Abstract
Study Objectives:
To compare the efficiency of a TCM scoring system that includes 3 independent predictors obtained by physical examination, computed tomography, and polysomnography with the standard Friedman staging system that includes only physical examination variables for predicting surgical outcomes in patients with obstructive sleep apnea syndrome who undergo velopharyngeal surgery.
Methods:
This prospective study was carried out in 265 patients with obstructive sleep apnea syndrome who underwent velopharyngeal surgery. All these patients were re-examined with polysomnography for evaluation of surgical outcomes at least 3 months after surgery. The efficacies in the surgical outcome prediction of 2 systems were calculated and compared.
Results:
The overall response rate and cure rate was 63.8% (169/265) and 22.3% (59/265), respectively. There were 32 patients with Friedman stage I, with a response rate and cure rate of 81.3% (26/32) and 28.1% (9/32), respectively, and 70 patients with TCM scores of < 14 with a response rate and cure rate of 91.4% (64/70) and 42.9% (30/70), respectively. Friedman stage and TCM grade were the only 2 factors independently predictive of surgical response (P < .05, odds ratio value = 0.642 and 0.382). The receiver operating characteristic curve analysis for surgical response showed that the area under the curve value was 0.600 for Friedman stage, which was significantly lower than that for TCM grade, 0.718 (P = .005). Apnea-hypopnea index and TCM grade were the only 2 factors independently predictive of surgical cure (P < .05, odds ratio value = 0.981 and 0.465).
Conclusions:
Compared with the Friedman staging system, the TCM scoring system was more efficient in selecting proper candidates for velopharyngeal surgery. The main reason may be its better utilization of patients’ preoperative information, especially the inclusion of physiological factors.
Clinical Trial Registration:
Registry: Chinese Clinical Trials Register; Name: Clinical Phenotypes and Precise Treatment of Adult OSA (Obstructive Sleep Apnea): A Multicenter Study; URL: http://www.ChiCTR.org.cn/showproj.aspx?proj=21189; Identifier: ChiCTR-ONC-17013132.
Citation:
Zhang J, Cao X, Yin G, et al. The significance of better utilization of patients’ preoperative information in predicting outcomes of velopharyngeal surgery: a prospective cohort study. J Clin Sleep Med. 2022;18(3):843–850.
Keywords: obstructive sleep apnea, velopharyngeal surgery, anatomy, physiology, prediction
BRIEF SUMMARY
Current Knowledge/Study Rationale: The objective efficacy of velopharyngeal surgery for treating obstructive sleep apnea syndrome (OSAS) is not high (40%–60%). During the past decades, several preoperative factors had been identified to be predictive for the outcomes of velopharyngeal surgery. Friedman et al had combined 3 such predictors from just physical examination to build a system called the Friedman staging system. Currently, this system is still commonly used for preliminary patient selection for velopharyngeal surgery. In fact, patients with OSAS always receive more examinations before surgery, and so, the utilization of just physical examination factors does not make full use of the clinical information. We hypothesized that a better use of the preoperative information of patients with OSAS could further improve the predictive efficacies for treatment outcomes.
Study Impact: In a prospective patient sample, the predictive efficacies of 2 systems were calculated and compared. One was the Friedman staging system, based on factors from just physical examination. The other was the TCM scoring system we had built, based on factors from physical examination, polysomnography, and upper airway imaging. We finally found that, compared with the Friedman staging system, the TCM scoring system was more efficient in selecting proper candidates for velopharyngeal surgery, especially in selecting patients who were more likely to be cured. These results suggest the importance of a better utilization of the preoperative information of patients with OSAS in patient selection for velopharyngeal surgery.
INTRODUCTION
Velopharyngeal surgery remains the most common treatment approach for obstructive sleep apnea syndrome (OSAS).1–3 Its major advantages are simple procedure, low risks of complications, good self-reported treatment outcomes, and excellent adherence. However, its objective efficacy remains limited: Only 40%–60% of patients respond well to surgery.4–6 Over the past decades, various outcome predictors have been evaluated for a reasonable selection of patients eligible to receive this type of surgery. Although the results are not always consistent, some preoperative factors, including body mass index (BMI), tonsil size, palate position, and some polysomnography (PSG) and imaging variables were identified to be predictive for the treatment outcomes.7–13
The clinical significance of a single predictor is always limited. Theoretically, the combination of multiple predictors could be useful in improving predictive efficacies. The Friedman staging system, which consists of tonsil size, palate position, and BMI, was developed based on such a hypothesis.14 This system is simple and is commonly used for preliminary patient selection at the outpatient department, as all 3 factors could be easily obtained by physical examination. In fact, patients with OSAS who undergo velopharyngeal surgery usually receive more preoperative examinations. Therefore, the utilization of information obtained from just physical examination for predicting treatment outcomes does not make full use of patients’ preoperative information.
In a previous study, we screened independent predictors from more preoperative data obtained from physical examination, PSG, and upper airway computed tomography (CT). Consequently, 3 independent predictors (tonsil grade, the percentage of time with oxygen saturation below 90% (CT90), and the hyoid position) were found and were further integrated into a new system called the TCM scoring system,12 which was proved to be efficient in identifying proper candidates for velopharyngeal surgery.12
We hypothesized that the TCM scoring system will more accurately predict surgical outcomes compared to the classic Friedman staging system in patients with OSAS who undergo velopharyngeal surgery. In the current study, a new sample of patients with OSAS from 3 medical centers who underwent such surgery was included. By comparisons of the capacities of these 2 systems for predicting surgical outcomes, we could also prove the importance of better utilization of patients’ information in improving patient selection efficacy, as our system relies on more preoperative examinations.
METHODS
Study population
Patients with OSAS who underwent velopharyngeal surgery at Beijing Tsinghua Changgung Hospital, Peking University First Hospital, and Beijing Friendship Hospital between December 2014 and March 2019 were included in this prospective cohort study. None of the 119 patients initially enrolled in our previous study12 were included in the present study. Inclusion criteria were (1) age > 18 years; (2) BMI ≤40 kg/m2; (3) refusal or intolerance to the first-line treatment of positive airway pressure; (4) no severe coexisting pulmonary, cardiovascular, or neuropsychiatric disorders; (5) no previous surgical treatment history for OSAS; and (6) no other surgical procedures (such as nasal or glossopharyngeal surgical procedures) performed during this velopharyngeal surgery. All patients underwent PSG tests at least 3 months after surgery. Patients who were lost to follow-up or who had BMI changes of > 3 kg/m2 at the time of postoperative PSG were excluded from final analyses. The study method was approved by the Beijing Tsinghua Changgung Hospital Institutional Review Board, and all patients provided their informed consent to the study.
Surgical procedure
The velopharyngeal operations performed in the patient sample were all a combination of revised uvulopalatopharyngoplasty with uvula preservation and transpalatal advancement pharyngoplasty. Patients with OSAS who underwent different velopharyngeal procedures were excluded. The detailed procedures for such surgeries have been previously published.15,16
Polysomnography
The preoperative and postoperative PSG tests were all done at the sleep centers where the surgeries were performed. All PSG tests were completed by recording the following: electroencephalogram, electrooculogram, electrocardiogram, chin electromyography, nasal flow pressure (thermistor and nasal pressure cannula), respiratory (thoracic and abdominal) movements, oxyhemoglobin saturation (pulse oximeter), and body position. All the signal data were analyzed by experienced technicians according to the same criteria, which were the latest scoring guidelines of the American Academy of Sleep Medicine.17 The PSG variables obtained for analyses included apnea-hypopnea index (AHI), obstructive AHI, the lowest oxygen saturation, and CT90 during sleep.
Physical examination and CT of the upper airway
Before surgery, all patients underwent physical examination and CT of the upper airway to obtain the following variables: BMI, palate position, tonsil size, and hyoid bone position, which was the vertical distance between the lower edge of the mandible and the lower edge of the hyoid (MH). These variables were all collected by 1 experienced physician to ensure a properly controlled bias. The tonsil size was evaluated according to the Brodsky Grading Scale.18 In this study, grade 0 and grade 1 tonsil size were both defined as grade 1. The palate position was evaluated according to the modified Mallampati grade.7 Meanwhile, to ensure the reproducibility and consistency of MH, all CT scans were performed during the expiratory phase, with the patients in a supine position and the Frankfort horizontal plane being perpendicular.12
Friedman staging system and TCM scoring system
The Friedman stages of all patients were evaluated according to the Friedman staging system based on tonsil size, palate position, and BMI (Table 1).14 TCM scores were calculated according to the TCM scoring system as previously described12 (Table 2). The total scores of all patients were calculated using the following equation: Total score = 2.7 tonsil size (score) + 2.2 CT90 (score) + 1.6 MH (score). All patients were grouped according to specific cutoff scores, which were TCM scores of < 14, 14–17, 17–22, and ≥ 22, respectively.
Table 1.
Friedman staging system.14
| Palate Position | Tonsil Size | BMI (kg/m2) | |
|---|---|---|---|
| Stage I | 1, 2 | 3, 4 | < 40 |
| Stage II | 1, 2 | 0, 1, 2 | < 40 |
| 3, 4 | 3, 4 | ||
| Stage III | 3, 4 | 0, 1, 2 | < 40 |
| Stage IV | 1, 2, 3, 4 | 0, 1, 2, 3, 4 | ≥ 40 |
| All patients with significant craniofacial or other anatomic deformities | |||
BMI = body mass index.
Table 2.
TCM scoring system.12
| Coefficient | Score | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Tonsil size | 2.7 | Grade 4 | Grade 3 | Grade 2 | Grade 1 |
| CT90 (%) | 2.2 | < 10 | 10–20 | 20–40 | ≥ 40 |
| MH (mm) | 1.6 | < 10 | 10–15 | 15–20 | ≥ 20 |
CT90 = percentage of time with oxygen saturation below 90%, MH = vertical distance between the lower edge of the mandible and the lower edge of the hyoid.
Definition of surgical outcomes
The classic definition of surgical outcomes according to the changes of AHI and the postoperative AHI values were used in this study.19 The surgical response was defined as a ≥ 50% decrease in AHI and a postoperative AHI of < 20 events/h. The surgical cure was defined as a postoperative AHI of < 5 events/h.
Statistical analysis
Common statistical analyses in this study were performed with SPSS 20.0 software package (IBM Corporation, Armonk, NY). In detail, the paired Student t test was used to compare preoperative and postoperative mean values, the unpaired Student t test was used to compare continuous variables between different groups, the Pearson chi square test was used to compare categorical variables between different groups, and multiple logistic regression analysis was used to evaluate the significance of independent variables.
Except for the above analyses, the receiver operating characteristic (ROC) curve test was used to determine predictive values of independent variables by calculating the area under the curve value. In this study, the ROC analyses and the comparison of different ROC curves were all performed with the MedCalc 20.0 software package (MedCalc Software bvba, Ostend, Belgium). The calculation of statistical power was performed with the PASS 15.0 software package (NCSS, Kaysville, UT).
All continuous variables were displayed as mean value ± standard deviation. For all analyses, a P value < .05 was considered to be statistically significant.
RESULTS
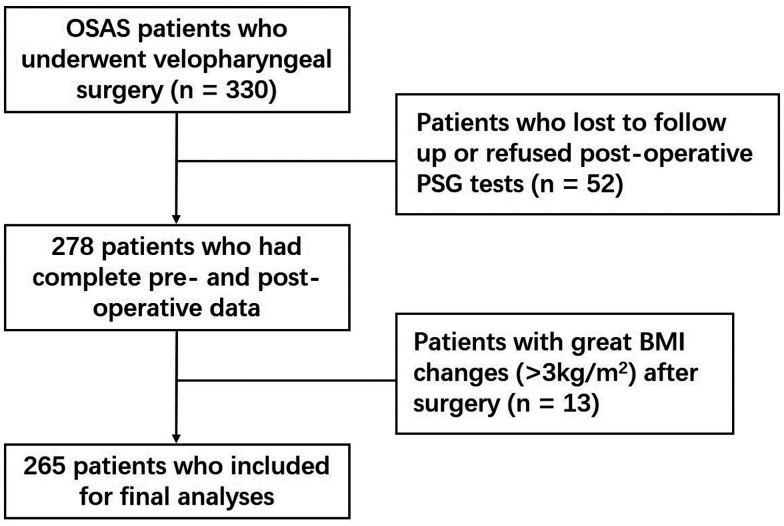
As shown in Figure 1, 330 patients with OSAS were initially included. Fifty-two of them were eventually excluded due to loss to follow-up or refusal of postoperative PSG test. As shown in Table 3, there were no significant differences between those who completed a postoperative PSG test and those who did not with respect to baseline information including age, sex, BMI, AHI, lowest oxygen saturation, Friedman stage, and TCM grade (all P > .05). Another 13 patients were further excluded due to great BMI changes (> 3 kg/m2) after surgery. Therefore, 265 patients with OSAS with an age range of 21–67 years were finally included in the data analyses, including 240 men (90.6%) and 25 women (9.4%).
Figure 1. Study flowchart.
BMI = body mass index, PSG = polysomnography, OSAS = obstructive sleep apnea syndrome.
Table 3.
The baseline information of the 330 patients with OSAS according to whether they had completed a postoperative PSG test or not.
| All Patientsa (n = 330) | Whether Patients Completed Postoperative PSG Test or Not | P | ||
|---|---|---|---|---|
| Yes (n = 278) | No (n = 52) | |||
| Age (y) | 39.6 ± 9.1 | 39.9 ± 9.0 | 37.9 ± 9.1 | .136 |
| Sex | .952 | |||
| Male | 299 (90.6%) | 252 | 47 | |
| Female | 31 (9.4%) | 26 | 5 | |
| BMI (kg/m2) | 27.5 ± 3.2 | 27.5 ± 3.3 | 27.8 ± 2.9 | .471 |
| AHI (events/h) | 53.5 ± 22.5 | 53.7 ± 21.8 | 52.6 ± 25.8 | .758 |
| LSAT (%) | 74.7 ± 10.2 | 74.6 ± 10.2 | 75.1 ± 10.2 | .725 |
| Friedman stage | .193 | |||
| Stage I | 42 (12.7%) | 34 | 8 | |
| Stage II | 169 (51.2%) | 138 | 31 | |
| Stage III | 119 (36.1%) | 106 | 13 | |
| TCM grade | .273 | |||
| < 14 | 93 (28.2%) | 74 | 19 | |
| 14–17 | 117 (35.5%) | 97 | 20 | |
| 17–22 | 100 (30.3%) | 89 | 11 | |
| ≥ 22 | 20 (6.1%) | 18 | 2 | |
aThe overall age, BMI, AHI, and LSAT were all described as average value ± standard deviation; the distributions of sex, Friedman stage, and TCM grade were all described as total number (percentage). AHI = apnea-hypopnea index, BMI = body mass index, LSAT = lowest oxygen saturation, OSAS = obstructive sleep apnea syndrome, PSG = polysomnography.
The overall AHI of the 265 patients with OSAS decreased significantly from 53.6 ± 21.7 events/h (range 5.3–115.7 events/h) to 18.1 ± 16.9 events/h after surgery (range 0.2–78.9 events/h) (P < .001). The overall obstructive AHI also decreased significantly from 49.0 ± 20.2 events/h (range 5.3–101.5 events/h) to 15.9 ± 14.9 events/h after surgery (range 0.2–70.5 events/h) (P < .001). There were 169 responders (63.8%) and 96 nonresponders (36.2%). Among the 169 responders, 59 patients were cured (AHI < 5 events/h) and the cure rate was 22.3%.
The baseline data based on treatment outcomes are shown in Table 4. Compared with nonresponders, responder patients had higher lowest oxygen saturation and higher ratios of small Friedman stages and small TCM grades (all P < .05). Meanwhile, compared with noncured patients, cured patients had lower BMI, lower AHI, higher lowest oxygen saturation, and higher ratios of small TCM grades (all P < .05).
Table 4.
The baseline and surgical information of the 265 patients according to surgical success and surgical cure.
| All Patientsa (n = 265) | Responders (n = 169) | Nonresponders (n = 96) | P | Cured Patients (n = 59) | Noncured Patients (n = 206) | P | |
|---|---|---|---|---|---|---|---|
| Age (y) | 40.2 ± 8.9 | 40.6 ± 9.3 | 39.6 ± 8.2 | .361 | 38.9 ± 9.3 | 40.6 ± 8.8 | .178 |
| Sex | .076 | .083 | |||||
| Male | 240 (90.6%) | 149 | 91 | 50 | 190 | ||
| Female | 25 (9.4%) | 20 | 5 | 9 | 16 | ||
| BMI (kg/m2) | 27.4 ± 3.3 | 27.2 ± 3.2 | 27.8 ± 3.4 | .179 | 26.4 ± 2.9 | 27.7 ± 3.4 | .005† |
| AHI (events/h) | 53.6 ± 21.7 | 51.7 ± 22.2 | 57.0 ± 20.5 | .060 | 43.1 ± 22.6 | 56.7 ± 20.6 | < .001† |
| LSAT (%) | 74.8 ± 10.2 | 76.1 ± 10.0 | 72.6 ± 10.2 | .007* | 79.5 ± 9.1 | 73.5 ± 10.1 | < .001† |
| Friedman stage | .010* | .325 | |||||
| Stage I | 32 (12.1%) | 26 | 6 | 9 | 23 | ||
| Stage II | 131 (49.4%) | 88 | 43 | 32 | 99 | ||
| Stage III | 102 (38.5%) | 55 | 47 | 18 | 84 | ||
| TCM grade | < .001* | < .001† | |||||
| < 14 | 70 (26.4%) | 64 | 6 | 30 | 40 | ||
| 14–17 | 91 (34.3%) | 56 | 35 | 18 | 73 | ||
| 17–22 | 86 (32.5%) | 46 | 40 | 11 | 75 | ||
| ≥ 22 | 18 (6.8%) | 3 | 15 | 0 | 18 |
aThe overall age, BMI, AHI, and LSAT were all described as average value ± standard deviation; the distributions of sex, Friedman stage, and TCM grade were all described as total number (percentage). *Significant differences were observed between responders and nonresponders with respect to LSAT, Friedman stage, and TCM grade (all P < .05). †Significant differences were observed between cured patients and noncured patients with respect to BMI, AHI, LSAT, and TCM grade (all P < .05). AHI = apnea-hypopnea index, BMI = body mass index, LSAT = lowest oxygen saturation.
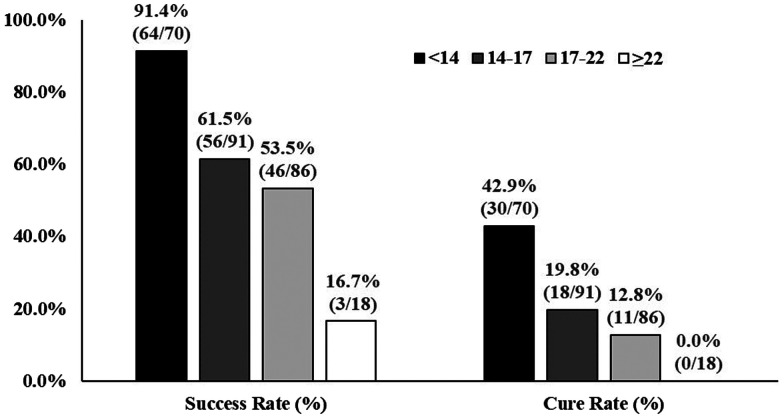
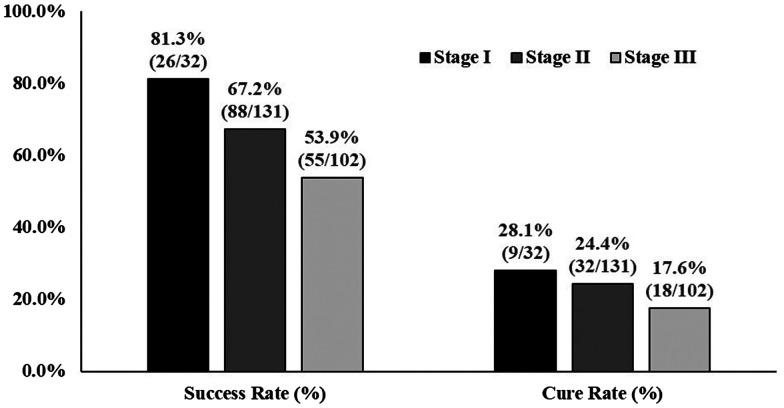
The distributions of surgical outcomes among patients with different TCM grades and Friedman stages are shown in Figure 2 and Figure 3. Patients with TCM scores of < 14 had a higher response rate and cure rate compared to those with TCM scores >14, including 14–17, 17–22, and ≥ 22, respectively (all P < .05). Patients with Friedman stage I also showed a higher response rate and cure rate than patients with Friedman stages II–III. However, only the comparison of the response rate between patients with Friedman stage I and patients with Friedman stage III showed significant difference (P < .05).
Figure 2. The relationship between TCM score grade and treatment outcomes.
Patients with TCM scores of < 14 had a higher response rate and cure rate compared to those with TCM scores > 14 (all P < .05). TCM = system based on 3 factors: tonsil grade, percentage of time with oxygen saturation below 90%, vertical distance between lower edge of the mandible and lower edge of hyoid.
Figure 3. The relationship between Friedman stage and treatment outcomes.
Only the comparison of response rate between patients with Friedman stage I and patients with Friedman stage III showed a significant difference (all P < .05).
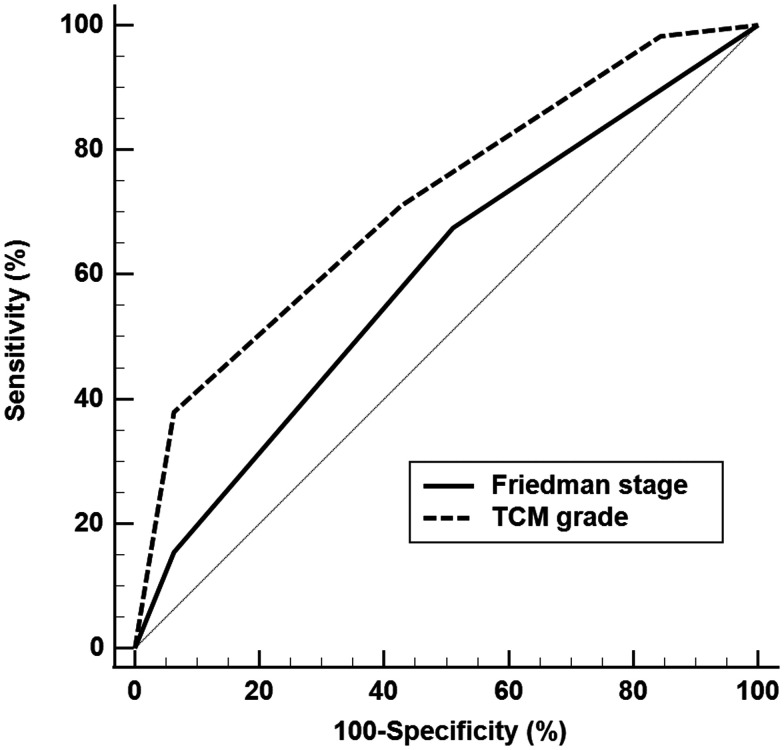
Two independent predictors for surgical response were found among all the variables analyzed in Table 4, which were Friedman stage (P = .046, odds ratio value = 0.642, 95% confidence interval [CI] = 0.416–0.992) and TCM grade (P < .001, OR value = 0.382, 95% CI = 0.273–0.534), respectively. As shown in Figure 4, the ROC analysis for surgical response showed that the area under the curve value was 0.600 for Friedman stage (P = .002, standard error = 0.032, 95% CI = 0.539–0.660), which was significantly lower than that for TCM grade, 0.718 (P < .001, standard error = 0.030, 95% CI = 0.659–0.771), (P = .005). The statistical power calculated for this comparison using a 2-sided z-test at a significance level of .05 could reach .951.
Figure 4. The receiver operating characteristic curve analyses of Friedman stage and TCM grade for surgical response.
The area under the curve value was significantly lower for Friedman stage than for TCM grade (P = .005). TCM = system based on 3 factors: tonsil grade, percentage of time with oxygen saturation below 90%, vertical distance between lower edge of the mandible and lower edge of hyoid.
Meanwhile, 2 independent predictors for surgical cure were found among the same group of variables, which were AHI (P = .017, odds ratio value = 0.981, 95% CI = 0.966–0.997) and TCM grade (P < .001, odds ratio value = 0.465, 95% CI = 0.306–0.705), respectively. The ROC analyses for surgical cure showed that the area under the curve was 0.672 for AHI (P < .001, 95% CI = 0.591–0.754) and 0.701 for TCM grade (P < .001, 95% CI = 0.627–0.775).
DISCUSSION
Our data showed that the TCM scoring system could more accurately predict surgical outcomes compared to the Friedman staging system in patients with OSAS undergoing velopharyngeal surgery. The Friedman staging system is based on only physical examination data,7 while the TCM scoring system relies on physical examination, PSG, and upper airway imaging data.12 The superiority of the TCM scoring system supported the importance of a better utilization of patients’ preoperative information in patient selection.
The standard Friedman staging system has been commonly applied for predicting treatment outcomes of velopharyngeal surgery.14 Several studies proved its clinical significance.20–22 Choi et al8 performed a meta-analysis that included 15 outcome predictor studies and 1,257 patients and found that Friedman stage I is a strong predictor for surgical response after uvulopalatopharyngoplasty, while Friedman stage III and low hyoid position are negative predictors, which is consistent with our data.
Compared with our previous retrospective study, the supporting evidence of the superiority of the TCM scoring system over the Friedman staging system in patient selection was much stronger in the current study. Except for the direct evidence that TCM grade was more efficient in predicting surgical response than Friedman stage with the comparison of ROC curves, there was also other evidence that could support our hypothesis, including the following: (1) the response rate and cure rate were higher in patients with TCM scores of < 14 than in patients with Friedman stage I (response rate: 91.4% vs 81.3%, cure rate 42.9% vs 28.1%); (2) the proportion of patients with TCM scores of < 14 was 2-fold higher than the proportion of patients with Friedman stage I (26.4% vs 12.1%), suggesting that more proper candidates could be selected by this system; (3) patients with TCM scores of < 14 showed a significantly higher response rate and cure rate than patients with TCM scores of 14–17, 17–22, and ≥ 22, while this was not observed in patients with Friedman stage I, who only showed a significantly higher response rate than patients with Friedman stage III; (4) the TCM grade is an independent predictive value for both surgical response and surgical cure, while the Friedman stage was found to be predictive only for surgical response; and (5) the response rate and cure rate of the 18 patients with TCM scores of ≥ 22 were only 16.7% and 0%, while such data of patients with Friedman stage III were 53.9% and 17.6%, suggesting that the TCM scoring system is also more efficient in selecting patients who are unsuitable for this operation.
Our results suggest that it would be possible to provide layer-layer progressive preoperative evaluations to different OSAS patients in clinical practice: if a patient could be selected as a proper candidate by a simple method, such as Friedman staging system, that patient would not require any further examination and could undergo surgery. If the result of the simple evaluation would not be so satisfactory, the patient could undergo a complex evaluation with more preoperative tests, such as a TCM scoring system basing on physical examination, PSG, and CT of the upper airway. Similarly, if the complex evaluation in some patients still suggested unsatisfactory predictions, such as those found in patients with TCM scores of 14–22 in this study, more valuable tests should be performed for a further evaluation, such as drug-induced sleep endoscopy or even complex methods for defining the physiological traits of this disease.23–25
The clinical implication of such layer-layer progressive evaluations could be highly cost-effective for both patients and surgeons, as this would lower medical costs due to no longer needing further tests in some patients. Taking drug-induced sleep endoscopy as an example, this test could evaluate the upper airway in a setting closely mimicking natural sleep and could provide more accurate information regarding potential collapse site(s) and responsible collapse structure(s), such as the velum, lateral oropharyngeal wall, tongue base, or epiglottis.26 It could then be a more valuable reference than routine awake tests in patient selection for upper airway surgery.27,28 However, this test costs more and often requires operating room time. We think that the preoperative tests should differ and should be individualized. Accurate but high-cost dynamic tests like drug-induced sleep endoscopy could only be suggested for patients for whom it is not possible to predict satisfactory surgical outcomes via routine tests.
There were also some other results worth discussing: first, in addition to anatomical factors, the TCM scoring system also included a physiological factor, CT90. This variable can reflect several physiological abnormalities that cannot directly be changed by surgery, such as unstable respiratory control, decreased respiration chemoreceptor sensitivities, and impaired upper airway muscular tension.29,30 Anatomical and physiological abnormalities are both involved in the pathogenesis of OSAS.29,31 Patients with great physiological abnormalities may not achieve complete alleviation of this disease from surgery.29 Second, in addition to TCM grade, AHI is also independently predictive of surgical cure, suggesting that the treatment effects brought by velopharyngeal operation are limited. Compared with patients with mild to moderate OSAS, those with severe disease are not likely to be cured with such treatment. Third, CT90, tonsil size, and MH were shown to be important values for predicting outcomes of velopharyngeal surgery in several previous studies.7–9,11,14,20,32,33 The results of our studies proved that combining multiple predictors could be useful in improving predictive efficacy.
This study has a few limitations: first, this study has a relatively small sample size. Second, patients were enrolled from 3 hospitals; although the preoperative tests and surgical procedures were all done according to the same criteria, there may still be differences. Third, the follow-up times in this study were relatively short (3–6 months). Finally, we did not incorporate data on subjective symptoms into analysis, such the Epworth Sleepiness Scale, sleep quality, or a life quality scale. Such information is also important for evaluating surgical outcomes, and it may not totally be represented by PSG outcomes.
To sum up, the TCM scoring system is more efficient in selecting candidates suitable for velopharyngeal surgery compared with the Friedman staging system. The main reason may be better utilization of patients’ preoperative information, especially the inclusion of physiological factors.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CI
confidence interval
- CT
computed tomography
- CT90
percentage of sleep time with oxygen saturation below 90%
- MH
vertical distance between the lower margin of the mandible and the lower margin of the hyoid
- OSAS
obstructive sleep apnea syndrome
- PSG
polysomnography
- ROC
receiver operating characteristic
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. Work for this study was performed at Beijing Tsinghua Changgung Hospital, Peking University First Hospital, and Beijing Friendship Hospital. This study was funded by Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (XMLX201703). The authors report no conflicts of interest.
REFERENCES
- 1. Kezirian EJ , Maselli J , Vittinghoff E , Goldberg AN , Auerbach AD . Obstructive sleep apnea surgery practice patterns in the United States: 2000 to 2006 . Otolaryngol Head Neck Surg. 2010. ; 143 ( 3 ): 441 – 447 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stuck BA , Ravesloot MJL , Eschenhagen T , de Vet HCW , Sommer JU . Uvulopalatopharyngoplasty with or without tonsillectomy in the treatment of adult obstructive sleep apnea—a systematic review . Sleep Med. 2018. ; 50 : 152 – 165 . [DOI] [PubMed] [Google Scholar]
- 3. Aurora RN , Casey KR , Kristo D , et al . American Academy of Sleep Medicine . Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults . Sleep. 2010. ; 33 ( 10 ): 1408 – 1413 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rosvall BR , Chin CJ . Is uvulopalatopharyngoplasty effective in obstructive sleep apnea? Laryngoscope. 2017. ; 127 ( 10 ): 2201 – 2202 . [DOI] [PubMed] [Google Scholar]
- 5. Sher AE , Schechtman KB , Piccirillo JF . The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome . Sleep. 1996. ; 19 ( 2 ): 156 – 177 . [DOI] [PubMed] [Google Scholar]
- 6. Holty JE , Guilleminault C . Surgical options for the treatment of obstructive sleep apnea . Med Clin North Am. 2010. ; 94 ( 3 ): 479 – 515 . [DOI] [PubMed] [Google Scholar]
- 7. Friedman M , Ibrahim H , Bass L . Clinical staging for sleep-disordered breathing . Otolaryngol Head Neck Surg. 2002. ; 127 ( 1 ): 13 – 21 . [DOI] [PubMed] [Google Scholar]
- 8. Choi JH , Cho SH , Kim SN , Suh JD , Cho JH . Predicting outcomes after uvulopalatopharyngoplasty for adult obstructive sleep apnea: a meta-analysis . Otolaryngol Head Neck Surg. 2016. ; 155 ( 6 ): 904 – 913 . [DOI] [PubMed] [Google Scholar]
- 9. Millman RP , Carlisle CC , Rosenberg C , Kahn D , McRae R , Kramer NR . Simple predictors of uvulopalatopharyngoplasty outcome in the treatment of obstructive sleep apnea . Chest. 2000. ; 118 ( 4 ): 1025 – 1030 . [DOI] [PubMed] [Google Scholar]
- 10. Shie DY , Tsou YA , Tai CJ , Tsai MH . Impact of obesity on uvulopalatopharyngoplasty success in patients with severe obstructive sleep apnea: a retrospective single-center study in Taiwan . Acta Otolaryngol. 2013. ; 133 ( 3 ): 261 – 269 . [DOI] [PubMed] [Google Scholar]
- 11. He M , Yin G , Zhan S , et al . Long-term efficacy of uvulopalatopharyngoplasty among adult patients with obstructive sleep apnea: a systematic review and meta-analysis . Otolaryngol Head Neck Surg. 2019. ; 161 ( 3 ): 401 – 411 . [DOI] [PubMed] [Google Scholar]
- 12. Zhang J , Li Y , Cao X , et al . The combination of anatomy and physiology in predicting the outcomes of velopharyngeal surgery . Laryngoscope. 2014. ; 124 ( 7 ): 1718 – 1723 . [DOI] [PubMed] [Google Scholar]
- 13. Zhang J , Ye J , Xian J , Wang J , Dong J . Upper airway anatomical changes after velopharyngeal surgery in obstructive sleep apnea patients with small tonsils . Otolaryngol Head Neck Surg. 2013. ; 149 ( 2 ): 335 – 341 . [DOI] [PubMed] [Google Scholar]
- 14. Friedman M , Ibrahim H , Joseph NJ . Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment . Laryngoscope. 2004. ; 114 ( 3 ): 454 – 459 . [DOI] [PubMed] [Google Scholar]
- 15. Han D , Ye J , Lin Z , Wang J , Wang J , Zhang Y . Revised uvulopalatopharyngoplasty with uvula preservation and its clinical study . ORL J Otorhinolaryngol Relat Spec. 2005. ; 67 ( 4 ): 213 – 219 . [DOI] [PubMed] [Google Scholar]
- 16. Ye JY , Yi B , Liu JM , et al . Combination of transpalatal advancement pharyngoplasty and H-uvulopalatopharyngoplasty for obstructive sleep apnea . Oper Tech Otolaryngol—Head Neck Surg. 2009. ; 20 ( 2 ): 152 – 158 . [PubMed] [Google Scholar]
- 17. Berry RB , Budhiraja R , Gottlieb DJ , et al . Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine . Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events . J Clin Sleep Med. 2012. ; 8 ( 5 ): 597 – 619 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brodsky L . Modern assessment of tonsils and adenoids . Pediatr Clin North Am. 1989. ; 36 ( 6 ): 1551 – 1569 . [DOI] [PubMed] [Google Scholar]
- 19. Kezirian EJ , Weaver EM , Criswell MA , de Vries N , Woodson BT , Piccirillo JF . Reporting results of obstructive sleep apnea syndrome surgery trials . Otolaryngol Head Neck Surg. 2011. ; 144 ( 4 ): 496 – 499 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xiong YP , Yi HL , Yin SK , et al . Predictors of surgical outcomes of uvulopalatopharyngoplasty for obstructive sleep apnea hypopnea syndrome . Otolaryngol Head Neck Surg. 2011. ; 145 ( 6 ): 1049 – 1054 . [DOI] [PubMed] [Google Scholar]
- 21. Li HY , Wang PC , Lee LA , Chen NH , Fang TJ . Prediction of uvulopalatopharyngoplasty outcome: anatomy-based staging system versus severity-based staging system . Sleep. 2006. ; 29 ( 12 ): 1537 – 1541 . [DOI] [PubMed] [Google Scholar]
- 22. Friedman M , Vidyasagar R , Bliznikas D , Joseph N . Does severity of obstructive sleep apnea/hypopnea syndrome predict uvulopalatopharyngoplasty outcome? Laryngoscope. 2005. ; 115 ( 12 ): 2109 – 2113 . [DOI] [PubMed] [Google Scholar]
- 23. Zhu M , Gong S , Ye J , Wang Y , Bai X , Peng KA . Predicting outcome of velopharyngeal surgery in drug-induced sleep endoscopy by traction velum . Eur Arch Otorhinolaryngol. 2021. ; 278 ( 3 ): 821 – 826 . [DOI] [PubMed] [Google Scholar]
- 24. Zhang P , Ye J , Pan C , Sun N , Kang D . The role of obstruction length and height in predicting outcome of velopharyngeal surgery . Otolaryngol Head Neck Surg. 2015. ; 153 ( 1 ): 144 – 149 . [DOI] [PubMed] [Google Scholar]
- 25. Owens RL , Edwards BA , Eckert DJ , et al . An integrative model of physiological traits can be used to predict obstructive sleep apnea and response to non positive airway pressure therapy . Sleep. 2015. ; 38 ( 6 ): 961 – 970 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Amos JM , Durr ML , Nardone HC , Baldassari CM , Duggins A , Ishman SL . Systematic review of drug-induced sleep endoscopy scoring systems . Otolaryngol Head Neck Surg. 2018. ; 158 ( 2 ): 240 – 248 . [DOI] [PubMed] [Google Scholar]
- 27. Lin HY , Lin YC , Hsu YS , et al . Comparison of findings between clinical examinations and drug-induced sleep endoscopy in patients with obstructive sleep apnea syndrome . Int J Environ Res Public Health. 2020. ; 17 ( 17 ): 6041 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stanley JJ . Drug-induced sleep endoscopy: techniques, interpretation and implications . Curr Opin Pulm Med. 2020. ; 26 ( 6 ): 623 – 628 . [DOI] [PubMed] [Google Scholar]
- 29. Eckert DJ , White DP , Jordan AS , Malhotra A , Wellman A . Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets . Am J Respir Crit Care Med. 2013. ; 188 ( 8 ): 996 – 1004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wellman A , Edwards BA , Sands SA , et al . A simplified method for determining phenotypic traits in patients with obstructive sleep apnea . J Appl Physiol (1985). 2013. ; 114 ( 7 ): 911 – 922 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jordan AS , McSharry DG , Malhotra A . Adult obstructive sleep apnoea . Lancet. 2014. ; 383 ( 9918 ): 736 – 747 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yin G , He M , Cao X , et al . Five-year objective and subjective outcomes of velopharyngeal surgery for patients with obstructive sleep apnea . Otolaryngol Head Neck Surg. 2020. ; 162 ( 1 ): 148 – 154 . [DOI] [PubMed] [Google Scholar]
- 33. Woodson BT , Conley SF . Prediction of uvulopalatopharyngoplasty response using cephalometric radiographs . Am J Otolaryngol. 1997. ; 18 ( 3 ): 179 – 184 . [DOI] [PubMed] [Google Scholar]