Abstract
Aim:
Quarantine due to the COVID-19 pandemic altered the supply and demand of health services. This, together with the ‘infodemic’ and generalized panic, could alter the patterns of self-medication in the population. The objective was to characterize the patterns of self-medication in four cities of Colombia during mandatory preventive isolation in 2020.
Methods:
This was a cross-sectional study done in four Colombian cities during mandatory national preventive isolation between June and September 2020. A sample of 397 adults who responded to an online survey, based on the Instrument for Systematic Data Collection for Self-medication (Instrumento de Recolección Sistemática de Datos para la Automedicación–IRIS-AM), was obtained. The use of social networks (including WhatsApp) as the source of information about medications was explored.
Results:
The 397 people surveyed had a median age of 31.0 years, and 58.2% were women. The prevalence of self-medication during lockdown was 34.3% (n = 136). Medications targeting the nervous system (n = 117; 86.0% of those participants with self-medication) and the musculoskeletal system (n = 68; 50.0%) were the most commonly used. Ten (7.4%) of the self-medicated patients reported doing so to prevent COVID-19, and 15 (11.0%) named social networks as the source of information.
Conclusion:
More than one-third of the participants reported self-medication during COVID-19 lockdown, mainly with analgesic-type nervous system medications. People who reported self-medication to prevent COVID-19 often got their information from social networks, the Internet, and WhatsApp.
Plain Language Summary
Self-medication during mandatory COVID-19 isolation
Introduction: Self-medication refers to the use of medications to treat self-diagnosed disorders or symptoms, and it can lead to health problems. This habit is widely practiced by the people, especially in low- and middle-income countries. The objective was to characterize the patterns of self-medication in four cities of Colombia during mandatory preventive isolation in 2020 due the quarantine by COVID-19 explored pandemic. Methods: We made a cross-sectional study between June and September 2020, and a sample of 397 adults who responded to an online survey. The use of social networks (including WhatsApp) as the source of information about medications was explored. Results: The prevalence of self-medication during lockdown was 34.3% (n = 136). Medications targeting the nervous system (n = 117; 86.0% of those participants with self-medication) and the musculoskeletal system (strategies n = 68; 50.0%) were the most commonly used. Conclusion: People who reported self-medication to prevent COVID-19 often got their information from social networks, the Internet, and WhatsApp. These findings raise the possibility of designing pedagogical strategies on this topic.
Keywords: COVID-19, drug utilization, misinformation, pharmacoepidemiology, self-medication
Introduction
The COVID-19 pandemic has affected all aspects of society, in particular the health of people, both physical and mental. Fear, anxiety, depression, and stress are common psychological reactions to the current pandemic1,2 and are promoted and perpetuated by a wide spectrum of variables, such as disinformation, social distancing measures, the economic crisis, and exposure to media.3–5 The overwhelming amount of information and the lack of precise conclusions generate confusion and panic and lead to distorted interpretations of the facts, 5 promoting behaviors that negatively affect health, 6 including self-medication. 7
Self-medication is defined as the use of medications, herbs, or home remedies on one’s own initiative or on the recommendation of another person, usually a friend, family member, neighbor, or pharmacist, without prior consultation with a doctor. 8 This large-scale phenomenon constitutes a public health problem associated with adverse outcomes that ultimately create an economic burden on health services.9,10 Multiple similar scenarios of misinformation and rumors amplified by social networks and media have been presented, with alleged potential therapies not approved for the treatment of COVID-19, such as hydroxychloroquine/chloroquine, chlorine dioxide solution, azithromycin, antiretrovirals, such as ritonavir and lopinavir, and nonsteroidal anti-inflammatory drugs such as ibuprofen.7,10,11 In previous epidemics, self-medication has increased in the general population, 12 and the current ‘infodemic’ of false news and rumors may also contribute to its increase in the current pandemic.
In Colombia, the first case of COVID-19 was recorded on 6 March 2020. 13 From then until 14 December 2021, more than 5,095,000 people have been infected in Colombia, 14 and the infection rate triggered strict mandatory preventive isolation during the first 6 months of the pandemic.15,16 During this period, the free movement of citizens was severely restricted, and many commercial, academic, and school activities as well as some health services were forced to close or operate through virtual means, 17 which caused, as in other countries, a drastic fall in the supply of health care. This, together with the generalized panic at the beginning of the pandemic and the fear of sanctions for violation of quarantine, led to a decreased demand for health services and the seeking of alternatives for the treatment of pathologies.18,19
Self-medication can generate complications ranging from medication shortages to bacterial resistance or to adverse reactions that can even lead to death.20,21 The characteristics of self-medication in the COVID-19 pandemic in Colombia are not well known and are reported mainly by unofficial sources, so this study sought to determine the self-medication practices during times of mandatory isolation for COVID-19 in a group of people in Colombia.
Methods
Study design and population
A cross-sectional descriptive observational study was conducted to characterize self-medication patterns in a population of the city of Pereira (Risaralda) and its surrounding area (including the neighboring cities: Dosquebradas, Santa Rosa de Cabal, and La Virginia).
Data were collected online through self-completed surveys built on the Google Forms platform, based on the Instrument for Systematic Data Collection for Self-medication (Instrumento para la Recolección de Información Sistemática en Automedicación–IRIS-AM)© prior authorization by the authors, 9 modified according to the variables of interest for this study. Nonprobabilistic convenience sampling was performed. The online data collection instrument was sent and publicly disseminated by social networks (Facebook, WhatsApp) and the advertising bulletins of two universities in the region and was available to the general population from June 30 to September 14, 2020. Age 18 years or older and agreement to participate in the study were the inclusion criteria. People who claimed to be health professionals were excluded.
The following groups of variables were included: (1) sociodemographic: age, sex, type of affiliation to the health system (subsidized, contributory, and other), educational level (highest completed: none, basic (primary and high school), technical, advanced (professional and postgraduate)), socioeconomic stratum (six strata grouped into low (1–2), medium (3–4), and high (5–6)), as well as area of residence, and so on; (2) prevalence of self-medication: use of medications without medical prescription: sometime in life and during isolation due to COVID-19; (3) nature of self-medication: name of medications used; type of medication used according to the ATC classification – Anatomical Therapeutic Chemical Classification System); (4) signs or symptoms that motivated self-medication, including prevention of COVID-19; (5) reasons for nonuse of health services; (6) source of information driving their decision and the source of the medication; and (7) comorbidities and comedications of the patient, for example, high blood pressure, ischemic heart disease, diabetes mellitus, dyslipidemia, cancer, hypothyroidism, asthma, chronic obstructive pulmonary disease, autoimmune diseases, HIV infection, smoking, and obesity.
Analysis
The data collected were exported to Microsoft Excel 2013 and analyzed with the statistical package SPSS Statistics version 26.0 for Windows (IBM, USA). Descriptive statistics are used to present the results. The χ 2 test was used to detect relationships between the consumption of medications to prevent COVID-19 and the other categorical variables. The level of statistical significance was set at p < 0.05.
The protocol was approved by the Bioethics Committee of the Universidad Tecnológica de Pereira in the category of ‘research without risk’, according to resolution No. 8430 of 1993 of the Ministry of Health of Colombia. The ethical principles and confidentiality of information established by the Declaration of Helsinki were respected. The participants granted their consent at the time they completed the electronic questionnaire.
Results
A total of 427 people initially answered the virtual questionnaire, and 397 questionnaires met the selection criteria and were analyzed. Of these, the median age of respondents was 31.0 years (interquartile range: 24.0–41.0 years), and the majority were women (n = 231; 58.2%) and resided in the city of Pereira (n = 256; 64.5%). The main socioeconomic level was medium (n = 235; 59.2%), most of them belonged to the contributory regime of the health system (n = 288; 72.5%), and most had a high educational level (advanced n = 268; 67.5%; Table 1).
Table 1.
General characteristics of the sample, discriminated by groups according to the history of self-medication since the beginning of isolation.
| Characteristics | Total (n = 397) | Self-medication (n = 136; 34.2%) | No Self-medication (n = 261; 65.7%) |
|---|---|---|---|
| Sex – n (%) | |||
| Woman | 231 (58.2) | 84 (61.8) | 147 (56.3) |
| Man | 164 (41.3) | 52 (38.2) | 112 (42.9) |
| Other | 2 (0.5) | 0 (0.0) | 2 (0.8) |
| Age – median (IQR) years | 31.0 (24.0–41.0) | 30.0 (23.0–39.0) | 31.0 (25.0–41.0) |
| Socioeconomic stratum – n (%) | |||
| Low (1–2) | 98 (24.7) | 29 (21.3) | 69 (26.4) |
| Medium (3–4) | 235 (59.2) | 80 (58.8) | 155 (59.4) |
| High (5–6) | 64 (16.1) | 27 (19.9) | 37 (14.2) |
| Affiliation to the health system – n (%) | |||
| Contributory or pay regime | 288 (72.5) | 97 (71.3) | 191 (73.2) |
| Subsidized by the state | 52 (13.1) | 19 (14.0) | 33 (12.6) |
| Not affiliated | 36 (9.1) | 9 (6.6) | 27 (10.3) |
| Does not know | 21 (5.3) | 11 (8.1) | 10 (3.8) |
| Education – n (%) | |||
| Basic (primary/high school) | 73 (18.4) | 26 (19.1) | 47 (18.0) |
| Technical | 56 (14.1) | 23 (16.9) | 33 (12.6) |
| Advanced (professional/postgraduate) | 268 (67.5) | 87 (64.0) | 181 (69.3) |
| Ethnicity – n (%) | |||
| Mestizo | 364 (91.7) | 120 (88.2) | 244 (93.5) |
| None/does not know | 12 (3.0) | 7 (5.1) | 5 (1.9) |
| Others | 21 (5.3) | 9 (6.6) | 12 (4.6) |
| Area of residence – n (%) | |||
| Urban | 369 (92.9) | 128 (94.1) | 241 (92.3) |
| Rural | 28 (7.1) | 8 (5.9) | 20 (7.7) |
| Comorbidities–n (%) | |||
| None | 259 (65.2) | 86 (63.2) | 173 (66.3) |
| 1 or more chronic conditions | 138 (34.8) | 50 (36.8) | 88 (33.7) |
| 1 or more pathologies with a high risk of mortality from COVID-19* | 86 (21.7) | 27 (19.9) | 59 (22.6) |
| Store medications at home – n (%) | 369 (92.9) | 135 (99.3) | 234 (89.7) |
| Recommend medications to other people – n (%) | 138 (34.8) | 61 (44.8) | 77 (29.5) |
IQR, interquartile range.
Pathologies with high mortality risk for COVID-19, according to the Centers for Disease Control and Prevention, CDC.
Of all the participants, 136 reported having self-medicated from the beginning of preventive isolation until the time of the survey, indicating a prevalence of self-medication in this period of 34.3% (95% confidence interval (CI): 29.6–39.2%) (Table 1). Most reported having self-medicated at some point in life (n = 342; 86.1% 95% CI: 82.4–89.4%). Likewise, 92.9% (n = 369) kept medications at home, and 34.8% (n = 138) recommended medications to other people. Storing medications at home (odds ratio (OR): 15.58; 95% CI: 2.09–115.92; p < 0.001) and having recommended medications to other people (OR: 1.94; 95% CI: 1.26–2.99; p = 0.002) were associated with self-medication during quarantine.
Table 2 shows the number of people who self-medicated with at least one drug from each pharmacological group. On average, 3.3 ± 1.9 self-medicating drugs were reported per person who self-medicated. Among the most commonly used pharmacological groups were nervous system medications (n = 117; 86.0% of those participants with self-medication reported during quarantine), mainly in the form of analgesics (i.e: of acetaminophen). Drugs for the musculoskeletal system (n = 68; 50.0%) and for the respiratory system (n = 56; 41.2%) were next in frequency.
Table 2.
Number of self-medicated people for each pharmacological group (n = 136).
| Drug group | Frequency n = 136 |
% |
|---|---|---|
| Number of reported drugs per person – mean ± SD | 3.3 ± 1.9 | |
| One | 19 | 14.0 |
| Two | 29 | 21.3 |
| Three or more | 88 | 64.7 |
| Nervous system | 117 | 86.0 |
| Analgesics | 117 | 86.0 |
| Acetaminophen | 116 | 85.3 |
| Other (psycholeptics, psychoanaleptics) | 8 | 5.9 |
| Musculoskeletal system | 68 | 50.0 |
| Anti-inflammatory and antirheumatic products | 64 | 47.1 |
| Muscle relaxants | 5 | 3.7 |
| Respiratory system | 56 | 41.2 |
| Antihistamines for systemic use | 36 | 26.5 |
| Cough and cold preparations | 33 | 24.3 |
| Alimentary tract and metabolism | 54 | 39.7 |
| Vitamins | 29 | 21.3 |
| Drugs for acid-related disorders | 23 | 16.9 |
| Other (drugs for constipation, antidiarrheals, etc) | 9 | 6.6 |
| Antiinfectives for systemic use | 20 | 14.7 |
| Antibacterials for systemic use | 17 | 12.5 |
| Antimycotics for systemic use | 3 | 2.2 |
| Blood and blood forming organs (antithrombotic agents) | 18 | 13.2 |
| Genito-urinary system and sex hormones (contraceptives) | 10 | 7.4 |
| Antiparasitic products, insecticides, and repellents | 9 | 6.6 |
| Antiprotozoals | 5 | 3.7 |
| Anthelmintics | 4 | 2.9 |
| Other | ||
| Systemic hormonal preparations* | 3 | 2.2 |
| Cardiovascular system | 2 | 1.5 |
| Dermatologicals | 1 | 0.7 |
| Other (natural products) | 26 | 19.1 |
SD, standard deviation.
Excluding sex hormones and insulins (corticosteroids for systemic use).
Among the other variables collected in relation to self-medication during lockdown, the most frequent reasons for self-medication were pain (n = 113; 83.1%), respiratory symptoms (n = 62; 45.6%), and systemic symptoms (n = 45; 33.1%; Table 3). The main reasons for not consulting a doctor (and choosing to self-medicate) were knowledge about the treatment for their discomfort (n = 113; 83.1%) and fear of contracting COVID-19 (n = 39; 28.7%).
Table 3.
Characterization of self-medication during mandatory preventive isolation (n = 136).
| Variable | n = 136 | % |
|---|---|---|
| Reasons for self-medication | ||
| Pain | 113 | 83.1 |
| Respiratory symptoms | 62 | 45.6 |
| Flu | 38 | 27.9 |
| Allergies | 29 | 21.3 |
| Cough | 13 | 9.6 |
| Systemic symptoms | 45 | 33.1 |
| Gastrointestinal symptoms | 37 | 27.2 |
| Others | 42 | 30.9 |
| COVID-19 ‘prevention’ | 10 | 7.4 |
| Aspirin | 7 | 5.1 |
| Chloroquine | 2 | 1.5 |
| Hydroxychloroquine | 2 | 1.5 |
| Azithromycin | 1 | 0.7 |
| Dexamethasone | 1 | 0.7 |
| Ivermectin | 1 | 0.7 |
| Reasons for not consulting | ||
| People refer to know the treatment for their condition | 113 | 83.1 |
| Fear of being infected by coronavirus | 39 | 28.7 |
| Difficult access to services due to administrative procedures | 20 | 14.7 |
| Little time availability | 19 | 14.0 |
| Fear of being penalized for leaving home | 10 | 7.4 |
| Mistrust in health personnel or institutions | 8 | 5.9 |
| Economic difficulties | 4 | 2.9 |
| Difficulty in transportation | 2 | 1.5 |
| Health system affiliation problem | 2 | 1.5 |
| Information sources | ||
| Medical formula from previous consultation | 59 | 43.4 |
| By a relative, friend, neighbor, or acquaintance | 48 | 35.3 |
| By custom, tradition, or popular culture | 48 | 35.3 |
| In a pharmacy | 25 | 18.4 |
| Social networks, internet, WhatsApp | 15 | 11.0 |
| By a health worker not authorized to prescribe | 11 | 8.1 |
| As part of an ongoing university training | 7 | 5.1 |
| Television, radio, newspaper, and newscast | 6 | 4.4 |
| Drug sources | ||
| Pharmacy | 112 | 82.4 |
| Home/family kit/relative | 56 | 41.2 |
| Stores/supermarket | 25 | 18.4 |
| A third-party person | 8 | 5.9 |
| Assessment of knowledge about medicines | ||
| Very high | 36 | 26.5 |
| High | 42 | 30.9 |
| Low | 48 | 35.3 |
| None | 10 | 7.3 |
Approximately half of the participants indicated that the source of information for their selection of self-medicating drugs was medical formulas from previous consultations (n = 59; 43.4%). Other sources also stood out, such as the reference of a relative, friend, neighbor, or acquaintance and popular customs, each reported by 48 participants (35.3%). A total of 15 people (11.0%) also reported having received information on social networks, the Internet, and WhatsApp (Table 3).
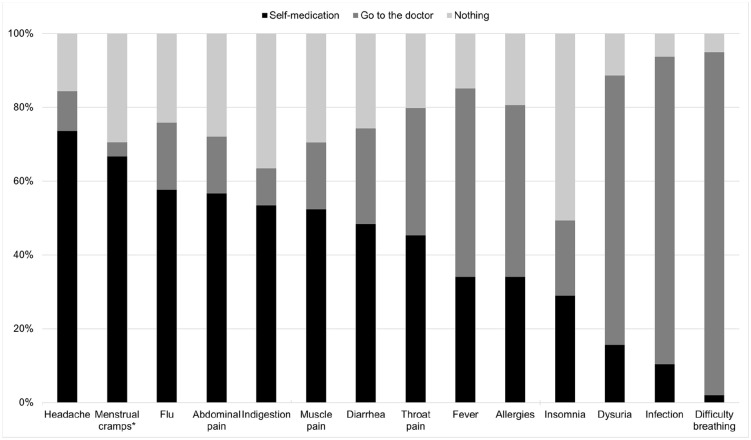
Table 4 shows the main reasons for self-medicating according to the subgroup of medication, taking into account that the same patient could report more than one group of medications and more than one reason for self-medication. From the questions about the behaviors taken against different hypothetical symptoms, it was found that the participants preferred to self-medicate for headache, menstrual cramps, flu symptoms, abdominal pain, indigestion symptoms, or muscle pain, while they would prefer to consult a doctor about dyspnea, other symptoms they associated with infections, or dysuria (Figure 1).
Table 4.
Main reasons for self-medication and the groups of drugs used by the participants.
| Drug group/self-medication reasons | Pain | Respiratory symptoms | Systemic symptoms | Gastrointestinal symptoms | Others | COVID-19 prevention | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 113 | % | n = 62 | % | n = 45 | % | n = 37 | % | n = 42 | % | n = 10 | % | |
| Nervous system | 106 | 93.8 | 53 | 85.5 | 40 | 88.9 | 33 | 89.2 | 33 | 78.6 | 8 | 80.0 |
| Musculoskeletal system | 64 | 56.6 | 30 | 48.4 | 31 | 68.9 | 23 | 62.2 | 20 | 47.6 | 3 | 30.0 |
| Respiratory system | 45 | 39.8 | 47 | 75.8 | 21 | 46.7 | 21 | 56.8 | 17 | 40.5 | 4 | 40.0 |
| Alimentary tract and metabolism | 47 | 41.6 | 27 | 43.5 | 21 | 46.7 | 28 | 75.7 | 20 | 47.6 | 5 | 50.0 |
| Anti-infectives for systemic use | 11 | 9.7 | 13 | 21.0 | 7 | 15.6 | 8 | 21.6 | 13 | 31.0 | 3 | 30.0 |
| Blood and blood forming organs (antithrombotic agents) | 15 | 13.3 | 9 | 14.5 | 6 | 13.3 | 7 | 18.9 | 8 | 19.0 | 7 | 70.0 |
| Genito-urinary system and sex hormones (contraceptives) | 10 | 8.8 | 4 | 6.5 | 4 | 8.9 | 3 | 8.1 | 9 | 21.4 | 0 | 0.0 |
| Antiparasitic products, insecticides and repellents | 8 | 7.1 | 5 | 8.1 | 5 | 11.1 | 4 | 10.8 | 5 | 11.9 | 4 | 40.0 |
| Other (natural products) | 21 | 18.6 | 15 | 24.2 | 11 | 24.4 | 9 | 24.3 | 13 | 31.0 | 4 | 40.0 |
| Drugs popularly associated with the treatment of COVID-19 | 9 | 8.0 | 8 | 12.9 | 7 | 15.6 | 4 | 10.8 | 7 | 16.7 | 4 | 40.0 |
Figure 1.
Behaviors taken against different hypothetical symptoms by the study participants (n = 397).
*Menstrual cramps calculated on the total response of women.
Ten patients (7.4%) specifically reported taking medications to prevent COVID-19, and five of them reported that the source of information was social networks (OR: 11.6; 95% CI: 2.87–46.94; p = 0.002). The other sources of information were not correlated with the consumption of drugs for this type of prevention. All patients who took chloroquine, hydroxychloroquine, and ivermectin cited prophylaxis against COVID-19, as did one of the patients who took azithromycin (1/7 = 14.3%). The other patients who took azithromycin indicated its use for fever, flu, and other types of infections. Finally, the taking of drugs for the prevention of COVID-19 was also related to distrust in health personnel or institutions (OR: 10.4; 95% CI: 2.05–52.49; p = 0.013) and fear of being sanctioned or fined for leaving the house (OR: 7.29; 95% CI: 1.54–34.41; p = 0.026).
Discussion
This study determined the prevalence of self-medication in general and during lockdown in response to the COVID-19 pandemic in a group of people from Colombia. Approximately 7% of respondents resorted to self-medication to protect against COVID-19, and this practice was related to the use of social networks, the Internet, and WhatsApp as a source of information. These data may be of interest to government entities and health service providers to promote better education of the population on issues of medications and self-medication during the current pandemic or similar situations.
When comparing the prevalence of self-medication with previous data from Colombia, similar values were found for both general self-medication (at any time in life) and recent self-medication. A 2013 study in Colombia described a prevalence of self-medication in the last 30 days of 32%, 9 similar to the 34% of this study during lockdown. This indicates that there do not seem to be significant variations in prevalence in terms of recent self-medication despite the current pandemic. This contrasts with findings reported in Kenya, where self-medication went from 36% before the pandemic to 60% during the pandemic, 22 although the population analyzed was health workers, a profession excluded from this analysis. In the previous Colombian study, people who kept medications at home and who recommended the use of medications to others were more likely to self-medicate, 9 which was also reflected in this population analyzed during the pandemic. Other factors reported in association with self-medication (in a study focused on antimicrobials) include, for example, level of education or age. 23
In a study conducted in Peru, it was found that 33.4% of the population surveyed had self-medicated during isolation due to the COVID-19 pandemic, 7 a value very similar to that of this study. However, this report specifically asked about self-medication with drugs probably used for the management or prevention of COVID-19, including azithromycin and hydroxychloroquine. 7 These medications, along with chloroquine and ivermectin, have been popularly proposed for the management and prevention of COVID-19, but they raise the risks of important adverse events, such as the prolongation of the QT interval. 24 In this study, respondents also reported the unprescribed consumption of these molecules.
Other studies have measured the prevalence of self-medication in the context of the pandemic, both at the level of medications in general and those specifically focused on preventing COVID-19. For example, in Togo during the first part of the pandemic, self-medication had a prevalence of 34.2%, 25 while in Nigeria it reached 41.0%, 26 in both countries coming mainly from the consumption of vitamin C. In this study, high values of vitamin consumption were also found, although the main drugs used in self-medication corresponded to analgesics, as has been seen in other publications.7,9
A high percentage of the respondents indicated the presence of respiratory symptoms as a reason for self-medication, mainly to help fight flu-like symptoms. Similarly high proportions of patients reported self-medication as an initial management alternative for diarrhea, sore throat, and fever. This is worrisome in the context of the pandemic because since it started, there has been a call to notify the health system of these symptoms to schedule medical consultations and to define the need for sampling for COVID-19, isolation, or hospitalization.27,28 On the contrary, the majority of the participants indicated that, in case of breathing difficulty, they would seek medical consultation as a first option.
Self-medication with anti-infective agents is a special point of attention. In this study, approximately 15% of participants who self-medicated used an antibiotic or an antifungal without a medical prescription. In a study that evaluated the practices of antibiotic consumption in a sample of patients from a health institution in Uganda, more than 20% had used antibiotics at some time without a medical prescription. 29 This was associated with some variables of interest, such as religion, which was not assessed in this study. A meta-analysis published in 2015 found an overall prevalence of antimicrobial self-medication of 39% in developing countries; however, the figures are highly variable, ranging from 4% to 91% according to the country. 23
Taking antibiotics without medical indication or evaluation represents serious problems for health care systems due to possible adverse reactions and the appearance of antibiotic resistance, 30 which may be even more serious in the context of the current COVID-19 pandemic. 31 Reports in France have described that adverse reactions to medications related to self-medication increased from 1.6% in 2019 to 3.7% during the pandemic, which highlights the importance of analyzing this type of situation in the current public health context. 32
Although few participants self-medicated to prevent COVID-19, they usually chose to do so based on information from social networks and WhatsApp. The COVID-19 infodemic is reflected not only in aspects of self-medication but also in other areas of vital importance to public health, such as the use of masks and the acceptance of vaccines, and an epidemiological model has even been proposed to try to mitigate its effects early through specially designed information surveillance systems. 33
The study has limitations inherent to its observational design. The sample size was small even though the questionnaire was disseminated through social networks and official channels of two higher-education institutions in the city. Likewise, the sample was a convenience sample, and the survey was self-administered precisely because of the COVID-19 lockdown situation. This could also have limited the access of some population groups to the survey and therefore the generalizability of the results. As a strength, this study used an instrument previously used in research on self-medication, and it included specific questions about COVID-19 and questions on the sourcing of information from social networks during the lockdown.
Conclusion
More than one-third of the participants reported self-medication during the preventive isolation time for COVID-19, mainly with analgesics. A fairly high proportion of people who reported self-medication to prevent COVID-19 cited social networks, the Internet, and WhatsApp as sources of information driving their choice. These data support the need to improve the education of the general community about the appropriate use of medications, improve access to reliable health information, and even convey the importance of seeking medical advice and reporting symptoms suggestive of COVID-19 instead of self-medication.
Footnotes
Author contributions: Andres Gaviria-Mendoza: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing – original draft.
Danny Alberto Mejia-Mazo: Data curation; Formal analysis; Investigation; Writing – original draft
Carolina Duarte-Blandon: Conceptualization; Data curation; Formal analysis; Investigation; Writing – original draft.
Juan Daniel Castrillon-Spitia: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Writing – original draft.
Manuel Enrique Machado-Duque: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Validation; Writing – original draft.
Luis Fernando Valladales-Restrepo: Data curation; Formal analysis; Methodology; Writing – original draft
Jorge Enrique Machado-Alba: Conceptualization; Investigation; Project administration; Supervision; Validation; Writing – review & editing.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jorge Enrique Machado-Alba  https://orcid.org/0000-0002-8455-0936
https://orcid.org/0000-0002-8455-0936
Availability of data and material: www.protocols.io
Code availability: dx.doi.org/10.17504/protocols.io.by43pyyn
Contributor Information
Andrés Gaviria-Mendoza, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia Grupo de Investigación Biomedicina, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia.
Danny Alberto Mejía-Mazo, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia.
Carolina Duarte-Blandón, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia.
Juan Daniel Castrillón-Spitia, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia Grupo de Investigación Biomedicina, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia.
Manuel Enrique Machado-Duque, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia Grupo de Investigación Biomedicina, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia.
Luis Fernando Valladales-Restrepo, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A., Pereira, Colombia Grupo de Investigación Biomedicina, Fundación Universitaria Autónoma de las Américas, Pereira, Colombia.
Jorge Enrique Machado-Alba, Grupo de Investigación en Farmacoepidemiología y Farmacovigilancia, Universidad Tecnológica de Pereira–Audifarma S.A, Pereira 660003, Colombia.
References
- 1. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 2020; 52: 102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yan J, Kim S, Zhang SX, et al. Hospitality workers’ COVID-19 risk perception and depression: a contingent model based on transactional theory of stress model. Int J Hosp Manag 2021; 95: 102935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. O’Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr 2020; 7: 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Thompson RR, Jones NM, Holman EA, et al. Media exposure to mass violence events can fuel a cycle of distress. Sci Adv 2019; 5: eaav3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alvarez-Risco A, Mejia CR, Delgado-Zegarra J, et al. The Peru approach against the COVID-19 infodemic: insights and strategies. Am J Trop Med Hyg 2020; 103: 583–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Garcia-Saiso S, Marti M, Brooks I, et al. The COVID-19 infodemic. Rev Panam Salud Publica 2021; 45: e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Quispe-Cañari JF, Fidel-Rosales E, Manrique D, et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharm J 2021; 29: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bennadi D. Self-medication: a current challenge. J Basic Clin Pharm 2013; 5: 19–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Machado-Alba JE, Echeverri-Cataño LF, Londoño-Builes MJ, et al. Factores económicos, sociales y culturales asociados con automedicación. Biomedica 2014; 34: 580–588. [DOI] [PubMed] [Google Scholar]
- 10. Yáñez JA, Chung SA, Román BR, et al. Prescription, over-the-counter (OTC), herbal, and other treatments and preventive uses for COVID-19. In: Dehghani MH, Karri RR, Roy S. (eds) Environmental and health management of novel coronavirus disease (COVID-19). London: Academic Press, 2021, pp.379–416. [Google Scholar]
- 11. Yazdany J, Kim AHJ. Use of hydroxychloroquine and chloroquine during the COVID-19 pandemic: what every clinician should know. Ann Intern Med 2020; 172: 754–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vygen S, Tiffany A, Rull M, et al. Changes in health-seeking behavior did not result in increased all-cause mortality during the Ebola outbreak in Western Area, Sierra Leone. Am J Trop Med Hyg 2016; 95: 897–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19), https://www.who.Int/emergencies/diseases/novel-coronavirus-2019?gclid=CjwKCAjwzaSLBhBJEiwAJSRokkpqRcUOClQtL-uYhAayBdWCnGjOhR0VCF6FMgbV7e65W1muDm-6lhoC6FUQAvD_BwE (2020, accessed 30 September 2020).
- 14. COVID-19 Dashboard by the Center for Systems Science Engineering (CSSE) at Johns Hopkins University (JHU). Johns Hopkins University, https://coronavirus.jhu.edu/data#charts (2020, accessed 30 September 2020). [Google Scholar]
- 15. Presidencia de la República de Colombia. Decreto1076 del 28 de Julio de 2020: Por el cual se imparten instrucciones en virtud de la emergencia sanitaria generada por la pandemia del Coronavirus COVID-19, y el mantenimiento del orden público. Bogotá D.C., https://dapre.presidencia.gov.Co/normativa/normativa/DECRETO%201076%20DEL%2028%20DE%20JULIO%20DE%202020.pdf (2020, accessed 30 September 2020). [Google Scholar]
- 16. Ministerio de Salud y Protección Social. Resolución 385 del 12 de Marzo de2020: Por la cual se declara la emergencia sanitaria por causa del coronavirus COVID-19 y se adoptan medidas para hacer frente al virus. Bogotá D.C., https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=119957 (2020, accessed 30 September 2020). [Google Scholar]
- 17. Presidencia de la República de Colombia. Decreto 457 del 23 de Marzo de2020: Por el cual se imparten instrucciones en virtud de la emergencia sanitaria generada por la pandemia del Coronavirus COVID-19 y el mantenimiento del orden público. Bogotá D.C., https://dapre.presidencia.gov.co/normativa/normativa/DECRETO%20457%20DEL%2022%20DE%20MARZO%20DE%202020.pdf (2020, accessed 30 September 2020). [Google Scholar]
- 18. Cifuentes MP, Rodriguez-Villamizar LA, Rojas-Botero ML, et al. Socioeconomic inequalities associated with mortality for COVID-19 in Colombia: a cohort nationwide study. J Epidemiol Community Health. Epub ahead of print 4 March 2021. DOI: 10.1136/jech-2020-216275. [DOI] [PubMed] [Google Scholar]
- 19. Xiao H, Dai X, Wagenaar BH, et al. The impact of the SARS-COV-2 pandemic on health services utilization in China: time-series analyses for 2016–2020. Lancet Reg Health West Pac 2021; 9: 100122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Saf 2001; 24: 1027–1037. [DOI] [PubMed] [Google Scholar]
- 21. Ruiz ME. Risks of self-medication practices. Curr Drug Saf 2010; 5: 315–323. [DOI] [PubMed] [Google Scholar]
- 22. Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J 2020; 28: 1149–1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ocan M, Obuku EA, Bwanga F, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health 2015; 15: 742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gerard A, Romani S, Fresse A, et al. ‘Off-label’ use of hydroxychloroquine, azithromycin, lopinavir-ritonavir and chloroquine in COVID-19: a survey of cardiac adverse drug reactions by the French Network of Pharmacovigilance Centers. Therapie 2020; 75: 371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sadio AJ, Gbeasor-Komlanvi FA, Konu RY, et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health 2021; 21: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wegbom AI, Edet CK, Raimi O, et al. Self-medication practices and associated factors in the prevention and/or treatment of COVID-19 Virus: a population-based survey in Nigeria. Front Public Health 2021; 9: 606801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ministerio de Salud y Protección Social. Lineamientos para la detección y manejo de casos de COVID-19 por los prestadores de servicios de salud en Colombia. Bogotá, https://www.minsalud.gov.co/Ministerio/Institucional/Procesos%20y%20procedimientos/GIPS05.pdf (2020, accessed 30 November 2020). [Google Scholar]
- 28. Ministerio de Salud y Protección Social Instituto Nacional de Salud. Instructivo para la vigilancia en salud pública intensificada de infección respiratoria aguda y la enfermedad asociada al nuevo coronavirus 2019 (COVID-19). Bogotá, http://www.saludcapital.gov.co/CTDLab/Publicaciones/Vigilancia_intensificada_COVID-19.pdf (2020, accessed 30 November 2020). [Google Scholar]
- 29. Nabaweesi I, Olum R, Sekite AB, et al. Antibiotic practices, perceptions and self-medication among patients at a National Referral Hospital in Uganda. Infect Drug Resist 2021; 14: 2155–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rather IA, Kim BC, Bajpai VK, et al. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci 2017; 24: 808–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alied M. Antimicrobial resistance, COVID-19 and self-medication in Syria: a potential boost for an already escalating problem. JAC Antimicrob Resist 2021; 3: dlab100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gras M, Gras-Champel V, Moragny J, et al. Impact of the COVID-19 outbreak on the reporting of adverse drug reactions associated with self-medication. Ann Pharm Fr 2021; 79: 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Scales D, Gorman J, Jamieson KH. The Covid-19 infodemic – applying the epidemiologic model to counter misinformation. N Engl J Med 2021; 385: 678–681. [DOI] [PubMed] [Google Scholar]