Abstract
Introduction
This systematic review investigated the efficacy of a meal sequence, the carbohydrate-later meal pattern (CL), on type 2 diabetes mellitus (T2DM).
Research design and methods
We searched the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, WHO International Clinical Trials Registry Platform, and ClinicalTrials.gov until April 2020 to perform meta‐analyses using random-effects models. Primary outcomes were hemoglobin A1c (HbA1c) and quality of life. Secondary outcomes were plasma concentrations of glucose, insulin and incretin 120 min after a meal, and any adverse outcomes. The revised Cochrane risk-of-bias tool and Grading of Recommendations, Assessment, Development, and Evaluation approach were used to assess the quality of individual studies and the body of evidence, respectively. The present study was registered in the UMIN Clinical Trials Registry.
Results
We included 230 participants in eight trials, including both trials that examined long-term changes (more than 2 months and less than 2 years) and short-term changes (in 2-hour postprandial values). CL resulted in a slight to no difference in HbA1c (mean difference (MD), −0.21% in the intervention group; 95% CI −0.44% to+0.03%), plasma glucose (MD,+4.94 mg/dL; 95% CI −8.34 mg/dL to +18.22 mg/dL), plasma insulin (MD, −3.63 μIU/mL; 95% CI −11.88 μIU/mL to +4.61 μIU/mL), plasma GLP-1 (MD, +0.43 pmol/L; 95% CI −0.69 pmol/L to +1.56 pmol/L), and plasma GIP (MD, −2.02 pmol/L; 95% CI −12.34 pmol/L to +8.31 pmol/L). All of these outcomes were of low-certainty evidence or very low-certainty evidence. None of the trials evaluated quality of life or adverse events.
Conclusions
There was no evidence for the potential efficacy of recommending CL beyond standard dietary advice on T2DM.
Trial registration number
UMIN000039979.
Keywords: diabetes mellitus, type 2, diet
Significance of this study.
What is already known about this subject?
The number of patients with diabetes worldwide is expected to increase and those with type 2 diabetes always initially require lifestyle guidance, including diet and exercise.
Current dietary strategies to attenuate postprandial glucose are based on total energy intake and consumption and the amount or type of carbohydrate consumed despite the difficulties associated with adhering to a healthy diet by some patients.
A meal sequence, the carbohydrate-later meal pattern, was focused on as an easy and effective strategy to reduce postprandial glucose excursions in previous trials.
What are the new findings?
We conducted a systematic review and meta-analysis in order to confirm whether the meal sequence, the carbohydrate-later meal pattern, would affect outcomes of diabetes.
Carbohydrate-later meal patterns may result in a slight to no difference in hemoglobin A1c after 2 months to 2 years. Similarly, carbohydrate-later meal patterns may result in a slight to no difference in plasma glucose, insulin, and incretin 120 min after meals.
There was no evidence for the potential efficacy of recommending carbohydrate-later meal patterns beyond standard dietary advice on type 2 diabetes.
How might these results change the focus of research or clinical practice?
These results suggest that the meal sequence will not be strongly prioritized in clinical practice.
Further large scale, well-designed randomized controlled trials of the meal sequence are warranted.
Introduction
Postprandial hyperglycemia is an independent risk factor for type 2 diabetes mellitus, and the control of postprandial glucose excursions has been suggested to reduce the progression of atherosclerosis and cardiovascular events.1 2 The number of patients with diabetes worldwide is expected to increase to 366 million by 2030,3 and those with type 2 diabetes always initially require lifestyle guidance, including diet and exercise. Current dietary strategies to attenuate postprandial glucose are based on total energy intake and consumption and the amount or type of carbohydrate consumed despite the difficulties associated with adhering to a healthy diet by some patients.4
A meal sequence, the carbohydrate-later meal pattern, was focused on as an easy and effective strategy to reduce postprandial glucose excursions in previous trials.5 This pattern means the order of eating within a meal. In other words, before consuming starchy or high glycemic index (GI) foods, eat carbohydrate-free or low GI foods first, such as proteins, fats, and vegetables. However, there have not yet been any systematic reviews that have examined the efficacy of this pattern, the meal sequence, to improve diabetes in randomized controlled trials (RCTs). Therefore, the meal sequence has never been presented in the diabetes guidelines as solid evidence.6–8
A systematic review of the effects of changing the order in which carbohydrates are consumed on improvements in diabetes is very important for establishing whether this strategy may be used in future clinical practice. Therefore, the purpose of the present study was to systematically review evidence in order to confirm whether the meal sequence, the carbohydrate-later meal pattern, would improve diabetes.
Materials and methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Online supplemental table S1 shows the PRISMA 2009 checklist. Detailed methods are described in UMIN000039979 in the UMIN Clinical Trials Registry (https://upload.umin.ac.jp/cgi-bin/ctr_e/ctr_view.cgi?recptno=R000045533).
bmjdrc-2021-002534supp001.pdf (928KB, pdf)
Eligibility criteria for included studies
We included all RCTs that examined the efficacy of meal sequence in patients with type 2 diabetes or pre-diabetic conditions. The details were as follows.
We included all RCTs irrespective of the publication status, including individual and crossover RCTs. All other non-RCTs were excluded. Studies in any language from any country and any follow-up periods were accepted for screening. Men and women of all ages were included. Studies on healthy subjects, patients with type 1 diabetes, and patients after surgery (eg, postgastrectomy patients) were excluded. Carbohydrate-later meal patterns were used as intervention criteria. Carbohydrates included rice, bread, and noodles; precarbohydrate meals included all sources of protein, fat, vitamins and minerals, and dietary fiber. If interventions other than the meal sequence were used, we only included cases in which the meal sequence alone was assessable (eg, typical diet instructions+meal sequence instructions vs typical diet instructions). The duration of the intervention was one or more meals, and the time of the meal was any time. However, supplements were excluded. The control group was defined as the carbohydrate-first meal pattern or a random meal sequence (no intervention for the meal sequence) and included typical dietary instructions. As criteria for inclusion, energy intakes by the intervention and control groups were similar, and any RCTs that required only the intervention group to eat something before the consumption of a carbohydrate were excluded.
Outcome measures
The following primary outcomes were measured:
Hemoglobin A1c (HbA1c) (national glycohemoglobin standardization program (NGSP)) follow-up.9
Physical component summary score (short form (SF) 36, SF12, and SF8).
Mental component summary score (SF36, SF12, and SF8).
Secondary outcomes were as follows:
Plasma glucose 120 min after a meal.
Plasma insulin 120 min after a meal.10
Plasma incretin (glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP)) 120 min after a meal.
All adverse events.
In accordance with current guidelines,6–8 the present study used HbA1c, which reflects long-term blood glucose levels, as the primary outcome and postprandial blood glucose levels as the secondary outcome.
Search methods for study identification
Electronic searches
To identify relevant trials, we searched the following electronic databases on 15 April 2020:
The Cochrane Central Register of Controlled Trials (CENTRAL).
MEDLINE via Ovid.
Embase via ProQuest.
See online supplemental method S1 for details on search strategies.
Searches of other resources
We also searched the following registries to identify completed but unpublished trials and investigate reporting bias.
WHO International Clinical Trials Platform Search Portal (ICTRP).
ClinicalTrials.gov.
See online supplemental method S1 for details on search strategies.
The references of both extracted studies and international guidelines6 8 were also checked. We contacted authors if the extracted studies lacked the necessary information.
Data collection and analysis
Study selection
Two independent reviewers screened the titles and abstracts identified in the search. All of the extracts from the two reviewers were subjected to a full-text review. They then decided independently whether to include the full text in the review. When it was an abstract-only study or when it was unclear whether it met the criteria for review, we contacted the original authors. Disagreements between the two reviewers were discussed and resolved among themselves. We discussed with a third reviewer where necessary. We followed a predefined protocol to screen abstracts and full texts and used predefined criteria in the registered protocol. One lead author (YO) checked all included studies and the exclusion criteria for all records subjected to the full-text screening procedure. Therefore, the decision did not systematically differ.
Data extraction and management
Data extraction in the present study was performed independently by two reviewers. Disagreements between the two reviewers were discussed and resolved among themselves. We discussed with a third reviewer where necessary and contacted the original author. If data for extraction were not available in the original paper, we contacted the authors to obtain them. Regarding the data extraction form, we used a prechecked form with 10 randomly selected studies. Please refer to online supplemental method S1 for details on extracted information.
Assessment of the risk of bias of included studies
Two reviewers conducted the study independently using the Risk of Bias 2 tool. Disagreements between the two reviewers were discussed and resolved by themselves. We discussed with a third reviewer where necessary.11
Measures of the treatment effect
Regarding continuous outcomes (HbA1c, plasma glucose, plasma insulin, and plasma incretin), the mean difference (MD) with 95% CI was shown.
HbA1c measured in Japan Diabetes Society (JDS) units was converted to NGSP units using the following formula: NGSP (%)=1.02*JDS (%)+0.25.12 GLP-1 and GIP measured in pg/mL were converted to pmol/L using the following formulas: GLP-1 (pmol/L)=GLP-1 (pg/mL) /3297.6×1000; GIP (pmol/L)=GIP (pg/mL) /4983.5×1000.13
All MDs and 95% CIs used absolute changes not relative changes.
Dealing with analyses
To integrate the means and SD of continuous variables, we followed the methods of the Cochrane handbook.14 Units of randomization: regarding crossover tests, we asked the authors for the first half of the data, used only the first half if available or used reported values if not available, and reflected them in the Risk of Bias 2. Multiple identical outcome assessments: the main outcome was HbA1c concentrations after the intervention, and if there were multiple endpoint measurements, the endpoint was 120 min later for the short-term intervention (assessment of one meal) and the longest follow-up period for the long-term intervention.
Dealing with missing values
Dropouts
Following the recommendations of The Cochrane Handbook,14 imputation was not performed. We conducted a meta-analysis of the data presented by the original authors.
Missing values
We contacted the original authors.
Missing statistics
If only SEs were reported, a SD was obtained from the SE of a mean by multiplying by the square root of the sample size: SD=SE * square root of N.14
Assessment of heterogeneity
We initially evaluated heterogeneity visually using a forest plot. We then calculated I2 values (I2 values of 0%–40%: may not be important; 30%–60%: may represent moderate heterogeneity; 50%–90%: may be substantial). The Cochrane χ2 test (Q-test) was performed for I2 values, and a p value <0.10 was considered to be significant.
Assessment of publication bias
We searched the Clinical Trials registry site (ClinicalTrials.gov, ICTRP) for studies that were completed but not yet published. The funnel plot assessed publication bias for the primary outcome (online supplemental figure S1).
Data synthesis
We pooled data using a random-effects model. The DerSimonian and Laird method was used in the random-effects meta-analysis.15 All analyses were conducted using Review Manager software (RevMan V.5.4.1; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Subgroup analysis and investigation of heterogeneity
We aimed to identify possible causes of heterogeneity. The following prespecified subgroup analyses of the primary outcomes were planned: (1) types of carbohydrate (rice or other than rice); (2) types of foods containing a small amount of carbohydrates with low GI (vegetables or other than vegetables); (3) duration of the follow-up (long- or short-term); and (4) meal types (breakfast, lunch, or dinner).
Sensitivity analysis
The following prespecified sensitivity analyses of primary outcomes were planned:
(1) repeating the analysis using a fixed-effects model instead of random-effects model; and (2) excluding studies with ‘the analysis including imputed data’.
Summary of findings table
The main results of our review are presented in the summary of findings table, which includes an overall grading of evidence related to each of the main outcomes using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach,16 based on the recommendations of the Cochrane Handbook.14
Registration and the differences between the protocol and review
We registered the protocol in UMIN000039979 in the UMIN Clinical Trials Registry (https://upload.umin.ac.jp/cgi-bin/ctr_e/ctr_view.cgi?recptno=R000045533).
The following is a list of items that were planned in the protocol but were ultimately not implemented (not possible to implement or did not need to be implemented).
Because the number of included trials was smaller than expected, we decided not to account for the duration of intervention as an inclusion criterion because of no strong justification, currently evaluating both short-term postprandial effects and effects of advice for a habitual diet. For the same reason, we did not perform stratified analysis by gender and did not use funnel plots for inference of publication or small-study bias though we generated them (online supplemental figure S1).
Results
Search results
After removing duplicates, we identified 3924 records during the search conducted in April 2020 (figure 1). We included 13 trials in the qualitative synthesis and detected one unpublished trial and four completed trials without clear data on outcomes. Ultimately, 230 participants in eight trials were included in the quantitative synthesis. These trials included both trials that examined long-term changes after 2 months or longer and trials that examined short-term changes in 2-hour postprandial values.
Figure 1.
PRISMA flow diagram. CENTRAL, Cochrane Central Register of Controlled Trials; Embase, Excerpta Medica Database; ICTRP, International Clinical Trials Platform Search Portal; MEDLINE, Medical Literature Analysis and Retrieval System On-Line; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1 and online supplemental table S2 summarize the published studies included in the qualitative synthesis.
Table 1.
Summary of published studies including a qualitative synthesis
| Source | Country | Men/women, n | Age, years | BMI, kg/m2 | Diabetes history, years | Follow-up period | Analysis |
| Bae et al (2018)23 | Korea | 5/10 | Mean 62.9 (SD 4.3) | Mean 24.8 (SD 3.5) | Mean 13.8 (SD 6.7) | 180 min | ITT |
| Imai et al (2010)24 | Japan | 7/8 | Mean 61.7 (SD 11.6) | Mean 24.7 (SD 4.3) | Mean 5.3 (SD 8.8) | 120 min | ITT |
| Imai et al (2011)25 | Japan | 48/53 | Mean 63.4 (SD 11.7) | Mean 23.4 (SD 4.1) | Mean 7.3 (SD 8.3) | 2 years | ITT |
| Imai et al (2012)*26 | Japan | – (Total 17) |
Mean 65.7 (SD 9.6) | – | – | 72 hours (3 days) | ITT |
| Imai et al (2013)27 | Japan | 6/13 | Mean 65.5 (SD 9.4) | Mean 22.5 (SD 3.1) | Mean 16.4 (SD 10.2) | 72 hours (3 days) | ITT |
| Imai et al (2014)*28 | Japan | – (Total 13) |
Mean 69.1 (SD 6.7) | – | – | ITT | |
| Kuwata et al (2016)*22 | Japan | 9/3 | Mean 59.7 (SD 9.7) | Mean 25.3 (SD 4.1) | Mean 3.6 (SD 5.5) | 240 min | ITT |
| Shukla et al (2017)29 | USA | 7/9 | Mean 57.7 (SD 7.6) | Mean 32.8 (SD 3.3) | Mean 3.8 (SD 2.4) | 180 min | ITT |
| Shukla et al (2018)*30 | USA | 7/9 | Mean 57.7 (SD 7.6) | Mean 32.8 (SD 3.3) | Mean 3.8 (SD 2.4) | 180 min | ITT |
| Shukla et al (2019)31 | USA | 4/11 | Mean 52.4 (SD 3.4) | Mean 34.2 (SD 1.1) | NA | 180 min | ITT |
| Trico et al (2016)32 | Italy | 13/7 | Mean 64.5 (SD 21.4) | Mean 30.6 (SD 3.5) | Less than 5 | 8 weeks | PP |
| Yabe et al (2019)33 | Japan | – (Total 29) |
Mean 49.5 (SD 5.9) | Mean 25.9 (SD 2.1) | NA | 22–26 weeks (6 months) | PP |
*Studies included in the qualitative synthesis.
BMI, body mass index; ITT, intention-to-treat; PP, per-protocol.
Primary outcomes
HbA1c
Data from three trials comprising 147 participants that measured HbA1c were pooled in our meta-analysis (table 2, figures 2 and 3A). Carbohydrate-later meal patterns may result in a slight to no difference in HbA1c (MD, 0.21% lower in the intervention group; 95% CI 0.44% lower to 0.03% higher; p=0.09; low-certainty evidence). No significant heterogeneity was indicated (tau2 <0.001; I2=0%) (table 2, figure 3A). As a subgroup analysis, we included rice only as the carbohydrate source; however, no change was observed in HbA1c with the intervention (online supplemental figure S2A). In the sensitivity analysis, although we also calculated a fixed effect model instead of a random effects model, the results were the same as those for the random effects model (online supplemental figure S2B). Similar results were obtained even when studies using imputed statistics were excluded (online supplemental figure S2C).
Table 2.
Summary of findings
| Outcomes | No. of participants (studies) followed up |
Certainty of the evidence (GRADE) |
Anticipated absolute effects | |
| Risk with the carbohydrate-first meal pattern or random meal sequence | Risk difference with the carbohydrate-later meal pattern§ | |||
| HbA1c concentrations (NGSP) | 147 (3 RCTs) |
⊕⊕ □ □ Low*† |
The mean HbA1c (%) ranged from 6.1% to 7.7% | MD 0.21% lower (0.44 lower to 0.03 higher) |
| Physical component summary score (SF36, SF12, SF8) | NR | |||
| Mental component summary score (SF36, SF12, SF8) | NR | |||
| Plasma glucose 120 min after meals | 143 (6 RCTs) |
⊕⊕ □ □ Low*† |
Mean plasma glucose (mg/dL) 120 min after all meals ranging from 97.1 to 281.5 mg/dL | MD 4.94 mg/dL higher (8.34 lower to 18.22 higher) |
| Plasma insulin 120 min after meals | 136 (5 RCTs) |
⊕⊕ □ □ Very low*†‡ |
Mean plasma insulin (μIU/mL) 120 min after meals ranging from 6.6 to 94.5 μIU/mL | MD 3.63 μIU/mL lower (11.88 lower to 4.61 higher) |
| Plasma GLP-1 120 min after meals | 76 (3 RCTs) |
⊕⊕ □ □ Low*† |
Mean plasma GLP-1 (pmol/L) 120 min after meals ranging from 3.2 to 22.3 pmol/L | MD 0.43 μIU/mL higher (0.69 lower to 1.56 higher) |
| Plasma GIP 120 min after meals | 44 (2 RCTs) |
⊕⊕ □ □ Low*† |
Mean plasma GLP-1 (pmol/L) 120 min after meals ranging from 24.1 to 76.5 pmol/L | MD 2.02 μIU/mL lower (12.34 lower to 8.31 higher) |
| All adverse events | NR | |||
GRADE Working Group grades of evidence.
High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is markedly different. Low certainty: our confidence in the effect estimate is limited: the true effect may be markedly different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be markedly different from the estimate of the effect.
*Downgraded due to the risk of bias.
†The sample size was small. The sample size did not meet the criteria of the optimal information size (OIS) (400). OIS was 400 if alpha D0:05, beta D0:2, delta D0:2.
‡The I2 statistic was higher than 60%, showing great heterogeneity and the direction of the effect was different.
§The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
GIP, glucose-dependent insulinotropic polypeptide; GLP-1, glucagon-like peptide-1; GRADE, Grading of Recommendations Assessment, Development and Evaluation; HbA1c, hemoglobin A1c; MD, mean difference; NGSP, national glycohemoglobin standardization program; NR, not reported; RCTs, randomized controlled trials; SF, short form.
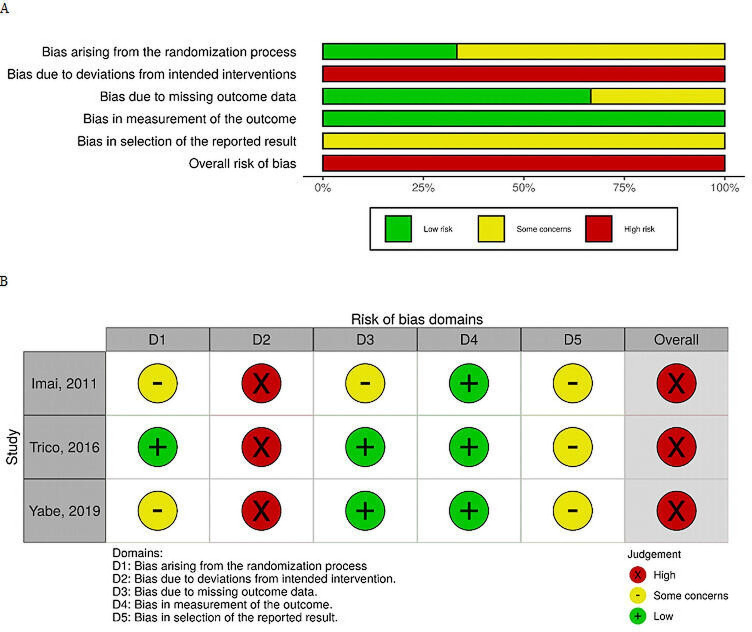
Figure 2.
(A) Risk of bias graph for HbA1c. (B) Risk of bias summary for HbA1c. (A) Review of author judgements on the risk for each bias item presented as percentages across trials. (B) Review of author judgements on the risk for each bias item in the trials. HbA1c, hemoglobin A1c.
Figure 3.
Forest plot of comparisons. GIP, glucose-dependent insulinotropic polypeptide; GLP-1, glucagon-like peptide-1; HbA1c, hemoglobin A1c; IV, inverse variance; NGSP, national glycohemoglobin standardization program.
Quality of life
We searched for quality of life indicator outcomes, specifically the physical and mental component summary scores based on the 12-item medical outcomes study short form health survey (SF-12), SF-36, or SF-8 but were unable to find a single outcome.
Secondary outcomes
Plasma glucose
Data from six trials that measured plasma glucose 120 min after meals in 143 participants were pooled for the meta-analysis (table 2, figure 3B, online supplemental figure S3). Carbohydrate-later meal patterns may result in a slight to no difference in plasma glucose (MD, 4.94 mg/dL higher in the intervention group; 95% CI, 8.34 mg/dL lower to 18.22 mg/dL higher; p=0.47; low-certainty evidence). No significant heterogeneity was indicated (tau2=1.35; I2=0%) (table 2, figure 3B). Subgroup analyses were conducted by lunch and dinner. We also performed stratified analyses by a short-term intervention (120 min after a meal) and the carbohydrate source of rice only or non-rice, but none of which showed significant changes in blood glucose levels due to the intervention (online supplemental figure S2D–H).
Plasma insulin
Data from five trials that measured plasma insulin after 120 min of meals in 136 participants were pooled for the meta-analysis (table 2, figure 3C, online supplemental figure S4). All trials measured blood insulin levels in μIU/mL. Evidence for the effects of carbohydrate-later meal patterns on plasma insulin was uncertain (MD, 3.63 μIU/mL lower in the intervention group; 95% CI 11.88 μIU/mL lower to 4.61 μIU/mL higher; p=0.39; very low-certainty evidence). Significant heterogeneity was observed (tau2=38.90; I2=68%) (table 2, figure 3C). As a subgroup analysis, we only examined the short-term intervention (120 min after the meal) and rice only or non-rice as the carbohydrate source, none of which resulted in a significant insulin change with the intervention (online supplemental figure S2I–K).
Plasma incretin
Data from three trials that measured plasma concentrations of GLP-1 and GIP 120 min after meals in 120 participants (table 2, figure 3D, E, online supplemental figure S5). Carbohydrate-later meal patterns may result in a slight to no difference in plasma GLP-1 (MD, 0.43 mg/dL higher in the intervention group; 95% CI 0.69 mg/dL lower to 1.56 mg/dL higher; p=0.45; low-certainty evidence). Carbohydrate-later meal patterns may result in a slight to no difference in plasma GIP (MD, 2.02 mg/dL lower in the intervention group; 95% CI 12.34 mg/dL lower to 8.31 mg/dL higher; p=0.70; low-certainty evidence). None of them indicated significant heterogeneities (tau2 <0.001; I2=0%) (table 2, figure 3D, E).
All adverse events
We searched for any adverse event outcomes through the intervention; however, none of the trials reported this outcome.
Discussion
Regarding primary outcomes, carbohydrate-later meal patterns may result in a slight to no difference in HbA1c after 2 months to 2 years. Similarly, for secondary outcomes, carbohydrate-later meal patterns may result in a slight to no difference in plasma glucose, insulin, and incretin 120 min after meals.
Given the effect size of −0.21% in HbA1c (as an absolute value) over 2 months or longer, the meal sequence may not need to be positively taught in clinical practice. In the current diabetes guidelines, diet and exercise therapy are fundamental for the management of diabetes.6–8 A systematic review of obese patients with type 2 diabetes reported that a weight loss of 5% or more resulted in reduction of HbA1c by 0.91% after 1 year,17 and total energy intake and appropriate BMI were emphasized as the most important factors. Although there is no clear evidence on nutrient intake proportions, a RCT reported that a low-carbohydrate diet resulted in reduction of HbA1c by 0.6% after 6 months.18 Regarding lipids, a previous systematic review reported that a diet with increased monounsaturated fatty acids produced reduction of HbA1c by 0.21% after 6 months compared with a diet that decreased it.19 Furthermore, a systematic review on exercise therapy reported that exercise for more than 12 weeks lowered HbA1c by 0.67%.20 The reduction of HbA1c by 0.21% due to the meal sequence in the present study was not as large as those by diet and exercise in these studies. In addition, a previous systematic review found that HbA1c lowering <0.3% had no effect, whereas HbA1c lowering ≥0.5% had a −13% (95% CI −20% to −5%) effect on major cardiovascular events.21 Therefore, a reduction of HbA1c by 0.21% is not considered to be a value with a certain effect and, thus, the meal sequence may not need to be intensively taught in clinical practice.
As a clinical implication, it may be better to prioritize conventional diet and exercise therapy. The clinical utility of the meal sequence remains unclear. In actual clinical practice, there are time and cost restrictions on dietary guidance. In the current dietary guidelines for diabetes care, dietitians and other healthcare providers initially prioritize the energy balance for patients with type 2 diabetes, particularly obese patients.8 In other words, they provide guidance to reduce total energy intake and increase physical activity. They then recommend an exercise strategy based on aerobic exercise, resistance exercise, or a combination. If more time is available or in consideration of other diseases, such as dyslipidemia, hypertension, and renal disease, a change in nutrient intake proportions and food intake may also be advised. The results of the present study suggest that the efficacy of the meal sequence on diabetes do not outweigh the importance of a known total energy balance (including energy restrictions, appropriate BMI, and exercise regimens), nutrient intake, and food content. Instructions by the meal sequence are not harmful. However, in consideration of the time and costs associated with counseling patients with diabetes, it may be more beneficial to prioritize conventional diet and exercise.
Since the results of the present study had a low certainty of evidence, they need to be interpreted with caution. Due to the very small number of RCTs on the meal sequence, the present results showed a low certainty of evidence. Although many RCTs have examined the efficacy of consuming some foods or nutrients (including supplements) before meals, they were excluded from this systematic review because of differences in total energy intake between the intervention and control groups, which made rigorous comparisons difficult. In order to increase the reliability of results, it is of the greatest importance to initially increase the sample size of trials examining the efficacy of the meal sequence on type 2 diabetes. Studies using the continuous glucose monitoring may be mandatory to decipher whether or not meal sequencing could be useful.22 It may also be possible to conduct higher quality RCTs in the future by rigorous randomization, the blinding of researchers, and the publication of protocols. Since the present results were based on patients with type 2 diabetes only, the generalizability of the results obtained to include healthy subjects and patients with type 1 diabetes is not possible. Similarly, since five out of the eight RCTs included in the present study were conducted on Asians, it remains unclear whether the same results may be obtained from a Western population, and this aspect also made it difficult to generalize the present results.
The limitations of the present study were as follows. First, we planned to include quality of life as a primary outcome because a balanced evaluation of interventions requires an analysis of both benefits and adverse effects; however, they were not reported by any of the RCTs included. Unlike trials in which medication was the intervention, trials in which dietary guidance was the intervention were more likely to lack these aspects. In long-term RCTs, a decrease in quality of life (eg, decreased social relationships and depressive tendencies) due to the inability to freely take in meals is expected. Therefore, quality of life needs to be evaluated in the design of future RCTs. Second, it is possible that underestimation of HbA1c may have occurred due to the inevitable decrease in compliance when looking at long-term effects. In addition, the decrease in compliance due to long-term intervention may have also contributed to the lower certainty of evidence. We could not identify any feeding trials that provided meals to improve compliance. The present study evaluated trials that tested an intervention of providing dietary advice. However, since no meaningful change was observed in plasma glucose at 2 hours in the short term, the order of meals may result in a slight to no difference in diabetes improvement as a whole. Third, there were very few RCTs examining the efficacy of meal sequence on HbA1c, and the wide range of intervention periods in the included articles made interpretation difficult. More importantly, the small number of RCTs produced results that were low certainty for both primary and secondary outcomes. We estimated ‘average’ effects from those limited number of trials. Therefore, some patients with diabetes may possibly gain benefit by carbohydrate-later meal patterns but many others may not. This study has not been able to clarify such a possibility distinct from no effect. Fourth, there were trials whose design was a cross-over RCT and for which data from only the first half or the corresponding t-test results and correlation coefficients needed for the calculations were not available. Incorporating data from the latter part of the study may be affected by carryover effects from the first half. However, we expected this carryover effects to lead to an underestimation of the results.
The strength of the present study was its carefully and rigorously designed screening, extraction, and scoring process based on the Cochrane Handbook.14 The present study is of importance because it is the first systematic review to examine the efficacy of the meal sequence on type 2 diabetes.
In conclusion, there was no evidence for the potential efficacy of recommending carbohydrate-later meal patterns beyond standard dietary advice on type 2 diabetes. These results suggest that the meal sequence will not be strongly prioritized in clinical practice. Further large-scale well-designed RCTs are warranted.
Acknowledgments
I would like to express our deepest gratitude to the Systematic Review Workshop Peer Support Group (SRWS-PSG) for their cooperation in the present study.
Footnotes
Contributors: YO, JW, and YK contributed substantially to the conceptualization, methodology, data analysis, interpretation, and writing of the manuscript; YO and HT were primarily engaged in study identification, study selection, data extraction, and evaluation. YO will be the guarantor of the entire content, will take full responsibility for the study and/or conduct of the study, will have access to the data, and will have control over the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Data to support the results of this study can be obtained from the original study. However, some values that were not published in the original paper can be obtained from the corresponding author upon reasonable request. In such cases, permission must be obtained from the corresponding author of the original paper at the same time.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Although this study involved human subjects, ethical approval was not obtained again for the present study because it had been approved in the individual original studies included in the systematic review. Participants in each study confirmed that they had given informed consent before participating in the study.
References
- 1.Cavalot F, Petrelli A, Traversa M, et al. Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga diabetes study. J Clin Endocrinol Metab 2006;91:813–9. 10.1210/jc.2005-1005 [DOI] [PubMed] [Google Scholar]
- 2.Leiter LA, Ceriello A, Davidson JA, et al. Postprandial glucose regulation: new data and new implications. Clin Ther 2005;27 Suppl B:27 Suppl B:S42–56. 10.1016/j.clinthera.2005.11.020 [DOI] [PubMed] [Google Scholar]
- 3.Wild S, Roglic G, Green A, et al. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–53. 10.2337/diacare.27.5.1047 [DOI] [PubMed] [Google Scholar]
- 4.Norris SL, Nichols PJ, Caspersen CJ, et al. Increasing diabetes self-management education in community settings. A systematic review. Am J Prev Med 2002;22:39–66. 10.1016/S0749-3797(02)00424-5 [DOI] [PubMed] [Google Scholar]
- 5.Nesti L, Mengozzi A, Tricò D. Impact of nutrient type and sequence on glucose tolerance: physiological insights and therapeutic implications. Front Endocrinol 2019;10:144. 10.3389/fendo.2019.00144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2020;41:255–323. 10.1093/eurheartj/ehz486 [DOI] [PubMed] [Google Scholar]
- 7.Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. Diabetol Int 2020;11:165–223. 10.1007/s13340-020-00439-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association . Standards of Medical Care in Diabetes-2020 Abridged for Primary Care Providers. Clin Diabetes 2020;38:10–38. 10.2337/cd20-as01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mottalib A, Salsberg V, Mohd-Yusof B-N, et al. Effects of nutrition therapy on HbA1c and cardiovascular disease risk factors in overweight and obese patients with type 2 diabetes. Nutr J 2018;17:42. 10.1186/s12937-018-0351-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Association AD. Postprandial blood glucose. Diabetes Care 2001;24:775–8. 10.2337/diacare.24.4.775 [DOI] [PubMed] [Google Scholar]
- 11.Sterne JAC, Savović J, Page MJ, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 12.Kashiwagi A, Kasuga M, Araki E, et al. International clinical harmonization of glycated hemoglobin in Japan: from Japan diabetes Society to national Glycohemoglobin standardization program values. J Diabetes Investig 2012;3:39–40. 10.1111/j.2040-1124.2012.00207.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyachi A, Kondo F, Kurita M, et al. Microbial degradation of linear peptides by strain B-9 of Sphingosinicella and its application in peptide quantification using liquid chromatography-mass spectrometry. J Biosci Bioeng 2015;119:724–8. 10.1016/j.jbiosc.2014.10.029 [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Thomas J. Cochrane Handbook for systematic reviews of interventions. 2 edn, 2019. [Google Scholar]
- 15.DerSimonian R, Laird N. Meta-Analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 16.Guyatt G, Oxman AD, Akl EA, et al. Grade guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. 10.1016/j.jclinepi.2010.04.026 [DOI] [PubMed] [Google Scholar]
- 17.Franz MJ, Boucher JL, Rutten-Ramos S, et al. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet 2015;115:1447–63. 10.1016/j.jand.2015.02.031 [DOI] [PubMed] [Google Scholar]
- 18.Yamada Y, Uchida J, Izumi H, et al. A non-calorie-restricted low-carbohydrate diet is effective as an alternative therapy for patients with type 2 diabetes. Intern Med 2014;53:13–19. 10.2169/internalmedicine.53.0861 [DOI] [PubMed] [Google Scholar]
- 19.Schwingshackl L, Strasser B, Hoffmann G. Effects of monounsaturated fatty acids on glycaemic control in patients with abnormal glucose metabolism: a systematic review and meta-analysis. Ann Nutr Metab 2011;58:290–6. 10.1159/000331214 [DOI] [PubMed] [Google Scholar]
- 20.Umpierre D, Ribeiro PAB, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA 2011;305:1790–9. 10.1001/jama.2011.576 [DOI] [PubMed] [Google Scholar]
- 21.Giugliano D, Chiodini P, Maiorino MI, et al. Cardiovascular outcome trials and major cardiovascular events: does glucose matter? A systematic review with meta-analysis. J Endocrinol Invest 2019;42:1165–9. 10.1007/s40618-019-01047-0 [DOI] [PubMed] [Google Scholar]
- 22.Kuwata H, Iwasaki M, Shimizu S, et al. Meal sequence and glucose excursion, gastric emptying and incretin secretion in type 2 diabetes: a randomised, controlled crossover, exploratory trial. Diabetologia 2016;59:453–61. 10.1007/s00125-015-3841-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bae JH, Kim LK, Min SH, et al. Postprandial glucose-lowering effect of premeal consumption of protein-enriched, dietary fiber-fortified bar in individuals with type 2 diabetes mellitus or normal glucose tolerance. J Diabetes Investig 2018;9:1110–8. 10.1111/jdi.12831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imai S, Matsuda M, Fujimoto S. Crossover Study of the Effect of "Vegetables Before Carbohydrates" on Reducing Postprandial Glucose and Insulin in Japanese Subjects with Type 2 Diabetes Mellitus. J Jpn Diabetes Soc 2010;53:112–5. [Google Scholar]
- 25.Imai S, Matsuda M, Hasegawa G, et al. A simple meal plan of 'eating vegetables before carbohydrate' was more effective for achieving glycemic control than an exchange-based meal plan in Japanese patients with type 2 diabetes. Asia Pac J Clin Nutr 2011;20:161–8. [PubMed] [Google Scholar]
- 26.Imai S, Fukui M, Ozasa N, et al. Eating vegetables before carbohydrates for test meals improves postprandial glucose excursions assessed by continuous glucose monitoring system both in patients with type 2 diabetes and in subjects with normal glucose tolerance. Diabetes 2012;1797:A70. [Google Scholar]
- 27.Imai S, Fukui M, Ozasa N, et al. Eating vegetables before carbohydrates improves postprandial glucose excursions. Diabet Med 2013;30:370–2. 10.1111/dme.12073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imai S, Fukui M, Ozasa N, et al. Glucose spikes of eating vegetables before carbohydrates with snacks at mid-afternoon are lower than that of eating carbohydrates before vegetables without snacks. Diabetologia 2014;57:S314. [Google Scholar]
- 29.Shukla AP, Andono J, Touhamy SH, et al. Carbohydrate-last meal pattern lowers postprandial glucose and insulin excursions in type 2 diabetes. BMJ Open Diabetes Res Care 2017;5:10.1136/bmjdrc-2017-000440 10.1136/bmjdrc-2017-000440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shukla AP, Mauer E, Igel LI, et al. Effect of food order on ghrelin suppression. Diabetes Care 2018;41:10.2337/dc17-2244:e76–7. 10.2337/dc17-2244 [DOI] [PubMed] [Google Scholar]
- 31.Shukla AP, Dickison M, Coughlin N, et al. The impact of food order on postprandial glycaemic excursions in prediabetes. Diabetes Obes Metab 2019;21:377–81. 10.1111/dom.13503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tricò D, Filice E, Trifirò S, et al. Manipulating the sequence of food ingestion improves glycemic control in type 2 diabetic patients under free-living conditions. Nutr Diabetes 2016;6:e226. 10.1038/nutd.2016.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yabe D, Kuwata H, Fujiwara Y, et al. Dietary instructions focusing on meal-sequence and nutritional balance for prediabetes subjects: an exploratory, cluster-randomized, prospective, open-label, clinical trial. J Diabetes Complications 2019;33:107450. 10.1016/j.jdiacomp.2019.107450 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2021-002534supp001.pdf (928KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data to support the results of this study can be obtained from the original study. However, some values that were not published in the original paper can be obtained from the corresponding author upon reasonable request. In such cases, permission must be obtained from the corresponding author of the original paper at the same time.