Abstract
Background:
In adolescents, the rate of meniscal injury at the time of anterior cruciate ligament (ACL) reconstruction, the rate of ACL graft revision, and clinical outcomes has not yet been investigated.
Hypothesis:
In patients younger than 16 years, the rate of meniscal injuries at the time of ACL reconstruction increases with time from injury. The mid-term revision rate and reoperation rate after ACL reconstruction with hamstrings and lateral tenodesis are lower than those reported in literature for isolate ACL reconstruction.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
Patients younger than 16 years who underwent ACL reconstruction with hamstring and lateral tenodesis, with a follow-up ≥2 years were included. The number of meniscal lesions was stratified according to the delay between injury-to-surgery (<3, 3-12, >12 months). All reoperations, Lysholm score, Knee Injury and Osteoarthritis Outcome Score subscales for pain (at rest and during activity), and return to sport were collected.
Results:
A total of 151 patients (mean age 14.8 ± 1.2 years) were included. Patients undergoing surgery at <3 months after injury had a lower meniscal injury rate (36%) than those treated at 3 to 12 months (55%) and >12 months (63%) after injury (P = 0.04). Medial meniscal lesions were more likely to be repaired when surgery was performed <3 months after injury (91%). Subjective follow-up data were available for 132 patients, and 19 were lost to follow-up. At 6.0 ± 2.6 years, 6% of patients underwent ACL revision; 1 of 20 (5%) patients with posterior tibial slope ≥12° and 4 of 45 (9%) patients with Tegner level ≥8. Nine new meniscal procedures were performed; 19% of repaired menisci underwent meniscectomy. Good or excellent Lysholm score was reported by 88% of patients; 56% of patients with concurrent lateral meniscectomy had pain during activity, 91% returned to sport, and 79% were still participating at final follow-up.
Conclusion:
Patients younger than 16 years undergoing ACL reconstruction within 3 months from injury had the lowest rate of meniscal injuries. ACL reconstruction with lateral tenodesis had low revision rate (6%) and good or excellent clinical outcomes in 88% of young adolescents.
Clinical Relevance:
Sport physicians should be aware that adolescent patients undergoing ACL reconstruction within 3 months after injury have the lowest rate of meniscal injuries; the mid-term revision rate of ACL reconstruction with lateral plasty is lower than 10% and the patients’ perceived outcomes are good with almost all patients returning to sport activity.
Keywords: young, adolescents, <16 years old, anterior cruciate ligament (ACL), failure, early, meniscus
Recent studies from registries and national databases have demonstrated that the rate of anterior cruciate ligament (ACL) ruptures in children and adolescents has increased over the past decade.18,19 A rapid growth of 15.7% in the 15- to 19-year-old cohort and of 27.6% in the 10- to 14-year-old cohort was in fact reported between 2007 and 2011, 29 and a 29-fold increase was estimated from 1997 to 2017. 18
The burden of pediatric and young adolescent ACL injuries motivated the urgent need of shared decision-making guidelines for the most appropriate management of this critical population, 2 since the outcomes and prognosis are far from being optimal. Studies have shown poor results with initial nonoperative management in young patients, where long-term meniscal or cartilage damage and instability were reported 13 ; thus, surgical management was advocated. However, controversies remain regarding both the timing of intervention and the surgical techniques.
Regarding the former aspect, Guenther et al 8 showed that a longer interval between injury and surgery was associated with an increased likelihood of new medial meniscal tears, particularly bucket handle tears. The authors thus suggested that ACL reconstruction within 1 year from injury may be warranted to reduce further meniscal lesions. Similarly, Lawrence et al 13 found that adolescent patients with ACL reconstruction performed after 3 months from injury had more medial meniscal tears and a lower chance of repair. For these reasons, early ACL reconstruction is considered the treatment of choice in young high-risk athletes,5,20 even if the exact timing remains controversial.
Regarding the surgical management of ACL injuries in pediatric and adolescent patients, potential damage of metaphyseal cartilage and growth disturbance has been reported with both physeal-sparing and trans-physeal techniques. Thus, the procedure of choice remains controversial. On the other hand, it should be acknowledged that growth disturbance could represent a concrete problem only in prepubescent patients with skeletal immaturity and 3 to 6 years of growth remaining, where all-epiphyseal techniques are suggested 5 ; for young adolescents with limited growth remaining, partial trans-physeal or adult reconstructions can be used. In these patients, usually aged between 14 and 16 years where the risk of physeal damage is negligible, 5 the main challenge is represented by an unacceptably high risk of ACL failure, which is reported to be in the range of 20% to 28%.5,26 Although lateral plasty has been suggested in this patient population,5,30 the evidence on the matter is scarce and an optimal technique has not been established. Therefore, there is the need to investigate different ACL reconstruction techniques involving lateral plasties in high-risk adolescent population. In this context, failure rates, subjective functional outcomes, return to sport, and reoperations represent important aspects to be investigated to determine the efficacy of the technique.
The aims of the present study are (1) to assess the prevalence of meniscal injuries at the time of ACL reconstruction in young adolescents less than 16 years old, (2) to assess the mid-term failure rate and reoperations of ACL reconstruction with hamstrings using an over-the-top plus lateral plasty technique, and (3) to assess subjective functional outcomes, pain and return to sport after the ACL reconstruction. The hypotheses were that (1) a progressively higher incidence of meniscal injuries can be found in patients with longer delay of ACL reconstruction, (2) the mid-term revision rate and reoperations after ACL reconstruction with hamstrings and lateral tenodesis are lower than those reported in literature for isolate ACL reconstruction (20%-28%),1,5,26,31 and (3) good functional score and return to sport can be found after ACL reconstruction with this technique.
Methods
Patient Selection
Prospectively collected patient practice database 7 was searched for demographic, injury, and surgical information. All consecutive patients younger than 16 years who underwent isolate primary ACL reconstructions between January 2007 and February 2017 at the Sport Traumatology Department of IRCCS Rizzoli Orthopedic Institute of Bologna, with at least 2 years of follow-up, were identified and screened for eligibility. Only primary ACL reconstructions with no other concomitant procedures except for meniscal treatment were considered eligible for inclusion. Patients were excluded if they had a previous ipsilateral or ACL injury or surgery.
All the patients were contacted by phone and interviewed by a trained researcher; Lysholm score, Knee Injury and Osteoarthritis Outcome Score (KOOS), and visual analogue scale (VAS) for pain (at rest and during activity) questionnaires were administered. The Tegner activity level was collected retrospectively to assess the preinjury, preoperative, postoperative, and final follow-up levels. The postoperative Tegner was defined as the higher value obtained after ACL reconstruction, during the considered follow-up. Possible reasons for not participating in sports were inquired as well. Patients and their medical charts were revised to identify further ipsilateral knee reoperations.26,28 Based on medical charts and interviews, the following information were obtained: age at surgery, sex, body mass index, preoperative Tegner activity level, time elapsed between injury and surgery, and date of further ipsilateral knee surgeries. Time elapsed between injury and surgery was categorized in 3 groups based on the existing literature8,13: <3 months, 3 to 12 months, and >12 months. Posterior tibial slope (PTS) was measured on preoperative radiographs, when available, according to Webb et al. 25 The protocols of this study were approved by the local ethics committee (CE AVEC: 265/2019/Oss/IOR).
Surgical Procedure
All patients were treated either with a single-bundle over-the-top ACL reconstruction plus lateral plasty using both hamstring tendons (gracilis and semitendinosus), 15 or with a slightly modified physeal-sparing technique aimed at preventing the degradation of metaphyseal cartilage. 22 After both hamstring tendons were harvested, preserving their tibial attachment, they were passed through the tibial tunnel (6-8 mm large, depending on the graft diameter) and over the top of the femur. Ten cycles of knee flexion-extension were performed for graft pretensioning. The knee was flexed to 45° with neutral tibial rotation, and a posterior drawer was applied. The tendons were then fixed to the cortical bone of the femur with 2 bone staples under manual maximum tension. The remaining part of the tendons was then passed deep to the iliotibial band, superficial to the lateral collateral ligament, and fixed with a single staple onto Gerdy’s tubercle as extra-articular plasty. In patients with open physis (active growth cartilage was assessed preoperatively with magnetic resonance images and intraoperatively with fluoroscope radiograph images), a modified over-the-top with lateral plasty was performed, 22 drilling an all-epiphyseal tunnel above the metaphyseal cartilage, under fluoroscopic guidance. In the case of meniscal ruptures, meniscal repair was aggressively pursued in lesions involving both red-on-red and red-on-white zone. An all-inside suture device (FasT-Fix, Smith & Nephew) was used to perform vertical or horizontal sutures based on the tear pattern.
All patients underwent the same postoperative rehabilitation protocol. A knee brace was not used postoperatively. Range of motion, quadriceps muscle active exercises, straight leg raises, and prone hamstring muscle-stretching exercises were all begun the day after surgery. Functional muscle stimulation was used for 2 hours, 3 times daily, for 4 weeks. Patients were allowed partial weightbearing during the first 2 weeks. Furthermore, patients were allowed full passive extension and active flexion through the range from 0° to 120° starting from the third postoperative day. Three weeks after surgery, full weightbearing was allowed. Stationary biking, active knee extension with weights, and one-quarter squats were introduced 4 weeks after surgery. Running was started at 3 months and training for pivoting sports activities after 6 months. Full return to sport was not permitted before 8 to 12 months.
Statistical Analysis
Statistical analysis was performed with MedCalc (Version 19.1.6, Acacialaan, MedCalc Software). Continuous variables were reported as mean ± standard deviation, while categorical variables were expressed as absolute number and proportion of the total sample. Only the Tegner activity level was reported as median value with interquartile ranges (IQRs). Categorical variables were compared with the chi-square or Fisher’s exact test. The risk of having meniscal tears at the time of ACL reconstruction among the groups with different surgical timing (<3 months, 3-12 months, or >12 months) was reported as odds ratio (OR) with 95% CI. Statistical significance was set with P < 0.05.
Results
Timing of Reconstruction and Meniscal Status
Overall, 151 consecutive patients younger than 16 years at the time of ACL reconstruction were included in the analysis (Table 1). There were 98 (65%) boys and 53 (35%) girls; mean age at surgery was 14.8 ± 1.2 years (range, 8.7-15.9 years). The modified physeal-sparing technique was used in 20 (13%) patients, 8 boys and 12 girls. ACL reconstructions were performed after a mean of 8.0 ± 10.5 months (range, 0.5-60 months) from injury: specifically, in 45 patients (30%) within 3 months, in 76 patients (50%) between 3 and 12 months, and in 30 patients (20%) after 12 months. A total of 77 patients (51%) were presenting lesions of either medial or lateral meniscus at the time of surgery (Table 2), and there was no significant difference in meniscal lesions between male and female patients. A lower rate of meniscal lesions was reported in those undergoing surgery within 3 months (36%) compared with those between 3 and 12 months (55%) and >12 months (63%) (P = 0.04) (Table 3). A significantly higher risk of having meniscal tears at the time of ACL reconstruction was thus reported both in patients with surgeries performed between 3 and 12 months and >12 months, in comparison with those with early (<3 months) reconstructions (Table 4). Moreover, patients undergoing surgery >12 months after injury had concomitant medial and lateral meniscal lesions in 20% of cases and an OR = 4.8 (95% CI 1.4-16.1; P = 0.01) in comparison with those treated ≤12 months after injury.
Table 1.
Demographic characteristics of the included patients
| Characteristics | Mean ± SD or n (%) |
|---|---|
| Age, y, at surgery (n = 151) | 14.8 ± 1.2 (range, 8.7-15.9) |
| <12 | 4 (3) |
| 12-14 | 18 (12) |
| 14-16 | 129 (85) |
| Time, mo, from injury to surgery | 8.0 ± 10.5 (range, 0.5-60) |
| <3 | 45 (30) |
| 3-12 | 76 (50) |
| >12 | 30 (20) |
| Sex | |
| Male | 98 (65) |
| Female | 53 (35) |
| Body mass index, kg/m2 | 22 ± 3 |
| Side | |
| Right | 83 (55) |
| Left | 68 (45) |
| Age, y, at follow-up (n = 132) | 20.7 ± 2.9 (range, 15.0-26.3) |
| Final follow-up, y | 6.0 ± 2.6 (range, 2.2-11.0) |
Table 2.
Meniscal lesions and treatment at the time of anterior cruciate ligament reconstruction
| Total, n (%) | Meniscectomy, n (%) | Repair, n (%) | |
|---|---|---|---|
| Medial | 48/151 (32) | 15/48 (31) | 33/48 (69) |
| Lateral | 41/151 (27) | 22/41 (54) | 19/41 (46) |
| Medial or lateral | 77/151 (51) | ||
| Medial and lateral | 12/151 (8) |
Table 3.
Number of meniscal lesions according to the timing of surgery
| Medial or Lateral, n (%) | Medial, n (%) | Lateral, n (%) | Medial and Lateral, n (%) | |
|---|---|---|---|---|
| <3 mo | 16/45 (36) | 12/45 (27) | 7/45 (15) | 3/45 (7) |
| 3-12 mo | 42/76 (55) | 23/76 (30) | 22/76 (29) | 3/76 (4) |
| >12 mo | 19/30 (63) | 13/30 (43) | 12/30 (40) | 6/30 (20) |
| P | 0.04* | 0.29 | 0.06 | 0.02* |
P < 0.05.
Table 4.
Risk of meniscal lesion compared with anterior cruciate ligament reconstruction within 3 months
| Lesion | Odds Ratio (95% CI) | P |
|---|---|---|
| Medial or lateral meniscal lesion | ||
| 3-12 mo | 2.2 (1.1-4.8) | 0.04* |
| >12 mo | 3.1 (1.2-8.2) | 0.02* |
| Medial meniscal lesion | ||
| 3-12 mo | — | n.s. |
| >12 mo | — | n.s. |
| Lateral meniscal lesion | ||
| 3-12 mo | — | n.s. |
| >12 mo | 3.6 (1.7-10.7) | 0.02* |
| Medial and lateral meniscal lesion | ||
| 3-12 mo | — | n.s. |
| >12 mo | — | n.s. |
s., not significant.
P < 0.05.
Meniscal repair was performed in 33 of 48 (69%) lesions of medial meniscus and in 19 of 41 (46%) lesions of lateral meniscus. A higher percentage of repairable medial meniscal tears was found in patients with ACL reconstruction performed within 3 months (92%) in comparison with those after 12 months (46%) (P = 0.05) (Table 5), thus showing a higher chance of repair (OR = 12.8, 95% CI 1.2-130, P = 0.03).
Table 5.
Proportion of meniscal lesions repaired at the time of anterior cruciate ligament reconstruction according to the different surgical timing
| Medial, n (%) | Lateral, n (%) | Medial or Lateral, n (%) | |
|---|---|---|---|
| <3 mo | 11/12 (92) | 3/7 (43) | 10/16 (63) |
| 3-12 mo | 16/23 (69) | 10/22 (45) | 24/42 (57) |
| >12 mo | 6/13 (46) | 6/12 (50) | 7/19 (37) |
| P | 0.05* | 0.95 | 0.24 |
P < 0.05.
ACL Revisions and Reoperations
A total of 19 patients (13%) were lost to follow-up because they changed their phone number or address; therefore, ACL revisions and reoperations were evaluated in 132 patients at a mean follow-up of 6.0 ± 2.6 years (range, 2.2-11.0 years) (Table 1). A total of 28 of 132 patients (21%) had a surgical procedure within the considered follow-up, with no significant difference between male and female patients. Eight patients (6%) underwent revision ACL reconstruction after a mean of 2.4 ± 1.2 years after surgery, with only 1 of them having a PTS ≥12°. Overall, among the 20 patients that had PTS ≥12°, only 1 failed (5%). Among the 45 patients with Tegner level ≥8, 4 failed (9%).
Nine other patients (7%) underwent an arthroscopic procedure for meniscal treatment; however, considering 4 further lesions treated at the time of revision ACL, the overall number of meniscal lesions after primary reconstruction was 13 (5 new lesions and 8 lesions of previously repaired menisci) (Table 6). Of all 42 meniscal sutures performed at the time of primary ACL reconstruction in the evaluated patients, 8 (19%) required a further meniscectomy (Table 6). A total of 10 (8%) hardware removal were performed because of local irritation, especially in patients younger than 14 years (5/19; 26%) rather than in those between 14 and 16 years (5/113; 4%) (P = 0.0008). A patient (0.8%) underwent arthroscopic lavage and debridement because of septic arthritis. No patients underwent corrective osteotomies or partial epiphysiodesis during the considered follow-up. Finally, 16 patients (12%) underwent contralateral ACL reconstruction.
Table 6.
Number of reoperations performed because of meniscal lesions and number of total meniscal lesions that occurred within the considered follow-up
| Total, n (%) | Meniscectomy, n | Repair, n | |
|---|---|---|---|
| New meniscal surgeries | |||
| Medial | 6 (5) | 4 | 2 |
| Lateral | 3 (2) | 3 | 0 |
| Total | 9 (7) | 7 | 2 |
| New lesions of intact menisci a | |||
| Medial | 3 (2) | 1 | 2 |
| Lateral | 2 (2) | 1 | 1 |
| Total | 5 (4) | 2 | 3 |
| Lesions of previous meniscal repair a | |||
| Medial (n = 29) | 4 (14) | 4 | 0 |
| Lateral (n = 13) | 4 (31) | 4 | 0 |
| Total (n = 42) | 8 (19) | 8 | 0 |
New lesions and lesions of previous meniscal repair take into account also 3 meniscal lesions treated at the time of revision anterior cruciate ligament reconstruction.
Postoperative Functional Outcomes and Return to Sport
Excluding the 8 patients who underwent revision ACL reconstruction, subjective functional evaluation was possible in 124 patients with a mean age of 20.7 ± 2.9 years at the time of questionnaire completion, on average 5.9 ± 2.4 years after ACL reconstruction. Mean Lysholm score was 94 ± 10, with 73% of patients rated as “excellent,” 15% as “good,” 9% as “fair,” and 2% as “poor.” Mean values of KOOS subscales were 97 ±7 for pain, 94 ± 10 for symptoms, 99 ± 3 for activities of daily living, 95 ± 11 for sport, and 88 ± 18 for quality of life. Mean VAS for pain (0-100) was 1.2 ± 8.5 at rest and 9.2 ± 17.1 during activity. A lower number of patients were pain-free during activity among those who underwent concurrent lateral meniscectomy (8 of 18; 44%) in comparison with those with intact or repaired lateral meniscus (78 of 106; 74%) (P = 0.003).
Overall, 91% of patients returned to sport after 7.6 ± 2.6 months and 68% at the same preinjury level. At the final follow-up, 79% were still participating in sports but only 35% at the same preinjury level. Tegner level was 7 (IQR 7-9) at the preinjury status, 1 (IQR 1-3) before surgery, 7 (5-8) after surgery, and 5 (IQR 4-7) at the final follow-up. In total, 59% of patients had a Tegner level ≥7 (level ≥8 in 26%) after ACL reconstruction (Figure 1). The reasons for decrease or abandonment of sport activity were personal (49%), fear of reinjury (34%), knee pain or impairment (13%), and problems in the contralateral knee (3%).
Figure 1.
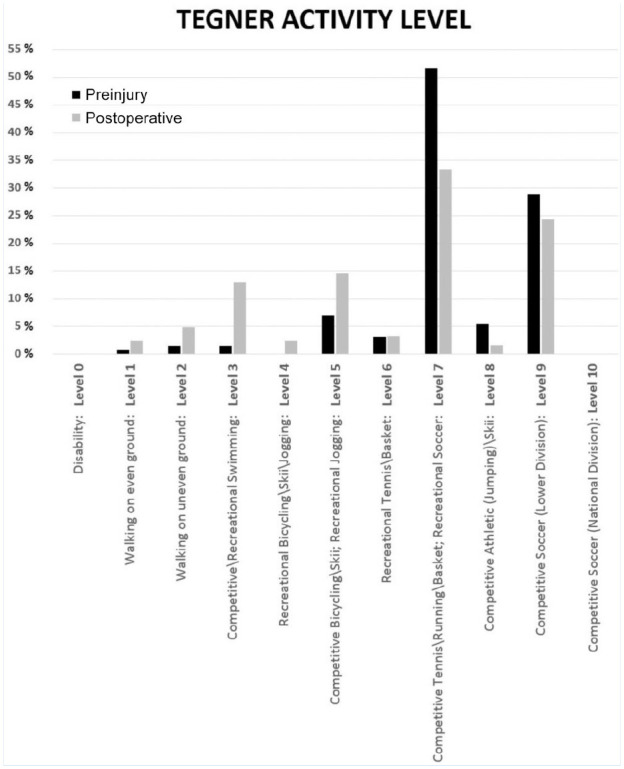
Tegner activity level before the injury (black bars) and after anterior cruciate ligament reconstruction (gray bars).
Discussion
The most important finding of the present study was that adolescent patients undergoing ACL reconstruction within 3 months from injury had the lowest rate of meniscal injuries and the best chance of repair, in comparison with those operated between 3 and 12 or after 12 months from injury. Moreover, the mid-term failure rate of the over-the-top plus lateral plasty reconstruction with hamstrings was lower than 10%, even in patients with high PTS or high level of activity. The overall reoperation rate was instead 21%, especially because of new meniscal tears or hardware removal. Finally, the subjective outcomes were good, with higher probability of postoperative pain in patients with lateral meniscectomy; almost all patients (91%) returned to sport practice. A deep analysis of the data from the present study offers some interesting considerations regarding the general management of young adolescent patients with ACL injury and regarding the peculiar surgical technique employed.
Timing of Reconstruction and Meniscal Status
The 51% rate of concomitant meniscal lesions reported in this population of young adolescents <16 years old is consistent with the 51.4% reported in a systematic review of 37 studies including 863 patients with a mean age of 13.2 years. 14 Moreover, the rate of medial lateral meniscal tears (32% and 27%) was similar to that reported in an analogous cohort of 100 <16 year old patients (32% and 29%). 21 A correlation of meniscal lesions associated with ACL injury and surgical timing has been established, even in adolescents6,13; however, different cutoffs for early reconstruction were suggested, determined both by deliberate choice and health systems capability. 13 As an example, the average time from injury to surgery was 1 year for 112 Canadian patients aged 11 to 16 years, 13 4 months in a series of 61 American patients aged 11 to 16 years 30 or 8.3 months in a systematic review of 24 studies of young patients. 14 Based on the results of the present study, surgical treatment within 3 months is recommended to minimize the risk of concurrent meniscal lesions and maximize the chance of repair. In fact, higher rates of meniscal lesions were reported in patients operated after 12 months and even in those operated between 3 and 12 months. Of note, almost all medial meniscal tears (92%) were repaired when operated within 3 months. Of course, the management of meniscal lesions in this retrospective study could have been influenced by the time since injury itself. However, considering the young age and the well-known deleterious effect of meniscal removal, 10 repair was aggressively pursued in as many lesions as possible. It was possible to repair 58% of the 89 meniscal lesions, which is similar to the 50% to 53% reported by Cordasco et al 5 in 275 patients aged between 12 and 20 years. This meniscus-preserving approach is recommended not only because of the long-term risk of osteoarthritis10,34 but also for short- to mid-term complications such as knee pain and lateral chondrolysis. 23 In fact, more than half of our patients with partial lateral meniscectomy at the time of ACL reconstruction complained of knee pain during activity, compared with less than 30% of those with intact or repaired meniscus.
Failures and Reoperations
ACL reconstruction failure represents a critical issue in young adolescent patients because of frequent concomitant hyperlaxity, common participation in high-level activities, and technical challenges related to potential growth plate damage.1,31 An important step in understanding the causes of the high failure rate in young patients 26 has been provided by Cordasco et al, 5 which stratified the revision rate according to skeletal maturity of 324 athletes younger than 20 years. The authors found a similar rate of 6% in elementary and middle school-aged patients (mean age, 12 years) and in skeletally mature high school athletes (mean age, 16.2 years), while a disproportionally higher rate of 20% in the middle group of patients from eighth and ninth grades aged usually between 13 and 15 years. The authors concluded that failure rate was independent from graft choice or surgical technique; rather, they focused their attention on the school grade and the level of competition to which patients were exposed after recovery, in a crucial phase of developmental growth. A high rerupture rate of 13% was reported also by Ho et al 9 in 285 patients with a mean age of 14.4 years, while an even higher rate of 28% was reported by Webster and Feller 26 in male patients younger than 18 years. For these reasons, Cordasco et al, 5 analyzing their data and the existing literature, developed a guideline for treating this high-risk population that entails a lateral extra-articular tenodesis in selected cases. A similar approach was suggested by Wilson et al, 30 who routinely performed an extra-osseous iliotibial band lateral augmentation in 57 adolescents aged 11 to 16 years, reporting reinjuries in only 5.3% and minimal growth disturbance. Very consistent outcomes in terms of failure (6%) in a similar population (9-16 years) were reported in the present study using an extra-osseous over-the-top ACL reconstruction combined with a lateral plasty using hamstrings. Moreover, a low acceptable rate was also reported in the subgroup of patients with PTS ≥12° (5%) and in those with Tegner level ≥8 (9%), which are those considered at higher risk. The clinical, objective, and radiological results of this procedure have already been reported in multiple studies in either adult7,15,16,32,34 or skeletally immature patients. 22 In the former super-selected population of 20 patients with a mean age of 12.3 years (range, 8-13 years), good subjective and objective outcomes were reported, with no reinjury after a mean follow-up of 5 years. Moreover, none of the patients developed valgus deformity and only 3 had minor long leg discrepancies, all not exceeding 1 cm. Thus, considering that the lateral plasty did not differ between the adult and physeal-sparing technique, such reconstruction can be considered safe at any age. In fact, no patients underwent partial epiphysiodesis or realignment osteotomy, an occurrence which has been reported to reach more than 1%. 18 A similar concept of combined intra-articular and extra articular extra-osseous reconstruction has already been employed by Kocher et al 12 using iliotibial band in 237 skeletally immature Tanner 1 or 2 patients, reporting satisfactory outcomes in terms of failure rate (6.6%), subjective scores, and respect of skeletal growth. Both techniques are easy to perform and respectful of immature physis, but the latter allows for increase of the graft size respective to the iliotibial band, which is only minimally affected, reducing the tissue invasively.
Regarding other reoperations, the overall rate of 21% was not far from the 24% reported in a similar population of 100 patients <16 years. 21 Of note, patients operated with this technique have a relevant chance to present hardware-related complaints, which could require surgical removal in up to 26% of patients <14 years.
The rate of new meniscal procedure near 10% at mid-term is in line with a previous study. 21 Interestingly, most of them were related to a previous repair; specifically, 19% of meniscal sutures performed at the time of primary reconstruction required a further meniscectomy. This result, apart from resembling the trend in the general population, 17 is also encouraging considering the aggressive indication of meniscal suture that allowed to repair more than half of concomitant meniscal lesions.
Postoperative Functional Outcomes and Return to Sport
Clinical subjective results were considered good or excellent in 88% of cases, with a mean Lysholm score (94 points), which is consistent with what was reported in a systematic review of 57 studies (95.7-96.8 points). 14 Moreover, KOOS subscales were good as well, confirming the efficacy of the procedure in young adolescents. It should be considered that questionnaires were obtained on an average of 6 years from surgery and at a mean age of 20.7 years in patients actively involved in sport practice. In fact, a high rate of return to sport (91%) was achieved, similarly to the general trend of the current literature (90%) 11 ; moreover, most patients were involved in high-demanding activities (Tegner level ≥7). Therefore, it is not surprising to note a relevant rate of patients that reduced their sport activity level from the first years after return to sport, to the mid-term follow-up. In fact, ACL injury and reconstruction has been reported to show good results in terms of short-term return to preinjury level, which tends to decline in around 30% of cases.4,24,33 The reasons for such phenomenon are under investigation,3,27 but in this study, it was mainly because of personal issues or fear of reinjury, thus not related to specific knee problems. If nonsurgical physiotherapy or psychological interventions do not improve this aspect, it should be investigated in further studies.
Limitations
This study presents limitations. First, patients were not evaluated objectively at final follow-up, objective laxity measurements were not available, and failures were only defined when patients underwent ACL revision surgery. Subclinical failure cases not requiring ACL reconstruction could have gone undetected. Unavoidably, this limitation is common in some studies26-28; on the other hand, the use of a clear outcome such as ACL revision leaves no room for interpretation.
A second limitation is the lack of objective criteria for return to sports; in this cohort of patients, only time-based criteria were used for sport resumption.
Conclusion
Young adolescents <16 years old undergoing ACL reconstruction within 3 months from injury had the lowest rate of meniscal injuries in contrast to those operated between 3 and 6 months and after 12 months; moreover, almost all medial meniscal lesions were repaired. ACL reconstruction with hamstring over-the-top and lateral plasty had a low revision rate (6%) and good or excellent clinical outcomes in 88% of young adolescents <16 years old, with knee pain mainly in those with concomitant lateral meniscectomy. Almost all patients returned to sport, but they tended to decline their activity level over time.
Acknowledgments
The authors want to thank Margaux Hylton for her contribution in the language revision of the manuscript.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iD: Luca Macchiarola  https://orcid.org/0000-0002-2351-8836
https://orcid.org/0000-0002-2351-8836
References
- 1. Anderson CN, Anderson AF. Management of the anterior cruciate ligament-injured knee in the skeletally immature athlete. Clin Sports Med. 2017;36:35-52. [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Ekås G, Grindem H, et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Knee Surg Sports Traumatol Arthrosc. 2018;26:989-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med. 2015;43:848-856. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40:2517-2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cordasco FA, Black SR, Price M, et al. Return to sport and reoperation rates in patients under the age of 20 after primary anterior cruciate ligament reconstruction: risk profile comparing 3 patient groups predicated upon skeletal age. Am J Sports Med. 2019;47:628-639. [DOI] [PubMed] [Google Scholar]
- 6. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40:2128-2133. [DOI] [PubMed] [Google Scholar]
- 7. Grassi A, Macchiarola L, Lucidi GA, et al. More than a 2-fold risk of contralateral anterior cruciate ligament injuries compared with ipsilateral graft failure 10 years after primary reconstruction. Am J Sports Med. 2020;48:310-317. [DOI] [PubMed] [Google Scholar]
- 8. Guenther ZD, Swami V, Dhillon SS, Jaremko JL. Meniscal injury after adolescent anterior cruciate ligament injury: how long are patients at risk? Clin Orthop Relat Res. 2014;472:990-997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ho B, Edmonds EW, Chambers HG, Bastrom TP, Pennock AT. Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: a review of 561 cases. J Pediatr Orthop. 2018;38:388-392. [DOI] [PubMed] [Google Scholar]
- 10. Hulet C, Menetrey J, Beaufils P, et al. Clinical and radiographic results of arthroscopic partial lateral meniscectomies in stable knees with a minimum follow up of 20 years. Knee Surg Sports Traumatol Arthrosc. 2015;23:225-231. [DOI] [PubMed] [Google Scholar]
- 11. Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019-1036. [DOI] [PubMed] [Google Scholar]
- 12. Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am. 2018;100:1087-1094. [DOI] [PubMed] [Google Scholar]
- 13. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-2587. [DOI] [PubMed] [Google Scholar]
- 14. Longo UG, Ciuffreda M, Casciaro C, et al. Anterior cruciate ligament reconstruction in skeletally immature patients: a systematic review. Bone Joint J. 2017;99-B:1053-1060. [DOI] [PubMed] [Google Scholar]
- 15. Marcacci M, Zaffagnini S, Giordano G, Iacono F, Presti ML. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: a prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am J Sports Med. 2009;37:707-714. [DOI] [PubMed] [Google Scholar]
- 16. Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc. 1998;6:68-75. [DOI] [PubMed] [Google Scholar]
- 17. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 201219;94:2222-2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nogaro MC, Abram SGF, Alvand A, Bottomley N, Jackson WFM, Price A. Paediatric and adolescent anterior cruciate ligament reconstruction surgery.Bone Joint J. 2020;102-B:239-245. [DOI] [PubMed] [Google Scholar]
- 19. Popkin CA, Wright ML, Pennock AT, et al. Trends in management and complications of anterior cruciate ligament injuries in pediatric patients: a survey of the PRiSM Society. J Pediatr Orthop. 2018;38:e61-e65. [DOI] [PubMed] [Google Scholar]
- 20. Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769-2776. [DOI] [PubMed] [Google Scholar]
- 21. Reid D, Leigh W, Wilkins S, Willis R, Twaddle B, Walsh S. A 10-year retrospective review of functional outcomes of adolescent anterior cruciate ligament reconstruction. J Pediatr Orthop. 2017;37:133-137. [DOI] [PubMed] [Google Scholar]
- 22. Roberti di, Sarsina T, Macchiarola L, Signorelli C, et al. Anterior cruciate ligament reconstruction with an all-epiphyseal “over-the-top” technique is safe and shows low rate of failure in skeletally immature athletes. Knee Surg Sports Traumatol Arthrosc. 2019;27:498-506. [DOI] [PubMed] [Google Scholar]
- 23. Sonnery-Cottet B, Archbold P, Thaunat M, Carnesecchi O, Tostes M, Chambat P. Rapid chondrolysis of the knee after partial lateral meniscectomy in professional athletes. Knee. 2014;21:504-508. [DOI] [PubMed] [Google Scholar]
- 24. Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50:744-750. [DOI] [PubMed] [Google Scholar]
- 25. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. 2013;41:2800-2804. [DOI] [PubMed] [Google Scholar]
- 26. Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:2827-2832. [DOI] [PubMed] [Google Scholar]
- 27. Webster KE, Feller JA. Expectations for return to preinjury sport before and after anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:578-583. [DOI] [PubMed] [Google Scholar]
- 28. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [DOI] [PubMed] [Google Scholar]
- 29. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36:447-452. [DOI] [PubMed] [Google Scholar]
- 30. Wilson PL, Wyatt CW, Wagner KJ, 3rd, Boes N, Sabatino MJ, Ellis HB., Jr. Combined transphyseal and lateral extra-articular pediatric anterior cruciate ligament reconstruction: a novel technique to reduce ACL reinjury while allowing for growth. Am J Sports Med. 2019;47:3356-3364. [DOI] [PubMed] [Google Scholar]
- 31. Wong SE, Feeley BT, Pandya NK. Complications after pediatric ACL reconstruction: a meta-analysis. J Pediatr Orthop. 2019;39:e566-e571. [DOI] [PubMed] [Google Scholar]
- 32. Zaffagnini S, Bruni D, Russo A, et al. ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports. 2008;18:573-581. [DOI] [PubMed] [Google Scholar]
- 33. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Return to sport after anterior cruciate ligament reconstruction in professional soccer players. Knee. 2014;21:731-735. [DOI] [PubMed] [Google Scholar]
- 34. Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45:3233-3242. [DOI] [PubMed] [Google Scholar]


