Abstract
In recent years, there have been advances in research regarding the prevalence of Adverse Childhood Experiences (ACEs) and resulting poor outcomes for children who have experiences ACES. ACE exposure has been connected with poor academic performance, poor health outcomes, and certain diseases. However, there is still relatively little known about the prevalence and impact of ACE exposure in early childhood. Using the 2016 National Survey of Children’s Health, this study assessed the prevalence of adverse childhood experiences for children under the age of six years. This research measured the impact of individual ACEs on health and developmental outcomes and found that financial hardship and parental mental illness both had increased odds of having health and developmental difficulties. Furthermore, this work finds that there is a dose-response relationship between ACE count and increased risk of health and developmental difficulties. Conversely, children who were reported as affectionate with their parent had decreased risk for health and developmental problems. Programs supporting families with young children should focus efforts on enhancing quality of attachment, especially for children experiencing ACEs.
Keywords: Adverse Childhood Experiences (ACEs), developmental cascades, resilience, protective factors, attachment
The study of Adverse Childhood Experiences (ACEs) is helpful in demonstrating how adversity is often associated with negative outcomes. The ACE questionnaire measures traumatic events in childhood, like abuse, neglect, and family dysfunction, that present a risk for future medical, academic, and social problems. High ACE scores have been determined to predict adult risky behavior and are associated with health and disability in childhood.1-4 Studying the impact of ACEs in childhood is important for developing interventions to help mitigate additional risks associated with ACE exposure. 5
Purpose of this Study
This study aims to add to the existing literature on ACEs by examining the impact of ACEs on development in early childhood. Due to the rapid brain development in young children, ACE exposure early in childhood may impact children’s health, learning, and behavior. 6 Using a developmental cascade framework to examine risk in early childhood, this study aims to examine developmental risk factors associated with individual and cumulative ACEs. 7 This research will supplement the body of literature on the achievement gap by including an in-depth analysis of multiple adversities, in addition to income, and examine the odds of additional associated medical and developmental risks. Understanding the prevalence of ACEs and the risks associated with ACEs in early childhood is critical for creating interventions that promote positive development for youth and inform parental education to minimize future ACE exposure.
Specifically, this study aims to examine the relationship of each individual ACE and the number of special health needs that represent chronic health conditions and developmental risk factors in young children (such as having emotional or behavioral problems). Furthermore, this study examines the likelihood of developmental risk factors with the increase in cumulative ACE score, examining a dose-response relationship to multiple developmental adversities. I hypothesized that children with higher ACE scores will have more health and developmental difficulties. Zero-inflated negative binominal regression was used to determine the likelihood of health and developmental problems in relation to the number of ACEs a child has experienced. Additionally, this relationship was examined for differences between children who demonstrate affection to their caregiver and those who rarely or never do.
Prior Literature
The ACE study measures traumatic events in childhood, like abuse, neglect and family dysfunction, that present a risk for future problems. The original 10 item ACE questionnaire includes questions regarding household dysfunction: parental separation, incidents of domestic violence, substance abuse, mental illness, and criminal behavior; abuse: psychological, physical, and emotional; and neglect: physical and emotional. 4
The initial ACE study found a strong relationship between exposure to abuse or household dysfunction during childhood and multiple health risk factors for the leading causes of death in adulthood. In their research Felitti et al 4 found that adults who had experienced 4 or more ACEs showed a 12 times higher prevalence of health risks such as alcoholism, drug use, depression, and suicide attempts. These findings raised awareness about the connection between childhood experiences and outcomes as an adult.
The study of ACEs demonstrates the many interconnected implications of risk. Traumatic events that occur within a child’s immediate environment impact the child’s development. Recent studies on ACEs have shown an increase in health and disability diagnosis associated with higher ACE scores.2,3 Due to this field of research, adversity is no longer perceived as solely a social issue, as it effects health and development also. Interventions such as the Center for Youth Wellness, 5 are targeting the medical, social, and psychological effects of adversities through a multidisciplinary approach. Supporting this complex relationship between ACEs and health other research found that children with special health care needs were more likely to have been reported as having experienced each individual ACE and had a higher average ACE score. 8
The study of adverse experiences focuses on the objective events but is not fully able to include the subjective interpretation of life events. Resilience, or positive adaptation, is evident from participants with high ACE scores in the initial ACE study given that the population examined was adults who were employed and insured, this signifies that even those adults who experienced significant adversity as a child were able to successfully meet social standards by obtaining employment. 4 This study represents the complex nature of risk and resilience since the participants were engaging in some maladaptive behaviors, while showing competence in other areas. While there was a strong correlation between ACEs and risky behavior such as addiction and obesity there is still variation in social outcomes.
A more recent study examined over 700 medical records of youth receiving medical services at an inner-city pediatric clinic. Researchers found a 30-fold increase in learning or behavior problems (as reported by parents) between children with high ACE scores (4 or more) compared to children with no ACEs. This work helps to connect the dots between social risk factors and educational outcomes.
Bower and Baldwin 2 studied the prevalence of ACEs among high school aged children in an urban school district. They found that the prevalence and specific type of adversities varied from different socioeconomic groups. Parental put downs were more common among children from higher socio-economic status (SES) and neighborhood violence was more common in children from lower SES backgrounds. The authors used multiple regression models to control for poverty when measuring the impact of ACEs on individual and school performance. Overall, higher ACE scores were significant in predicting grades, school achievement, and drug abuse. Average ACE scores for schools were associated with state test scores, graduation rates, and college attendance rates.
In a nationally representative study, children with higher ACE exposure were less likely to be engaged in school and more likely to repeat a grade. Furthermore, children with more than 2 aces were more likely to have attention deficit hyperactivity disorder (ADHD), behavior problems, and to bully others. 1 The ACE studies have been helpful in connecting cumulative risks with academic, health, and social outcomes.
Additional research shows that having a trusting adult present in childhood can serve as a buffer for the negative impact of ACEs. A study in the United Kingdom studied the impact of ACEs on health harming behaviors in adulthood and the mitigating effect of having an always available adult present in childhood. The increase of ACEs without the support of a trusted adult was associated with a higher ratio of harmful health behaviors. Even in participants with zero ACEs there were higher rates of smoking and poor diet in those without a trusting adult available during childhood. 9 This research signifies the importance of having available adults as a mitigating factor for adversities including economic deprivation as well as other ACEs. This study is significant in that is suggests that even while many of the ACE questions are directly related to parental stressors, there is still variation in adult outcomes based on having the support of a trusting adult in childhood. This could help inform perspective interventions aimed at mitigating the impact of ACEs in early childhood.
Furthermore, the role of attachment has previously been established as critical during the early childhood years. Masten, 10 states:
“The attachment relationship, in the elaborated theory, serves as a template for future relationships. A secure early attachment bond cascades to foster close relationships in subsequent years with friends, mentors, and romantic partners, serving protective functions for human adaptation over the life course. Research has demonstrated that sensitive, consistent caregiving enhances the quality of the attachment relationships, forecasting better social and emotional development.” (p. 20)
Thus, in early childhood, secure attachment can be preventative in nature, promote positive relational development, or protective in nature, depending on the context.
Developmental Opportunities
Furthermore, there are 3 natural periods in development where youth are especially susceptible to change. The first critical period of development is in early childhood years where brain development is rapidly occurring, and children are in a state of neural plasticity. Any exposure to adversity, or ACEs, during this period of development may hinder healthy development. 6 Prior research on early exposure of abuse and neglect has established the consequences on the developing brain altering normative development. 11 Additionally, another critical period of development occurs in adolescents, where the brain is experiencing neural pruning and individuals are seeking a sense of identity. And finally, the transition into adulthood is a crucial period for developing self-efficacy, pursuing meaning, and exposure to opportunities for success. 12 These developmental transitions are periods of vulnerability and opportunity. Research measures for resilience in youth need to consider developmental timing for determining potential risks, protective factors, and outcome measures. Parents are particularly important in raising young children as they pass along genes, impact the environment and provide experiences; all of which has the potential for both positive and negative impact on development. 13 Prior research associated exposure to ACEs in early childhood with academic and behavioral difficulties in kindergarten. 14 This study considers the role of parental stressors and other ACEs, in early childhood when children are especially reliant on their parents in connection to the child’s developmental outcomes.
Developmental Cascades
This study of risk and development is fitting with the framework of developmental cascades. Masten and Cicchetti 7 define developmental cascades as “the cumulative consequences for development of the many interactions and transactions occurring in developing systems that result in spreading effects across levels, among domains at the same level, and across different systems or generations.” (p. 491). This framework can be used to explain the impact of family systems on individual child development and the relationship between one area of development on another. The study of developmental cascades encompasses the impact of one system on another area of development, such as the connection between ACE exposure in childhood and health outcomes in adulthood. 4 This negative type of developmental cascade is also referred to as a risk cascade. 12 Conversely, a positive developmental cascade may be triggered by the impact of an intervention that promotes a healthy developmental trajectory that has lasting effects. This type of cascade is evident in the research on the effectiveness of interventions in early childhood that promote skills for school readiness and parental education that alter the predicted course of development and have a lasting impact. 15 Likewise, Masten and Cicchetti, 7 state:
“Well-times and targeted interventions could interrupt negative or promote positive cascades; these efforts may work by counteracting negative cascades, by targeting the reduction of problems, or by targeting improvements in competence in domains that increase the probability of better function in other domains.” (p. 491)
Understanding the impact of developmental risk cascades in early childhood is especially important for tailoring interventions that can promote a positive developmental trajectory given that the return on investment is greater during early childhood. 16 Therefore, the study of ACEs on the developing child could provide information for interventions to prevent future ACEs and reduce the negative impact of ACEs on development.
Research Questions:
(1) Is there a difference between individual ACEs in predicting the increased likelihood for health and developmental problems?
(2) What predictive power does ACE count have in determining the likelihood of cumulative health and developmental problems in early childhood?
(3) Does the relative risk of ACE score on health and developmental outcomes differ for children who are affectionate with their parent?
Methods
For this study data from the 2016 National Survey for Children’s Health (NSCH) will be used. This dataset, developed by the Health Resources and Service Administration (HRSA) and Maternal and Child Health Bureau (MCHB), provides data on multiple aspects of children’s health and development. The participant sample includes a nationally representative sample of noninstitutionalized children between the ages of newborn and 17 years. Initially, 139 923 households were screened for age eligible children and then one child was selected at random for an interview regarding health and wellbeing. Surveys were administered both by mail and via the internet. A total of 50 212 surveys were completed by parents or guardians. 17 The 2016 NSCH data also includes information on children with special health care needs. Data collection instruments can be found at https://www.childhealthdata.org/learn-about-the-nsch/survey-instruments.
Participants
For this analysis only information using the topical questionnaire for children who were 5 years old or younger are included. Data are weighted to represent the population of noninstitutionalized children nationally and in each state. This analysis includes a subpopulation of children under the age of 6—the age most heavily relying on parents for protection and educational opportunities. There is a total of 14 494 survey responses for children under the age of 6 (29% of the total surveyed sample).
Measures
Demographic characteristics. For this analysis, I have included age (in years), gender, and race/ethnicity (Hispanic, white, Black, other/multi-racial) as control variables. Additionally, a ratio of the household poverty provided by NSCH is included in the descriptive demographic table, but not controlled for in the analysis due to the overlap with the ACE question “How often has it been hard to get by on your family’s income—hard to cover basics like food or housing?”
Adverse Childhood Experiences (ACEs)
The NSCH measure for ACEs is based on parent report and are measured as being either present or absent. The wording of the NSCH ACE questionnaire was modified from the original screener used by the Center for Disease Control (CDC) to minimize under-reporting. 18 The 9 ACE questions were included based on the observable nature of items on which parents can report. The ACE scale included one question for each of the following: economic hardship, parental divorce, death of a parent, parental incarceration, mental illness of a family member, drug/alcohol abuse of family member, domestic violence, neighborhood violence, and racial discrimination. The 9 questions used to measure ACEs are listed in Table 4. The low non-response rate (1.4%) for the ACE questions signifies that the measures were acceptable for respondents. The NSCH-ACE measure is determined to collectively measure overall adversity (Cronbach’s alpha = .66). This is consistent with the findings of Bethell et al 19 confirmatory factor analysis and latent class analysis supporting the usage of the NSCH-ACE measure for assessing cumulative risk.
Table 4.
Survey Question and Prevalence of Each NSCH-ACEs.
| Type of adverse childhood experience | Prevalence for children under 5% | Missing values % |
|---|---|---|
| Difficult to get by on current income | 18.6 | 1.8 |
| Parent or guardian divorced or separated | 9.4 | 2.3 |
| Parent or guardian died | 0.8 | 2.6 |
| Parent or guardian served time in jail | 2.9 | 2.7 |
| Saw or heard parents or adults slap, hit, kick, punch one another in the home | 2.4 | 2.8 |
| Was a victim of violence or witnessed violence in neighborhood | 1 | 2.9 |
| Lived with anyone who was mentally ill, suicidal, or severely depressed | 4.2 | 2.8 |
| Lived with anyone who had a problem with alcohol or drugs | 4.2 | 2.7 |
| Treated or judged unfairly because of his or her race or ethnic group | 0.8 | 2.4 |
| Number of ACEs (mean) | 0.44 | 1.4 |
| 0 ACEs | 70.9 | |
| 1 ACE | 18.9 | |
| 2-3 ACEs | 7 | |
| 4 or more ACEs | 1.8 |
Special health care needs
Five questions were asked in the initial screener regarding special health care needs of children, representing overall problems with health and development. In determining the special health care needs (SHCN) status, NSCH combined several health risks including (1) taking prescription medication, (2) requiring more medical/mental health/educational services than usual for the child’s age, (3) having a condition that limits ability to do age-appropriate tasks, (4) needing special therapies (physical, occupational, or speech), or (5) having ongoing emotional, developmental, or behavioral concerns. If respondents answered yes to any condition a follow up question was asked regarding if the condition is expected to last 12 months or longer. SHCN status is determined based on the presence of a qualifying factor and the anticipated duration of more than 12 months. NSCH also included a total count of qualifying factors that determine whether a child is considered to have special health care needs. 18 An additional variable is available for children who have 2 or more qualifying factors signifying a greater developmental impact of one condition or the presence of multiple comorbid conditions. This analysis includes the total count of all qualifying factors.
Analysis
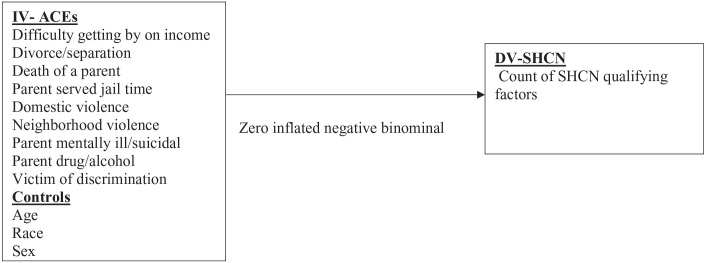
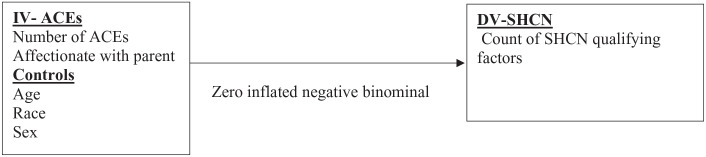
To investigate the impact of individual ACE predictive power and cumulative ACE count on children’s overall health and development, 2 separate zero inflated negative binomial regression models were used. One model was used measuring the individual impact of each ACE (Figure 1). This model will be helpful to measure the direct impact of specific adversities in order to plan targeted interventions. A second model was measured to examine the cumulative impact of ACE count on health and developmental outcomes (Figure 2). This model examines the total cumulative impact of adversities in early childhood.
Figure 1.
Relationship of individual ACEs to the relative risk of cumulative health and developmental impairments.
Abbreviations: ACEs, Adverse Childhood Experiences; CSHCN, Child with Special Health Care Needs.
Figure 2.
Relationship of total ACE score to the relative risk of total health and developmental impairments.
Abbreviations: ACEs, Adverse Childhood Experiences; CSHCN, Child with Special Health Care Needs.
In preparation for data analysis, I examined all variable distribution for normality. Distribution of the continuous independent variable and missing data patterns were assessed. Regarding the ACE count, the skew (3.07) and kurtosis (15.26) fell outside the acceptable range (<3), for this reason and to enhance readability, ACE score will be categorized as (1) 0 ACEs, (2) 1 ACE, (3) 2 or 3 ACEs, or (4) 4 or more ACEs. These categories are consistent with previous research on ACEs.2,4,9
There is no missing data for factors considered as special health needs as these questions were asked in the screener administered before the full questionnaire was completed. As seen in Table 4, missing data for the ACE questions are relatively low (less than 5% for all measures). I found no significant predictors of missingness relative to the variables in my dataset. Therefore, complete case analysis will be used. This decision is supported by the notion that it would be inappropriate to impute sensitive information such as ACE scores or diagnosis.
Variance inflation factors for all variables were <3.0, suggesting no multicollinearity of the data. 20 To determine the best fitting model Poisson regression model (PRM), negative binomial regression model (NBRM), zero inflated Poisson (ZIP), and zero inflated negative binomial (ZINB) models were compared. Zero inflated negative binomial model was preferred over other models based on the AIC and BIC (shown in Table 1). The α (IRR = 0.64, se = 0.16, 95% CI = 0.4, 1.03) is not equal to zero signifying over dispersion of the data, justifying the appropriate use of the zero inflated negative binomial model. In this data having zero qualifying health care needs could be due to lack of qualifying factors or could be lack of health care access to evaluate special health needs. In this data there were a significant percent of children without health care needs. Having no qualifying health needs was associated with younger children, with 95% of children under the age of 1 having zero special health care factors, whereas 84% of children 5 years old had zero qualifying special health care needs (shown in Table 2).
Table 1.
Model Fit Comparisons.
| PRM | NBRM | ZIP | ZINB | |
|---|---|---|---|---|
| BIC | 18 936.89 | 14 780.78 | 14 586.42 | 14 516.85 |
| AIC | 18 883.95 | 14 720.27 | 14 518.35 | 14 441.22 |
Table 2.
Percent of Special Health Care Needs by Age.
| SHCN count | <1 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| No SHCN | 95.25 | 92.88 | 89.67 | 85.97 | 85.10 | 83.63 |
| 1 SHCN | 2.21 | 4.20 | 5.36 | 6.56 | 6.90 | 7.77 |
| 2 SHCN | 1.24 | 1.33 | 1.49 | 2.73 | 3.35 | 3.60 |
| 3 SHCN | 0.70 | 0.58 | 1.56 | 1.98 | 2.17 | 2.04 |
| 4 SHCN | 0.38 | 0.58 | 1.31 | 2.09 | 1.73 | 2.16 |
| 5 SHCN | 0.22 | 0.44 | 0.60 | 0.67 | 0.75 | 0.80 |
Results
Descriptive statistics for the early childhood population are shown in Table 3. The greatest proportion of sample participants were white (70%), followed by other or mixed-racial (14%). The population of this study had slightly more males (51.8%) than females. Children’s age ranged between 1 month and 5 years old with the mean age of 2.6 years old (SD = 1.64). The majority of respondents reported their family income to be above 400% of the federal poverty level with about 10% falling at or below the poverty level.
Table 3.
Sample Characteristics and Prevalence of Special Health Care Needs by ACE count category: Children Ages 0-5 National Survey for Children’s Health 2016.
| Characteristics | Total n = 14 494 |
0 or 1 ACE n = 13 016 |
2 or more ACES n = 1280 |
|---|---|---|---|
| Gender % | |||
| Male | 51.8 | ||
| Female | 48.2 | ||
| Race% | |||
| Hispanic | 10.9 | ||
| White | 70.0 | ||
| Black | 5.1 | ||
| Other/Multi-racial | 14.0 | ||
| Age in years % | |||
| <1 | 12.8 | ||
| 1 | 15.6 | ||
| 2 | 19.4 | ||
| 3 | 17.5 | ||
| 4 | 17.5 | ||
| 5 | 17.2 | ||
| Poverty level % | |||
| At or below 100% FPL | 9.9 | ||
| 100%-199% FPL | 16.0 | ||
| 200%-399% FPL | 32.3 | ||
| Above 400% FPL | 41.8 | ||
| Special Health Care Needs (SHCN) % | 11.6 | 10.4 | 24.1 |
| SHCN—prescription meds | 7.2 | 6.5 | 14.5 |
| SHCN—elevated use of services | 6.1 | 5.3 | 13.8 |
| SHCN—functional limitations | 3.1 | 2.7 | 6.9 |
| SHCN—need/get therapy | 4.1 | 3.5 | 9.5 |
| SHCN—due to emotional, behavioral or developmental delays | 3.3 | 2.6 | 9.9 |
| SHCN based on 2 or more factors% | 5.9 | 5.0 | 15.0 |
This table also includes the percent of children with each qualifying special health need for children with 2 or more ACEs in comparison with those with less than 2 ACEs. A higher proportion of children with 2 or more ACEs experience each of the individual health and developmental conditions. This cut off was used because the overall prevalence of ACEs was fairly low for the early childhood population and this gives an idea of differences on health factors between the group with low adversity and those with moderate or high levels of adversity. Children with special health care needs comprised 11.6% of the sample (shown in Table 3). Taking prescription medication was the most common qualifying factor (7.2%), followed by elevated use of medical or educational services (6.1%), and the fewest number of children (3.3%) qualified based on emotional, behavioral, or developmental needs.
Special health care needs were considered for children with less than 2 ACEs and for children with 2 or more ACEs, this showed differences in the proportion of children within each group who had qualifying special health care needs. 24.1% of children with 2 or more ACEs qualified as having special health care needs, whereas only 10.4% of children with less than 2 ACEs qualified. A greater proportion of children with 2 or more ACEs was found for each of the qualifying factors when compared to children with less ACEs. Additionally, 15% of children with 2 or more ACES also had 2 or more special health care needs, whereas only 5% of children with less than 2 ACEs had multiple health needs. This signifies a difference in the prevalence of special health care needs for young children with ACEs.
Table 4 shows the prevalence of the sample having experienced each individual ACE and broken down by ACE count categories. Of the children in this sample 70.9% had experienced zero ACEs with the average ACE score of 0.44 (SD = 0.92). As represented in Table 4 the prevalence of each individual adversity is low with the most common adversities being financial hardship (18.6%) and parental separation (9.4%).
In the first model, the relative risk of special health needs was determined for each of the ACE questions individually. The model controls for race and sex. Significant findings showed the expected special health needs count increase by 84% for children whose families reported financial hardship (IRR = 1.84, se = 0.12, z = 9.30, P < .001, 95% CI = 1.62, 2.10) and increased by 42% for children who lived with someone who had a mental illness (IRR = 1.42, se = 0.16, z = 3.18, P < .001, 95% CI = 1.14, 1.76). Model results are displayed in Table 5.
Table 5.
Incidence-Rate Ratio for Increased Health and Developmental Difficulties by Individual ACE Exposure and by Cumulative ACE Score.
| Adverse childhood experience | Special health care needs count | |||||
|---|---|---|---|---|---|---|
| Individual ACEs | % | IRR | Std. Err. | z | P | 95%CI |
| Difficult to get by on current income | 84 | 1.84 | 0.12 | 9.30 | .00*** | 1.62-2.1 |
| Parent or guardian divorced or separated | 2 | 1.02 | 0.09 | 0.23 | .82 | 0.86-1.21 |
| Parent or guardian died | −18 | 0.82 | 0.23 | −0.70 | .49 | 0.47-1.43 |
| Parent or guardian served time in jail | 13 | 1.13 | 0.15 | 0.95 | .34 | 0.87-.147 |
| Saw or heard parents or adults slap, hit, kick, punch one another in the home | −1 | 0.99 | 0.15 | −0.04 | .97 | 0.74-1.34 |
| Was a victim of violence or witnessed violence in neighborhood | 21 | 1.21 | 0.24 | 0.96 | .34 | 0.82-1.78 |
| Lived with anyone who was mentally ill, suicidal, or severely depressed | 42 | 1.42 | 0.16 | 3.18 | .001** | 1.14-1.76 |
| Lived with anyone who had a problem with alcohol or drugs | 6 | 1.06 | 0.14 | 0.45 | .66 | 0.82-1.36 |
| Treated or judged unfairly because of his or her race or ethnic group | 23 | 1.23 | 0.29 | 0.89 | .37 | 0.78-1.96 |
| Total ACE score | ||||||
| 1 ACE | 68 | 1.68 | 0.11 | 7.96 | .00*** | 1.48-1.91 |
| 2-3 ACEs | 83 | 1.83 | 0.16 | 6.98 | .00*** | 1.55-2.18 |
| 4 or more ACEs | 137 | 2.37 | 0.30 | 6.87 | .00*** | 1.85-3.03 |
| Child is affectionate with adult | −33 | 0.67 | 0.06 | –4.57 | .00*** | 1.77-3.08 |
Models controls for age, sex, and race.
***P < .001. **P < .01. *P < .05.
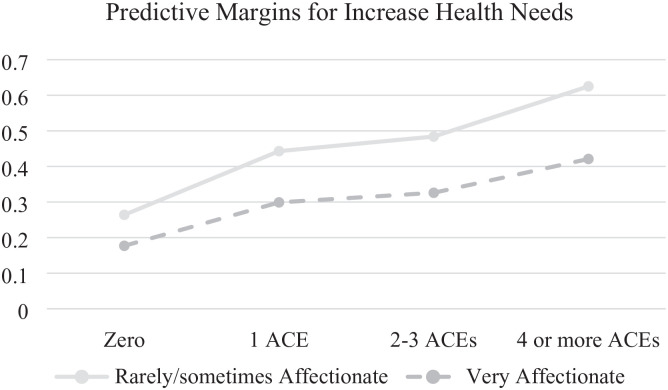
A zero inflated negative binominal model was used to determine the predictive power of ACE count on cumulative health care needs. In the second model, after controlling for race and sex, the relative risk of special health care needs was determined based on the cumulative ACE count category and by attachment to caregiver. Overall, there was a strong positive relationship between the number of ACEs a child had experienced and the count of special health care needs (displayed in Table 5). Compared to those with zero ACEs, children with one ACE have 68% higher odds of having special health care needs (IRR = 1.68, se = 0.11, z = 7.69, P < .001, 95% CI = 1.48, 1.91). Children with 2 or 3 ACEs have 83% higher odds of having special health care needs relative to those with no ACEs (IRR = 1.83, se = 0.16, z = 6.98, P < .001, 95% CI = 1.55, 2.18). Lastly, children who experienced 4 or more ACEs had 137% increase odds when compared to those with no ACEs (IRR = 2.37, se = 0.30, z = 6.87, P < .001, 95% CI = 1.85, 3.03).
Alternatively, there was a 33% decrease in odds of special health care needs for children who were reported as being affectionate with their caregiver relative to those who were not (IRR = 0.67, se = 0.06, z = −4.57, P < .001, 95% CI = 1.77, 3.08). This relationship is depicted in Figure 3. An ANOVA was used to test the significance of the difference in mean qualifying factors by affection at each ACE count category. Findings indicated a statistically significant (P < .001) difference for children with less than 4 ACEs (results not shown). For children with 4 or more ACEs, being affectionate with a parent was not significant in predicting mean number of special health care factors.
Figure 3.
Predictive margins by ACE score for increased health and developmental difficulties sorted by affectionate children.
Discussion
During the period of early childhood, children are rapidly developing neurological connections; thus, development during these crucial years is also associated with success in later years. 6 In this nationally representative sample of young children, experiencing ACEs was associated with poor health and developmental outcomes. Similar to prior ACE research, this study finds significant predictive power in cumulative ACE count and increased odds for worse overall outcomes with high ACE scores.1-4 This phenomenon of ACE count predicting poor health and developmental outcomes, which is in turn predictive of difficulties later in life, is considered a risk cascade 7 . Conversely, children with no or low ACEs were less likely to experience health and developmental difficulties, and are therefore, likely to continue experiencing success on age salient tasks, this represents a positive developmental trajectory or success cascade. The desired outcome of interventions would be to alter the developmental trajectory for those youth who have experienced adversity and put into place factors which will promote future successes.
In this study individual ACEs were measured for predictive power and it was found that many of the ACEs when measured individually did not have significant predictive power in determining the odds for increase health and developmental difficulties. The 2 ACEs that were statistically significant (financial hardship and living with someone with a mental illness) both had slightly larger confidence intervals indicating that there is variance in outcome for children who have experienced those ACEs. Financial hardship has been determined to be associated with many additional risk factors, such as poor health and development, so this finding aligns with prior research on the impacts of poverty. 21 Prior research on parental depression and mental illness has noted the impact of depression on the social-emotional development of children. Furthermore, there is notable differences in the parent-child attachment for children whose parent has a mental illness. 22 Additionally, parental mental illness may be associated with increased odds for special health needs based on the genetic risk of passing down emotional difficulties to the child.
The second model used in this study confirmed that higher ACE scores are associated with increased risk for health and developmental factors. These findings confirm the suggestions from Bethell et al 19 to use an ACE score to measure cumulative risk. Relative to children with no ACEs, children who have experienced ACEs had an increased risk for taking prescription medication, requiring more medical/educational services than typical for their age, have limitations that impact their daily functioning, receiving special services, or having emotional, behavioral, or developmental difficulties. This study adds to the growing body of literature around ACEs in that it links adversity to health and developmental difficulties in childhood.1-3 These special health and developmental needs in early childhood have implications for future developmental trajectories. 6
These findings also add to the literature connecting childhood adversity to adult health outcomes. Comple-menting prior work focusing on adult health behaviors, this study provides information connecting ACE exposure to health and developmental outcomes during childhood that may influence the health disparities observed in adulthood. 4 Recent research predicts that prevention of ACEs would lead to a significant decrease in depression, kidney disease, stroke, coronary heart disease, cancer, diabetes, and obesity in America. 23 Furthermore, ACE prevention was associated with predictive decreases in health risk behaviors (smoking and drinking) in adulthood and in socioeconomic challenges such as unemployment.
This study highlights the risk cascade associated with early childhood exposure to ACEs and health and developmental outcomes. Given the connection between health and development for young children, this work has implications for both pediatricians and early childhood educators. Given the frequent contact with families and length of time working with a family, these professionals are uniquely positioned to identify ACEs and developmental outcomes. Additionally, they can provide resources or referrals for families in order to promote positive developmental trajectories. Programs such as Head Start, Nurse Home Visiting, Universal Pre-Kindergarten and other preventative programs may help reduce the achievement gap and health disparities noted in other studies.2,3,24 Guidance from the National Center for Injury Prevention and Control echoes this need in emphasizing the role of quality care and education in early childhood in preventing future ACE exposure. 25
Lastly, this study contributes to the growing body of literature around resilience in examining the role of secure attachment in altering the impact of ACEs on health and development. Children who were reported showing affection to their parent had a decreased risk for health and developmental difficulties when compared to children with the same number of ACEs who did not frequently show affection toward their parent. This finding contributes to the work of Bellis et al 9 in confirming the role of a secure attachment in undermining the negative impact of ACEs. This confirms the notion that parents can serve as protective factors in mitigating the impact of risks and promoting resilience in youth. 12
Limitations and Recommendations
While this study adds to the growing body of literature regarding ACEs and ACE resilience, it is not without limitations. The dataset used for this analysis was a convenient nationally representative sample, yet the NSCH data may not be fully representative of children experiencing ACEs since the majority of the sample had experienced none. Additionally, the sample was composed of majority white and affluent respondents. Furthermore, the nature of the NSCH questionnaire was self-report which may have been biased by social desirability. 26
One limitation in measuring developmental cascades is that it does not measure developmental changes over time. The data being used takes into consideration the parents’ perspective in health conditions expected to last at least 12 months, but this does not give a complete picture of the relationship between ACEs and children’s developmental trajectories. The nature of the NSCH data provides rich data from a single time point, but there is currently no publicly available longitudinal data measuring ACEs in childhood.
While the difference in predictive power of ACEs on cumulative health outcomes were examined both for children with and without an affectionate relationship with their parent, the analysis used does not measure a moderating effect. Additionally, research on resilience includes many parental characteristics that serve as protective factors. 12 In this analysis the only parent level measures were the ACEs. It is recommended that further research be conducted to look at the positive impact that families can have in lessening the impact of ACEs.
Conclusion
This study enriches the rapidly expanding literature on adverse childhood experiences and developmental implications, by narrowing the focus to early childhood where children are most reliant on their families and therefore may be most susceptible to family dysfunction and other ACEs. This study uses a nationally representative sample to confirm the risk cascade relationship between increased ACEs and risk for health and developmental difficulties. Furthermore, this study begins to examine the role parent-child attachment can play in promoting resilience in the face of adversity. The findings from this study underscore the importance of tailored interventions to prevent further risks and promote positive developmental trajectories during early childhood.
Footnotes
Author Contributions: The author confirm contribution to the paper as follows: study conception and design; analysis and interpretation of results; draft manuscript preparation and review.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Erica M. Webster  https://orcid.org/0000-0001-8915-0280
https://orcid.org/0000-0001-8915-0280
References
- 1. Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff. 2014;33(12):2106-2115. doi: 10.1377/hlthaff.2014.0914 [DOI] [PubMed] [Google Scholar]
- 2. Bower C, Baldwin S. Poverty, Stress, and Academic Performance: ACE Scores and the WSCC Model in an Urban District. SSRN Electronic Journal, 2017. [Google Scholar]
- 3. Burke Harris N. The Deepest Well: Healing the Long-Term Effects of Childhood Adversity. Houghton Mifflin Harcourt; 2018. [Google Scholar]
- 4. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14(4):245-258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 5. Center for Youth Wellness. ACEs and toxic stress. n.d. Accessed 2019. https://centerforyouthwellness.org/
- 6. Center on the Developing Child. The foundations of lifelong health are built in early childhood. 2010. www.developingchild.harvard.edu
- 7. Masten AS, Cicchetti D. Developmental cascades. Dev Psychopathol. 2010;22:491-495. [DOI] [PubMed] [Google Scholar]
- 8. Seok D, Murphy D, Abdi F. Children With Special Health Care Needs Are More Likely to Have Adverse Childhood Experiences. Child Trends. 2019. https://www.childtrends.org/children-with-special-health-care-needs-are-more-likely-to-have-adverse-childhood-experiences [Google Scholar]
- 9. Bellis MA, Hardcastle K, Ford K, et al. Erratum to: does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences - a retrospective study on adult health-harming behaviours and mental well-being. BMC Psychiatry. 2017;17(1):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Masten AS. Resilience theory and research on children and families: past, present, and promise. J Fam Theory Rev. 2018;10:12-31. doi: 10.1111/jftr.12255 [DOI] [Google Scholar]
- 11. Bick J, Nelson CA. Early adverse experiences and the developing brain. Neuropsychopharmacology. 2016;41:177-196. doi: 10.1038/npp.2015.252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Masten AS. Ordinary Magic: Resilience in Development. Guilford Press; 2015. [Google Scholar]
- 13. National Scientific Council on the Developing Child. The timing and quality of early experiences combine to shape brain architecture. Working paper no. 5. 2007. www.developingchild.harvard.edu
- 14. Jimenez ME, Wade R, Jr, Lin Y, Morrow L. M, Reichman N. E. Adverse experiences in early childhood and kindergarten outcomes. Pediatrics. 2016;137(2):e20151839. doi: 10.1542/peds.2015-1839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aikens N, Kopack Klein A, Tarullo L, West J. Getting Ready for Kindergarten: Children’s Progress During Head Start. FACES 2009 Report. OPRE Report 2013-21a. Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services; 2013. [Google Scholar]
- 16. Executive Office of the President of the United States. The Economics of Early Childhood. Executive Office of the President of the United States; 2014. [Google Scholar]
- 17. Child and Adolescent Health Measurement Initiative. “2016 National Survey of Children’s Health, Sampling and Survey Administration.” Data Resource Center, supported by Cooperative Agreement 1-U59-MC06980-01 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). 2017. www.childhealthdata.org [Google Scholar]
- 18. U.S. Census Bureau. 2016 National Survey of Children’s Health: Methodology Report. US Census Bureau. 2018. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2016-NSCH-Methodology-Report.pdf [Google Scholar]
- 19. Bethell CD, Carle A, Hudziak J, et al. Methods to assess adverse childhood experiences of children and families: toward approaches to promote child well-being in policy and practice. Acad Pediatr. 2017;17(7):S51-S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kline RB. Principles and Practice of Structural Equation. The Guilford Press; 2011. [Google Scholar]
- 21. Jensen E. Teaching With Poverty in Mind : What Being Poor Does to Kids’ Brains and What Schools Can Do About It. ASCD; 2009. [Google Scholar]
- 22. Woolhouse H, Gartland D, Mensah F, Giallo R, Brown S. Maternal depression from pregnancy to 4 years postpartum and emotional/behavioural difficulties in children: results from a prospective pregnancy cohort study. Arch Womens Ment Health. 2016;19(1):141-151. [DOI] [PubMed] [Google Scholar]
- 23. Merrick MT, Ford DC, Ports KA, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention - 25 states, 2015-2017. MMWR Morb Mortal Wkly Rep. 2019;68(44):999-1005. doi: 10.15585/mmwr.mm6844e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Blodgett C, Lanigan JD. The association between adverse childhood experience (ACE) and school success in elementary school children. Sch Psychol Q. 2018;33(1):137-146. doi: 10.1037/spq0000256 [DOI] [PubMed] [Google Scholar]
- 25. Fortson BL, Klevens J, Merrick MT, Gilbert LK, Alexander SP. Preventing Child Abuse and Neglect: A Technical Package for Policy, Norm, and Programmatic Activities. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 26. Fisher RJ, Katz JE. Social-desirability bias and the validity of self-reported values. Psychol Market. 2000;17(2):105-120. doi: [DOI] [Google Scholar]