Abstract
Background
Umbilical venous catheters (UVCs) are often used in ill neonates. Infection related to the use of these catheters may cause significant morbidity and mortality. The use of prophylactic antibiotics has been advocated for newborns with umbilical venous catheters in order to reduce the risk of colonisation and acquired infection. Prophylactic antibiotics may be effective in preventing catheter‐related blood stream infection, but may have the undesirable effect of promoting the emergence of resistant strains of micro‐organisms.
Objectives
The primary objective was to assess whether prophylactic antibiotics in neonates with UVCs reduce mortality and morbidity. In separate comparisons, we planned to review two different policies regarding the prophylactic use of antibiotics in neonates with umbilical venous catheters: 1) Among neonates with UVCs, a policy of prophylactic antibiotics for the duration of catheterization (or other fixed duration of antibiotic treatment) versus placebo or no treatment; 2) Among neonates with UVCs who had been started on antibiotics at the time of catheterization, but whose initial cultures to rule out sepsis are negative, a policy of continuing versus discontinuing prophylactic antibiotics.
Search methods
We searched MEDLINE (January 1966 to April 2005), CINAHL (1982 to April 2005), the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2005). This search was updated in November 2010.
Selection criteria
Randomised controlled trials or quasi‐randomised trials in which newborn infants with UVCs are randomised to receive prophylactic antibiotics versus placebo or no treatment.
Data collection and analysis
Two reviewers independently assessed trial quality.
Main results
One poor quality study met the criteria for inclusion in this review. Twenty‐nine term infants, who had UVCs inserted specifically for transfusion procedures for hyperbilirubinaemia or polycythaemia, allocated non‐randomly (alternate allocation) to treatment (n = 15) or control (n = 14) groups. Those in the treatment group received penicillin and gentamicin for three days. 5/15 infants given antibiotics and 5/14 control infants having positive blood cultures three days after catheter insertion. All positive blood cultures were considered contaminated, due to lack of corroborating clinical and haematological evidence of infection. Therefore, no infants were identified with evidence of septicaemia.
Authors' conclusions
There is insufficient evidence from randomised trials to support or refute the use of prophylactic antibiotics when UVCs are inserted in newborn infants. There is no evidence to support or refute continuing antibiotics once initial cultures rule out infection in newborn infants with UVCs.
Plain language summary
Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical venous catheters
There is insufficient evidence from randomised trials to either support or refute the routine use of preventive antibiotics in newborn babies with umbilical vein catheters. Sick newborn babies occasionally require the insertion of an umbilical vein catheter (a special tube) that goes into the vein in the umbilicus (belly button). This allows fluid and medicines to be given. Some people believe that antibiotics should be given to all babies with umbilical vein catheters in order to reduce the chance of infection occurring. However, antibiotics can have unwanted effects. The reviewers found insufficient evidence to either support or refute the routine use of antibiotics for all babies with umbilical vein catheters.
Background
Description of the condition
Umbilical venous catheters are commonly used in the management of newborn infants who are preterm or have other potentially life‐threatening illness. The use of central venous catheters is recognised as a risk factor for nosocomial infection (Adams‐Chapman 2002; Chien 2002; Nagata 2002; Stoll 2002). It is unclear whether umbilical venous catheters are an independent risk factor for late‐onset sepsis. Stoll (Stoll 2002) analysed numerous factors in a multivariate model and did not find umbilical venous catheters to be an independent significant risk. However, Chien (Chien 2002), on behalf of the Canadian Neonatal Network, concluded that umbilical venous catheters are a significant risk factor. Hyperalimentation with parenteral nutrition is an indication for the use of umbilical venous catheters, and is also a risk factor for nosocomial infection (Adams‐Chapman 2002). Nosocomial infection may cause significant morbidity and mortality (Stoll 2002). Morbidity may include increased duration of respiratory illness, including chronic lung disease, and need for respiratory support (Stoll 2002; Ogawa 1999); increased length of hospital stay (Stoll 2002; Isaacs 2003); and impaired neurodevelopmental outcome (Stoll 2004). The extent of the problem of infection related to umbilical venous catheters is largely unknown due to the widespread use of antibiotics in the population of infants who have umbilical venous catheters.
Patients requiring umbilical venous catheters may, by virtue of their underlying illness, have impaired defence mechanisms ‐ both local and systemic. Prematurity is recognised as a risk factor for late onset sepsis (Dear 1999). Preterm neonates are at high risk of infection because of impaired immunity and umbilical venous catheters may further increase this risk because they are foreign bodies.
Description of the intervention
It is common practice in neonatal units to start antibiotics in infants with respiratory distress and suspected infection, or in those delivered following preterm labour. Many of these infants will have an umbilical venous catheter inserted. It is not clear whether antibiotics should be discontinued if no infection is proven. It has been common practice in some neonatal units that if the infant has an umbilical venous catheter then antibiotics be continued in order to reduce the rate of colonisation of the umbilicus and likewise reduce the risk of acquired infection.
How the intervention might work
Prophylactic antibiotics may be effective in preventing catheter‐related blood stream infection (CRBSI), but may have the undesirable effect of promoting the emergence of resistant strains of micro‐organisms (Freij 1999). A policy of prophylactic antibiotic use should take into account this possibility, and has been used as a basis for arguing against its implementation (Isaacs 2000; Isaacs 2003). Promotion of the emergence of resistant strains of organisms may vary between different antibiotics.
Why it is important to do this review
A recent Cochrane systematic review on the use of prophylactic antibiotics for neonates with umbilical artery catheters showed that there is no evidence from randomised trials to support or refute the use of prophylactic antibiotics when using umbilical artery catheters in newborn infants (Inglis 2004).
Objectives
The primary objective was to assess whether prophylactic antibiotics, in neonates with umbilical venous catheters, reduce mortality and morbidity. Morbidity included proven septicaemia, clinical septicaemia, and suspected septicaemia. Septicaemia was as defined in individual studies.
In separate comparisons, we planned to review two different policies regarding the prophylactic use of antibiotics in neonates with umbilical venous catheters:
1) Among neonates with umbilical venous catheters, a policy of prophylactic antibiotics for the duration of catheterization (or other fixed duration of antibiotic treatment) versus placebo or no treatment. This addresses the question of whether or not neonates with umbilical venous catheters, who do not have clinical or laboratory evidence of infection at that time, should be routinely started on antibiotics at the time of catheterization.
2) Among neonates with umbilical venous catheters who had been started on antibiotics at the time of catheterization, but whose initial cultures to rule out sepsis are negative, a policy of continuing versus discontinuing prophylactic antibiotics. This addresses the question of whether or not antibiotics should routinely be stopped at the time rule out sepsis cultures are reported as negative.
Data permitting, subgroup analyses were planned to determine whether results differ by: gestational age (e.g. preterm versus term, < 28 weeks gestational age (GA) or not); type of antibiotic (e.g. penicillins, macrolides, aminoglycosides, cephalosporins, or combinations).
Methods
Criteria for considering studies for this review
Types of studies
We planned to include the following: randomised controlled trials in which either individual newborn infants or clusters of infants are randomised to receive prophylactic antibiotics versus placebo or no treatment; some types of non‐randomised trials, i.e. quasi‐randomised trials, in which either individual newborn infants or clusters of infants are allocated to receive prophylactic antibiotics versus placebo or no treatment.
Trials where the unit of allocation is the catheter (in which case different catheters within the same patient might be managed differently) were not included.
Trials where the cluster unit is time were not included (as this would not allow the assessment of antibiotic resistance).
Types of participants
Neonates with umbilical venous catheters. The standard definition of "neonate" was used i.e. up to 28 days of age.
Types of interventions
Any antibiotic, or combination of antibiotics, versus placebo or no treatment. This could include: 1) a policy of all neonates with umbilical venous catheters having antibiotics compared with placebo or no treatment; or 2) a policy of neonates with umbilical venous catheters continuing on antibiotics, once initial cultures to rule out sepsis are negative, compared with ceasing antibiotics and continuing on placebo and/or no treatment.
Types of outcome measures
Primary outcomes
Mortality (neonatal, at hospital discharge, or at one year, eighteen months, two years, or five years).
Proven septicaemia (blood culture positive) or either suspected septicaemia or clinical septicaemia (however defined in individual studies)
Septicaemia might occur more than once in the same patient and may be reported in several different ways. We planned to tabulate this as a categorical outcome (e.g. proportion of patients having one or more episodes).
Secondary outcomes
Chronic lung disease (oxygen requirement at 36 weeks post‐menstrual age).
Duration of ventilation (hours or days).
Duration of respiratory support (hours or days).
Duration of oxygen therapy (hours or days).
Duration of hospital stay (days).
Number of resistant organisms (i.e. species) identified per time period per infant or per cluster unit.
Neurodevelopmental outcome (cerebral palsy, sensorineural hearing loss, visual impairment and/or developmental delay will be considered as separate components ‐ at one year, eighteen months, two years, or five years).
Search methods for identification of studies
See: Cochrane Neonatal Review Group search strategy
The standard search strategy for the Cochrane Neonatal Review Group was used. We searched MEDLINE from 1966 to April 2005, CINAHL from 1982 to April 2005, and the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2005) using the following strategy:
MeSH search terms ("Umbilicus" AND "Catheterization") OR the textwords ("umb$" AND ("cathet$" OR "cannul$")) OR "UVC" OR "umbilical vein catheter" OR "umbilical venous catheter" AND MeSH search term "Infant, newborn" OR the textwords "neonat$" OR "infant"' AND MeSH search term "Antibiotics" OR the textword "antibiotic" AND MeSH search terms "Chemoprevention" OR "Antibiotic Prophylaxis" OR the textword "prophyl$".
We also searched previous reviews (including cross references). Searches were not restricted to publications in the English language or published data.
In November 2010 we updated the search as follows: MEDLINE (search via PubMed), CINAHL, EMBASE and CENTRAL (The Cochrane Library) were searched from 2005 to 2010. Search terms: ((Umbilicus AND Catheterization) OR (umbi* AND (cathet* OR cannul*)) OR UVC OR umbilical vein catheter OR umbilical venous catheter) AND ((infant, newborn[MeSH] OR newborn OR neon* OR neonate OR neonatal OR premature OR low birth weight OR vlbw OR LBW) AND (randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized[tiab] OR placebo[tiab] OR clinical trials as topic[mesh] OR randomly[tiab] OR trial[ti]) NOT (animals[mh] NOT humans[mh]))
In November 2010 clinicaltrials.gov and controlled‐trials.com were also searched for relevant studies.
Data collection and analysis
We used the standard methods of the Cochrane Collaboration and its Neonatal Review Group.
Selection of studies
The two authors worked independently to search for and assess trials for inclusion and methodological quality.
Data extraction and management
The authors extracted data independently. Differences were resolved by discussion. We contacted the second author of the study by Bhatt et al (Bhatt 1970) for additional information or data.
Assessment of risk of bias in included studies
The methodological quality of the included studies were assessed using the following key criteria: allocation concealment (blinding of randomisation), blinding of intervention, completeness of follow‐up, and blinding of outcome measurement/assessment. For each criterion, assessment was yes, no, can't tell. Two review authors separately assessed each study. Any disagreement was resolved by discussion. This information was added to the Characteristics of Included Studies table.
In addition, for the update in 2010, the following issues were evaluated and entered into the Risk of Bias table:
1) Sequence generation (checking for possible selection bias). Was the allocation sequence adequately generated? For each included study, we categorized the method used to generate the allocation sequence as:
‐ adequate (any truly random process e.g. random number table; computer random number generator);
‐ inadequate (any non random process e.g. odd or even date of birth; hospital or clinic record number);
‐ unclear.
(2) Allocation concealment (checking for possible selection bias). Was allocation adequately concealed? For each included study, we categorized the method used to conceal the allocation sequence as:
‐ adequate (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
‐ inadequate (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
‐ unclear.
(3) Blinding (checking for possible performance bias). Was knowledge of the allocated intervention adequately prevented during the study? At study entry? At the time of outcome assessment? For each included study, we categorized the methods used to blind study participants and personnel from knowledge of which intervention a participant received. Blinding was assessed separately for different outcomes or classes of outcomes. We categorized the methods as:
‐ adequate, inadequate or unclear for participants;
‐ adequate, inadequate or unclear for personnel;
‐ adequate, inadequate or unclear for outcome assessors.
In some situations there may be partial blinding e.g. where outcomes are self‐reported by unblinded participants but they are recorded by blinded personnel without knowledge of group assignment. Where needed “partial” was added to the list of options for assessing quality of blinding.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations). Were incomplete outcome data adequately addressed? For each included study and for each outcome, we described the completeness of data including attrition and exclusions from the analysis. We noted whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported or supplied by the trial authors, we re‐included missing data in the analyses. We categorized the methods as:
‐ adequate (< 20% missing data);
‐ inadequate (≥ 20% missing data):
‐ unclear.
(5) Selective reporting bias. Are reports of the study free of suggestion of selective outcome reporting? For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found. We assessed the methods as:
‐ adequate (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
‐ inadequate (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
‐ unclear.
(6) Other sources of bias. Was the study apparently free of other problems that could put it at a high risk of bias?
For each included study, we described any important concerns we had about other possible sources of bias (for example, whether there was a potential source of bias related to the specific study design or whether the trial was stopped early due to some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as:
‐ yes; no; or unclear.
If needed, we planned to explore the impact of the level of bias through undertaking sensitivity analyses.
Measures of treatment effect
Analysis of individual trials: For continuous variables such as duration of oxygen therapy, mean differences, and 95% confidence intervals were to be reported. For categorical outcomes such as mortality, the relative risks (RR) and 95% confidence intervals were to be reported.
Unit of analysis issues
Trials where the unit of allocation is the catheter (in which case different catheters within the same patient might be managed differently) were not included.
Assessment of heterogeneity
We estimated the treatment effects of individual trials and examined heterogeneity between trials by inspecting the forest plots and quantifying the impact of heterogeneity using the I2 statistic. If we detected statistical heterogeneity, we planned to explore the possible causes (for example, differences in study quality, participants, intervention regimens, or outcome assessments) using post hoc sub group analyses. We planned to use a fixed effects model for meta‐analysis.
Data synthesis
For pooled results: for continuous variables, weighted mean differences (WMD) and 95% confidence intervals were to be reported. For categorical outcomes, the relative risks (RR) and 95% confidence intervals were to be reported. For significant findings, the risk difference (RD) and number needed to treat (NNT) were also to be reported. Each treatment effect was to be tested for heterogeneity to help determine suitability for pooling of results in a meta‐analysis. The fixed effects model was to be used for meta‐analysis. If there were sufficient included studies, heterogeneity was to be assessed using the I squared test. If statistical heterogeneity was found the authors planned to look for an explanation. If studies with heterogenous results were thought to be comparable, a random effects model was to be used to combine the data.
Subgroup analysis and investigation of heterogeneity
Data permitting, subgroup analyses were planned to determine whether results differ by: gestational age (e.g. preterm versus term, < 28 weeks gestational age (GA) or not); type of antibiotic (e.g. penicillins, macrolides, aminoglycosides, cephalosporins, or combinations).
Sensitivity analysis
Data permitting, a sensitivity analysis was planned to see if results differed by quality of included studies i.e. adequacy of randomisation ‐ quasi randomised versus randomised.
Results
Description of studies
The search strategy identified four potentially eligible reports. Two of the trials (Bard 1973; Cowett 1977) were excluded because they were studies of infants with umbilical artery catheters. Another (Bhatt 1970) was excluded because, as far as we could ascertain, it was a study of arterial catheters. This study was published only in Abstract form and involved 192 infants randomly assigned to treatment (i.e. prophylactic antibiotics) and control groups. The published abstract contained little methodological or outcome data. We contacted one of the authors (JEH) and were advised that no further data was available. The author advised also that, to her knowledge, the study only involved infants with arterial catheters.
The study by Pulido et al (Pulido 1985) was included. The study attempted to address the question of whether term infants with umbilical venous catheters had lower rates of infection when given antibiotic prophylaxis, compared with untreated controls. The study was non‐randomised (quasi‐randomised, using alternate group allocation), was small, of short duration, and involved infants with very specific indications for umbilical venous catheter insertion: i.e. catheters were inserted for transfusion procedures in infants with hyperbilirubinaemia or polycythaemia. There was a wide range of age at enrolment (1 ‐ 10 days). Twenty‐nine term infants with umbilical venous catheters were allocated non‐randomly (quasi‐randomised ‐ alternate allocation) to treatment (n = 15) or control (n = 14) groups. Those in the treatment group received penicillin and gentamicin for three days, but no mention is made of duration of catheterization. It is possible that duration of treatment exceeded duration of catheterization or vice versa. Two peripheral blood cultures were drawn from all study infants three days after catheter insertion. Results were presented as number of positive blood cultures and number of true‐positive blood cultures.
Risk of bias in included studies
There were significant methodological flaws in the only study identified (Pulido 1985) for inclusion in this review:
the study was non‐randomised (quasi‐randomised, using alternate group allocation);
the intervention appears to have been non‐blinded, but the report is not explicit on this matter;
it is unknown whether outcome assessment was blind;
completeness of follow up is unclear;
allocation concealment was not blinded.
Effects of interventions
One study (Pulido 1985) was included in this review.
For primary outcomes:
Proven septicaemia ‐ 5/15 intervention and 5/14 control infants had positive blood cultures three days after UVC insertion. All positive blood cultures were considered contaminated, due to lack of corroborating clinical and haematological evidence of infection. Therefore, no infants were identified with evidence of septicaemia.
Mortality ‐ not assessed/reported.
For secondary outcomes:
Chronic lung disease (oxygen requirement at 36 weeks post‐menstrual age) ‐ not assessed/reported.
Duration of ventilation (hours or days) ‐ not assessed/reported.
Duration of respiratory support (hours or days) ‐ not assessed/reported.
Duration of oxygen therapy (hours or days) ‐ not assessed/reported.
Duration of hospital stay (days) ‐ not assessed/reported.
Number of resistant organisms ‐ not assessed/reported.
Neurodevelopmental outcome ‐ not assessed/reported.
Discussion
This review has attempted to determine whether prophylactic antibiotics are warranted in either of two circumstances: 1. Should infants with umbilical venous catheters be commenced on routine prophylactic antibiotics at the time of catheter insertion? 2. Should infants with umbilical venous catheters, who are commenced on antibiotics pending investigation results, be continued on antibiotics once initial infection is ruled out?
A major limiting factor in trying to determine the place of prophylactic antibiotics in infants with umbilical venous catheters is that catheter placement is quite often undertaken, for ease of fluid and drug administration, in the context of clinical circumstances (e.g. respiratory distress, preterm delivery) which may reflect infection. Newborn infants in such circumstances are usually commenced on antibiotics because their clinical circumstances may indicate infection at the same time that they may lead to the decision to insert an umbilical venous catheter. Because the majority of newborns in whom umbilical venous catheters are placed would be treated in this way, the first scenario described above would be relevant to relatively few newborns. The second scenario described above would be the more common one encountered.
One non‐randomised (quasi‐randomised) trial was found for inclusion in this review. Pulido et al (Pulido 1985) performed a small study on the use of antibiotic prophylaxis in infants undergoing transfusion procedures for hyperbilirubinaemia or polycythaemia via an umbilical venous catheter. The authors conclude that no infant in the study developed septicaemia following the procedure, and that the use of antibiotic prophylaxis is not indicated. A study of this size would have been underpowered to detect anything other than a very large effect. The study covered a period of only two months. It has been noted previously that nosocomial infections can occur in clusters (Adams‐Chapman 2002). If the study under consideration here coincided with a nadir in nosocomial infection, then the resultant underestimation of septicaemia rates in one or both arms of the study could have affected the conclusions. It is difficult to generalise the findings of this study for a number of reasons. Since its publication there have been significant changes in the practice of neonatal medicine, including use and maintenance of vascular access devices. The use of umbilical venous catheters in this study was for specific indications and the background risk of infection in the study subjects may have been low. The average age at catheter insertion in this study was probably significantly greater than would be seen in most units today. Given the poor methodological quality of the study, we cannot rely on the results provided with regard to effects on infection rates.
Quasi‐randomised trials are inherently prone to bias, and their results should be interpreted with caution. The alternate group assignment makes the upcoming treatment group allocation predictable, and that is a problem in the case of every eligible infant. Also, if two equally eligible infants present at the same time with different risks for infection a clinician might (consciously or not) enter them into the study in the order that would allow the infant that they believed should receive antibiotics to get antibiotics. If a large number of infants were enrolled in this way, serious imbalance in the treatment groups with respect to factors affecting the outcome would result (Hennekens 1987).
In order to justify the use of prophylactic antibiotics (rather than treatment of infection as it arises) in infants with umbilical venous catheters, there should be evidence that the benefit outweighs the harm. This should include an adequate assessment not only of short term outcomes such as infection rate and duration of hospital admission, but also of long term outcomes such as mortality, long term respiratory morbidity and neurodevelopmental outcome.
Theoretical concerns about the potential harm of prophylactic antibiotic use include emergence of resistant strains of bacteria, superinfection and drug toxicity. Altered antibiotic resistance patterns may be of consequence not only to the individual in whom prophylactic antibiotics are used but also to other patients within the hospital setting and to the broader community.
Authors' conclusions
Implications for practice.
There is insufficient evidence from published clinical trials to support or refute the use of prophylactic antibiotics when inserting umbilical venous catheters in newborn infants.
There is no evidence from clinical trials to support or refute continuing antibiotics once initial cultures rule out infection in newborn infants with umbilical venous catheters.
Implications for research.
If prophylactic antibiotics are to be considered when inserting umbilical venous catheters, then good quality randomised controlled trials are required to show that their benefits outweigh the harms. Unfortunately, most newborn infants who have umbilical venous catheters inserted are likely to receive antibiotics to cover possible infection and a randomised controlled trial may not be practicable or ethical.
A more pressing question is whether infants who initially receive antibiotics for presumed infection should be continued on antibiotics once initial cultures rule out infection. Good quality randomised controlled trials are required to address this issue.
What's new
| Date | Event | Description |
|---|---|---|
| 7 December 2010 | New search has been performed | This review updates the existing review "Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical venous catheters" published in the Cochrane Database of Systematic Reviews (Inglis 2005). One trial was added to the excluded studies Seliem 2010. No changes to conclusions. |
History
Protocol first published: Issue 2, 2005 Review first published: Issue 4, 2005
| Date | Event | Description |
|---|---|---|
| 16 October 2008 | Amended | Converted to new review format. |
Acknowledgements
We thank Dr Luis Altamirano for his translation of the study by Pulido et al (Pulido 1985).
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
Data and analyses
Comparison 1. Prophylactic antibiotics versus no antibiotics.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Septicaemia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
1.1. Analysis.
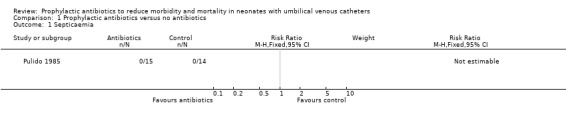
Comparison 1 Prophylactic antibiotics versus no antibiotics, Outcome 1 Septicaemia.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Pulido 1985.
| Methods | This non‐randomised (quasi‐randomised ‐ alternate allocation) study took place between July and August 1984 at a regional neonatal intensive care unit in Chile. Enrolled infants were allocated alternately into intervention and control groups. All subjects had 2 peripheral blood cultures and a full blood count (FBC) drawn three days following the procedure. At this stage antibiotics were discontinued if there was deemed to be no clinical or laboratory (i.e. FBC) evidence of infection. Blood cultures were read at 7 days. Septicaemia was defined as positive blood culture combined with clinical and laboratory evidence of infection. Intervention was probably not blinded. Completeness of follow up is not addressed. It is unclear whether outcome assessment was blinded. | |
| Participants | Twenty‐nine infants were studied. All were term. Twenty‐three underwent exchange transfusion for hyperbilirubinaemia, and 6 underwent globulophoresis (partial exchange transfusion) for hematocrit greater than 0.70. All infants had their procedures performed via umbilical venous catheter. Infants requiring repeat procedures were excluded from the study (the number of such infants, if any, is not specified). There were 15 infants in the intervention group and 14 in the control group. | |
| Interventions | Infants in the intervention group (n = 15) received penicillin and gentamicin for 3 days following the procedure. Control infants (n = 14) received no antibiotics. No placebo was used. Other care was similar. | |
| Outcomes | Septicaemia: based on positive blood culture (3 days after UVC insertion) in conjunction with clinical and haematological evidence of infection. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | This non‐randomised (quasi‐randomised ‐ alternate allocation) study took place between July and August 1984 at a regional neonatal intensive care unit in Chile. Enrolled infants were allocated alternately into intervention and control groups. |
| Allocation concealment? | High risk | |
| Blinding? All outcomes | Unclear risk | Intervention was probably not blinded. It is unclear whether outcome assessment was blinded. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Completeness of follow up is not addressed. |
FBC = full blood count and examination
UVC = umbilical venous catheter
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bard 1973 | Study of umbilical artery catheters. |
| Bhatt 1970 | Published in Abstract form only. The second author was contacted and could offer no further data, except that the study involved infants with arterial, rather than venous, catheters. |
| Cowett 1977 | Study of umbilical artery catheters. |
| Seliem 2010 | Wrong intervention (not systemic antibiotics) |
Contributions of authors
Preparation of protocol ‐ GDI Revision of protocol ‐ MWD Searches for published and unpublished studies ‐ GDI and MWD Inclusion assessments ‐ GDI and MWD Validity assessments ‐ GDI and MWD Data collection ‐ GDI and MWD Data entry ‐ GDI and MWD Data Analysis ‐ GDI and MWD Preparation of review ‐ GDI Revision of review ‐ MWD
The November 2010 update was conducted centrally by the Cochrane Neonatal Review Group staff (Yolanda Montagne, Diane Haughton, and Roger Soll). This update was reviewed and approved by GDI.
Sources of support
Internal sources
Grantley Stable Neonatal Unit, Royal Brisbane and Women's Hospital, Brisbane, Australia.
Dept of Paediatrics and Child Health, University of Queensland, Brisbane, Australia.
Neonatal Unit, Department of Pediatrics, McMaster University, Hamilton, Canada.
External sources
No sources of support supplied
Declarations of interest
None
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Pulido 1985 {published data only}
- Pulido N, Montesinos A, Arriaza M, Esparza P. Prophylactic use of antibiotics in umbilical catheterization in newborn infants [Uso profilactico de antibioticos en cateterismo umbilical en recien nacidos]. Revista Chilena de Pediatria 1985;56:247‐9. [PubMed] [Google Scholar]
References to studies excluded from this review
Bard 1973 {published data only}
- Bard H, Albert G, Teasdale F, Doray B, Martineau B. Prophylactic antibiotics in chronic umbilical artery catheterization in respiratory distress syndrome. Archives of Disease in Childhood 1973;48:630‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhatt 1970 {published data only (unpublished sought but not used)}
- Bhatt DR, Hodgman JE, Tatter D. Evaluation of prophylactic antibiotics during umbilical catheterization in newborns. Clinical Research 1970;18:217. [Google Scholar]
Cowett 1977 {published data only}
- Cowett RM, Peter G, Hakanson DO, Stern L, Oh W. Prophylactic antibiotics in neonates with umbilical artery catheter placement: a prospective study of 137 patients. The Yale Journal of Biology and Medicine 1977;50:457‐63. [PMC free article] [PubMed] [Google Scholar]
Seliem 2010 {published data only}
- Seliem W, Abdel‐Hady H, El‐Nady G. Amikacin‐heparin lock for prevention of catheter‐related bloodstream infection in neonates with extended umbilical venous catheters use: A randomized controlled trial. Journal of Neonatal‐Perinatal Medicine 2010;3:33‐41. [Google Scholar]
Additional references
Adams‐Chapman 2002
- Adams‐Chapman I, Stoll BJ. Prevention of nosocomial infections in the neonatal intensive care unit. Current Opinion in Pediatrics 2002;14:157‐64. [DOI] [PubMed] [Google Scholar]
Chien 2002
- Chien L, MacNab Y, Aziz K, Andrews W, McMillan DD, Lee SK, Canadian Neonatal Network. Variations in central venous catheter‐related infection risks among Canadian neonatal intensive care units. Pediatric Infectious Disease Journal 2002;21:505‐11. [DOI] [PubMed] [Google Scholar]
Dear 1999
- Dear P. Infection in the newborn. In: Rennie JM, Roberton NRC editor(s). Textbook of Neonatology. 3rd Edition. Edinburgh: Churchill Livingstone, 1999:1109‐202. [Google Scholar]
Freij 1999
- Freij BJ, McCracken Jr GH. Acute infections. In: Avery GB, Fletcher MA, MacDonald MG editor(s). Neonatology: pathophysiology and management of the newborn. 5th Edition. Philadelphia: Lippincott Williams & Wilkins, 1999:1189‐230. [Google Scholar]
Hennekens 1987
- Hennekens CH, Buring JE. Intervention studies. In: Mayrent SL editor(s). Epidemiology in medicine. Boston: Little, Brown & Company, 1987:178‐212. [Google Scholar]
Inglis 2004
- Inglis GDT, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical artery catheters. Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD004697.pub2] [DOI] [PubMed] [Google Scholar]
Isaacs 2000
- Isaacs D. Rationing antibiotic use in neonatal units. Archives of Disease in Childhood. Fetal and neonatal edition 2000;82:F1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Isaacs 2003
- Isaacs D, Australasian Study Group for Neonatal Infections. A ten year, multicentre study of coagulase negative staphylococcal infections in Australasian neonatal units. Archives of Disease in Childhood. Fetal and neonatal edition 2003;88:F89‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nagata 2002
- Nagata E, Brito AS, Matsuo T. Nosocomial infections in a neonatal intensive care unit: incidence and risk factors. American Journal of Infection Control 2002;30:26‐31. [DOI] [PubMed] [Google Scholar]
Ogawa 1999
- Ogawa Y, Shimizu H, Takasaki J, Nakamura T. Strategy for the prevention and treatment of chronic lung disease of the premature infant. Pediatric Pulmonology 1999;Supp 18:212‐5. [DOI] [PubMed] [Google Scholar]
Stoll 2002
- Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Late‐onset sepsis in very low birth weight neonates: The experience of the NICHD Neonatal Research Network. Pediatrics 2002;110:285‐91. [DOI] [PubMed] [Google Scholar]
Stoll 2004
- Stoll BJ, Hansen NI, Adams‐Chapman I, Fanaroff AA, Hintz SR, Vohr B, Higgins RD. Neurodevelopmental and growth impairment among extremely low‐birth‐weight infants with neonatal infection. JAMA 2004;292:2357‐65. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Inglis 2005
- Inglis GDT, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical venous catheters. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD005251.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


