Abstract
Open tibial plafond fracture with massive bone loss presents a challenge for orthopedic surgeons. Particularly unusual is extrusion of an osteoarticular segment of the distal tibia. Here we present the case of such a patient, who was treated using osteochondral allograft (OCA) and fusion procedures. The patients can regain independent walking without pain within 6 months, indicating that OCA may be a sensible option for the treatment of open tibial plafond fracture with extrusion of the osteoarticular distal tibia in cases in which the surrounding soft tissue is intact but bone reimplantation is not possible due to severe damage and contamination.
Keywords: Ankle joint, Limb salvage, Massive bone loss, Osteochondral allograft, Tibial plafond fracture
Introduction
Tibial plafond fractures account for 5 to 10% of all tibial fractures [1], most of which are caused by high-energy trauma such a motor vehicle accident, falls from a height resulting in severe bone and articular comminution, bone loss, open fracture, and soft tissue compromise [2]. The management of open fracture and severe osteoarticular bone loss consists of reimplantation, autogenous bone graft, bone allograft, bone transportation, and amputation.
In this case, the patient presented with a type IIIA open fracture involving distal tibial and osteoarticular bone loss (10.5 cm), which was treated with debridement and a spanning external fixator and then ORIF with OCA and tibiotalar fusion. Few reports describing the treatment of extruded osteoarticular segments of the distal tibia have been published.
Case presentation
In February 2020, an otherwise healthy 21-year-old man was injured when his motorcycle collided with a car. The patient was brought to the hospital for severe trauma. He stated that he had no relevant medical history and had not undergone any previous surgical procedures. On initial examination, the patient was fully conscious with open fractures in his lower right lower leg. He had an 8 cm contaminated open wound on the lateral aspect of the right heel (Fig. 1A). The dorsalis pedis and posterior tibial artery pulse were palpable, sensation was intact at the dorsal and plantar of the foot, and the patient was able to flex and extend his toes. He was hemodynamically stable. Radiographs revealed a 10.5 cm bone loss of the tibial diaphysis and plafond with the medial malleolus and some part of the metaphysis remaining, and a fracture of the middle fibula (Fig. 1B).
Fig. 1.
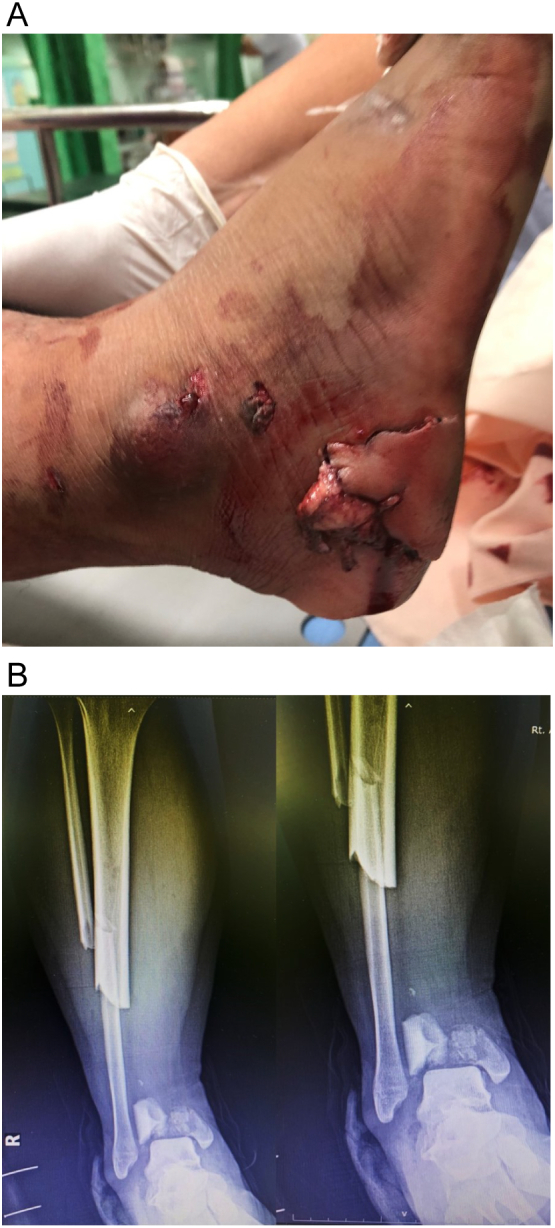
(A) An inside-out open wound on the lateral aspect of the right heel was initially observed. (B) Initial radiograph of the right leg revealed massive bone loss of the distal tibia and fracture of the midshaft fibula.
Surgical technique
At the initial operation, the left heel wound was debridement and copiously irrigated with normal saline pulse lavage. A piece of the patient's tibia was found at the scene of the accident. It was cleaned with sterile saline and brought in with the patient, but the first orthopedic team determined that the bone could not be used for reimplantation due to severe contamination with soil. Provisional stabilization was accomplished using a joint-bridging triangular external fixator, and open reduction and internal fixation was performed on the middle fibula with a one-third tubular plate to maintain the length of the leg (Fig. 2). There was no soft tissue defect, and the wound was loosely primary closure.
Fig. 2.
Postoperative radiographs after the first operation. A joint-bridging triangular external fixator was used and open reduction and internal fixation with a one-third tubular plate at the shaft fibula were performed.
The second operation was performed after the wound had completely healed without sign of infection and the patient had been treated with intravenous antibiotics for 20 days. The external fixator was removed, and a new 15 cm longitudinal incision was made on the anteromedial aspect of the distal tibia and ankle. The remaining bone of the medial malleolus and metaphysis was removed and used as an autogenous bone graft at the tibial and allograft docking site. Bone defect reconstruction was accomplished with a matched with 11 cm OCA fixed with a distal tibial locking plate (ANGIUS tibial plate; Intercus, German). The allograft was sterilized with 25 kilograys (kGy) of gamma radiation. Decortication of the articular surface of the distal tibia and talar dome was performed to prepare the tibiotalar joint, which was then fused with three screws through the distal tibial locking plate and two 4.0 cancellous screws at the lateral side (Fig. 3). Fusion was performed at neutral flexion and 10 degrees of external rotation. Systemic antibiotic therapy was continued for 2 weeks after the second operation. Following the operation, non-weight bearing ambulation with assistive devices as possible, and partial weight-bearing was allowed 2 months later.
Fig. 3.

Postoperative radiographs after the second operation. A matched OCA was fixed with a distal tibial locking plate. Tibiotalar joint fusion with multiple screws was performed and an autogenous bone graft was placed around the docking site.
Results
The patient was able to walk independently without pain and was able to stand on one leg on the injured side 6 months after surgery (Fig. 4). Postoperative radiographs at 12 and 24 months showed progression of interval healing callus formation at the tibial and allograft docking site (Fig. 5A, B). A scanogram revealed the right leg to be 2 cm shorter than the left (Fig. 6).
Fig. 4.
At 6 months post-operation, the patient was ambulating independently without pain and was able to stand on one leg on the injured side. AOFAS score was 79.
Fig. 5.

(A) Postoperative radiographs at 12 months revealed interval healing callus formation at the tibial and allograft docking site. (B) Postoperative radiographs at 24 months.
Fig. 6.

Scanogram at 12 months revealed that the right leg was 2 cm shorter than the left.
The patient has been undergoing follow-up for 24 months and is now able to jump but has some limitations about running and exercise. No specific complications have been observed. His American Orthopedic Foot and Ankle Society (AOFAS) score was measured at 79 points due to restriction of sagittal and highfoot motion because of tibiotalar joint fusion. The patient stated that he is very pleased with the outcomes of the treatment, which has resulted in pain-free ambulation without any restrictions in daily activities.
Discussion
Most tibial plafond fractures are due to high-energy trauma and are often associated with compromised soft tissues or bone loss. The reconstruction method is often determined by factors such as the patients' the severity, economic status, the surgeon's skills, and the availability of instruments [3]. Biological reconstruction has been shown to provide patients with superior long-term results over other alternatives. Ideally, it should involve the use of living or native bone, eliminate the possibility of infection, ensure callus regeneration and remodeling as well as good function, facilitate soft tissue attachment and durable reconstruction for a lifetime [4].
Typically, autogenous bone graft, cancellous allograft, synthetic bone substitutions, and demineralized bone matrix are used to treat small defects of metaphyseal bone loss (<5 cm) resulting from impaction at the time of injury [5]. In cases of a significant bone defect (>5 cm), reconstructive management for large bone defects can involve autograft, allograft, and non-biological materials. Autografts such as vascularized fibular graft transfer. The induced membrane technique and distraction osteogenesis is another alternative available for the reconstruction of bone defects and the main non-biological materials are endoprosthesis [6], [7]. Although there are several limbs salvaging operative options for management of open tibial plafond fracture with massive bone loss, each has inherent limitations, also are often complicated with infection, soft tissue loss, deformity, muscle contractures, shortening, osteopenia, and joint stiffness.
There have been some previous studies reporting a traumatic massive osteoarticular bone loss in the tibial plafond. Meininger et al. [8], for example, reported successful reimplantation of an extruded distal tibial osteoarticular segment 20 cm long with intramedullary nail fixation in a 33-year-old male. At 18 months, the patient had returned to work. Farrelly et al. [9] reported a 14-year-old female who was treated with reimplantation of an extruded distal tibial osteoarticular 15 cm long with plate and screw fixation, external fixator, and skin flap coverage. The patient was able to walk after 9 months. Reimplantation is one option for treating this condition if the bone was found at the scene of injury. However, this technique cannot be used if the bone has severe comminution or contamination. In our case, the first orthopedic team determined that the bone exhibited severe contamination.
An alternative method of treating an extruded distal tibial osteoarticular segment is the use of an external fixator for bone transport. Kim et al. [10] performed segmental bone transport on an approximately 12.5 cm osteoarticular segment of the distal tibia and talus in a 39-year-old female who was injured in a traffic accident. Distal tibiofibular, calcaneofibular, talonavicular, and fusion were performed at 7 months after injury. The patient demonstrated full weight-bearing after 9 months' treatment and 5 years' follow-up. The patient was able to walk without any restrictions with some limitations on running and exercising. Nonetheless, this surgical method requires training and experience to master, is time-consuming, and is physically and psychologically demanding for the patient [11].
Orthopedic oncologists have also used various methods of reconstruction after tumor resection at the distal tibia including massive allograft, prosthetic replacement, vascularized or non-vascularized autograft, recycled tumor-bearing bone, and bone transport [12]. However, there is no consensus about which is the gold standard treatment, as each technique has advantages and disadvantages. Andreas et al. [13] compared limb salvage using allograft and amputation for distal tibia osteosarcoma and reported higher average MSTS functional scores for patients that underwent limb salvage as opposed to those who had an amputation, but the incidence of complications such as fracture, nonunion, and deep infection was similar. However, soft tissue compromise and open fracture are key conditions that differentiate trauma patients from those with tumors. There is a high risk of infection when using osteoarticular allograft for reconstruction in cases of trauma. Fortunately, our patient had an inside-out open wound at the lateral aspect of the heel, whereas the soft tissue at the medial aspect (operative site) remained healthy, making OCA an appropriate treatment option. We used gamma irradiation from cobalt-60 to terminally sterilize bone allografts. Although sterilization of the fresh frozen allograft is critical [14], it may adversely affect the mechanical and biological properties of bone allografts by degrading the collagen in the bone matrix. In addition, OCA may result in graft resorption, lack of osteogenic capacity (especially osteogenesis and osteoinduction), immune rejection, and disease transmission [15]. In some countries, it is significantly difficult to obtain allograft as a biological reconstruction material because of socio-religious or cost problem. Gede EWI et al. [16] reported bone recycling using liquid nitrogen as a bone reconstruction procedure in malignant and recurrent benign aggressive bone tumor of the distal tibia and provide a good functional score with no infection and local recurrent. This technique may be applied to trauma cases. The decision to amputate or salvage a limb should also be based on factors such as the patient's pre-injury status, injury-related factors (location, soft tissue injury, contamination, and physiological status), the patient's wishes, and available resources [17].
Conclusion
OCA may be a sensible option in the treatment of open fracture of the tibial plafond with extrusion of the osteoarticular distal tibia in cases where the surrounding soft tissue is intact but bone reimplantation is not possible due to severe damage or contamination.
Funding
No funding.
Ethical approval
Approval taken from Hospital Ethical Committee.
Consent to participate
There is written consent of participation by the patient.
Consent for publication
There is written consent of publication by the patient.
Availability of data and material
Any further data and material can be received through contacting the corresponding author.
Code availability
Not applicable.
Declaration of competing interest
There are no conflicts of interest for any of the authors.
References
- 1.Bourne R.B. Pylon fractures of the distal tibia. Clin. Orthop. Relat. Res. 1989:42–46. [PubMed] [Google Scholar]
- 2.Muller F.J., Nerlich M. Tibial pilon fractures. Acta Chir. Orthop. Traumatol. Cechoslov. 2010;77:266–276. [PubMed] [Google Scholar]
- 3.Shin K.H., Park H.J., Yoo J.H., Hahn S.B. Reconstructive surgery in primary malignant and aggressive benign bone tumor of the proximal humerus. Yonsei Med. J. 2000;41:304–311. doi: 10.3349/ymj.2000.41.3.304. [DOI] [PubMed] [Google Scholar]
- 4.Lesensky J., Prince D.E. Distraction osteogenesis reconstruction of large segmental bone defects after primary tumor resection: pitfalls and benefits. Eur. J. Orthop. Surg. Traumatol. 2017;27(6):715–727. doi: 10.1007/s00590-017-1998-5. [DOI] [PubMed] [Google Scholar]
- 5.Bear J., Rollick N., Helfet D. Evolution in management of tibial pilon fractures. Curr. Rev. Musculoskelet. Med. 2018;11:537–545. doi: 10.1007/s12178-018-9519-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob N., Amin A., Giotakis N., Narayan B., Nayagam S., Trompeter A.J. Management of high-energy tibial pilon fractures. Strateg.Trauma Limb. Reconstr. 2015;10:137–147. doi: 10.1007/s11751-015-0231-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Migliorini F., La Padula G., Torsiello E., Spiezia F., Oliva F., Maffulli N. Strategies for large bone defect reconstruction after trauma, infections or tumour excision: a comprehensive review of the literature. Eur. J. Med. Res. 2021;26:118. doi: 10.1186/s40001-021-00593-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meininger A.K., Figuerres B.F., Parameswaran A.D., Nam E.K., Kapotas J.S. Extruded osteoarticular distal tibia: success at 18-month follow-up with reimplantation. J. Orthop. Trauma. 2010;24:e102–e107. doi: 10.1097/BOT.0b013e3181db72cf. [DOI] [PubMed] [Google Scholar]
- 9.Farrelly E., Ferrari L., Roland D., Difelice G.S. Reimplantation of an extruded osteoarticular segment of the distal tibia in a 14-year-old girl. Case report and review of the literature. J. Orthop. Trauma. 2012;26:e24–e28. doi: 10.1097/BOT.0b013e31821a06b0. [DOI] [PubMed] [Google Scholar]
- 10.Kim S.W., Seo D.-K., Lee C.-C., Kim H., Hwang I.-Y. Successful limb salvage using bone transport for complete loss of distal tibia and talus: a case report. J. Foot Ankle Surg. 2019;58:195–199. doi: 10.1053/j.jfas.2018.08.024. [DOI] [PubMed] [Google Scholar]
- 11.Rohilla R., Siwach K., Devgan A., Singh R., Wadhwani J., Ahmed N. Outcome of distraction osteogenesis by ring fixator in infected, large bone defects of tibia. J. Clin. Orthop. Trauma. 2016;7(Suppl 2):201–209. doi: 10.1016/j.jcot.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao Z., Yan T., Guo W., Yang R., Tang X., Wang W. Surgical options and reconstruction strategies for primary bone tumors of distal tibia: a systematic review of complications and functional outcome. J. Bone Oncol. 2019;14 doi: 10.1016/j.jbo.2018.100209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mavrogenis A.F., Abati C.N., Romagnoli C., Ruggieri P. Similar survival but better function for patients after limb salvage versus amputation for distal tibia osteosarcoma. Clin. Orthop. Relat. Res. 2012;470:1735–1748. doi: 10.1007/s11999-011-2238-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh R., Singh D., Singh A. Radiation sterilization of tissue allografts: a review. WorldJ. Radiol. 2016;28(4):355–369. doi: 10.4329/wjr.v8.i4.355. 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Delloye C., van Cauter M., Dufrane D., Francq B.G., Docquier P.-L., Cornu O. Local complications of massive bone allografts: an appraisal of their prevalence in 128 patients. Acta Orthop. Belg. 2014;80(2):196–204. [PubMed] [Google Scholar]
- 16.EWI Gede, Ida Ayu A.A., Setiawan I.G.N.Y., Aryana I.G.N.W., I Ketut S., I Ketut S.K. Outcome of bone recycling using liquid nitrogen as bone reconstruction procedure in malignant and recurrent benign aggressive bone tumour of distal tibia: a report of four cases. J. Orthop. Surg. (Hong Kong) 2017;25(2) doi: 10.1177/2309499017713940. [DOI] [PubMed] [Google Scholar]
- 17.Qureshi M.K., Ghaffar A., Tak S., Khaled A. Limb salvage versus amputation: a review of the current evidence. Cureus. 2020;12(8) doi: 10.7759/cureus.10092. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Any further data and material can be received through contacting the corresponding author.




