the availability of care. Some strategies to reduce COVID-19 transmission were barriers to access, but others supported safe maternity care. The availability of COVID-19 screening also facilitated women to continue receiving quality care. However, the inconsistent type and availability of COVID-19 tests across regions did not always mean midwives could screen pregnant women for COVID-19.
Changes in location of provision of care
Antenatal and postpartum care, which were previously available at all community maternity care facilities, were only available in specific settings during the COVID-19 pandemic. In Surabaya, midwives reported that maternity care was centralised to the primary health centre at the time of data collection due to closures of the village and integrated health post, for example:
“Village midwives have been relocated to primary health centre since March 2020. Since April 2020, the integrated health post has been closed. So, maternity care [during the COVID-19 pandemic] is fully provided at primary health centre.” (Kartika, Surabaya, village midwife)
Most midwives in Mataram said that maternity care was provided mainly at the village health post, as explained here:
“[During the COVID-19 pandemic] the integrated health posts are closed, and we limit the number of visitors at the primary health centre. Pregnant women only visit the primary health centre for their first antenatal care visit, and after that, they should check their pregnancy at the village health post. We are worried that pregnant women will get exposed to COVID-19 if they visit the primary health centre regularly since many people with suspected COVID-19 come to the primary health centre to get tested.” (Tuti, Mataram, primary health centre midwife)
Home visits, which were previously conducted to provide basic antenatal or postpartum care, such as blood pressure measurement, abdominal examination and assessment of postpartum women experiencing health issues who were unable to travel to the health facility, were also not conducted. One midwife said:
“Before the COVID-19 pandemic, we conducted home visit for women with high-risk pregnancy or women with postpartum complications. Now, we are not able to do it. Home visits have been cancelled.” (Nurul, Surabaya, primary health centre midwife).
Postponed or cancelled maternity care
In the local policies, pregnant women are required to consult with general practitioners in the first and third trimester of pregnancy to screen pregnancy and childbirth risks. However, due to the changes in the frequency of antenatal care visits, midwives reported that some women postponed their consultation with the general practitioner. One midwife said:
“Pregnant women are suggested to have their first antenatal care visit after 28 weeks of pregnancy. They will have blood check, consultation with a general practitioner, nutritionist and psychologist on their first visit.” (Wulan, Surabaya, primary health centre midwife)
Apart from a one-on-one consultation with health workers, pregnant women typically attend antenatal education class to improve their knowledge and skills on healthy pregnancy and childbirth preparation and share their experiences with other women. In our study, midwives reported cancelling the education classes due to social restrictions prohibiting gatherings of large numbers of people as articulated here:
“We used to have monthly antenatal education classes. One class consisted of three sessions and a minimum of five women. Each session focused on different topics, such as healthy pregnancy, and childbirth preparation. However, since the pandemic started, all health programs, including antenatal education classes, which require us [health workers] to gather people have been cancelled.” (Anisa, Surabaya, village midwife)
Strategies to reduce COVID-19 transmission at maternity care facilities
Midwives in the two regions has a range of measure to protect women and themselves from COVID-19. One of the most reported measures was to limit physical contact between women and midwives during antenatal care by installing protection barrier shields in the consultation room, for example:
“At each [consultation] table, now we have protection shields so we do not have direct contact with women [during antenatal care].” (Putri, Mataram, village midwife)
Some primary health centre midwives in both regions also reduced the capacity of the consultation room to maintain physical distancing, as explained here:
“Before the pandemic, there were three midwives at consultation room providing care to three women. One midwife provided care to one woman. During the pandemic, we only allow one midwife and one woman in the room.” (Intan, Mataram, primary health centre midwife)
Some midwives in Surabaya reduced the number of beds available at the labour ward to reduce the capacity of the ward, as evidenced here:
“We used to have three beds, and now we only have two beds to limit the number of patients. We only can help a maximum of two pregnant women for delivery. If we have more than two women, we will refer them to the closest primary health centre.” (Nurul, Surabaya, primary health centre midwife)
The number of visitors was limited to one or two family members to reduce risk of COVID-19 exposure, as this midwife said:
“We only allow one family member, husband or other family members [at health facility]. Before the pandemic, a lot of family members visited primary health centre to show sympathy and support.” (Citra, Mataram, village health post)
Some midwives in Surabaya and Mataram provided antenatal and postpartum care only to women living in their primary health centre working areas to prevent overcrowding health facilities. They said:
“Before the pandemic, many pregnant women living outside our primary health centre working area checked their pregnancy with us. Now, we only provide antenatal care for women living in our working area. If they live outside our working area, we will ask them to check their pregnancy at the closest primary health centre to their houses.” (Siti, Surabaya, primary health centre midwife)
Suggesting that pregnant women in the first trimester of pregnancy receive care with private midwives or hospitals was mentioned by some midwives in Surabaya as a strategy in preventing overcrowding in the public facilities. For example:
“We suggest first trimester pregnant women to check their pregnancy at other health facilities, such as private midwives or Women and Children Hospital, to minimise their contact with other people coming to the primary health centre for massive COVID-19 testing.” (Kartika, Surabaya, village midwife)
In addition, screening was conducted at primary health centre in Surabaya to ensure that only women with health issues received care at the health facility.
“We do screening at the entrance of primary health centre. We asked women their gestational age, whether they have medical issues. Healthy pregnant women sent back home since only women with medical issues who are allowed to do a consultation at the primary health centre” (Wulan, Surabaya, primary health centre midwife).
In Surabaya, women who were not in the active phase of labour were asked to wait at home to minimise contact with health workers and other patients at the health facility.
“If women are in the latent phase of labour, we ask them to go home and back to the primary health centre when they are in the active phase of labour.” (Nurul, Surabaya, primary health centre midwife)
COVID-19 screening for pregnant women
As part of childbirth preparation, pregnant women in the third trimester must get tested for COVID-19. The test result was used to decide childbirth location and refer women to the hospital if they need further medical support. In Surabaya, pregnant women were tested using a Polymerase Chain Reaction (PCR) test at the primary health centre. In Mataram, pregnant women could get the COVID-19 test using the COVID-19 rapid antigen test either at the primary health centre or village health post as PCR test was only available at hospitals. Midwives in Surabaya and Mataram shared that despite being infected with COVID-19, pregnant women continued to receive antenatal care at a hospital. One midwife explained:
“Pregnant women who tested positive with COVID-19 should be referred to hospitals which have been assigned to care for pregnant women with COVID-19. Pregnant women with serious symptoms are usually isolated at the hospital. If women are isolated at a hospital, antenatal check-ups will be done by health workers at the hospital. We will continue to provide antenatal care to women after they complete their isolation.” (Dina, Surabaya, village midwife)
Motivation
In our study, motivation refers to the processes that energise and direct behaviour related to providing care, including emotional regulation, professional roles and identities, and belief about consequences (Michie et al., 2011). In our study, motivation included midwives' willingness to keep women informed about healthy pregnancy and childbirth preparation and willingness to continue providing maternity care after women's isolation. This willingness was crucial to ensure women continued receiving quality maternity care during the pandemic. However, without adequate PPE, providing maternity care to women suspected COVID-19 put midwives and women at higher risk of COVID-19.
Asking pregnant women to self-learn about healthy pregnancy and childbirth preparation
Due to cancelled antenatal education classes, several midwives asked pregnant women to self-learn about healthy pregnancy and childbirth preparation and providing WhatsApp consultation.
“Although antenatal education sessions are cancelled, we asked pregnant women to learn the materials from the women and child health book. They also can look for that information online.” (Ayu, Mataram, primary health centre midwife,)
Providing maternity care for women with suspected COVID-19
Some midwives in Mataram discussed that they continued to provide maternity care for women with suspected COVID-19. Several midwives in Mataram continued to provide antenatal care at the health facility for pregnant women with COVID-19, as evidenced here:
“If pregnant women have a positive result of rapid test, we suggest them to stay at home… They can still visit the primary health centre for antenatal care, but we always wear PPE when helping them.” (Rizka, Mataram, primary health centre midwife)
Similarly, most midwives in Mataram said that if the rapid antigen test was positive, they continued to help women give birth at their health facility without conducting a PCR test to assess the actual condition of pregnant women more accurately. PCR tests were only available at hospitals. One midwife said:
“If the rapid test result is positive and pregnant women are healthy, they are not high-risk pregnant women; we help them to deliver their babies at primary health centre” (Rizka, Mataram, primary health centre midwife)
The decision to continue helping women give birth at their health facility was often due to the difficulty in finding a referral hospital. Most midwives in Mataram felt helpless providing care to women with suspected COVID-19. One midwife explained:
“We used to refer pregnant women with a positive result of a rapid test to hospital for childbirth. We were worried (of being infected with COVID-19) if we helped them deliver their babies. Since it is difficult to refer women to the hospital, we do not have any choice. We help them at the primary health centre. If not us, who will help them?” (Intan, Mataram, primary health centre midwife)
For pregnant women self-isolating at home, most midwives in Mataram continued the provision of antenatal care only after women completed their isolation. Similarly, midwives in Surabaya and Mataram continued to deliver postpartum care for women who tested positive to COVID-19 after they were cleared to end isolation.
“If the [PCR] test comes out with positive result, pregnant women will be referred to hospital for childbirth…. Women will receive first postpartum care at the hospital and continue receive [postpartum] care there when they are still diagnosed with positive to COVID-19. We will continue providing the postpartum care after women are discharged from the hospital.” (Siti, Surabaya, primary health centre midwife)
Discussion
Indonesia faced considerable challenges through several waves of COVID-19 in 2021. Our findings show that maternity care provision in two regions in Indonesia underwent substantial changes during the COVID-19 pandemic. These changes mostly related to behavioural regulation, professional roles and identities, and environmental context and resources and they act as facilitators and barriers in providing high-quality maternity care during the COVID-19 pandemic. Changes in maternity care provision from midwives’ perspectives can serve as facilitators and barriers for women to receive adequate care during the pandemic. Reduced number of in-person visits with irregular telehealth consultations, limited antenatal care for women with low-risk pregnancies and reduced number of companions contribute to the main barriers of high-quality maternity care during the pandemic. However, creating an appointment system was a useful innovation that could facilitate safe maternity care. Similarly, policies implemented at maternity care facilities and midwives’ motivation could serve as facilitators and barriers in providing high-quality maternity care during the pandemic. Changes in the location of maternity care and postponed or cancelled maternity care contribute to the main barriers of high-quality maternity care during the pandemic. However, women can continue to receive safe and adequate maternity care due to some strategies to reduce the COVID-19 transmission, availability of maternity care for women suspected or confirmed with COVID-19 and availability of COVID-19 screening.
Our study identified most barriers to the provision of maternity care during the COVID-19 pandemic related to Capability domain, consisting of changes in the provision of care based on midwives’ initiatives. Many of the changes in our study context contradict the WHO and UNFPA (2020) and the Indonesian Association for Obstetrics and Gynaecology (2020) guidelines. For example, midwives reduced the number of antenatal and postpartum care visits, but the recommended number of visits is fewer than what is recommended by WHO and UNFPA (2020), which are eight antenatal care and four postpartum visits with some visits may be conducted remotely, and the Indonesian Association for Obstetrics and Gynaecology (2020) guidelines, which are at minimum six visits for antenatal and four visits for postpartum care. As a result of the pandemic, the Indonesian Association for Obstetrics and Gynaecology (2020) recommended telehealth consultation to replace reduced visits, but this was not always available. In addition, the number of companions was limited or non-existent, despite guidelines recommend maintaining companionship during COVID-19 pandemic to encourage positive experiences of care (WHO and UNFPA, 2020). These modifications may then ultimately result in negative experience of care for women (Mortazavi and Ghardashi, 2021; Whipps et al., 2021) and potentially negative pregnancy outcomes. Despite this, midwives in Mataram and Surabaya adapted their practice to support high-quality maternity care during the pandemic. Implementation of appointment systems prior to in-person visits could minimise COVID-19 transmission at health facilities, and reduced wait times and overcrowding which were previously major challenges (Jones et al., 2021; Steenland et al., 2019).
Two of the three factors in the Motivation domain are facilitators of providing high-quality maternity care. Maternity care providers’ motivation has been known to have significant role in the continuity of maternity care provision during emergencies (Erland and Dahl, 2017; Hazfiarini et al., 2021). However, motivation of midwives in the study to continue providing maternity care might put them and women at risk of COVID-19. Midwives reported continuing to provide care to women suspected of COVID-19 at their health facilities, where women should have been referred to hospitals for further medical support. Adequate protection for women and maternity care providers should be available at community maternity care facilities to reduce their risk of getting COVID-19 during care provision.
Finally, the opportunity to provide safe maternity care which can protect both women and maternity care providers is critical (WHO and UNFPA, 2020). In line with clinical recommendation from International Federation of Gynecology and Obstetrics (FIGO) to conduct COVID-19 screening for women (Poon et al., 2020), COVID-19 screening was conducted to women in the third trimester of pregnancy. This ensures that women with COVID-19 can receive appropriate and adequate care based on their needs, while the safe provision of care at the primary health centre or village health post can be delivered to healthy women. Another key facilitator of the provision of high-quality maternity care during the pandemic is a continuation of maternity care to women suspected or confirmed with COVID-19. A qualitative study in Ethiopia has discovered stigma towards women suspected or confirmed COVID-19 and experiencing the stigma refrained women from accessing maternity care (Hailemariam et al., 2021). Stigma is one type of mistreatment that can impact women's positive experiences of care care (Bohren et al., 2015; Tunçalp et al., 2015). Although we did not explore stigma in this study, availability of policies to provide maternity care to women suspected or confirmed with COVID-19 could support women to continue accessing high quality of maternity care despite their COVID-19 situation.
We explored midwives’ experiences of providing maternity care during the pandemic, and more research is needed to consider how women and their families experience maternity care, as well as policymakers, make decisions about changes to healthcare during emergencies. For example, in Australia, similar changes were made to maternity care provision during the pandemic, and a qualitative study reported on women's experiences of navigating changing health systems, desiring more choice and control over their pregnancy and care, and experiences of infection prevention measures (Sweet et al., 2021b). Moreover, we found that the main barriers to the high-quality provision of maternity care are related to changes that were not from evidence-based guidance, representing a critical guideline implementation gap. Therefore, effective training on how to provide safe and high-quality maternity care during the pandemic is needed, along with more monitoring and evaluation to ensure improved guideline implementation. Moreover, maternity care should still aim to encourage women's positive care experiences, for example, by providing telehealth consultations to replace the reduced visits and allowing women to be accompanied by their partners or family members throughout maternity care.
Strengths and limitations
Our study uses rigorous qualitative methods and behaviour change frameworks to contribute to better understanding of maternity care provision during the COVID-19 pandemic in Indonesia and identify areas for improvement. The first and second authors are Indonesian women who have experience working in maternity care provision in Indonesia.
We conducted online interviews but at times there were difficulties with the connectivity and internet connection, hence interviews had to be stopped and restarted which disrupted the flow of the conversation. We used a stratified purposive sampling approach to aim for diversity in participants, but these participants’ experiences may not represent all Indonesian midwives. Data collection took place prior to the devastating June to September 2021 COVID-19 wave, which may have had further implications on the way maternity care was provided. However, data saturation was reached, indicating our findings were rich and in-depth.
Conclusions
The COVID-19 pandemic has resulted in various changes in the provision of maternity care in Surabaya and Mataram, Indonesia. Using the TDF and COM-B model allowed us to understand how the changes influenced high-quality maternity care provision during the pandemic and is a starting point to improve maternity care provision by clarifying barriers and facilitators. The critical barriers in maternity care provision during the pandemic are the changes in the provision of maternity care that are not based on developed guidelines. To improve the provision of care, barriers across three COM-B domains should be eliminated, and facilitators should be enhanced.
CRediT authorship contribution statement
Alya Hazfiarini: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Writing – review & editing, Visualization, Project administration. Rana Islamiah Zahroh: Formal analysis, Writing – original draft, Writing – review & editing, Visualization. Shahinoor Akter: Conceptualization, Methodology, Writing – review & editing, Supervision. Caroline S.E. Homer: Conceptualization, Methodology, Writing – review & editing, Supervision. Meghan A. Bohren: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Ethical approval
The Medicine & Dentistry Human Ethics Sub-Committee of the University of Melbourne (ethics ID number: 2057852.1) and the Health Research Ethics Committee of the Faculty of Public Health of Airlangga University, Indonesia (ethics ID number: 102/EA/KEPK/2020) granted ethical approval for this study.
Funding sources
This research did not receive any financial support. AH is sponsored by Australian Awards Scholarship (OASIS ID: ST000WAU5) for her master's degree, funded by Australian Department of Foreign Affairs and Trade (DFAT). RIZ is supported by Melbourne Research Scholarship and Human Rights Scholarship from The University of Melbourne. CSEH is supported by a National Health and Medical Research Council (NHMRC) Principal Research Fellowship. MAB is supported by an Australian Research Council Discovery Early Career Researcher Award (DE200100264) and a Dame Kate Campbell Fellowship (University of Melbourne Faculty of Medicine, Dentistry, and Health Sciences).
Acknowledgments
We would like to thank midwives for their participation in the study and colleagues working at primary health centres in Surabaya and Mataram who helped distribute the recruitment advertisement.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.midw.2022.103291.
Appendix. Supplementary materials
References
- Asefa A., Semaan A., Delvaux T., Huysmans E., Galle A., Sacks E., Bohren M.A., Morgan A., Sadler M., Vedam S., Benova L. The impact of COVID-19 on the provision of respectful maternity care: Findings from a global survey of health workers. Women Birth. 2021;0 doi: 10.1016/j.wombi.2021.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins L., Francis J., Islam R., O'Connor D., Patey A., Ivers N., Foy R., Duncan E.M., Colquhoun H., Grimshaw J.M., Lawton R., Michie S. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017;12:77. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren M.A., Vogel J.P., Hunter E.C., Lutsiv O., Makh S.K., Souza J.P., Aguiar C., Coneglian F.S., Diniz A.L.A., Tunçalp Ö., Javadi D., Oladapo O.T., Khosla R., Hindin M.J., Gülmezoglu A.M. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic review. PLOS Med. 2015;12 doi: 10.1371/journal.pmed.1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006:77. [Google Scholar]
- Broom A., Willis E. In: Researching Health : Qualitative, Quantitative and Mixed Methods. Saks M., Allsop J., editors. SAGE; 2007. Competing paradigms and health research; pp. 16–31. [Google Scholar]
- Coxon K., Turienzo C.F., Kweekel L., Goodarzi B., Brigante L., Simon A., Lanau M.M. The impact of the coronavirus (COVID-19) pandemic on maternity care in Europe. Midwifery. 2020;88 doi: 10.1016/j.midw.2020.102779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- District Health Office of Mataram, 2012. Health Profile of Mataram 2012.
- Edhlund B., McDougall A. Version 12 for Windows. QSR International Pty Ltd.; Melbourne, Australia: 2019. NVivo 12 essentials. [Google Scholar]
- Erland E., Dahl B. Midwives’ experiences of caring for pregnant women admitted to Ebola centres in Sierra Leone. Midwifery. 2017;55:23–28. doi: 10.1016/j.midw.2017.08.005. [DOI] [PubMed] [Google Scholar]
- Guest G., Namey E., Chen M. A simple method to assess and report thematic saturation in qualitative research. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0232076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailemariam S., Agegnehu W., Derese M. Exploring COVID-19 related factors influencing antenatal care services uptake: A qualitative study among women in a rural community in Southwest Ethiopia. J. Prim. Care Commun. Health. 2021;12 doi: 10.1177/2150132721996892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazfiarini A., Akter S., Homer C.S.E., Zahroh R.I., Bohren M.A. We are going into battle without appropriate armour’: A qualitative study of Indonesian midwives’ experiences in providing maternity care during the COVID-19 pandemic. Women Birth. 2021 doi: 10.1016/j.wombi.2021.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helmyati S., Dipo D.P., Adiwibowo I.R., Wigati M., Safika E.L., Hariawan M.H., Destiwi M., Prajanta Y., Penggalih M.H., Sudargo T., Herawati D.M., Marthias T., Masrul M., Trisnantoro L. Monitoring continuity of maternal and child health services, Indonesia. Bull. World Health Organ. 2022;100:144A–154A. doi: 10.2471/BLT.21.286636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indonesian Association for Obstetrics and Gynaecology, 2020. Recommendations for handling corona virus infection (COVID-19) in maternal (pregnancy, childbirth and postpartum).
- Indonesia's COVID-19 task force, 2021. COVID-19 map [WWW Document]. covid19.go.id. URL https://covid19.go.id/peta-sebaran (accessed 12.16.21).
- Johariyah Zubaedah, Widyawati D.S.N., EndahPurnamaningsih S., Margaretha M. How maternal and neonatal services at the community level during the COVID-19 pandemic in Indonesia? Syst. Rev. Pharm. 2020;11:237–242. doi: 10.31838/srp.2020.11.34. [DOI] [Google Scholar]
- Jones L., Damayanti N.A., Wiseman N., Harris N. Factors shaping uptake of antenatal care in surabaya municipality, indonesia: a qualitative study. Kesmas J. Kesehat. Masy. Nas. Natl. Public Health J. 2021;16 doi: 10.21109/kesmas.v16i3.4849. [DOI] [Google Scholar]
- Mahendradhata, Y., Trisnantoro, L., Listyadewi, S., Soewondo, P., Marthias, T., Harimurti, P., Prawira, J., 2017. The republic of indonesia health system review.
- Michie S., van Stralen M.M., West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortazavi F., Ghardashi F. The lived experiences of pregnant women during COVID-19 pandemic: a descriptive phenomenological study. BMC Pregnancy Childbirth. 2021;21:193. doi: 10.1186/s12884-021-03691-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panda S., O'Malley D., Barry P., Vallejo N., Smith V. Women's views and experiences of maternity care during COVID-19 in Ireland: a qualitative descriptive study. Midwifery. 2021;103 doi: 10.1016/j.midw.2021.103092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon L.C., Yang H., Kapur A., Melamed N., Dao B., Divakar H., Mclntyre H.D., Kihara A.B., Ayres-deCampos D., Ferrazzi E.M., Di Renzo G.C., Hod M. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: Information for healthcare professionals. Int. J. Gynecol. Obstet. 2020 doi: 10.1002/ijgo.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provincial Health Office of East Java Province, 2018. Health profile of east java province 2018.
- Sadler G.R., Lee H.-C., Seung-Hwan Lim R., Fullerton J. Recruiting hard-to-reach United States population sub-groups via adaptations of snowball sampling strategy. Nurs. Health Sci. 2010;12:369–374. doi: 10.1111/j.1442-2018.2010.00541.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenland M., Dula J., de Albuquerque A., Fernandes Q., Cuco R.M., Chicumbe S., Gudo E.S., Sequeira S., McConnell M. Effects of appointment scheduling on waiting time and utilisation of antenatal care in Mozambique. BMJ Glob. 2019;4 doi: 10.1136/bmjgh-2019-001788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet L., Bradfield Z., Vasilevski V., Wynter K., Hauck Y., Kuliukas L., Homer C.S.E., Szabo R.A., Wilson A.N. Becoming a mother in the ‘new’ social world in Australia during the first wave of the COVID-19 pandemic. Midwifery. 2021;98 doi: 10.1016/j.midw.2021.102996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet L., Wilson A.N., Bradfield Z., Hauck Y., Kuliukas L., Homer C.S.E., Szabo R.A., Wynter K., Vasilevski V. Childbearing women's experiences of the maternity care system in Australia during the first wave of the COVID-19 pandemic. Women Birth. 2021 doi: 10.1016/j.wombi.2021.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Government of East Java Province, 2020. COVID-19 Data in East Java Province and Surabaya [WWW Document]. Jatim Tanggap COVID-19. URL http://infocovid19.jatimprov.go.id (accessed 8.15.20).
- The Government of Indonesia, 2020. COVID-19 Data in Indonesia [WWW Document]. COVID-19 Indones. URL https://covid19.go.id/peta-sebaran (accessed 8.15.20).
- The Government of West Nusa Tenggara Province, 2020. COVID-19 Data in West Nusa Tenggara Province and Mataram [WWW Document]. COVID-19 Data West Nusa Tenggara Prov. URL https://corona.ntbprov.go.id/list-data (accessed 8.15.20).
- Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19:349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Tunçalp Ӧ., Were W., MacLennan C., Oladapo O., Gülmezoglu A., Bahl R., Daelmans B., Mathai M., Say L., Kristensen F., Temmerman M., Bustreo F. Quality of care for pregnant women and newborns—the WHO vision. BJOG Int. J. Obstet. Gynaecol. 2015;122:1045–1049. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whipps M.D.M., Phipps J.E., Simmons L.A. Perinatal health care access, childbirth concerns, and birthing decision-making among pregnant people in California during COVID-19. BMC Pregnancy Childbirth. 2021;21:477. doi: 10.1186/s12884-021-03942-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiasih R., Hidayat D., Zakaria H., Utama D.Q., Komariah M., Maryam N.N.A., Arifin H., Agustina H.S., Nelson K. Self-fetal wellbeing monitoring and ante-natal care during the COVID-19 pandemic: a qualitative descriptive study among pregnant women in indonesia. Int. J. Environ. Res. Public. Health. 2021;18:11672. doi: 10.3390/ijerph182111672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organ; 2021. WHO Coronavirus Disease (COVID-19) Dashboard [WWW Document]https://covid19.who.int/table accessed 9.28.21. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2016. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. [PubMed] [Google Scholar]
- World Health Organization . COVID-19 Technical Brief for Maternity Services. 2020. United Nations Population Fund. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.