Abstract
Objectives
To examine the association between the COVID-19 pandemic and opioid use among nursing home residents followed up to March 2021, and possible variation by dementia and frailty status.
Design
Population-based cohort study with an interrupted time series analysis.
Setting and Participants
Linked health administrative databases for residents of all nursing homes (n = 630) in Ontario, Canada were examined. Residents were divided into consecutive weekly cohorts (first observation week was March 5 to 11, 2017 and last was March 21 to March 27, 2021).
Methods
The weekly proportion of residents dispensed an opioid was examined overall and by strata defined by the presence of dementia and frailty. Autoregressive Integrated Moving Average models with step and ramp intervention functions tested for immediate level and slope changes in weekly opioid use after the onset of the pandemic (March 1, 2020) and were fit on prepandemic data for projected trends.
Results
The average weekly cohort ranged from 76,834 residents (prepandemic) to 69,359 (pandemic period), with a consistent distribution by sex (69% female) and age (54% age 85 + years). There was a statistically significant increased slope change in the weekly proportion of residents dispensed opioids (parameter estimate (β) = 0.035; standard error (SE) = 0.005, P < .001). Although significant for all 4 strata, the increased slope change was more pronounced among nonfrail residents (β = 0.038; SE = 0.008, P < .001) and those without dementia (β = 0.044; SE = 0.008, P < .001). The absolute difference in observed vs predicted opioid use in the last week of the pandemic period ranged from 1.25% (frail residents) to 2.28% (residents without dementia).
Conclusions and Implications
Among Ontario nursing home residents, there was a statistically significant increase in opioid dispensations following the onset of the pandemic that persisted up to 1 year later. Investigations of the reasons for increased use, potential for long-term use and associated health consequences for residents are warranted.
Keywords: COVID-19, opioid use, nursing home, time-series analysis
In Canada and other countries, the COVID-19 pandemic has been associated with pronounced adverse health and quality of life outcomes among older adults living in nursing homes.1, 2, 3 As COVID-19 cases increased across homes, associated staffing shortages and public health restrictions led to significant disruptions in health and social care services and the loss of in-person family/friend caregiver supports for residents.3, 4, 5 As a result, many residents experienced increased social isolation and new or aggravated physical and mental health concerns.6 , 7 These intersecting care and health challenges may have contributed to important changes in the prescribing and clinical oversight of select medication classes that pose potential risks for older residents,8, 9, 10 many of whom are frail and/or have dementia.11
Previously, we showed that the initial wave of the COVID-19 pandemic (March to July 2020) was associated with an increase in the use of psychotropics among nursing home residents in Ontario, Canada.11 We also observed a statistically significant but modest absolute increase (1.1%) in opioid use among residents. The reasons for this rise in opioid use are unclear. It may reflect their increased use for pain or behavioral management coupled with the lack of nonpharmacologic options for these indications,12 , 13 as well as for symptom management and palliative care of residents with COVID-19.14 Conversely, others have suggested the potential for opioid underuse during the pandemic because of disruptions in palliative care services15 and heightened difficulties in assessing pain.13
As both the over- and underuse of opioids may pose serious risks to the health and well-being of residents,16, 17, 18 it is important to understand the longer-term changes in opioid dispensations associated with the COVID-19 pandemic in this care setting and whether use varied for residents more vulnerable to potentially inappropriate use. Our objectives were to examine (1) whether the COVID-19 associated increase in opioid use observed among Ontario nursing home residents during the first wave persisted over the second wave (to March 2021), and (2) if opioid dispensations varied by resident dementia and frailty status. We focused on dementia and frailty to examine resident subgroups with an increased likelihood for opioid use during the pandemic and/or associated adverse effects.12 , 13 , 16
Methods
Study Design and Setting
We conducted a population-based cohort study with interrupted time-series analysis of opioid dispensations among nursing home residents in Ontario, Canada, from March 5, 2017 to March 27, 2021, using clinical and health administrative databases. Ontario's publicly funded provincial health plan covers most nursing home costs, including prescription medications listed on the provincial drug formulary, as well as all medically necessary hospital and physician services. During this period, there were 630 nursing homes in operation in Ontario.
Data Sources and Participants
We used the Registered Persons Database, Ontario Drug Benefit claims database, Discharge Abstract Database, Ontario Health Insurance Plan claims database and Continuing Care Reporting System. Databases were linked using encoded identifiers and analyzed at ICES. This study was authorized under section 45 of Ontario's Personal Health Information Protection Act, which does not require research ethics board review.
For each week in our study period starting on a Sunday (index date), beginning with March 5 to 11, 2017 and ending March 21 to 27, 2021, we created a cohort of persons residing in Ontario nursing homes who were alive and eligible to receive medication on the index date. Nursing home residence was determined using a validated algorithm based on medication claims (Ontario Drug Benefit) and physician visits (Ontario Health Insurance Plan).19 On each weekly index date, we excluded residents concurrently admitted to an inpatient facility (0.3% to 1.2% of residents across study weeks), without a previous full Resident Assessment Instrument Minimum Data Set, version 2.0 (RAI-MDS 2.0; 2.6% to 3.6%) administered, with missing age and/or sex, or ≥110 years of age (<0.01% across study weeks).
Measures
At the index date for each weekly cohort, age, sex and date of death were obtained from the Registered Persons Database and inpatient admissions from the Discharge Abstract Database. Data from residents' most recent full RAI-MDS 2.0 completed prior to the study week were used to derive a validated frailty index20 (with those exhibiting >30% of potential health deficits defined as frail) and identify the presence of dementia (from the diagnostic checklist).
We computed the proportion of residents (per 100) where a course of opioid therapy (estimated using the dispensation data and days supplied) overlapped the observation week by at least one day.11 The 156 weeks prior to, and the 56 weeks post-March 1, 2020, were defined as the prepandemic and pandemic periods, respectively.
Analysis
Autoregressive Integrated Moving Average (ARIMA) models21 , 22 with step and ramp intervention functions were used to test for an immediate level change and slope change in weekly opioid use following March 1, 2020, both in the overall time-series and stratified by resident frailty and dementia status. We first differenced our weekly time-series data by a lag of 1 week to achieve stationarity and account for longitudinal time trends in medication use. Autocorrelation function and partial autocorrelation function correlograms identified the need for moving average terms at a lag of 1 and 2 weeks, and an autoregressive term at a lag of 52 weeks to account for annual trend. We fit our ARIMA models on data from the prepandemic period to forecast predicted opioid use in the hypothetical absence of a pandemic.
In separate sensitivity analyses, we repeated ARIMA modeling: (1) excluding residents with an inpatient hospitalization and/or outpatient consultation for palliative care (since April 2002) prior to each study week; and (2) testing alternate intervention points aligned with Ontario-wide public health restrictions (March 14, 2020) and peak mortality within LTC homes (April 19, 2020).3 , 23
Results
The average weekly cohort ranged from 76,834 residents (prepandemic) to 69,359 (pandemic period). There was a consistent distribution by sex (average 69% female), age (54% age 85 + years) and dementia diagnosis (64%) over these periods. The average proportion of residents defined as frail increased slightly from the pre- (58%) to the post-pandemic (60%) period, as did the average proportion receiving palliative care services or consults (14.2% to 18.5%).
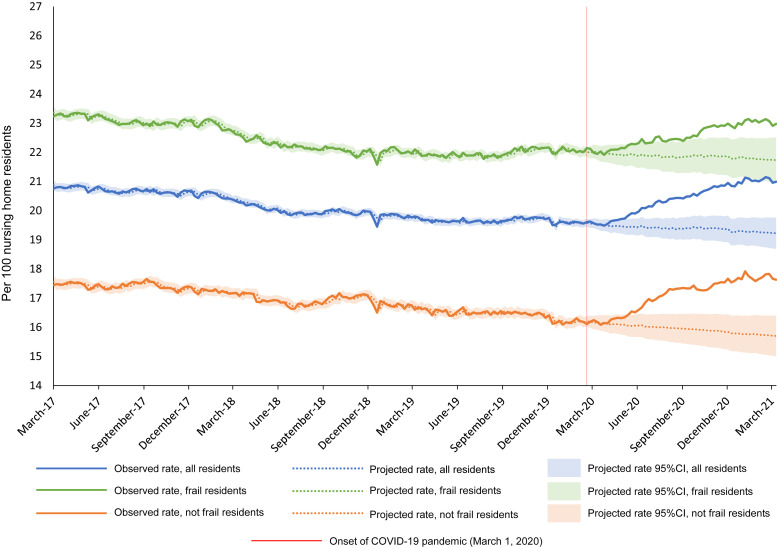
Relative to nonfrail residents, those identified as frail were more likely to be dispensed opioids throughout the study period (Figure 1 ). Those with dementia showed a lower prevalence of opioid use compared with the nondementia group during this period (Figure 2 ). Across all strata there was a modest decline in weekly opioid dispensations evident during the prepandemic period.
Fig. 1.
Observed weekly proportion of Ontario nursing home residents dispensed opioids compared with projected use, all residents and by frailty (frail vs not frail).
Fig. 2.
Observed weekly proportion of Ontario nursing home residents dispensed opioids compared with projected use, all residents and by dementia (diagnosis present vs absent).
Following the onset of the pandemic there was a statistically significant increased slope change in the weekly proportion of residents dispensed opioids [parameter estimate (β) = 0.035; standard error (SE) = 0.005, P < .001] (Table 1 ). Although statistically significant for both nonfrail (β = 0.038; SE = 0.008, P < .001) and frail (β = 0.024; SE = 0.007, P < .001) residents, it was more pronounced in the nonfrail group. Similarly, though there was also a statistically significant increased slope change in the weekly proportion of residents dispensed opioids following the pandemic onset among both those with (β = 0.031; SE = 0.007, P < .001) and without (β = 0.044; SE = 0.008, P < .001) dementia, it was more pronounced among the nondementia group. Consistent findings of a statistically significant increased slope change in opioid dispensations were observed when (1) excluding residents receiving palliative care services (β = 0.037; SE = 0.006, P < .001) and (2) using March 14, 2020 (β = 0.035; SE = 0.005, P < .001) or April 19, 2020 (β = 0.034; SE = 0.006, P < .001) as alternate intervention dates.
Table 1.
ARIMA Model Results Summarizing the Association of the COVID-19 Pandemic With Opioid Prescribing in Ontario Nursing Homes, Overall and by Frailty and Dementia
| Nursing Home Residents | Prepandemic Period∗ |
Pandemic Period† |
Step Intervention‡ |
Ramp Intervention§ |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average Observed Weekly Proportion of Users in Period | Observed Proportion of Users in Last Week of the Period‖ | Average Observed Weekly Proportion of Users in Period | Observed Proportion of Users in Last Week of the Period∗∗ | Predicted†† Proportion of Users in Last Week of the Period∗∗ | Absolute Difference in Observed vs Predicted†† Users in Last Week of the Period∗∗ | Parameter Estimate (SE) | P Value | Parameter Estimate (SE) | P Value | |
| All residents | 20.10 | 19.56 | 20.39 | 20.99 | 19.22 | 1.77 | −0.030 (0.054) | .581 | 0.035 (0.005) | <.001 |
| Resident frailty | ||||||||||
| Not frail | 16.92 | 16.18 | 17.09 | 17.63 | 15.70 | 1.93 | −0.120 (0.084) | .156 | 0.038 (0.008) | <.001 |
| Frail | 22.42 | 22.01 | 22.57 | 22.98 | 21.73 | 1.25 | 0.065 (0.073) | .372 | 0.024 (0.007) | .001 |
| Dementia diagnosis | ||||||||||
| No dementia | 24.97 | 24.05 | 24.98 | 25.63 | 23.35 | 2.28 | −0.100 (0.085) | .241 | 0.044 (0.008) | <.001 |
| Dementia | 17.35 | 16.95 | 17.78 | 18.36 | 16.72 | 1.64 | 0.012 (0.066) | .859 | 0.031 (0.007) | <.001 |
First observation week of period: March 5, 2017 to March 11, 2017; Last observation week of period: February 23 to February 29, 2020.
First observation week of period: March 1, 2020 to March 7, 2020; Last observation week of period: March 21 to March 27, 2021.
The step intervention tests for an initial immediate level change in weekly medication use following the onset of the pandemic.
The ramp intervention tests for a change in the slope of weekly medication use in the pandemic period versus the prepandemic period.
Observation week: February 23 to February 29, 2020.
Observation week: March 21 to March 27, 2021.
The final ARIMA model for each medication class was applied to only observation weeks from the pre-pandemic period to predict use in the hypothetical absence of a pandemic.
The absolute difference in observed vs projected opioid use in the last week of the pandemic period was higher for nonfrail (1.93%) than frail (1.25%) residents and for residents without dementia (2.28%) than with (1.64%) (Table 1; Figures 1 and 2).
Discussion
Among nursing home residents in Ontario, Canada, we observed a statistically significant increase in opioid dispensations following the onset of the pandemic that persisted to the end of March 2021. Unexpectedly, the slope change in opioid use was more pronounced among nonfrail residents and those without dementia. The absolute increase in use across strata 1 year after the onset of the pandemic was generally modest but more pronounced (∼2%) among residents without dementia and those who were not frail.
Data regarding opioid use by nursing home residents during the COVID-19 pandemic are scarce, despite the potential for increased use (for acute or chronic pain)12 , 24 as well as underuse due to poorer pain detection and management13 during this time. Our findings illustrate that the initial rise in opioid use we observed during the first wave of the pandemic11 was not a temporary one but rather remained consistent with a week over week increase in use (ie, positive slope change) over the second wave as well. Though an increase in opioid use during the early months of the pandemic may reflect appropriate and rational prescribing (eg, increased need for end-of-life care and/or management of pain), the finding that this increased use persisted over a period when COVID-19 deaths in Ontario nursing homes were substantially lower23 and remained evident in analyses excluding residents receiving palliative care services, raises concerns regarding both the reasons for continued use and associated opioid-related health risks for older residents. Further investigation via interprofessional case conferences of the factors driving continued opioid use in the nursing home setting and the need for deprescribing interventions are warranted.
Though still statistically significant, the more muted slope change and absolute increase in weekly opioid dispensations evident among frail residents and those with dementia may be viewed positively given their heightened risks for adverse opioid-related effects.16 It also appears that opioids were not primarily being used to manage increased behaviors among residents with dementia during the initial waves of the pandemic, though definitive conclusions require further data on indications for use. An alternative explanation, assuming some increase in opioid prescribing was warranted and appropriate, is that these residents may have been under-treated. It is well known that nursing home residents with cognitive and communication impairments are less likely to have their pain adequately recognized or treated18 and their risk for undertreatment may have increased during the pandemic given staffing shortages and visitor restrictions. Conversely, nonfrail residents and those without dementia may have been able to effectively communicate their pain (and have it recognized by care providers), which may have resulted in their increased likelihood to be dispensed an opioid (especially given the reduced access to nonpharmacologic pain management strategies during the pandemic). Further work is needed to determine if the overall increase in opioid use and differences observed for those with and without frailty or dementia represent appropriate prescribing.
It is also interesting to consider the historical trends in opioid use in nursing homes. Throughout our study period, weekly opioid use was higher among frail residents and those without dementia. We showed similar findings for these strata in an earlier study of opioid prescribing patterns among Ontario nursing home residents between 2009 and 2017.25 However, contrary to our current study illustrating an overall decline in opioid use in the few years prior to the pandemic, this earlier study revealed an increase in prevalent opioid use (largely driven by increased hydromorphone use) that was more pronounced among residents who were frail or had dementia. Though analytical approaches differed between these studies, both reveal important historical and pandemic related changes in opioid prescribing patterns within this care setting that are unlikely to be explained by changing resident characteristics alone.
Important strengths of our study include the use of population-based clinical and health administrative data and robust analytical methods covering the first and second waves of the pandemic. Limitations include the use of dispensations to estimate medication exposure, uncertainty about the persistence of use at the individual level, and absence of information on treatment indications, appropriateness and associated health and quality of life outcomes. We are also unable to comment on the relevance of home specific COVID-19 infection or death rates to the observed opioid changes.
Conclusions and Implications
In this population-based, time-series analysis of Ontario nursing home residents, we observed a statistically significant increase in the use of opioids following the onset of the COVID-19 pandemic that persisted up to 1 year later. Although absolute differences were small, they were more pronounced for residents without dementia or frailty. Prescribers face significant challenges in balancing the need for effective pain management with the potential risks posed by opioid medications in older nursing home residents. These challenges were likely complicated with the emergence of the pandemic and in the absence of clear guidance and policy regarding pain management in nursing home settings, may have contributed to a rise in opioid use that persisted beyond what may be appropriate. There is a need for in-depth investigation of the reasons for this increased opioid use and possible consequences which may include a higher risk of falls and worsening frailty among this population.
Acknowledgments
We thank IQVIA Solutions Canada Inc. for use of their Drug Information File.
Footnotes
This research was funded by the CIHR through operating grant (#PJT 168914, Understanding and optimizing opioid use in long term care), by ICES through an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-term Care (MLTC) and with support from the Ontario Health Data Platform (OHDP), a Province of Ontario initiative to support Ontario's ongoing response to COVID-19 and its related impacts.
The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by the ICES, the MOH or MLTC, the OHDP, its partners, or the Province of Ontario is intended or should be inferred. Parts of this material are based on data and information compiled and provided by CIHI; however, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of CIHI.
CM and SB reported receiving grants from the Canadian Institutes of Health Research (CIHR), Canada, and nonfinancial support from ICES, Canada (formerly Institute for Clinical Evaluative Sciences). Authors have no other conflicts of interest to disclose.
The data set from this study is held securely in coded form at ICES. Although data sharing agreements prohibit ICES from making the data set publicly available, access may be granted to those who meet prespecified criteria for confidential access at https://www.ices.on.ca/DAS. Please contact the authors for any supplemental information related to the study such as the study protocol, analysis plan, or analytic code. The full data set creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely on coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
References
- 1.Public Health Agency of Canada COVID-19 Surveillance and Epidemiology Team Descriptive epidemiology of deceased cases of COVID-19 reported during the initial wave of the epidemic in Canada, January 15 to July 9, 2020. Can Commun Dis Rep. 2020;46:344–348. doi: 10.14745/ccdr.v46i10a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Comas-Herrera A., Zalakaín J., Lemmon E., et al. Mortality associated with COVID-19 in care homes: international evidence. 2021. https://ltccovid.org/wp-content/uploads/2021/02/LTC_COVID_19_international_report_January-1-February-1-1.pdf
- 3.Canadian Institute for Health Information . CIHI; Ottawa, ON: 2021. The Impact of COVID-19 on Long-Term Care in Canada: Focus on the First 6 Months.https://www.cihi.ca/sites/default/files/document/impact-covid-19-long-term-care-canada-first-6-months-report-en.pdf [Google Scholar]
- 4.Xu H., Intrator O., Bowblis J.R. Shortages of staff in nursing homes during the COVID-19 pandemic: what are the driving factors? J Am Med Dir Assoc. 2020;21:1371–1377. doi: 10.1016/j.jamda.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verbeek H., Gerritsen D.L., Backhaus R., et al. Allowing visitors back in the nursing home during the COVID-19 crisis: a Dutch national study into first experiences and impact on well-being. J Am Med Dir Assoc. 2020;21:900–904. doi: 10.1016/j.jamda.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levere M., Rowan P., Wysocki A. The adverse effects of the COVID-19 pandemic on nursing home resident well-being. J Am Med Dir Assoc. 2021;22:948–954. doi: 10.1016/j.jamda.2021.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu C.H., Wang J., Fukui C., et al. The impact of COVID-19 on social isolation in long-term care homes: perspectives of policies and strategies from six countries. J Aging Soc Policy. 2021;33:459–473. doi: 10.1080/08959420.2021.1924346. [DOI] [PubMed] [Google Scholar]
- 8.Ailabouni N.J., Hilmer S.N., Kalisch L., et al. COVID-19 pandemic: considerations for safe medication use in older adults with multimorbidity and polypharmacy. J Gerontol A Biol Sci Med Sci. 2021;76:1068–1073. doi: 10.1093/gerona/glaa104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard R., Burns A., Schneider L. Antipsychotic prescribing to people with dementia during COVID-19. Lancet Neurol. 2020;19:892. doi: 10.1016/S1474-4422(20)30370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leontjevas R., Knippenberg I.A.H., Smalbrugge M., et al. Challenging behavior of nursing home residents during COVID-19 measures in the Netherlands. Aging Ment Health. 2021;25:1314–1319. doi: 10.1080/13607863.2020.1857695. [DOI] [PubMed] [Google Scholar]
- 11.Campitelli M.A., Bronskill S.E., Maclagan L.C., et al. Comparison of medication prescribing before and after the COVID-19 pandemic among nursing home residents in Ontario, Canada. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.18441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clauw D.J., Häuser W., Cohen S.P., Fitzcharles M.A. Considering the potential for an increase in chronic pain after the COVID-19 pandemic. Pain. 2020;161:1694–1697. doi: 10.1097/j.pain.0000000000001950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheikh F., Elon R.D., Katz M.J., Brandt N. COVID-19 pandemic and management of chronic pain in nursing homes. J Am Med Dir Assoc. 2021;22:518–519. doi: 10.1016/j.jamda.2021.01.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reppas-Rindlisbacher C., Rochon P.A., Stall N.M. The COVID-19 pandemic and drug prescribing in Ontario nursing homes—from confinement syndrome to unconfined prescribing. JAMA Netw Open. 2021;4:e2119028. doi: 10.1001/jamanetworkopen.2021.19028. [DOI] [PubMed] [Google Scholar]
- 15.Martinsson L., Strang P., Bergström J., Lundström S. Were clinical routines for good end-of-life care maintained in hospitals and nursing homes during the first three months of the outbreak of COVID-19? A national register study. J Pain Symptom Manage. 2021;61:e11–e19. doi: 10.1016/j.jpainsymman.2020.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLachlan A.J., Bath S., Naganathan V., et al. Clinical pharmacology of analgesic medicines in older people: impact of frailty and cognitive impairment. Br J Clin Pharmacol. 2011;71:351–364. doi: 10.1111/j.1365-2125.2010.03847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lapane K.L., Quilliam B.J., Chow W., Kim M. The association between pain and measures of well-being among nursing home residents. J Am Med Dir Assoc. 2012;13:344–349. doi: 10.1016/j.jamda.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Lapane K.L., Dubé C., Hume A.L., et al. Priority-setting to address the geriatric pharmacoparadox for pain management: a nursing home stakeholder Delphi study. Drugs Aging. 2021;38:327–340. doi: 10.1007/s40266-021-00836-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ng R., Lane N., Tanuseputro P., et al. Increasing complexity of new nursing home residents in Ontario, Canada: a serial cross-sectional study. J Am Geriatr Soc. 2020;68:1293–1300. doi: 10.1111/jgs.16394. [DOI] [PubMed] [Google Scholar]
- 20.Maclagan L.C., Maxwell C.J., Gandhi S., et al. Frailty and potentially inappropriate medication use at nursing home transition. J Am Geriatr Soc. 2017;65:2205–2212. doi: 10.1111/jgs.15016. [DOI] [PubMed] [Google Scholar]
- 21.Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helfenstein U. The use of transfer function models, intervention analysis and related time series methods in epidemiology. Int J Epidemiol. 1991;20:808–815. doi: 10.1093/ije/20.3.808. [DOI] [PubMed] [Google Scholar]
- 23.Ontario Agency for Health Protection and Promotion (Public Health Ontario) Queen's Printer for Ontario; Toronto, ON: 2021. Enhanced Epidemiological Summary: COVID-19 in Long-Term Care Home Residents in Ontario - January 15, 2020 to February 28, 2021.https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/06/covid-19-epi-ltch-residents.pdf?la=en [Google Scholar]
- 24.Brennan P.L., SooHoo S. Effects of mental health disorders on nursing home residents' nine-month pain trajectories. Pain Med. 2020;21:488–500. doi: 10.1093/pm/pnz177. [DOI] [PubMed] [Google Scholar]
- 25.Iaboni A., Campitelli M.A., Bronskill S.E., et al. Time trends in opioid prescribing among Ontario long-term care residents: a repeated cross-sectional study. CMAJ Open. 2019;7:e582–e589. doi: 10.9778/cmajo.20190052. [DOI] [PMC free article] [PubMed] [Google Scholar]