Abstract
Coccidioidomycosis is a disease found in the southwestern United States and caused by inhalation of arthroconidia of Coccidioides immitis and posadasii. Although the disease is most commonly asymptomatic or respiratory, it has a propensity to disseminate to any tissue in the body with the most common being skin, bone, joints, and central nervous system. This case demonstrates the dissemination of coccidioidomycosis to several foci along with a rare form of parenchymal dissemination with an unusual neuroradiological finding.
Keywords: coccidioidomycosis, valley fever, dissemination, fungal infection, meningitis, soft tissue infection
Introduction
Coccidioidomycosis (CM) refers to the disease caused by the dimorphic fungi Coccidioides immitis and posadasii and is endemic to California, Arizona, Northern Mexico, and Central and South America. Infection occurs from the inhalation of arthroconidia aerosolized from the soil. About 97% of reported cases are located in Arizona and California where C immitis is the dominant pathogen. Although the numbers vary from year to year, there is a roughly 3-fold increase from 2006 to 2019 as per California Department of Public Health.1-3
Approximately 60% of all cases are asymptomatic. Of the 40% of symptomatic cases, the vast majority are pulmonary infections. These are most often influenza-like illnesses or resemble of community-acquired pneumonia. Approximately 11% of cases disseminate to virtually every part of the body outside the lung. 4 The rate of extrapulmonary dissemination is quite low in patients with Caucasian ancestry, but with a significant increase in incidence for persons of Filipino or African ancestry. Frequency of dissemination may be as high as 30% to 50% of infections for immunosuppressed patients. When dissemination occurs, it most commonly involves skin, soft tissue, joints and bones as well as the central nervous system (CNS). The most common CNS infection is meningitis. On extremely rare occasions, Coccidioides has also been found to cause intraparenchymal brain disease.3-6
Case Presentation
A 27-year-old Latinx man who was in his usual state of health until 2 months prior to admission when he developed cough and fatigue. He was seen at another institution and was diagnosed with right lower lobe pneumonia and treated with a combination of azithromycin and amoxicillin.
Symptoms persisted unabated, and 4 days prior to admission, he was seen at the emergency department of a second outside facility with continued respiratory complaints. At that time, he complained of fever, rigors, night sweats, nausea, vomiting, anorexia, weight loss, photophobia, and headaches. He noted the appearance of persistent cutaneous lesions to the right lower lip and temporal scalp for 3 weeks. The emergency physician at the outside institution suspected cutaneous CM. Initial laboratory examination revealed an absolute eosinophil count of 900/mm3. Enzyme-linked immunoassay (EIA) of the serum revealed positive immunoglobulin M (IgM) and immunoglobulin G (IgG) Coccidioides antibodies. The patient was referred to our institution for further care.
The patient presented to our institution with above issues and additional complaints of “lower back pain.” Physical examination demonstrated a 2 cm eruption lesion on the right lower lip and 1 cm eruption lesion on the central frontal head. Neurological examination was normal. Noncontrast computed tomography (CT) of the brain was unremarkable. Lumbar puncture and analysis of the cerebrospinal fluid (CSF) revealed an opening pressure of 270 mm H2O and white blood cell count of 520 with lymphocytes of 53%, neutrophils of 13%, and eosinophils of 20%. The glucose was 22 mg/dL and protein was 99 mg/dL. Coccidioides antibody analysis of the CSF showed immunodiffusion (ID) IgG positive and complement fixation (CF) of 1:8. Coccidioidal serology (serum) demonstrated ID IgM, ID IgG positive, and CF of 1:256. A diagnosis of coccidioidal meningitis was made and the patient was placed on 1200 mg fluconazole daily.
Plastic surgery was performed on the cutaneous skin lesions along the right lower lip and right temporal scalp. Histopathology demonstrated Coccidioides spherules with endosporulation.
The patient was discharged and followed up at the Valley Fever Institute. The patient returned 2 months after discharge complaining of right knee and buttock pain as well as short-term memory loss. Physical examination showed marked warmth and tenderness of the right buttock and sacroiliac joint.
The CT scan of the abdomen and pelvis with contrast demonstrated a large multiloculated fluid collection in the gluteus maximus and iliopsoas with extension and involvement of the right sacroiliac joint (Figure 1). The patient subsequently underwent image-guided drainage with pigtail catheter placement of his right gluteal abscess. Fungal culture of the abscess fluid grew C immitis.
Figure 1.

CT scan demonstrating large, multiloculated gluteal abscess.
Abbreviation: CT, computed tomography.
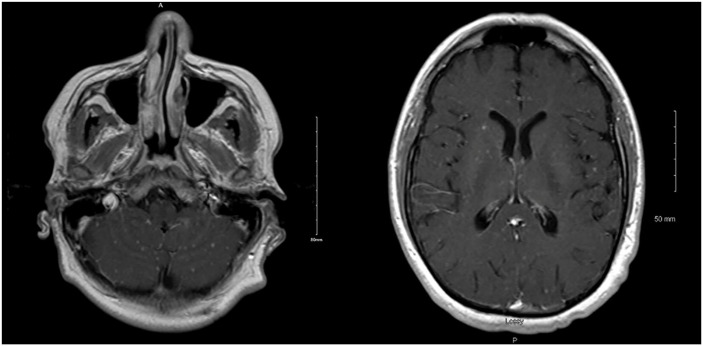
Magnetic resonance imaging (MRI) of brain with and without contrast showed slight meningeal thickening with increased enhancement. Also noted were numerous 1 to 2 mm enhancing foci in the brain parenchyma resembling shotgun pallets (Figure 2). This unique finding was hypothesized to be cerebral parenchymal coccidioidal dissemination.
Figure 2.
T1 MRI postcontrast showing numerous scattered enhancing nodules of intraparenchymal cocci resembling shotgun pallets.
Abbreviation: MRI, magnetic resonance imaging.
Due to the severity and extent of his disease, he was additionally placed on liposomal amphotericin B, 5 mg/kg, infusion with a daily regimen for 14 days. He was then transitioned to a triweekly schedule and extended to a total of 18 weeks. Because of concerns for a poor response to fluconazole, he was transitioned to isavuconazonium 372 mg daily. Follow-up MRI of his brain showed complete resolution of intraparenchymal lesions.
Four years post initial presentation, the patient is still regularly seen at the Valley Fever Institute. His treatment was changed from isavuconazonium to itraconazole due to issues with coverage and cost. His condition remains relatively stable. His CF titers of serum and CSF have decreased to 1:4 (Figures 3 and 4). The duration of his treatment is set to be lifelong.
Figure 3.
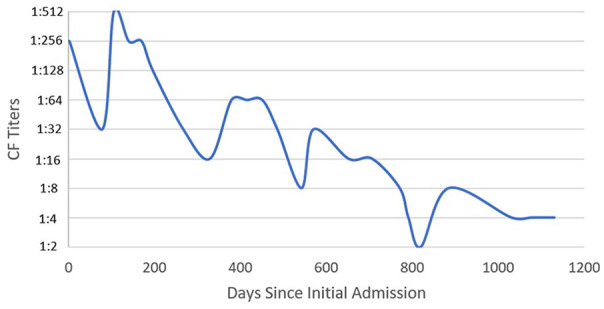
Patient’s serum CF titers over the treatment course.
Abbreviation: CF, complement fixation.
Figure 4.
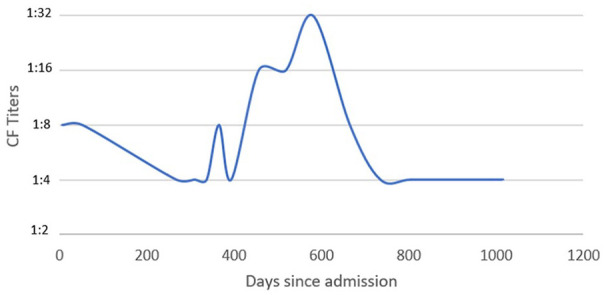
Patient’s CSF complement fixation titers over the course of treatment.
Abbreviation: CSF, cerebrospinal fluid.
Discussion
Disseminated Coccidioides by convention is the infection that is not confined to the pulmonary space. Meningeal, osteoarticular, and cutaneous are the most common foci of dissemination. There have been reports of dissemination to virtually every part of the body. 3 In this case, the patient demonstrated extensive hematogenous spread with soft tissue, osseous, and CNS dissemination.
Meningitis is the most severe form of extrapulmonary CM. Untreated meningitis is universally fatal. 7 The most common neuroradiological findings are meningeal enhancement, hydrocephalus, and spinal arachnoiditis. 3 The first intraparenchymal brain lesion was reported by Jacobson in 1928 as a 4-mm lesion in a 31-year-old Filipino man found during autopsy. There have been multiple reports of intraparenchymal lesions since, with the majority being singular granulomatous lesions.8-10
Neuroradiological imaging of our patient demonstrated the typical leptomeningeal enhancements with a unique radiological pattern of numerous scattered foci of intraparenchymal dissemination. Given the unique nature of this finding, we cannot report for certain it is coccidioidal dissemination without a brain biopsy. Post antifungal treatment, resolution in the neuroradiological imaging strongly suggests coccidioidal dissemination. This patient’s CNS findings further emphasize the importance of atypical presentations of coccidioidal dissemination. Therein, we report what is presumed to be a unique and unusual finding in CNS dissemination.
Footnotes
Authors’ Note: This case was presented at the American Federation of Medical Research’s Western Conference, Carmel, CA, in January 2019.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Ethical approval to report this case was obtained from the Kern Medical Institutional Review Board.
Informed consent: Informed consent for patient information to be published in this article was obtained.
ORCID iDs: Rupam Sharma  https://orcid.org/0000-0003-3457-4371
https://orcid.org/0000-0003-3457-4371
Arash Heidari  https://orcid.org/0000-0003-1091-348X
https://orcid.org/0000-0003-1091-348X
References
- 1. Galgiani JN, Ampel NM, Blair JE, et al. 2016 Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the treatment of coccidioidomycosis. Clin Infect Dis. 2016;63(6):e112-e146. doi: 10.1093/cid/ciw360. [DOI] [PubMed] [Google Scholar]
- 2. Sondermeyer Cooksey GL, Nguyen A, Vugia D, et al. Regional analysis of coccidioidomycosis incidence—California, 2000–2018. MMWR Morb Mortal Wkly Rep. 2020;69(48):1817-1821. doi: 10.15585/mmwr.mm6948a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Johnson RH, Sharma R, Kuran R, et al. Coccidioidomycosis: a review. J Investig Med. 2021;69(2):316-323. doi: 10.1136/jim-2020-001655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carey A, Gorris ME, Chiller T, Jackson B, Beadles W, Webb BJ. Epidemiology, clinical features, and outcomes of coccidioidomycosis, Utah, 2006–2015. Emerg Infect Dis. 2021;27(9):2269-2277. doi: 10.3201/eid2709.210751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heidari A, Gholam S, Johnson RH. Three cases of brain intraparenchymal coccidioidomycosis. Open Forum Infect Dis. 2016;3(suppl_1):1606. doi: 10.1093/ofid/ofw172.1306. [DOI] [Google Scholar]
- 6. Stevens DA. Coccidioidomycosis. N Engl J Med. 1995;332(16):1077-1082. doi: 10.1056/NEJM199504203321607. [DOI] [PubMed] [Google Scholar]
- 7. Vincent T, Galgiani JN, Huppert M, Salkin D. The natural history of coccidioidal meningitis: VA-Armed Forces cooperative studies, 1955-1958. Clin Infect Dis. 1993;16(2):247-254. doi: 10.1093/clind/16.2.247. [DOI] [PubMed] [Google Scholar]
- 8. Malo J, Luraschi-Monjagatta C, Wolk DM, Thompson R, Hage CA, Knox KS. Update on the diagnosis of pulmonary coccidioidomycosis. Ann Am Thorac Soc. 2014;11(2):243-253. doi: 10.1513/AnnalsATS.201308-286FR. [DOI] [PubMed] [Google Scholar]
- 9. Banuelos AF, Williams PL, Johnson RH, et al. Central nervous system abscesses due to coccidioides species. Clin Infect Dis. 1996;22(2):240-250. doi: 10.1093/clinids/22.2.240. [DOI] [PubMed] [Google Scholar]
- 10. McGahan J, Graves D, Palmer P, Stadalnik RC, Dublin AB. Classic and contemporary imaging of coccidioidomycosis. AJR Am J Roentgenol. 1981;136(2):393-404. doi: 10.2214/ajr.136.2.393. [DOI] [PubMed] [Google Scholar]