Abstract
Background:
Cigarette smokers report increases in smoking urge in response to exposure to electronic nicotine delivery systems (ENDS) and dual users, i.e. smokers who also vape ENDS, may exhibit greater cue reactivity than exclusive smokers. The current investigation examined reactivity to a variety of ENDS cues across a large sample of cigarette smokers and dual ENDS users.
Methods:
Young adult smokers (N = 345; ≥5 cigarettes per day) were recruited between 2013–2019 for participation in a series of within-subjects laboratory-based studies. Participants completed surveys before and after exposure to a confederate-delivered control cue (water) and an active cue, including cigarette or ENDS cues ranging from first generation “cigalikes” to a fourth generation “pod-mod”. Main outcomes were post-cue changes in desire for combustible cigarettes and e-cigarettes, and smoking behavior as determined by the smoking latency portion of the Smoking Lapse Paradigm after cue exposure.
Results:
Relative to smokers who do not use ENDS, dual users demonstrated higher baseline desire for ENDS and greater ENDS cue reactivity (across product types) in terms of post-cue increases in smoking urge and shorter latency to smoking choice. In contrast, reactivity to the cigarette cue was similar across groups.
Conclusions:
Dual users show heightened ENDS cue reactivity on smoking urge and behavior relative to never users of ENDS, regardless of the type of ENDS cue. Given their reactivity to both cigarette and ENDS cues, it may be difficult for dual users to transition to exclusive vaping or quit tobacco product use altogether.
Keywords: Electronic Nicotine Delivery Systems (ENDS), Electronic Cigarettes (E-Cigarettes), Dual Use, Smoking, Craving
1. Introduction
Over the past decade, the increasing prevalence of the use of electronic nicotine delivery systems (ENDS), also known as electronic cigarettes (e-cigarettes), has raised a significant public health debate (Helen & Eaton, 2018; Dai & Leventhal, 2019). If ENDS offer a less harmful method of nicotine delivery than smoking combustible cigarettes and do not adversely affect smoking cessation, there may be a net public health benefit, but if their use poses long-term health risks and/or drives the initiation and maintenance of tobacco product use in youth and young adults, then ENDS represent a public health burden (Lee et al., 2018; Barrington-Trimis et al. 2016). An important consideration is the possibility that ENDS may provide a more accessible means of nicotine delivery than combustible cigarettes, for example, by allowing smokers to get a nicotine dose in places where smoking is banned, thus facilitating a transition to “dual use,” defined as co-use of cigarettes and ENDS (Zhuang et al., 2016). Of concern is that relative to exclusive ENDS users and smokers, dual users perceive less danger from vaping but may incur more overall adverse health effects (Cooper et al., 2017; Rass et al., 2015; Kim et al., 2015; Wang et al., 2018).
Relevant to the issue of dual use is that ENDS use closely resembles combustible smoking in terms of analogous hand-to-mouth movements, inhalation and exhalation behaviors, and production of exhaled aerosols that resemble smoke. Currently unknown, however, is the extent to which those closely-aligned aspects of ENDS use to traditional smoking affect dual users. Whereas there is a growing body of literature examining the physiological and psychological effects of vaping, there has been a paucity of research focusing on the effects of vaping in persons who are passively exposed to ENDS use. Our research group has conducted several studies in this area and we have consistently demonstrated that passive exposure to the use of a variety of ENDS and heated tobacco products evokes acute increases in both the desire to smoke and vape in young adult smokers (King et al., 2016; King et al., 2018; Vena et al., 2019; Vena et al., 2020b; Brett et al., 2021). Of note, ENDS’ elicititation of desire to smoke is seen in devices that more closely resemble combustible cigarettes (King et al., 2015) as well as larger tank devices that are visually distinct from cigarettes (Vena et al., 2020a). Others have observed cue-specific craving among dual users in response to combustible and electronic cigarettes, but without evidence of cross-cue reactivity when active cues were interspersed with control cues across multiple trials (Dowd & Tiffany, 2019). As over a quarter of smokers also use ENDS (Owusu et al., 2019), elucidating potential mechanisms that underlie dual use behavior is essential. It is possible that, relative to exclusive smokers, dual users may be more susceptible to the motivational salience of ENDS as cues that evoke urges for both cigarettes and e-cigarettes. Further, as device types continue to evolve in both appearance and functionality the question of which devices elicit urges to smoke in observers remains relevant. This cue sensitivity may be clinically significant as it could conceivably propel concomitant smoking and vaping behavior and make it more difficult to eventually reduce or quit tobacco use. Examination of the role of recent or lifetime vaping among smokers as an individual difference factor in ENDS cue reactivity has not been possible due to sample size limitations in our prior investigations.
Thus, the present study aimed to overcome the aforementioned limitation by aggregating data across five previous studies to examine reactivity to ENDS cues in smokers with varying levels of co-occurring ENDS use. We predicted ENDS cue reactivity, in terms of e-cigarette and cigarette desire, would be stronger in current (past month) dual users than in lifetime (>1 year) or never users of ENDS. Our secondary goal was to examine whether the use of smaller, non tank-based ENDS (e.g., cigalike and JUUL) would elicit greater cue reactivity than tank-based, larger ENDS with less resemblance to cigarettes (vape pens and mods).
2. Methods
2.1. Design
Data were combined across five within-subject human laboratory studies conducted in young adult smokers between 2013–2018. The total number of participants was N=345. Study protocols were identical across studies with the only differences being the type of ENDS cue delivered and inclusion of a smoking latency task in four of the five studies. Participants were tested individually in controlled laboratory sessions to examine responses to a confederate-delivered control cue followed by an active cue, i.e., confederate using an e-cigarette (n=264; Vena et al., 2019; Vena et al., 2020a; Vena et al., 2020b) or combustible cigarette (n=81; King et al., 2015; King et al., 2018). Cue delivery was conducted within an ecologically-valid social interaction to mimic real-world exposures to products.
2.2. Participants
Candidates were recruited via online advertisements with the study masked as an examination of “moods, behaviors, and social interactions” to reduce selection bias and expectancy about exposure to cues. Participants were debriefed on the actual purpose upon study completion. Inclusion criteria were: 18–35 years of age, daily smoking (5–30 cigarettes/day), not currently attempting to quit smoking, no prior participation in our studies, English fluency, and no major physical or mental disorders or hearing or visual impairments that would hinder participation.
Eligibility was determined without regard to past ENDS use history to avoid biasing the sample. Consistent with prior investigations (Owusu et al., 2019), four ENDS use subgroups were derived. Among participants exposed to ENDS cues, these included: past-month dual users (n=65; reporting ENDS use in the past 30 days), past-year dual users (n=97; ENDs use > 30 days and ≤ one year ago), lifetime users (n=52; ENDS use > one year ago), and never users (n=50; denied any prior ENDS use). The same criteria was applied to participants exposed to cigarette cues and included past-month dual users (n=18), past-year dual users (n=35), lifetime users (n=10), and never users (n=18).
2.3. Procedure
Individuals meeting initial inclusion criteria on the telephone screen were invited to an in-person screening. They were instructed to abstain from alcohol and recreational drugs for ≥24 hours and cigarette smoking for ≥1 hour. The screening consisted of informed consent, verbal confirmation of recent abstinence, and assessment of demographic, health, and substance use behaviors. Candidates completed questions about smoking history and cigarette preference, including the Fagerström Test for Nicotine Dependence (FTND; Heatherton et al., 1991), a timeline follow-back calendar for past month estimates of smoking (Sobell & Sobell, 1992), scales for negative affect [Beck Depression Inventory (BDI); Beck et al., 1961; State-Trait Anxiety Inventory (STAI-Trait); Spielberger, 1970] and alcohol drinking (AUDIT; Babor et al., 2001). They also underwent breath tests for alcohol (BrAC=<.003; three candidates were disqualified for exceeding that threshold) and expired air carbon monoxide (< 40 ppm) as a general indicator to support self-reported time since last cigarette (McKee, 2009; Pang & Leventhal, 2013; Drobes & Tiffany, 1997). Ninety-four percent of screened candidates across all studies were deemed eligible and agreed to partake in the two hour study session. The studies were approved by the University of Chicago Institutional Review Board and sessions were conducted in comfortable, living room-like rooms in the Clinical Addictions Research Laboratory at the University of Chicago.
The session commenced with baseline surveys (for details, see Dependent Measures) followed by introducing the participant to the study confederate, i.e., a hired lab member who portrayed the role of another study participant. After the introduction, the research assistant informed them that they would each be assigned a randomized task, i.e., eating, drinking, smoking/vaping, having a conversation, or viewing pictures, by choosing one card from a small stack of about 6 cards. The participant always chose first, and the presentation of cards was rigged so that the conversation task was selected. The confederate would then choose a card, seemingly at random, but, outside the view of the participant, the assistant slipped in a card in the left position that the confederate appeared to randomly choose and this card always had the task of drinking water.
The second task followed a similar procedure, with the participant seemingly randomly choosing a card with conversation again as his/her task, and the confederate selecting the added card (unbeknownst to the participant) with either smoking or vaping as the task, depending on the study. For both first and second tasks, the conversation task was facilitated by the research assistant asking the participant to choose from a short list of topics (favorite tv shows or movies, pets, weather, etc.) and providing a card with suggested conversation starters to facilitate the interaction. The confederate was told for both tasks to drink/smoke/vape as much or as little as they liked during that period, but actually the confederate was pre-trained to deliver the cue about 8–10 times in a natural way during the conversation. Surveys were repeated immediately after the first and second tasks as well as in a final administration 20-minutes post second task after a brief rest period.
After the cue phase, in four of the five studies (King et al., 2018; Vena et al., 2019; Vena et al., 2020a; Vena et al., 2020b), the participant underwent a 50-minute smoking latency task from the Smoking Lapse Paradigm (McKee, 2009). They were presented with a tray with a cigarette of their preferred brand (including menthol vs non), a lighter, and a doorbell to ring if they chose to smoke, else receive $0.20 for every five minutes of refraining (Pang & Leventhal, 2013). The instructions included that this last portion would be 50 minutes regardless of their choice to smoke or not. Consistent with prior studies (Vena et al., 2020a; Vena et al., 2020b; Pang & Leventhal, 2013), participants who did not smoke during the task were coded as 50 minutes (the maximum time value). Following the latency task, participants completed items on ENDS and other tobacco product use history. These questions were always presented at the end of the session to minimize focus on ENDS prior to the cue period.
Cues:
Study cues were delivered by a paid confederate trained on standardized cue delivery in a natural manner with the goal of 8–10 hand-to-mouth movements for each cue. The control cue was a non-branded 12 oz. water bottle and it was selected since it is a common oral consummatory behavior with frequent hand-to mouth movements similar to smoking but neutral in terms of smoking associations (King et al., 2015; Vena et al., 2019; Drboes & Tiffany, 1997). Products were used in real-time (e.g., confederates did vape the ENDS, drink the water, etc.) during all cue exposures. For the active cues, the ENDS product ranged from a 1st generation cigalike (King et al., 2015), 2nd generation vape pen (King et al., 2018), 3rd generation mod (Vena et al, 2019; Vena et al., 2020a), and 4th generation JUUL pod-mod (Vena et al., 2020b). The cigarette cue was a standard combustible cigarette (American Spirit, Camel, etc.). The ENDS product used for each study was based on primary user preferences at the time, and devices evolved rapidly over the span of this research program (Yingst et al., 2019).
2.4. Dependent Measures
The primary dependent measures were the Brief Questionnaire of Smoking Urges (BQSU) total score and visual analogue scale (VAS) items of desire for “a cigarette (your preferred brand)” and “an electronic cigarette” each rated from ‘not at all’ (0) to ‘most ever’ (100; Cox et al., 2001). The primary variable from the behavioral smoking task was number of minutes (i.e., latency) to smoke.
2.5. Statistical Analyses
Analyses were conducted in 2020. Participant demographics and smoking background variables were compared across the four subgroups using ANOVA or Chi-Square tests, as appropriate. Generalized estimating equations (GEE) models were employed on the three main outcomes and examined group, time, and their interactions. Signficant effects were examined via post-estimation tests with p-values corrected by Bonferroni methods for multiple comparisons. The analyses were conducted separately for responses to the ENDS and cigarette cues, and included covariates that differed across the subgroups. Smoking latency after the ENDS cues was examined by a Cox Proportional-Hazards model for survival analysis. Notably, the latency task was conducted in 138 participants after the ENDS cue phase and in 12 particpants after the cigarette cue phase, thus, for the latter, a survival analysis could not be done due to the small sample size.
3. Results
Participant (N=264) characteristics across the four subgroups exposed to the ENDS cues are presented in Table 1. The groups differed on age, education, and race, but not sex, ethnicity, sexual orientation, negative affect (BDI, STAI-Trait), or alcohol drinking (AUDIT). The groups did not differ on smoking background; overall, participants smoked slightly less than a half pack of cigarettes per day on average and had moderate/low nicotine dependence. Baseline cigarette urge and desire (i.e., craving at the start of the experimental sessions) did not differ across the groups and was generally in the moderate range. In contrast, baseline e-cigarette desire was significantly higher in past-month dual users versus all other groups, and also higher in past-year dual users than lifetime or never ENDS users. Background characteristics across the groups in the 81 participants exposed to the cigarette cue are presented in the appendix. They were similar to participants exposed to ENDS cues and the only variable that differed across subgroups was sex, with lifetime ENDS users having a higher percentage of females compared with the other groups.
Table 1.
Group Characteristics and Smoking Background
| Never (N) | Lifetime (L) | Past Year (PY, | P.st Month (PM) | P | |
|---|---|---|---|---|---|
|
| |||||
| Demographics: | |||||
| Sample Size | 50 | 52 | 97 | 65 | |
| Age (Yr) | 28.2 (.65) | 27.2 (.58) | 27.4 (.47) | 25.5 (.56) | 0.009 |
| Education (Yr) | 13.2 (.28) | 13.6 (.24) | 14.3 (.21) | 14.0 (.21) | 0.007 |
| Sex (% male)a | 29 (60%) | 20 (38%) | 59 (61%) | 34 (52%) | 0.053 |
| Race: | |||||
| White | 12 (24%) | 27 (52%) | 39 (40%) | 31 (48%) | |
| Black | 32 (64%) | 19 (37%) | 34 (35%) | 16 (25%) | |
| Other | 6 (12%) | 6 (12%) | 24 (25%) | 18 (28%) | <0.001 |
| Ethnicity (% Hispanic) | 4 (8%) | 6 (12%) | 11 (11.3%) | 13 (20.0%) | 0.232 |
| Sexual Orientation (% Heterosexual) | 33 (89%) | 32 (70%) | 47 (64%) | 35 (74%) | 0.162 |
| BDI | 6.8 (1.26) | 9.4 (1.21) | 8.2 (.86) | 7.4 (.82) | 0.401 |
| STAIT | 43.9 (1.30) | 42.5 (1.25) | 43.0 (.94) | 43.0 (1.15) | 0.887 |
| AUDIT | 8.6 1.17) | 7.8 (.85) | 8.6 (.69) | 8.8 (.82) | 0.865 |
| Smoking Patterns and use: | |||||
| Cigarettes smoked per day | 8.4 (.62) | 10.3 (.68) | 9.3 (.56) | 8.7 (.59) | 0.240 |
| FTND | 4.1 (.38) | 4.1 (.28) | 3.9 (.23) | 3.6 (.32) | 0.639 |
| Menthol Preference | 33 (67%) | 38 (73%) | 51 (54%) | 39 (67%) | 0.276 |
| Hours since last reported cigaretteb | 1.8 (.97) | 2.1 (.81) | 2.1 (.71) | 3.8 (1.4) | 0.089 |
| CO (ppm)b | 11.0 (12.0) | 10.0 (10.0) | 11.0 (13.0) | 7.0 (9.0) | 0.015 |
| Baseline Craving: | |||||
| BQSU | 41.5 (1.76) | 40.1 (1.38) | 43.0 (1.11) | 42.3 (1.41) | 0.494 |
| Cigarette Desire | 65.5 (3.56) | 63.0 (2.66) | 63.0 (2.66) | 65.5 (2.69) | 0.858 |
| E-Cigarette Desire | 6.4 (1.82) | 9.3 (2.29) | 9.3 (2.29) | 35.4 (3.31) | <0.001 |
Note. Groups are shown by ENDS use status; never, lifetime, past year, and past month users. Values are Mean (SEM) or N (%), as indicated. Variables were compared between groups with Student’s t test or chi-square as appropriate.
Sex assigned at birth, by participant self-report; AUDIT= Alcohol Use Disorders Identification Test.
CO and Hours since last reported cigarette values are medians due to non-normal distribution, and compared via Kruskal-Wallis test. CO=Carbon Monoxide; FTND=Fagerström Test for Nicotine Dependence.
The main results of subjective responses to the ENDS cues are displayed in Figure 1. For BQSU smoking urge, there was a group by time interaction [χ2(9)=27.5, p<0.001] such that the ENDS cues produced increases in smoking urge in all subgroups except for ENDS never users. These smoking urge increases were relative to the baseline and water cue response and observed at both the immediate and 20-minute post ENDS cue intervals (post-estimation tests, ps<0.05; Figure 1A). For cigarette desire in reponse to the ENDS cues, there was a main effect of time [χ2(3)=178.4, p<0.001], with the ENDS cues producing increases at both post-cue intervals across the subgroups (Figure 1B), with no group by time interaction [χ2(9)=9.11, p=0.427].
Figure 1. Smoking urge, cigarette and e-cigarette desire response to ENDS cues across groups.
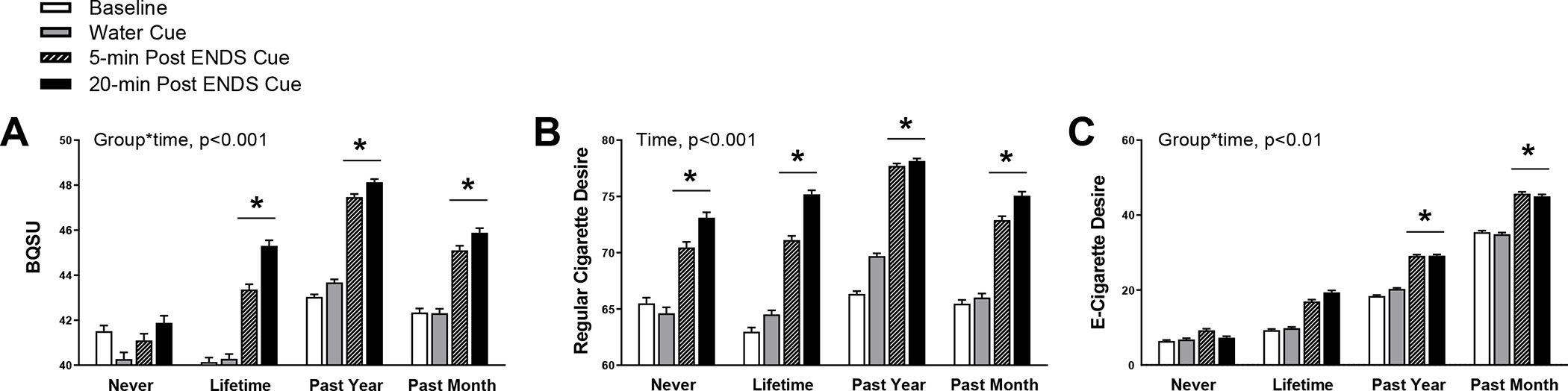
Data are Mean ± SEM. Subjective ratings of smoking urge (A), cigarette desire (B), and e-cigarette desire (C) occurred on a visual analog scale ranging from 0–100. The time points include baseline, 5 minutes following delivery of a water cue, and 5 and 20 minutes after delivery of the vaping cue. *p < 0.05 for 5-min=20-min > Baseline=Water cue
For e-cigarette desire, past-month dual users reported the greatest desire across all time points, followed by past-year dual users, lifetime users, and never users [group: χ2(3)=63.5, p<0.001]. There was also a significant group by time interaction [χ2(9)=22.43, p<0.01] such that the ENDS cues significantly increased e-cigarette desire relative to baseline and water cue response at both post-cue intervals (post-estimation tests, ps<0.05; Figure 1C) in all subgroups except for never users.
The aforementioned analyses were repeated with ENDS product type (tank-based vs. non-tank based) included as a covariate and all main effects and interactions remained significant. ENDS product type did not influence cigarette desire or BQSU smoking urge responses (ps>0.46 for main effects and interactions) but did affect e-cigarette desire such that the non tank-based products produced higher e-cigarette desire than tank-based products [χ2(1)=4.06, p<0.05] for all subgroups [group × cue type, χ2(3)=0.29, p=0.961].
Subjective responses in participants exposed to the cigarette cue are displayed in Figure 2. The cigarette cue significantly increased both smoking urge (BQSU) and desire for a cigarette at both post-cue time points and across all subgroups [BQSU, time: (χ2(3)=69.8, p<0.001; cigarette desire, time: (χ2(3)=43.8, p<0.001; post-estimation tests, p<.05; Figures 2A, 2B]. Overall e-cigarette desire was higher in past-month dual users compared with all other groups [group: χ2(3)=31.2, p<0.001; post-estimation tests, p<.05; Figure 2C], but the cigarette cue did not evoke increases in this measure for any of the subgroups.
Figure 2. Smoking urge, cigarette and e-cigarette desire response to the cigarette cue across groups.
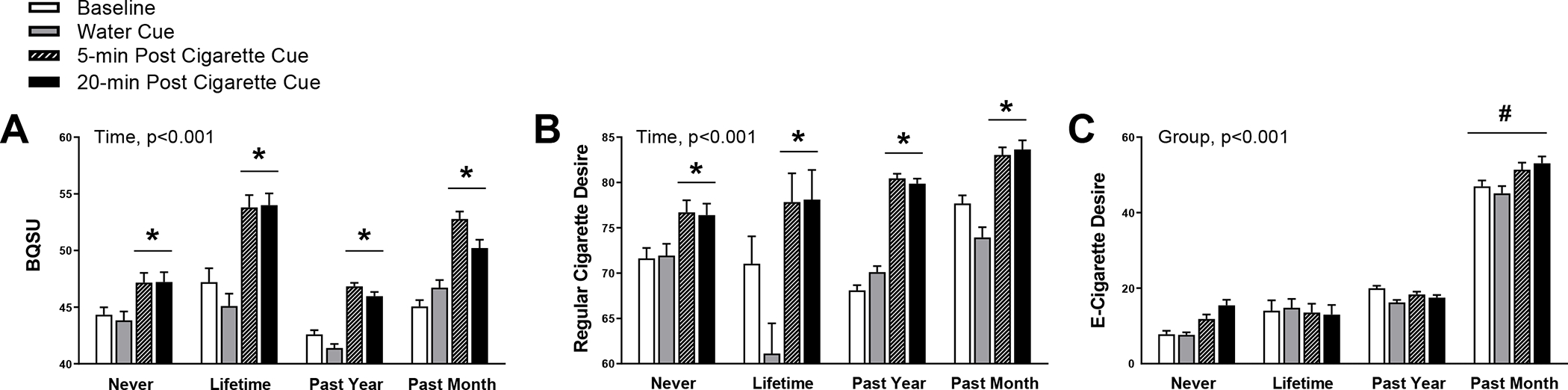
Data are Mean ± SEM. Subjective ratings of smoking urge (A), cigarette desire (B), and e-cigarette desire (C) occurred on a visual analog scale ranging from 0–100. The time points include baseline, 5 minutes following delivery of a water cue, and 5 and 20 minutes after delivery of the vaping cue. *p < 0.05 for 5-min=20-min > Baseline=Water cue; #p < 0.05 for past month > past year=lifetime=never
Finally, for smoking behavior, Figure 3 depicts the Kaplan-Meier estimate of survival function for time to smoke (smoking latency) in response to the ENDS cues across the subgroups. The Cox Hazard Model indicated that the ENDS cues produced shorter latencies to smoke in past-month dual users [Hazard ratio = 3.11 (1.43 SE), p=.014] and past-year dual users [Hazard ratio = 2.67 (1.34 SE), p=.035)] relative to never users of ENDS.
Figure 3. Kaplan-Meier survival estimates.
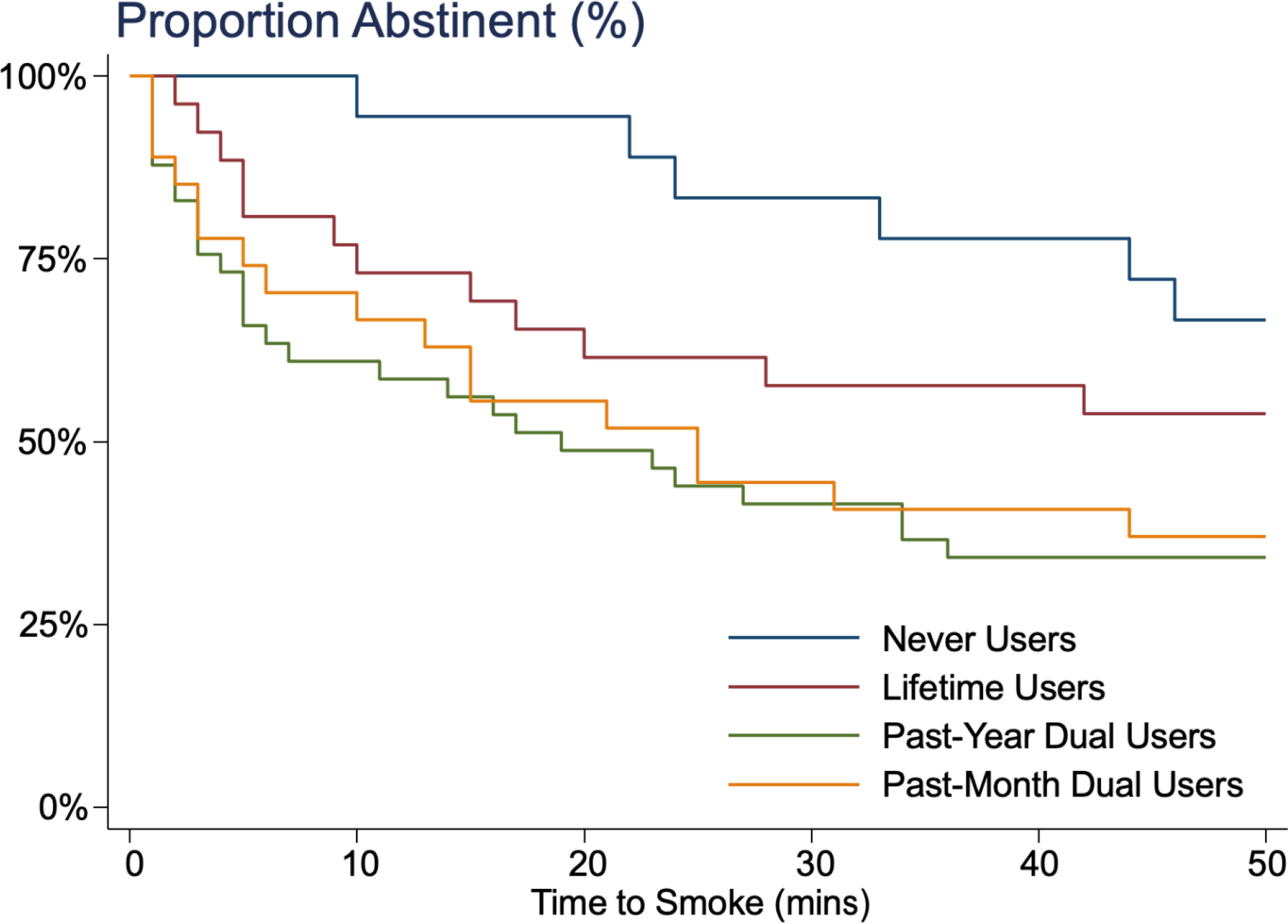
Survival function for smoking latency (time to smoke) from a Cox Hazard Model in 138 participants who underwent the latency portion of the Smoking Lapse Paradigm twenty minutes after the ENDS cue phase finished. Subgroups included ENDS never users (n=24), lifetime users (n=29), past-year dual users (n=51), and past-month dual users (n=34). The ENDS cues produced shorter latencies to smoke in past-month and past year dual users (ps<.05) relative to never users.
4. Discussion
Findings supported the hypothesis that dual users show heightened ENDS cue reactivity as evidenced by greater increases in smoking urge and smoking behavior relative to cigarette smokers who never used ENDS. This higher sensitivity to ENDS cues was evident in dual users who vaped both in the past month as well as the past year and observed across all ENDS product type cues, including cigalikes, vape pens, mods, and JUUL. Dual users also exhibited more sensitivity to ENDS cues in evoking e-cigarette desire; this was particularly notable as they already exhibited higher baseline e-cigarette desire than lifetime or never ENDS users. In addition to heightened ENDS cue reacitvity, dual users were similarly highly sensitive to combustible cigarette cues as non-dual users. Taken together, this is the first study, to our knowledge, to examine smokers across a range of ENDS use patterns and results demonstrate that dual users are at a particular disadvantage when exposed to others’ smoking and vaping, as they exhibit pronounced increases in smoking urge and behavior and higher baseline e-cigarette desire that is potentiated after such exposures.
Dual users’ heightened sensitivity to ENDS cues has important implications for understanding mechanisms underlying dual use and extrapolation to real-life exposures. While dual users may have variable access to their personal products (cigarettes and/or ENDS), they are also likely exposed to product use in certain environmental exposures and these vary in predictability, intensity, and/or duration. Thus, we may speculate that dual users, compared with smokers who do not vape, may be more prone to surges in cigarette (or nicotine) craving due to the prevalence of passive exposures to ENDS. This could negatively impact an attempt to be tobacco-free as the dual user may be vulnerable to smoke, as shown in the present study’s latency to smoke data, or use an ENDS product, if available, in order to relieve cue-induced desire to smoke or vape, thus potentially hampering a quit attempt. As the studies were cross-sectional in nature, whether enhanced sensitivity to ENDS cues was pre-morbid or developed as the result of dual use cannot be discerned. However, as a minority of dual users successfully transition from dual use to exclusive vaping or abstinence from tobacco products (Coleman et al., 2019; Persokie et al., 2019), the proliferation of ENDS may decrease the odds of complete product switching and require additional intervention strategies for treatment success in dual users. Future work should examine this possible mechanism of dual use and weigh any impact of ENDS exposure with the potential net benefit of ENDS for smoking harm reduction.
The present analysis is the first to examine craving responses to an ENDS cue in current smokers both with and without a history of e-cigarette use. Theoretically, these cues would not be expected to elicit an appetitive response in exclusive smokers, as shown by their lack of smoking urge response to ENDS cues, however, at the same time, they did show increased cigarette desire in response to the ENDS cues. This highlights that ENDS cues could be generalizable to elicit desire to smoke, even in smokers who have never used ENDS and regardless of the device type (i.e. cigalikes, vape pens, mods, JUUL, etc.). This may be due to ENDs sharing features of traditional smoking in termse of hand-to mouth movements and inhalation/exhalation behaviors. Alternatively, as cigarette desire was assessed using a single item measure and smoking urge assessed via the 10-item BQSU, different measures may be more or less sensitive to changes in cue-elicited craving (Cox et al., 2001; Kozlowski et al., 1996; West & Ussher 2010). Nevertheless, the ENDS cues, despite having evoked a increased desire for cigarettes in exclusive smokers, produced a significantly longer latency to initiate smoking, once the choice was given, relative to past-month or past-year dual users.
As shown in this analysis aggregating data across several studies, there was no evidence of cross-cue reactivity for the traditional cigarette cue, that is, cigarette smoking exposure did not evoke desire for e-cigarettes. This observation is supported by our prior work as well as recent work by Dowd and Tiffany (King et al., 2016; King et al., 2018; Dowd & Tiffany, 2019), who reported a reduction in e-cigarette craving in dual users exposed to a lit tobacco cigarette. Although this remains an emerging area of research, one hypothesis is that smoking is more finely ingrained and portrayed as a distinct behavior from ENDS use. As we are now entering the second decade of ENDS availability and product use world-wide, there may be more depictions and experiences of co-use that may conceivably affect cigarette cues cross-generalizing to e-cigarette vaping desire in the future.
4.2. Limitations
There are numerous strengths of the current study, including a large sample size across several investigations, a consistent lab paradigm used across studies that has shown reliability (McKee, 2009; Pang & Leventhal, 2013), and cue exposures that mimic those often encountered in the natural environment. Still, there are some limitations worth noting. First, control and active cues were presented in a fixed order with the control cue always preceeding the active cue. While temporal effects of reponses to the active versus control cue cannot be ruled out, fixed order is a common approach in cue reactivity studies and cue studies that have used between-subjects designs have shown similar effects (Vena et al., 2019; Sayette et al., 2001; Maloney et al., 2016). Second, as this investigation merged several prior studies, there were differences in ENDS products available and user preferences over time. Related, detailed data were not obtained on participants’ vaping history, intensity, and nicotine content. Also, the small sample size for participants exposed to the active comparison cue, traditional smoking, precluded analysis of smoking behavior (latency) to this condition. Finally, the current studies cannot address whether dual users would have chosen to use an ENDS over a combusted cigarette during the behavioral choice task, leaving the question of which product would be preferred after ENDS cue exposures.
Dual users exhibited substantial reactivity to ENDS cues such that exposure to ENDS, regardless of device type (i.e., cigalike, vape pen, tank-based mod, or JUUL) evoked desire for both ENDS and combustible cigarettes and increased smoking behavior. This study provides further evidence that dual users are a unique group with distinct mechanisms that underlie use behaviors compared with exclusive smokers or ENDS users. Still, exclusive smokers also responded to the ENDS cues, suggesting that cross-cue generalization may occur regardless of ENDS use history, raising concerns that widespread adoption and use of ENDS may negatively impact smoking cessation efforts. While use of ENDS may help some smokers reduce their use of combustible cigarettes (Hajek et al., 2019), dual users appear especially sensitive to the motivational salience of ENDS use, and this may impair their ability to resist smoking. Research employing translational, wide-ranging perspectives is needed to further elucidate the potential factors that underlie dual tobacco product use and inform targeted cessation interventions for those who wish to quit both ENDS and combustible smoking.
Supplementary Material
Highlights.
Smokers who also use electronic nicotine delivery systems (ENDS) are ‘dual users’
Past-year dual users show higher baseline ENDS desire than exclusive smokers
Reactivity to ENDS cues across product types was heightened in dual users
Cigarette cue produced similar smoking urge regardless of ENDS use patterns
ENDS cues produced greater smoking behavior in dual users vs. exclusive smokers
Role of Funding Source
This research was supported by NIDA (R01-DA044210). Salary support for EIB was provided by National Institutes of Health (T32-DA043469). The funding source had no role in any aspect of this research.
Footnotes
Conflict of Interest
Dr. King provides consultation with the Respiratory Health Association. The other authors have no declarations.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The alcohol use disorders identification test: Guidelines for use in. World Health Organization. Recuperado de https://apps.who.int/iris/handle/10665/67205. [Google Scholar]
- Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, Samet JM, Leventhal AM, & McConnell R (2016). E-cigarettes and future cigarette use. Pediatrics, 138(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An inventory for measuring depression. Archives of general psychiatry, 4(6), 561–571. [DOI] [PubMed] [Google Scholar]
- Brett EI, Miloslavich K, Vena A, Didier N, & King AC (2021). Effects of Visual Exposure to IQOS Use on Smoking Urge and Behavior. Tobacco Regulatory Science, 7(1), 31–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman B, Rostron B, Johnson SE, Persoskie A, Pearson J, Stanton C, Choi K, Anic G, Goniewicz ML, et al. , & Hyland A (2019). Transitions in electronic cigarette use among adults in the Population Assessment of Tobacco and Health (PATH) Study, Waves 1 and 2 (2013–2015). Tobacco control, 28(1), 50–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper M, Loukas A, Harrell MB, & Perry CL (2017). College students’ perceptions of risk and addictiveness of e-cigarettes and cigarettes. Journal of American College Health, 65(2), 103–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox LS, Tiffany ST, & Christen AG (2001). Evaluation of the brief questionnaire of smoking urges (QSU-brief) in laboratory and clinical settings. Nicotine & tobacco research, 3(1), 7–16. [DOI] [PubMed] [Google Scholar]
- Dai H, & Leventhal AM (2019). Prevalence of e-cigarette use among adults in the United States, 2014–2018. Jama, 322(18), 1824–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd AN, & Tiffany ST (2019). Comparison of tobacco and electronic cigarette reward value measured during a cue-reactivity task: an extension of the Choice Behavior Under Cued Conditions procedure. Nicotine and Tobacco Research, 21(10), 1394–1400. [DOI] [PubMed] [Google Scholar]
- Drobes DJ, & Tiffany ST (1997). Induction of smoking urge through imaginal and in vivo procedures: physiological and self-report manifestations. Journal of abnormal psychology, 106(1), 15. [DOI] [PubMed] [Google Scholar]
- Hajek P, Phillips-Waller A, Przulj D, Pesola F, Myers Smith K, Bisal N, et al. , & McRobbie HJ (2019). A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine, 380(7), 629–637. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, & Fagerstrom KO (1991). The Fagerström test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British journal of addiction, 86(9), 1119–1127. [DOI] [PubMed] [Google Scholar]
- Helen GS, & Eaton DL (2018). Public health consequences of e-cigarette use. JAMA internal medicine, 178(7), 984–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AE, Lee YO, Shafer P, Nonnemaker J, & Makarenko O (2015). Adult smokers’ receptivity to a television advert for electronic nicotine delivery systems. Tobacco control, 24(2), 132–135. [DOI] [PubMed] [Google Scholar]
- King AC, Smith LJ, Fridberg DJ, Matthews AK, McNamara PJ, & Cao D (2016). Exposure to electronic nicotine delivery systems (ENDS) visual imagery increases smoking urge and desire. Psychology of Addictive Behaviors, 30(1), 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Smith LJ, McNamara PJ, & Cao D (2018). Second generation electronic nicotine delivery system vape pen exposure generalizes as a smoking cue. Nicotine and Tobacco Research, 20(2), 246–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Smith LJ, McNamara PJ, Matthews AK, & Fridberg DJ (2015). Passive exposure to electronic cigarette (e-cigarette) use increases desire for combustible and e-cigarettes in young adult smokers. Tobacco control, 24(5), 501–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozlowski LT, Pillitteri JL, Sweeney CT, Whitfield KE, & Graham JW (1996). Asking questions about urges or cravings for cigarettes. Psychology of Addictive Behaviors, 10(4), 248. [Google Scholar]
- Lee HW, Park SH, Weng MW, Wang HT, Huang WC, Lepor H, Wu X, Chen L, & Tang MS (2018). E-cigarette smoke damages DNA and reduces repair activity in mouse lung, heart, and bladder as well as in human lung and bladder cells. Proceedings of the National Academy of Sciences, 115(7), E1560–E1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maloney EK, & Cappella JN (2016). Does vaping in e-cigarette advertisements affect tobacco smoking urge, intentions, and perceptions in daily, intermittent, and former smokers?. Health communication, 31(1), 129–138. [DOI] [PubMed] [Google Scholar]
- McKee SA (2009). Developing human laboratory models of smoking lapse behavior for medication screening. Addiction biology, 14(1), 99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owusu D, Huang J, Weaver SR, Pechacek TF, Ashley DL, Nayak P, & Eriksen MP (2019). Patterns and trends of dual use of e-cigarettes and cigarettes among US adults, 2015–2018. Preventive medicine reports, 16, 101009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang RD, & Leventhal AM (2013). Sex differences in negative affect and lapse behavior during acute tobacco abstinence: a laboratory study. Experimental and clinical psychopharmacology, 21(4), 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persoskie A, O’Brien EK, & Poonai K (2019). Perceived relative harm of using e- cigarettes predicts future product switching among US adult cigarette and e- cigarette dual users. Addiction, 114(12), 2197–2205. [DOI] [PubMed] [Google Scholar]
- Rass O, Pacek LR, Johnson PS, & Johnson MW (2015). Characterizing use patterns and perceptions of relative harm in dual users of electronic and tobacco cigarettes. Experimental and clinical psychopharmacology, 23(6), 494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Litten RZ, & Allen JP (1992). Measuring alcohol consumption. Totowa, NJ: : Humana Press 1992. 41–72. doi: 10.1007/978-1-4612-0357-5_3 [DOI] [Google Scholar]
- Spielberger CD (1970). Manual for the State-trait Anxietry, Inventory. Consulting Psychologist. [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Shiffman S, & Perrott MA (2001). A multi-dimensional analysis of cue- elicited craving in heavy smokers and tobacco chippers. Addiction, 96(10), 1419–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vena A., Howe M., Cao D., & King A. (2019). The role of E-liquid vegetable glycerin and exhaled aerosol on cue reactivity to tank-based electronic nicotine delivery systems (ENDS). Psychopharmacology, 236(7), 2083–2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vena A, Miloslavich K, Cao D, & King A (2020a). Cue salience of the use of an electronic nicotine delivery system (ENDS) device marketed to women. Addictive behaviors, 100, 106116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vena A, Miloslavich K, Howe M, Cao D, & King AC (2020b). Exposure to JUUL use: cue reactivity effects in young adult current and former smokers. Tobacco Control. [DOI] [PubMed] [Google Scholar]
- Wang JB, Olgin JE, Nah G, Vittinghoff E, Cataldo JK, Pletcher MJ, & Marcus GM (2018). Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PloS one, 13(7), e0198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West R, & Ussher M (2010). Is the ten-item Questionnaire of Smoking Urges (QSU-brief) more sensitive to abstinence than shorter craving measures?. Psychopharmacology, 208(3), 427–432. [DOI] [PubMed] [Google Scholar]
- Yingst J, Foulds J, Veldheer S, & Du P (2019). Device characteristics of long term electronic cigarette users: a follow-up study. Addictive behaviors, 91, 238–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


