ABSTRACT
Although Wnt signaling is clearly important for the intestinal epithelial homeostasis, the relevance of various sources of Wnt ligands themselves remains incompletely understood. Blocking the release of Wnt in distinct stromal cell types suggests obligatory functions of several stromal cell sources and yields different observations. The physiological contribution of epithelial Wnt to tissue homeostasis remains unclear. We show here that blocking epithelial Wnts affects colonic Reg4+ epithelial cell differentiation and impairs colonic epithelial regeneration after injury in mice. Single-cell RNA analysis of intestinal stroma showed that the majority of Wnt-producing cells were contained in transgelin (Tagln+) and smooth muscle actin α2 (Acta2+) expressing populations. We genetically attenuated Wnt production from these stromal cells using Tagln-Cre and Acta2-CreER drivers, and found that blockage of Wnt release from either epithelium or Tagln+ and Acta2+ stromal cells impaired colonic epithelial healing after chemical-induced injury. Aggregated blockage of Wnt release from both epithelium and Tagln+ or Acta2+ stromal cells drastically diminished epithelial repair, increasing morbidity and mortality. These results from two uncharacterized stromal populations suggested that colonic recovery from colitis-like injury depends on multiple Wnt-producing sources.
KEY WORDS: Wntless, Wnt, Tagln, Acta2, Gpr177, Colitis, Wound healing, Intestinal stem cell
Summary: Aggregated blockage of Wnt release from both epithelium and Tagln+ or Acta2+ stromal cells drastically diminished epithelial regeneration suggesting that colonic recovery from colitis-like injury depends on multiple Wnt-producing sources.
INTRODUCTION
Wingless-type MMTV integration site family members (Wnts) are secreted glycolipoproteins engaging in short-range signaling (Willert et al., 2003; Willert and Nusse, 2012). Newly synthesized Wnt proteins are lipidated in endoplasmic reticulum by an acyltransferase, Porcupine (Porcn) (Takada et al., 2006), then transported by Wntless (Wls, or Gpr177 in mice) transmembrane protein for secretion (Bänziger et al., 2006; Bartscherer et al., 2006). Binding of extracellular Wnts to their Frizzled receptors in ligand-receiving cells initiate a signal cascade (Schulte, 2010; Schulte and Bryja, 2007; Wu and Nusse, 2002), inactivating the glycogen synthase kinase 3 (GSK3)-containing cytoplasmic destruction machinery and stabilizing β-Catenin (Cadigan and Peifer, 2009; Huang and He, 2008; MacDonald et al., 2009). Binding of β-Catenin to Tcf factors in nucleus drives a gene program related to cellular growth and proliferation (He et al., 2004; MacDonald and He, 2012; Tamai et al., 2000; Wehrli et al., 2000). Abnormal activation of canonical Wnt pathway in most human colon cancers highlights its profound influence on cellular behavior (Angers and Moon, 2009; Clevers and Nusse, 2012; de Lau et al., 2007; MacDonald et al., 2009; Nusse et al., 2008; Polakis, 2007; Reya and Clevers, 2005). Noncanonical Wnt molecules also activate pathways such as Rho family small GTPases to control cellular migration (Boutros and Mlodzik, 1999; Eaton et al., 1996; Fanto et al., 2000; Habas et al., 2003, 2001; Sakamori et al., 2014; Strutt et al., 1997; Wallingford and Habas, 2005).
The development and maintenance of intestinal epithelium depend on intact Wnt signaling. Removing β-catenin or Tcf4 from mouse intestinal epithelia impaired crypt formation causing lethality (Fevr et al., 2007; Korinek et al., 1998; van de Wetering et al., 2002; van Es et al., 2012). Systemic overexpression of a Wnt antagonist dickkopf homolog 1 induced severe damages to adult intestines (Kuhnert et al., 2004; Pinto et al., 2003). Although Wnt signaling is clearly important, the importance of Wnts themselves is not as clear. Paneth cells were first shown as the primary source of Wnts in small intestine (Gregorieff et al., 2005); ex vivo cultured Lgr5+ intestinal stem cells (ISCs) (Barker et al., 2007), when associated with Paneth cells, showed enhanced enteroid-forming capability (Sato et al., 2011). Enteroids lacking Wnt3 could not be properly passaged (Farin et al., 2012), while enteroids lacking Wls or Porcn failed to grow ex vivo (Kabiri et al., 2014; Valenta et al., 2016). The growth of above epithelial Wnt deficient enteroids could nevertheless be rescued via supplementing stromal cells or stromal Wnt proteins to the culture (Kabiri et al., 2014; Valenta et al., 2016; Farin et al., 2012). These observations, combined with the overall lack of in vivo phenotype in the absence of epithelial Wnt3 (Farin et al., 2012), Vps35 (de Groot et al., 2013), Porcn (Kabiri et al., 2014; San Roman et al., 2014) or Wls (Valenta et al., 2016), collectively suggested that although epithelial Wnts were required to support ISCs ex vivo, their physiological relevance remained unclear in the presence of a potentially redundant stromal source of Wnt. The question regarding the importance of Wnts themselves was further highlighted by the observation that R-spondin was more powerful than Wnts in activating Wnt signaling (Yan et al., 2017).
Existing literature suggested a complexity and functional divergence of various stromal sources of Wnt. The stroma of the intestinal lamina propria consist myofibroblasts, fibroblasts, vascular and visceral smooth muscles, as well as innate and professional immune cells (Powell et al., 2011). Some of these cell lineages express Wnt2b, Wnt4 and Wnt5a (Farin et al., 2012; Gregorieff et al., 2005; Miyoshi et al., 2012). Myh11-CreER-mediated ablation of Porcn in intestinal myofibroblasts alone or in combination with epithelial Porcn deletion did not perturb intestinal epithelial homeostasis (San Roman et al., 2014), marking myofibroblasts a non-essential stromal Wnt source. However, deleting Porcn from myofibroblasts expressing Pdgf receptor α (Pdgfrα) blocked intestinal crypt formation (Greicius et al., 2018). Foxl1-expressing cells were subsequently identified as Pdgfrα+ telocytes that immediately juxtaposed epithelium, produced Wnts, R-spondin 3 and gremlin proteins, but lacked myofibroblast markers. Genetic ablation of Foxl1+ cells or inhibition of Wnt production by Foxl1-expressing cells, disrupted ISC homeostasis in both small intestine and colon (Aoki et al., 2016; Shoshkes-Carmel et al., 2018). McCarthy and co-workers recently identified a gremlin 1-producing CD81+ Pdgfrαlow population, referred to as trophocytes, present immediately below crypts and contributing to ISC maintenance in vivo (McCarthy et al., 2020). In the colon, CD34+; α-smooth muscle actin-negative pericryptal stromal cells expressing Wnt2b, R-spondin 1 and gremlin 1, were shown to support Lgr5+ ISCs ex vivo (Stzepourginski et al., 2016). Preventing Wnt secretion from a heterogenous Gli1+ stromal population disrupted colonic crypt homeostasis (Degirmenci et al., 2018). In small intestines, however, these Wnt2b-enriched Gli1+ cells were proposed to be a reserve Wnt source for epithelial Wnt deprivation. In addition to above homeostasis conditions, Wnt5a+ mesenchymal cells were also shown to promote colonic crypt regeneration after biopsy injury (Miyoshi et al., 2012), whereas Wnt deprivation from intestinal mononuclear phagocytes exacerbated irradiation-induced mucosal damage (Saha et al., 2016).
The above studies, on the one hand, illustrated the ISC-supporting roles of Wnt-producing epithelial and stromal cell types, but, on the other hand, led to perplexing questions. First, if Wnts from specific stromal cell type are obligatory for ISC homeostasis in vivo, then what is the physiological purpose of making epithelial Wnts, especially those from Paneth cells have the prime access to ISCs in the small intestine? Second, transcriptomes of Gli1+ or Pdgfrα+ cells appeared to intersect those of myofibroblasts, yet different Cre drivers yielded distinct, sometimes opposite, outcomes regarding whether, when and where an intestinal phenotype was observed (Degirmenci et al., 2018; San Roman et al., 2014; Greicius et al., 2018; Shoshkes-Carmel et al., 2018). It is also plausible that: (1) instead of the existence of a specific obligatory Wnt-supplying cell type, the quantity of Wnt molecules collected from various adjacent sources in the niche might be crucial for intestinal homeostasis; and (2) epithelial Wnt production may be essential during mucosal injury that disrupts epithelial-mesenchymal interactions. Based on these hypotheses, we describe the under-appreciated role of epithelial Wnts in homeostasis and during various injuries. A single-cell (sc) RNA survey of intestinal stroma revealed that mesenchymal Wnt producers were constrained to cell clusters expressing transgelin (Tagln, also known as SM22α) (Dong et al., 2012) or Acta2. By using Tagln-Cre and Acta2-CreER drivers to abrogate Wnt productions in these stromal subsets, we demonstrate that the abundance of Wnts collected from multiple tissue sources at the regenerating niche may be crucial for colonic healing after injury.
RESULTS
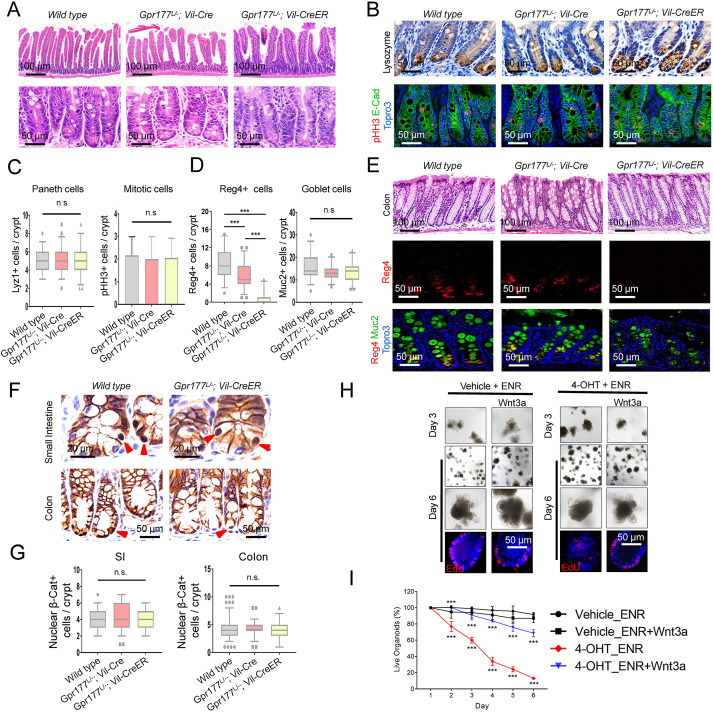
Blocking epithelial Wnts impaired colonic Reg4 cell differentiation
Global or tissue-specific ablation of Wls (Gpr177 in mouse) in various animals caused phenotypes resembling loss of Wnt signaling (Bnziger et al., 2006; Bartscherer et al., 2006; Fu et al., 2009) due to its indispensable function for Wnt secretion (Ching and Nusse, 2006; Das et al., 2012; Port and Basler, 2010). Using constitutive (Villin-Cre) or inducible (Villin-CreER) intestinal epithelial cell (IEC) drivers, we performed Gpr177 ablation to abrogate epithelial Wnt production. Mice lacking IEC-specific Gpr177 did not show histological abnormality in small intestines (Fig. 1A) or alterations in Paneth or mitotic cell numbers in the crypts (Fig. 1B,C, quantified from three mice for each genotype). The deletion of Gpr177 specifically in IECs was further assessed by immunogold labeling of endogenous Gpr177 in wild-type and Gpr177L/−;Vil-Cre intestines. Gpr177+ gold particles were diminished by 90% in endoplasmic reticulum (ER), 91% in non-ER cytoplasmic region and 93% in plasma membrane of Gpr177-deficient Paneth cells (Fig. S1A,B, quantified in Fig. S1C). No obvious change was detected in stromal cells of the same tissues (Fig. S1A,B).
Fig. 1.
Inhibition of epithelial Wnts impaired colonic Reg4+ cell differentiation. (A) Histology of Gpr177L/−;Vil-Cre and Gpr177L/−;Vil-CreER mouse small intestines was the same as wild-type controls. (B) Immunohistochemistry for lysozyme and pHH3 showed normal Paneth and mitotic cells. (C) The numbers of Paneth or mitotic cells per crypt were not changed (n=3 mice per genotype). (D) The numbers of Reg4+ deep crypt secretory (DCS) colonic cells, but not goblet cells, were significantly decreased in Gpr177L/−;Vil-Cre and Gpr177L/−;Vil-CreER mouse colons (n=3 mice per genotype). (E) Histology and Reg4/Muc2 staining showed reduced Reg4+ cells in Gpr177L/−;Vil-Cre and Gpr177L/−;Vil-CreER mouse colons. (F) Immunohistochemistry for β-catenin showed unchanged nuclear β-catenin-positive cells in Gpr177L/−;Vil-Cre and Gpr177L/−;Vil-CreER mouse small intestinal or colonic crypts. (G) The numbers of nuclear β-catenin-positive cells per crypt were not changed (n=3 mice per genotype). (H) Gpr177L/−;Vil-CreER mouse enteroids cultured in ENR medium were treated with 4-OHT to delete Gpr177. Bright-field and fluorescent EdU images represented day 3 and 6 after 4-OHT or vehicle treatment, in the presence of exogenous Wnt3a. Wnt3a notably enhanced survival at day 6 when compared with vehicle group. Data are representative of three independent experiments. (I) Numbers of viable enteroids were counted daily following 4-OHT treatment. Wnt3a notably enhanced the survival of 4-OHT-treated enteroids when compared with no Wnt groups. Statistical significance provided for 4-OHT_ENR+Wnt3a versus 4-OHT_ENR and 4-OHT_ENR versus Vehicle_ENR. ***P<0.001. Data are mean±s.e.m. from at least three independent experiments. Also see Fig. S1.
Despite the lack of histological abnormality, Gpr177-deficient colonic epithelium had a significant reduction of Reg4+ cells, previously reported as deep crypt secretory (DCS) cells, in both Vil-Cre- and Vil-CreER-driven homozygotes (Fig. 1D,E). This change has not been previously reported and was specific to Reg4+ cells. No change was found in the number of Muc2+ goblet cells in the same tissues (Fig. 1D,E, Fig. S1D). The number of nuclear β-catenin+ cells in both small intestine and colonic epithelia were equivalent between wild-type and Gpr177-deficient epithelium (Fig. 1F,G, Fig. S1E). Quantitative RT-PCR supported the immunohistochemistry finding that there was no transcriptional alteration in canonical Wnt targets or in Paneth cell genes (Fig. S1F).
Gpr177L/L;Vil-Cre mouse crypts failed to develop into enteroids in regular ENR medium ex vivo (Fig. S1G). The enteroid growth could be partially restored if recombinant Wnt3a or CHIR (the GSK3 inhibitor) was supplemented at seeding (Fig. S1G). We then cultured enteroids from non-induced adult Gpr177L/−;Villin-CreER mice in ENR medium for 4 days, followed by 4-OHT administration for 12 h to induce Gpr177 deletion. Addition of 4-OHT, but not vehicle, caused growth arrest of nearly 90% Gpr177L/−;Vil-CreER enteroids 5 days after 4-OHT treatment (Fig. 1H,I). Recombinant Wnt3a proteins, when added into ENR medium upon 4-OHT withdrawal, significantly improved the survival and growth of Gpr177L/−;Vil-CreER enteroids, judged by enteroid budding morphologies and by EdU incorporation (Fig. 1H,I). These results documented a previously undescribed inhibition of Reg4 cell differentiation in colon upon epithelial Wnt inhibition.
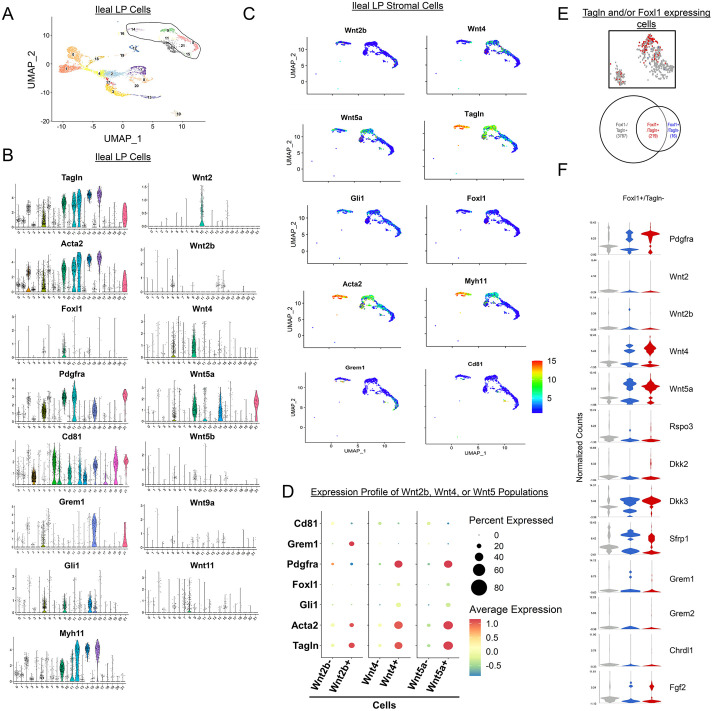
Tagln+ stromal domain encompasses subepithelial Wnt producers
Previous studies investigating sources of stromal Wnts using Myh11, Gli1, Pdgfrα, Cd81 or Foxl1 as markers suggested partial overlap among these cell populations, but the extent was not examined in detail. To gain a systematic understanding of the overall distribution of Wnt producers within intestinal stroma, we conducted a single-cell RNA sequencing (scRNA-seq) analysis of mouse total ileal stromal tissue. Uniform manifold approximation and projection (UMAP) analyses revealed 22 cell clusters encompassing major lamina propria cell types (Fig. 2A). By examining all mouse Wnt genes, we were able to map six major Wnt-expressing cell clusters (Fig. 2A). Cluster 9 was identified as the largest Wnt4- and Wnt5a-expressing cluster co-expressing Foxl1, Pdgfra and Gli1 (Fig. 2B). This cluster also robustly expressed Tagln, Acta2 and Myh11, genes that are expressed by fibroblast, myofibroblast and smooth muscle cells. Other Wnt4- and Wnt5a-expressing clusters are 5, 11, 14 and 21, where a small number of Foxl1+ cells were found. Clusters 5, 11 and 21 co-expressed high levels of Pdgfra while cluster 14 did not. Gli was highly expressed in 5 and 14, but not as highly in clusters 11 and 21. However, all these clusters were marked by Tagln and Acta2 (Fig. 2B). In contrast to the Wnt4- and Wnt5a- expressing clusters, cluster 15 was defined by Wnt2b-expressing Pdgfralow trophocytes, as observed by the presence of Cd81 and Grem1 (McCarthy et al., 2020), and the absence of Foxl1. In addition, this cluster expressed lower abundance of Tagln, Acta2 and Myh11 (Fig. 2B). Examination of Tagln-expressing Wnt-producing clusters 5, 9, 11, 14 and 21, in light of Pdgfra, Gli1 and Foxl1 suggested that they were substantially overlapped by Tagln-, Acta2- and Myh11-expressing cell populations (Fig. 2C).
Fig. 2.
The Tagln+ stromal domain encompassed the majority of subepithelial Wnt producers. (A) Uniform manifold approximation and projection (UMAP) of 8767 mouse ileal stromal cells resulted in 22 distinct clusters. Wnt-expressing clusters are circled on the UMAP plot. (B) Violin plots showed the stromal domains expressing Wnt ligands and key stromal cell markers (Foxl1, Gli1, Pdgfrα, Cd81 and Grem1) across the 22 clusters. Tagln and Acta2 were highly expressed in the major Wnt2b-, Wnt4- and Wnt5a-expressing clusters. (C) UMAP plots for clusters 5, 9, 11, 14 and 21 showed a containment of these Wnt-producing cells by Tagln and Acta2. (D) Differential expression of Tagln, Acta2, Foxl1, Gli1, Pdgfrα, Grem1 and Cd81 in Wnt2b− and Wnt2b+ cells, Wnt4− and Wnt4+ cells, and Wnt5a− and Wnt5a+ cells. (E) t-SNE plot and Venn diagram highlighted Tagln+/Foxl1−, Tagln+/Foxl1+ and Tagln−/Foxl1+ populations with exact numbers of cells in each population. Sixteen out of 235 Foxl1+ cells did not express Tagln. (F) Violin plots showed a similar transcriptomic expression between Tagln+/Foxl1+ and Tagln−/Foxl1+ populations, for Wnt, R-Spondin, DKK, Fgf, Sfrp1 and Grem molecules. Also see Fig. S2.
Compared with the population that do not express Wnt2b, Wnt4 or Wnt5a, cells expressing a high abundance of these ligands also expressed abundant Tagln and Acta2 compared with Gli1 and Foxl1 (Fig. 2D). We then used a single-cell deep constrained clustering (scDCC) approach, a newly developed deep learning model that guides the clustering by giving weight to marker genes (here, we used Wnt5a and Wnt4, respectively). These Wnt-based clusterings demonstrated a high abundance of Tagln, Acta2, Pdgfra, Myh11, Gli1 and Foxl1, and a low abundance of Cd81 in Wnt5a-expressing and Wnt4-expressing stromal clusters (circled) (Fig. S2A,B).
Compared with the heterogeneous nature of Gli1+ cells (Degirmenci et al., 2018), Foxl1+ telocytes represented a specific cell population shown to support ISC homeostasis (Shoshkes-Carmel et al., 2018). The majority of Foxl1-expressing cells also expressed Tagln (Fig. 2E), and Tagln was not detected in 16 Foxl1+ cells. Examining the transcriptome of Foxl1+/Tagln− and Foxl1+/Tagln+ cells revealed their high expression of Wnt4, Wnt5a, Pdgfra and Gli1 (Fig. 2F). Gene-specific analysis (GSA) identified only six genes differentially expressed between Foxl1+/Tagln− and Foxl1+/Tagln+ populations, while 614 genes were differentially expressed between Foxl1−/Tagln+ and Foxl1+/Tagln+ populations (Fig. S2C-G), suggesting that Foxl1 defines a strict subset of Tagln+ cell population. Overall, these analyses revealed that Tagln+ domains encompassed the major stromal Wnt producers, and there was a high degree of overlap among reported stromal cell lineages, except for Pdgfralow trophocytes (McCarthy et al., 2020).
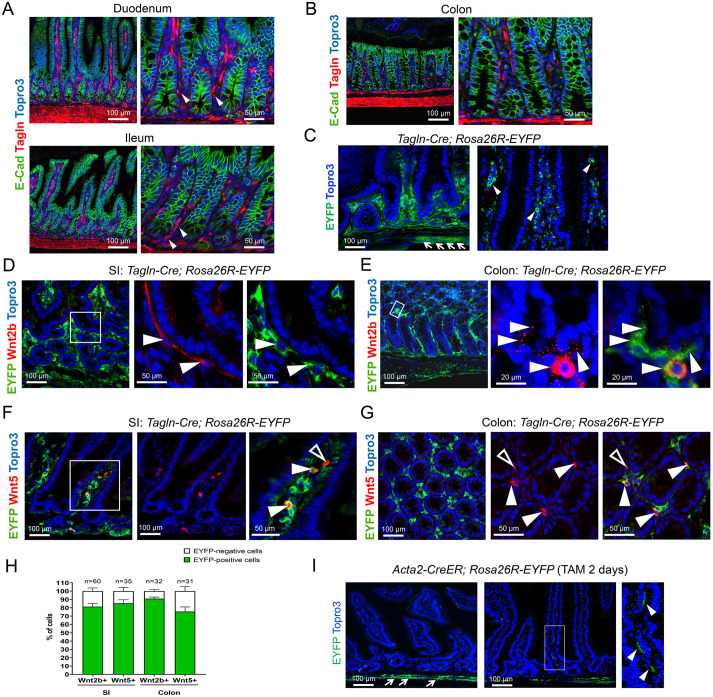
Tagln-Cre and Acta2-CreER targeted intestinal stromal domains
Examination of endogenous Tagln expression revealed a mesenchymal domain throughout the intestinal tract (Fig. 3A), consistent with its reported expression in fibroblasts, myofibroblasts and smooth muscles (Katajisto et al., 2008; Kuhbandner et al., 2000; Dong et al., 2012). In duodenum and ileum, we found that subset of Tagln-expressing cells was in immediate proximity of crypt cells, wrapping the epithelial glands and extending into villus mesenchymal region (Fig. 3A). A similar pattern was found in colon (Fig. 3B).
Fig. 3.
Tagln-Cre and Acta2-CreER targeted anatomically different stromal compartments. (A,B) Immunostaining for Tagln (SM22) showed a broad Tagln-expressing stromal domain in small intestine and colon. Some Tagln+ cells were in immediate proximity to crypts (arrowheads). (C) Tagln-Cre;Rosa26R-EYFP mice showed Cre-mediated recombination in stromal domain in a similar pattern to endogenous Tagln+ cells. Arrows and arrowheads indicate Tagln-Cre-expressing cells underneath the crypt and villus epithelium, respectively. (D-G) Co-staining of Wnt2b or Wnt5 with EYFP in Tagln-Cre;Rosa26R-EYFP mouse small intestine and colon showed Cre-activated reporter expression in Wnt2b+ and Wnt5+ cells (white arrowheads). Cells that did not show EYFP are indicated by open arrowheads. (H) The vast majority of Wnt2b+ and Wnt5+ cells were labeled by Tagln-Cre. (I) Acta2-CreER;Rosa26R-EYFP mice showed a different Cre reporter domain towards the outer smooth muscle layers of the intestine. Arrows and arrowheads indicate Acta2-expressing cells underneath the crypt and villus epithelium, respectively. Data are mean±s.e.m. from at least three independent experiments. Also see Fig. S3.
We crossed Tagln-Cre mouse (Boucher et al., 2003; Holtwick et al., 2002) to Rosa26R reporter mice (Srinivas et al., 2001), and found that Tagln-Cre activated reporter expression in a pattern similar to endogenous Tagln (Fig. 3C, compare with A). We next stained for endogenous Wnt proteins in Tagln-Cre;Rosa26REYFP mouse intestinal tissues. In both small intestine and colon, a subset of Tagln-Cre expressing cells (EYFP+) co-expressed Wnt2b (white arrows, Fig. 3D,E). Some Wnt2b-expressing Tagln+ cells showed a large cell body with long processes and were located underneath the epithelium (Fig. 3D), resembling what was described for telocytes. Close examination revealed Wnt2b+ vesicular puncta in the vicinity of cells with strong cytoplasmic Wnt2b staining (arrowheads in Fig. 3E, Fig. S3A). A subset of Tagln-Cre-expressing cells expressed endogenous Wnt5 (Fig. 3F,G), and tended to show a different localization and cell shapes. Close examination revealed both perinuclear and vesicular localization of Wnt5 (Fig. S3B). Examination of GFP positivity for Wnt2b+ or Wnt5+ cells suggested that the majority of them were labeled by Tagln-Cre (Fig. 3H), consistent with scRNA-seq results (Fig. 2C,D).
In addition to Tagln-Cre, we also examined the Acta2-CreER driver (a knock-in allele referred to as Acta2-CreER hereafter) (Manieri et al., 2015) and observed a slightly narrow Cre-expressing stromal domain, with scattered EYFP+ cells detected in the lamina propria of villi in Acta2-CreER;Rosa26REYFP mice (Fig. 3I). The relatively constrained Acta2-CreER activity reflected a potential mosaic recombination by this tamoxifen-inducible line, as opposed to the constitutive expression of Tagln-Cre. We then used these two stromal drivers to assess the contribution of Wnts produced by Tagln+ and Acta2+ cells to intestinal homeostasis, which have not been studied before.
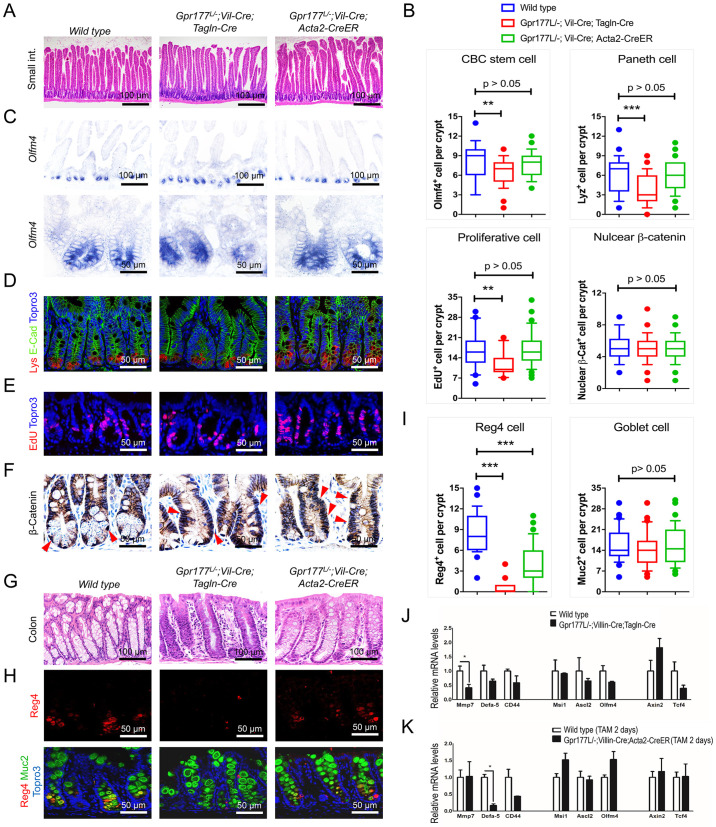
Preventing Wnt production in epithelium and in Tagln+ or Acta2+ cells diminished colonic Reg4 cells
We crossed Gpr177 flox mice to Tagln-Cre or Acta2-CreER mice. Gpr177L/L; Tagln-Cre mice did not display global intestinal defects. Similarly, tamoxifen-treated Gpr177L/L; Acta2-CreER mice did not exhibit any defects, observations reminiscent of a previous report using Myh11-Cre to delete Porcn in myofibroblasts (San Roman et al., 2014). We then developed Gpr177L/−;Vil-Cre;Tagln-Cre as well as Gpr177L/−;Vil-Cre;Acta2-CreER mice to remove Gpr177 from both epithelium and Tagln+ or Acta2+ stromal cells. In situ hybridization for Gpr177 showed effective gene ablation in both epithelial and stromal compartments (Fig. S4A,B).
Gpr177L/−;Vil-Cre;Tagln-Cre mouse intestines appeared histologically normal (Fig. 4A) but with reduced crypt base columnar cells (CBCs) marked by Olfm4 by in situ (Fig. 4C, quantified in 4B), Paneth cells (Fig. 4D, quantified in 4B) and proliferative cells marked by 30 min EdU labeling (Fig. 4E, quantified in 4B) or by PCNA staining (Fig. S4C). No change was detected for nuclear β-catenin+ cells (Fig. 4F, quantified in 4B). Examination of Gpr177L/−;Vil-Cre;Tagln-Cre mouse colons showed a notable alteration of glandular morphology (Fig. 4G), accompanied by a diminished number of Reg4+ cells (Fig. 4H, quantified in 4I). Goblet cells remained unchanged in the same tissue (Fig. 4H, quantified in 4I, also see Fig. S4D).
Fig. 4.
Wnt deprivation from epithelium and Tagln+ or Acta2+ cells diminished Reg4 cell differentiation in colon. (A) Histology analysis did not show differences in Gpr177L/−;Vil-Cre;Tagln-Cre and Gpr177L/−;Vil-Cre;Acta2-CreER mouse small intestines. (B-F) Gpr177L/−;Vil-Cre;Tagln-Cre intestines had reduced Olfm4+ (C), Lyz1+ (D) and EdU+ (E) cell numbers but unchanged numbers of nuclear β-catenin+ cells (F) (red arrowheads). Gpr177L/−;Vil-Cre;Acta2-CreER mice showed no detectable difference in the above analysis. n=3 mice per genotype. Fifty crypts of the small intestine were counted per marker per genotype. (G-I) Histology (G) and immunostaining for Reg4 and Muc2 (H) showed diminished and significantly reduced DCS cells (H) in Gpr177L/−;Vil-Cre;Tagln-Cre and Gpr177L/−;Vil-Cre;Acta2-CreER mouse colons, respectively. Goblet cells were not changed. n=3 mice per genotype. (J,K) Quantitative RT-PCR detected a reduction in Mmp7 in Gpr177L/−;Vil-Cre;Tagln-Cre intestines and a reduction in Defa5 in Gpr177L/−;Vil-Cre;Acta2-CreER intestines. n=3 mice per genotype. Data are mean±s.e.m. from at least three independent experiments. *P<0.05. Also see Fig. S4.
A similar reduction of colonic Reg4+ cells was observed in Gpr177L/−;Vil-Cre;Acta2-CreER mice (Fig. 4H), but to a less extent compared with Gpr177L/−;Vil-Cre;Tagln-Cre mice (Fig. 4I). However, Gpr177L/−;Vil-Cre;Acta2-CreER mice did not show other changes in CBCs, Paneth cells or proliferative cells (Fig. 4A-F). Quantitative RT-PCR analysis showed a significant reduction in Gpr177 transcripts in Gpr177L/−;Vil-Cre;Acta2-CreER intestine (Fig. S4E), suggesting the lack of phenotypic difference was not due to an inefficient deletion.
Quantitative RT-PCR analysis detected a significantly reduced Mmp7 in Gpr177L/−;Vil-Cre;Tagln-Cre intestines (Fig. 4J), and reduced Defa5 in Gpr177L/−;Vil-Cre;Acta2-CreER intestines (Fig. 4K). Mmp7 and Defa5 represented signature markers of mature Paneth cells. These results suggested an additive impact of Wnts from epithelium and Tagln+ or Acta2+ stromal cells on Reg4+ cell differentiation.
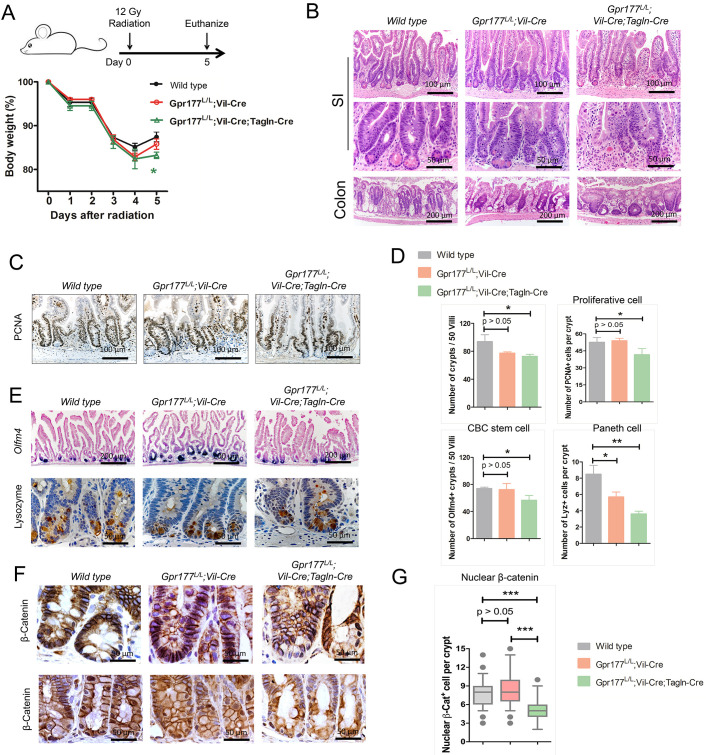
Blocking Wnts released from the epithelium and from Tagln+ cells modestly affected regeneration following irradiation
Whole-body irradiation rapidly eliminates proliferating intestinal stem cells (ISCs) (Potten, 1977) and elicits epithelial regeneration (Yu et al., 2018; Zhang et al., 2020). We asked whether Wnts produced in epithelium and Tagln stromal cells participated in irradiation-induced regeneration. Adult control, Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice (all littermates) received 12 Gy whole-body irradiation (n=6 for each genotype, from at least three different litters). All mice showed a similar trend of body weight loss starting from day 3 (Fig. 5A). On day 5, wild-type and Gpr177L/L; Vil-Cre mice showed a weight gain whereas Gpr177L/L;Vil-Cre;Tagln-Cre mice displayed the smallest weight gain (P<0.05, Fig. 5A). Upon sacrifice, Gpr177L/L;Vil-Cre;Tagln-Cre intestines showed a reduced number of regenerative crypts (Fig. 5B, quantified in 5D), proliferative cells (Fig. 5C,D), CBCs and Paneth cells (Fig. 5D,E). Gpr177L/L;Vil-Cre mice exhibited only a moderate reduction of Paneth cells (P<0.05, Fig. 5D,E). Nuclear β-catenin+ cell numbers were significantly reduced in crypts of regenerating Gpr177L/L;Vil-Cre;Tagln-Cre intestines (two morphologically different regions shown in Fig. 5F,G). The observed modest reduction of body weight and epithelial regeneration in Gpr177L/L;Vil-Cre;Tagln-Cre mice collectively indicated a resilience to abrogated Wnt production from the epithelium and Tagln+ stromal cells under the context of irradiation.
Fig. 5.
Blocking Wnts from epithelium and Tagln+ cells modestly affected irradiation-induced regeneration. (A) Schematic diagram and body-weight analysis of mice exposed to 12 Gy total body irradiation. The Gpr177L/L;Vil-Cre;Tagln-Cre mice showed a modestly significant body-weight reduction at day 5 after irradiation. n=6 mice per genotype. (B,C,E) Post-irradiated Gpr177L/L;Vil-Cre;Tagln-Cre mice had fewer regenerative crypts (B), PCNA+ proliferating crypt cells (C), Olfm4+ cells in the crypt (E) and Lyz1+ cells in the crypt (E). Gpr177L/L;Vil-Cre mice showed modestly reduced Lyz1+ cells. (D) Number of crypts, PCNA+ cells, Olfm4+ crypts and Lyz1+ cells were quantified for wild-type, Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice intestines shown by representative images. n=3 mice per genotype. (F,G) Gpr177L/L;Vil-Cre;Acta2-CreER mice showed reduced number of nuclear β-catenin+ cells in regenerating crypts of distinct small intestinal regions (n=3 mice per genotype). Boxes in G represent 2nd and 3rd quartiles, and bottom and top whiskers represent 10% and 90% of the data. Outliers are shown as dots. Data are mean±s.e.m. from at least three independent experiments. ***P<0.001.
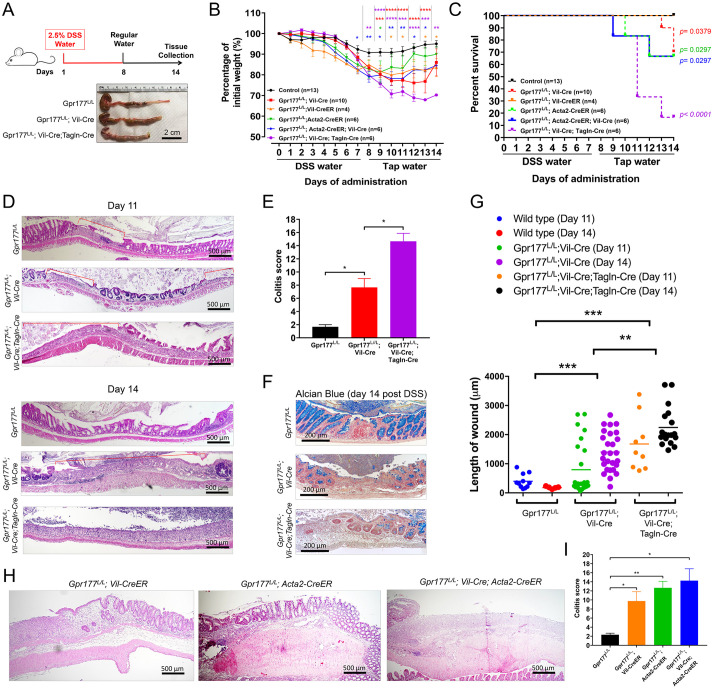
Colonic healing from DSS-induced mucosal injury requires Wnts from epithelial cells, and Tagln+ and Acta2+ stromal cells
Compared with irradiation that primarily eliminated cycling ISCs, dextran sulfate sodium (DSS) induces mucosal demolishing damage, characterized by epithelial death, ulceration, impairment of glandular architecture and inflammation. Upon DSS withdrawal, colonic epithelia heal through regeneration (Yu et al., 2020). As Wnt signaling was shown to play a role in DSS-induced epithelial recovery (Koch et al., 2011), we further asked whether colonic epithelial restoration required Wnts from epithelial or Tagln+ and Acta2+ cells. We treated Gpr177L/L;Vil-Cre (n=10) and Gpr177L/L;Vil-Cre;Tagln-Cre mice (n=6) with 2.5% DSS in drinking water for 7 days and returned them to regular water for another 7 days to allow recovery (Fig. 6A). We used littermates that were Cre negative, as well as mice expressing Cre only, and tamoxifen-injected wild-type and Vil-CreER mice (non-littermates) as controls (n=13). Strikingly, compared with control mice, Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice showed significantly more body weight losses (Fig. 6B). All control mice and most Gpr177L/L;Vil-Cre mice survived the entire 14-day procedure, whereas Gpr177L/L;Vil-Cre;Tagln-Cre mice exhibited mortality from day 9 (Fig. 6C), an early point of recovery. Gpr177L/L;Vil-Cre;Tagln-Cre survivors did not exhibit body weight gain, which was observed for wild-type and Gpr177L/L;Vil-Cre mice during recovery phase (Fig. 6B). Gpr177L/L;Vil-Cre;Tagln-Cre survivors showed shortened colons upon sacrifice on day 14 (Fig. 6A).
Fig. 6.
Colonic regeneration required Wnts from epithelial and distinct stromal compartments. (A) Experimental scheme showing 7 days of 2.5% DSS treatment and 7 days of recovery by administering regular drinking water. Representative colon photographs at the end of the experiment (day 14) showed a reduced colon length and small cecum in Gpr177L/L;Vil-Cre;Tagln-Cre mice. (B) Body weight analysis of mice of various genotypes, with indicated numbers, showed increased morbidity when either epithelial or stromal Wnts were blocked. Gpr177L/L;Vil-Cre;Tagln-Cre mice (purple line) exhibited the worst disease activities with minimal body-weight recovery. Controls included Gpr177 flox/flox (no cre) littermates, as well as Vil-Cre-only mice, and tamoxifen-injected wild-type and Vil-CreER mice (non-littermates). Also see Fig. S5A. (C) No mortality was observed for wild-type mice during the experiment, whereas increased lethality was found for Gpr177L/L;Vil-Cre;Tagln-Cre (purple line) and Gpr177L/L;Vil-Cre;Acta2-CreER mice (blue line). Controls included Gpr177 flox/flox (no cre) littermates, as well as Vil-Cre-only mice, and tamoxifen-injected wild-type and Vil-CreER mice (non-littermates). Also see Fig. S5A. (D) Representative colon histology images of day 11 and day 14 mice following DSS treatment. Red brackets indicate regions of epithelial ulceration. (E) Scoring of mucosal damage showed increased disease indexes in Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice. (F) Alcian Blue staining showed a reduction of goblet cell differentiation in recovering colons of Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice. (G) Microscopic measurement of the lengths of ulceration, at day 11 and 14, showed an advancement of the pathologies in Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice. Gpr177L/L;Vil-Cre;Tagln-Cre colons had the largest epithelial wounds. (H,I) Histology and colitis-scoring of mouse colons at day 14 of experiments showed worse colitis in Gpr177L/L;Acta2-CreER and Gpr177L/L;Vil-CreER mice, whereas the worst disease index was in Gpr177L/L;Vil-Cre;Acta2-CreER mice. Data are mean±s.e.m. from at least three independent experiments. ***P<0.001. Also see Fig. S5.
Pathological evaluation revealed greater epithelial damages in Gpr177L/L;Vil-Cre mice than wild type, and the worst colitis in Gpr177L/L;Vil-Cre;Tagln-Cre mice on day 14 (Fig. 6D,E). Colitis scoring based on ulceration, crypt death, immune cell infiltration, thickness of colonic wall and loss of goblet cell, reached the same conclusion for day 11 (Fig. S5B).
Control mouse colonic mucosa collected on day 11 already exhibited prominent wound-healing activities, including the formation of nascent crypts flanking the wound, epithelial proliferation and migration towards the surfaces of the wound (red brackets designate ulceration, Fig. 6D). Control mouse mucosa showed near-complete healing on day 14, exemplified as a restoration of goblet cell-filled glandular structures (Fig. 6F). In contrast, Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mice had significantly larger and more ulcerations at the beginning and end of recovery (Fig. 6D,G). On day 11, Gpr177L/L;Vil-Cre;Tagln-Cre mouse colons showed continuous ulceration, massive immune cell infiltration and a severely thickened colonic wall (Fig. 6D). On day 14, Gpr177L/L;Vil-Cre;Tagln-Cre survivors had scattered colonic crypts with diminished goblet cell differentiation (Fig. 6D,F).
The impact of Gpr177 removal from intestinal epithelium or Tagln+ stromal cells on colonic epithelial resolution demonstrated here was never described. We therefore also performed DSS experiments on Gpr177L/L;Vil-CreER mice to validate this finding. Tamoxifen-induced Gpr177L/L;Vil-CreER mice showed a similarly exacerbated colitis morbidity to that seen in Gpr177L/L;Vil-Cre mice (Fig. 6B,H,I). The above changes were not due to toxicity of Cre or CreER, as mice expressing Cre or CreER only did not exhibit difference from wild-type mice (Fig. S5A). In addition, we used a single administration of tamoxifen (75 mg/kg) in all our CreER experiments, and this was well below the reported toxicity-inducing dose (Bohin et al., 2018; Huh et al., 2010). Indeed, wild-type mice or CreER mice treated with this tamoxifen dose did not show difference in terms of body weight recovery in response to DSS treatment (Fig. S5A).
As Acta2-CreER targeted a relatively restricted stromal domain (Fig. 3I), we asked whether Wnts produced by Acta2+ stromal cells also contributed to colonic wound healing. Surprisingly, both Gpr177L/L;Acta2-CreER (n=6) and Gpr177L/L;Vil-Cre;Acta2-CreER (n=6) mice showed increased morbidity (Fig. 6B,C). We noted that Gpr177L/L;Vil-Cre;Acta2-CreER mice showed a worse body weight recovery than Gpr177L/L;Acta2-CreER mice, starting from day 9 (Fig. 6B). The slower recovery was consistent with their greater colitis shown at pathological levels (Fig. 6H,I). These analyses suggested that Wnts produced by epithelial cells, and by Tagln+ and Acta2+ cells were all important for colonic wound healing and the disease severities were proportionally correlated with additive Wnt inhibition from different tissue compartments.
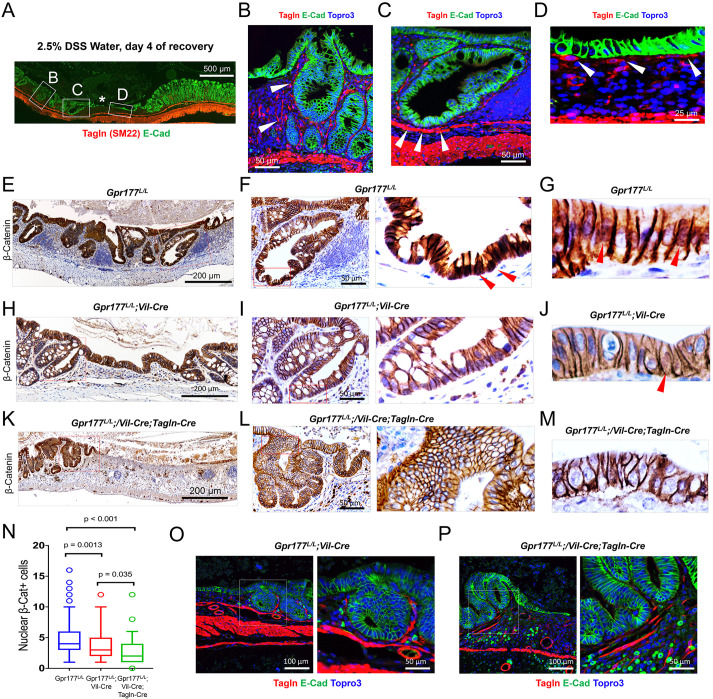
Wnts from wound-associated Tagln+ cells are required for β-catenin nuclear localization in regenerative epithelium
DSS treatment disrupted the colonic mucosal microenvironment by severely demolishing glandular structure and epithelial-stromal interaction. We examined the localization of Tagln+ cells in DSS-treated colonic mucosa 4 days after withdrawing DSS treatment, a time point when epithelial recovery was prominent (Fig. 7A). Compared with colons at steady states (Fig. 3A), DSS-treated colons contained increased number of Tagln+ cells surrounding the hyperplastic crypts (white arrows, Fig. 7B). Immediately flanking the ulcered region (asterisk in Fig. 7A), Tagln-expressing cells were detected at the base of nascent crypt (white arrows, Fig. 7C) and underneath the single layer of wound-covering epithelium (white arrows, Fig. 7D).
Fig. 7.
Tagln+ cells promoted β-catenin nuclear localization in regenerative colon epithelial cells. (A-D) Immunostaining for endogenous Tagln+ cells showed their adjacent localizations to regenerative crypt (B), at the base of wound-flanking nascent crypt (C) and underneath the wound-covering epithelial monolayer (D). Asterisk indicates an ulcerated region flanked by regenerating epithelia. Arrowheads indicate Tagln-expressing cells underneath the colonic epithelium. (E-N) Immunostaining showed strong nuclear β-catenin (red arrowheads) in wild-type regenerating colonic epithelium within crypt cells (F) and within wound-covering epithelial cells (G). Reduced numbers of nuclear β-catenin cells were found in wound-flanking epithelium of Gpr177L/L;Vil-Cre (H-J) and Gpr177L/L;Vil-Cre;Tagln-Cre (K-M) mouse colons. (O,P) Immunostaining showed the presence of Tagln+ cells near the regenerative crypts of Gpr177L/L;Vil-Cre and Gpr177L/L;Vil-Cre;Tagln-Cre mouse colons, suggesting the diminished epithelial nuclear β-catenin and regeneration were due to lack of Wnt production rather than to lack of Tagln+ cells. Data are mean±s.e.m. from at least three independent experiments. Also see Fig. S6.
Within these regenerating epithelia associated with Tagln+ cells, epithelial cells with nuclear β-catenin were found (red arrows, Fig. 7E-G). We found a significant reduction in such nuclear β-catenin+ regenerative epithelial cells in Gpr177L/L;Vil-Cre (Fig. 7H-J) and Gpr177L/L;Vil-Cre;Tagln-Cre colons (Fig. 7K-M). Compared with Gpr177L/L;Vil-Cre colons, Gpr177L/L;Vil-Cre;Tagln-Cre colons showed a further reduction of nuclear β-catenin+ epithelial cells (Fig. 7N). As Tagln+ cells were prominently observed near the injured epithelia (Fig. 7O,P), these changes were apparently caused by lack of Wnt production in the niche, rather than lack of Tagln+ cells. We further examined three canonical Wnt targets, CD44, Myc and Axin2, by immunostaining (Fig. S6A-C). Gpr177L/L;Vil-Cre;Tagln-Cre colons showed the lowest CD44 and Axin2 in regenerative epithelia (Fig. S6B and C). These results collectively suggested that, in absence of epithelial Wnts, inhibition of Wnt production from Tagln+ or Acta2+ cells diminished nuclear β-catenin accumulation and canonical Wnt signaling in regenerative epithelial cells.
DISCUSSION
By ablating Wnt secretion from two distinct stromal populations via Tagln-Cre and Acta2-CreER drivers, or from epithelium using Villin-Cre or Villin-CreER, we demonstrated that diminishing Wnt production from either epithelial or these particular stromal subsets compromised the regenerative capability of colonic epithelium. We further showed that aggregated Wnt deprivation from epithelium as well as from Tagln+ or Acta2+ subsets exacerbated the mucosal damage. In addition to documenting a previously undescribed role of epithelial Wnts in colonic Reg4 cell differentiation and injury-induced regeneration, our findings supported a model that the accumulated Wnt molecules from multiple tissue sources collected at ISC niche may be crucial for injury-induced regeneration.
Literature documenting the growth-driving effects of various Wnts on intestinal stem cell renewal and enteroid growth. Farin et al. and Valenta et al. showed that the addition of Wnt2b was sufficient to restore growth of Wnt3Δ/Δ enteroids and Wls-deficient enteroids (Farin et al., 2012; Valenta et al., 2016). Wnt5a treatment also resulted in the growth of Wls-deficient crypts into small spheroids (Valenta et al., 2016). Kabiri et al. showed that stromal cells promoted survival and growth of Porcn-deficient enteroids and supported epithelial regeneration in IEC-specific Porcn-deficient mice post-radiation injury (Kabiri et al., 2014). Deleting Porcn in telocytes reduced epithelial proliferation in the small and large intestine (Shoshkes-Carmel et al., 2018). Furthermore, mice with Wnt5a deleted in telocytes showed shortened intestines, an observation that was attributed to increased apoptosis in the neonatal mice (Kondo and Kaestner, 2021). Upon infection with rotavirus (RV), an enteric pathogen that affects differentiated cells, the number of CBCs expanded and the proliferating cells migrated faster. Mice lacking epithelial Wnt did not exhibit a similar response post-infection, suggesting the role of epithelial Wnts in inducing a regenerative response to infection (Zou et al., 2018). In et al. (2020) demonstrated a mosaic expression of Wnt2b in specific epithelial cells of human colonic crypts and undifferentiated colonoids. In response to E. coli-secreted cytotoxin EspP-induced injury to colonoids, there was an increase in Wnt2b-expressing cells (In et al., 2020). The infected colonoids failed to survive in the absence of epithelial Wnts when treated with a Porcn inhibitor, suggesting the importance of epithelial Wnts for colonic regeneration in response to injury. In the context of these studies, we delineated the functional contribution of Wnts from two uncharacterized stromal populations (Tagln+ and SMA+) to the homeostasis of small and large intestines.
In homeostasis, we found that either constitutive (by Villin-Cre) or inducible (by Villin-CreER) deletion of epithelial Wls/Gpr177 led to reduction of Reg4+ deep crypt secretory (DCS) cells in the colon, an observation that was not reported before. This change was specific to DCS cells as goblet cells and enterocyte numbers were not affected. DCS cells were originally identified as Paneth cell equivalents that support colonic stem cells (Sasaki et al., 2016). Compared with ablation of epithelial Wnt alone, removing Wnt productions from both epithelium and Tagln+ cells resulted in a near-complete inhibition of DCS differentiation, suggesting that the differentiation or maturation of colonic DCS cells were proportionally sensitive to a cumulative loss of Wnt availability in the niche. Previous DCS ablation studies documented their indispensable role in maintaining colonic stem cell homeostasis in vivo (Sasaki et al., 2016). Interestingly, the different extent of DCS cell loss in Gpr177L/L;Vil-Cre and in Gpr177L/L;Vil-Cre;Tagln-Cre colons positively correlated with different degrees of colonic damage manifested by these DSS-treated homozygotes. Wnt-dependent DCS differentiation identified here offered a mechanism that might contribute to the impaired colonic epithelial repair after Wnt deprivation from epithelial and Tagln+/Acta2+ cell populations.
Bulk RNA-seq and scRNA-seq studies used sorted Foxl1+ or Gli1+ cells for transcriptomic analysis (Degirmenci et al., 2018; Shoshkes-Carmel et al., 2018). By contrast, our scRNA study surveyed the intact stroma without selecting or filtering out a specific subepithelial population. The analysis revealed substantial overlaps among Pdgfrα+, Gli1+ and Foxl1+ cell clusters, all of which robustly co-expressed Tagln, Acta2 and Myh11. Interestingly, our scRNA analysis also confirmed the Wnt2b-expressing Cd81+ Pdgrfalo cluster (McCarthy et al., 2020), which does not express abundant Tagln, Acta2 and Myh11. Ninety three percent of Foxl1+ cells expressed Tagln, a gene encoding an actin-binding protein. Tagln-expressing cells define the widest spectrum of mesenchymal domain, including vascular and visceral smooth muscles, myofibroblasts and fibroblasts (Dong et al., 2012). This mesenchymal cell population has previously been shown to regulate intestinal epithelial proliferation and polyposis (Katajisto et al., 2008). We demonstrated that endogenous Tagln+ cells wrapped around crypts in steady-state small intestine and colon. In DSS-treated colon, Tagln+ cells were immediately associated with the regenerating epithelium flanking the wound. Based on our Cre reporter analysis, Tagln-Cre conceivably targeted more Wnt-producing cells than Acta2-CreER, possibly owing to their constitutive versus inducible expression features. In line with this, combined Wnt inhibition by Villin-Cre and Tagln-Cre caused the strongest colonic damage, reflected by the highest morbidity and lethality, and a continuous loss of epithelium even in late recovery stage. In addition to chemical injury, we also observed moderately impaired regeneration following irradiation. The stronger impact elicited by DSS could be due to its robust and comprehensive epithelium-damaging effect that was not limited only to cycling ISCs in the way that the irradiation was.
Although Acta2-CreER marked a slightly constrained stromal subset, compared with controls, mice lacking Wnt production from these cells also exhibited a pronounced colonic damage, suggesting that even these smaller stromal subsets actively contributed to epithelial regeneration during injury. Interestingly, this same Acta2+ cell population was shown to migrate to colonic wound sites and, when mucosally transplanted, improved colonic epithelial healing after biopsy injury (Manieri et al., 2015). Our data suggested that the presence of Acta2+ cells near epithelial wound might promote colonic healing through Wnt-dependent mechanisms.
Blocking Wnt production from Foxl1+ cells caused severe damage to epithelium in both small intestine and colon in unchallenged mice (Shoshkes-Carmel et al., 2018), whereas blocking Wnts from Gli1+ cells resulted in collapse of colonic crypts and death (Degirmenci et al., 2018). Our scRNA analysis suggested that Foxl1+ cells represented a fraction of Tagln+ domain, and that the majority of Foxl1+ cells expressed Tagln. In homeostasis, we did not observe pronounced epithelial damage in small intestines or colons when using various single or combinatory Cre strategies. Our study aligns with the accumulating evidence suggesting that Foxl1+ cells may not function as canonical Wnt producers, in spite of expressing Wnt4 and Wnt5a (McCarthy et al., 2020). It is plausible that the Cd81+ Pdgfrαlow trophocytes, which have been shown to maintain intestinal stem cells in vivo (McCarthy et al., 2020), may not be effectively deleted by Tagln-Cre and Acta2-CreER drivers reported in this study. Nevertheless, we revealed that blocking Wnt from either the Tagln+ or Acta2+ compartment attenuated colonic epithelial regeneration upon DSS injury. Thus, the non-primary Wnt-producing stromal cells also played a role in supporting injury-induced colonic epithelial regeneration. Taken together, we conclude that the differentiation and regeneration of colonic epithelium are sensitive to Wnt abundance in ISC niche collected from multiple tissue sources.
MATERIALS AND METHODS
Mice and treatment
Gpr177LoxP/LoxP (Gpr177L/L), Gpr177+/−, Acta2-CreER, Vil-Cre and Villin-CreER mice have been described previously (el Marjou et al., 2004; Fu et al., 2011, 2009; Madison et al., 2002; Manieri et al., 2015). Tagln-Cre mice (Boucher et al., 2003; Holtwick et al., 2002) were obtained from the Jackson Laboratory (stock 004746). For tamoxifen treatment, adult mice were intraperitoneally injected with a single dose of tamoxifen (75 mg/kg body weight). For total body irradiation, mice were subjected to 12 Gy γ-irradiation, followed by monitoring of body weight daily. For 5-ethynyl-2′-deoxyuridine (EdU) labeling, EdU (2.5 mg/kg) (Thermo Fisher Scientific, C10338) was injected 30 min before mice were sacrificed at the indicated days (Yu et al., 2018). Mice were maintained on a C57BL/6 and 129 mixed background. All experiments were performed on littermates unless explicitly stated in results. Data were quantified from a minimum of three different litters. Numbers of animals used were described in figure legend. All experimental procedures with mice were approved by Rutgers Institutional Animal Care and Use Committee.
Immunohistochemistry and immunofluorescence staining
Procedures and antibodies for immunohistochemistry and immunofluorescence have been described previously (Das et al., 2015; Feng et al., 2017). In brief, the intestinal tissues were fixed in 4% PFA at 4°C overnight, embedded in paraffin wax and cut into 5 μm sections. For immunofluorescence staining, the slides were rehydrated, subjected to antigen retrieval (citrate acid buffer, pH 6) and incubated in the blocking buffer (PBS containing 0.1% Triton X-100 with 2% normal serum and 2% BSA) at room temperature for 1 h. Then the slides were probed with the primary antibodies at 4°C overnight. Lysozyme (Biogenex, AR024-5R, 1:1), GFP (Invitrogen, A11122 and Abcam, ab6673, 1:500), E-cadherin (BD Transduction Laboratories, 610182, 1:500), pHH3 (Millipore, 06-570, 1:500), Reg4 (R&D Systems, AF1379, 1:100), Muc2 (Santa Cruz Biotechnology, sc-15334, 1:200), EdU (Thermo Fisher Scientific, C10338), Wnt5a/b (Cell Signaling Technology, 2530s), Wnt2b (Abcam, ab50575) and Sm22 (Abcam, ab14106, 1:250) staining was performed according to the manufacturer's instructions. The next day, slides were washed three times with PBS and then incubated with Alexa-labeled secondary antibody (Thermo Fisher Scientific, 1:1000) in the dark for 1-2 h. The samples were counterstained with Topro-3 (Thermo Fisher Scientific, T3605, 1:300) and mounted with the ProLong Gold anti-fade mounting media (Thermo Fisher Scientific, P36930). Images were taken using a Zeiss laser scanning microscope. For immunohistochemistry staining, the slides were hydrated, subjected to antigen retrieval (citrate acid buffer, pH 6) and quenched for endogenous peroxidase. The samples were incubated in the blocking buffer at room temperature for 1 h and then incubated with Lysozyme (Biogenex, AR024-5R, 1:8), β-catenin (BD Transduction Laboratories, 610153, 1:1000), PCNA (Santa Cruz Biotechnology, sc-56, 1:1000), Myc (Millipore Sigma, CBL430, 1:100), CD44 (Cell Signaling Technology, 3570, 1:100) and Axin2 (Thermo Fisher Scientific, MA5-32646, 1:100) antibodies at 4°C overnight. The next day, slides were washed three times with PBS and then incubated with biotin-labeled secondary antibody (Vector Laboratories, 1:500) for 1-2 h. Staining was developed using an ABC Kit (Vector Laboratories, PK-6100) and followed by the DAB kit (Vector Laboratories, SK-4100). The samples were counterstained with Hematoxylin (Vector Laboratories, H-3404) and mounted with cytoseal mounting media (Thermo Fisher Scientific, 8310-4). Images were taken under the Nikon (TE2000-U) light microscope.
Quantitative real-time PCR
Quantitative RT-PCR has been described previously (Das et al., 2015; Gao and Kaestner, 2010; Gao et al., 2009; Sakamori et al., 2012, 2014), with a list of primers provided in Table S1. Threshold cycle (Ct) values obtained for each gene were normalized to Ct values obtained for either β-actin or hypoxanthine-guanine phosphoribosyl transferase (Hprt). Data were obtained from three independent biological samples with three technical replicates.
RNA in situ hybridization
The procedure was followed as previously described (Gregorieff and Clevers, 2010) with the following modifications. In brief, cryo-sections were cut at 8 μm, thawed at room temperature for 15 min and post-fixed in 4% PFA. After incubating the tissue sections in 0.25% acetic anhydride solution, the sections were incubated in the hybridization solution with the probes, as mentioned below, for 24-48 h. The concentration of Olfm4 probe is 1 μg/ml and Gpr177 probe is 2 μg/ml. The sections were incubated with antibody overnight at 4°C and then in BM-Purple (Roche, 11 442 074 001) for up to 24 h in the dark. Slides were counterstained with Nuclear Fast Red (Vector Laboratories, H-3403) and mounted with Cytoseal mounting media (Thermo Fisher Scientific, 8310-4). Images were taken with a Nikon (TE2000-U) light microscope.
Organoid culture
Procedures for crypt isolation and organoid culture were as previously described (Das et al., 2015; Sato and Clevers, 2013; Sato et al., 2009). Organoids isolated from Gpr177L/L;Vil-Cre mice were cultured in ENR media for 7 days and counted daily. Wnt3a (100 ng/ml and 200 ng/ml) and CHIR (3 μM) were added to the epidermal growth factor/Noggin/R-spondin1 (ENR) media at day 1. Organoids isolated from Gpr177L/−;Vil-CreER mice were cultured in ENR media for 5 days. Vehicle or 4-OHT (0.5 μM) was added to the media for 12 h on day 6. The organoids were then cultured in ENR media without or with Wnt3a (100 ng/ml). The organoids were counted daily and imaged on day 6. EdU (10 μm) was added into the culture media for 30 min on day 6. The organoids were fixed in 4% PFA and the EdU staining was performed according to the manufacturer's instructions.
DSS-induced experimental colitis
The mice were administered with 2.5% dextran sulfate sodium (DSS, Colitis grade, 36-50 kDa, MP Biologics, SKU 0216011080) in tap water for 7 days and recovered with tap water for another 7 days. The body weight of individual mice was monitored daily and the graph was plotted using GraphPad Prism version 8.3. Colon tissues were harvested for pathological analysis. Colonic damage was scored blindly by a GI pathologist as described previously (Chassaing et al., 2014) in Fig. 6E,I. Briefly, scores (0-4) were assigned based on the severity of epithelial injury and leukocyte infiltration into the mucosa, submucosa and muscularis. These three scores were multiplied by an extended factor to assess the extent of the change: 1 for focal, 2 for patchy and 3 for diffuse, and summed to achieve the final score out of the maximal score of 36. In Fig. S5, colitis scoring was performed by an independent experimentalist using a different method described previously (Chinen et al., 2011).
Single-cell dissociation and sorting
The distal ileum of a wild-type mouse was harvested and briefly rinsed in ice-cold PBS (Fisher Scientific, SH30256LS). The tissue was opened longitudinally, rinsed in ice-cold PBS and further sliced to 1-2 mm pieces. The pieces were rinsed in 30 ml of ice-cold PBS by inverting the Falcon tube 10-15 times. The pieces were then transferred into fresh 30 ml of ice-cold PBS. This step was repeated until the solution remained clear after inverting. Each piece was then transferred to 30 ml crypt isolation buffer, containing 5 mM EDTA (Invitrogen, AM9260G), 2% BSA (Sigma, A3294) and HBSS Ca/Mg-free (Sigma, H9394), and shaken at 37°C for 15 min. The tube was subsequently vigorously shaken to release the epithelial layer from the pieces, after which the solution was discarded. This was repeated in another 30 ml of crypt isolation buffer. The pieces were then incubated in DMEM/F12 medium (Thermo Fisher, 12634-010) for 10 min on a Petri dish at room temperature. The solution was discarded, and the pieces were thoroughly minced. 10 ml of digestion buffer [100 U/ml Collagenase II (Thermo Fisher, 17101015), 500 U/ml DNase I (QIAGEN, 79254) and HBSS Ca/Mg free] was added to the minced tissue and shaken at 37°C for 30 min. The tissue was completely digested, and the solution was passed through a 70 µM cell strainer into a 50 ml Falcon tube. The tube was centrifuged at 200 g for 10 min. The pellet was resuspended in 1 ml of FACS solution (2% BSA in PBS). The single-cell suspensions were stained with DAPI prior to sorting. Single-cell suspensions were subjected to sorting by BD Biosciences Aria II Flow Cytometer (BD FACSAria II). Single viable lamina propria lymphocytes and mesenchymal cells were gated by forward scatter, side scatter and negative staining for DAPI.
Droplet-based scRNA-seq
Cell number and viability were determined by a propidium iodide-based fluorescence assay using Moxi GO II System, Orflo Prod#MXG102 (ORFLO Technologies). Droplet-based single-cell partitioning and single-cell RNA-seq libraries were generated using the Chromium Single-Cell 3′ Reagent v3 Kit (10X Genomics) on the 10X Chromium Controller as per the manufacturer's protocol. Live cells in single-cell suspension with 95% viability were mixed with gel beads, reverse transcription reagents and partitioning oil into a single-cell 3′ Chip and loaded onto 10X Chromium Controller for GEM generation. Briefly, the protocol includes reverse transcription, cleanup, cDNA amplification, fragmentation, end repair and A-tail prep, adapter ligation, and incorporation of sample indices into finished libraries, which are compatible with Illumina next-generation sequencing platforms. Sample quantification and quality control were determined using Qubit Fluorometer (Invitrogen, Life Technologies) and TapeStation (Agilent Technologies), respectively. cDNA libraries were sequenced on Illumina NovaSeq 6000 sequencer (Illumina) with a configuration of 28/8/0/91 bp for cell barcode, sample barcode, i5 index, and mRNA reads, respectively, as recommended by 10X Genomics. The Chromium Single Cell Software is used to analyze and visualize single-cell 3′ RNA-seq data produced by the 10X Chromium Platform. The 10X chromium software package includes Cell Ranger Pipelines and Loupe Cell Browser. Cell Ranger pipelines use raw 10X single-cell sequencing data from an Illumina sequencer and perform demultiplexing, unique barcode processing and single-cell 3′ gene counting.
For Fig. 2A-D, the wild-type count matrix files generated by Cell Ranger were transformed into the count matrix by R (version 3.6.1). Count matrices for different groups were combined and used as the input for Seurat package (version 3.1.0) (Butler et al., 2018; Stuart et al., 2019). Data normalization was performed by Seurat using the ‘LogNormalize’ method. Briefly, the gene counts for each cell were divided by the total counts for that cell and multiplied by the scale factor (10,000). The data were then natural log transformed. Cells with fewer than 200 expressed genes and genes expressed in fewer than three cells were removed from the downstream analyses. The top 2000 variable genes were used to perform PCA (primary component analysis). Ten out of 20 PCs were selected for doing clustering and Uniform Manifold Approximation and Projection (UMAP). DE (differential expression) was performed by Seurat using the Wilcoxon test. DEGs with P≤0.05, logFC>0.2 and percentage of expression in each group >0.25 were visualized by generating a heat map. Based on the expression of Wnts indicated in Fig. 2B, clusters 4, 9, 11, 14 and 21 were further selected to visualize the expression of key Wnts and stromal markers mentioned in Fig. 2C.
For Fig. S2A,B, single-cell deep constrained clustering (scDCC) was performed for Wnt4 and Wnt5a. The top 2000 most highly variable genes were identified using Seurat with the selection method of vst that calculates feature variance by fitting the variance-mean relationship. The expression data of these genes was then fed to scDCC, a deep learning model that requires two inputs: expression data and marker genes. In this study, scDCC was based on marker genes Wnt4 and Wnt5a. The restriction of binding genes was based on their distances from each other. If the distance between two genes was among the top 10% farthest distances, they were marked as not being connected, whereas if their distance was smaller than 90% of distances of other gene pairs, they were marked as must be connected. After scDCC reduced the dimensions of the scRNA-seq data, t-SNE was applied for visualization.
For Fig. 2E,F and Fig. S2C-G, the wild-type count matrix file generated by Cell Ranger was imported to Partek flow software for secondary data analysis. The single-cell analysis was generated using Partek Flow, version 9.0, build 9.0.20.0202. For each cell, quality control metrics such as number of read counts, number of detected genes and percentage of mitochondrial reads were calculated and used to filter out low-quality cells. The data were then log2+1 normalized based on counts per million and the genes that were not expressed in at least 99% of the cells were excluded from the dataset. Principal components (PCs) were calculated for the samples and the scree plot was used to determine the number of PCs to be used. Based on the PC value, cells were divided into clusters in an unsupervised fashion. The ANOVA test was used to identify differentially expressed genes (DEGs) for each cluster by comparing genes in all the clusters, filtering genes that were upregulated by 1.5-fold and then sorting them by ascending P-value. The clusters were then visualized using t-Distributed Stochastic Neighbor Embedding (t-SNE). Based on the expression of Tagln and Foxl1, the cells were selected and classified. DEGs were identified for the three populations, Foxl1−/Tagln+, Foxl1+/Tagln+ and Foxl1+/Tagln−, and the signature DEG genes (FDR set up ≤1e-8, fold change>2) were visualized by generating a heat map and by generating violin plots for genes of interest.
Transmission EM analysis and Gpr177 immunogold labeling
TEM procedures have been described previously (Gao and Kaestner, 2010; Sakamori et al., 2012). For Gpr177 immunogold labeling and EM analysis, duodenal and jejunal tissues were dissected from wild-type and Gpr177L/; Vil-Cre mice and immediately fixed as ∼1 mm fragments in 2.5% paraformaldehyde in cacodylate buffer (pH 7.4) overnight. The tissue was then sliced to 100-200 μm thickness on a vibratome and frozen between two brass ‘top-hats’ in a HPM010 (Abra Fluid) at 5000 PSI at −180°C. Next, the frozen tissue was transferred to frozen glass-distilled 100% acetone and dehydrated at −90°C for 48 h. The tissue was then infiltrated with HM-20 lowicryl and polymerized with 360 nm light at −50°C in a dry nitrogen environment. Tissue sections cut 60 nm thick containing Paneth cells were immunolabeled with Gpr177 antibody (Fu et al., 2009) at 1:250 to 1:50 in 5% BSA, 0.1% ice-cold water fish gelatin in PBS (pH 7.4). No primary antibody control and Gpr177-deficient cells were used in initial tests to optimize labeling conditions. Images shown were immunolabeled with 1:100 dilution of primary antibody. Stable antigen-antibody complexes were detected with protein A conjugated to either 15 nm gold colloids or 20 nm gold colloids. Imaging was performed with a FEI Tecnai-12 microscope at 80 keV using a nominal magnification of 6500×. Montage images were collected using Serial EM and stitched together with the IMOD subroutine Blendmont (Kremer et al., 1996; Mastronarde, 2005). Each image has a pixel dimension of ∼3 nm such that each spherical gold particle should fill five pixels and resizing of the images should provide information to reveal the approximate volume the gold would occupy in the images. Immunogold particles were counted manually, excluding particles within nuclear area. Area and perimeter of individual Paneth cells were measured using Photoshop CS. Number of immunogold particles in each subcellular compartment per unit area (for ER and Golgi) or per unit length (for plasma membrane) were calculated and compared by t-test.
Quantifications and statistical analyses
Quantification was made from at least three animals per genotype for each experiment, as previously described (Das et al., 2015; Feng et al., 2017). All comparisons were made among littermates. 50-100 crypts of small intestine and about 50 colonic crypts were counted per marker per genotype. For the number of regenerative crypts, all crypts were counted within 50 villi regardless of their sectioned shape. Length of wound was measured along multiple wound beds by ImageJ and the average length was calculated. Statistical significance was analyzed using Student's t-test, two-tailed, unpaired or one-way ANOVA. *P<0.05; **P<0.01; ***P<0.001. In Fig. 2, the statistical significance for body weights was analyzed using two-way ANOVA and the survival curve was analyzed using Gehan-Breslow-Wilcoxon test. Graphs were made using GraphPad Prism version 7.02, 8.3 and 9.
Supplementary Material
Acknowledgements
We thank Juan Flores, Sheila Bandyopadhya and Ivor Joseph for their helpful discussion of the work.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Author contributions
Conceptualization: S.D., Q.F., N.G.; Methodology: S.D., Q.F., I.B., X.L., H.L., O.P.-C.; Software: I.B., X.L., H.L.; Validation: S.D., Q.F., I.B., X.L., H.L., S.Y., X.Z., Y.L.; Formal analysis: S.D., Q.F., I.B., O.P.-C., S.Y., X.Z., Y.L., Z.W., L.Z., T.C.W.; Investigation: S.D., Q.F., I.B., S.Y., X.Z., Y.L., Z.W., E.M.B., M.P.V., W.H., L.Z., T.C.W.; Resources: O.P.-C., M.P.V., W.H., L.Z., T.C.W., N.G.; Data curation: S.D., Q.F., I.B., X.L., H.L.; Writing - original draft: S.D., Q.F., I.B., E.M.B., N.G.; Writing - review & editing: I.B., E.M.B., N.G.; Visualization: S.D., Q.F., I.B., X.L., H.L.; Supervision: E.M.B., N.G.; Project administration: N.G.; Funding acquisition: N.G.
Funding
This work was supported by National Institutes of Health grants (R01DK102934, R01AT010243 and R01DK119198; R01DE015654 and R01DE026936 to W.H.), an American Cancer Society Scholar Award (RSG-15-060-01-TBE), National Science Foundation/Biology/Instrument Development for Biological Research grants (1353890 and 195282), a Rutgers Initiative for Multidisciplinary Research Teams (IMRT) award to N.G. and with a New Jersey Commission on Cancer Research Postdoctoral Fellowship (DFHS16PPC045 to Q.F.). Deposited in PMC for release after 12 months.
Data availability
The single-cell RNA-seq data have been deposited in GEO under accession number GSE151152.
Peer review history
The peer review history is available online at https://journals.biologists.com/dev/article-lookup/doi/10.1242/dev.199587.
References
- Angers, S. and Moon, R. T. (2009). Proximal events in Wnt signal transduction. Nat. Rev. Mol. Cell Biol. 10, 468-477. 10.1038/nrm2717 [DOI] [PubMed] [Google Scholar]
- Aoki, R., Shoshkes-Carmel, M., Gao, N., Shin, S., May, C. L., Golson, M. L., Zahm, A. M., Ray, M., Wiser, C. L., Wright, C. V.et al. (2016). Foxl1-expressing mesenchymal cells constitute the intestinal stem cell niche. Cell. Mol. Gastroenterol. Hepatol. 2, 175-188. 10.1016/j.jcmgh.2015.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bänziger, C., Soldini, D., Schütt, C., Zipperlen, P., Hausmann, G. and Basler, K. (2006). Wntless, a conserved membrane protein dedicated to the secretion of Wnt proteins from signaling cells. Cell 125, 509-522. 10.1016/j.cell.2006.02.049 [DOI] [PubMed] [Google Scholar]
- Barker, N., van Es, J. H., Kuipers, J., Kujala, P., van den Born, M., Cozijnsen, M., Haegebarth, A., Korving, J., Begthel, H., Peters, P. J.et al. (2007). Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 449, 1003-1007. 10.1038/nature06196 [DOI] [PubMed] [Google Scholar]
- Bartscherer, K., Pelte, N., Ingelfinger, D. and Boutros, M. (2006). Secretion of Wnt ligands requires Evi, a conserved transmembrane protein. Cell 125, 523-533. 10.1016/j.cell.2006.04.009 [DOI] [PubMed] [Google Scholar]
- Bohin, N., Carlson, E. A. and Samuelson, L. C. (2018). Genome toxicity and impaired stem cell function after conditional activation of CreER(T2) in the intestine. Stem Cell Rep. 11, 1337-1346. 10.1016/j.stemcr.2018.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boucher, P., Gotthardt, M., Li, W.-P., Anderson, R. G. W. and Herz, J. (2003). LRP: role in vascular wall integrity and protection from atherosclerosis. Science 300, 329-332. 10.1126/science.1082095 [DOI] [PubMed] [Google Scholar]
- Boutros, M. and Mlodzik, M. (1999). Dishevelled: at the crossroads of divergent intracellular signaling pathways. Mech. Dev. 83, 27-37. 10.1016/S0925-4773(99)00046-5 [DOI] [PubMed] [Google Scholar]
- Butler, A., Hoffman, P., Smibert, P., Papalexi, E. and Satija, R. (2018). Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat. Biotechnol. 36, 411-420. 10.1038/nbt.4096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadigan, K. M. and Peifer, M. (2009). Wnt signaling from development to disease: insights from model systems. Cold Spring Harb. Perspect. Biol. 1, a002881. 10.1101/cshperspect.a002881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassaing, B., Aitken, J. D., Malleshappa, M. and Vijay-Kumar, M. (2014). Dextran sulfate sodium (DSS)-induced colitis in mice. Curr. Protoc. Immunol. 104, 15-25. 10.1002/0471142735.im1525s104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinen, T., Komai, K., Muto, G., Morita, R., Inoue, N., Yoshida, H., Sekiya, T., Yoshida, R., Nakamura, K., Takayanagi, R.et al. (2011). Prostaglandin E2 and SOCS1 have a role in intestinal immune tolerance. Nat. Commun. 2, 190. 10.1038/ncomms1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ching, W. and Nusse, R. (2006). A dedicated Wnt secretion factor. Cell 125, 432-433. 10.1016/j.cell.2006.04.018 [DOI] [PubMed] [Google Scholar]
- Clevers, H. and Nusse, R. (2012). Wnt/β-catenin signaling and disease. Cell 149, 1192-1205. 10.1016/j.cell.2012.05.012 [DOI] [PubMed] [Google Scholar]
- Das, S., Yu, S., Sakamori, R., Stypulkowski, E. and Gao, N. (2012). Wntless in Wnt secretion: molecular, cellular and genetic aspects. Front. Biol. 7, 587-593. 10.1007/s11515-012-1200-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das, S., Yu, S., Sakamori, R., Vedula, P., Feng, Q., Flores, J., Hoffman, A., Fu, J., Stypulkowski, E., Rodriguez, A.et al. (2015). Rab8a vesicles regulate Wnt ligand delivery and Paneth cell maturation at the intestinal stem cell niche. Development 142, 2147-2162. 10.1242/dev.121046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot, R. E. A., Farin, H. F., Macůrková, M., van Es, J. H., Clevers, H. C. and Korswagen, H. C. (2013). Retromer dependent recycling of the Wnt secretion factor Wls is dispensable for stem cell maintenance in the mammalian intestinal epithelium. PLoS ONE 8, e76971. 10.1371/journal.pone.0076971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lau, W., Barker, N. and Clevers, H. (2007). WNT signaling in the normal intestine and colorectal cancer. Front. Biosci. 12, 471-491. 10.2741/2076 [DOI] [PubMed] [Google Scholar]
- Degirmenci, B., Valenta, T., Dimitrieva, S., Hausmann, G. and Basler, K. (2018). GLI1-expressing mesenchymal cells form the essential Wnt-secreting niche for colon stem cells. Nature 558, 449-453. 10.1038/s41586-018-0190-3 [DOI] [PubMed] [Google Scholar]
- Dong, L.-H., Lv, P. and Han, M. (2012). Roles of SM22α in cellular plasticity and vascular diseases. Cardiovasc. Hematol. Disord. Drug Targets 12, 119-125. 10.2174/1871529X11202020119 [DOI] [PubMed] [Google Scholar]
- Eaton, S., Wepf, R. and Simons, K. (1996). Roles for Rac1 and Cdc42 in planar polarization and hair outgrowth in the wing of Drosophila. J. Cell Biol. 135, 1277-1289. 10.1083/jcb.135.5.1277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- el Marjou, F., Janssen, K.-P., Chang, B. H.-J., Li, M., Hindie, V., Chan, L., Louvard, D., Chambon, P., Metzger, D. and Robine, S. (2004). Tissue-specific and inducible Cre-mediated recombination in the gut epithelium. Genesis 39, 186-193. 10.1002/gene.20042 [DOI] [PubMed] [Google Scholar]
- Fanto, M., Weber, U., Strutt, D. I. and Mlodzik, M. (2000). Nuclear signaling by Rac and Rho GTPases is required in the establishment of epithelial planar polarity in the Drosophila eye. Curr. Biol. 10, 979-988. 10.1016/S0960-9822(00)00645-X [DOI] [PubMed] [Google Scholar]
- Farin, H. F., Van Es, J. H. and Clevers, H. (2012). Redundant sources of Wnt regulate intestinal stem cells and promote formation of Paneth cells. Gastroenterology 143, 1518-1529.e7. 10.1053/j.gastro.2012.08.031 [DOI] [PubMed] [Google Scholar]
- Feng, Q., Bonder, E. M., Engevik, A. C., Zhang, L., Tyska, M. J., Goldenring, J. R. and Gao, N. (2017). Disruption of Rab8a and Rab11a causes formation of basolateral microvilli in neonatal enteropathy. J. Cell Sci. 130, 2491-2505. 10.1242/jcs.201897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fevr, T., Robine, S., Louvard, D. and Huelsken, J. (2007). Wnt/β-catenin is essential for intestinal homeostasis and maintenance of intestinal stem cells. Mol. Cell. Biol. 27, 7551-7559. 10.1128/MCB.01034-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu, J., Jiang, M., Mirando, A. J., Ivy Yu, H.-M. and Hsu, W. (2009). Reciprocal regulation of Wnt and Gpr177/mouse Wntless is required for embryonic axis formation. Proc. Natl. Acad. Sci. USA 106, 18598-18603. 10.1073/pnas.0904894106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu, J., Ivy Yu, H.-M., Maruyama, T., Mirando, A. J. and Hsu, W. (2011). Gpr177/mouse Wntless is essential for Wnt-mediated craniofacial and brain development. Dev. Dyn. 240, 365-371. 10.1002/dvdy.22541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, N. and Kaestner, K. H. (2010). Cdx2 regulates endo-lysosomal function and epithelial cell polarity. Genes Dev. 24, 1295-1305. 10.1101/gad.1921510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, N., White, P. and Kaestner, K. H. (2009). Establishment of intestinal identity and epithelial-mesenchymal signaling by Cdx2. Dev. Cell 16, 588-599. 10.1016/j.devcel.2009.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregorieff, A. and Clevers, H. (2010). In situ hybridization to identify gut stem cells. Curr. Protoc. Stem Cell Biol. Chapter 2, Unit 2F 1. 10.1002/9780470151808.sc02f01s12 [DOI] [PubMed] [Google Scholar]
- Gregorieff, A., Pinto, D., Begthel, H., Destree, O., Kielman, M. and Clevers, H. (2005). Expression pattern of Wnt signaling components in the adult intestine. Gastroenterology 129, 626-638. 10.1016/j.gastro.2005.06.007 [DOI] [PubMed] [Google Scholar]
- Greicius, G., Kabiri, Z., Sigmundsson, K., Liang, C., Bunte, R., Singh, M. K. and Virshup, D. M. (2018). PDGFRalpha(+) pericryptal stromal cells are the critical source of Wnts and RSPO3 for murine intestinal stem cells in vivo. Proc. Natl. Acad. Sci. USA 115, E3173-E3181. 10.1073/pnas.1713510115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habas, R., Kato, Y. and He, X. (2001). Wnt/Frizzled activation of Rho regulates vertebrate gastrulation and requires a novel Formin homology protein Daam1. Cell 107, 843-854. 10.1016/S0092-8674(01)00614-6 [DOI] [PubMed] [Google Scholar]
- Habas, R., Dawid, I. B. and He, X. (2003). Coactivation of Rac and Rho by Wnt/Frizzled signaling is required for vertebrate gastrulation. Genes Dev. 17, 295-309. 10.1101/gad.1022203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, X., Semenov, M., Tamai, K. and Zeng, X. (2004). LDL receptor-related proteins 5 and 6 in Wnt/β-catenin signaling: arrows point the way. Development 131, 1663-1677. 10.1242/dev.01117 [DOI] [PubMed] [Google Scholar]
- Holtwick, R., Gotthardt, M., Skryabin, B., Steinmetz, M., Potthast, R., Zetsche, B., Hammer, R. E., Herz, J. and Kuhn, M. (2002). Smooth muscle-selective deletion of guanylyl cyclase-A prevents the acute but not chronic effects of ANP on blood pressure. Proc. Natl. Acad. Sci. USA 99, 7142-7147. 10.1073/pnas.102650499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, H. and He, X. (2008). Wnt/β-catenin signaling: new (and old) players and new insights. Curr. Opin. Cell Biol. 20, 119-125. 10.1016/j.ceb.2008.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh, W. J., Mysorekar, I. U. and Mills, J. C. (2010). Inducible activation of Cre recombinase in adult mice causes gastric epithelial atrophy, metaplasia, and regenerative changes in the absence of “floxed” alleles. Am. J. Physiol. Gastrointest. Liver Physiol. 299, G368-G380. 10.1152/ajpgi.00021.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- In, J. G., Yin, J., Atanga, R., Doucet, M., Cole, R. N., DeVine, L., Donowitz, M., Zachos, N. C., Blutt, S. E., Estes, M. K., et al. (2020). Epithelial WNT2B and desert hedgehog are necessary for human colonoid regeneration after bacterial cytotoxin injury. iScience 23, 101618. 10.1016/j.isci.2020.101618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabiri, Z., Greicius, G., Madan, B., Biechele, S., Zhong, Z., Zaribafzadeh, H., Edison, Aliyev, J., Wu, Y., Bunte, R.et al. (2014). Stroma provides an intestinal stem cell niche in the absence of epithelial Wnts. Development 141, 2206-2215. 10.1242/dev.104976 [DOI] [PubMed] [Google Scholar]
- Katajisto, P., Vaahtomeri, K., Ekman, N., Ventelä, E., Ristimäki, A., Bardeesy, N., Feil, R., DePinho, R. A. and Mäkelä, T. P. (2008). LKB1 signaling in mesenchymal cells required for suppression of gastrointestinal polyposis. Nat. Genet. 40, 455-459. 10.1038/ng.98 [DOI] [PubMed] [Google Scholar]
- Koch, S., Nava, P., Addis, C., Kim, W., Denning, T. L., Li, L., Parkos, C. A. and Nusrat, A. (2011). The Wnt antagonist Dkk1 regulates intestinal epithelial homeostasis and wound repair. Gastroenterology 141, 259-268, 268 e251-258. 10.1053/j.gastro.2011.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo, A. and Kaestner, K. H. (2021). FoxL1+ mesenchymal cells are a critical source of Wnt5a for midgut elongation during mouse embryonic intestinal development. Cells Dev. 165, 203662. 10.1016/j.cdev.2021.203662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek, V., Barker, N., Moerer, P., van Donselaar, E., Huls, G., Peters, P. J. and Clevers, H. (1998). Depletion of epithelial stem-cell compartments in the small intestine of mice lacking Tcf-4. Nat. Genet. 19, 379-383. 10.1038/1270 [DOI] [PubMed] [Google Scholar]
- Kremer, J. R., Mastronarde, D. N. and McIntosh, J. R. (1996). Computer visualization of three-dimensional image data using IMOD. J. Struct. Biol. 116, 71-76. 10.1006/jsbi.1996.0013 [DOI] [PubMed] [Google Scholar]
- Kuhbandner, S., Brummer, S., Metzger, D., Chambon, P., Hofmann, F. and Feil, R. (2000). Temporally controlled somatic mutagenesis in smooth muscle. Genesis 28, 15-22. [DOI] [PubMed] [Google Scholar]
- Kuhnert, F., Davis, C. R., Wang, H.-T., Chu, P., Lee, M., Yuan, J., Nusse, R. and Kuo, C. J. (2004). Essential requirement for Wnt signaling in proliferation of adult small intestine and colon revealed by adenoviral expression of Dickkopf-1. Proc. Natl. Acad. Sci. USA 101, 266-271. 10.1073/pnas.2536800100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald, B. T. and He, X. (2012). Frizzled and LRP5/6 receptors for Wnt/β-catenin signaling. Cold Spring Harb. Perspect. Biol. 4, a007880. 10.1101/cshperspect.a007880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald, B. T., Tamai, K. and He, X. (2009). Wnt/β-catenin signaling: components, mechanisms, and diseases. Dev. Cell 17, 9-26. 10.1016/j.devcel.2009.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madison, B. B., Dunbar, L., Qiao, X. T., Braunstein, K., Braunstein, E. and Gumucio, D. L. (2002). Cis elements of the villin gene control expression in restricted domains of the vertical (crypt) and horizontal (duodenum, cecum) axes of the intestine. J. Biol. Chem. 277, 33275-33283. 10.1074/jbc.M204935200 [DOI] [PubMed] [Google Scholar]
- Manieri, N. A., Mack, M. R., Himmelrich, M. D., Worthley, D. L., Hanson, E. M., Eckmann, L., Wang, T. C. and Stappenbeck, T. S. (2015). Mucosally transplanted mesenchymal stem cells stimulate intestinal healing by promoting angiogenesis. J. Clin. Invest. 125, 3606-3618. 10.1172/JCI81423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastronarde, D. N. (2005). Automated electron microscope tomography using robust prediction of specimen movements. J. Struct. Biol. 152, 36-51. 10.1016/j.jsb.2005.07.007 [DOI] [PubMed] [Google Scholar]
- McCarthy, N., Manieri, E., Storm, E. E., Saadatpour, A., Luoma, A. M., Kapoor, V. N., Madha, S., Gaynor, L. T., Cox, C., Keerthivasan, S.et al. (2020). Distinct mesenchymal cell populations generate the essential intestinal BMP signaling gradient. Cell Stem Cell 26, 391-402.e395. 10.1016/j.stem.2020.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyoshi, H., Ajima, R., Luo, C. T., Yamaguchi, T. P. and Stappenbeck, T. S. (2012). Wnt5a potentiates TGF-β signaling to promote colonic crypt regeneration after tissue injury. Science 338, 108-113. 10.1126/science.1223821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nusse, R., Fuerer, C., Ching, W., Harnish, K., Logan, C., Zeng, A., ten Berge, D. and Kalani, Y. (2008). Wnt signaling and stem cell control. Cold Spring Harb. Symp. Quant. Biol. 73, 59-66. 10.1101/sqb.2008.73.035 [DOI] [PubMed] [Google Scholar]
- Pinto, D., Gregorieff, A., Begthel, H. and Clevers, H. (2003). Canonical Wnt signals are essential for homeostasis of the intestinal epithelium. Genes Dev. 17, 1709-1713. 10.1101/gad.267103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polakis, P. (2007). The many ways of Wnt in cancer. Curr. Opin. Genet. Dev. 17, 45-51. 10.1016/j.gde.2006.12.007 [DOI] [PubMed] [Google Scholar]
- Port, F. and Basler, K. (2010). Wnt trafficking: new insights into Wnt maturation, secretion and spreading. Traffic 11, 1265-1271. 10.1111/j.1600-0854.2010.01076.x [DOI] [PubMed] [Google Scholar]
- Potten, C. S. (1977). Extreme sensitivity of some intestinal crypt cells to X and γ irradiation. Nature 269, 518. 10.1038/269518a0 [DOI] [PubMed] [Google Scholar]
- Powell, D. W., Pinchuk, I. V., Saada, J. I., Chen, X. and Mifflin, R. C. (2011). Mesenchymal cells of the intestinal lamina propria. Annu. Rev. Physiol. 73, 213-237. 10.1146/annurev.physiol.70.113006.100646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reya, T. and Clevers, H. (2005). Wnt signalling in stem cells and cancer. Nature 434, 843-850. 10.1038/nature03319 [DOI] [PubMed] [Google Scholar]
- Saha, S., Aranda, E., Hayakawa, Y., Bhanja, P., Atay, S., Brodin, N. P., Li, J., Asfaha, S., Liu, L., Tailor, Y.et al. (2016). Macrophage-derived extracellular vesicle-packaged WNTs rescue intestinal stem cells and enhance survival after radiation injury. Nat. Commun. 7, 13096. 10.1038/ncomms13096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamori, R., Das, S., Yu, S., Feng, S., Stypulkowski, E., Guan, Y., Douard, V., Tang, W., Ferraris, R. P., Harada, A.et al. (2012). Cdc42 and Rab8a are critical for intestinal stem cell division, survival, and differentiation in mice. J. Clin. Invest. 122, 1052-1065. 10.1172/JCI60282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamori, R., Yu, S., Zhang, X., Hoffman, A., Sun, J., Das, S., Vedula, P., Li, G., Fu, J., Walker, F.et al. (2014). CDC42 Inhibition Suppresses Progression of Incipient Intestinal Tumors. Cancer Res. 74, 5480-5492. 10.1158/0008-5472.CAN-14-0267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- San Roman, A. K., Jayewickreme, C. D., Murtaugh, L. C. and Shivdasani, R. A. (2014). Wnt secretion from epithelial cells and subepithelial myofibroblasts is not required in the mouse intestinal stem cell niche in vivo. Stem Cell Rep. 2, 127-134. 10.1016/j.stemcr.2013.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki, N., Sachs, N., Wiebrands, K., Ellenbroek, S. I., Fumagalli, A., Lyubimova, A., Begthel, H., van den Born, M., van Es, J. H., Karthaus, W. R.et al. (2016). Reg4+ deep crypt secretory cells function as epithelial niche for Lgr5+ stem cells in colon. Proc. Natl. Acad. Sci. USA 113, E5399-E5407. 10.1073/pnas.1607327113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato, T. and Clevers, H. (2013). Primary mouse small intestinal epithelial cell cultures. Methods Mol. Biol. 945, 319-328. 10.1007/978-1-62703-125-7_19 [DOI] [PubMed] [Google Scholar]
- Sato, T., Vries, R. G., Snippert, H. J., van de Wetering, M., Barker, N., Stange, D. E., van Es, J. H., Abo, A., Kujala, P., Peters, P. J.et al. (2009). Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459, 262-265. 10.1038/nature07935 [DOI] [PubMed] [Google Scholar]
- Sato, T., van Es, J. H., Snippert, H. J., Stange, D. E., Vries, R. G., van den Born, M., Barker, N., Shroyer, N. F., van de Wetering, M. and Clevers, H. (2011). Paneth cells constitute the niche for Lgr5 stem cells in intestinal crypts. Nature 469, 415-418. 10.1038/nature09637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte, G. (2010). International union of basic and clinical pharmacology. LXXX. The class Frizzled receptors. Pharmacol. Rev. 62, 632-667. 10.1124/pr.110.002931 [DOI] [PubMed] [Google Scholar]
- Schulte, G. and Bryja, V. (2007). The Frizzled family of unconventional G-protein-coupled receptors. Trends Pharmacol. Sci. 28, 518-525. 10.1016/j.tips.2007.09.001 [DOI] [PubMed] [Google Scholar]
- Shoshkes-Carmel, M., Wang, Y. J., Wangensteen, K. J., Tóth, B., Kondo, A., Massasa, E. E., Itzkovitz, S. and Kaestner, K. H. (2018). Subepithelial telocytes are an important source of Wnts that supports intestinal crypts. Nature 557, 242-246. 10.1038/s41586-018-0084-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivas, S., Watanabe, T., Lin, C.-S., William, C. M., Tanabe, Y., Jessell, T. M. and Costantini, F. (2001). Cre reporter strains produced by targeted insertion of EYFP and ECFP into the ROSA26 locus. BMC Dev. Biol. 1, 4. 10.1186/1471-213X-1-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strutt, D. I., Weber, U. and Mlodzik, M. (1997). The role of RhoA in tissue polarity and Frizzled signalling. Nature 387, 292-295. 10.1038/387292a0 [DOI] [PubMed] [Google Scholar]
- Stuart, T., Butler, A., Hoffman, P., Hafemeister, C., Papalexi, E., Mauck, W. M., III, Hao, Y., Stoeckius, M., Smibert, P. and Satija, R. (2019). Comprehensive integration of single-cell data. Cell 177, 1888-1902 e1821. 10.1016/j.cell.2019.05.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stzepourginski, I., Nigro, G., Jacob, J. M., Dulauroy, S., Sansonetti, P. J., Eberl, G. and Peduto, L. (2016). CD34+ mesenchymal cells are a major component of the intestinal stem cells niche at homeostasis and after injury. Proc. Natl. Acad. Sci. USA 114, E506-E513. 10.1073/pnas.1620059114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takada, R., Satomi, Y., Kurata, T., Ueno, N., Norioka, S., Kondoh, H., Takao, T. and Takada, S. (2006). Monounsaturated fatty acid modification of Wnt protein: its role in Wnt secretion. Dev. Cell 11, 791-801. 10.1016/j.devcel.2006.10.003 [DOI] [PubMed] [Google Scholar]
- Tamai, K., Semenov, M., Kato, Y., Spokony, R., Liu, C., Katsuyama, Y., Hess, F., Saint-Jeannet, J.-P. and He, X. (2000). LDL-receptor-related proteins in Wnt signal transduction. Nature 407, 530-535. 10.1038/35035117 [DOI] [PubMed] [Google Scholar]
- Valenta, T., Degirmenci, B., Moor, A. E., Herr, P., Zimmerli, D., Moor, M. B., Hausmann, G., Cantù, C., Aguet, M. and Basler, K. (2016). Wnt ligands secreted by subepithelial mesenchymal cells are essential for the survival of intestinal stem cells and gut homeostasis. Cell Rep. 15, 911-918. 10.1016/j.celrep.2016.03.088 [DOI] [PubMed] [Google Scholar]
- van de Wetering, M., Sancho, E., Verweij, C., de Lau, W., Oving, I., Hurlstone, A., van der Horn, K., Batlle, E., Coudreuse, D., Haramis, A.-P.et al. (2002). The β-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell 111, 241-250. 10.1016/S0092-8674(02)01014-0 [DOI] [PubMed] [Google Scholar]
- van Es, J. H., Haegebarth, A., Kujala, P., Itzkovitz, S., Koo, B.-K., Boj, S. F., Korving, J., van den Born, M., van Oudenaarden, A., Robine, S.et al. (2012). A critical role for the Wnt effector Tcf4 in adult intestinal homeostatic self-renewal. Mol. Cell. Biol. 32, 1918-1927. 10.1128/MCB.06288-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallingford, J. B. and Habas, R. (2005). The developmental biology of Dishevelled: an enigmatic protein governing cell fate and cell polarity. Development 132, 4421-4436. 10.1242/dev.02068 [DOI] [PubMed] [Google Scholar]
- Wehrli, M., Dougan, S. T., Caldwell, K., O'Keefe, L., Schwartz, S., Vaizel-Ohayon, D., Schejter, E., Tomlinson, A. and DiNardo, S. (2000). arrow encodes an LDL-receptor-related protein essential for Wingless signalling. Nature 407, 527-530. 10.1038/35035110 [DOI] [PubMed] [Google Scholar]
- Willert, K. and Nusse, R. (2012). Wnt proteins. Cold Spring Harb. Perspect. Biol. 4, a007864. 10.1101/cshperspect.a007864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willert, K., Brown, J. D., Danenberg, E., Duncan, A. W., Weissman, I. L., Reya, T., Yates, J. R. and Nusse, R. (2003). Wnt proteins are lipid-modified and can act as stem cell growth factors. Nature 423, 448-452. 10.1038/nature01611 [DOI] [PubMed] [Google Scholar]
- Wu, C.-H. and Nusse, R. (2002). Ligand receptor interactions in the Wnt signaling pathway in Drosophila. J. Biol. Chem. 277, 41762-41769. 10.1074/jbc.M207850200 [DOI] [PubMed] [Google Scholar]
- Yan, K. S., Janda, C. Y., Chang, J., Zheng, G. X. Y., Larkin, K. A., Luca, V. C., Chia, L. A., Mah, A. T., Han, A., Terry, J. M.et al. (2017). Non-equivalence of Wnt and R-spondin ligands during Lgr5(+) intestinal stem-cell self-renewal. Nature 545, 238-242. 10.1038/nature22313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, S., Tong, K., Zhao, Y., Balasubramanian, I., Yap, G. S., Ferraris, R. P., Bonder, E. M., Verzi, M. P. and Gao, N. (2018). Paneth cell multipotency induced by notch activation following injury. Cell Stem Cell 23, 46-59.e45. 10.1016/j.stem.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, S., Balasubramanian, I., Laubitz, D., Tong, K., Bandyopadhyay, S., Lin, X., Flores, J., Singh, R., Liu, Y., Macazana, C.et al. (2020). Paneth cell-derived lysozyme defines the composition of mucolytic microbiota and the inflammatory tone of the intestine. Immunity 53, 398-416.e398. 10.1016/j.immuni.2020.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., Bandyopadhyay, S., Araujo, L. P., Tong, K., Flores, J., Laubitz, D., Zhao, Y., Yap, G., Wang, J., Zou, Q.et al. (2020). Elevating EGFR-MAPK program by a nonconventional Cdc42 enhances intestinal epithelial survival and regeneration. JCI Insight 5, e135923. 10.1172/jci.insight.135923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, W. Y., Blutt, S. E., Zeng, X. L., Chen, M. S., Lo, Y. H., Castillo-Azofeifa, D., Klein, O. D., Shroyer, N. F., Donowitz, M. and Estes, M. K. (2018). Epithelial WNT ligands are essential drivers of intestinal stem cell activation. Cell Rep. 22, 1003-1015. 10.1016/j.celrep.2017.12.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.