Abstract
Background:
Biomechanical knee asymmetry is commonly present after anterior cruciate ligament (ACL) reconstruction. Factors that could assist in identification of asymmetrical biomechanics after ACL reconstruction could help clinicians in making return-to-play decisions. The purpose of this study is to determine factors that may contribute to knee biomechanical asymmetry present after ACL reconstruction.
Hypothesis:
We hypothesized that quadriceps strength and activation and patient-reported function would allow for identification of patients with symmetrical knee biomechanics.
Study Design:
Cross-sectional study.
Level of Evidence:
Level 3.
Methods:
Thirty-one subjects (18 women; time since ACL reconstruction = 284.4 ± 53.6 days) who underwent ACL reconstruction and were to return to activity were recruited. Participants completed bilateral assessments of isokinetic quadriceps strength, quadriceps activation using the superimposed burst technique, and biomechanical function testing during a single-leg forward hop. The International Knee Documentation Committee (IKDC) subjective knee form was also completed. Symmetry values were calculated for each variable. Decision trees were utilized to determine which input factors (quadriceps strength symmetry, quadriceps activation symmetry, IKDC score, age, sex, height, mass, graft type) were able to identify participants who had symmetrical knee flexion angles (KFAs) and extension moments. Angles and moments were considered symmetrical if symmetry values were ≥90%.
Results:
Quadriceps strength and activation symmetry were able to predict whether a patient landed with symmetrical or asymmetrical KFAs, with thresholds of 77.2% strength symmetry and 91.3% activation symmetry being established. Patient-reported function and quadriceps strength were factors that allowed for classification of participants with symmetrical/asymmetrical knee extension moments, with thresholds of 89.1 for the IKDC and 80.0% for quadriceps strength symmetry.
Conclusions:
Quadriceps strength contributed to both models and appears to be a critical factor for achieving symmetrical knee biomechanics. High patient-reported function and quadriceps activation are also important for restoring knee biomechanical symmetry after ACL reconstruction.
Clinical Relevance:
Quadriceps strength and activation and patient-reported function may be able to assist clinicians in identifying ACL patients with symmetrical/asymmetrical knee biomechanics.
Keywords: muscle, biomechanics, knee, quadriceps, strength
Knee biomechanical asymmetries are commonplace after ACL injury and reconstruction.12,26 If left unresolved, the persistence of biomechanical asymmetries may result in decreased functional performance, 11 increased risk for secondary injury, 28 and the development of accelerated knee osteoarthritis (OA). 5 Young athletes with asymmetrical knee flexion excursions, for example, exhibit decreased self-reported function 2 years after ACL reconstruction while patients who display knee extension moment asymmetries are at a 4 times greater risk for secondary ACL injury. 28 Furthermore, long-lasting alterations in knee motion or loading relative to pre-ACL injury status (ie, asymmetries) may promote catabolic processes in knee articular cartilage, resulting in structural decline and early onset of knee OA.3,7 Given the negative repercussions biomechanical asymmetries can have on patients who have undergone ACL reconstruction, it is imperative to better understand factors that may contribute to the development of these abnormal movement strategies so that they can be better targeted with appropriate interventions.
Quadriceps muscle strength and activation are often impaired after ACL reconstruction 19 and may affect the recovery of symmetrical knee joint mechanics. Our prior work has shown that at the time of return to activity after ACL reconstruction, patients who exhibit more symmetrical quadriceps strength and activation also exhibit more symmetrical knee biomechanics during a single-leg forward hop. 26 Similar findings have been noted during gait, where patients 7 months after ACL reconstruction with greater quadriceps strength symmetry exhibited more symmetrical knee flexion angles (KFAs) and moments. 32 However, other research has shown conflicting findings wherein patients 6 months after ACL reconstruction displayed symmetrical knee biomechanics despite exhibiting asymmetrical quadriceps strength. 29 It is plausible that the discrepancy in results could be attributed to differences in study design/testing (ie, participant sex, time of testing, strength assessment used, task performed during biomechanical analysis). Nonetheless, the lack of agreement among previous research underscores the need to clarify the role of quadriceps strength on knee biomechanics after ACL reconstruction. Moreover, it is not currently clear what thresholds of quadriceps strength and activation symmetry are able to identify patients who are more likely to achieve symmetrical knee biomechanical function. Such knowledge would have substantial clinical value to aid in identifying patients who may require extended rehabilitation.
Patient-reported outcome measures are often employed after ACL reconstruction to track patient progress, function, and symptoms during recovery. 2 Furthermore, they have been used to estimate the risk for posttraumatic OA after ACL reconstruction. 24 Poor patient-perceived knee function after ACL reconstruction could be indicative of abnormal knee movement and loading. 9 In fact, previous research has demonstrated that patients after ACL reconstruction with asymmetrical sagittal plane knee biomechanical function had lower patient-reported outcome scores (measured via the Knee Injury and Osteoarthritis Outcome Score). 12 It remains unclear, however, if patient-reported outcomes of knee function could aid in identifying patients who would display symmetrical knee biomechanics during tasks like landing. Furthermore, identifying cutoff values that aid in determining symmetrical biomechanical profiles could help establish clinical guidance for return-to-activity criteria.
The ubiquitous nature of asymmetrical biomechanics after ACL reconstruction and the propensity for these asymmetries to promote deleterious alterations in knee joint health underscore the need to discover factors contributing toward their development. Therefore, this study aimed to determine whether quadriceps strength, activation, and patient-reported outcomes at the time of return to activity would aid in identifying patients who can successfully reestablish sagittal plane knee biomechanical symmetry after ACL reconstruction. We hypothesized that quadriceps strength and self-reported knee function would be the factors predominantly responsible for predicting patients that achieved biomechanical symmetry in the KFA and knee extension moment after ACL reconstruction.
Methods
Participants
Thirty-one subjects who underwent ACL reconstruction and who completed postoperative rehabilitation in our clinic and were cleared to return to activity (eg, competitive and recreational sports) participated in this study (Table 1). Subjects were eligible to participate if they (1) were between 14 and 30 years of age, (2) did not have a previous ACL injury or prior knee surgery, (3) did not have a cardiac demand-type pacemaker, and (4) were not pregnant. All subjects were required to read and sign the informed consent before study participation. Subjects younger than 18 years were required to sign an assent and both parents were required to consent. This study was approved by the University of Michigan Medical School Institutional Review Board.
Table 1.
Demographic and predictor variable information for symmetrical and asymmetrical knee flexion angle groups (mean ± SD)
| Group | Age, y | Height, cm | Mass, kg | Time From ACL Recons-truction to Testing, d | Sex | Concomitant surgery | Graft Type | Surgical Limb Is Dominant Limb a | ACL Limb Single-Leg Hop Distance | KFA Symmetry | Quadriceps Strength Symmetry | CAR Symmetry | IKDC Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symmetrical KFA (N = 11) |
17.6 ± 2.9 | 174.0 ± 2.2 | 70.9 ± 15.8 | 285.0 ± 54.6 | Male = 5; female = 6 | 1 LM repair 3 LM debride 1 MM repair Part LMEX |
2 Ham 1 Quad 8 BPTB |
5 = yes;6 = no | 146.0 ± 33.2 | 97.1 ± 5.0 | 85.1 ± 11.7 | 98.5 ± 5.9 | 89.0 ± 6.7 |
| Asymmetrical KFA (N = 20) |
17.0 ± 2.2 | 170.2 ± 18.43 | 76.7 ± 9.1 | 286.2 ± 56.6 | Male = 8; female = 12 | 6 LM repair 2 MM repair 1 Part LMEX |
3 Ham 1 Quad 16 BPTB |
7 = yes;10 = no 3 = unknown |
131.9 ± 27.4 | 76.2 ± 6.4 | 71.9 ± 16.1 | 96.3 ± 7.6 | 85.6 ± 9.4 |
BPTP, bone-patellar tendon-bone; CAR, central activation ratio; Ham, hamstring; IKDC, International Knee Documentation Committee; KFA, knee flexion angle; LM, lateral meniscus; LMEX, lateral meniscectomy; MM, medial meniscus; Quad, quadriceps.
Dominant limb defined as what leg would be used to kick a ball.
Study Overview
Subjects performed all study-related tests in either 1 or 2 sessions, depending on their availability. If data were collected in a single session, quadriceps strength and activation testing was performed first and motion capture testing was completed last. For subjects electing to do 2 testing sessions, strength and activation was always performed in one session and motion capture in the other. The average time from surgery for the testing sessions is as follows: quadriceps strength and activation (283.32 ± 52.67 days postoperative) and motion capture (285.50 ± 54.51 days postoperative).
Quadriceps Activation
Bilateral quadriceps muscle activation was examined with the superimposed burst (SIB) technique. For this testing, subjects were seated in an isokinetic dynamometer (Biodex Medical Systems) with the knee and hip flexed to 90° and then were secured with straps across the torso, waist, thigh, and shank. Electrodes (Dura-Stick II [7 × 13 cm] Chattanooga Group) were placed over the distal aspect of the vastus medialis and the proximal aspect of the vastus lateralis. Before testing, subjects warmed up with submaximal contractions after which they were instructed to complete a minimum of 3 repetitions of a maximal voluntary isometric knee extension contraction (MVIC) without an applied SIB. Subjects continued to perform MVICs until the examiner noted no increase in torque. Once the MVIC was established, subjects performed 3 MVIC repetitions, but with the application of a supramaximal stimulus (100 pulses/s, 600 μs pulse duration, 10 pulse train, 130 V; Grass S88 Dual Output Square Pulse Stimulator/SIU8T Stimulus Isolation Unit, Grass Technologies) delivered to the quadriceps. The torque signal during testing was sent from the Biodex using a custom-made cable to an A/D board (DAQ model USB-6251 multifunction I/O Device, National Instruments) and was displayed and recorded using a custom-written LabVIEW program (LabVIEW Version 8.5, National Instruments). For SIB trials, the supramaximal stimulus was triggered by our LabVIEW program and was delivered once subjects matched their MVIC knee extension torque output, and then dropped by 1 N·m.15,18,27
Voluntary peak torque and peak torque resulting from the SIB were recorded during the SIB trials and were used to calculate the central activation ratio (CAR). The CAR is calculated by dividing the peak MVIC torque by the peak SIB isometric knee extension torque, and then multiplying by 100. 14
Quadriceps Strength
Subjects performed bilateral isokinetic knee extension strength testing at 60 deg/s on the Biodex with the hip flexed to 90°. Subjects completed a standardized warmup, after which they were instructed to perform 5 repetitions of maximal knee extension/flexion contractions.
Peak torque values were recorded for the 5 isokinetic knee extension repetitions and the peak value for each limb was used to calculate the quadriceps index ([injured limb/noninjured limb] × 100). Limb testing order was randomized before subject arrival.
International Knee Documentation Committee Subjective Knee Evaluation Form
To capture patient-reported knee function, participants were asked to complete the International Knee Documentation Committee (IKDC) form for subjective knee function. The IKDC is a reliable and valid measure of patient-reported function in the ACL population. 33 The IKDC is composed of 18 questions covering 3 different domains: (1) symptoms, (2) sports and daily activities, and (3) function. The IKDC was scored on a 0 to 100 scale with 100 being representative of highest knee function.
Knee Biomechanics Testing
Single-Leg Forward Hop
Participants were asked to perform a single-leg forward hop for maximal distance.4,20 During the hopping task, biomechanical data were collected with a Vicon motion capture system (Vicon MX, Oxford Metrics) sampling at 240 Hz, used in conjunction with an AMTI force platform (OR 6-7, Advanced Medical Technology, Inc) sampling at 1200 Hz.
To determine hop distance, subjects performed successive hops, with 1 minute of rest in between, until no increase in distance was noted. A minimum of 3 hops had to be performed. Once maximal hop distance was determined, that distance was measured from the center of the force platform to a marked location on the floor that was used as the starting point for the trial.
Subjects then performed 3 successful hop attempts. The order of limb testing was randomized before the beginning of the testing session.
Biomechanical Data Processing
Lower limb joint rotations in the sagittal plane were determined using a 3-dimensional coordinate system and retroreflective markers similar to our previous work. 17 The markers were placed on precise locations per segment: torso (7th cervical vertebrae, 10th thoracic vertebrae, bilateral acromion process, and sternum), pelvis (bilateral anterior superior iliac spine, bilateral iliac crest, and bilateral posterior superior iliac spine), thigh (greater trochanter, distal thigh, medial and lateral femoral epicondyle), lower leg (tibial tuberosity, lateral lower leg, distal lower leg, medial and lateral malleoli), and foot (calcaneus, navicular, base of fifth metatarsal, and head of the first metatarsal). Once markers were properly placed and secured, subjects were asked to stand on the center of the force platform so that a static trial in alignment with the laboratory coordinate system could be recorded. From the static trial, we used Visual3D software (Version 4.0, C-Motion) to generate a kinematic model of the skeletal segments. 22 The 3-dimensional marker trajectories recorded during each dynamic hopping trial were subsequently processed with the respective subject’s Visual 3D model to solve for the generalized coordinates of each frame. Joint rotations were calculated using the Cardan rotation sequence (X, Y, Z) 8 and were expressed relative to the subject’s neutral position recorded from the static trial. Ground-reaction force data were sampled and synchronized with the kinematic data and both were filtered with a fourth-order, zero-lag, low-pass Butterworth filter with 12-Hz cutoff frequency. 23 Filtered ground-reaction force data and joint rotations were then submitted to standard inverse dynamics within Visual 3D. Sagittal plane knee joint moments were expressed as flexion-extension moments with regard to the Cardan axes of the local joint coordinate system. Moments were normalized to subject body height and mass and represented as internal moments.
The landing phase for the single-leg forward hop task was time normalized from initial contact, occurring when the vertical ground-reaction force exceeded 10 N, to 250 ms post-initial contact.10,17 This time window was selected as it was considered to include the time when the knee was maximally loaded (ie, peak flexion/extension moments and peak ground-reaction force had occurred in all subjects during this window). Ensemble averages for sagittal plane KFAs and knee extension moments were calculated for the landing phase.17,22 From the created ensemble averages, we recorded the peak sagittal plane knee joint rotations and knee moments and converted them into symmetry scores in the same manner as the quadriceps index.
Statistical Analysis
Two decision tree analyses using the classification and regression tree modeling were created to assess factors that predict peak sagittal plane KFA and peak knee extension moment symmetry. KFAs and moments were dichotomously characterized as symmetrical or asymmetrical. Values were considered symmetrical if the index was 90% or greater and considered asymmetrical if indices were <90%. The 90% threshold was chosen because healthy subjects present with symmetrical KFAs and knee moments during movement that are above this level. 30 Factors/predictors considered in the decision tree included (1) age, (2) sex, (3) mass, (4) height, (5) graft type, (6) isokinetic quadriceps index at the time of return to activity, (7) CAR symmetry at the time of return to activity, (8) IKDC score at the time of return to activity, and (9) time from surgery to biomechanical testing. The conditions of the decision tree analysis were as follows: maximum depth of tree, 5; minimum value of parent node, 4; and minimum value of child node, 2. Analyses were performed using Statistical Package for the Social Sciences (SPSS) (Version 26, IBM Corporation).
Results
Symmetry data for outcome and predictor variables along with relevant surgical information and demographics for participants classified with symmetrical and asymmetrical KFAs and knee extension moments can be found in Tables 1 and 2. ACL limb and uninjured limb data for participants classified with symmetrical and asymmetrical KFAs and knee extension moments can be found in Appendix Tables A1 and A2 (available in the online version of this article).
Table 2.
Demographic and predictor variable information for symmetrical and asymmetrical knee extension moment groups (mean ± SD)
| Group | Age, y | Height, cm | Mass, kg | Time From ACL Recons-truction to Testing, d | Sex | Concomitant Surgery | Graft Type | Surgical Limb Is Dominant Limb a | ACL Limb Single-Leg Hop Distance | KEM Symmetry | Quadriceps Strength Symmetry | CAR Symmetry | IKDC Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symmetrical KEM (N = 11) |
16.8 ± 2.4 | 171.9 ± 7.9 | 71.0 ± 16.1 | 285.3 ± 57.4 | Male = 4; female = 6 | 3 LM repair 3 LM debride |
3 Ham 2 Quad 5 BPTB |
5 = yes; 6 = no | 135.9 ± 27.9 | 99.0 ± 6.4 | 84.2 ± 12.8 | 95.9 ± 7.4 | 89.3 ± 8.6 |
| Asymmetrical KEM (N = 20) |
17.4 ± 2.5 | 172.1 ± 11.4 | 76.4 ± 17.9 | 292.6 ± 47.6 | Male = 9; female = 12 | 4 LM repair 3 MM repair 3 part LMEX |
2 Ham 19 BPTB |
7 = yes; 10 = no 3 = unknown |
140.2 ± 30.5 | 74.1 ± 8.9 | 72.3 ± 16.3 | 97.7 ± 6.9 | 85.7 ± 8.4 |
BPTB, bone-patellar tendon-bone; CAR, central activation ratio; Ham = hamstring; IKDC, International Knee Documentation Committee; KEM, knee extension moment; LM, lateral meniscus; LMEX, lateral meniscectomy; MM, medial meniscus; Quad = quadriceps.
Dominant limb defined as what leg would be used to kick a ball.
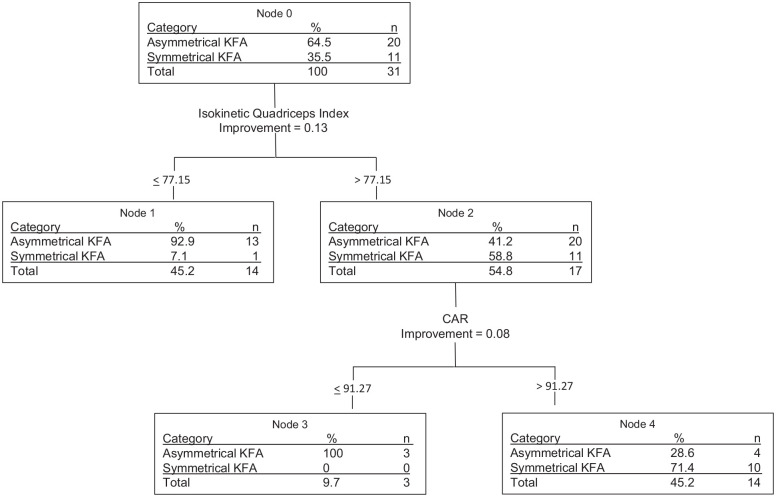
The decision tree for peak KFA highlighted isokinetic quadriceps index as the most important predictive factor. After quadriceps index, CAR was the only other variable that improved the model’s predictability (Figure 1).
Figure 1.
Decision tree for knee flexion angle. CAR, central activation ratio; KFA, knee flexion angle.
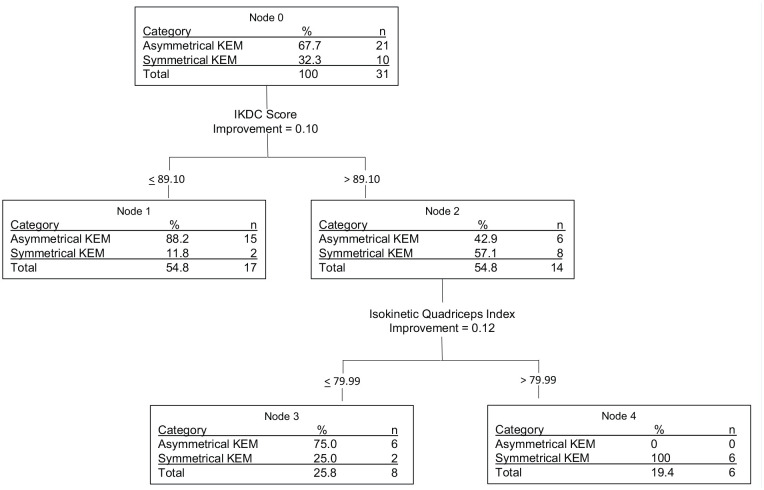
The score on the IKDC was identified as the most important predictive factor in the decision tree for the knee extension moment. After IKDC, only quadriceps index was identified as an additional predictor (Figure 2).
Figure 2.
Decision tree for knee extension moment. IKDC, International Knee Documentation Committee; KEM, knee extension moment.
Discussion
The purpose of this study was to examine if quadriceps strength and activation symmetry as well as patient-reported knee function could be utilized to predict patients that would have symmetrical sagittal plane knee biomechanics during hopping after ACL reconstruction. We found that quadriceps strength and activation symmetry allowed for patients with symmetrical KFAs to be identified, while self-reported function and quadriceps strength symmetry allowed for detection of patients with symmetrical knee extension moments. The KFA decision tree was robust as it correctly classified between 80% and 90% of patients into their respective groups, while the knee extension moment decision tree was perfect in identifying patients with asymmetrical knee extension moments, but only fair in identifying those with symmetrical moments.
Quadriceps strength symmetry was the most important predictive factor contributing to successful identification of patients with a symmetrical KFA in the current study. Previous research 26 has shown that isokinetic and isometric quadriceps strength symmetry during hopping is associated and/or correlated with the KFA, which corroborates our finding. Achieving isokinetic quadriceps strength symmetry of at least 77% was the threshold for classification into the symmetrical KFA group, suggesting that greater quadriceps strength symmetry is important for KFA symmetry. While we hypothesized that higher strength symmetry would lead to higher KFA symmetry, the 77% threshold value was lower than anticipated. Quadriceps strength symmetry is considered to be clinically acceptable at levels of 80%16,31 or 90%1,13,21 and as such we hypothesized that strength symmetry of at least 80% may be required to achieve adequate neuromuscular control and acceptable KFA symmetry. However, this was not the case. Adequate muscle forces may be produced during landing tasks using a variety of strategies and may not require higher magnitudes of quadriceps strength or strength symmetry to achieve the necessary forces to control knee flexion during landing. Regardless, our results indicate that higher quadriceps strength symmetry can predict symmetry in the KFA and patients achieving more than 77% quadriceps strength symmetry are more likely than not to land with symmetrical sagittal plane knee angles.
In addition to quadriceps strength symmetry, quadriceps CAR symmetry also contributed to the decision tree model’s ability to identify patients with symmetrical KFAs. We identified that a CAR symmetry of 91.2% was the threshold value associated with a more symmetrical KFA. It is not surprising that the CAR, a measure of muscle activation failure or quadriceps neurological inhibition, helped predict knee flexion symmetry. Greater quadriceps activation symmetry may allow for more symmetrical recruitment of the quadriceps muscles during gait, which could contribute to greater, more symmetrical knee flexion excursions. No prior work has examined the relationship between quadriceps CAR symmetry and KFA symmetry, but existing data 34 do support that CAR is related to knee mechanics in patients after ACL reconstruction. Furthermore, experimental models that induce quadriceps inhibition have been shown to elicit changes in sagittal plane knee flexion suggesting that quadriceps inhibition can alter knee motion. 25 Therefore, rehabilitation strategies aimed at reversing neurological inhibition may be critical to promote the recovery of knee biomechanical function after ACL reconstruction.
The present study illustrates that patient-reported knee function, as measured by the IKDC, was the largest predictor of patients who achieved symmetrical knee extensor moments. Our findings suggest ACL-reconstructed patients with high perceived knee function (IKDC > 89.1) were more likely to load their knees equally during a landing task. It is possible patients with high function may not adapt a compensatory landing strategy aimed at avoiding or underloading the ACL limb due to neuromuscular deficiencies. Prior work supports a relationship between sagittal plane knee moments and patient-reported function. For example, asymmetries during a single-leg drop landing at return to sport have been previously shown to be linked with patient-reported knee function, measured using the Knee Injury and Osteoarthritis Outcome Score (KOOS), at 2 years after ACL reconstruction. 12 Similarly, lower KOOS indicating lower self-reported knee function have been shown to be related to sagittal plane knee moments in patients 8 months after ACL reconstruction. 6 Our work reinforces these findings and expands on them to show ACL patients with IKDC scores ≥89 are likely to restore symmetrical knee loading during landing at the time they return to activity.
Symmetrical quadriceps strength, secondary to patient-reported knee function, was an additional contributor to the predictive model’s ability to identify patients with symmetrical knee extension moments. Participants with quadriceps strength symmetry >80% were more likely to hop with symmetrical knee extension moments. The quadriceps musculature plays a key role during landing as it is necessary to produce sufficient sagittal plane moments to control knee motion and dissipate impact forces. Quadriceps strength in the ACL-reconstructed limb that is not symmetrical to the contralateral, uninjured limb is suggestive of lingering quadriceps muscle weakness. Lingering weakness may lead to poor neuromuscular control during landing that puts the knee at risk for further injury or future joint degeneration. The ability of quadriceps strength to help classify patients as symmetrical or asymmetrical knee joint loaders is not surprising given their functional role described earlier. Furthermore, previous research 26 supports a relationship between knee extensor moments and quadriceps strength, with ACL reconstruction patients with stronger quadriceps also having more symmetrical knee extensor moments and patients with weaker quadriceps having more asymmetrical knee extensor moments. Our work is the first to show, however, that quadriceps symmetry of 80% may be adequate, when combined with adequate patient function, to produce symmetrical knee joint loads.
This study has limitations. The sample size for this study is small. We opted to consider a heterogeneous ACL sample in this study who had a variety of concomitant injuries/surgeries, different graft types, and so on, which could affect our decision tree models. We chose a heterogeneous sample as we believe it is most representative of the true ACL population and thus wanted our outcomes to be of value to this larger population of interest. Last, the model predicting the knee extensor moment symmetry using IKDC and isokinetic strength was only able to classify symmetrical patients accurately 60% of the time while asymmetrical loaders were classified correctly 100% of the time. This suggests that an IKDC score <89 combined with quadriceps strength <80% may be a useful metric to use to determine when patients are landing with asymmetrical mechanics. Furthermore, it supports that while achieving these cut-points may make a patient more likely to be a symmetrical loader, it does not ensure symmetry.
Conclusion
Quadriceps strength and activation symmetry classified patients who landed with symmetrical or asymmetrical KFAs after ACL reconstruction, while patient-reported function (ie, IKDC) and quadriceps strength classified patients landing with symmetrical or asymmetrical knee extension moments. Quadriceps strength and patient-reported function assessments can be easily completed in a clinical setting and should be utilized to help clinicians determine if patients are landing with symmetrical biomechanics at the time of a return-to-activity decision.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381211004932 for Factors That Predict Sagittal Plane Knee Biomechanical Symmetry After Anterior Cruciate Ligament Reconstruction: A Decision Tree Analysis by Riann M. Palmieri-Smith, Michael T. Curran, Steven A. Garcia and Chandramouli Krishnan in Sports Health: A Multidisciplinary Approach
Acknowledgments
The authors would like to thank Megan Kujawa for her assistance with data processing.
Footnotes
The following author declared potential conflicts of interest: R.M.P.-S. is an associate editor for Sports Health: A Multidisciplinary Approach.
ORCID iD: Steven A. Garcia  https://orcid.org/0000-0001-6266-0184
https://orcid.org/0000-0001-6266-0184
References
- 1. Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Almangoush A, Herrington L. Functional performance testing and patient reported outcomes following ACL reconstruction: a systematic scoping review. Int Sch Res Notices. 2014;2014:613034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arokoski JP, Jurvelin JS, Vaatainen U, Helminen HJ. Normal and pathological adaptations of articular cartilage to joint loading. Scand J Med Sci Sports. 2000;10:186-198. [DOI] [PubMed] [Google Scholar]
- 4. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697-1705. [DOI] [PubMed] [Google Scholar]
- 5. Chaudhari AM, Briant PL, Bevill SL, Koo S, Andriacchi TP. Knee kinematics, cartilage morphology, and osteoarthritis after ACL injury. Med Sci Sports Exerc. 2008;40:215-222. [DOI] [PubMed] [Google Scholar]
- 6. Chen AJ, Tatarski RL, Perry J, Quatman CE, Hewett TE, Di Stasi S. Single-leg hop mechanics are correlated with self-reported knee function early after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2020;73:35-45. [DOI] [PubMed] [Google Scholar]
- 7. Chmielewski TL. Asymmetrical lower extremity loading after ACL reconstruction: more than meets the eye. J Orthop Sports Phys Ther. 2011;41:374-376. [DOI] [PubMed] [Google Scholar]
- 8. Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115:344-349. [DOI] [PubMed] [Google Scholar]
- 9. Culvenor AG, Collins NJ, Guermazi A, et al. Early patellofemoral osteoarthritis features one year after anterior cruciate ligament reconstruction: symptoms and quality of life at three years. Arthritis Care Res (Hoboken). 2016;68:784-792. [DOI] [PubMed] [Google Scholar]
- 10. Deneweth JM, Bey MJ, McLean SG, Lock TR, Kolowich PA, Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. Am J Sports Med. 2010;38:1820-1828. [DOI] [PubMed] [Google Scholar]
- 11. Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc. 2018;26:426-433. [DOI] [PubMed] [Google Scholar]
- 12. Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43:2727-2737. [DOI] [PubMed] [Google Scholar]
- 13. Keays SL, Bullock-Saxton JE, Newcombe P, Keays AC. The relationship between knee strength and functional stability before and after anterior cruciate ligament reconstruction. J Orthop Res. 2003;21:231-237. [DOI] [PubMed] [Google Scholar]
- 14. Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19:861-869. [DOI] [PubMed] [Google Scholar]
- 15. Krishnan C, Allen EJ, Williams GN. Torque-based triggering improves stimulus timing precision in activation tests. Muscle Nerve. 2009;40:130-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee JH, Bae DK, Song SJ, Cho SM, Yoon KH. Comparison of clinical results and second-look arthroscopy findings after arthroscopic anterior cruciate ligament reconstruction using 3 different types of grafts. Arthroscopy. 2010;26:41-49. [DOI] [PubMed] [Google Scholar]
- 17. Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve biomechanical limb symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2015;30:738-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve quadriceps function post-ACL reconstruction. Knee. 2015;22:270-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lisee C, Lepley AS, Birchmeier T, O’Hagan K, Kuenze C. Quadriceps strength and volitional activation after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Sports Health. 2019;11:163-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40:2348-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lynch AD, Logerstedt DS, Grindem H, et al. Consensus criteria for defining ‘successful outcome’ after ACL injury and reconstruction: a Delaware-Oslo ACL cohort investigation. Br J Sports Med. 2015;49:335-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McLean SG, Huang X, Su A, Van Den Bogert AJ. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon). 2004;19:828-838. [DOI] [PubMed] [Google Scholar]
- 23. Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434-1443. [DOI] [PubMed] [Google Scholar]
- 25. Palmieri-Smith RM, Kreinbrink J, Ashton-Miller JA, Wojtys EM. Quadriceps inhibition induced by an experimental knee joint effusion affects knee joint mechanics during a single-legged drop landing. Am J Sports Med. 2007;35:1269-1275. [DOI] [PubMed] [Google Scholar]
- 26. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sport Med. 2015;43:1662-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Palmieri-Smith RM, Thomas AC, Karvonen-Gutierrez C, Sowers M. A clinical trial of neuromuscular electrical stimulation in improving quadriceps muscle strength and activation among women with mild and moderate osteoarthritis. Phys Ther. 2010;90:1441-1452. [DOI] [PubMed] [Google Scholar]
- 28. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Roewer BD, Di Stasi SL, Snyder-Mackler L. Quadriceps strength and weight acceptance strategies continue to improve two years after anterior cruciate ligament reconstruction. J Biomech. 2011;44:1948-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2015;47:1426-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shelbourne KD, Foulk DA. Timing of surgery in acute anterior cruciate ligament tears on the return of quadriceps muscle strength after reconstruction using an autogenous patellar tendon graft. Am J Sports Med. 1995;23:686-689. [DOI] [PubMed] [Google Scholar]
- 32. Shi H, Huang H, Ren S, et al. The relationship between quadriceps strength asymmetry and knee biomechanics asymmetry during walking in individuals with anterior cruciate ligament reconstruction. Gait Posture. 2019;73:74-79. [DOI] [PubMed] [Google Scholar]
- 33. van Meer BL, Meuffels DE, Vissers MM, et al. Knee injury and Osteoarthritis Outcome Score or International Knee Documentation Committee Subjective Knee Form: which questionnaire is most useful to monitor patients with an anterior cruciate ligament rupture in the short term? Arthroscopy. 2013;29:701-715. [DOI] [PubMed] [Google Scholar]
- 34. Ward SH, Blackburn JT, Padua DA, et al. Quadriceps neuromuscular function and jump-landing sagittal-plane knee biomechanics after anterior cruciate ligament reconstruction. J Athl Train. 2018;53:135-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381211004932 for Factors That Predict Sagittal Plane Knee Biomechanical Symmetry After Anterior Cruciate Ligament Reconstruction: A Decision Tree Analysis by Riann M. Palmieri-Smith, Michael T. Curran, Steven A. Garcia and Chandramouli Krishnan in Sports Health: A Multidisciplinary Approach