Abstract
Nonsuicidal self-injury (NSSI) has been identified as one of the strongest predictors of suicide attempts. Wall/object punching is a particularly prevalent form of NSSI among male veterans that has been linked to both impulsivity and anger. The objective of the present study was to examine the indirect effect of impulsivity on wall/object punching via anger. Participants included 124 veterans (32 identified as women, 92 identified as men) with at least one psychiatric disorder. A third of the sample met criteria for NSSI disorder (33.1%) with nearly a half of the remaining sample endorsing NSSI. Almost half (41.94%) of the sample endorsed wall/object punching. Consistent with our hypothesis, impulsivity was significantly associated with anger, which was, in turn, significantly associated with wall/object punching. Impulsivity was found to be indirectly related to wall/object punching via anger. These findings underscore the significance of assessing and treating anger among veterans engaging in wall/object punching. Improving our knowledge of anger and impulsivity and their relationship with this particularly prevalent form of NSSI among veterans may lead to a better understanding of suicide risk among veterans and inform future treatments.
Keywords: Anger, Nonsuicidal self-injury, Impulsivity, Veterans, Wall Punching
Nonsuicidal self-injury (NSSI) refers to the intentional destruction of one’s own body tissue (e. g., cutting, burning, sticking sharp objects, skin picking, biting, and scratching) with no conscious suicidal intent (Klonsky, 2011; Nock, 2010). NSSI has been linked to adverse outcomes such as negative affect, severe injury, clinical distress, and is one of the strongest longitudinal predictors of prospective suicide attempts (Briere & Gil, 1998; Franklin et al., 2017; Ribeiro et al., 2016). Recent work has highlighted the occurrence of NSSI in military personnel and veterans, reporting a variety of prevalence rates depending on the sample being examined (Bryan & Bryan, 2014; Holiday et al., 2018; Kimbrel et al., 2016, 2018). Among non-treatment seeking samples, prevalence rates of 6% have been reported (Kimbrel et al., 2016). In another study, of service members and veterans enrolled in college classes, 14% reported a lifetime history of NSSI (Bryan & Bryan, 2014). Among survivors of military sexual trauma, a lifetime prevalence of 25% has been reported (Holliday et al., 2018), and among veterans seeking treatment for PTSD, 82% endorsed engaging in NSSI in their lifetime (Kimbrel et al., 2018).
Through the expansion of NSSI research into the veteran population, wall/object punching has been identified as a prevalent, yet understudied, form of NSSI (Kimbrel et al., 2018). Wall/object punching has largely remained understudied due to many of the NSSI assessments being designed for women and adolescents girls who have historically engaged in other forms of NSSI (i.e., cutting, biting, scratching; Bresin & Schoenleber, 2015; Kimbrel et al., 2017). Kimbrel and colleagues (2018) found that 43% of veterans reported engaging in wall/object punching in the past year, and that this behavior was strongly associated with more traditional forms (i.e., cutting, burning, scratching, etc.) of NSSI and provided the most relief from negative affect creating a negative reinforcement loop—a key maintenance factor of NSSI (Kimbrel et al., 2018). Additionally, they found that wall/object punching was distinctly related to suicidal ideation. With NSSI being identified as a unique predictor of suicide, and rising concerns regarding suicidal behavior in veteran populations (Hoge, 2019), there is a need to understand what mechanisms contribute to engagement in this unique form of NSSI to intervene effectively.
One potential construct that may be related to wall/object punching is impulsivity (Hamza et al., 2015). Impulsivity has been linked to other forms of NSSI, with one study finding that individuals engaging in NSSI had higher levels of impulsivity and an increased tendency to engage in NSSI when experiencing negative affect, as compared to noninjurers (Glenn & Klonsky, 2010). Glenn and Klonsky (2010) have further suggested that the elevated impulsivity observed among individuals engaging in NSSI may be due to their higher levels of emotional dysregulation and negative affect. That is, individuals with NSSI may be more likely to act impulsively when dealing with negative emotions, including using NSSI to reduce the intensity of their emotions (Glenn & Klonsky, 2010). One study that qualitatively examined the role of impulsivity in NSSI found that there was a potential link between impulsivity and engagement in wall/object punching, but impulsivity was not systematically assessed and there were only two instances of wall/object punching mentioned as occurring in the sample (Lockwood et al., 2020). It is possible that impulsivity plays a role in the engagement in wall/object punching, as this form of NSSI has been found to provide high levels of relief from negative affect (Kimbrel et al., 2018). Moreover, one form of negative affect that may explain the relationship between impulsivity and wall/object punching is anger.
Evidence suggests that a primary function of NSSI is an attempt to regulate emotion (Briere & Gil, 1998; Klonsky, 2011; Zetterqvist et al., 2013). Dysregulated anger is a prevalent concern for veterans, and recent studies have begun to examine its role in relation to NSSI (Dillon et al., 2021; Cassiello-Robbins et al., 2021). For example, anger has been identified as a significant predictor of NSSI in veterans with NSSI disorder and as a strong antecedent of wall/object punching specifically (Cassiello-Robbins et al., 2021; Dillon et al., 2021). Similarly, anger and impulsivity have been studied together in veteran populations with studies finding anger and impulsivity being positively correlated to suicide risk, predictive of impulsive aggression, and risk factors for increased PTSD severity (Chemtob et al., 1994; Giegling et al., 2009; Horesh et al., 1997; Teten et al., 2010). Contractor and colleagues (2015) found that anger mediated the relationship between impulsivity and PTSD severity in a sample of veterans and suggest that anger may act as mobilizing emotion in the veteran population.
Taken together, this research suggests both impulsivity and anger many play a role in wall/object punching among veterans; however, to date, no studies have examined the interplay of these constructs regarding this form of NSSI. Given that anger has been identified as a clear antecedent and mobilizing emotion for engagement in NSSI, and that impulsivity’s role with wall/object punching may also be explained by anger (Cassiello-Robbins et al., 2021; Dillon et al., 2021), we hypothesized that impulsivity would be indirectly related to wall/object punching via anger.
Methods and Materials
Participants and Procedures
Participants included 124 veterans who participated in a one-year longitudinal study focused on examining the impact of NSSI on veterans’ functional outcomes as well as observing differences in individuals with NSSI disorder compared to individuals who engage in NSSI but do not meet criteria for the disorder and psychiatric controls. The current study focused on the baseline data from this larger study (see Mann et al., 2020 and Patel et al., 2021 for additional information on the parent study). Participants were recruited via clinician referrals, mailings targeting veterans who had sought care in VA PTSD clinics, and phone calls and letters to veterans who had agreed to be listed in research recruitment databases. The study proactively recruited veterans with a history of NSSI and NSSI disorder to ensure sufficient representation in the final sample. To be eligible, participants had to be veterans, 18 years or older, with at least one psychiatric disorder as diagnosed by the Structured Clinical Interview for DSM-5 Disorder–Research Version (First et al., 2015). Exclusion criteria were lifetime bipolar or psychotic spectrum disorder or imminent risk for suicide or homicide. All study procedures were approved by the Durham VA Institutional Review Board (IRB). After giving written informed consent, participants completed a battery of clinical interviews and self-report measures. Participants received $100 for completion of the baseline assessment.
The mean age of the sample was 48.7 years (SD = 13.0; range: 23–77). Approximately one quarter of the sample identified as women (n = 32; 25.8%). Over half of the sample identified as Black (n = 64; 51.6%), 41.9% (n = 52) identified as White, 4.0% (n = 5) identified as Other or declined to answer, 1.6% (n = 2) identified as more than one race, and 0.8% (n = 1) identified as Asian. Regarding ethnicity, 1.6% (n = 2) identified as Hispanic. Regarding NSSI history, 33.1% (n = 41) of the sample met criteria for a current diagnosis of NSSI disorder. Of the remaining 83 veterans, about half (n = 42) reported a lifetime history of NSSI behavior but did not meet criteria for NSSI disorder, whereas the other half (n = 41) reported no lifetime history of NSSI. The most common psychiatric disorders among participants were posttraumatic stress disorder (PTSD) and major depressive disorder (MDD), with 77.4% (n = 96) meeting criteria for current PTSD and 58.9% (n = 73) meeting criteria for current MDD.
Measures
The UPPS-P Impulsive Behavior Scale (UPPS-P; Lynam et al., 2006) was used to assess impulsivity. The UPPS-P is a 59-item self-report measure that assesses multiple facets of impulsivity (i.e., negative urgency, positive urgency, lack of premeditation, lack of perseverance, sensation seeking) on a scale of 1 (agree strongly) to 4 (disagree strongly). A total score is calculated by reverse-scoring appropriate items, calculating mean scores for each subscale, and summing mean scores. Higher values indicate more impulsive behavior. The UPPS-P has demonstrated high internal consistency, and good convergent and discriminant validity (Cyders & Smith, 2007; Smith et al., 2007). In the current sample, the internal consistency was excellent, Cronbach’s α = .91.
The Dimensions of Anger Reactions Scale (DAR; Novaco, 1975) was used to assess anger. The DAR is a seven-item self-report measure that assesses the frequency, intensity, and duration of anger, as well as the impact of anger on social relationships, work, and health. Items are rated on a scale of 0 (not at all) to 8 (exactly so). Items are summed to make a total score. The DAR has demonstrated good concurrent, discriminant, and incremental validity (Novaco et al., 2012). In the current sample, the internal consistency was excellent, Cronbach’s α = .91.
Wall/object punching was assessed with the item following item: “In the past year (12 months), have you ever intentionally punched or hit walls or objects to the point of bruising or bleeding?” This item was added on to the Deliberate Self-Harm Inventory (DSHI; Gratz, 2001), which is a self-report measure that assesses the presence of 17 different types of NSSI, but does not assess wall/object punching, specifically.
Data Analytic Plan
Data analyses were performed using SAS 9.4 (SAS Institute Inc., 2013). First, intercorrelations between the primary study variables were examined. Next, the indirect effect between impulsivity and wall/object punching via anger, covarying for gender, current PTSD diagnosis, and current MDD diagnosis, was tested using the method of Hayes (2017) with PROCESS version 3.5.1 for SAS. The PROCESS procedure used logistic regression to model the probability of engaging in wall/object punching in the past year. The indirect path was estimated using a bootstrap procedure with 10,000 resamples generated to estimate bias-corrected 95% confidence intervals (CIs). The effect is considered to be statistically significant if the 95% confidence interval does not contain zero (Preacher & Hayes, 2004). Direct and indirect effects were estimated on a log-odds metric and converted to odds ratios by exponentiating them.
Results
Almost half of the participants (n = 52; 41.94%) reported engaging in wall/object punching in the past year. Descriptive information and intercorrelations among variables are presented in Table 1. Significant positive associations were identified between wall/object punching, impulsivity, and anger. The sample mean for anger (DAR) was 28.27 (SD = 15.3), which is higher than that of a validation study using a large sample (n = 3,528) of treatment-seeking soldiers who had been deployed in Iraq and Afghanistan (M = 19.1; SD = 14.9; Novaco et al., 2012). However, it was lower than reported means from other PTSD treatment studies of veterans (e.g., M = 32.54, SD = 12.24 [Forbes et al., 2008] and M = 34.7, SD = 12.2 [Forbes et al., 2004]). The sample mean for impulsivity (UPPS-P) was 11.14 (SD = 1.70), which is slightly higher than other studies of impulsivity in veterans (e.g., M = 10.49 [Brown et al., 2018] and M = 10.21 [Bjork et al., 2021]).
Table 1.
Descriptive statistics and intercorrelations for study variables.
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1.Wall/Object Punching | 0.42 | 0.50 | -- | ||||
| 2. DAR Total | 28.27 | 15.30 | 0.37*** | -- | |||
| 3. UPPS-P Total | 11.14 | 1.70 | 0.23* | 0.31** | -- | ||
| 4. Male Gender | 0.74 | 0.44 | −0.09 | −0.06 | −0.01 | -- | |
| 5. Current PTSD | 0.77 | 0.42 | 0.19* | 0.37*** | −0.09 | −0.05 | |
| 6. Current MDD | 0.59 | 0.49 | 0.28** | 0.43*** | 0.23* | −0.16 | 0.37*** |
Note. DAR = Dimensions of Anger Reactions scale; UPPS-P = Impulsive Behavior Scale; PTSD = Posttraumatic stress disorder; MDD = Major depressive disorder.
p < .001;
p < .01;
p < .05.
We examined a model testing the indirect effect of impulsivity (UPPS-P) on wall/object punching via anger (DAR; see Figure 1), while covarying for gender, current PTSD, and current MDD. The association between impulsivity (UPPS-P) and anger (DAR) was significant (b = 3.00, SE = 0.69, t = 4.35, p < .001). The association between anger (DAR) and wall/object punching was also significant (b = 0.04, SE = 0.02, Z = 2.51, p = .012). Additionally, the indirect effect of impulsivity (UPPS-P) on wall/object punching through anger (DAR) was significant (indirect effect = 0.13, SE = 0.06, 95% CI [0.03, 0.27]). The odds ratio for this indirect effect was OR = 1.13, 95% CI [1.03, 1.31]. The direct effect of impulsivity (UPPS-P) on wall/object punching when accounting for anger (DAR) was not significant (direct effect = 0.12, OR = 1.13, SE = 0.13, Z = 0.90, p = 0.37).
Figure 1.
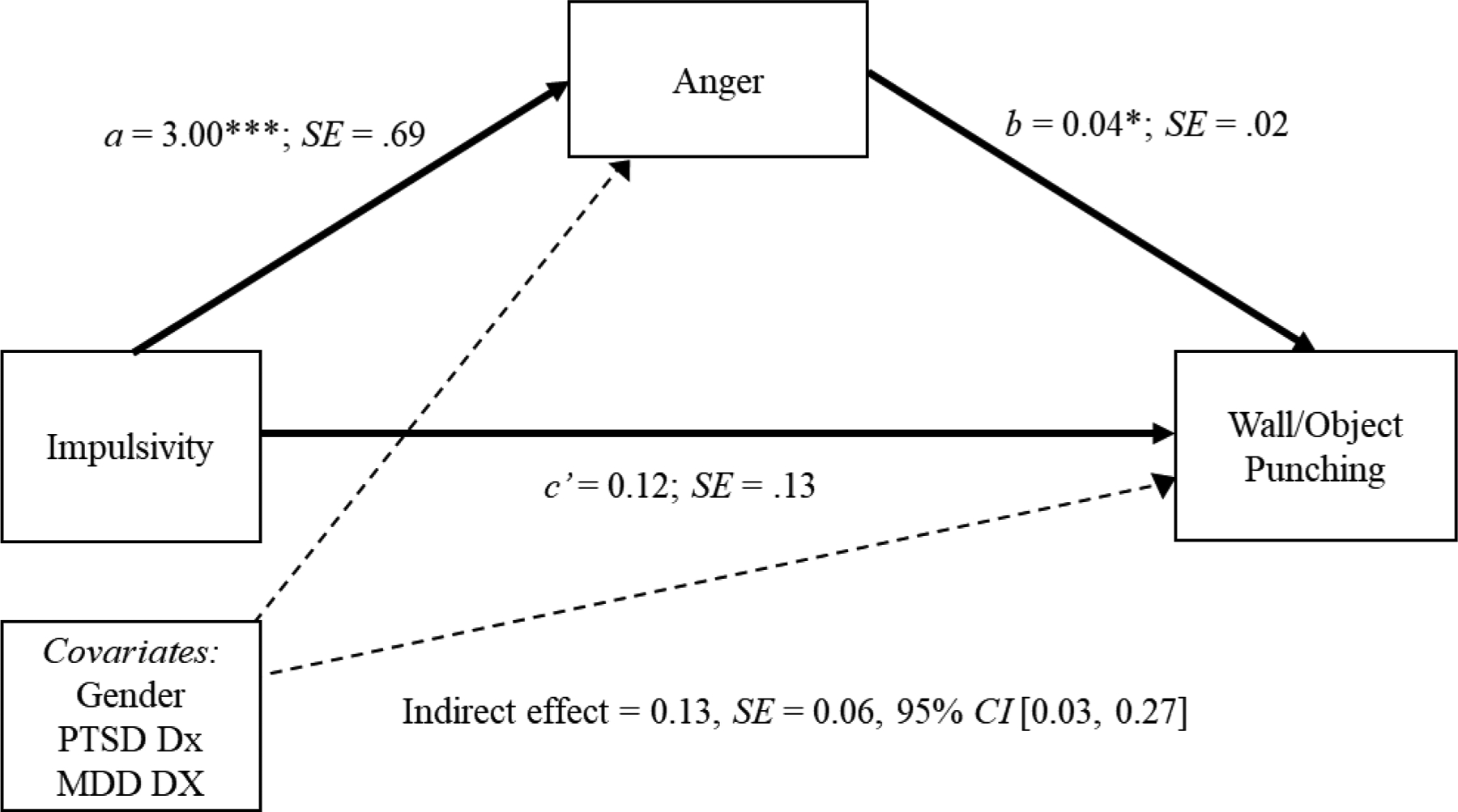
Path coefficients for indirect effect analysis on wall/object punching in the past year. Note: b and c’ are unstandardized logistic regression coefficients and a is an unstandardized OLS regression coefficient. **p < .01, ***p < .001.
Discussion
The goal of the present work was to examine the relationship between impulsivity, anger, and wall/object punching in a sample of veterans diagnosed with psychiatric disorders, when covarying for gender, PTSD, and MDD. Consistent with our hypothesis, we found that impulsivity was indirectly related to wall/object punching via anger. Anger, impulsivity, and wall/punching were significantly associated with one another; however, when controlling for anger, impulsivity was no longer significantly related to wall/object punching, indicating that anger accounted for the relationship between impulsivity and wall/object punching in our sample.
Notably, nearly half (41.94%) of the participants reported engaging in wall/object punching in the past year, which is consistent with prevalence rates from other samples of veterans with psychiatric disorders (Kimbrel et al., 2018), and further highlights the importance of learning more about this under-recognized form of NSSI. Our results further implicate impulsivity and anger as important factors to consider among veteran who self-injure. Anger is conceptualized as an approach-oriented negative emotion (Carver & Harmon-Jones, 2009). Among impulsive individuals, increased anger may drive self-destructive, aggressive behaviors like wall/object punching. This pattern is particularly important because prior research has found that both anger (Dillon et al., 2020; Dobscha et al., 2014; Wilks et al., 2019) and NSSI (Franklin et al., 2017; Ribeiro et al., 2016) are significantly associated with increased suicide risk.
Clinically, our findings add to the literature highlighting the importance of assessing and treating anger and impulsivity in veterans. Interventions that target emotion regulation and/or distress tolerance are likely needed to help veterans manage anger and impulsivity. Evidence-based treatments such as cognitive-behavioral therapy (CBT) for anger or dialectical behavior therapy (DBT) may be effective to address anger, impulsivity, and NSSI. There have been very few controlled trials of CBT for anger in this population (see Van Voorhees et al., 2019) and, to our knowledge, none have examined NSSI as an outcome. Findings from studies of DBT in veteran samples are limited and findings have been mixed (see Gromatsky et al., 2021). Conversely, DBT has been found to be an effective treatment of NSSI reduction in individuals with BPD (Stanley et al., 2007). There have been several pilot studies of innovative anger reduction treatments for veterans that may also be useful to reduce NSSI, such as Manage Emotions to Reduce Aggression (MERA; Miles et al., 2020), a three-session treatment targeting impulsive aggression, and an eight-session computerized treatment to reduce hostile interpretation bias in veterans with anger difficulties (Dillon et al., 2020). Additional research is needed explore the effectiveness of such interventions for the veteran population.
The present findings should also be interpreted within the context of several limitations. First, this study only observed one type of NSSI and its relationship with anger and impulsivity. Though the present study does not focus on other NSSI behaviors, the findings described are important in further demonstrating the validity of wall/object punching as a form of NSSI. Future studies are needed to determine whether similar patterns are observed for other forms of NSSI. Second, the present study used cross-sectional data, which prevents determination of the direction of effects. The data relied on retrospective self-report measures, which may have been affected by participant biases or memory. Use of a longitudinal design and/or ecological momentary assessment may be helpful to address these limitations in future research. Third, due to our sample being a sample of veterans diagnosed with psychiatric disorder(s), the findings cannot be generalized to either the civilian or general veteran population. Future studies should seek to not only investigate this relationship in the general population but also psychiatric subsamples of veterans (i.e., veterans with PTSD compared to veterans with PTSD and comorbid depressive disorder).
The results of the present study indicate that anger may play a key role in the relationship between impulsivity and wall/object punching engagement in veterans. With the high rate of veteran suicide (17 suicides daily; Department of Veterans Affairs, 2021) and NSSI’s association with suicide attempts (Franklin et al., 2017), it is vital to expand on the present preliminary findings in order to determine the direction of these relationships. Further research is also warranted to determine both the mechanistic and directional relationships among these variables in order to inform future research and clinical interventions. Future research should also seek to investigate other mechanisms that could explain these relationships (e.g., ruminative cognitive style, dichotomous thinking, lack of social support).
Acknowledgements
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the United States Government or Department of Veterans Affairs (VA). This work was supported by Merit Award #I01CX001486 to Dr. Kimbrel from the Clinical Sciences Research and Development Service (CSR&D) of VA Office of Research and Development (VA ORD). Dr. Dillon was supported by a Career Development Award (IK2RX002965) from the Rehabilitation Research and Development Service of VA ORD. Dr. Beckham was supported by a Senior Research Career Scientist award (1K6BX003777) from the CSR&D of VA ORD.
References
- Bjor JM, Reiswebe J, Burchet JR, Plonsk PE, Konov AB, Lopez-Guzma S, & Dismuke-Gree CE (2021). Impulsivity and Medical Care Utilization in Veterans Treated for Substance Use Disorder. Substance Use & Misuse, 56(12), 1741–1751. 10.1080/10826084.2021.1949603 [DOI] [PubMed] [Google Scholar]
- Bresin K, & Schoenleber M (2015). Gender differences in the prevalence of nonsuicidal self-injury: A meta-analysis. Clinical psychology review, 38, 55–64. 10.1016/j.cpr.2015.02.009 [DOI] [PubMed] [Google Scholar]
- Briere J, & Gil E (1998). Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. The American journal of orthopsychiatry, 68(4), 609–620. 10.1037/h0080369 [DOI] [PubMed] [Google Scholar]
- Brown RC, Overstreet C, Sheerin C, Berenz E, Hawn S, Pickett T, McDonald S, Danielson CK, & Amstadter AB (2018). The Nomological Network of a Behavioral Distress Tolerance Task in Veterans. Journal of Traumatic Stress, 31(6), 876–885. 10.1002/jts.22349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan C, & Bryan A (2014). Nonsuicidal self‐injury among a sample of united states military personnel and veterans enrolled in college classes. Journal of Clinical Psychology, 70, 874–885. 10.1002/jclp.22075 [DOI] [PubMed] [Google Scholar]
- Carver CS, & Harmon-Jones E (2009). Anger is an approach-related affect: Evidence and implications. Psychological Bulletin, 135(2), 183–204. 10.1037/a0013965 [DOI] [PubMed] [Google Scholar]
- Chemtob CM, Hamada RS, Roitblat HL, & Muraoka MY (1994). Anger, impulsivity, and anger control in combat-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 62(4), 827–832. 10.1037/0022-006X.62.4.827 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Armour C, Wang X, Forbes D, & Elhai JD (2015). The mediating role of anger in the relationship between PTSD symptoms and impulsivity. Psychological Trauma: Theory, Research, Practice, and Policy, 7(2), 138–145. 10.1037/a0037112 [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT (2007). Mood-based rash action and its components: Positive and negative urgency. Personality and Individual Differences, 43, 839–850. 10.1016/j.paid.2007.02.008 [DOI] [Google Scholar]
- Department of Veterans Affairs, 2021. National veteran suicide prevention annual report, Retrieved from. https://www.mentalhealth.va.gov/docs/data-sheets/2021/2021-National-Veteran-Suicide-Prevention-Annual-Report-FINAL-9-8-21.pdf
- Dillon KH, Medenblik AM, Mosher TM, Elbogen EB, Morland LA, & Beckham JC (2020). Using Interpretation Bias Modification to Reduce Anger in Veterans with Posttraumatic Stress Disorder: A Pilot Study. Journal of traumatic stress, 33, 857–863. 10.1002/jts.22525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon KH, Van Voorhees EE, & Elbogen EB (2020). Associations between anger and suicidal ideation and attempts: a prospective study using the National Epidemiological Survey on Alcohol and Related Concerns. Journal of Psychiatric Research, 122, 17–21. 10.1016/j.jpsychires.2019.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobscha SK, Denneson LM, Kovas AE, Teo A, Forsberg CW, Kaplan MS, Bossarte R, & McFarland BH (2014). Correlates of suicide among veterans treated in primary care: Case–control study of a nationally representative sample. Journal of General Internal Medicine, 29(4), 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes D, Hawthorne G, Elliott P, McHugh T, Biddle D, Creamer M, & Novaco RW (2004). A concise measure of anger in combat‐related posttraumatic stress disorder. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 17, 249–256. 10.1023/B:JOTS.0000029268.22161.bd [DOI] [PubMed] [Google Scholar]
- Forbes D, Parslow R, Creamer M, Allen N, McHugh T, & Hopwood M (2008). Mechanisms of anger and treatment outcome in combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 21, 142–149. 10.1002/jts.20315 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- Giegling I, Olgiati P, Hartmann AM, Calati R, Möller HJ, Rujescu D, & Serretti A (2009). Personality and attempted suicide. Analysis of anger, aggression and impulsivity. Journal of psychiatric research, 43(16), 1262–1271. 10.1016/j.jpsychires.2009.04.013 [DOI] [PubMed] [Google Scholar]
- Glenn CR, & Klonsky ED (2010). A multimethod analysis of impulsivity in nonsuicidal self-injury. Personality Disorders: Theory, Research, and Treatment, 1(1), 67–75. https://doi-org.proxy.lib.duke.edu/10.1037/a0017427 [DOI] [PubMed] [Google Scholar]
- Gratz KL (2001). Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment, 23(4), 253–263. 10.1023/A:1012779403943 [DOI] [Google Scholar]
- Gromatsky M, Mann AJ, Kimbrel NA, & Dillon KH (2022). NSSI Among Military Servicemembers and Veterans. In The Handbook of Nonsuicidal Self-Injury. Oxford University Press. [Google Scholar]
- Hamza CA, Willoughby T, & Heffer T (2015). Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clinical Psychology Review, 38, 13–24. https://doi-org.proxy.lib.duke.edu/10.1016/j.cpr.2015.02.010 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Press. [Google Scholar]
- Hoge CW (2019). Suicide Reduction and Research Efforts in Service Members and Veterans-Sobering Realities. JAMA psychiatry, 76(5), 464–466. 10.1001/jamapsychiatry.2018.4564 [DOI] [PubMed] [Google Scholar]
- Holliday R, Smith NB, & Monteith LL (2018). An initial investigation of nonsuicidal self-injury among male and female survivors of military sexual trauma. Psychiatry Research, 268, 335–339. 10.1016/j.psychres.2018.07.033 [DOI] [PubMed] [Google Scholar]
- Horesh N, Rolnick T, Iancu I, Dannon P, Lepkifker E, Apter A, & Kotler M (1997). Anger, impulsivity and suicide risk. Psychotherapy and psychosomatics, 66(2), 92–96. 10.1159/000289115 [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Calhoun PS, & Beckham JC (2017). Nonsuicidal self-injury in men: a serious problem that has been overlooked for too long. World psychiatry : official journal of the World Psychiatric Association (WPA), 16(1), 108–109. 10.1002/wps.20358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, & Morissette SB (2016). Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research, 243, 232–237. 10.1016/j.psychres.2016.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Thomas SP, Hicks TA, Hertzberg MA, Clancy CP, Elbogen EB, Meyer EC, DeBeer BB, Gross GM, Silvia PJ, Morissette SB, Gratz KL, Calhoun PS, & Beckham JC (2018). Wall/Object Punching: An important but under‐recognized form of nonsuicidal self‐injury. Suicide Life Threat Behav, 48(5), 501–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED (2011). Non-suicidal self-injury in United States adults: prevalence, sociodemographics, topography and functions. Psychological medicine, 41(9), 1981–1986. 10.1017/S0033291710002497 [DOI] [PubMed] [Google Scholar]
- Lockwood J, Townsend E, Allen H, Daley D, & Sayal K (2020). What young people say about impulsivity in the short-term build up to self-harm: A qualitative study using card-sort tasks. PloS one, 15(12), e0244319. 10.1371/journal.pone.0244319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynam DR, Whiteside SP, Smith GT, & Cyders MA (2006). The UPPS-P: Assessing five personality pathways to impulsive behavior. West Lafayette, IN: Purdue University [Google Scholar]
- Mann AJ, Van Voorhees EE, Patel TA, Wilson SW, Gratz KL, Calhoun PS, Beckham JC, & Kimbrel NA (2020) Nail-biting, scab-picking, and tattooing as nonsuicidal self-injury (NSSI): A deviant case series analysis of the proposed NSSI disorder diagnostic criteria. Journal of Clinical Psychology, 2020, 1–18. 10.1002/jclp.23008 [DOI] [PubMed] [Google Scholar]
- Miles SR, Kent TA, Stanley M, Thompson KE, Sharp C, Niles BL, … & Peterson AL (2020). Manage Emotions to Reduce Aggression: A Pilot Study of a Brief Treatment to Help Veterans Reduce Impulsive Aggression. The Journal of Nervous and Mental Disease, 208, 897–903. Doi: 10.1097/NMD.0000000000001229 [DOI] [PubMed] [Google Scholar]
- Nock MK (2010). Self-injury. Annual review of clinical psychology, 6, 339–363. 10.1146/annurev.clinpsy.121208.131258 [DOI] [PubMed] [Google Scholar]
- Novaco RW (1975). Dimensions of anger reactions. Irvine, CA: University of California, 639. [Google Scholar]
- Novaco RW, Swanson RD, Gonzalez OI, Gahm GA, & Reger MD (2012). Anger and postcombat mental health: validation of a brief anger measure with U.S. soldiers postdeployed from Iraq and Afghanistan. Psychological assessment, 24(3), 661–675. 10.1037/a0026636 [DOI] [PubMed] [Google Scholar]
- Patel TA, Mann A, Blakey SM, Aunon FM, Calhoun PS, Beckham JC, & Kimbrel NA (2021). Diagnostic Correlates of Nonsuicidal Self-Injury Disorder among Veterans with Psychiatric Disorders. Psychiatry research, 296, 113672. 10.1016/j.psychres.2020.113672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments & Computers, 36(4), 717–731. 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc 2013. SAS/ACCESS® 9.4 Interface to ADABAS: Reference. Cary, NC: SAS Institute Inc. [Google Scholar]
- Smith GT, Fischer S, Cyders MA, Annus AM, Spillane NS, McCarthy DM (2007). On the validity and utility of discriminating among impulsivity-like traits. Assessment, 14, 155–170. 10.1177/1073191106295527 [DOI] [PubMed] [Google Scholar]
- Stanley B, Brodsky B, Nelson JD, & Dulit R (2007). Brief dialectical behavior therapy (DBT-B) for suicidal behavior and non-suicidal self injury. Archives of suicide research : official journal of the International Academy for Suicide Research, 11(4), 337–341. 10.1080/13811110701542069 [DOI] [PubMed] [Google Scholar]
- Teten AL, Miller LA, Stanford MS, Petersen NJ, Bailey SD, Collins RL, Dunn NJ, & Kent TA (2010). Characterizing aggression and its association to anger and hostility among male veterans with post-traumatic stress disorder. Military medicine, 175(6), 405–410. 10.7205/milmed-d-09-00215 [DOI] [PubMed] [Google Scholar]
- Van Voorhees EE, Dillon KH, Wilson SM, Dennis PA, Neal LC, Medenblik AM, … & White JD (2019). A comparison of group anger management treatments for combat veterans with PTSD: Results from a quasi-experimental trial. Journal of Interpersonal Violence, 10.1177/0886260519873335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks CR, Morland LA, Dillon KH, Mackintosh MA, Blakey SM, Wagner HR, VA Mid-Atlantic MIRECC Workgroup, & Elbogen EB (2019). Anger, social support, and suicide risk in U.S. military veterans. Journal of Psychiatric Research, 109, 139–144. 10.1016/j.jpsychires.2018.11.026 [DOI] [PubMed] [Google Scholar]
- Zetterqvist M, Lundh LG, Dahlström Ö, & Svedin CG (2013). Prevalence and function of non-suicidal self-injury (NSSI) in a community sample of adolescents, using suggested DSM-5 criteria for a potential NSSI disorder. Journal of Abnormal Child Psychology, 41, 759–773. doi: 10.1007/s10802-013-9712-5 [DOI] [PubMed] [Google Scholar]


