Abstract
Objectives
The aim of the current study is to gain insight into the factors that benefit vitality and resilience of healthcare workers during the COVID-19 pandemic, to develop and direct specific support strategies.
Design, setting and participants
This study applies a qualitative design, consisting of six focus groups and five interviews among 38 frontline healthcare workers in a large Dutch academic hospital. Included were professionals of the intensive care unit, COVID-19 departments, infection prevention units and facility management services. The study was conducted in October and November 2020, during the second wave of the COVID-19 pandemic.
Data analysis
Thematic analysis was applied to focus group and interview data to gain insight into the factors that contribute to maintaining vitality and resilience, and to assess specific support needs.
Results
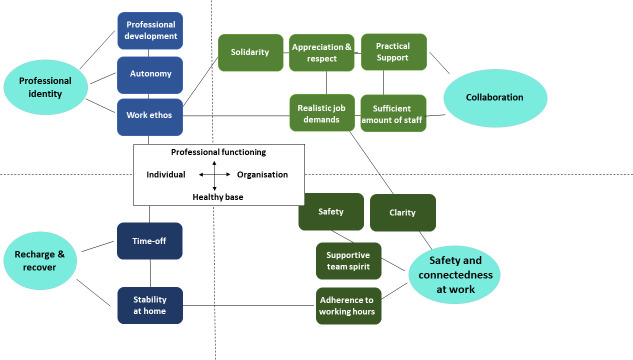
Data analysis of the focus groups and individual interviews resulted in a thematic map of the factors that contribute to maintaining resilience and vitality. The map stretches over two axes: one ranging from a healthy basis to adequate professional functioning and the other from individual to organisation, resulting in four quadrants: recharge and recover (healthy basis, individual), safety and connectedness at work (healthy basis, organisational), collaboration (professional functioning, organisational) and professional identity (professional functioning, individual).
Conclusion
Areas for organisational support strategies to increase vitality and resilience among healthcare professionals are: consistent communication, realistic job performance expectations, monitor and improve mental resilience, showing appreciation and act upon practical support requests.
Keywords: COVID-19, mental health, qualitative research
Strengths and limitations of this study.
This study goes beyond merely assessing stress and mental health reports of healthcare professionals during the COVID-19 pandemic.
A qualitative design was applied to study the specific support needs of healthcare professionals.
Study insights are summarised in two concise thematic maps, which suggest feasible interventions to meet healthcare professionals’ support needs.
However, the effectiveness of the proposed interventions has not been tested yet.
The study protocol intended a mixed-method design; however, the survey response rate was not sufficient to draw valid conclusions; therefore, these results were omitted from reporting.
Introduction
The COVID-19 pandemic had a significant impact on the physical and mental functioning of healthcare professionals.1–6 The need for high-intensity medical care rapidly increased during the COVID-19 pandemic, resulting in stressful work circumstances.7 First, at the departments in direct contact with patients with COVID-19, professionals were confronted with the intensity of continuously wearing personal protective equipment, changes in responsibilities and tasks, moral dilemmas and the risk of infection for the healthcare professionals themselves and consequently their families.8–16 Interpersonal contact with patients’ family members, one of the core features of the professional practice of nurses, was dramatically reduced due to visiting limitations in most hospitals.17 18 This sudden shift in activities and responsibilities required additional competences to maintain high-quality healthcare. Second, professionals at non-COVID-19 departments were confronted with a sudden change of or reduction in tasks, as all focus was on the COVID-19 departments. This resulted in delay of treatment of non-COVID-19 healthcare problems and scheduled appointments, including increased waiting times.19–21 Third, the COVID-19 pandemic not only impacted the healthcare workers within hospitals but also hospital workers who suddenly had to work from home. In addition to the temporary loss of the work environment and direct contact with colleagues, homeworkers might lack a sense of purpose, solidarity and valuable contribution to the crisis situation.22
In the short term, work-related stressors can cause fatigue, sleep disorders, mistakes and moral distress.23 Long-term effects of high work pressure include burnout, depression and post-traumatic stress disorder, which may result in dropout due to sick leave or abandonment of paid employment.24–26 These adverse outcomes can be counterbalanced by vitality, resilience and job satisfaction of professionals.27 28 Strengthening of these aspects may positively influence healthcare professionals’ retention for work, which may be even more necessary in times of crisis.29–31 Therefore, the aim of the current study is to gain insight into the factors that benefit vitality and resilience, to develop and direct support strategies that meet healthcare professionals’ needs.
Methods
Study design
A qualitative design was applied. The study consisted of focus groups and individual interviews, carried out in the Erasmus University Medical Center, a large academic hospital in the Netherlands with 16 485 employees and 1125 beds, located in the second largest city of the Netherlands and one of the leading national hospitals in the COVID-19 related care. There were 68 intensive care unit (ICU) beds, of which half were taken by patients with COVID-19, and two clinics with together 42 beds, with in total 34 patients with COVID-19 admitted at the time the study was conducted (reference date 2 November 2020). The study protocol was previously published.32 The study was originally set up as a mixed-methods study. It was foreseen that a sufficient number of hospital workers would respond to in-company announcements to fill out an online survey. In practice, the number of respondents was lower than expected (<5% of the employees), and no ‘random’ selection could be made in such a way that results would be representative. Therefore, we only report the results of the qualitative component of the planned study. The study was conducted in October and November 2020, during the second wave of the COVID-19 pandemic. The study was supported by the Hospital Board of Directors.
Patient and public involvement
Patients and the public were not involved in the design and conduct of this study.
Participants
Intended groups for the focus groups were: professionals from the ICU, the COVID-19 department, the infection prevention unit and workers of the facility management services. Participants were selected and invited by the research team in collaboration with the team managers or division managers. Intended group size was 6 to 10 participants. Participation was voluntary and all participants provided written informed consent and filled out a short questionnaire on demographic variables. Focus groups were led by LWK, with the support of MVM. Both are female senior investigators with a background in psychology. Both are clinicians as well, one in the field of psychiatry (LWK) and the other in the field of ICU nursing (MVM).
Measures
Based on the literature, a topic list was created to guide and structure the focus group meetings (online supplemental appendix S1). The two main questions were: (1) ‘Which factors contribute to maintaining or regaining vitality and resilience, during the second COVID-19 wave?’ and (2) ‘Based on the factors just mentioned, what would be interventions, or policies, that are appropriate to your needs (in terms of maintaining resilience and vitality)?’. So the second question build on the answers given to the first question. For each of the two main questions, the answers were further explored to gain understanding of why/what caused that the factors or interventions mentioned were so important for maintain vitality and resilience. Prior to each meeting, participants provided written informed consent and filled out a short questionnaire on demographic variables.
bmjopen-2021-059124supp001.pdf (210.3KB, pdf)
Data analysis
Focus groups and interview data were analysed by means of thematic analysis.33 This method allows for a detailed and rich description and organisation of the data and investigation of patterns of response or meaning within the data set. Our analysis takes an essentialist, semantic approach and combined inductive and deductive analysis. To start with, the focus groups and individual interview data were audiotaped and transcribed verbatim by an external professional organisation for interview transcription in healthcare. Next, two researchers (MRdV and LWK) read the transcripts in detail and performed preliminary manual coding of the transcripts. Each one of them individually developed a list of preliminary (sub)themes. They made use of mind maps (MRdV) and tables (LWK) to organise the data. After that, they compared and discussed both their lists until agreement on one single analysis framework. Only after that, one researcher (MRdV) coded all transcripts line by line, according to the coding framework in NVivo V.12 software. Memos for comments were used during coding. In case the code ‘other’ was used for a specific text fragment, these fragments were discussed by both researchers and assigned to a new or existing subtheme best reflecting the contents of the otherwise uncategorised text fragment. During and after coding, the two researchers met regularly to review and check the (sub)themes for internal homogeneity and external heterogeneity. The two researchers examined each (sub)theme for its interrelation with other (sub)themes. Based on this analysis, overarching themes were defined to come to a coherent account and accompanying narrative of the data to answer each of the two research questions.
Results
Demographics
Six focus groups were held with intensivists, infection prevention experts, assistant infection prevention experts, nurses of COVID-19 wards, physicians COVID-19 departments (pulmonologists and internist/infectiologists) and workers from the facility management services. It proved difficult to invite sufficient numbers of healthcare workers at the same time to meet the intended group sizes, due to the high workload these professionals faced during the second COVID-19 wave. We, therefore, reduced the group size to four to eight participants and included an extra focus group (facility management services). Because of the high workload and time constraints, the scheduled focus group interview with ICU nurses was replaced by three individual interviews. Due to the limited number of medical microbiologists, the focus group has been replaced by two individual interviews. All interviews were conducted by LWK. A total of 38 professionals participated in the focus groups and interviews (see table 1).
Table 1.
Demographic data participant focus groups (N=38).
| N | |
| Gender | |
| Male | 11 |
| Female | 27 |
| Age (in years) | |
| <25 | 1 |
| 26–35 | 10 |
| 36–45 | 11 |
| 46–55 | 6 |
| 56> | 10 |
| Function | |
| Physician | 13 |
| Nurse | 7 |
| Expert infection prevention assistant | 8 |
| Infection prevention | 4 |
| Facility service worker | 6 |
Factors contributing to the vitality and resilience of healthcare workers during COVID-19
Data analysis resulted in 4 main and 14 subthemes. The examination of each subtheme for its contribution to (build or maintain) vitality and resilience, and the analysis of the cohesion and inter-relations between themes according to this rationale, resulted to in a thematic map (figure 1). The map has two axes: one ranging from a healthy basis to adequate professional functioning and the other from individual to organisation, resulting in four quadrants: recharge and recover (healthy basis, individual), safety and connectedness at work (healthy basis, organisational), collaboration (professional functioning, organisational) and professional identity (professional functioning, individual). The themes and subthemes are described in detail below.
Figure 1.
Thematic map of factors contributing to vitality and resilience.
Recharge and recover (healthy basis, individual factors)
This theme refers to the possibility to recharge and recover from working, as this was perceived of crucial importance to continue working in the current situation and also to ensure employability in the future. In this sense, this theme also is about the sustainability of workers and their retention for work. Subthemes are ‘time-off’ and ‘stability at home’.
Time-off
This subtheme refers to time-off from work, and also to the expressed wish to take a break from COVID-19 in general. Time-off could be spent in various ways, named were sports, hobbies, time with family and time to rest. In some instances, increased time needed for recovery was reported:
after three weeks of holiday, I thought: I can take it completely 200%! But the curve spiralled down much faster than the first time, also because there are just too many other things at play that need attention…. people who are ill or take care of others, but colleagues as well. Of whom you think, yes, you know, when are they going to collapse?
Stability at home
A stable home situation was considered of extra importance during the hectic of the pandemic. It was important as a source of joy and support, but sometimes as an extra stressor when it comes to combining a hectic work situation with children at home school and informal care tasks.
…in the end you want your child to be doing all right. And that just gives you peace of mind. And I can work just fine if I know that my daughter is taken care off.
Safety and connectedness at work (healthy basis, organisational factors)
This theme refers to the importance of feeling safe at work, whether it is with regard to one’s own health and sufficient protection material (subtheme ‘safety’), or with regard to knowing what to do expect at work, as the absence of this can cause feelings of insecurity (subtheme ‘clarity’). The subtheme ‘adherence to working hours’ may seem a bit of an outsider here, but this subtheme is included because limiting working over hours was perceived as a protective factor/safeguard against exhaustion. This theme also refers to the importance of a sense of belonging and feeling at ease with direct colleagues as is covered by the subtheme ‘supportive team spirit’.
Safety
This subtheme covers several areas and included good and sufficient protective personal equipment, supervision of compliance with the COVID-19 rules by hospital staff and by visitors, stability of the work environment and the protection of older/vulnerable staff. For instance, the quote below is from a professional who felt unsafe at times because of a vulnerable health:
So that is already a pressure on me personally, that I belong to a high-risk population.
Clarity
Clarity was needed first and for all with regards to knowing which care will and will not continue, and per when. Furthermore, respondents marked clarity with regards to the division of tasks within the team, and regarding the COVID-19 rules on the work floor as important:
I would like to see more clarity indeed. That you do the tasks that you are actually there for, so to say
Supportive team spirit
This subtheme refers to a healthy basis of individual workers within the team and entails the importance of safety and trust within a team. It also includes a sense of belonging and connection with team members, for instance via humour:
Sometimes almost morbid humour, but that is what you need to process things.
Adherence to working hours
Topics within this subtheme were: taking breaks, setting limits to overtime and having the possibility to take days off/vacation. These help to prevent getting overinvolved in work and to keep sufficient personal distance to work. The quote below illustrates the difference between occasional and structural working late:
Yesterday I wasn't home until eight o'clock and at nine o'clock I was already behind the computer until eleven o'clock. Yes, and this morning I was here again at 7:30 am. That’s nice for once, but it just keeps going.
Collaboration (professional functioning, organisational factors)
This theme is about aspects of work related to working together in a large hospital. Subthemes often include quotes about perceived or hoped for communication and behaviour by the ‘the higher management layers’, for instance about which and how expectations on work (performance) are being communicated. Subthemes within this theme are ‘solidarity’, ‘appreciation and respect’, ‘practical support’, ‘realistic job demands’ and ‘sufficient amount of staff’.
Solidarity
This subtheme refers to solidarity within the team, between departments within the hospital and between hospital regions in the Netherlands.
I think the best thing we can learn from the first wave and what we should try to take into the second wave is solidarity. It’s gone now. And I think that says it all.
Appreciation and respect
This subtheme was defined in terms of personal attention, showing appreciation, being trusted, realism, respect, sincere and adequate responding to answers when asked ‘what do you need?’, and bonus/salary. The following quote combines several of these elements:
Appreciation starts to feel like a trick the moment you don't support it with…. If you don't act like it.
Practical support
Generic topics were: food in the department (soup, fruit), grocery shopping service, good parking opportunities, support for childcare and timely replenishment of materials at departments. Department-specific topics were: well-equipped ICU overnight rooms, better aprons in the ICU, work telephones with e-mail function and good-quality material for internal transport. The quote below provides an example of generic type of practical support:
I think what they [the hospital board] did with the delivery service of those groceries, that was a very good move to relieve your private life.
Realistic job demands
This subtheme was the positive counterpart of a “high workload”, as this quote below illustrates:
But what seriously threatens vitality and resilience, I think, is the fact that now you are also expected to keep the plates spinning. And if you think logically, you just can not.
Sufficient amount of staff
This was a recurrent topic throughout all layers of the organisation; from structural secretarial support to medical specialists. An example is the following quote:
You want to be able to do your job well. And if the shortness of staff forces you to deliver poor quality work, that’s just not in your nature
Professional identity (professional functioning, individual factors)
This theme refers to the more individualistic work-related aspects that contribute to staying vital at work. Subthemes refer to the possibility to grow in one’s work (subtheme ‘professional development’), various aspects of professional autonomy (subtheme ‘autonomy’) and personal beliefs on and values in how one’s work-related tasks should be carried out (subtheme ‘work ethos’).
Professional development
This subtheme refers to the opportunity to continue academic tasks and career development next to providing patient care during COVID-19 and access to professional training and education, as the quote below shows:
You now face situations that you would probably not have faced normally during your career as resident, so you may also learn things from that.
Autonomy
Autonomy in job performance, for example, about the timing of breaks and working from home was considered important to persevere harsh working circumstances. This subtheme also referred to respect for the autonomy from specific occupational groups. The quote below illustrates the importance of autonomy and was said in the context that workers were repeatedly reminded not to use too many face masks because of scarcity:
It feels like you're being reprimanded, like a little kid. As if you can't bear the responsibility yourself. It’s really not that I walk with a mask for fun…
Work ethos
This subtheme refers to delivering quality, achieving success, being able to contribute, pleasure in work, curiosity, facing challenges, being meaningful. People find satisfaction and self-esteem in the fact that they can do their work in a high-quality way. If this is not possible, for whatever reason, this has a negative impact on resilience and vitality, as this quote shows:
Look, as of my profession, I have seen many patients dying and that is what it is, provided you have done everything you can do. But if you get the feeling that you have fallen short and that perhaps in another era, that patient would have survived, that is a feeling you may have for a while, but you should not have for too long…
Organisational interventions that could contribute to vitality and resilience
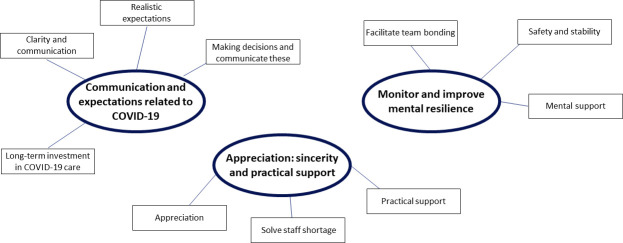
Analysis of the focus group and interview data on which interventions would benefit the vitality and resilience of healthcare workers resulted in three main themes, all referring to areas for organisational support strategies to increase vitality and resilience among professionals: communication and expectations related to COVID-19; monitor and improve the mental resilience of workers and appreciation: sincerity and practical support. The thematic map is presented in figure 2, and the main themes with their subthemes are addressed the text below.
Figure 2.
Thematic map of organisational interventions that could contribute to vitality and resilience.
Communication and expectations related to COVID-19
During this second COVID-19 wave, there was a clear informational need among respondents, for instance, with regards to the downscaling of regular care and upscaling of COVID-19 care. Furthermore, consistency in communication was felt to be important: getting different messages is confusing and may even lead to a decreased support for organisational policy. In addition to making decisions and communicating these, respondents felt it was important for the higher management to have realistic expectations. It was perceived unrealistic to continue all care at the same pace during the persisting pandemic. Long-term investment in COVID-19 care was suggested as an option to combat ad hoc organisation of this type of care. This was thought to potentially benefit the continuity of personnel, quality and professional development opportunities.
Monitor and improve mental resilience
First, we found that professionals derive support and strength from contact with their colleagues. Second, although the availability of mental support teams was positively valued, few made use of them. At the same time, respondents indicated that such help would be beneficial for others. Triage in offering mental support is required: easy accessible and at team level when possible, but with the option for rapidly scaling up to individual professional help when needed. Furthermore, it was noted that the fulfilment of basic human needs, such as safety and rest, also contributes to professionals’ mental resilience. Professionals who are feeling unsafe or depleted from energy do not have their full capacity to perform on work-related tasks that require focus, decision-making capacities and emotional stability.
Appreciation: sincerity and practical support
Feeling appreciated and supported by management and/or coworkers was described as important for maintaining vitality. When it comes to expressing appreciation, it was felt important that this was done in a sincere and person-directed manner. Respondents were adverse to compliments just for the sake of compliments, and in those situations, compliments sorted adverse effect. In addition, our results showed that the need for appreciation existed through all organisational layers, so not only along top–down lines, but also vice versa and horizsontally. Furthermore, it was mentioned that when managers informed on what they could do to help, they should also be reliable in the follow-up to the responses given. In this sense, practical support, be it on specific requests or in general, was also experienced as an expression of appreciation. A specific type of practical support mentioned was support in terms of attracting new personnel to alleviate work pressure.
Discussion
Data analysis resulted in a thematic map of the factors that contribute to maintaining resilience and vitality in healthcare professionals during the COVID-19 pandemic. This map was derived by inductive analysis of our focus groups and interview data. However, reflecting on our map, one may note resemblance with existing theories in organisational and clinical psychology.34 35 In this respect, it may be helpful to examine our findings in conjunction with the Job Demands-Resources model of burnout.35 This model discerns job demands and job resources. Job demands refer to ‘those physical, social or organisational aspects of the job that require sustained physical or mental effort and are, therefore, associated with certain physiological and psychological costs’. As described in the introduction, working during the COVID-19 pandemic comes with a number stressors,7–15 17 18 which add to the already existing job demands. High job demands are related to exhaustion,35 a core symptom of burnout. Indeed, our findings as well as those of other studies and guidelines underline the importance of getting enough rest and having the opportunity to recharge.36–38 Job resources present the other side of the coin and refer to ‘those physical, psychological, social or organisational aspects of the job that are functional in achieving work goals; reduce job demands at the associated physiological and psychological costs and stimulate personal growth and development’. In this way, one could say that our findings as presented in figure 1 represent the resources that were considered important by the participants. Interestingly, our findings here are largely covered by the five domains of basic human needs as discerned in schema-focused therapy,34 a widely used type of psychotherapy. These domains are: attachment and security; autonomy; competence and identity; freedom to express important needs and feelings; spontaneity and play and realistic boundaries and self-control. Sufficient resources are needed to cope with environmental demands and meet personal professional standards in job performance. If this is not the case, an individual may respond with reduced motivation and finally job withdrawal as a means to protect oneself against future frustration and (perceived) failure.35 This underlines the importance for organisations to invest in retaining the resources of and for their healthcare workers. Our findings offer insight into the most important resources in this respect (figure 1) and the areas for organisational interventions (figure 2).
Results from the focus groups and interviews showed that both practical and team support were valued highly in the support needs of healthcare professionals during COVID-19. With regards to support from the managers, it was emphasised that this support should be sincere and that both listening to and acting on expressed needs were important. These findings are in line with findings from other recent studies.39–42 Of particular interest, here is the study by Bennett et al42 where data of healthcare workers experience was collected through an anonymous website.42 Results of this study showed that lack of support by the senior management severely impacted on professionals’ well-being and motivation. Similarly, the study by Dopelt et al16 found that a lack of recognition and appreciation led to frustration and disappointment in healthcare workers.16 Next to support by managers, team support and bonding turned out to be important. For this purpose, people usually reverted to natural, pre-existing bonds of trust. The power of positive team spirit and bonding should not be underestimated: it is known from the literature on major disasters that the connection between members from the same group (ie, the community), harbours strong protective and healing potential.26 39 43 Furthermore, a study by Muller et al44 found that healthcare workers reported low interest in professional help and greater reliance on social support and contact; and that social support correlated with less mental health problems during the COVID-19 pandemic.44 These findings underline the need for interventions aiming at facilitating support at the workplace, especially as these may help to identify those workers who are in need for more intensive treatment.45
A strength of this study lies in the succeeding of that many live focus group interviews in a short time span, wherein busy participants were both allowed and took the time to participate in his study. The fact that one of the senior investigators (MVM) involved in the focus group interviews is experienced as ICU nurse, which is both a strength and a limitation. The strength lies in increased sensitivity to issues at stake at an ICU ward. A limitation, however, may be potential difficulty to take an outsider position. Therefore, interviews with ICU nurses where held by LK solely. Another limitation of this study is the selection of focus groups, which included frontline healthcare workers only. Overall outcomes would be more generalisable if we also had included groups of homeworkers and professionals from non-COVID departments. Another limitation of this study concerns the low response rate on the survey. Consequently, no ‘random’ selection could be made for the quantitative study, and reporting these results would evoke questions about the representativeness of the results. We, therefore, could not report this study as a mixed-methods study, as was originally intended.
Furthermore, these results are obtained at a large academic hospital in Western Europe, and results, therefore, cannot be generalised, as perceptions and values of professionals may differ according to culture and context.
Conclusion
This study provides insight into the specific support needs of healthcare workers during the COVID-19 pandemic. Our results point towards the importance of clear and consistent communication, realistic job performance expectations, the monitoring and improvement of mental resilience, showing sincere appreciation and acting on practical support requests. Consequently, organisational interventions to monitor and promote vitality and resilience among healthcare professionals during the COVID-19 pandemic should focus on these particular topics.
Supplementary Material
Acknowledgments
The authors would like to thank all the participating respondents for their involvement in the study.
Footnotes
Contributors: LWK: study design, data collection, data analysis, writing of the paper; guarantor author with MVM MRdV: data collection, data analysis, writing of the paper; KOH: review of the paper; TAK-P: review of the paper; AdP: review of the paper; WJGH: study design, review of the paper; JJVB: study design, review of the paper; MVM: study design and protocol, data collection, review of the pape, guarantor author with LWK.
Funding: This work was internally supported by the board of Erasmus MC (no grant number applicable).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Anonymised data gathered and analysed during the current study are not publicly available due to legal and ethical restrictions. These data can be requested from the corresponding author at a reasonable request by scientists wishing to use them for non-commercial purposes.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants but Erasmus MC Medical Ethics Committee (MEC-2020-0705) exempted this study Participants gave informed consent to participate in the study before taking part.
References
- 1.Azoulay E, De Waele J, Ferrer R, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 2020;10:1–8. 10.1186/s13613-020-00722-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kok N, Hoedemaekers A, van der Hoeven H, et al. Recognizing and supporting morally injured ICU professionals during the COVID-19 pandemic. Intensive Care Med 2020;46:1653–4. 10.1007/s00134-020-06121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901–7. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3:e203976–e76. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solms L, van Vianen AEM, Theeboom T, et al. Keep the fire burning: a survey study on the role of personal resources for work engagement and burnout in medical residents and specialists in the Netherlands. BMJ Open 2019;9:e031053. 10.1136/bmjopen-2019-031053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prins JT, Hoekstra-Weebers JEHM, van de Wiel HBM, et al. Burnout among Dutch medical residents. Int J Behav Med 2007;14:119–25. 10.1007/BF03000182 [DOI] [PubMed] [Google Scholar]
- 7.Trappenburg J, Bleijenberg N, Cate D. Co-Fit: Behoud van korte en Lange termijn fysieke/mentale gezondheid en inzetbaarheid van zorgprofessionals blootgesteld AAN Covid-19 crisis werkomstandigheden. UMCU/HU/THINC, 2020. [Google Scholar]
- 8.Gold JA. Covid-19: adverse mental health outcomes for healthcare workers. British Medical Journal Publishing Group, 2020. [DOI] [PubMed] [Google Scholar]
- 9.Maunder R, Hunter J, Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168:1245–51. [PMC free article] [PubMed] [Google Scholar]
- 10.Ulrich CM. Ebola is causing moral distress among African healthcare workers. BMJ 2014;349:g6672. 10.1136/bmj.g6672 [DOI] [PubMed] [Google Scholar]
- 11.Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009;54:302–11. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bukhari EE, Temsah MH, Aleyadhy AA, et al. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak perceptions of risk and stress evaluation in nurses. J Infect Dev Ctries 2016;10:845–50. 10.3855/jidc.6925 [DOI] [PubMed] [Google Scholar]
- 13.Zhu Z, Xu S, Wang H. COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. MedRxiv 2020. [Google Scholar]
- 14.Xiao H, Zhang Y, Kong D, et al. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 2020;26:e923549. 10.12659/MSM.923549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Wang C, Pan W, et al. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in Wuhan and Shanghai, China. Front Psychiatry 2020;11:1154. 10.3389/fpsyt.2020.565520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dopelt K, Bashkin O, Davidovitch N, et al. Facing the Unknown: Healthcare Workers’ Concerns, Experiences, and Burnout during the COVID-19 Pandemic—A Mixed-Methods Study in an Israeli Hospital. Sustainability 2021;13:9021. 10.3390/su13169021 [DOI] [Google Scholar]
- 17.Bagnasco A, Zanini M, Hayter M, et al. COVID 19-A message from Italy to the global nursing community. J Adv Nurs 2020;76:2212–4. 10.1111/jan.14407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murthy S, Gomersall CD, Fowler RA. Care for critically ill patients with COVID-19. JAMA 2020;323:1499–500. 10.1001/jama.2020.3633 [DOI] [PubMed] [Google Scholar]
- 19.Strong SM, Magama Z, Mallick R, et al. Waiting for myomectomy during the COVID-19 pandemic: the vicious cycle of psychological and physical trauma associated with increased wait times. Int J Gynaecol Obstet 2020;151:303–5. 10.1002/ijgo.13340 [DOI] [PubMed] [Google Scholar]
- 20.Beisani M, Vilallonga R, Petrola C, et al. Effects of COVID-19 lockdown on a bariatric surgery waiting list cohort and its influence in surgical risk perception. Langenbecks Arch Surg 2021;406:1–8. 10.1007/s00423-020-02040-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goyal N, Venkataram T, Singh V, et al. Collateral damage caused by COVID-19: change in volume and spectrum of neurosurgery patients. J Clin Neurosci 2020;80:156–61. 10.1016/j.jocn.2020.07.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joly H. Lead your team into a post-pandemic world, 2020. [Google Scholar]
- 23.De Villers MJ, DeVon HA. Moral distress and avoidance behavior in nurses working in critical care and noncritical care units. Nurs Ethics 2013;20:589–603. 10.1177/0969733012452882 [DOI] [PubMed] [Google Scholar]
- 24.Moss M, Good VS, Gozal D, et al. An official critical care societies collaborative statement: Burnout syndrome in critical care health care professionals: a call for action. Am J Crit Care 2016;25:368–76. 10.4037/ajcc2016133 [DOI] [PubMed] [Google Scholar]
- 25.van Mol MMC, Kompanje EJO, Benoit DD, et al. The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS One 2015;10:e0136955. 10.1371/journal.pone.0136955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Troglio da Silva FC, Neto MLR. Psychiatric disorders in health professionals during the COVID-19 pandemic: a systematic review with meta-analysis. J Psychiatr Res 2021;140:474–87. 10.1016/j.jpsychires.2021.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Mol MMC, Nijkamp MD, Bakker J, et al. Counterbalancing work-related stress? work engagement among intensive care professionals. Aust Crit Care 2018;31:234–41. 10.1016/j.aucc.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 28.Schaufeli WB, Salanova M, González-romá V, et al. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. J Happiness Stud 2002;3:71–92. 10.1023/A:1015630930326 [DOI] [Google Scholar]
- 29.Schaufeli WB. Engaging leadership in the job demands-resources model. Career Development International 2015;20:446–63. 10.1108/CDI-02-2015-0025 [DOI] [Google Scholar]
- 30.Bakker AB, Demerouti E, Sanz-Vergel AI. Burnout and work engagement: the JD–R approach, 2014. [Google Scholar]
- 31.Yu F, Raphael D, Mackay L, et al. Personal and work-related factors associated with nurse resilience: a systematic review. Int J Nurs Stud 2019;93:129–40. 10.1016/j.ijnurstu.2019.02.014 [DOI] [PubMed] [Google Scholar]
- 32.van Mol M, de Veer M, de Pagter A, et al. Vitality, resilience and the need for support among hospital employees during the COVID-19 pandemic: study protocol of a mixed-methods study. BMJ Open 2021;11:e049090. 10.1136/bmjopen-2021-049090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 34.Young J, Klosko J, Weishaar M. Schemagerichte therapie: handboek voor therapeuten.[Scheme based therapy: Manual for therapists. Houten, the Netherlands: Bohn Stafleu van Loghum, 2004. [Google Scholar]
- 35.Demerouti E, Bakker AB, Nachreiner F, et al. The job demands-resources model of burnout. J Appl Psychol 2001;86:499–512. 10.1037/0021-9010.86.3.499 [DOI] [PubMed] [Google Scholar]
- 36.Maslow AH. A theory of human motivation. Psychol Rev 1943;50:370–96. 10.1037/h0054346 [DOI] [Google Scholar]
- 37.Highfield J, Johnson E, Jones T, et al. The psychological needs of healthcare staff as a result of the coronavirus pandemic. Br Psychol Soc 2020. [Google Scholar]
- 38.Chen Q, Liang M, Li Y, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e15–16. 10.1016/S2215-0366(20)30078-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020;368:m1211. 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- 40.Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care 2020;9:241–7. 10.1177/2048872620922795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shahil Feroz A, Ali NA, Feroz R, et al. Exploring community perceptions, attitudes and practices regarding the COVID-19 pandemic in Karachi, Pakistan. BMJ Open 2021;11:e048359. 10.1136/bmjopen-2020-048359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bennett P, Noble S, Johnston S, et al. COVID-19 Confessions: a qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open 2020;10:e043949. 10.1136/bmjopen-2020-043949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wind TR, Komproe IH. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc Sci Med 2012;75:1715–20. 10.1016/j.socscimed.2012.06.032 [DOI] [PubMed] [Google Scholar]
- 44.Muller AE, Hafstad EV, Himmels JPW, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res 2020;293:113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tannenbaum SI, Traylor AM, Thomas EJ, et al. Managing teamwork in the face of pandemic: evidence-based tips. BMJ Qual Saf 2021;30:59–63. 10.1136/bmjqs-2020-011447 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059124supp001.pdf (210.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Anonymised data gathered and analysed during the current study are not publicly available due to legal and ethical restrictions. These data can be requested from the corresponding author at a reasonable request by scientists wishing to use them for non-commercial purposes.