Abstract
Background
SDHB is one of the major genes predisposing to paraganglioma/pheochromocytoma (PPGL). Identifying pathogenic SDHB variants in patients with PPGL is essential to the management of patients and relatives due to the increased risk of recurrences, metastases and the emergence of non-PPGL tumours. In this context, the ‘NGS and PPGL (NGSnPPGL) Study Group’ initiated an international effort to collect, annotate and classify SDHB variants and to provide an accurate, expert-curated and freely available SDHB variant database.
Methods
A total of 223 distinct SDHB variants from 737 patients were collected worldwide. Using multiple criteria, each variant was first classified according to a 5-tier grouping based on American College of Medical Genetics and NGSnPPGL standardised recommendations and was then manually reviewed by a panel of experts in the field.
Results
This multistep process resulted in 23 benign/likely benign, 149 pathogenic/likely pathogenic variants and 51 variants of unknown significance (VUS). Expert curation reduced by half the number of variants initially classified as VUS. Variant classifications are publicly accessible via the Leiden Open Variation Database system (https://databases.lovd.nl/shared/genes/SDHB).
Conclusion
This international initiative by a panel of experts allowed us to establish a consensus classification for 223 SDHB variants that should be used as a routine tool by geneticists in charge of PPGL laboratory diagnosis. This accurate classification of SDHB genetic variants will help to clarify the diagnosis of hereditary PPGL and to improve the clinical care of patients and relatives with PPGL.
Keywords: genetic variation, databases, genetic, adrenal gland diseases, genetic testing, human genetics
Introduction
The SDHB protein (OMIM185470) corresponds to the catalytic iron-sulfur subunit of the heterotetrameric succinate dehydrogenase (SDH) complex, a component of both the tricarboxylic acid cycle and the mitochondrial respiratory chain (complex II). Germline inactivating SDHB pathogenic variants were first identified in kindreds with familial pheochromocytoma and paraganglioma (PPGL).1 Paragangliomas (PGL) and pheochromocytomas (PCC) are rare neuroendocrine tumours arising from the sympathetic/parasympathetic ganglia and the adrenal medulla, respectively. Among human tumours, PPGLs show the highest frequency of hereditary forms of the disease, representing at least 35% of all cases.2 For this reason, some PPGL guidelines recommend that genetic testing should be considered in all patients with PPGL.3 4 Over 20 genes are known to increase susceptibility to PPGL. SDHB, which acts as a tumour suppressor gene, is one of the most frequently involved, considering that around 10% of all PPGL cases carry an SDHB-pathogenic variant, including patients with apparently sporadic disease.2 5–7 SDHB therefore is included in the primary (also referred to as ‘basic’) panel of genes routinely analysed in patients with PPGL, all of which were validated as bona fide susceptibility genes.2 4 SDHB pathogenic variants most commonly predispose to head and neck PGLs, sympathetic PGLs and PCCs, and also give rise to renal cell carcinomas (RCC), wild-type gastrointestinal stromal tumours (wtGIST) and pituitary adenomas.8 Moreover, SDHB pathogenic variants have been associated with a high risk of metastasis and a poor prognosis.9 10 As SDHB patients face a high risk of disease recurrence, possible emergence of non-PPGL tumours such as RCCs and wtGISTs and metastatic evolution, it is essential to patient management and follow-up that the identification of an SDHB variant is followed by an accurate classification as ‘disease causing’ or not. Determining the pathogenicity of an SDHB variant is also a precondition for presymptomatic genetic testing of relatives and the appropriate management of carriers of pathogenic variants. Indeed, the ‘unclassified genetic variants’ working group at the International Agency for Research on Cancer recommends that predictive genetic testing of at-risk relatives should be confined to pathogenic or likely pathogenic variants.11
Public gene-specific databases already exist for various PPGL susceptibility genes. The NGS in PPGL (NGSnPPGL) Study Group—which includes 18 experts from 8 countries and includes both clinicians and basic researchers involved in PPGL genetic testing and genetic counseling—published a consensus statement in 2017 emphasising the importance of multi-institutional, internationally shared efforts to compile resources for genomic, clinical and functional data, including the comprehensive annotation of variants and encouraging public sharing of novel variants.2
The SDHB variant database was created in 2005, using the Leiden Open Variation Database (LOVD) platform (https://databases.lovd.nl/shared/genes/SDHB).12 The database mainly consists of variants extracted from the published literature but increasingly includes directly submitted variants. As of September 2020, the LOVD-SDHB comprises 288 unique variants for which a detailed nomenclature, clinical and segregation data, as well as publication references are available.13
Here, we present an international initiative of the NGSnPPGL study group to provide a comprehensive annotation of SDHB variants, to gather variants identified in laboratories worldwide that perform SDHB molecular analysis and to collect extensive data associated with these variants including patient phenotype and in silico, functional or additional analyses performed in each case. Based on these data, each variant was classified according to both the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology criteria,14 and the NGSnPPGL guidelines,2 into one of five classes of pathogenicity.11 All variants were then manually reviewed by a panel of international experts in the field, leading to a consensus classification. Our main goal was to provide a freely available, expert-curated, SDHB variant database, offering an accurate and harmonised interpretation that will improve the care of patients and families carrying these variants.
Methods
Data collection
Data on patients carrying an SDHB variant were submitted by 10 laboratories worldwide, which routinely perform the SDHB genotyping and belong to the European Network for the Study of Adrenal Tumors (ENS@T) and/or the Pheochromocytoma and paraganglioma RESearch Support Organization (PRESSOR) and/or the French Oncogenetics Network of Rare Neuroendocrine Tumors (TENgen network). Data on 737 index cases were collected, including 386 from France (5 laboratories located in Georges Pompidou European Hospital—Paris, La Conception hospital—Marseille, Hospices Civils—Lyon, Centre hospitalo-universitaire—Lille and Centre hospitalo-universitaire—Angers), 215 from the UK (Cambridge/Birmingham), 71 from Spain (Madrid), 32 from the USA (San Antonio, Texas), 20 from Italy (Firenze) and 13 from Australia (Sydney). Patients carrying only well-known single nucleotide polymorphisms of SDHB gene were not enrolled.
Clinical data collected for each index case included the type, number and site of tumours; the age at diagnosis; the metastatic status (defined by the presence of metastases in non-paraganglial tissue15); the biochemical secretion profile and the family history of SDHB spectrum tumours. Co-segregation data in families were reported when available.
All data have been collected retrospectively and de-identified.
Molecular data
The nuclear SDHB gene (1p36) covers 8 exons and encodes a 281 amino acid protein.
Genotyping of leucocyte DNA was performed locally and included the sequencing of the full coding regions and exon-intron junctions using the Sanger or the next-generation sequencing (NGS) methods together with search for large rearrangements using Multiplex Ligation-dependent Probe Amplification (MLPA, MRC-Holland).
All variants were annotated according to the NM_003000.2 reference transcript on genome assembly GRCh37 (hg19) and following Human Genome Variation Society nomenclature (https://varnomen.hgvs.org/). For each variant, the DNA and protein changes were collected. Other tested genes and the co-occurrence of additional variants of interest were specified by submitters when pertinent.
Previous reports for each variant were checked in dbSNP, exome variant server, gnomAD and ClinVar databases through AlamutVisual software, V.2.10 (Interactive Biosoftware, Sophia Genetics) (online supplemental table 1). Variant frequencies in reference populations and literature references were included when available.
jmedgenet-2020-107652supp001.xlsx (14.2KB, xlsx)
In silico predictions
For missense variants, in silico analyses were performed based on amino acid conservation among 14 orthologs and expressed as a ratio between 0 and 1 (x orthologs sharing the same amino acid/14), nucleotide conservation was based on PhyloP and Grantham distance score and predicted impact were derived from PolyPhen2 (HumVar), SIFT, Align-GVGD and Mutation Taster. Predicted impact according to MaxEntScan and NNSplice was estimated for variants with a potential splice effect (splicesite synonymous and intronic variants). The tools used and the corresponding thresholds are described in online supplemental table 1.
Additional data
Supporting information such as loss of heterozygosity (LOH) in tumour DNA, cDNA analysis, SDHB and/or SDHA immunohistochemistry on FFPE tumour tissue sections, SDH enzymatic activity and other pertinent assays were reported when available (online supplemental table 2). Because SDHB functions as a tumour suppressor gene with loss of the wild-type allele in tumour tissue, LOH analysis was performed when both germline and tumour samples were available. In case of variants possibly leading to abnormal splicing, cDNA analysis was performed when leucocyte or tumour RNA was available. SDHB immunohistochemistry and SDH enzymatic activity measurement are useful tools to discriminate SDHx-related and non-SDHx-related tumours, as a loss of SDHB protein or SDH activity reliably signals the presence of an SDHx deleterious variant in tumour cells.16 17 Negative SDHB immunostaining or loss of SDH activity, combined with negative SDHC, SDHD and SDHA (or positive SDHA immunohistochemistry18) genotyping, is a hallmark of SDHB loss-of-function variants. When available, tumour classification in cluster 1A (SDHx-related), 1B (VHL-related) or 2A (RET/NF1/sporadic tumours), according to previous transcriptomic analyses19 20 was specified, as well as SDHB protein expression as evaluated by western blot analysis (online supplemental figure 1).
jmedgenet-2020-107652supp002.xlsx (44.2KB, xlsx)
jmedgenet-2020-107652supp003.pdf (35.6KB, pdf)
Variant classifications
All variants were classified according to ACMG criteria14 adjusted to SDHB gene and PPGL specificities (online supplemental figure 1). As they are not applicable and/or established for the SDHB gene, the following criteria were not considered: PS4 (prevalence in affected individuals statistically increased over controls); BP1 (missense in gene where only truncating cause disease); PP2 (missense in gene with low rate of benign missense variants and pathogenic missenses common); PM1 (mutational hot spot or well-studied functional domain without benign variation); PM3 (for recessive disorders, detected in trans with a pathogenic variant); PM6 and PS2 (because de novo cases are very rare, SDHB variants are usually inherited, even from unaffected parents due to low penetrance of the disease). As there are multiple PPGL susceptibility genes, PP4 criteria (patient’s phenotype or family history highly specific for gene) were not retained for classification. Additional data criteria were adapted as follows: benign strong (loss of the allele carrying the SDHB variant in tumour DNA), benign supporting (no LOH at the SDHB locus, assay not in favour of SDHB loss of function), pathogenic supporting (LOH at the SDHB locus), pathogenic moderate (assay in favour of SDH loss of function without all SDHx genes analysed), pathogenic strong (evidence for SDH loss of function and no additional variant found in SDHx genes), pathogenic very strong (evidence for SDHB-specific loss of function) (online supplemental figure 1). We also considered other criteria calibrated between benign strong and pathogenic strong according to number of published cases and previously reported evidence.
Variants were also classified according to the NGSnPPGL study group framework2 based on the frequency of the variant in the general population, the variant type, in silico predictions, co-segregation in families and the results of additional information or assays available in the literature or for the submitted cases (online supplemental figure 2).
jmedgenet-2020-107652supp004.pdf (11.3KB, pdf)
Both classifications assigned each variant to one of the following classes: benign variant (BV, class 1), likely benign variant (LBV, class 2), variant of unknown significance (VUS, class 3), likely pathogenic variant (LPV, class 4) or pathogenic variant (PV, class 5).
After data collection, in silico analyses and variant classification according to both ACMG and NGSnPPGL study group guidelines were performed by a sole investigator (LBA) for consistency.
Curation by experts
After standardised ACMG and NGGnPPGL study group classification, manual review of each variant was independently carried out by five experts (NB, JPB, MR, FS, AC), which involved choosing between two assigned classes when they were different, or applying a different classification based on personal expertise.
In case of discordance between expert classifications after the first round of reviewing, a second round of expert curation (NB, JPB, MR, PLD, RAT) was performed in order to achieve a consensus class for each variant.
Results
Characterisation of the patient cohort
Clinical data were collected for 737 index cases carrying a SDHB variant (table 1).
Table 1.
Clinical presentation of patients included in the study
| Clinical data | All index cases with SDHB variant (n=737) | Index cases with (likely) pathogenic SDHB variant (n=614) | |
| Number and location of tumours | Single PPGL | 618 (84.5%) | 514 (84.3%) |
| Single headandneck PGL | 213 (44.8%) | 171 (44.5%) | |
| Single TAP-PGL | 184 (38.7%) | 166 (43.2%) | |
| Single PCC | 78 (16.4%) | 47 (12.2%) | |
| Location not specified | 143 | 130 | |
| Multiple PPGL | 103 (14.1%) | 89 (14.6%) | |
| RCC only | 8 (1.1%) | 5 (0.8%) | |
| GIST only | 2 (0.3%) | 2 (0.3%) | |
| Number and location of tumours not specified | 6 | 4 | |
| Benign/metastatic status | Metastatic disease | 133 (35.8%) | 122 (40%) |
| Benign disease | 238 (64.2%) | 183 (60%) | |
| Metastatic status not specified | 366 | 309 | |
| Familial/Sporadic presentation | Family history | 159 (29.8%) | 142 (33.1%) |
| No family history | 374 (70.2%) | 287 (66.9%) | |
| Family history not specified | 204 | 185 | |
GIST, gastrointestinal stromal tumour; PCC, pheochromocytoma; PGL, paraganglioma; PPGL, paraganglioma/pheochromocytoma; RCC, renal cell carcinoma; TAP-PGL, thoracic, abdominal or pelvic PGL.
Patients were affected by a single PPGL in 84.5% (618/731) of cases, multiple (2–7) PPGL in 14.1% (103/731), RCC only in 1.1% (8/731) and GIST only in 2 cases. The tumour location was unknown for six patients. Among patients affected by a single PPGL with known location, 213 had a head and neck PGL (44.8%), 184 a thoracic, abdominal or pelvic PGL (38.7%) and 78 a PCC (16.4%). The precise tumour location was not specified for other patients (n=143). Metastatic disease was diagnosed in 133 patients, corresponding to 35.8% of cases with known benign/metastatic status. When family history was known, the disease was familial in 29.8% of cases (159/533). Twenty-three per cent of patients were affected during their fourth decade. The minimum age at diagnosis was 6 years, the mean age was 36 years and the maximum age was 83 years.
Variant characterisation
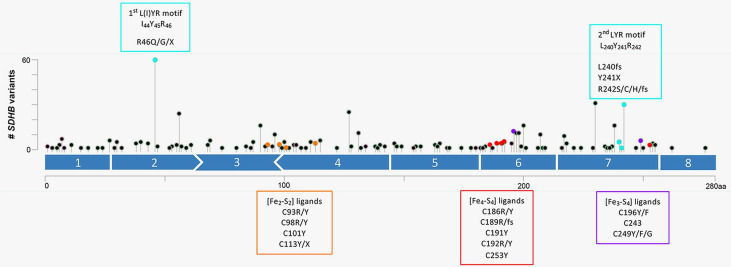
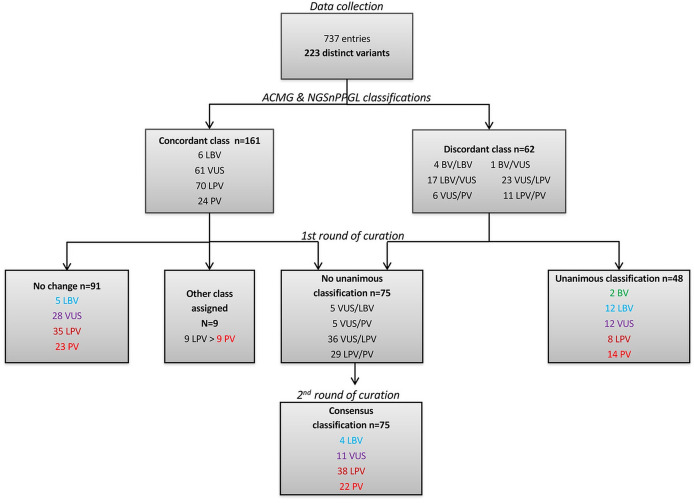
A total of 223 distinct variants have been collected from the 737 entries (online supplemental table 2). Of these, 122 variants were found only once, 75 occurred 2–5 times, 12 were found 6–10 times, 9 variants occurred between 11 and 20 times and 5 variants were found 20 or more times. As regards the type of variant, 162 (73%) were nucleotide substitutions including missense (n=98, 44%), nonsense (n=21, 9%), splicesite (n=20, 9%), mid-intronic (n=12, 5%), synonymous (n=6, 3%), 5' untranslated region (n=3, 1%) and initiation codon (n=2, 1%) variants. Other variants consisted of 61 (27%) deletions or duplications including indels leading to a frameshift (n=38, 17%), large deletions/duplications (n=14, 6%), in-frame deletions (n=4, 2%) or indels affecting non-coding regions (n=3, 1%) or splicesites (n=2, 1%) (figure 1). SDHB exonic variants are distributed along the entire coding sequence of the gene (figure 2). Relative to exon size, SDHB substitutions or indels are more frequent in exon 7 (36 variants for 123 bp), exon 6 (29 variants for 102 bp) and exon 4 (36 variants for 137 bp). Exon 8 is rarely involved, with only two substitutions within 78 bp.
Figure 1.
Distribution of SDHB variants according to the type of alteration RGT: rearrangement. UTR, untranslated region.
Figure 2.
Diagram of the coding SDHB variants along the amino acid sequence L(I)YR motifs are shown in blue. The cysteine residues ligating the [Fe2-S2], the [Fe4-S4] and the [Fe3-S4] are shown in orange, red and purple, respectively. Diagram is displayed as lollipop symbols designed using the Mutation Mapper tool of the cBioPortal website. The Y axis represents the number of occurrences of variant in one residue.
Of the 223 distinct variants, 166 had been previously described (135 in SDHB-LOVD, 107 in ClinVar, 84 in dbSNP, 49 in gnomAD and 14 in ESP). To our knowledge, 57 variants have not been previously reported in any database (online supplemental table 2).
Variant classification based on ACMG and NGSnPPGL recommendations
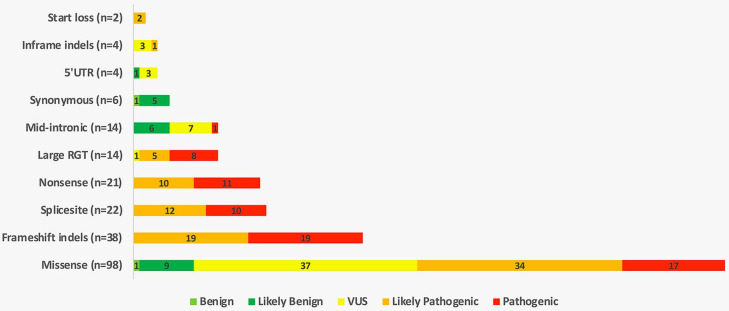
Each variant was classified according to criteria from both the ACMG and NGSnPPGL frameworks (figure 3). This step led to concordant classification of 161 variants, comprising 6 LBV, 61 VUS, 70 LPV and 24 PV variants. Sixty-two variants showed discordant ratings based on ACMG and NGSnPPGL criteria, including 4 BV/LBV, 1 VUS/BV, 17 VUS/LBV, 23 LPV/VUS, 6 VUS/PV and 11 LPV/PV.
Figure 3.
Strategy for variant classification. ACMG, American College of Medical Genetics and Genomics; BV, benign variant; LBV, likely benign variant; LPV, likely pathogenic variant; PV, pathogenic variant; VUS, variant of unknown significance.
Variant assessment by a panel of experts
After the first round of manual reviewing of all variants by the experts, the ACMG/NGSnPPGL classification, when concordant, remained unchanged for 91/161 variants (5 LBV, 28 VUS, 35 LPV and 23 PV). All experts agreed to convert nine originally LPV to PV including three gross deletions (deletion encompassing exons 1–7, exons 2–8 or the whole gene), two affecting splice junctions (c.423+1G>C and c.540G>C), 3 missense (p.Gly208Glu, p.Arg230His and p.Cys253Tyr) and one nonsense (p.Arg90Ter) variant, due to cumulative evidence of pathogenicity and/or high recurrence in patients.
For variants that were originally discordant between the two classification systems (n=62), the first round of curation led to the unanimous assignment of 48 variants to a single class, including 2 BV, 12 LBV, 12 VUS, 8 LPV and 14 PV (figure 3).
Variant classification after the second round of curation
Following the first expert review, 75 variants remained without an unanimous classification, comprising 5 VUS or LBV, 5 VUS or PV, 36 VUS or LPV and 29 LPV or PV. These 75 variants were then submitted to a second round of expert review. Based on a careful review of additional data obtained during the reviewing process (new publications, SDHB immunohistochemistry results, description of new probands carrying the variant) and on their own expertise, the curators reached consensus on all variants.
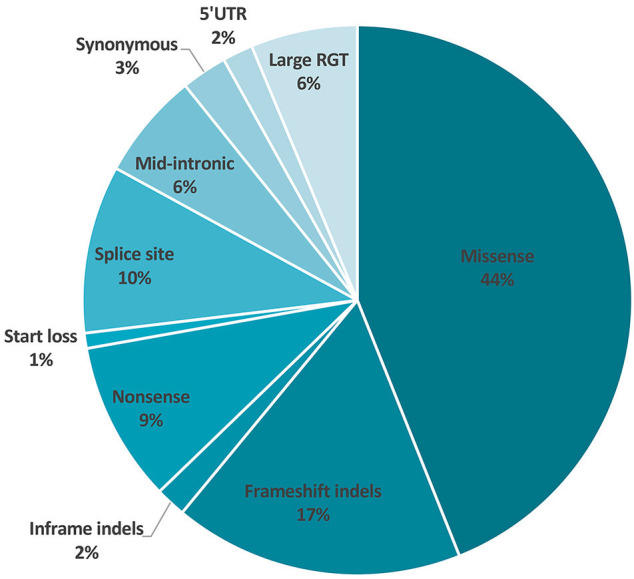
After the final round of curation, the 223 distinct SDHB variants were classified as follows: 2 benign, 21 likely benign, 51 VUS, 83 likely pathogenic and 66 pathogenic variants (figures 3 and 4).
Figure 4.
Distribution of SDHB variant types according to the 5-tier classification. VUS, variant of unknown significance; UTR, untranslated region.
Discussion
With extensive data collected from 737 SDHB-positive index cases, this study provides the first comprehensive overview of SDHB variants identified worldwide. The 223 distinct variants reported here were first classified according to a five-tier grouping using both the ACMG guidelines and the recommendations specifically designed for PPGL susceptibility genes established by the NGSnPPGL study group. All variants were then curated by a panel of international experts in the field based on two rounds of review. This multistep process resulted in a consensus classification for each variant. This expert-curated SDHB variant database is now freely available for the scientific community in the LOVD system (https://databaseslovdnl/shared/genes/SDHB).12
The distribution of variant types in this study is in accordance with prior reports.21 Regarding missense variants, 38% are located in either L(I)YR Fe-S transfer motifs or in the Fe-S cluster-ligating cysteines as previously reported (figure 2).22 The high rate of gross SDHB deletions or duplications, carried by 12% of index cases (86/737) and including hotspots such as exon 1 deletion (see below), is confirmed in this study and emphasises the importance of searching for large rearrangements using NGS or dedicated methods like MLPA.23 Most variants were reported only once (55%, n=123) but 14 were recorded >10 times including the deletion of exon 1 (52 reports), the c.72+1A>G and c.137G>A variants (39 reports each) and the c.166_170del and the c.689G>A variants (21 reports each), thereby revealing several likely mutational hot spots or founder mutations.21 24 25 The founder Dutch mutations c.423+1G>A and SDHB exon 3 deletion were reported 18 and 9 times, respectively.26 Twenty-five per cent of the variants reported here had not been previously described.
Until recently, laboratories largely used their own methods to assess variant pathogenicity, leading to discrepancies between interpretations.27 Guidelines for variant interpretation were established in 2015 by the ACMG, encouraging harmonisation in variant classification.14 These guidelines have now been widely adopted by laboratories internationally. However, some ACMG criteria may be applied or weighted differently depending on the laboratory.28 Moreover, as ACMG guidelines aim at being applicable to all genes that cause Mendelian disorders, they cannot take into account the specificities of one particular gene or disease.14 This consideration has prompted to the development of many national or international consortia of experts on particular genes or diseases, and has led to the development of dedicated recommendations for variant interpretation. Regarding cancer predisposing genes, these international efforts have mainly been initiated for common cancers such as breast cancer or Lynch syndrome29–31 or ‘iconic’ tumour suppressor genes such as TP53.32 Regarding PPGL predisposition, the international NGSnPPGL study group recently published guidelines designed specifically for PPGL susceptibility genes.2 One of the main goals of these guidelines is to minimise the number of VUS because inconclusive report on these variants may cause confusion and anxiety for both patients and physicians. Moreover, this situation can introduce ambiguities in patient care because no established medical management for VUS carriers exists. Finally, a VUS cannot be used in predictive gene testing in relatives. Resolving the pathogenicity of a VUS is therefore essential. In the context of predisposition to PPGL, patients carrying a germline likely pathogenic or pathogenic variant in a PPGL susceptibility gene should undergo lifelong follow-up including, in the case of SDHB, careful monitoring for risk of metastases, GIST or RCC development.33 Moreover, as SDHB-related PPGL can occur early in childhood, predictive genetic testing and subsequent first screening by imaging, together with long-life surveillance, should be started at age 5–6 years in carriers of likely pathogenic/pathogenic SDHB variants.34
The ACMG and NGSnPPGL criteria were applied to assess all variants collected. The class assigned by both methods was the same in the majority of cases (n=161, 72%). In case of discordance (n=62, 28%), the ACMG classification generally assigned VUS (n=45) while the NGSnPPGL framework only assigned two VUS. These results suggest that the NGSnPPGL disease-specific recommendations are more pertinent for PPGL genetic counselling than standard ACMG criteria. In total, one or both methods ended in a VUS status for almost half of variants (n=108, 48%). After curation by experts, most were reassessed and the number of VUS decreased dramatically to 51 in total (22%). This result highlights both the challenge and the important impact of SDHB variant interpretation performed by experts.
In total, 77% (n=172) of variants described in the present study could be classified either as benign/likely benign (10%, n=23) or as likely pathogenic/pathogenic (67%, n=149). The relatively low rate of non-pathogenic variants is explained because frequent or well-known polymorphisms were not collected. Results of additional/functional data were helpful for classification of 94 (42%) variants. Depending on variants, we compiled results obtained from mutated tumour tissue and comprising SDHB±SDHA immunohistochemistry (n=75), LOH detection (n=26), transcriptomic clustering (n=24), cDNA analysis (n=15), western blot analysis (n=7) and measurement of SDH enzymatic activity (n=6) (online supplemental table 2 and figure 1).
Considering the whole cohort of 737 affected patients, 614 of them (83.3%) carry a likely pathogenic or a pathogenic variant. The comparison of the clinical data available for both populations (table 1) revealed no significant difference, confirming that the patient’s phenotype does not allow to classify a variant as pathogenic or not. Noticeably, the occurrence of GIST or RCC is not associated with a specific genotype as all variants identified in patients with GIST or RCC were also found in patients with PPGL only.
Finally, class 3 includes 51 variants with limited data or/and no relevant or contradictory evidence for pathogenicity such as immunohistochemistry results, mostly because no tumour tissue was available or because discordant results were obtained. As expected, VUS exclusively comprise non-truncating variants, including 37/98 missense, 10/18 non-coding variants and 3/4 in-frame indels. Moreover, we were unable to determine the pathogenicity of whole gene SDHB duplication.
Finally, the consensus classification (as well as pertinent information and the following comment: ‘variant classified by experts from the NGSnPPGL study group (ENS@T/PRESSOR)’) for the 223 collected variants has been deposited in the LOVD-SDHB database in order to share a free, valuable and updated resource with the community. International efforts should continue, and laboratories/centres are encouraged to systematically submit and review data for new variants and for already reported VUS, because reassessment may result in changes in variant classification as new evidence becomes available.
In summary, we collected SDHB variants worldwide and gathered an international group of curators committed to working together to expertly classify these variants. These experts undertook a joint effort to collect, share, integrate and then discuss multiple strands of evidence pertaining to SDHB genetic variants, with the objective of determining the clinical relevance of a variant to ultimately improve the clinical utility of genetic testing in patients and their relatives.
Acknowledgments
The authors are grateful to the PPGL working group of the European Network for the Study of Adrenal Tumours (ENS@T) and the Pheochromocytoma and paraganglioma RESearch Support Organisation (PRESSOR) for their support. The authors from France thank INSERM and the French National Cancer Institute (INCA) for their financial support to the French registry for SDH-related paraganglioma (PGL.R) and the Groupe des Tumeurs Endocrines, réseau des laboratoires (TENgen) network.
Footnotes
Contributors: Conceptualisation: A-PG-R, PLD, MR, JPB, NB. Data curation: LBA, AC, FS, RAT, PLD, MR, JPB, NB. Formal analysis: LBA, NB. Methodology: LBA, NB. Resources: ERM, AC, AB, SG, TE, PP, RC-B, DM-P, AM, JF, FS, RAT, PLD, MR, JPB. Supervision: A-PG-R, PLD, MR, NB. Writing-original draft: LBA, NB. Writing-review and editing: LBA, ERM, AC, AB, SG, TE, PP, RC-B, DM-P, AM, JF, A-PG-R, FS, RAT, PLD, MR, JPB, NB.
Funding: This work was supported in part by a salary grant to NB from Cancer Research for PErsonalized Medicine (CARPEM). ERM acknowledges funding from the European Research Council (Advanced Researcher Award), NIHR (Senior Investigator Award and Cambridge NIHR Biomedical Research Centre) and Cancer Research UK Cambridge Cancer Centre. The University of Cambridge has received salary support in respect of ERM from the NHS in the East of England through the Clinical Academic Reserve. PLD receives support from the National Institutes of Health (NIH)-National Institute of General Medical Science (NIGMS) GM114102, NIH-National Center for Advancing Translational Science (NCATS) Clinical Translational Science Award (CTSA) UL1 TR001120 and UL1 TR002645, the Mays Cancer Center NIH-National Cancer Institute (NCI) P30 CA54174, Alex’s Lemonade Childhood Foundation, with support from Northwest Mutual and Flashes of Hope, and University of Texas Health System- STARS Award. RAT holds a Miguel Servet-I research contract by Institute of Health Carlos III (ISCIII) of the Ministry of Economy (CP17/00199) and Competitiveness; is supported by an Olga Torres Foundation Emerging researcher grant and by the Swiss Bridge Award for cancer immunotherapy research; and received research grants from BeiGene, Novartis and AstraZeneca. Cancer Genetics, Kolling Institute, Sydney acknowledges support from the Hillcrest Foundation (Perpetual Trustees). JPB in Leiden, The Netherlands acknowledges support from the Paradifference Foundation. MR is supported by the Instituto de Salud Carlos III (ISCIII), Acción Estratégica en Salud, cofounded by FEDER (grant number PI17/01796).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as supplementary information. Consensus classification of SDHB variants are freely available in the public Leiden Open Variation Database (LOVD) system https://databases.lovd.nl/shared/genes/SDHB.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the institutional review board of CPP Ile de France II (IRB 00001072) and by the UT Health San Antonio (HSC20060069H). The study was performed in agreement with the Declaration of Helsinki. All patients provided local written informed consent for PPGL genetic testing, data collection and use of clinical and genetic data for research projects.
References
- 1. Astuti D, Latif F, Dallol A, Dahia PL, Douglas F, George E, Sköldberg F, Husebye ES, Eng C, Maher ER. Gene mutations in the succinate dehydrogenase subunit SDHB cause susceptibility to familial pheochromocytoma and to familial paraganglioma. Am J Hum Genet 2001;69:49–54. 10.1086/321282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. NGS in PPGL (NGSnPPGL) Study Group, Toledo RA, Burnichon N, Cascon A, Benn DE, Bayley J-P, Welander J, Tops CM, Firth H, Dwight T, Ercolino T, Mannelli M, Opocher G, Clifton-Bligh R, Gimm O, Maher ER, Robledo M, Gimenez-Roqueplo A-P, Dahia PLM. Consensus statement on next-generation-sequencing-based diagnostic testing of hereditary phaeochromocytomas and paragangliomas. Nat Rev Endocrinol 2017;13:233–47. 10.1038/nrendo.2016.185 [DOI] [PubMed] [Google Scholar]
- 3. Lenders JWM, Duh Q-Y, Eisenhofer G, Gimenez-Roqueplo A-P, Grebe SKG, Murad MH, Naruse M, Pacak K, Young WF, Endocrine Society . Pheochromocytoma and paraganglioma: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2014;99:1915–42. 10.1210/jc.2014-1498 [DOI] [PubMed] [Google Scholar]
- 4. Lenders JWM, Kerstens MN, Amar L, Prejbisz A, Robledo M, Taieb D, Pacak K, Crona J, Zelinka T, Mannelli M, Deutschbein T, Timmers HJLM, Castinetti F, Dralle H, Widimský J, Gimenez-Roqueplo A-P, Eisenhofer G. Genetics, diagnosis, management and future directions of research of phaeochromocytoma and paraganglioma: a position statement and consensus of the Working group on endocrine hypertension of the European Society of hypertension. J Hypertens 2020;38:1443–56. 10.1097/HJH.0000000000002438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ben Aim L, Pigny P, Castro-Vega LJ, Buffet A, Amar L, Bertherat J, Drui D, Guilhem I, Baudin E, Lussey-Lepoutre C, Corsini C, Chabrier G, Briet C, Faivre L, Cardot-Bauters C, Favier J, Gimenez-Roqueplo A-P, Burnichon N. Targeted next-generation sequencing detects rare genetic events in pheochromocytoma and paraganglioma. J Med Genet 2019;56:513–20. 10.1136/jmedgenet-2018-105714 [DOI] [PubMed] [Google Scholar]
- 6. Castro-Vega LJ, Lepoutre-Lussey C, Gimenez-Roqueplo A-P, Favier J. Rethinking pheochromocytomas and paragangliomas from a genomic perspective. Oncogene 2016;35:1080–9. 10.1038/onc.2015.172 [DOI] [PubMed] [Google Scholar]
- 7. Currás-Freixes M, Inglada-Pérez L, Mancikova V, Montero-Conde C, Letón R, Comino-Méndez I, Apellániz-Ruiz M, Sánchez-Barroso L, Aguirre Sánchez-Covisa M, Alcázar V, Aller J, Álvarez-Escolá C, Andía-Melero VM, Azriel-Mira S, Calatayud-Gutiérrez M, Díaz José Ángel, Díez-Hernández A, Lamas-Oliveira C, Marazuela M, Matias-Guiu X, Meoro-Avilés A, Patiño-García A, Pedrinaci S, Riesco-Eizaguirre G, Sábado-Álvarez C, Sáez-Villaverde R, Sainz de Los Terreros A, Sanz Guadarrama Óscar, Sastre-Marcos J, Scolá-Yurrita B, Segura-Huerta Ángel, Serrano-Corredor MdelaS, Villar-Vicente MR, Rodríguez-Antona C, Korpershoek E, Cascón A, Robledo M. Recommendations for somatic and germline genetic testing of single pheochromocytoma and paraganglioma based on findings from a series of 329 patients. J Med Genet 2015;52:647–56. 10.1136/jmedgenet-2015-103218 [DOI] [PubMed] [Google Scholar]
- 8. Mannelli M, Canu L, Ercolino T, Rapizzi E, Martinelli S, Parenti G, De Filpo G, Nesi G. Diagnosis of endocrine disease: SDHx mutations: beyond pheochromocytomas and paragangliomas. Eur J Endocrinol 2018;178:R11–17. 10.1530/EJE-17-0523 [DOI] [PubMed] [Google Scholar]
- 9. Amar L, Baudin E, Burnichon N, Peyrard S, Silvera S, Bertherat J, Bertagna X, Schlumberger M, Jeunemaitre X, Gimenez-Roqueplo A-P, Plouin P-F. Succinate dehydrogenase B gene mutations predict survival in patients with malignant pheochromocytomas or paragangliomas. J Clin Endocrinol Metab 2007;92:3822–8. 10.1210/jc.2007-0709 [DOI] [PubMed] [Google Scholar]
- 10. van Hulsteijn LT, Dekkers OM, Hes FJ, Smit JWA, Corssmit EPM. Risk of malignant paraganglioma in SDHB-mutation and SDHD-mutation carriers: a systematic review and meta-analysis. J Med Genet 2012;49:768–76. 10.1136/jmedgenet-2012-101192 [DOI] [PubMed] [Google Scholar]
- 11. Plon SE, Eccles DM, Easton D, Foulkes WD, Genuardi M, Greenblatt MS, Hogervorst FBL, Hoogerbrugge N, Spurdle AB, Tavtigian SV, IARC Unclassified Genetic Variants Working Group . Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum Mutat 2008;29:1282–91. 10.1002/humu.20880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bayley J-P, Devilee P, Taschner PEM. The SDH mutation database: an online resource for succinate dehydrogenase sequence variants involved in pheochromocytoma, paraganglioma and mitochondrial complex II deficiency. BMC Med Genet 2005;6:39. 10.1186/1471-2350-6-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ben AIM L, Maher ER, Cascon A, Barlier A, Giraud S, Ercolino T, Pigny P, Clifton-Bligh RJ, Mirebeau-Prunier D, Mohamed A, Favier J, Gimenez-Roqueplo AP, Schiavi F, Toledo RA, Dahia PLM, Robledo M, Bayley JP, Burnichon N. [Dataset] Data. Available: https://databases.lovd.nl/shared/genes/SDHB [Accessed 21 Jul 2021].
- 14. Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, Committee A, ACMG Laboratory Quality Assurance Committee . Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of medical genetics and genomics and the association for molecular pathology. Genet Med 2015;17:405–23. 10.1038/gim.2015.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lam AK-Y. Update on adrenal tumours in 2017 World Health organization (who) of endocrine tumours. Endocr Pathol 2017;28:213–27. 10.1007/s12022-017-9484-5 [DOI] [PubMed] [Google Scholar]
- 16. Gimenez-Roqueplo A-P, Favier J, Rustin P, Rieubland C, Kerlan V, Plouin P-F, Rötig A, Jeunemaitre X. Functional consequences of a SDHB gene mutation in an apparently sporadic pheochromocytoma. J Clin Endocrinol Metab 2002;87:4771–4. 10.1210/jc.2002-020525 [DOI] [PubMed] [Google Scholar]
- 17. van Nederveen FH, Gaal J, Favier J, Korpershoek E, Oldenburg RA, de Bruyn EMCA, Sleddens HFBM, Derkx P, Rivière J, Dannenberg H, Petri B-J, Komminoth P, Pacak K, Hop WCJ, Pollard PJ, Mannelli M, Bayley J-P, Perren A, Niemann S, Verhofstad AA, de Bruïne AP, Maher ER, Tissier F, Méatchi T, Badoual C, Bertherat J, Amar L, Alataki D, Van Marck E, Ferrau F, François J, de Herder WW, Peeters M-PFMV, van Linge A, Lenders JWM, Gimenez-Roqueplo A-P, de Krijger RR, Dinjens WNM. An immunohistochemical procedure to detect patients with paraganglioma and phaeochromocytoma with germline SDHB, SDHC, or SDHD gene mutations: a retrospective and prospective analysis. Lancet Oncol 2009;10:764–71. 10.1016/S1470-2045(09)70164-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Papathomas TG, Oudijk L, Persu A, Gill AJ, van Nederveen F, Tischler AS, Tissier F, Volante M, Matias-Guiu X, Smid M, Favier J, Rapizzi E, Libe R, Currás-Freixes M, Aydin S, Huynh T, Lichtenauer U, van Berkel A, Canu L, Domingues R, Clifton-Bligh RJ, Bialas M, Vikkula M, Baretton G, Papotti M, Nesi G, Badoual C, Pacak K, Eisenhofer G, Timmers HJ, Beuschlein F, Bertherat J, Mannelli M, Robledo M, Gimenez-Roqueplo A-P, Dinjens WN, Korpershoek E, de Krijger RR. SDHB/SDHA immunohistochemistry in pheochromocytomas and paragangliomas: a multicenter interobserver variation analysis using virtual microscopy: a Multinational Study of the European Network for the Study of Adrenal Tumors (ENS@T). Mod Pathol 2015;28:807–21. 10.1038/modpathol.2015.41 [DOI] [PubMed] [Google Scholar]
- 19. Burnichon N, Vescovo L, Amar L, Libé R, de Reynies A, Venisse A, Jouanno E, Laurendeau I, Parfait B, Bertherat J, Plouin P-F, Jeunemaitre X, Favier J, Gimenez-Roqueplo A-P. Integrative genomic analysis reveals somatic mutations in pheochromocytoma and paraganglioma. Hum Mol Genet 2011;20:3974–85. 10.1093/hmg/ddr324 [DOI] [PubMed] [Google Scholar]
- 20. Dahia PLM, Familial Pheochromocytoma Consortium . Transcription association of VHL and SDH mutations link hypoxia and oxidoreductase signals in pheochromocytomas. Ann N Y Acad Sci 2006;1073:208–20. 10.1196/annals.1353.023 [DOI] [PubMed] [Google Scholar]
- 21. Pasini B, Stratakis CA. Sdh mutations in tumorigenesis and inherited endocrine tumours: lesson from the phaeochromocytoma-paraganglioma syndromes. J Intern Med 2009;266:19–42. 10.1111/j.1365-2796.2009.02111.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Saxena N, Maio N, Crooks DR, Ricketts CJ, Yang Y, Wei M-H, Fan TW-M, Lane AN, Sourbier C, Singh A, Killian JK, Meltzer PS, Vocke CD, Rouault TA, Linehan WM. SDHB-Deficient cancers: the role of mutations that impair iron sulfur cluster delivery. J Natl Cancer Inst 2016;108:djv287. 10.1093/jnci/djv287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Burnichon N, Rohmer V, Amar L, Herman P, Leboulleux S, Darrouzet V, Niccoli P, Gaillard D, Chabrier G, Chabolle F, Coupier I, Thieblot P, Lecomte P, Bertherat J, Wion-Barbot N, Murat A, Venisse A, Plouin P-F, Jeunemaitre X, Gimenez-Roqueplo A-P, network PN, PGL.NET network . The succinate dehydrogenase genetic testing in a large prospective series of patients with paragangliomas. J Clin Endocrinol Metab 2009;94:2817–27. 10.1210/jc.2008-2504 [DOI] [PubMed] [Google Scholar]
- 24. Cascón A, Landa I, López-Jiménez E, Díez-Hernández A, Buchta M, Montero-Conde C, Leskelä S, Leandro-García LJ, Letón R, Rodríguez-Antona C, Eng C, Neumann HPH, Robledo M. Molecular characterisation of a common SDHB deletion in paraganglioma patients. J Med Genet 2008;45:233–8. 10.1136/jmg.2007.054965 [DOI] [PubMed] [Google Scholar]
- 25. Solis DC, Burnichon N, Timmers HJLM, Raygada MJ, Kozupa A, Merino MJ, Makey D, Adams KT, Venisse A, Gimenez-Roqueplo A-P, Pacak K. Penetrance and clinical consequences of a gross SDHB deletion in a large family. Clin Genet 2009;75:354–63. 10.1111/j.1399-0004.2009.01157.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Niemeijer ND, Rijken JA, Eijkelenkamp K, van der Horst-Schrivers ANA, Kerstens MN, Tops CMJ, van Berkel A, Timmers HJLM, Kunst HPM, Leemans CR, Bisschop PH, Dreijerink KMA, van Dooren MF, Bayley J-P, Pereira AM, Jansen JC, Hes FJ, Hensen EF, Corssmit EPM. The phenotype of SDHB germline mutation carriers: a nationwide study. Eur J Endocrinol 2017;177:115–25. 10.1530/EJE-17-0074 [DOI] [PubMed] [Google Scholar]
- 27. Amendola LM, Jarvik GP, Leo MC, McLaughlin HM, Akkari Y, Amaral MD, Berg JS, Biswas S, Bowling KM, Conlin LK, Cooper GM, Dorschner MO, Dulik MC, Ghazani AA, Ghosh R, Green RC, Hart R, Horton C, Johnston JJ, Lebo MS, Milosavljevic A, Ou J, Pak CM, Patel RY, Punj S, Richards CS, Salama J, Strande NT, Yang Y, Plon SE, Biesecker LG, Rehm HL. Performance of ACMG-AMP Variant-Interpretation guidelines among nine laboratories in the clinical sequencing exploratory research Consortium. Am J Hum Genet 2016;98:1067–76. 10.1016/j.ajhg.2016.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rehm HL. A new era in the interpretation of human genomic variation. Genet Med 2017;19:1092–5. 10.1038/gim.2017.90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cline MS, Liao RG, Parsons MT, Paten B, Alquaddoomi F, Antoniou A, Baxter S, Brody L, Cook-Deegan R, Coffin A, Couch FJ, Craft B, Currie R, Dlott CC, Dolman L, den Dunnen JT, Dyke SOM, Domchek SM, Easton D, Fischmann Z, Foulkes WD, Garber J, Goldgar D, Goldman MJ, Goodhand P, Harrison S, Haussler D, Kato K, Knoppers B, Markello C, Nussbaum R, Offit K, Plon SE, Rashbass J, Rehm HL, Robson M, Rubinstein WS, Stoppa-Lyonnet D, Tavtigian S, Thorogood A, Zhang C, Zimmermann M, Burn J, Chanock S, Rätsch G, Spurdle AB, BRCA Challenge Authors . Brca challenge: BRCA exchange as a global resource for variants in BRCA1 and BRCA2. PLoS Genet 2018;14:e1007752. 10.1371/journal.pgen.1007752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Plazzer JP, Sijmons RH, Woods MO, Peltomäki P, Thompson B, Den Dunnen JT, Macrae F. The insight database: utilizing 100 years of insights into Lynch syndrome. Fam Cancer 2013;12:175–80. 10.1007/s10689-013-9616-0 [DOI] [PubMed] [Google Scholar]
- 31. Spurdle AB, Healey S, Devereau A, Hogervorst FBL, Monteiro ANA, Nathanson KL, Radice P, Stoppa-Lyonnet D, Tavtigian S, Wappenschmidt B, Couch FJ, Goldgar DE, ENIGMA . ENIGMA--evidence-based network for the interpretation of germline mutant alleles: an international initiative to evaluate risk and clinical significance associated with sequence variation in BRCA1 and BRCA2 genes. Hum Mutat 2012;33:2–7. 10.1002/humu.21628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Soussi T, Leroy B, Taschner PEM. Recommendations for analyzing and reporting TP53 gene variants in the high-throughput sequencing era. Hum Mutat 2014;35:766–78. 10.1002/humu.22561 [DOI] [PubMed] [Google Scholar]
- 33. Favier J, Amar L, Gimenez-Roqueplo A-P. Paraganglioma and phaeochromocytoma: from genetics to personalized medicine. Nat Rev Endocrinol 2015;11:101–11. 10.1038/nrendo.2014.188 [DOI] [PubMed] [Google Scholar]
- 34. Jochmanova I, Abcede AMT, Guerrero RJS, Malong CLP, Wesley R, Huynh T, Gonzales MK, Wolf KI, Jha A, Knue M, Prodanov T, Nilubol N, Mercado-Asis LB, Stratakis CA, Pacak K. Clinical characteristics and outcomes of SDHB-related pheochromocytoma and paraganglioma in children and adolescents. J Cancer Res Clin Oncol 2020;146:1051–63. 10.1007/s00432-020-03138-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jmedgenet-2020-107652supp001.xlsx (14.2KB, xlsx)
jmedgenet-2020-107652supp002.xlsx (44.2KB, xlsx)
jmedgenet-2020-107652supp003.pdf (35.6KB, pdf)
jmedgenet-2020-107652supp004.pdf (11.3KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All data relevant to the study are included in the article or uploaded as supplementary information. Consensus classification of SDHB variants are freely available in the public Leiden Open Variation Database (LOVD) system https://databases.lovd.nl/shared/genes/SDHB.