Abstract
Background:
The incidence of anterior cruciate ligament (ACL) injuries is commonly reported as an annual incidence rate. There is relatively little information about the seasonal aspects of these injuries. The aim of the current study was to analyze the distribution of ACL injuries during the season in nonprofessional soccer, handball, and basketball based on a retrospective analysis of a hospital-based registry.
Hypothesis:
ACL injuries in soccer, handball, and basketball were more common within the first 2 months of the season in comparison with the rest of the year.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
Injury occurrence during the calendar year was divided into 6 periods of 2 months, with segment 1 (S1) representing the first 2 months of the season. For soccer, S1 corresponded to September and October. The season started 1 month later for handball and basketball, so S1 represented October and November. Chi-square tests were used to analyze the distribution of ACL injuries among segments according to gender, age, sports, and injury mechanism (contact/noncontact).
Results:
A total of 371 ACL injuries were included (soccer, 258, handball, 56, basketball, 57). Overall, the distribution of ACL injuries was not uniform across the segments (P < 0.01). Almost one-third of the ACL injuries occurred in S1 (n = 104; 28%). Significant differences could be observed according to sports (P < 0.01). There were fewer ACL injuries in S2 for soccer compared with basketball (P < 0.05). In S5, there were significantly more ACL injuries in soccer compared with handball and basketball (P < 0.05).
Conclusion:
A high occurrence of ACL injuries was reported immediately within the first 2 months of the season in nonprofessional soccer, handball, and basketball sports.
Clinical Relevance:
These findings indicate that ACL injury prevention programs should be started in the preseason period to allow for gradual increases of load.
Keywords: anterior cruciate ligament, injury, epidemiology, prevention
Although physical activity has many well-known benefits, it also involves a significant risk of injury. In team ball sports, knee injuries to the anterior cruciate ligament (ACL) are of particular importance.12,18 They compromise the integrity of the long-term knee function in athletes, as well as their ability to return to sport. Only 55% of athletes return to preinjury level of competitive sport after ACL reconstruction, 2 so these injuries have often been associated with the end of a team ball sport career. In addition, ACL injuries increase the risk of developing early knee osteoarthritis 17 leading to extensive medical care in the long term. Besides the financial burden, the health-related quality of life (HRQoL) is significantly reduced in the ACL-injured patients compared with age-matched norms. 7 To date, ACL injuries thus continue to represent a significant burden for both the injured athlete and the society.
Because of the burden of ACL injuries, many efforts have been directed toward ACL injury prevention. Although prevention programs significantly reduce the incidence of noncontact ACL injuries, 19 the overall ACL injury rate has continued to increase over the past decade, mostly in young athletes. 20 The annual incidence of ACL injuries is commonly reported in the literature, but there is little information about the seasonal aspects of these injuries. In professional soccer, the highest rate of ACL injury was detected during the preseason period from July to August. The injury rate then declined from August to November. 13 However, the seasonal incidence of ACL injuries in nonprofessional soccer, handball, and basketball remains unknown. Such findings may provide valuable information as to when ACL injury prevention programs should be started.
The aim of the current study was to analyze the distribution of ACL injuries during the season in team ball sports, based on a retrospective analysis of a hospital-based registry. It was hypothesized that ACL injuries in soccer, handball, and basketball were more common within the first 2 months of the season in comparison with the rest of the year.
Methods
Patients with an ACL injury were selected from a hospital registry by one of the authors. The diagnosis of the ACL rupture was confirmed through clinical examination and magnetic resonance imaging as well as arthroscopy where applicable. Patients were included if they had a sport injury that had occurred in soccer, handball, or basketball between September 2011 and October 2018 and were involved in a nonprofessional organized competitive sport before the injury. They were excluded if the date of injury was uncertain (ie, only the year of injury was known or several knee sprains had occurred and may have led to the ACL injury) or if they were over 35 years of age at the time of the injury or were not involved in competitive sport (soccer, handball, or basketball) before the injury. Patients over 35 years of age were excluded, as they were less likely to have been involved in a competitive pivot sport before the injury. 14
To analyze the seasonal aspect of ACL injuries within these ball team sports, the calendar year was divided into 6 segments of 2 months (segments 1 to 6) (Table 1). Segment 1 (S1) represented the first 2 months of the sport season. S1 corresponded to September/October for soccer and October/November for handball and basketball.
Table 1.
Definition of segments through the calendar year according to sport a
| January | February | March | April | May | June | July | August | September | October | November | December | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Soccer | S3 In season |
S4 In season |
S5 Off-season |
S6 Preseason |
S1
In season |
S2 In season |
|||||||
| Handball Basketball |
S2 In season |
S3 In season |
S4 In season |
S5 Off-season |
S6 Preseason |
S1
In season |
S2 In season |
||||||
Segment 1 (S1) represents the first 2 months of the sport season.
Further information extracted from the registry included the following: gender (male/female); age (<21 or 21-35 years); sport at injury (soccer, handball, and basketball); injury mechanism (contact vs noncontact); previous ACL reconstruction (yes/no); and contralateral ACL injury (yes/no). A contact injury was defined as any kind of physical contact by another player whether it was directly to the knee or another body part prior to the onset of the injury. Conversely, a noncontact injury represented an ACL injury without any physical contact between players.
All patients gave their written informed consent to participate in the study. The study protocol was approved by the national ethics committee for research (No. 201101/05).
Statistical Analysis
Statistical analyses were performed using Version 25.0 of the SPSS software.
Chi-square tests determined whether the distribution of ACL injuries differed between segments according to gender, age categories, sport, injury mechanism, history of previous ACL reconstruction, and contralateral ACL injuries. Each expected cell count was checked to determine whether it was greater than 5. If more than 20% of cells revealed lower values, the exact significance was calculated to verify test validity. To counteract the problem of multiple comparisons, Bonferroni correction was used. Cramer V was reported as an effect size measurement. Significance was set at P < 0.05 for all analyses. All data are given as means ± SDs.
Results
A total of 1103 ACL injuries were extracted from the hospital registry from September 2011 to October 2018 of which 905 were sports injuries. In all, 512 injuries occurred during soccer, handball, or basketball, of which 462 had a precise date of injury (month and year of the injury confirmed). A total of 371 (men: n = 282, 24 ± 5 years of age at the injury, 179 ± 7 cm, 77 ± 11 kg; women: n = 89, 23 ± 5 years of age at the injury, 168 ± 7 cm, 65 ± 8 kg) injuries in athletes younger than 35 years were included: 258 ACL injuries occurred in soccer, 56 in handball, and 57 in basketball. In total, 86 patients (23%) had suffered a previous ACL injury (35 had a graft rupture, 46 had a contralateral ACL injury, and 5 had both).
The overall distribution of ACL injuries was not uniform across the seasonal segments (P < 0.01). S1 was the segment in which most ACL injuries occurred (n = 104; 28%). The distribution in the other segments was similar and as follows: S2: n = 48, 13%; S3: n = 60, 16%; S4: n = 59, 16%; S5: n = 45, 12%; S6, n = 55, 15%.
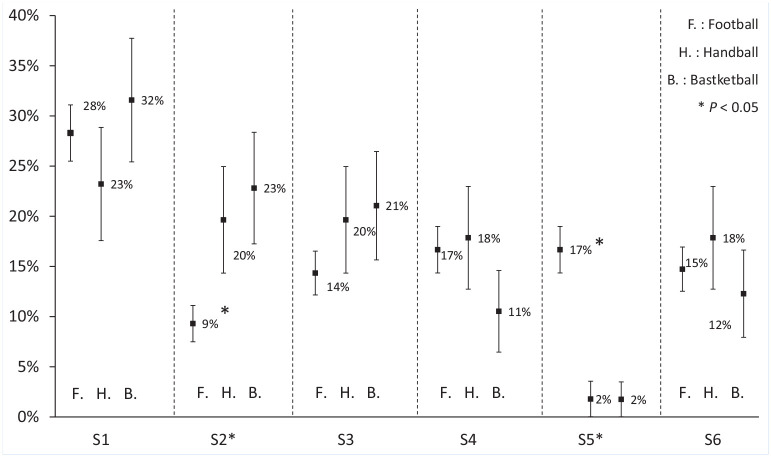
No difference in injury distribution could be found between genders, age categories, injury mechanisms, athletes with or without a previous ACL reconstruction, or between patients with or without a contralateral ACL injury (Table 2). A significant difference in the distribution of ACL injuries was found between sports (Figure 1; P < 0.01). In particular, there were fewer ACL injuries in S2 for soccer (9% of all of all ACL injuries in soccer occurred in S2) compared with basketball (23% of all ACL injuries in basketball occurred in S2) (P < 0.05). In S5, there were significantly more ACL injuries in soccer (17% of all ACL injuries in soccer occurred in S5) compared with handball (2% of all ACL injuries in handball occurred in S5) and basketball (2% of all ACL injuries in basketball occurred in S5) (P < 0.05).
Table 2.
Distribution of anterior cruciate ligament (ACL) injuries among segments according to gender, age category, injury mechanism, previous ACL reconstruction, and contralateral ACL injurya
| Gender | Age Category | Injury Mechanism | Previous ACL Reconstruction | Contralateral ACL Injury | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <21 y | 21-35 y | Noncontact | Contact | No | Yes | No | Yes | |
| P | n.s. | n.s. | n.s. | n.s. | n.s | |||||
| Cramer V | 0.15 | 0.13 | 0.15 | 0.01 | 0.16 | |||||
| Total (n) | 282 | 89 | 134 | 237 | 240 | 131 | 331 | 40 | 320 | 51 |
| S1 | 77 27% [22-33] |
27 30%[21-40] |
45 34% [26-42] |
59 25% [19-30] |
62 26% [20-31] |
42 32% [24-40] |
93 28% [23-33] |
11 27.5% [14-41] |
93 29% [24-34] |
11 21.5% [10-33] |
| S2 | 31 11% [7-14] |
18 20% [12-29] |
17 13% [7-18] |
31 13% [9-17] |
37 16% [11-20] |
11 8% [4-13] |
41 12% [9-16] |
7 17.5% [6-29] |
35 11% [8-14] |
13 25% [14-37] |
| S3 | 46 16% [12-21] |
14 16% [8-23] |
24 18% [11-24] |
36 15% [11-20] |
34 14% [10-19] |
26 20%[13-27] |
51 15.5% [12-19] |
9 22.5% [10-35] |
51 16% [12-20] |
9 17.5% [7-28] |
| S4 | 46 16% [12-21] |
13 15% [7-22] |
19 14% [8-20] |
40 17% [12-22] |
36 15% [10-20] |
23 18% [11-24] |
53 16% [12-20] |
6 15% [4-26] |
53 17% [12-21] |
6 12% [3-21] |
| S5 | 38 13% [9-17] |
7 8% [2-13] |
15 11% [6-17] |
30 13% [8-17] |
32 13% [9-18] |
13 10% [5-15] |
42 13% [9-16] |
3 7.5% [–1-16] |
39 12% [9-16] |
6 12% [3-21] |
| S6 | 45 16% [12-20] |
10 11% [5-18] |
14 10% [5-16] |
41 17% [12-22] |
39 16% [7-18] |
16 12% [7-18] |
51 15.5% [12-19] |
4 10% [1-19] |
49 15% [11-19] |
6 12% [3-21] |
n, % [95% CI]. n.s., not significant.
Figure 1.
Distribution of anterior cruciate ligament injuries among segments according to sport. *Differs significantly from other columns P < 0.05.
Discussion
The main finding of this study was that almost one-third of all ACL injuries in team ball sports (28%) occurred within the first 2 months of the season. There were relatively fewer ACL injuries in soccer (9%) compared with handball (20%) and basketball (23%) in S2. The opposite could be observed in S5 where there were more ACL injuries in soccer than in handball and basketball. The distribution of ACL injuries was thus not uniform across the season and differed between sports.
Our findings are in general agreement with the literature. Anderson et al 1 reported that the ACL injury incidence was higher in the early part of the regular season compared with the preseason, the rest of the season, or the postseason in National Collegiate Athletic Association (NCAA) athletes in basketball, lacrosse, and soccer. However, the authors could not find any significant season segment effect for basketball or soccer. In the analysis of 148 consecutive ACL injuries across 10 seasons of professional Italian football, 4 previous authors could observe a peak of ACL injuries in September-October, representing the first 2 months of the season in the present study (S1), and a second peak from March to May (similar to S5 in the present study). Slater et al 16 observed the trends of first and recurrent ACL injuries in collegiate (2009-2010 through 2016-2017) and high school athletes (2011-2012 through 2013-2014) in American high schools and NCAA schools. 16 In total, 373 noncontact ACL injuries were recorded, of which 23% occurred in preseason, 74% during the regular season, and 3% in the off-season. An additional finding of their study was that the odds of a recurrent ACL injury compared with a first injury during preseason were 2.8 times that of regular season. 16 In other words, athletes with a previous ACL injury were at more risk of sustaining a second ACL injury during the preseason compared with first injuries. In the present study, the distribution of ACL injuries did not differ between patients with or without a previous ACL reconstruction, or between patients with or without a contralateral ACL injury. A larger cohort may be needed before being able to draw any conclusion. However, the overall incidence of second ACL tears in our cohort of 23% does agree with the second injury rate in athletes younger than 25 years. 21
Overall, there is a significant risk of injury during more intense training periods or during phases in which acute training loads change. 8 The high incidence of ACL injuries in the first 2 months of the season as observed in the present study may thus be due to a combination of sudden spikes in training and/or match load and a lack of physical fitness. 8
A significant difference in the distribution of ACL injuries was found between sports. An explanation for this finding is that the soccer season is much more variable and dependent on outdoor conditions in comparison with indoor sports. For example, there were relatively fewer ACL injuries in soccer (9%) compared with handball (20%) and basketball (23%) in S2. The low number of ACL injuries in S2 in soccer (November and December) may thus reflect bad meteorological conditions over the seasons studied within this study. In contrast, a significantly higher incidence rate was found in S5 in soccer compared with basketball and handball. Cumulative fatigue over the course of multiple training sessions or matches may have heightened athletes’ risk of injury. 6 Managing players’ loading and minimizing exposure to sustained elevated loads thus appears important for injury prevention. The findings of the current study support the idea that an ACL injury prevention program should be initiated in the preseason and continued over the season. According to the position statement of the National Athletic Training Association, 11 such programs should be multicomponent and be performed at least 2 to 3 times per week throughout the preseason and in-season to ensure sufficient time to modify athletes’ neuromuscular risks.
Extrinsic factors may have contributed to the high number of ACL injuries at the beginning of the season. A correlation between the head coach’s leadership style and the incidence of severe injuries and players’ availability has been shown in professional soccer. 5 Other factors such as weather and type of floor may also play a role in the incidence of ACL injuries, as they may disturb the interactions between the footwear and the playing surface. High evaporation rates in the month before the match were associated with increased ACL injuries in the Australian Football League. 10 Olsen et al 9 showed that the risk of ACL injury was 2.35 times higher on synthetic indoor floors in elite Norwegian handball female athletes compared with injuries on wooden floors.
Several limitations need to be acknowledged. The main limitation of the present study was that data were based on the retrospective analysis of a hospital registry. The risk of retrospective surveillance is that fewer injuries may be recorded compared with a prospective injury registration. 3 The incidence thus may not be representative of all ACL injuries occurring in major team ball sports during the season, the data could not be cross-checked with injury data from the relevant sports organizations, and the athlete exposure could not be determined. Information on when the injury exactly occurred in the sports season calendar and whether the injury occurred during a match or training and/or player position were not available. Future studies will need to consider these important aspects to improve the understanding of the problem. The distinction between contact and noncontact injuries may be arbitrary, as these data were based on patient reports and not actual video coverage. Because of these limitations, we emphasize that the results of this study should be interpreted with caution. Further studies are needed to determine the role of gender, age, injury mechanism, and previous injuries on the distribution of ACL injuries during the season. However, in a context where a systematic recording of ACL injuries by sports organizations is still nonexistent or at its very beginnings in many countries, 15 the current retrospective analysis does provide important information pertaining to injury incidence in nonprofessional sports throughout a season. Coaches and practitioners should be aware of the increased number of ACL injuries during the first 2 months of a season and be cautious to implement ACL injury prevention programs during the preseason period.
Conclusion
Hospital registry data suggest a seasonal variability of ACL injuries in nonprofessional team ball sports such as soccer, handball, and basketball. The findings identified a high occurrence of ACL injuries within the first 2 months of a new season, thereby indicating the need for implementation of ACL injury prevention programs during the preseason period.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iD: Romain Seil  https://orcid.org/0000-0001-8806-9384
https://orcid.org/0000-0001-8806-9384
References
- 1. Anderson T, Wasserman EB, Shultz SJ. Anterior cruciate ligament injury risk by season period and competition segment: an analysis of National Collegiate Athletic Association Injury Surveillance Data. J Athl Train. 2019;54:787-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 3. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. 2020;54:372-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Della Villa F, Buckthorpe M, Grassi A, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med. 2020;54:1423-1432. [DOI] [PubMed] [Google Scholar]
- 5. Ekstrand J, Lundqvist D, Lagerbäck L, Vouillamoz M, Papadimitiou N, Karlsson J. Is there a correlation between coaches’ leadership styles and injuries in elite football teams? A study of 36 elite teams in 17 countries. Br J Sports Med. 2018;52:527-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gabbett TJ, Nassis GP, Oetter E, et al. The athlete monitoring cycle: a practical guide to interpreting and applying training monitoring data. Br J Sports Med. 2017;51:1451-1452. [DOI] [PubMed] [Google Scholar]
- 7. Hoogeboom TJ, den Broeder AA, de Bie RA, van den Ende CH. Longitudinal impact of joint pain comorbidity on quality of life and activity levels in knee osteoarthritis: data from the Osteoarthritis Initiative. Rheumatology (Oxford). 2013;52:543-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones CM, Griffiths PC, Mellalieu SD. Training load and fatigue marker associations with injury and illness: a systematic review of longitudinal studies. Sports Med. 2017;47:943-974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Relationship between floor type and risk of ACL injury in team handball. Scand J Med Sci Sports. 2003;13:299-304. [DOI] [PubMed] [Google Scholar]
- 10. Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29:196-200. [DOI] [PubMed] [Google Scholar]
- 11. Padua DA, DiStefano LJ, Hewett TE, et al. National Athletic Trainers’ Association position statement: prevention of anterior cruciate ligament injury. J Athl Train. 2018;53:5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614-621. [DOI] [PubMed] [Google Scholar]
- 13. Schiffner E, Latz D, Grassmann JP, et al. Anterior cruciate ligament ruptures in German elite soccer players: epidemiology, mechanisms, and return to play. Knee. 2018;25:219-225. [DOI] [PubMed] [Google Scholar]
- 14. Seil R, Mouton C, Lion A, Nührenbörger C, Pape D, Theisen D. There is no such thing like a single ACL injury: profiles of ACL-injured patients. Orthop Traumatol Surg Res. 2016;102:105-110. [DOI] [PubMed] [Google Scholar]
- 15. Seil R, Mouton C, Theisen D. How to get a better picture of the ACL injury problem? A call to systematically include conservatively managed patients in ACL registries. Br J Sports Med. 2016;50:771-772. [DOI] [PubMed] [Google Scholar]
- 16. Slater LV, Wasserman EB, Hart JM. Trends in recurrent anterior cruciate ligament injuries differ from new anterior cruciate ligament injuries in college and high school sports: 2009-2010 through 2016-2017. Orthop J Sports Med. 2019;7:2325967119883867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Meer BL, Oei EH, Meuffels DE, et al. Degenerative changes in the knee 2 years after anterior cruciate ligament rupture and related risk factors: a prospective observational follow-up study. Am J Sports Med. 2016;44:1524-1533. [DOI] [PubMed] [Google Scholar]
- 18. Waldén M, Hägglund M, Magnusson H, Ekstrand J. Anterior cruciate ligament injury in elite football: a prospective three-cohort study. Knee Surg Sports Traumatol Arthrosc. 2011;19:11-19. [DOI] [PubMed] [Google Scholar]
- 19. Webster KE, Hewett TE. Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs. J Orthop Res. 2018;36:2696-2708. [DOI] [PubMed] [Google Scholar]
- 20. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 21. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]