Summary
Five billion people lack access to surgical care worldwide; climate change is the biggest threat to human health in the 21st century. This review studies how climate change could be integrated into national surgical planning in the Western Pacific region. We searched databases (PubMed, Web of Science, and Global Health) for articles on climate change and surgical care. Findings were categorised using the modified World Health Organisation Health System Building Blocks Framework. 220 out of 2577 records were included. Infrastructure: Operating theatres are highly resource-intensive. Their carbon footprint could be reduced by maximising equipment longevity, improving energy efficiency, and renewable energy use. Service delivery Tele-medicine, outreaches, and avoiding desflurane could reduce emissions. Robust surgical systems are required to adapt to the increasing burden of surgically treated diseases, such as injuries from natural disasters. Finance: Climate change adaptation funds could be mobilised for surgical system strengthening. Information systems: Sustainability should be a key performance indicator for surgical systems. Workforce: Surgical providers could change clinical, institutional, and societal practices. Governance: Planning in surgical care and climate change should be aligned. Climate change mitigation is essential in the regional surgical care scale-up; surgical system strengthening is also necessary for adaptation to climate change.
Keywords: Climate change, Surgical system strengthening, Western pacific, Natural disasters, National health planning
Abbreviations: CO2, Carbon dioxide; DALY, Disability-adjusted life year; FEMAT, Fiji Emergency Medical Assistance Team; GHG, Greenhouse gas; HVAC, Heating, ventilation, and air conditioning; HICs, High-income countries; IPCC, Intergovernmental Panel on Climate Change; kgCO2e, Kilograms of carbon dioxide equivalent; LCoGS, Lancet Commission on Global Surgery; LCA, Life-cycle analysis; LED, Light-emitting diode; LMICs, Low- and middle-income countries; NSOAP, National Surgical, Obstetric, and Anaesthesia Plan; OR, Operating Room; SUD, Single-use device; SOA, Surgical, obstetric, and anaesthesia; WASH, Water, sanitation, and hygiene
Research in context.
Evidence before this study
Surgical system strengthening has been identified as a priority in the Western Pacific region. At the same time, the Western Pacific is among the most vulnerable regions to the effects of climate change and natural disasters. Considerations of climate change have been largely missing from the global surgery literature. We searched databases (PubMed, Web of Science, and Global Health) using the keywords climate change (“climate change”, “global warming”, “greenhouse gas”), and surgical, obstetric, anaesthesia, and trauma care (“surgical procedures”, “operating room”, “anaesthesia”, “maternal health”, “trauma”). We found previous reviews have focused on high-income countries rather than low- and middle-income countries (LMICs) and clinical practice rather than the broader health system.
Added value of this study
This is the first review to incorporate the perspectives of LMICs, a category encompassing many countries in the Western Pacific region, in considering the implications of climate change for surgical system strengthening. We took a system-based approach and provided a big picture overview of strategies for building sustainable and climate-resilient surgical systems. We comprehensively reviewed the available literature and generated policy-oriented recommendations contextualised to the diverse geographic, social, and economic circumstances of the Western Pacific region.
Implications of all the available evidence
Climate change and surgical system strengthening are closely linked. Actions for climate change mitigation and adaptation should be taken across surgical system infrastructure, service delivery, workforce, information management, finance, and governance, and could hence generate substantial co-benefits in financial cost savings and improving care access and quality. More research is urgently required to report the carbon footprint of surgical care, monitor the impact of climate change on surgically treated diseases, and share ground-up innovations across diverse income levels and geographic settings in the Western Pacific region.
Alt-text: Unlabelled box
Introduction
Surgical, obstetric, and anaesthesia care is required to treat a range of conditions, including obstructed labour, cancer, traumatic injuries, acute abdominal conditions, and congenital anomalies, among others. However, five billion people lack access to safe and affordable surgical care when required.1 In 2015, the Lancet Commission on Global Surgery (LCoGS) recommended scaling up surgical, obstetric, and anaesthesia care (SOA) care (referred to broadly as ‘surgical care’a) through developing national surgical plans.1
Climate change is the biggest threat to human health in the 21st century and has important implications for surgical care.2 Surgical care delivery could affect both climate change mitigation – the prevention of climate change, and adaptation – reducing vulnerabilities to the effects of climate change. On the one hand, surgical care provision can be carbon intensive: the health sector, as a whole, contributes about 4·9% of total global greenhouse gas (GHG) emissions.3 On the other hand, surgical system strengthening is essential in response to rising disease burdens from climate change, such as injuries from natural disasters.4
The intersection between climate change and surgical system strengthening is significant to the Western Pacific region.b Despite substantial geographic, economic, and social diversity, the region has a shared vulnerability to climate change and natural disasters.5 Between 1970 and 2011, 75% of the global natural disaster fatalities occurred in the Asia-Pacific region.6 The 2021 Intergovernmental Panel on Climate Change (IPCC) Sixth Assessment Report projected heavy precipitations, floods, and cyclones to intensify across the Asia-Pacific region under all future climate trajectories.7 At the same time, surgical system strengthening has been identified as a regional priority. In 2019, Pacific Health Ministers, at their 13th biennial meeting, committed to developing National Surgical, Obstetric, and Anaesthesia Plans (NSOAPs) towards achieving the Healthy Island Vision.8 In 2020, Member States unanimously endorsed the World Health Organization (WHO) Action Framework for Safe and Affordable Surgery in the Western Pacific Region at the 71st Regional Committee Meeting.9
As countries in the Western Pacific scale up surgical care, there is a unique opportunity to reimagine and build sustainable and climate-resilient surgical systems. This is urgently required as climate change has become a rapid, widespread, and unprecedented reality and as the COVID-19 pandemic provides an opportunity to build back better.7 Climate change is relevant to both low- and middle-income countries (LMICs) developing surgical systems and high-income countries (HICs) retrofitting and redesigning surgical systems. Much of the global surgery literature, including the LCoGS, has not taken climate change into account.1 The Western Pacific region could lead by example in pioneering surgical system strengthening in the context of climate change and identifying transferrable solutions that are globally relevant. Therefore, this narrative review aims to comprehensively examine the available literature and generate evidence-based, policy-oriented recommendations for integrating climate change into national surgical planning in the Western-Pacific region.
Methods
Search strategy and selection criteria
We conducted a literature search of PubMed, Web of Science, and Global Health in August 2020 and updated it in April 2021. We combined two categories of search terms: climate change (“climate change”, “global warming”, “greenhouse gas”), and surgical, obstetric, anaesthesia, and trauma care (“surgical procedures”, “operating room”, “anaesthesia”, “maternal health”, “trauma”). A full list of search terms is presented in the supplementary material. Search terms on specific mediators of climate change, such as heat or food insecurity, were not included as the primary purpose of the review was to capture the broad impact of climate change on surgical care. We identified further relevant literature from the references of included articles and an expert-generated list of key regional grey literature publications in view of the interdisciplinary nature of this topic.
Articles were screened in two stages; RQ and LV screened the titles and abstracts of the retrieved literature, then full-text reviews were performed by RQ, LV, EFY, and OE. We included articles published after 1990 that described the effects of anthropogenic climate change on surgical and anaesthesia care and vice versa. Articles were excluded if their full texts were unavailable, if they studied non-human subjects, conditions not requiring surgical care, environmental impacts other than climate change, or if they lacked sufficient regional relevance.
Data extraction
Data were extracted using the modified WHO Health Systems Building Block Framework, which is used for developing NSOAPs.10,11 Results were thematically synthesised in six domains: infrastructure, service delivery, workforce, information management, financing, and governance (Figure 1).
Figure 1.
A framework for developing National Surgical, Obstetric, and Anaesthesia Plans (NSOAPs).11
Role of funding source
None.
Results
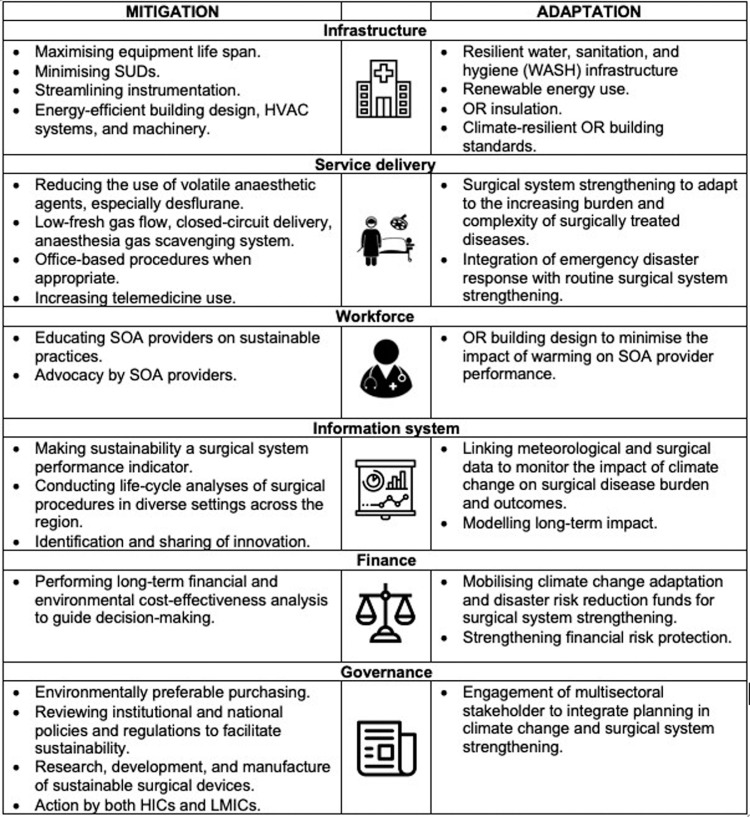
We screened 2577 unique records and included 220 records in the final review. A complete list of included papers is provided in the supplementary material. Results were synthesised and presented by health system domain (Figure 2). We noted that the literature on this topic includes many commentaries and opinion pieces; however, a formal quality assessment is beyond the scope of this review. There are a few hot spots where the evidence is more mature, such as the impact of heat on birth outcomes, anaesthetic drugs and inhaled agents, and reusable versus disposable equipment. However, despite the growth in literature over the last five years, the evidence is still limited in many other areas. Most studies were conducted in HICs, with very few in LMICs, a category to which many countries in the Western-Pacific region belong.
Figure 2.
Strategies for climate change mitigation and adaptation in surgical system strengthening.
GHG = greenhouse Gas Emissions; HVAC = heating, ventilation, and air conditioning; HIC = high-income country; LMIC = low- and middle- income country; OR = operating Room; SOA = surgery, obstetrics and anaesthesia; SUD = single-use devices.
Infrastructure
Mitigation
Operating rooms (ORs) are a highly resource-intensive component of the health system. They can be three to six times more energy-intensive than the hospital average and consume 40–60% of a facility's supply chain.12 Environmental impact assessment through life-cycle analyses (LCA) has shown the emission profile of surgical procedures to vary substantially by facility and procedure. The main sources of GHG emissions from surgical procedures are equipment and consumables, inhaled anaesthetic agents, and energy use. Studies have shown that a combination of measures targeted at different sources can reduce the carbon footprint of ORs by 80–95%.13,14
Equipment and consumables
Equipment and supplies are found to contribute to 60–70% of total GHG emissions of surgical procedures when anaesthesia and energy usage are optimised.12,13
The majority of emissions arise from the manufacturing process. This calls for strategies to maximise equipment lifespan and reduce emissions per use. A number of studies in HICs have demonstrated reusable equipment to be environmentally superior to single-use devices (SUDs) for a wide range of equipment and procedures, potentially reducing GHG emissions by up to 90%.15, 16, 17, 18, 19, 20, 21, 22, 23 The few studies that found SUDs to be environmentally beneficial have all been conducted in Australia, where electricity is mainly generated from the carbon-intensive source of coal.15,24,25 Environmentally preferable purchasing policies could guide the selection of equipment and consumables based on their long-term financial and environmental cost rather than their up-front cost.26 In LMICs, around 40% of equipment and consumables can be non-functional due to the lack of maintenance.27 This can be improved through strengthening biomedical engineering services.
The number of instruments opened per case can be reduced to the minimum required. A large proportion of instruments may only be included to anticipate surgeons’ needs and end up unused28. Thiel et al. found that minimising the number of SUDs opened decreased GHG emissions in laparoscopic surgery (excluding anaesthesia) by 70% in a United States hospital.13 A more parsimonious approach to surgical trays has been demonstrated to be feasible and cost-effective. Substantial environmental benefit is foreseeable and should be quantified by future studies.29
Energy use
In HICs, energy use has been found to account for between 10 and 80% of total OR emissions.12 The most significant contributors are heat, ventilation, and air-conditioning (HVAC) systems, followed by lighting and machinery.12,30,31 ORs are highly energy-intensive due to their unique requirement for stringent temperature and ventilation control for patient safety and microbial control. Occupancy sensors or energy-efficient scheduling, such as adapted weekend settings, could reduce HVAC energy consumption when ORs are not in use.32,33 The energy demand for lighting and machinery could be reduced by replacing older equipment with more energy-efficient options, such as light-emitting diode (LED) lights.26,34 There may be efficiencies with scale: providers in LMICs found increasing surgical volume and maximising OR occupancy reduced the per-case carbon footprint.35
Emissions attributable to energy use varies widely between facilities due to the differences in energy source. Health systems with carbon-intensive electricity sources have substantially higher GHG emissions from energy use and surgical equipment reprocessing.12,15,24,25 This highlights that surgical system sustainability cannot occur in isolation without overall energy sector decarbonisation.
Adaptation and resilience
Infrastructural resilience in OR building design, energy infrastructure, and water, sanitation, and hygiene (WASH) facilities is necessary for adaptation to climate extremes.
Energy reliability is a common issue in LMICs and could be exacerbated by electricity line damage during heavy precipitation and high winds.36 Power outages have been associated with adverse obstetric and surgical outcomes,37,38 and could disrupt the cold supply chains of essential obstetric medications.39 Off-grid facility-based renewable energy generation and renewable energy-powered devices, such as dryers and autoclaves, could provide a win-win opportunity for sustainability and climate resilience.40
Safe surgery cannot occur without adequate WASH facilities. Climate extremes such as heavy precipitation, floods, and droughts could compromise water supply and quality. This risk could be reduced by infrastructural considerations, such as non-return valves to prevent backflow, sealed covers for septic tanks, locating storage tanks away from flood-prone areas, and placing vents above the flood-line.36 Moreover, long-term water collection systems could balance water excess and shortage during floods and droughts and reduce water consumption from other sources.36
Building climate-resilient infrastructure involves the whole health system and may, in some cases, necessitate relocating entire health facilities from disaster-prone sites. ORs are particularly vulnerable to climate extremes due to their strict ventilation and temperature requirements.33 White reflective roofs, retrofitting insulation, energy-efficient windows, and heat or coolness recovery devices could improve both OR energy efficiency and resilience to temperature extremes.36,41 Climate-resilient OR building standards should be developed, particularly in tropical areas of the Western Pacific region,.42
Service delivery
Mitigation
Anaesthesia
Inhaled anaesthetic agents are potent greenhouse gases. Among them, desflurane has the greatest global warming potential (GWP), more than 2000 times that of carbon dioxide (CO2), while sevoflurane is only 130 times as potent as CO2.13 Halothane, an anaesthetic gas essentially obsolete in most HICs, remains widely used in parts of the Western Pacific region. Its GWP has not been well studied and warrants further attention.43
While patient safety must be the primary driver for anaesthetic care delivery, several strategies could reduce its GHG emissions.
-
•
Disproportionate use of desflurane has been found to be responsible for up to 80% of GHG emissions in ORs in HICs.12,44 Systematically switching from desflurane to sevoflurane can lead to a ten-fold reduction in carbon footprint and significant cost savings.45
-
•
The use of volatile anaesthetic agents could be profoundly limited by preferentially using total intravenous anaesthesia and regional anaesthesia when appropriate.46, 47, 48 Regional anaesthesia could have additional advantages in low-resource and hard-to-reach settings, including cost, safety, OR efficiency, and the potential for task-shifting to non-specialist providers,49 thereby improving access as well as sustainability.
-
•
Using low fresh gas flow or closed-circuit delivery can reduce the volume of volatile gas consumed by 20%.45,50,51
-
•
New technologies, such as Dynamic Gas Scavenging Systems or silica zeolite, can absorb, destroy, and even recycle anaesthetic waste gases.52, 53, 54
Surgery
The mode of surgical care delivery can also alter its carbon footprint. Studies have found emissions of robotic surgery > laparoscopic surgery > open surgery.30,55 This is primarily due to CO2 use for insufflation and a greater number of single-use instruments.13,56 However, studies conducted thus far have not considered the potential environmental benefit of minimally invasive surgery in reducing the postoperative length of stay or readmissions from sequelae of open surgery, such as adhesive bowel obstruction and incisional hernia.57 Studies examining long-term environmental impact are required before conclusions could be drawn. The mode of surgery should be selected primarily based on clinical indications. Laparoscopic surgery has proven clinical benefits over open surgery in many circumstances. However, environmental impact should weigh more heavily into consideration where there is clinical equipoise, such as between robotic and laparoscopic surgery.
In terms of the location of surgery, performing minor operations, such as skin lesion excision and carpal tunnel release, in a clinic setting where appropriate could reduce GHG emissions associated with maintaining an OR environment and improve service access when ORs are unavailable.47
Travel-related emissions
In HICs, innovative service delivery models such as telemedicine and mobile outreaches have been found to reduce GHG emissions from patient travel while offering more accessible, patient-centred care.58, 59, 60 In LMICs, improving district-level surgical care capacity could reduce referrals to higher centres. Overall domestic surgical system strengthening could reduce the number of overseas medical referrals and specialist visits, particularly in Pacific Island Countries. The environmental benefits of both strategies could be speculated but are yet to be quantified.
Adaptation
Not only does surgical care delivery impact climate change, but climate change could also increase the burden of diseases requiring surgical care.
Direct impacts
By increasing temperature, precipitation, and extreme weather events, climate change can increase the incidence, range, and complexity of infectious, non-communicable, maternal, and neonatal conditions requiring surgical care (Table 1). This calls for surgical system strengthening as a part of climate change adaptation in response to the increasing burden of diseases requiring surgical care.42
Table 1.
The potential direct impact of climate change on diseases requiring surgical, obstetric, anaesthesia, and trauma care.
| Surgical disease categories |
||||
|---|---|---|---|---|
| Climatic variables | Infections | Non-communicable diseases | Trauma | Maternal and neonatal conditions |
| Increase in temperature | Necrotising vibrio skin infections61, 62, 63, 64 Schistosomiasis causing bladder cancer65 Fungal sinusitis66 Sinusitis67 |
Skin cancers68, 69, 70, 71, 72 Kidney stones73, 74, 75 Testicular torsion76 |
Road traffic accidents77,78 All categories of injury77 |
Pre-term birth (meta-analysis of 47 studies79) Stillbirth (meta-analysis of 8 studies79) Low birth weight (systematic review of 28 studies80) Pre-eclampsia81,82 Premature rupture of membranes83 Congenital heart disease62 |
| Increase in precipitation | Acute glaucoma77 Kidney stones75 |
Road traffic accidents84 | Pre-term birth85 Low birth weight85 Pre-eclampsia86 |
|
| Extreme weather events | Bushfires – Burns87 Flood/storms –injuries4,5,88,89 |
|||
Natural disasters
Among the direct effects of climate change, extreme weather events are of particular relevance to the Western Pacific region. Climate change is expected to increase the frequency and severity of extreme weather events throughout the Western Pacific region, such as floods and cyclones in Asia and the Pacific, and droughts and bushfires in Australia.7,68,90,91
Strengthening domestic surgical care capacity in LMICs is critical for mounting a rapid and effective disaster trauma response. Studies found that foreign field hospitals were rarely deployed early enough across LMICs,92,93 whereas local surgical responses, such as after the 2008 Sichuan earthquake in China, have been effective in averting disability-adjusted life years (DALYs) and economic loss.94 However, the availability and quality of surgical services at the district level have been found to be a critical gap in the health system response to extreme weather events in Vietnam.89
There is increasing recognition that disaster trauma response should not be an isolated vertical intervention but rather integrated into the broader surgical system. Surgical needs after sudden-onset disasters have been widely documented to include not only traumatic injuries but also non-traumatic emergencies, such as Caesarean sections and hernia repairs.88,95,96
Significant synergy exists between emergency trauma response and routine surgical system strengthening.94,97 For example, when not deployed, the Fiji Emergency Medical Assistance Team (FEMAT) is integrated into routine surgical service delivery by providing outreach surgical services in district hospitals. This strengthens both first-level hospital surgical capacity and keeps FEMAT in a state of constant readiness for deployment.
During the COVID-19 pandemic, the versatility of surgical systems has become apparent as ORs, surgical supply chains, and human resources have been converted to provide critical surge capacity worldwide.98 As countries battle climate-induced natural disasters during the COVID-19 pandemic, the need for surgical system strengthening as a part of multi-hazard emergency preparedness and overall health system resilience is ever more highlighted.
Indirect impacts and co-benefits
Climate change could have complex and interconnected impacts on surgically treated diseases and surgical complications in the Western Pacific region through changing physical, social, and economic environments. For example, drought and saltwater intrusion could impair access to WASH and increase the risk of surgical site infections.91,99 Food insecurity could lead to both malnutrition and non-communicable diseases and increase the risk of peri-operative complications.100
The potential co-benefits of climate change mitigation and surgical disease prevention should be explored. For example, active and public transport could reduce GHG emissions and road traffic injuries requiring surgical care.68
Workforce
Mitigation
Educating SOA providers on sustainability has been found to reduce the carbon footprint of their clinical practice.45,101,102 Focused educational initiatives have been successful in reducing OR waste production by 50% and GHG emissions from anaesthesia care by 64%, and generated cost savings in HICs. 45,51,103, 104, 105 Beyond dedicated educational sessions, the literature also recommends embedding climate change into continuous medical education and routine training curricula.28,101,105,106 Successful education programs have used personal narratives for emotional appeal and targeted the multi-disciplinary team.105,106 They have integrated environmental stewardship with patient outcomes and cost savings to emphasise the triple bottom line of people, planet, and economic benefit. 45,51
Beyond changing individual practices, SOA providers have a powerful voice in advocating for institutional and societal changes, such as hospital procurement, industry equipment design, and governmental mitigation targets.102,107,108 SOA providers have a track record of successfully influencing policy in seatbelt and helmet use for trauma risk reduction. They have a responsibility to do so again with climate change.109 Professional engagement in climate change has been an area of significant progress in the global effort to combat climate change within the last decade and should continue into the future.110
Adaptation
Increasing temperature due to climate change could reduce workability in many parts of the Western Pacific region.9 This most significantly affects outdoor workers and labourers. However, indoor hospital spaces for surgical care, such as gynaecology scanning rooms, have also been found to be affected.111
The work performance of SOA providers could be compromised if OR temperature regulation mechanisms are overwhelmed. Hot temperatures can impair surgeons’ performance by decreasing manual dexterity and increasing self-rated physical demand and frustration levels.112,113 Although OR air-conditioning systems provide an effective means of climate change adaptation, they could paradoxically worsen climate change and harm health through energy use and air pollutant production.68,110 The energy-efficient OR building design considerations aforementioned in the infrastructure section could also reduce air conditioner use and improve workability.41
Information management
Health information system
Firstly, environmental sustainability should be incorporated as a key performance indicator for surgical systems in addition to the six LCoGS indicators.1 As healthcare access and quality improve in LMICs, GHG emissions are expected to increase. However, the positive correlation between healthcare quality and GHG emissions ceases after a point. Beyond 500–600 kg of carbon dioxide equivalent (kgCO2e), additional increases in per-capita healthcare emissions are not associated with improved human development index anymore.3 Therefore, emissions per procedure should be monitored and reported at the individual, departmental, facility, and national levels to drive quality monitoring and improvement towards sustainability.51
Secondly, a lack of information has been cited as the main barrier to sustainable practices.102 Life-cycle emissions of equipment and medications should be made readily available to inform clinical practice and environmentally preferable purchasing decisions. Solutions suggested include displaying emission information on product packaging and in mobile applications.45,101
Thirdly, meteorological data should be linked with surgical data to examine the impact of weather variables on surgically treated diseases and surgical care outcomes.68,110,114 They could be coupled with disease-specific registries or existing efforts to monitor peri-operative complications, such as peri-operative mortality as an LCoGS indicator.1 Quality data are notably lacking in disaster response.93 National databases on extreme weather events and surgically treated conditions should be maintained.115
Research
Most of the studies included in this review have been conducted in HICs. Aside from a few well-researched areas, such as heat-related birth outcomes and anaesthetic gases, the evidence on this topic is still limited and dominated by commentaries and opinion pieces. There is a need for more research on this topic in the Western Pacific region, particularly from LMICs. Future research could follow three directions below:
-
1.
Reporting and tracking emissions from surgical care: The GHG emission profile of surgical procedures are highly context- and procedure-specific. Results from one facility or country may not be readily generalisable to another. There is a need for LCAs across more facilities and procedures in the region to identify locally contextualised solutions for emission reduction. Whilst LCAs can be highly resource- and labour-intensive, top-down regional and country-level modelling could be combined with bottom-up process-based analyses of a representative sample of countries, facilities, and procedures across sub-regions and income levels.32
-
2.
Modelling the impact of climate change on surgical care provision. Surgically treated diseases have, thus far, not been well covered by studies on the health impact of climate change.78 Very few studies have modelled the long-term effects of climate change on the burden of surgically treated diseases to inform future surgical system design.
-
3.
Identification and sharing of innovations. Sustainable SOA care can be achieved by low-tech and no-tech innovations, such as outreach services, and high-tech innovations, such as volatile anaesthetic agent scavenging and recycling.52 For example, by adopting a range of measures to maximise OR turnover, Aravind hospital in India was able to provide cataract surgery at 5% of the emissions in the United Kingdom.116 There is a need for SOA providers to work together with scientists and the industry to develop technological innovations, such as solar-powered devices.40
Finance
Strategies to reduce emissions in SOA care often have significant financial co-benefits. Despite the upfront cost of capital purchases, studies have demonstrated substantial long-term cost savings from measures, such as improving building energy efficiency, reprocessing instruments, anaesthesia gas scavengers, and telemedicine.15,24,26,51,52,59,60 The results of life-cycle economic and environmental analyses must be taken into account by hospital managers, donors, and financial mechanisms in supporting sustainable infrastructural upgrades.
Costs saved could directly benefit individual patients. For example, telehealth services could mitigate financial risk arising from out-of-pocket expenditures for transport.59,117 Financial risk protection will be increasingly indispensable to surgical system strengthening as poverty, resource uncertainty, and inequity are predicted to increase with climate change.2
The importance of surgical system strengthening in climate change mitigation and adaptation should be recognised by funders, bilateral and multilateral agencies, financing mechanisms, and philanthropic organisations. Currently, only a very small proportion of the available climate change adaptation funds has been allocated to health-related programs,110,118 even less to surgical care.89 Such funds could be mobilised as an additional source for surgical system strengthening.
While foreign field hospitals in natural disasters have attracted a lot of international attention and resources, their effectiveness and accountability have been questioned.92,95 Disaster relief funds could be channelled into baseline surgical system strengthening as an effective and sustainable means of providing an emergency trauma response.
Governance
Facility level
Beyond changing individual clinician practices, institutional practices in procurement, energy use, and service design should be shifted towards sustainability.45 Environmentally preferable purchasing policies should be developed to guide sustainable procurement decisions.119,120
National level
Strategic planning in surgical system strengthening, climate change mitigation and adaptation, and disaster risk reduction should be closely integrated.103,121 Collaboration between multisectoral stakeholders is required for a health-in-all policy approach.
Regulation and policies should facilitate sustainability where possible. For example, SUD reprocessing can lead to environmental and cost benefits and is increasingly used in both HICs and LMICs.28 It is prohibited in many countries despite being shown to be safe in approved contexts.122 With more evidence being generated in the future, regulations could be updated to delineate the appropriate parameters around its use.
Private sector engagement is indispensable due to its role in surgical device research, development, and manufacture. Sustainability in the surgical device industry could be shaped by governments through funding, regulation, and incentives, and by clinicians through advocacy and lobbying.101,108
The participation of diverse stakeholders, especially civil society and service users, could be facilitated through consultative processes indigenous to the Western Pacific region, such as the Talanoa Dialogue launched by Fiji at the United Nations Climate Change negotiations.123
International level
Although there has been an accelerated focus on surgical system strengthening in LMICs, HICs in the Western Pacific region also play an important role. HICs produce substantially more GHG emissions from surgical care than LMICs. For example, emissions from minimally invasive surgery alone in the United States are estimated to be higher than the gross national emission of some countries.56 HICs in the region have both the responsibility and the ability to make a significant contribution to climate change mitigation by transforming their surgical systems.
Discussion
We conducted a comprehensive narrative review and outlined policy recommendations for integrating climate change perspectives into surgical system strengthening in the Western Pacific region. Not only must climate change mitigation be an essential consideration in the regional surgical care scale-up, but surgical system strengthening is also necessary for climate change adaptation and disaster preparedness. As countries in the Western Pacific strengthen their surgical systems, they have a unique opportunity to reimagine and redesign sustainable and climate-resilient surgical systems with co-benefits for the environment, finance, and service quality, pioneering a path for the region and beyond.
Previous reviews have been conducted on climate change and surgical care; however, they primarily focused on HICs. Our study is one of the first to incorporate LMIC challenges and perspectives. This is important as countries in the Western Pacific region span a range of income status. Moreover, previous reviews have mostly focused on sustainability in clinical care provision, whereas we examined the implications of climate change for the broader surgical system across all health system domains.
The strength of this review is that it provides a comprehensive overview of a large body of literature on a novel and important topic. Our search strategy was extensive but not exhaustive due to the expansive and interdisciplinary nature of this topic. Poor data availability and inconsistent quality of evidence, particularly from LMICs, limit our recommendations. Moreover, the recommendations outlined in this review are not one-size-fits-all. Results from one country may not be readily generalisable across the whole region due to diverse social, economic, geographical, and cultural contexts. Our study provides a framework for approaching the integration of climate change into surgical system strengthening. Strategies for doing so must be locally contextualised to each country and facility.
There is an imperative for more research from diverse settings across the Western Pacific region to identify strategies and innovations for climate change mitigation and adaptation in surgical system strengthening in each context. The number of publications on this topic from the Western Pacific region should be monitored by country, sub-region, and income status to encourage diverse representation.
Considerations of climate change mitigation and adaptation must be integrated into surgical system strengthening in the Western Pacific region. The time to act is now as climate change has already become a part of our reality. Even modest reductions in global warming will avoid serious incremental increases in climate extremes.7 As we plan to build back better from the COVID-19 pandemic, there is a unique and critical window to create sustainable and resilient surgical systems to face the larger climate crisis.
SOA providers have a track record in effecting successful public policy changes for surgically treated diseases such as trauma prevention. As the IPCC sixth assessment report declares a code red for the planet,7 SOA providers have the responsibility to urgently attend to this ‘trauma call’ and lead the advocacy for climate change mitigation and adaptation in surgical system strengthening and beyond.
Declaration of interests
The authors declare no conflict of interest.
Acknowledgments
Contributors
RQ, LV, EFY, OE, and CDM conceptualised and designed the study with input from AW. The literature review and screening were performed by RQ and LV. Input on additional literature sources was provided by JT, LS, EM, and AW. RQ, LV, EFY, and OE extracted and analysed the study data. RQ drafted the manuscript. LV created the figures. All authors contributed to data interpretation and manuscript review and editing. All authors read and approved the final manuscript, and agreed to be accountable for all aspects of the work.
Acknowledgments
The authors would like to acknowledge Philip J. Landrigan for his review and feedback on an early version of the manuscript.
Consent for publication
All authors approved the final version submitted for publication.
Data sharing statement
All data analysed in this review are included in the references and the Supplementary materials.
Footnotes
“Surgical care” is an overarching term used to denote care for adults and children delivered by anaesthetists, obstetricians and gynaecologists, and surgeons from various backgrounds including, but not limited to, adult and paediatric general surgery, orthopaedics, neurosurgery, urology, ophthalmology, otorhinolaryngology, and vascular surgery, as well as nursing, midwifery, and all allied health professionals.
The Western Pacific region is defined according to the WHO region designation and comprises 37 countries. (https://www.who.int/westernpacific/about/where-we-work Accessed August 27th, 2021).
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100407.
Appendix. Supplementary materials
References
- 1.Meara J.G., Leather A.J.M., Hagander L., et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 2.Costello A., Abbas M., Allen A., et al. Managing the health effects of climate change: lancet and University College London Institute for Global Health Commission. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 3.Romanello M., McGushin A., Napoli C.D., et al. The 2021 report of the lancet countdown on health and climate change: code red for a healthy future. Lancet. 2021;398:1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PubMed] [Google Scholar]
- 4.Lee E.E., Stewart B., Zha Y.A., Groen T.A., Burkle F.M., Kushner AL. Surgical care required for populations affected by climate-related natural disasters: a global estimation. PLoS Curr. 2016;8 doi: 10.1371/currents.dis.e601960a8cd66c3083d160877abfdde4. ecurrents.dis.e601960a8cd66c3083d160877abfdde4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Regional Office for the Western Pacific. Climate change and health in the Western Pacific region: synthesis of evidence, profiles of selected countries and policy direction. Manila, Philippines, 2015.
- 6.Hashim J.H., Hashim Z. Climate change, extreme weather events, and human health implications in the Asia Pacific region. Asia Pac J Public Health. 2016;28:8S–14S. doi: 10.1177/1010539515599030. [DOI] [PubMed] [Google Scholar]
- 7.IPCC . Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; Cambridge, UK: 2021. Summary for policymakers. In Press. [Google Scholar]
- 8.WHO . World Health Organization; Tahiti, French Polynesia: 2019. Outcomes of the Thirteenth Pacific Health Ministers Meeting. [Google Scholar]
- 9.World Health Organization Regional Office for the Western Pacific. Action framework for safe and affordable surgery in the Western Pacific region: 2021–2030. Manila, Philippines, 2021.
- 10.Peters A.W., Roa L., Rwamasirabo E., et al. National surgical, obstetric, and anesthesia plans supporting the vision of universal health coverage. Glob Health Sci Pract. 2020;8:1–9. doi: 10.9745/GHSP-D-19-00314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Truché P., Shoman H., Reddy C.L., et al. Globalization of national surgical, obstetric and anesthesia plans: the critical link between health policy and action in global surgery. Glob Health. 2020;16:1. doi: 10.1186/s12992-019-0531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacNeill A.J., Lillywhite R., Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381–e388. doi: 10.1016/S2542-5196(17)30162-6. [DOI] [PubMed] [Google Scholar]
- 13.Thiel C.L., Woods N.C., Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am J Public Health. 2018;108:S158–S164. doi: 10.2105/AJPH.2018.304397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thiel C.L., Schehlein E., Ravilla T., et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43:1391–1398. doi: 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGain F., Story D., Lim T., McAlister S. Financial and environmental costs of reusable and single-use anaesthetic equipment. Br J Anaesth. 2017;118:862–869. doi: 10.1093/bja/aex098. [DOI] [PubMed] [Google Scholar]
- 16.McGain F., McAlister S., McGavin A., Story D. The financial and environmental costs of reusable and single-use plastic anaesthetic drug trays. Anaesth Intensive Care. 2010;38:538–544. doi: 10.1177/0310057X1003800320. [DOI] [PubMed] [Google Scholar]
- 17.Eckelman M., Mosher M., Gonzalez A., Sherman J. Comparative life cycle assessment of disposable and reusable laryngeal mask airways. Anesth Analg. 2012;114:1067–1072. doi: 10.1213/ANE.0b013e31824f6959. [DOI] [PubMed] [Google Scholar]
- 18.Sherman J.D., Raibley L.A., Eckelman MJ. Life cycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anesth Analg. 2018;127:434–443. doi: 10.1213/ANE.0000000000002683. [DOI] [PubMed] [Google Scholar]
- 19.Leiden A., Cerdas F., Noriega D., Beyerlein J., Herrmann C. Life cycle assessment of a disposable and a reusable surgery instrument set for spinal fusion surgeries. Resour Conserv Recycl. 2020;156 [Google Scholar]
- 20.Unger S., Landis A. Assessing the environmental, human health, and economic impacts of reprocessed medical devices in a Phoenix hospital's supply chain. J Clean Prod. 2016;112:1995–2003. [Google Scholar]
- 21.Vozzola E., Overcash M., Griffing E. An environmental analysis of reusable and disposable surgical gowns. AORN J. 2020;111:315–325. doi: 10.1002/aorn.12885. [DOI] [PubMed] [Google Scholar]
- 22.Overcash M. A comparison of reusable and disposable perioperative textiles: sustainability state-of-the-art 2012. Anesth Analg. 2012;114:1055–1066. doi: 10.1213/ANE.0b013e31824d9cc3. [DOI] [PubMed] [Google Scholar]
- 23.Donahue L.M., Hilton S., Bell S.G., Williams B.C., Keoleian GA. A comparative carbon footprint analysis of disposable and reusable vaginal specula. Am J Obstet Gynecol. 2020;223 doi: 10.1016/j.ajog.2020.02.007. 225.e1-225.e7. [DOI] [PubMed] [Google Scholar]
- 24.McGain F., McAlister S., McGavin A., Story D. A life cycle assessment of reusable and single-use central venous catheter insertion kits. Anesth Analg. 2012;114:1073–1080. doi: 10.1213/ANE.0b013e31824e9b69. [DOI] [PubMed] [Google Scholar]
- 25.Davis N.F., McGrath S., Quinlan M., Jack G., Lawrentschuk N., Bolton DM. Carbon footprint in flexible ureteroscopy: a comparative study on the environmental impact of reusable and single-use ureteroscopes. J Endourol. 2018;32:214–217. doi: 10.1089/end.2018.0001. [DOI] [PubMed] [Google Scholar]
- 26.Kwakye G., Brat G.A., Makary MA. Green surgical practices for health care. Arch Surg. 2011;146:131–136. doi: 10.1001/archsurg.2010.343. [DOI] [PubMed] [Google Scholar]
- 27.Perry L., Malkin R. Effectiveness of medical equipment donations to improve health systems: how much medical equipment is broken in the developing world? Med Biol Eng Comput. 2011;49:719–722. doi: 10.1007/s11517-011-0786-3. [DOI] [PubMed] [Google Scholar]
- 28.Sanabria A., Kowalski L.P., Nixon I.J., et al. Considerations for environmentally sustainable head and neck surgical oncology practice. Am J Otolaryngol. 2020;41 doi: 10.1016/j.amjoto.2020.102719. [DOI] [PubMed] [Google Scholar]
- 29.Toor J., Abbas A., Ahuja C.S., Finkelstein J.A., Yee A.J., Larouche J. Optimizing the spine surgery instrument trays to immediately increase efficiency and lower costs in the operating room. Spine J. 2021;21:S177. doi: 10.1016/j.xnsj.2023.100208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thiel C.L., Eckelman M., Guido R., et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779–1786. doi: 10.1021/es504719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Campion N., Thiel C.L., DeBlois J., Woods N.C., Landis A.E., Bilec MM. Life cycle assessment perspectives on delivering an infant in the US. Sci Total Environ. 2012;425:191–198. doi: 10.1016/j.scitotenv.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rizan C., Steinbach I., Nicholson R., Lillywhite R., Reed M., Bhutta MF. The carbon footprint of surgical operations: a systematic review. Ann Surg. 2020;272:986–995. doi: 10.1097/SLA.0000000000003951. [DOI] [PubMed] [Google Scholar]
- 33.Yau Y. Analyses of heat recovery devices in the HVAC system in an operating theatre in the tropics. Build Serv Eng Res Technol. 2010;31:341–355. [Google Scholar]
- 34.Kagoma Y.K., Stall N., Rubinstein E., Naudie D. People, planet and profits: the case for greening operating rooms. CMAJ. 2012;184:1905–1911. doi: 10.1503/cmaj.112139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Venkatesh R., van Landingham S.W., Khodifad A.M., et al. Carbon footprint and cost-effectiveness of cataract surgery. Curr Opin Ophthalmol. 2016;27:82–88. doi: 10.1097/ICU.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization Regional. WHO guidance for climate-resilient and environmentally sustainable healthcare facilities. Geneva, Switzerland, 2020.
- 37.Apenteng B.A., Opoku S.T., Ansong D., Akowuah E.A., Afriyie-Gyawu E. The effect of power outages on in-facility mortality in healthcare facilities: evidence from Ghana. Glob Public Health. 2018;13:545–555. doi: 10.1080/17441692.2016.1217031. [DOI] [PubMed] [Google Scholar]
- 38.Koroglu M., Irwin B.R., Grépin KA. Effect of power outages on the use of maternal health services: evidence from Maharashtra, India. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2018-001372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arya SC. Global climate warming and performance of therapeutic agents in obstetrics and gynecology. Int J Gynaecol Obstet. 1999;65:209–210. doi: 10.1016/s0020-7292(98)00211-2. [DOI] [PubMed] [Google Scholar]
- 40.Panwar N.L., Kaushik S.C., Kothari S. Thermal modeling and experimental validation of solar tunnel dryer: a clean energy option for drying surgical cotton. Int J Low Carbon Technol. 2013;11:16–19. [Google Scholar]
- 41.Yau YH. The use of a double heat pipe heat exchanger system for reducing energy consumption of treating ventilation air in an operating theatre—a full year energy consumption model simulation. Energy Build. 2008;40:917–925. [Google Scholar]
- 42.World Health Organization Regional Office for the Western Pacific. Climate change and health in small island developing states: a WHO special initiative, Pacific island countries and areas. Manila, Philippines, 2018.
- 43.Vollmer M.K., Rhee T.S., Rigby M., et al. Modern inhalation anesthetics: potent greenhouse gases in the global atmosphere. Geophys Res Lett. 2015;42:1606–1611. [Google Scholar]
- 44.Richter H., Weixler S., Schuster M. The carbon footprint of anaesthesia: how the choice of volatile anaesthetic affects the CO2 emissions of a department of anaesthesiology. Anasthesiol Intensivmed. 2020;61:154–161. [Google Scholar]
- 45.Meyer M.J. Desflurane should des-appear: global and financial rationale. Anesth Analg. 2020;131:1317–1322. doi: 10.1213/ANE.0000000000005102. [DOI] [PubMed] [Google Scholar]
- 46.Petre M.-.A., Malherbe S. Environmentally sustainable perioperative medicine: simple strategies for anesthetic practice. Can J Anaesth. 2020;67:1044–1063. doi: 10.1007/s12630-020-01726-0. [DOI] [PubMed] [Google Scholar]
- 47.Bravo D., Gaston R.G., Melamed E. Environmentally responsible hand surgery: past, present, and future. J Hand Surg Am. 2020;45:444–448. doi: 10.1016/j.jhsa.2019.10.031. [DOI] [PubMed] [Google Scholar]
- 48.McGain F., Muret J., Lawson C., Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 2020;125:680–692. doi: 10.1016/j.bja.2020.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dohlman L.E., Kwikiriza A., Ehie O. Benefits and barriers to increasing regional anesthesia in resource-limited settings. Local Reg Anesth. 2020;13:147–158. doi: 10.2147/LRA.S236550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glenski T.A., Levine L. The implementation of low-flow anesthesia at a tertiary pediatric center: a quality improvement initiative. Pediatr Anesth. 2020;30:1139–1145. doi: 10.1111/pan.13994. [DOI] [PubMed] [Google Scholar]
- 51.Van Norman G.A., Jackson S. The anesthesiologist and global climate change: an ethical obligation to act. Curr Opin Anaesthesiol. 2020;33:577–583. doi: 10.1097/ACO.0000000000000887. [DOI] [PubMed] [Google Scholar]
- 52.Yasny J.S., White J. Environmental implications of anesthetic gases. Anesth Prog. 2012;59:154–158. doi: 10.2344/0003-3006-59.4.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ishizawa Y. Special article: general anesthetic gases and the global environment. Anesth Analg. 2011;112:213–217. doi: 10.1213/ANE.0b013e3181fe02c2. [DOI] [PubMed] [Google Scholar]
- 54.Rauchenwald V., Rollins M.D., Ryan S.M., et al. New method of destroying waste anesthetic gases using gas-phase photochemistry. Anesth Analg. 2020;131:288–297. doi: 10.1213/ANE.0000000000004119. [DOI] [PubMed] [Google Scholar]
- 55.Woods D.L., McAndrew T., Nevadunsky N., et al. Carbon footprint of robotically-assisted laparoscopy, laparoscopy and laparotomy: a comparison. Int J Med Robot. 2015;11:406–412. doi: 10.1002/rcs.1640. [DOI] [PubMed] [Google Scholar]
- 56.Power N.E., Silberstein J.L., Ghoneim T.P., Guillonneau B., Touijer KA. Environmental impact of minimally invasive surgery in the United States: an estimate of the carbon dioxide footprint. J Endourol. 2012;26:1639–1644. doi: 10.1089/end.2012.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ewbank C., Stewart B., Bruns B., et al. The development of a surgical care and climate change matrix: a tool to assist with prioritization and implementation strategies. Ann Surg. 2020:e50–e51. doi: 10.1097/SLA.0000000000003980. [DOI] [PubMed] [Google Scholar]
- 58.Bond A., Jones A., Haynes R., et al. Tackling climate change close to home: mobile breast screening as a model. J Health Serv Res Policy. 2009;14:165–167. doi: 10.1258/jhsrp.2009.008154. [DOI] [PubMed] [Google Scholar]
- 59.Paquette S., Lin JC. Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg. 2019;59:167–172. doi: 10.1016/j.avsg.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 60.Andrew N., Barraclough K.A., Long K., et al. Telehealth model of care for routine follow up of renal transplant recipients in a tertiary centre: a case study. J Telemed Telecare. 2020;26:232–238. doi: 10.1177/1357633X18807834. [DOI] [PubMed] [Google Scholar]
- 61.Brehm T.T., Berneking L., Rohde H., et al. Wound infection with vibrio harveyi following a traumatic leg amputation after a motorboat propeller injury in Mallorca, Spain: a case report and review of literature. BMC Infect Dis. 2020;20:104. doi: 10.1186/s12879-020-4789-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leng F., Lin S., Wu W., Zhang J., Song J., Zhong M. Epidemiology, pathogenetic mechanism, clinical characteristics, and treatment of vibrio vulnificus infection: a case report and literature review. Eur J Clin Microbiol Infect Dis. 2019;38:1999–2004. doi: 10.1007/s10096-019-03629-5. [DOI] [PubMed] [Google Scholar]
- 63.Sganga G., Cozza V., Spanu T., Spada P.L., Fadda G. Global climate change and wound care: case study of an off-season vibrio alginolyticus infection in a healthy man. Ostomy Wound Manag. 2009;55:60–62. [PubMed] [Google Scholar]
- 64.Huang K.-.C., Weng H.-.H., Yang T.-.Y., Chang T.-.S., Huang T.-.W., Lee M.S. Distribution of fatal vibrio vulnificus necrotizing skin and soft-tissue infections: a systematic review and meta-analysis. Medicine (Baltimore) 2016;95:e2627. doi: 10.1097/MD.0000000000002627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kehinde E.O., Anim J.T., Hira PR. Parasites of urological importance. Urol Int. 2008;81:1–13. doi: 10.1159/000137633. [DOI] [PubMed] [Google Scholar]
- 66.Lee J.S., Shin S.Y., Lee K.H., Kim S.W., Cho JS. Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur Arch Otorhinolaryngol. 2013;270:1673–1677. doi: 10.1007/s00405-012-2234-x. [DOI] [PubMed] [Google Scholar]
- 67.Bhattacharyya N. Does annual temperature influence the prevalence of otolaryngologic respiratory diseases? Laryngoscope. 2009;119:1882–1886. doi: 10.1002/lary.20613. [DOI] [PubMed] [Google Scholar]
- 68.Smith K.R., Woodward A., Campbell-Lendrum D., et al. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. 2014. Human health: impacts, adaptation, and co-benefits. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change [Field, C.B., V.R. Barros, D.J. Dokken, K.J. Mach, M.D. Mastrandrea, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada, R.C. Genova, B. Girma, E.S. Kissel, A.N. Levy, S. MacCracken, P.R. Mastrandrea, and L.L. White (eds.)]. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2014:709–754. [Google Scholar]
- 69.Hiatt R.A., Beyeler N. Cancer and climate change. Lancet Oncol. 2020;21:e519–e527. doi: 10.1016/S1470-2045(20)30448-4. [DOI] [PubMed] [Google Scholar]
- 70.Wright C.Y., du Preez D.J., Millar D.A., Norval M. The epidemiology of skin cancer and public health strategies for its prevention in Southern Africa. Int J Environ Res Public Health. 2020;17:1017. doi: 10.3390/ijerph17031017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Makin J. Implications of climate change for skin cancer prevention in Australia. Health Promot J Austr. 2011;22 doi: 10.1071/he11439. Spec No: S39-41. [DOI] [PubMed] [Google Scholar]
- 72.Diffey B. Climate change, ozone depletion and the impact on ultraviolet exposure of human skin. Phys Med Biol. 2004;49:R1–11. doi: 10.1088/0031-9155/49/1/r01. [DOI] [PubMed] [Google Scholar]
- 73.Venugopal V., Latha P.K., Shanmugam R., et al. Risk of kidney stone among workers exposed to high occupational heat stress - a case study from southern Indian steel industry. Sci Total Environ. 2020;722 doi: 10.1016/j.scitotenv.2020.137619. [DOI] [PubMed] [Google Scholar]
- 74.Johnson R.J., Sánchez-Lozada L.G., Newman L.S., et al. Climate change and the kidney. Ann Nutr Metab. 2019;74(Suppl 3):38–44. doi: 10.1159/000500344. [DOI] [PubMed] [Google Scholar]
- 75.Dallas K.B., Conti S., Liao J.C., et al. Redefining the stone belt: precipitation is associated with increased risk of urinary stone disease. J Endourol. 2017;31:1203–1210. doi: 10.1089/end.2017.0456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Paladino J.R., Korkes F., Glina S. Testicular torsion and climate changes in macroregions of São Paulo, Brazil. Einstein (Sao Paulo) 2021;19:eAO5472. doi: 10.31744/einstein_journal/2021AO5472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee H., Myung W., Kim H., Lee E.-.M., Kim H. Association between ambient temperature and injury by intentions and mechanisms: a case-crossover design with a distributed lag nonlinear model. Sci Total Environ. 2020;746 doi: 10.1016/j.scitotenv.2020.141261. [DOI] [PubMed] [Google Scholar]
- 78.Parks R.M., Bennett J.E., Tamura-Wicks H., et al. Anomalously warm temperatures are associated with increased injury deaths. Nat Med. 2020;26:65–70. doi: 10.1038/s41591-019-0721-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chersich M.F., Pham M.D., Areal A., et al. Associations between high temperatures in pregnancy and risk of preterm birth, low birth weight, and stillbirths: systematic review and meta-analysis. BMJ. 2020;371:m3811. doi: 10.1136/bmj.m3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bekkar B., Pacheco S., Basu R., DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cil G., Cameron TA. Potential climate change health risks from increases in heat waves: abnormal birth outcomes and adverse maternal health conditions. Risk Anal. 2017;37:2066–2079. doi: 10.1111/risa.12767. [DOI] [PubMed] [Google Scholar]
- 82.Shashar S., Kloog I., Erez O., et al. Temperature and preeclampsia: epidemiological evidence that perturbation in maternal heat homeostasis affects pregnancy outcome. PLoS One. 2020;15 doi: 10.1371/journal.pone.0232877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ha S., Liu D., Zhu Y., Sherman S., Mendola P. Acute associations between outdoor temperature and premature rupture of membranes. Epidemiology. 2018;29:175–182. doi: 10.1097/EDE.0000000000000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu A., Soneja S.I., Jiang C., et al. Frequency of extreme weather events and increased risk of motor vehicle collision in Maryland. Sci Total Environ. 2017;580:550–555. doi: 10.1016/j.scitotenv.2016.11.211. [DOI] [PubMed] [Google Scholar]
- 85.Chacón-Montalván E.A., Taylor B.M., Cunha M.G., Davies G., Orellana J.D.Y., Parry L. Rainfall variability and adverse birth outcomes in Amazonia. Nat Sustain. 2021;4:583–594. [Google Scholar]
- 86.Hlimi T. Association of anemia, pre-eclampsia and eclampsia with seasonality: a realist systematic review. Health Place. 2015;31:180–192. doi: 10.1016/j.healthplace.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 87.Smith J.W., Maddern GJ. Surgical implications of global warming. Med J Aust. 2011;195:324. doi: 10.5694/mja11.10649. [DOI] [PubMed] [Google Scholar]
- 88.Natuzzi E.S., Joshua C., Shortus M., et al. Defining population health vulnerability following an extreme weather event in an urban Pacific Island environment: Honiara, Solomon Islands. Am J Trop Med Hyg. 2016;95:307–314. doi: 10.4269/ajtmh.16-0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Van Minh H., Tuan Anh T., Rocklöv J., et al. Primary healthcare system capacities for responding to storm and flood-related health problems: a case study from a rural district in central Vietnam. Glob Health Action. 2014;7:23007. doi: 10.3402/gha.v7.23007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hijioka Y., Lin E., Pereira J.J., et al. Part B: Regional Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. 2014. Asia. [Barros, V.R., C.B. Field, D.J. Dokken, M.D. Mastrandrea, K.J. Mach, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada, R.C. Genova, B. Girma, E.S. Kissel, A.N. Levy, S. MacCracken, P.R. Mastrandrea, and L.L. White (eds.)]. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2014:1327–1370. [Google Scholar]
- 91.Nurse L.A., McLean R.F., Agard J., et al. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part B: Regional Aspects. 2014. Small island. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change [Barros, V.R., C.B. Field, D.J. Dokken, M.D. Mastrandrea, K.J. Mach, T.E. Bilir, M. Chatterjee, K.L. Ebi, Y.O. Estrada, R.C. Genova, B. Girma, E.S. Kissel, A.N. Levy, S. MacCracken, P.R. Mastrandrea, and L.L. White (eds.)]. Cambridge, United Kingdom and New York, NY, USA: Cambridge University Press; 2014:1613–1654. [Google Scholar]
- 92.Amat Camacho N., Karki K., Subedi S., von Schreeb J. International emergency medical teams in the aftermath of the 2015 Nepal earthquake. Prehosp Disaster Med. 2019;34:260–264. doi: 10.1017/S1049023X19004291. [DOI] [PubMed] [Google Scholar]
- 93.von Schreeb J., Riddez L., Samnegård H., Rosling H. Foreign field hospitals in the recent sudden-onset disasters in Iran, Haiti, Indonesia, and Pakistan. Prehosp Disaster Med. 2008;23:144–151. doi: 10.1017/s1049023x00005768. discussion 152-153. [DOI] [PubMed] [Google Scholar]
- 94.Pyda J., Patterson R.H., Caddell L., et al. Towards resilient health systems: opportunities to align surgical and disaster planning. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2019-001493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Nickerson J.W., Chackungal S., Knowlton L., McQueen K., Burkle FM. Surgical care during humanitarian crises: a systematic review of published surgical caseload data from foreign medical teams. Prehosp Disaster Med. 2012;27:184–189. doi: 10.1017/S1049023X12000556. [DOI] [PubMed] [Google Scholar]
- 96.Read D.J., Holian A., Moller C.-.C., Poutawera V. Surgical workload of a foreign medical team after Typhoon Haiyan. ANZ J Surg. 2016;86:361–365. doi: 10.1111/ans.13175. [DOI] [PubMed] [Google Scholar]
- 97.Khan T., Quintana L., Aguilera S., et al. Global health, global surgery and mass casualties. I. Rationale for integrated mass casualty centres. BMJ Glob Health. 2019;4 doi: 10.1136/bmjgh-2019-001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bouchard M.E., Sheneman N., Hey M.T., Hoemeke L., Abdullah F. Investments in surgical systems contribute to pandemic readiness and health system resilience. J Public Health Pol. 2021;42:493–500. doi: 10.1057/s41271-021-00292-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McIver L., Kim R., Woodward A., et al. Health impacts of climate change in Pacific Island countries: a regional assessment of vulnerabilities and adaptation priorities. Environ Health Perspect. 2016;124:1707–1714. doi: 10.1289/ehp.1509756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Cauchi J.P., Correa-Velez I., Bambrick H. Climate change, food security and health in Kiribati: a narrative review of the literature. Glob Health Action. 2019;12 doi: 10.1080/16549716.2019.1603683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.White S.M., Shelton CL. Abandoning inhalational anaesthesia. Anaesthesia. 2020;75:451–454. doi: 10.1111/anae.14853. [DOI] [PubMed] [Google Scholar]
- 102.Ryan S., Sherman J. Sustainable anesthesia. Anesth Analg. 2012;114:921–923. doi: 10.1213/ANE.0b013e31824fcea6. [DOI] [PubMed] [Google Scholar]
- 103.Guetter C.R., Williams B.J., Slama E., et al. Greening the operating room. Am J Surg. 2018;216:683–688. doi: 10.1016/j.amjsurg.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 104.Southorn T., Norrish A., Gardner K., Baxandall R. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J Perioper Pract. 2013;23:144–146. doi: 10.1177/175045891302300605. [DOI] [PubMed] [Google Scholar]
- 105.Zuegge K.L., Bunsen S.K., Volz L.M., et al. Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg. 2019;128:e97–e99. doi: 10.1213/ANE.0000000000003771. [DOI] [PubMed] [Google Scholar]
- 106.Shelton C.L., McBain S.C., Mortimer F., White SM. A new role for anaesthetists in environmentally-sustainable healthcare. Anaesthesia. 2019;74:1091–1094. doi: 10.1111/anae.14647. [DOI] [PubMed] [Google Scholar]
- 107.Woodward A. Climate change and the surgeon: what is the problem? Why is it so hard? What can be done? ANZ J Surg. 2019;89:1358–1363. doi: 10.1111/ans.15562. [DOI] [PubMed] [Google Scholar]
- 108.Özelsel T.J.-.P., Sondekoppam R.V., Buro K. The future is now—it's time to rethink the application of the Global Warming Potential to anesthesia. Can J Anesth/J Can Anesth. 2019;66:1291–1295. doi: 10.1007/s12630-019-01385-w. [DOI] [PubMed] [Google Scholar]
- 109.Sherman J.D., McGain F., Lem M., Mortimer F., Jonas W.B., MacNeill AJ. Net zero healthcare: a call for clinician action. BMJ. 2021;374:n1323. doi: 10.1136/bmj.n1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Watts N., Amann M., Arnell N., et al. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PubMed] [Google Scholar]
- 111.Gough H., Faulknall-Mills S., King M.-.F., Luo Z. Assessment of overheating risk in gynaecology scanning rooms during near-heatwave conditions: a case study of the royal berkshire hospital in the UK. Int J Environ Res Public Health. 2019;16:3347. doi: 10.3390/ijerph16183347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Palejwala Z., Wallman K., Ward M.K., et al. Effects of a hot ambient operating theatre on manual dexterity, psychological and physiological parameters in staff during a simulated burn surgery. PLoS One. 2019;14 doi: 10.1371/journal.pone.0222923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hakim M., Walia H., Dellinger H.L., et al. The effect of operating room temperature on the performance of clinical and cognitive tasks. Pediatr Qual Saf. 2018;3:e069. doi: 10.1097/pq9.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kaplan G.G., Dixon E., Panaccione R., et al. Effect of ambient air pollution on the incidence of appendicitis. CMAJ. 2009;181:591–597. doi: 10.1503/cmaj.082068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Greenough G., McGeehin M., Bernard S.M., Trtanj J., Riad J., Engelberg D. The potential impacts of climate variability and change on health impacts of extreme weather events in the United States. Environ Health Perspect. 2001;109:191–198. doi: 10.1289/ehp.109-1240666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Thiel C.L., Schehlein E., Ravilla T., et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43:1391–1398. doi: 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dorrian C., Ferguson J., Ah-See K., et al. Head and neck cancer assessment by flexible endoscopy and telemedicine. J Telemed Telecare. 2009;15:118–121. doi: 10.1258/jtt.2009.003004. [DOI] [PubMed] [Google Scholar]
- 118.Rumsey M., Fletcher S.M., Thiessen J., et al. A qualitative examination of the health workforce needs during climate change disaster response in Pacific Island countries. Hum Resour Health. 2014;12:9. doi: 10.1186/1478-4491-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yates E.F., Bowder A.N., Roa L., et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann Surg. 2021;273:1108–1114. doi: 10.1097/SLA.0000000000004755. [DOI] [PubMed] [Google Scholar]
- 120.Somner J.E.A., Connor A., Benjamin L. Eyes, economics and the environment: should green issues drive changes in ophthalmic care?–yes. Eye (Lond) 2010;24:1309–1311. doi: 10.1038/eye.2010.64. [DOI] [PubMed] [Google Scholar]
- 121.Roa L., Velin L., Tudravu J., McClain C.D., Bernstein A., Meara JG. Climate change: challenges and opportunities to scale up surgical, obstetric, and anaesthesia care globally. Lancet Planet Health. 2020;4:e538–e543. doi: 10.1016/S2542-5196(20)30247-3. [DOI] [PubMed] [Google Scholar]
- 122.Ubaldi K. Reprocessing single-use devices in the ambulatory surgery environment. AORN J. 2019;109:452–462. doi: 10.1002/aorn.12639. [DOI] [PubMed] [Google Scholar]
- 123.COP23 Presidency Secretariat. Talanoa dialogue: from ambition to action. 2017 https://cop23.com.fj/wp-content/uploads/2019/03/Talanoa-Dialogue_Report_F_February-19-20193.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.