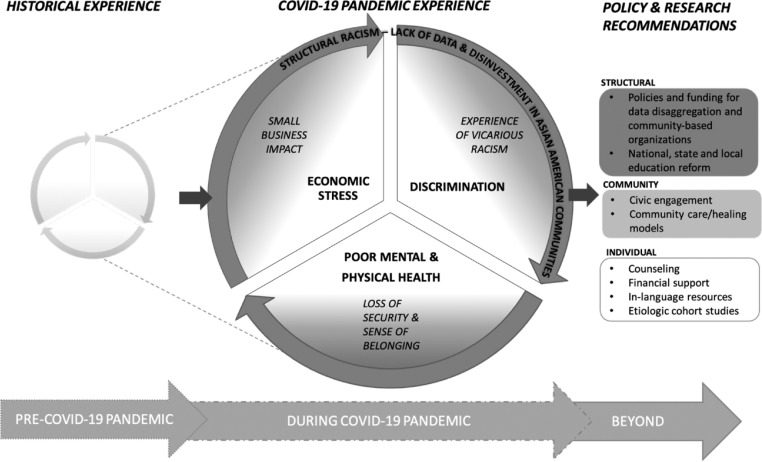
COVID-19 has negatively impacted communities across the United States and globally – exposing health, social, and economic inequities for many racialised and minoritised groups, including Asian Americans. Recent research suggests that due to lower testing rates and greater disease severity at hospital admittance, Asian Americans have higher excess all-cause mortality and COVID-19 case-fatality than non-Hispanic White Americans.1 Asian Americans, particularly those less-educated, also experienced more job loss and were slower to regain employment compared to all other US racial groups.2 Such impacts have been experienced in the context of surging anti-Asian racism, where almost half of hate incidents included anti-China or anti-immigrant rhetoric.3 To effectively mitigate the long-term impacts of the pandemic on health in Asian American communities, we must contextualize and intervene in concerted efforts, recognizing new threats as well as pre-existing threats that have been exacerbated during the pandemic. Thus, we propose a Syndemic Framework to understand Asian American health in the context of COVID-19 that account for the interrelatedness, interaction and synergy of threats that disproportionately impact Asian Americans, and which are driven by structural racism (Figure 1). Structural racism is defined as a system of policies, norms, and practices that reinforce racial inequities. An example of structural racism is the perpetual lack of or poor-quality disaggregated data on Asian Americans in research and policymaking, which results in an inability to reveal existing health inequities.
Figure 1.
Syndemic framework to understand Asian American Health in the context of COVID-19.
Our Syndemic Framework is informed by Singer's Syndemic approach,4 which refers to compounding and exacerbating adverse effects from the interactions of health conditions with pre-existing “inequality caused by poverty, stigmatization, stress, or structural violence.”5 These structural inequities have long impacted Asian Americans, particularly those with liminal legal status, and with family histories of displacement, colonization, and imperialism. Despite these pre-existing inequalities, re-imagination of Asian Americans as the model minority is a form of structural racism specific to Asian Americans that contributes to inequities by suggesting that Asian Americans are a homogeneous group who do not experience problems comparable to other communities of color.6 This myth reinforces and is reinforced by inadequate and poor-quality data on Asian Americans, which in turn impacts resource allocation to support community health, including linguistically- and culturally-appropriate health care.7
Within the context of structural racism, COVID-19 has magnified multiple threats, including anti-Asian discrimination and violence, economic challenges, and health and mental health challenges, due to the focus on individual behaviors to reduce health inequalities and failure to address known social determinants of health before the COVID-19 pandemic. These interrelated challenges and the need for a Syndemic Framework are illustrated through findings from our Asian American and Native Hawaiian/Pacific Islander COVID-19 Needs Assessment Project,8 which was conducted with 3,726 Asian Americans between January-April 2021 to examine impacts of the pandemic and needs of Asian American communities. For example, individuals who experienced anti-Asian discrimination were 2.09 times (95% CI: 1.45–3.02) more likely to endorse psychological distress than those who did not face discrimination, even after accounting for pandemic-related stressors like food access and income loss; Asian Americans earning $25,000 or less reported 14 times more food insufficiency than those earning $150,000 or more (11.4% vs. 0.8%); and Asian-language respondents were more likely to report anxiety about job loss due to their race/ethnicity compared to English-language respondents.
This syndemic of COVID-19 and anti-Asian racism expands to increased experiences of vicarious racism and negative impacts on Asian American-owned small businesses, and decreased sense of security and belonging, which will have long-term consequences on the health of Asian Americans. Based on our Syndemic Framework, we recommend the following multi-level and multi-dimensional research and policy actions:
-
(1)
At the structural level, we need national, state, and local reform to comprehensively change the policies and practices that perpetuate structural and interpersonal racism. For example, policy for meaningful inclusion of Asian Americans in administrative data, the availability of disaggregated data, and more standardization of health materials and information in multiple languages are necessary. However, policy alone is insufficient. Funding is needed to overhaul these data systems and modify community participatory data collection practices to understand how these data should be collected and why Asian Americans should trust systems seeking these data.
-
(2)
At the community level, we recommend advancing community models that promote healing and resilience; and that center community and cultural values and practices. Given structural factors such as limited numbers of linguistically and culturally appropriate providers, and cultural factors such as shame and stigma about seeking Westernized mental health care,9 community-based programs that promote holistic wellness, such as cooking, gardening, and cultural movement like tai chi, can supplement other healthcare services.
-
(3)
At the individual- and family- level, more funding is needed to support the economic, health, and mental health recovery of those Asian Americans who have been most impacted by the syndemic. Funding should be directed towards trusted brokers in the community – such as community-based and faith-based organizations.
-
(4)
More research, in partnership with communities, is needed to identify the nuanced sociocultural etiology of health inequities stemming from systemic racism and discrimination; and to address the current mental health crisis amongst Asian Americans.
These proposed actions are to mitigate negative syndemic impacts, to improve the visibility of Asian Americans across all sectors including public health; and to increase solidarity and trust among Asian Americans and with other marginalized communities. Our Syndemic Framework can be used to better address the historically-embedded complex threats Asian Americans are facing. Failure to address the multitude of health and economic challenges, as inextricably tied to anti-Asian racism and reinforced by structural racism, through policy change and research will exacerbate health inequities in Asian American and other communities now and in the future.
Declaration of interests
No authors have conflicts of interest.
Funding
This publication is supported in part by Ford Foundation, JPB Foundation, W.K. Kellogg Foundation, California Endowment, Weingart Foundation, and California Wellness Foundation through the fiscal sponsorship of the National Urban League to the Asian American Psychological Association. The preparation of this manuscript was supported in part by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (NIMHD) Award Number U54MD000538, National Institute on Drug Abuse (NIDA) Award Number 3R01DA036749 - 05S1, National Heart, Lung, Blood Institute (NHLBI) Community Engagement Alliance (CEAL) Non-Federal 1OT2HL156812–01, Westat Sub-OTA No: 6793–02-S013, U.S. Department of Health & Human Services, Centers for Disease Control and Prevention (CDC) Award Numbers NU38OT2020001477, CFDA number 93.421 and 1NH23IP922639–01–00, CFDA number 93.185. LÐ is funded by the NIH Resource Centers for Minority Aging Research (RCMAR) Award Number 5P30AG059302. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the funders. No funders had any role in the writing of the manuscript or the decision to submit it for publication. No authors were paid to write this article by any company or agency. All authors accept responsibility to submit for publication.
References
- 1.Yan B.W., Hwang A.L., Ng F., Chu J.N., Tsoh J.Y., Nguyen T.T. Death toll of COVID-19 on Asian Americans: disparities revealed. J Gen Intern Med. 2021 doi: 10.1007/s11606-021-07003-0. Epub 2021/08/05PubMed PMID: 34347256; PubMed Central PMCID: PMCPMC8335981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim A.T., Kim C., Tuttle S.E., Zhang Y. COVID-19 and the decline in Asian American employment. Res Soc Stratif Mobil. 2021;71 doi: 10.1016/j.rssm.2020.100563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yellow Horse A.J, Jeung R, Tang B, et al. Stop AAPI Hate National Report 3/19/20-6/30/21. 2021.
- 4.Singer M. John Wiley & Sons; 2009. Introduction to Syndemics: A Critical Systems Approach to Public and Community Health. [Google Scholar]
- 5.Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–950. doi: 10.1016/s0140-6736(17)30003-x. [DOI] [PubMed] [Google Scholar]
- 6.Yi S.S., Doan L.N., Choi J.K., et al. With no data, there's no equity: addressing the lack of data on COVID-19 for Asian American communities. Lancet eClinicalMedicine. 2022 doi: 10.1016/j.eclinm.2021.101165. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park S., Stimpson J.P., Pintor J.K., et al. The effects of the affordable care act on health care access and utilization among Asian American subgroups. Med Care. 2019;57(11):861–868. doi: 10.1097/mlr.0000000000001202. PubMed PMID: 00005650-201911000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Saw A, Doan LN, Takeuchi DT, et al. Asian American and native Hawaiian/Pacific islander COVID-19 needs assessment. 2021.
- 9.Okazaki S., Kassem A.M., Tu M.C. Addressing Asian American mental health disparities: putting community-based research principles to work. Asian Am J Psychol. 2014;5(1):4–12. doi: 10.1037/a0032675. PubMed PMID: 2014-12688-002. [DOI] [Google Scholar]