Symptomatic anemia is the most common manifestation in patients with lower-risk myelodysplastic syndrome (MDS) that requires treatment. Although both recombinant erythropoietin and lenalidomide are modestly effective as single agents, combined treatment yields a significantly higher and durable erythroid response.1,2 However, less than 50% of patients respond, therefore predictive biomarkers may assist in treatment selection for these patients. NLRP3 inflammasome-directed pyroptosis, irrespective of the functional classes of underlying somatic mutations, drives ineffective erythropoiesis, the common phenotype of lower-risk MDS.3 Although how MDS-related somatic mutations of disparate functional classes (e.g., RNA splicing and epigenetic regulation) activate the NLRP3 inflammasome remains elusive, they are linked to genomic instability with excessive reactive oxygen species production.4,5 Furthermore, NLRP3 can also be activated by aberrantly elevated proinflammatory cytokines, such as S100A9, in the bone marrow microenvironment of MDS.4 Apoptosis-associated speck-like protein containing a CARD (ASC) is the adapter molecule that binds NLRP3 in response to activating signals, which then polymerizes to generate docking sites for the caspase- 1 effector that instructs a number of cellular processes, including interleukin-1β production and lytic cell death, i.e., pyroptosis.6 ASC filaments cluster into a solitary signal complex referred to as a speck, which is released upon cytolysis and circulates for extended periods because of its inherent resistance to proteolytic degradation. 7 Circulating ASC speck is a measurable biomarker of pyroptosis, and elevated levels have previously been found in patients with known NLRP3 inflammasome activation, such as those with cryopyrin-associated periodic syndrome and Schnitzler syndrome.8 Capturing elevated circulating interleukin-1β, the typical downstream effector of inflammasome activation, is less practical given its very short half-life9 and it is virtually undetectable in plasma even in patients with active cryopyrin-associated periodic syndrome and Schnitzler syndrome.8 Peripheral blood plasma ASC speck levels are almost exclusively elevated in patients with lower-risk MDS, compared to other hematologic malignancies, and like the myeloid-related inflammatory protein S100A9, provide an index of the magnitude of medullary pyroptosis.4,10 In the current study, we explored whether peripheral blood plasma ASC speck level may serve as a biomarker of response in lower-risk MDS patients who received lenalidomide with or without epoetin β.
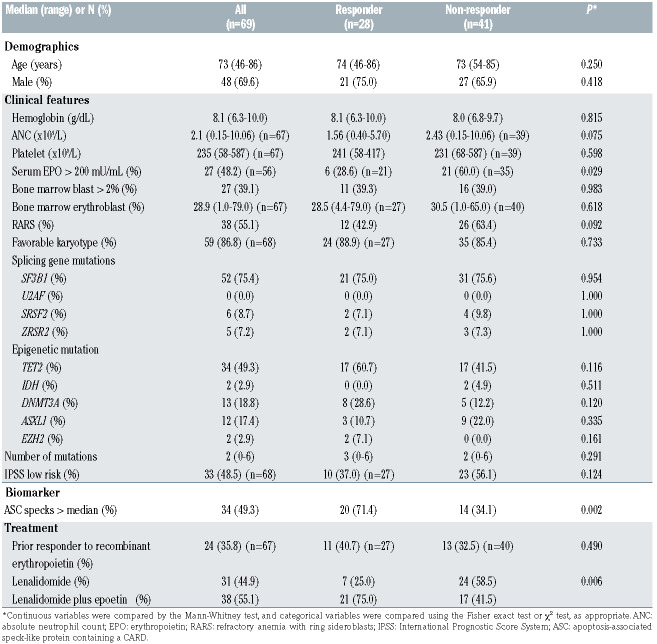
Table 1.
Characteristics of patients.
Peripheral blood plasma samples collected at the time of enrolment were available from 69 of 99 patients with International Prognostic Scoring System (IPSS) low- or intermediate-1-risk (i.e., lower-risk), non-deletion (5q) MDS who were enrolled in the GFM-Len-Epo-08 trial and completed four cycles (16 weeks) of study treatment. This Groupe Francophone des Myelodysplasies trial, registered as NCT01718379, was a randomized multicenter phase III study in transfusion-dependent lower-risk MDS patients comparing treatment with lenalidomide to the combination of lenalidomide and epoetin β. All patients had failed to respond to or relapsed after initial treatment with recombinant erythropoietin. Hematologic improvement of erythroid lineage (HI-E), the primary endpoint of the study, was evaluated after four cycles of treatment according to International Working Group 2006 criteria. Further details of the trial were described previously.2 The mean percentage of ASC specks was measured in peripheral blood plasma using flow cytometry and its level was glucose-adjusted with log10-transformation to adjust for hyperglycemia-induced inflammasome activation.10,11 Covariates associated with HI-E were analyzed using binary logistic regression by including variables with clinical and statistical relevance in univariate analysis (P<0.05) into the multivariate model. Interactions between variables and treatment were assessed by the Gail-Simon test. SPSS 26 (Armonk, NY, USA) and R 4.0.3 (R Core Team) were used for statistical analyses. This study was approved by the institutional review board.
The median age of the 69 patients at enrolment was 73 years (range, 46-86) and 69.6% were male (Online Supplementary Table S1). Based on the World Health Organization 2008 classification, 38 patients (55.1%) had refractory anemia with ring sideroblasts. Conventional karyotype was classified as favorable in 59 of 68 patients (86.8%) according to the classical IPSS. The median number of mutations in each patient was two (range, 0-6). Mutations in SF3B1 and TET2 were detected in 52 (75.4%) and 34 (49.3%) patients, respectively. Lenalidomide and lenalidomide plus epoetin β were administered to 31 and 38 patients, respectively. After completion of 16 weeks of study treatment, 7 of 31 (22.6%) and 21 of 38 (55.3%) patients achieved a HI-E (P=0.006). Comparison of response according to baseline clinical parameters showed a significantly higher frequency of elevated ASC specks (defined as above the median level, 71.4% vs. 34.1%, P=0.002) but less frequent elevation of serum erythropoietin level (defined as >200 mU/mL, 28.6% vs. 60.0%, P=0.029) in responders. Although limited by sample size, a higher frequency of elevated ASC specks was consistently found in responders compared to non-responders of each treatment arm (lenalidomide, 57.1% vs. 29.2%, P=0.210; lenalidomide plus epoetin β, 76.2% vs. 41.2%, P=0.046). DNMT3A was more frequently mutated in responders, but the difference was not statistically significant (28.6% vs. 12.2%, P=0.120). Other baseline parameters, including bone marrow blast percentage, karyotype classification and numbers of mutations, were also not significantly different between responders and non-responders (Table 1). In the multivariate analysis including ASC specks and serum erythropoietin, and adjusted for DNMT3A mutational status1,12 and treatment arm, both elevated ASC specks (odds ratio [OR]=4.963, 95% confidence interval [95% CI]: 1.445-17.045, P=0.011) and serum erythropoietin (OR=0.119, 95% CI: 0.025-0.561, P=0.007) were independently associated with HI-E. As expected, combined treatment remained significant (OR=6.535, 95% CI: 1.622-26.334, P=0.008). Of note, there was no significant interaction between each of these two biomarkers and treatment arm. Of 56 patients with both biomarkers available at inclusion, elevation in ASC specks showed a sensitivity and specificity of 71.4% and 74.3%, respectively, to predict HI-E, and addition of serum erythropoietin could improve the specificity to 88.6% with a reduction of sensitivity to 42.9%. No response (0.0%) was observed in patients with low ASC specks plus elevated serum erythropoietin, while the response rate was 69.2% in those with elevated ASC specks plus low serum erythropoietin (P<0.001) (Figure 1).
Figure 1.
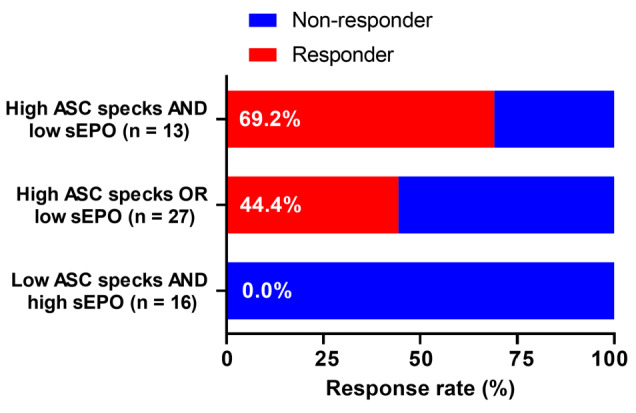
Erythroid response stratified by status of biomarkers. ASC: apoptosis- associated speck-like protein containing a CARD; sEPO, serum erythropoietin.
Ineffective erythropoiesis is a hallmark of lower-risk MDS, and NLRP3 inflammasome-directed pyroptosis serves as a common underlying driver licensed by both the extrinsic proinflammatory cytokine milieu and intrinsic somatic mutations.3,4 Compared to single-agent treatment, lenalidomide with recombinant erythropoietin produces a higher rate of erythroid response.1,2 Our study showed that elevation of ASC specks, a specific and measurable surrogate of pyroptosis, was independently predictive of this response. Moreover, the lower serum erythropoietin in responders may similarly reflect suppression of erythropoietin liberation in response to anemia by pyroptotic inflammatory proteins. Levels of the myeloid-related inflammatory protein S100A9 increase directly with ASC specks in lower-risk MDS, and similarly serve as an index of the extent of medullary pyroptosis. S100A9 suppresses erythropoietin release in vitro in HepG2 hepatoma cells and its levels in lower-risk MDS patients correlate inversely with serum erythropoietin concentration, supporting the notion that inflammatory cytokines also suppress erythropoietin production in vivo.13 These observations suggest that patients with greater medullary inflammasome activation, identified by the dual pyroptotic biomarkers (ASC specks and erythropoietin), may represent a distinct subset of patients among those with lower-risk MDS who could benefit more from treatment with lenalidomide and recombinant erythropoietin. Mechanistically, lenalidomide was shown to reduce the steady-state S100A9 production by peripheral blood mononuclear cells from patients with non-del(5q) MDS and diminished the suppression of erythropoietin elaboration by S100A9.13 It could also stabilize the erythropoietin receptor by inhibiting the E3 ubiquitin ligase RNF41, to strengthen erythropoietin receptor signaling.14 Practically, ASC speck is a relatively novel biomarker that is not yet available as a routine diagnostic test. Additional studies are required to identify a clinically applicable cutoff to specifically recognize lower-risk MDS with inflammasome activation. Patients with these characteristics may also be optimal candidates for NLRP3 or other inflammasome-targeted therapy. In particular, targeting interleukin-1β represents a promising approach given the successful experience of interleukin-1β blockade (e.g., by canakinumab, an interleukin- 1β neutralizing monoclonal antibody) in conditions with NLRP3 inflammasome activation, such as cryopyrin- associated periodic syndrome and Schnitzler syndrome. 15 We recently launched a phase Ib/II trial (NCT04798339) to evaluate canakinumab plus recombinant erythropoietin in lower-risk MDS patients in whom prior treatment with an erythropoiesis-stimulating agent failed. This trial may provide more information on inflammasome- targeted therapies in MDS patients in the near future.
Supplementary Material
References
- 1.List AF, Sun Z, Verma A, et al. Lenalidomide-epoetin alfa versus lenalidomide monotherapy in myelodysplastic syndromes refractory to recombinant erythropoietin. J Clin Oncol. 2021;39(9):1001-1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toma A, Kosmider O, Chevret S, et al. Lenalidomide with or without erythropoietin in transfusion-dependent erythropoiesis-stimulating agent-refractory lower-risk MDS without 5q deletion. Leukemia. 2016;30(4):897-905. [DOI] [PubMed] [Google Scholar]
- 3.Sallman DA, List A. The central role of inflammatory signaling in the pathogenesis of myelodysplastic syndromes. Blood. 2019; 133(10):1039-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basiorka AA, McGraw KL, Eksioglu EA, et al. The NLRP3 inflammasome functions as a driver of the myelodysplastic syndrome phenotype. Blood. 2016;128(25):2960-2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen L, Chen JY, Huang YJ, et al. The augmented R-loop is a unifying mechanism for myelodysplastic syndromes induced by highrisk splicing factor mutations. Mol Cell. 2018;69(3):412-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Broz P, Dixit VM. Inflammasomes: mechanism of assembly, regulation and signalling. Nat Rev Immunol. 2016;16(7):407-420. [DOI] [PubMed] [Google Scholar]
- 7.Lu A, Magupalli VG, Ruan J, et al. Unified polymerization mechanism for the assembly of ASC-dependent inflammasomes. Cell. 2014;156(6):1193-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rowczenio DM, Pathak S, Arostegui JI, et al. Molecular genetic investigation, clinical features, and response to treatment in 21 patients with Schnitzler syndrome. Blood. 2018;131(9):974-981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lachmann HJ, Lowe P, Felix SD, et al. In vivo regulation of interleukin 1beta in patients with cryopyrin-associated periodic syndromes. J Exp Med. 2009;206(5):1029-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Basiorka AA, McGraw KL, Abbas-Aghababazadeh F, et al. Assessment of ASC specks as a putative biomarker of pyroptosis in myelodysplastic syndromes: an observational cohort study. Lancet Haematol. 2018;5(9):e393-e402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee HM, Kim JJ, Kim HJ, Shong M, Ku BJ, Jo EK. Upregulated NLRP3 inflammasome activation in patients with type 2 diabetes. Diabetes. 2013;62(1):194-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chesnais V, Renneville A, Toma A, et al. Effect of lenalidomide treatment on clonal architecture of myelodysplastic syndromes without 5q deletion. Blood. 2016;127(6):749-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cluzeau T, McGraw KL, Irvine B, et al. Pro-inflammatory proteins S100A9 and tumor necrosis factor-α suppress erythropoietin elaboration in myelodysplastic syndromes. Haematologica. 2017; 102(12):2015-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basiorka AA, McGraw KL, De Ceuninck L, et al. Lenalidomide stabilizes the erythropoietin receptor by inhibiting the E3 ubiquitin ligase RNF41. Cancer Res. 2016;76(12):3531-3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jesus AA, Goldbach-Mansky R. IL-1 blockade in autoinflammatory syndromes. Annu Rev Med. 2014;65:223-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.