Abstract
Objective
To evaluate the relationship between antibiotic exposure and subsequent psychiatric disorders in a Pediatric primary care setting.
Study design
We conducted a retrospective cohort study using electronic clinical record data for patients ages 8–20 years seen in the outpatient setting of a large urban primary health care practice from 1/1/13 to 12/1/2018. We employed adjusted Cox regression analyses to study the relationship between prescriptions for anti-infective agents and subsequent diagnosis of anxiety or depression.
Results
Prescription of anti-infective medication was associated with a hazard rate ratio (HRR) of 1.21 (95%-CI = 1.00–1.45). A first prescription for a broad-spectrum antibiotic (compared to those with no prescription, narrow-spectrum prescription, or topical prescription) was associated with an HRR of 1.27 (95%-CI = 1.04–1.54). The number of anti-infectives prescribed over the course of the study period was associated with an HRR of 1.05 (95%-CI = 1.00–1.10). There was no significant relationship between prescription of topical or narrow-spectrum antibiotics, antifungal, or antiviral medication and subsequent diagnosis of anxiety or depression. Stratified analysis revealed that the association between anti-infective prescription and anxiety and depression was driven by males, among whom prescription of any antibiotic was associated with an HRR of 1.45 (95%-CI = 1.05–1.99).
Conclusions
Infections treated with broad-spectrum antibiotics were associated with increased risks of anxiety and/or depression, especially in males. Exploration of the relationship between antibiotic exposure and subsequent mental health disorders is warranted along with continued vigilance in antibiotic prescribing practices in children.
Keywords: Antibiotic, Anti-infective, Depression, Anxiety, Microbiome, Life span, Gut-brain axis
Abbreviations: Johns Hopkins Community Physicians, JHCP; Electronic Medical Record, EMR
Highlights
-
•
Previous studies have demonstrated a connection between anti-infectives and an increased risk of psychiatric disorders.
-
•
Infections treated with antibiotics were associated with increased risks of anxiety and/or depression in this study.
-
•
Exploration of the relationship between antibiotic exposure and subsequent mental health disorders is warranted.
1. Introduction
Anxiety and depression are common psychiatric disorders diagnosed in children. The CDC reported in the National Survey of Children's Health that 7.1% (4.4 million) of US children aged 3 to 17 have been diagnosed with anxiety and 3.2% (1.9 million) with depression (Ghandour et al., 2019). The rates of ever having either of these disorders are on the rise for children aged 6–17 years, increasing from 5.4% in 2003 to 8.4% in 2011 (Bitsko et al., 2018). Left untreated, anxiety and depression during childhood can lead to life-long serious mental health conditions and an increased risk of suicide (Curtin and Heron, 2019).
It has become increasingly evident that the composition of the microbial organisms on mucosal surfaces, denoted as the microbiome, may be related to brain functioning. This relationship is likely mediated by a number of related pathways characterized as the gut brain axis. The composition of the microbiome within an individual can be determined by a number of factors including both genetic and environmental factors. Exposure to broad-spectrum antibiotics prescribed for the treatment of infectious diseases is one of the most common environmental factors which can affect the microbiome (Mayer et al., 2014). This is particularly the case for infants and young children in light of the frequent occurrence of infections and the prescription of antibiotics.
Recent population and register based studies performed in Northern Europe have shown that exposure to anti-infectives, and particularly to antibiotics, prescribed to treat infections in infancy and childhood are associated with an increased risk of the subsequent development of psychiatric disorders (Köhler-Forsberg et al., 2019; Köhler et al., 2017). Increased risk was associated with the number of antibiotic administrations and with agents having a broader antibiotic spectrum. These studies suggest strategies may be developed to identify individuals at high risk for these disorders as a result of antibiotic exposure. However, testing this effect in clinical care settings in diverse populations will be a critical next step to identify additional risk factors and ensure these results are generalizable to more diverse populations. In this study, we replicate the time to event adjusted regression analyses performed previously using Northern European data, but due to the differences in population demographics (Northern European studies represented largely homogenous white populations, whereas our data also represents a sizeable proportion of African American children) the results from this work are more generalizable to American children.
The aim of this study is to investigate whether infections treated with anti-infectives are associated with subsequent development of anxiety and/or depression in a primary care health system in the United States. In addition, risk differences between types of anti-infective agents as well as risk differences between broad and narrow-spectrum antibiotics are investigated.
2. Materials & methods
This cohort study was conducted using data from the Johns Hopkins Community Physicians group practice (JHCP), a system that includes 40 locations providing ambulatory general and specialty care throughout the Baltimore-Washington area. Patient data was extracted from Epic, the electronic medical records system used by JHCP since 2013. The institutional review boards of Johns Hopkins and JHCP approved this study as minimal risk and waived the requirement for informed consent.
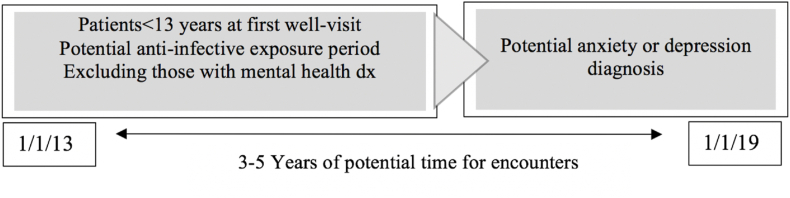
The study cohort included patients of JHCP pediatric and family practices, ages 8–20 years old who had at least 3 “well visits” between January 1, 2013 and January 1, 2019. “Well visits” were defined as encounters with a chief complaint code of "Well child care", "Immunizations", "Annual exam", "School physical", or "Sports physical". Patients were excluded if they were older than 13 years old at the time of the first recorded encounter or if they had a follow up time of less than 3 years. The entry into the population, or study baseline, for each patient is the time of first JHCP encounter during the study period (see Fig. 1).
Fig. 1.
Conceptual Timeline.
The outcome of interest was a new diagnosis of anxiety and/or depression, as indicated by the encounter diagnosis in the medical record. For those with the outcome of interest, patients were excluded if there was a diagnosis of a mental health disorder in the patient's history or problem list prior to the first recorded encounter. Patients with ADHD represented a large portion of this population and thus were retained in the cohort. Additionally, patients with the outcome of interest were excluded if they did not have at least one well visit prior to the encounter with the anxiety/depression diagnosis.
The exposure of interest was the prescription of anti-infective medications, specifically broad-spectrum antibiotics, in the course of a JHCP encounter. For comparison, data was also collected on other types of prescriptions, including antiviral and antifungal medications as well as topical and narrow-spectrum antibiotics. In order to get a sense of the specific infection diagnoses for which the anti-infectives were being prescribed, we categorized encounter diagnosis codes for the included encounters into broad categories, such as “respiratory infection” and “genitourinary infection”. Demographic data, such as race/ethnicity, age, sex, and type of insurance was also extracted from each patient's medical record. Type of insurance was categorized as Medicare/Medicaid, commercial, self-pay, or other.
Cox proportional hazard models were used to examine the risk of anxiety/depression diagnosis as it related to prescription of antibiotics. Exposure was defined in three different ways, the first was “ever” exposure to any kind of antibiotic, antiviral, or antifungal medication during the time period of the study. Second, in order to explore the type of antibiotic prescribed and compare to other types of medications, we focused on the category of antibiotic and infection at first prescription of any antibiotics during the time period of the study. We assessed the relationship between sex and anti-infectives, as well as infection category, using chi-squared statistics as well as adjusted Cox regression modeling. Finally, we used a count of the number of antibiotic prescriptions over the course of the study period in order to assess a dose-response relationship. We tested the Cox proportional hazard assumptions using Kaplan Meier analyses and Schoenfeld residuals.
3. Results
The study population consisted of 5244 individuals, 532 patients who met the criteria for the outcome of interest, and 4712 patients who did not have the outcome of interest. Among those who were diagnosed with anxiety and/or depression, the mean age at first JHCP encounter during the study period was 10.41 (SD = 1.54), whereas among the comparison group (no anxiety/depression diagnosis during the study time period) the mean age at first JHCP encounter during the study period was 9.9 (SD = 1.57, p < .0001, Table 1). Females were more likely than males to have an anxiety or depression diagnosis (15.6% of females, 7.3% of males, p < .0001). Non-Hispanic white patients were also much more likely to have an anxiety or depression diagnosis (12.4% of NH White, 8.0% of NH African American, p < .0001). Among the entire study population, 72.1% of patients had private insurance, and 26.8% were insured by Medicaid, and this did not differ significantly by outcome group. Additionally, 9.1% of these patients had a recoded ADHD diagnosis, 0.2% had a recorded suicide attempt, and 50.0% had a recorded prescription for an antibiotic. The mean number of antibiotic prescriptions during the study period was 1.02 (SD = 1.62).
Table 1.
Patient characteristics.
| Characteristics | Total Study Population | No Anxiety/Depression Dx | Anxiety/Depression Dx | p value |
|---|---|---|---|---|
| N | 5244 | 4712 | 532 | |
| Age at 1st JHCP encounter (during the study period) | ||||
| Mean (SD) | 9.92 (1.6) | 9.86 (1.57) | 10.41 (1.54) | 0.000 |
| Male | 2599 (49.6%) | 2423 (93.2%) | 176 (7.3%) | |
| Female | 2645 (50.4%) | 2289 (86.5%) | 356 (15.6%) | 0.000 |
| Race/Ethnicity | ||||
| Non-Hispanic African American | 2236 (46.3%) | 2057 (92.0%) | 179 (8.0%) | 0.000 |
| Non-Hispanic White | 2025 (41.9%) | 1774 (87.6%) | 251 (12.4%) | |
| Non-Hispanic Asian | 230 (4.8%) | 211 (91.7%) | 19 (8.2%) | |
| Hispanic | 313 (6.5%) | 274 (87.5%) | 39 (12.5%) | |
| Other | 25 (0.5%) | 19 (76.0%) | 6 (24%) | |
| Insurance at JHCP first encounter | ||||
| Medicare/Medicaid | 1388 (26.8%) | 1256 (90.5%) | 132 (9.5%) | 0.717 |
| Commercial | 3735 (72.1%) | 3341 (89.5%) | 394 (10.5%) | |
| Self pay | 25 (0.5%) | 23 (92.0%) | 2 (8.0%) | |
| Other | 32 (0.6%) | 29 (90.6%) | 3 (9.4%) | |
| Ever ADHD Dx | ||||
| No | 4766 (90.9%) | 4335 (93.1%) | 431 (9.0%) | 0.000 |
| Yes | 478 (9.1%) | 377 (78.9%) | 101 (21.1%) | |
| Ever Suicide Attempt | ||||
| No | 5234 (99.8%) | 4708 (90.0%) | 526 (10.0%) | 0.000 |
| Yes | 10 (0.2%) | 4 (40.0%) | 6 (60.0%) | |
| Any Anti-Infective Rx | ||||
| No | 2452 (46.8%) | 2247 (91.6%) | 205 (8.4%) | 0.000 |
| Yes | 2792 (53.2%) | 2465 (88.3%) | 327 (11.7%) | |
| Any Antibiotics | ||||
| No | 2780 (53.0%) | 2540 (91.4%) | 240 (8.6%) | 0.000 |
| Yes | 2464 (47.0%) | 2172 (88.1%) | 292 (11.9%) | |
| 1st Antibiotics Rx | ||||
| NA | 2780 (53.0%) | 2540 (88.1%) | 240 (8.6%) | 0.000 |
| Broad | 1728 (33.0%) | 1508 (87.3%) | 220 (12.7%) | |
| Narrow | 130 (2.5%) | 122 (93.8%) | 8 (6.2%) | |
| Topical | 606 (11.6%) | 542 (89.4%) | 64 (10.6%) | |
| Total # of Antibiotics Rx | ||||
| Mean (SD) | 1.02 (1.6) | 0.99 (1.58) | 1.29 (1.93) | 0.000 |
| Any Anti-Fungal Rx | ||||
| No | 4701 (89.7%) | 4224 (89.9%) | 477 (10.1%) | 0.990 |
| Yes | 543 (10.4%) | 488 (89.9%) | 55 (10.1%) | |
| Any Anti-Viral Rx | ||||
| No | 4939 (94.8%) | 4441 (90.0%) | 498 (10.0%) | 0.550 |
| Yes | 305 (5.8%) | 271 (88.9%) | 34 (11.1%) | |
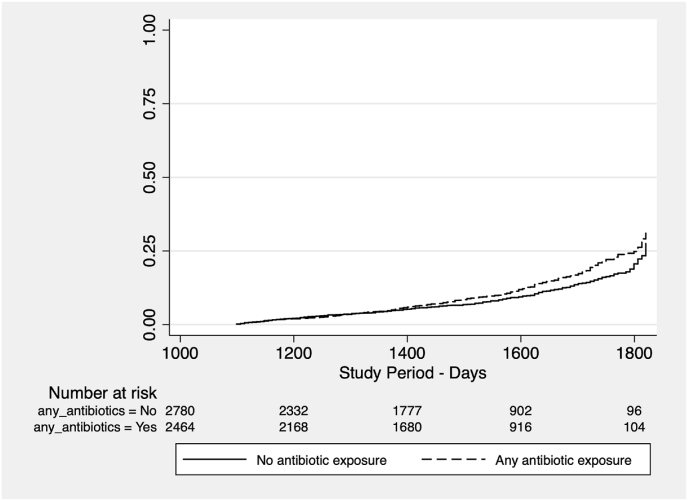
Prescription of any anti-infective during the study period was associated with a slightly increased risk of anxiety and/or depression by an Adjusted Hazard Rate Ratio (HRR) of 1.21 (95% CI = 1.00–1.45) and prescription of any antibiotic was associated with an HRR of 1.19 (95% CI = 1.00–1.43) (See Fig. 2, Table 2). When antibiotics were analyzed by type (no antibiotic, broad-spectrum, narrow-spectrum, and topical) broad-spectrum antibiotics were associated with an HRR of 1.27 (95% CI = 1.04–1.54). The total number of antibiotic prescriptions during the study period was associated with an HRR of 1.05 (95% CI = 1.00–1.10). Antiviral, antifungal, narrow-spectrum antibiotics, and topical antibiotics were not significantly associated with anxiety and/or depression diagnoses (see Table 2).
Fig. 2.
Kaplan Meier Graph – anxiety/depression diagnosis and antibiotic exposure.
Table 2.
Multivariate Cox Proportional Hazard Model adjusted for age, race, sex, and insurance status Relationship with outcome of Anxiety and/or Depression Diagnosis.
| Anti-infective agent | No. of cases (%) | HRR | 95% CI | p value | |
|---|---|---|---|---|---|
| Any anti-infective prescription | 327 (61.5%) | 1.21 | 1.00 | 1.45 | 0.044 |
| Any antibiotics | 292 (54.9%) | 1.19 | 1.00 | 1.43 | 0.054 |
| No antibiotics | 240 (45.1%) | Reference Category | |||
| Broad spectrum | 220 (41.3%) | 1.27 | 1.04 | 1.54 | 0.017 |
| Narrow spectrum | 8 (1.5%) | 0.65 | 0.32 | 1.33 | 0.240 |
| Topical | 64 (12.0%) | 1.10 | 0.83 | 1.47 | 0.499 |
| Number of antibiotics (mean ± SD) | 1.02 ± 1.62 | 1.05 | 1.00 | 1.10 | 0.063 |
| Any antifungal | 55 (10.3%) | 0.90 | 0.67 | 1.21 | 0.496 |
| Any antiviral | 34 (6.4%) | 1.06 | 0.73 | 1.54 | 0.744 |
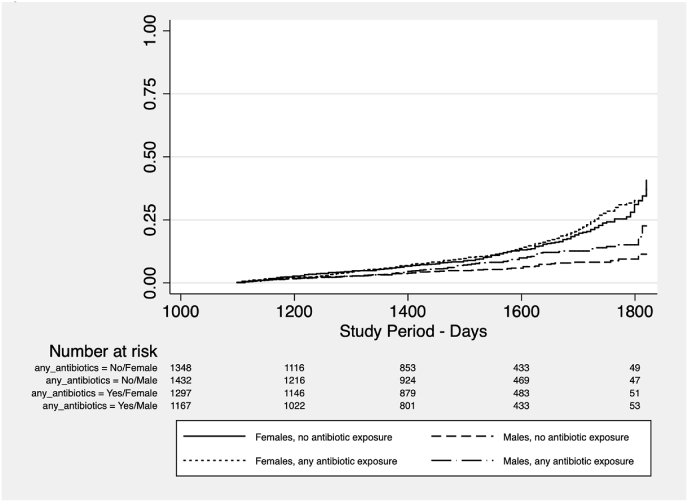
When stratified by sex (see Fig. 3, Table 2, Table 3), among males, any anti-infective prescription was associated with an HRR of 1.46 (95% CI = 1.05–2.02), and prescription of any antibiotic was associated with an HRR of 1.45 (95% CI = 1.05–1.99). Broad-spectrum antibiotics were associated with an HRR of 1.56 (95% CI = 1.12–2.19). The total number of antibiotic prescriptions during the study period was not significantly associated with anxiety and/or depression diagnoses, nor were antiviral, antifungal, narrow-spectrum antibiotics, nor topical antibiotic prescriptions among males. Among females, none of the exposure measures was significantly associated with anxiety/depression diagnosis.
Fig. 3.
Kaplan Meier Graph - anxiety/depression diagnosis and antibiotic exposure stratified by sex.
Table 3.
-Multivariate Cox Proportional Hazard model adjusted for age, race, and insurance status - Stratified by Sex
Relationship with Outcome of Anxiety and/or Depression Dx.
| Males | |||||||
|---|---|---|---|---|---|---|---|
| Anti-infective agent: | HRR | 95% CI | p value | ||||
| Any anti-infective prescription | 1.46 | 1.05 | 2.02 | 0.024 | |||
| Any antibiotics | 1.45 | 1.05 | 1.99 | 0.022 | |||
| No antibiotics | Reference category | ||||||
| Broad spectrum | 1.56 | 1.12 | 2.19 | 0.009 | |||
| Narrow spectrum | 0.71 | 0.17 | 2.93 | 0.639 | |||
| Topical | 1.22 | 0.72 | 2.07 | 0.456 | |||
| Number of antibiotics (mean ± SD) | 1.03 | 0.94 | 1.13 | 0.585 | |||
| Any antifungal | 0.71 | 0.37 | 1.35 | 0.291 | |||
| Any antiviral |
0.82 |
0.42 |
1.62 |
0.574 |
|||
| Females | |||||||
| Any anti-infective prescription | 1.08 | 0.87 | 1.35 | 0.495 | |||
| Any antibiotics | 1.08 | 0.87 | 1.34 | 0.507 | |||
| No antibiotics | Reference category | ||||||
| Broad spectrum | 1.13 | 0.89 | 1.44 | 0.301 | |||
| Narrow spectrum | 0.59 | 0.26 | 1.34 | 0.205 | |||
| Topical | 1.04 | 0.74 | 1.47 | 0.805 | |||
| Number of antibiotics (mean ± SD) | 1.05 | 1.00 | 1.11 | 0.064 | |||
| Any antifungal | 0.96 | 0.69 | 1.34 | 0.831 | |||
| Any antiviral | 1.15 | 0.74 | 1.80 | 0.528 | |||
The most common type of infection in this population was respiratory infection (65.5%, see Table 4). When stratified by sex, males had higher rates of respiratory infection than females (71.0% in males versus 61.2% in females, p < .0001) and females had higher rates of genitourinary infection (11.0% in females versus 1.6% in males, p < .0001).
Table 4.
Infection type by sex.
| Female | Male | Total | p value∗ | |
|---|---|---|---|---|
| Skin infection | 20 (5.0%) | 11 (3.5%) | 31 (4.3%) | 0.324 |
| Viral infection | 33 (8.2%) | 27 (8.5%) | 60 (8.3%) | 0.882 |
| Genitourinary infection | 44 (11.0%) | 5 (1.6%) | 49 (6.8%) | <.0001 |
| Respiratory infection | 246 (61.2%) | 225 (71.0%) | 471 (65.5%) | 0.006 |
| Other infection | 18 (4.5%) | 16 (5.1%) | 34 (4.7%) | 0.721 |
| STI routine screen | 32 (8.0%) | 23 (7.3%) | 55 (7.7%) | 0.724 |
| Other | 9 (2.2%) | 10 (3.2%) | 19 (2.6%) | 0.447 |
∗p value is from Chi-Squared test.
4. Discussion
We found evidence of an increased risk of anxiety or depression following broad-spectrum antibiotic exposure in a large primary care health system in the United States, specifically among males. These results are consistent with previous studies which used large scale, national health record data to address this question in a population consisting largely of individuals from Northern Europe (Köhler-Forsberg et al., 2019; Köhler et al., 2017). The recently more widespread availability of electronic medical record data allowed us to investigate these associations in a diverse population of children and adolescents living in an urban area in the United States.
Using clinical record data, we were able to replicate time-to-event statistical methods from research conducted using national health record data from Denmark (Köhler et al., 2017). It should be noted that our data source and population differ from that used in previous work. While Denmark offers a complete medical registry of data for all encounters and patients in the country, our patient data is limited to encounters occurring within this health system, meaning we could be missing data from encounters with outside providers. Additionally, the Denmark data represents a largely homogeneously white population. The population in this study was more diverse, with the largest groups being non-Hispanic African American (46%) and non-Hispanic white (42%). Thus, our findings from this research are more generalizable to many populations across the world that are heterogeneous and more diverse than those upon which the previous work in Europe was based.
Further studies should explore the source of potential sex differences in the relationship between antibiotic exposure and mental health. Studies suggest male children and adolescents may be more susceptible to changes in the microbiome, which ultimately leads to a dysregulation of the gut-brain axis, whereas females are more susceptible to hormonal differences and changes in adolescence (Kushak and Winter 2020; Kozyrskyj et al., 2016; Albert, 2015). It is also possible that the relationship is due to the different types of infections common among boys versus girls in early childhood. Among the first visits with antibiotic prescription in our study, males were more frequently diagnosed with respiratory infections than females and females were more frequently diagnosed with genitourinary infections. Thus, the different types of infection and/or antibiotics prescribed for these conditions could be behind the sex differences seen in the results. Ultimately, a better understanding of the pathogenic mechanisms underlying the relationships between infections, anti-infective agents, and mental health will help us delineate possible causes between the sex differences found in our study.
In order to sample only those patients that received the majority of their care within the JHCP system, we identified patients with at least three well-visits during the study period. We limited our population to those with at least three years of encounter data in order to allow for sufficient time for patients to potentially develop the outcome of interest. That said, we can only speak to prescriptions and diagnoses that took place during the study period, January 1, 2013 to January 1, 2019. Our exposure categories refer largely to the first recorded anti-infective exposure during our study period, not during a patient's lifetime. Lastly, more information on family history could help account for genetic predisposition toward depression and anxiety, but this information was largely unavailable in patients' EMR.
As stated earlier, it is notable that the males in the patient population appear to be primarily responsible for the correlation between antibiotic exposure and anxiety/depression. This is despite the fact that within our population, there are more females with an anxiety and/or depression diagnosis, indicating that surveillance bias may not be contributing to this association. It is also notable that Non-Hispanic African Americans were less likely to have a recorded anxiety or depression diagnosis. There could be many reasons for this, including racial bias in diagnosis, inequitable access to mental health professionals who make these diagnoses, or race-related mistrust of mental health care services (Garb, 2021; Cook et al., 2019). While this study was not designed to examine the causes of this racial disparity in diagnosis, it is an area that merits further study. While some previous work has noted the possibility of sex and race bias in ADHD and behavioral diagnoses, there is no substantial evidence of sex bias in diagnosis of anxiety and mood disorders (Garb, 2021; Tsirgiotis et al., 2021).
The potential for surveillance bias should be considered, given that parents who sought medical care for a child's infection may be inherently more likely to also seek care for anxiety or mood disorders, but it is unlikely that this sort of bias would differ by sex. It is also notable that other anti-infective medications included in this analysis, including antifungal agents, antiviral agents, and topical antibiotics, were not significantly related to the outcome measures. If surveillance bias were entirely responsible for the correlations found in this work, we would expect to see a relationship between these exposures and the outcome, as well.
Our findings suggest that children, particularly males, who receive antibiotic treatment for an infectious disease in childhood may be at increased risk for subsequent anxiety or depression. The mechanisms behind this association may be related to microbial modification due to the antibiotic treatment, the effects of the underlying infection for which the antibiotic is prescribed, or some combination of the two. The approximately 50% increase in hazard risk of anxiety and/or depression in males receiving broad-spectrum antibiotics is sizeable; if there is a causal link, a substantial number of cases in the population might be prevented by limiting the use of broad-spectrum antibiotics to cases where they are medically necessary. The vigilant and accurate diagnosis of non-severe infections in the primary care setting, and the judicious use of antibiotics, could help us to determine whether the infections themselves or the treatment are responsible for the observed increase in anxiety and depression, ultimately helping to prevent behavioral and psychiatric disorders in children, adolescents, and young adults.
Funding
Johns Hopkins Biostatistics, Epidemiology, and Data Management (BEAD) Core (internal funding); This work was also supported by the Stanley Medical Research Institute (grant #7R-1690) and by the NIMH P50 Silvio O. Conte Center at Johns Hopkins (grant #MH-94268).
Declaration of competing interest
The authors certify that they have no affiliations with or involvement in any organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- Albert P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015;40(4):219–221. doi: 10.1503/jpn.150205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsko R.H., Holbrook J.R., Ghandour R.M., et al. Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. J. Dev. Behav. Pediatr. 2018;39(5):395–403. doi: 10.1097/DBP.0000000000000571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B.L., Hou S.S., Lee-Tauler S.Y., et al. A review of mental health and mental health care disparities research: 2011-2014. Med. Care Res. Rev. 2019;76:683–710. doi: 10.1177/1077558718780592. [DOI] [PubMed] [Google Scholar]
- Curtin S.C., Heron M. Death rates due to suicide and homicide among persons aged 10-24: United States, 2000-2017. NCHS Data Brief. 2019;(352):1–8. [PubMed] [Google Scholar]
- Garb H.N. Race bias and gender bias in the diagnosis of psychological disorders. Clin. Psychol. Rev. 2021;90:102087. doi: 10.1016/j.cpr.2021.102087. [DOI] [PubMed] [Google Scholar]
- Ghandour R.M., Sherman L.J., Vladutiu C.J., et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J. Pediatr. 2019;206:256–267 e253. doi: 10.1016/j.jpeds.2018.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köhler O., Petersen L., Mors O., et al. Infections and exposure to anti-infective agents and the risk of severe mental disorders: a nationwide study. Acta Psychiatr. Scand. 2017;135(2):97–105. doi: 10.1111/acps.12671. [DOI] [PubMed] [Google Scholar]
- Köhler-Forsberg O., Petersen L., Gasse C., Mortensen P.B., Dalsgaard S., Yolken R.H., Benros M.E. A nationwide study in Denmark of the association between treated infections and the subsequent risk of treated mental disorders in children and adolescents. JAMA Psychiatr. 2019;76(3):271–279. doi: 10.1001/jamapsychiatry.2018.3428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozyrskyj A.L., Kalu R., Koleva P.T., Bridgman S.L. Fetal programming of overweight through the microbiome: boys are disproportionately affected. J. Dev. Orig. Health Dis. 2016;7(1):25–34. doi: 10.1017/S2040174415001269. [DOI] [PubMed] [Google Scholar]
- Kushak R.I., Winter H.S. Gut microbiota and sex in autism spectrum disorders [published online ahead of print, 2020 Jul 27] Curr. Pediatr. Rev. 2020 doi: 10.2174/1573396316999200727123026. 10.2174/1573396316999200727123026. [DOI] [PubMed] [Google Scholar]
- Mayer E.A., Knight R., Mazmanian S.K., Cryan J.F., Tillisch K. Gut microbes and the brain: paradigm shift in neuroscience. J. Neurosci. 2014;34(46):15490–15496. doi: 10.1523/JNEUROSCI.3299-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsirgiotis J.M., Young R.L., Weber N. A mixed-methods investigation of diagnostician Sex/Gender-bias and challenges in assessing females for autism spectrum disorder. J. Autism Dev. Disord. 2021 doi: 10.1007/s10803-021-05300-5. www.scopus.com [Internet] [DOI] [PubMed] [Google Scholar]