Abstract
SARS-CoV-2 is primarily known to cause respiratory symptoms. However, in this global COVID-19 pandemic, we have come across many extrapulmonary manifestations during and in the immediate post-COVID phase such as gastrointestinal symptoms, kidney and liver injury, myocardial dysfunction and acute coronary syndromes, and neurological, thromboembolic, dermatological, and musculoskeletal disorders. We present 2 such unusual cases of post-COVID complications—diffuse panniculitis and inflammatory myositis, as well as their clinical and FDG PET/CT imaging features.
Key Words: FDG PET/CT, COVID-19, viral, polymyositis, lobular panniculitis
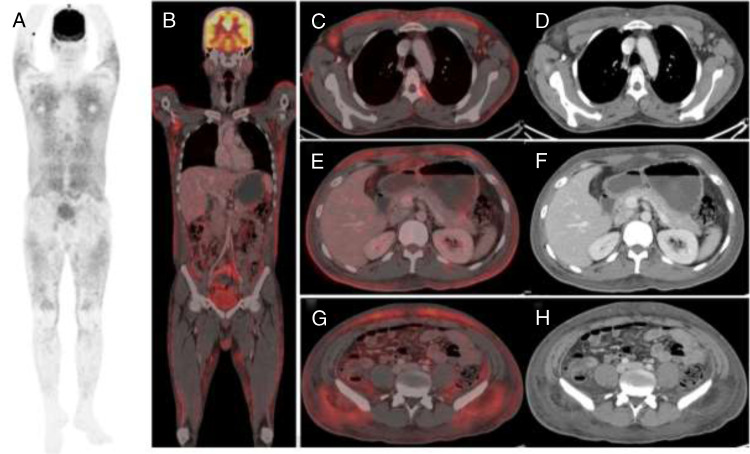
FIGURE 1.
A 32-year-old man, a week after recovery from COVID-19 (RT-PCR negative), developed multiple small, painful red cutaneous nodules over the bilateral shin and upper limbs associated with high-grade fever (101–102°F), as well as mild swelling along the abdominal wall, which raised suspicion of erythema nodosum. WBCs showed rising trend (10,940/μL). Symptoms showed no relief to antibiotic doxycycline. Blood cultures revealed no growth, with normal chest x-ray. The patient was referred for 18F-FDG PET/CT scan to evaluate infective focus. PET/CT MIP (A), coronal (B), transaxial fused (C, E, G), and axial CECT images (D, F, H) showed FDG-avid patchy areas of subcutaneous and visceral fat stranding all over the body, appearing inflammatory suggesting diffuse panniculitis. Excisional biopsy from abdominal fat revealed neutrophilic lobular panniculitis. Lobular panniculitis is a neutrophilic infiltration of fat lobules, not associated with vasculitis, and considered an atypical rare subcutaneous variant of Sweet syndrome.1 It may be idiopathic or associated with hematological malignancies, drugs, systemic disorders, or viral infections, such as SARS-CoV-2 in our case. Excessive cytokine (IL-4, IL-5) production and exaggerated neutrophilic host immune response to COVID-19 infection lead to neutrophilic infiltration in subcutaneous fat.2,3 Patient showed good symptomatic response to Wysolone 40 mg.
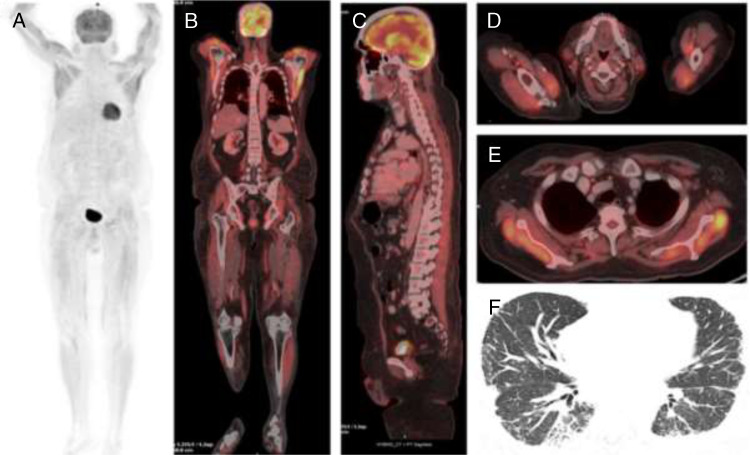
FIGURE 2.
A 57-year-old man, 2 months after recovery from COVID-19 pneumonia, complained of bilateral lower-limb weakness progressively involving bilateral upper limbs, with difficulty in lifting hands over head. No muscular pain nor skin changes observed. Urinary bladder and bowel function were normal. He was on tapering steroids and nintedanib for post-COVID lung fibrosis. Initially steroid-induced myopathy was suspected. 18F-FDG PET/CT scan was advised to rule out paraneoplastic syndrome. PET/CT MIP (A), coronal (B), sagittal (C), and transaxial fused (D and E) images showed abnormal increased FDG uptake in multiple muscle regions, more intense in the upper-limb muscles, suggesting possibility of inflammatory polymyositis (PM) and changes of interstitial lung disease with septal thickening and bronchiectatic changes in the right lower lobe (axial CT image F). Creatine phosphokinase level was raised (3736 IU/L). Antinuclear and anti–smooth muscle antibodies were negative. Anti–Jo-1 myositis-specific antibody was positive. It is commonly seen in PM associated with viral infections, directed against antihistidyl-tRNA synthetase.4 Presence of anti–Jo-1 myositis-specific antibody is associated with features of myositis, interstitial lung disease (as seen on our case),4,5 arthritis, fever, Raynaud phenomena, and mechanic's hand, referred to as antisynthetase syndrome. Electromyography nerve conduction velocity study further confirmed our diagnosis of inflammatory myositis, and biopsy was not performed. Patient was started on mycophenolate mofetil and showed improvement. PM, an autoimmune idiopathic inflammatory myopathy, is triggered by malignancies, drugs, and viral infections6,7 like SARS-CoV-2 in our case. Proposed immune-mediated mechanism of muscle damage by SARS-CoV-2 is secondary to cytokine storm inflammatory response and cellular protein alteration by virus causing loss of tolerance of self-antigens and autoantibody production.7,8 In view of ongoing COVID-19 pandemic, it is important for nuclear medicine physicians to be familiar with presentation and imaging findings of inflammatory syndromes associated with SARS-CoV-2–like myositis and panniculitis on 18F-FDG PET/CT scan to aid interpretation, diagnosis, and patient care.
Footnotes
Conflicts of interest and sources of funding: none declared.
Authors' contribution: P.M. contributed to the concepts, design, definition of intellectual content, literature search, clinical studies, data acquisition, data analysis, manuscript preparation, manuscript editing, manuscript review, and as a guarantor. S.D. contributed to the concepts, design, definition of intellectual content, literature search, data acquisition, data analysis, manuscript preparation, manuscript editing, manuscript review, and as a guarantor. R.D., R.R., D.S., and S.N. contributed to the concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Contributor Information
Divya Shivdasani, Email: drdivyashivdasani@gmail.com.
Debdip Roy, Email: debdiproy9@gmail.com.
Rachita Rungta, Email: rachitarungta7@gmail.com.
Shreya Dang, Email: dr.shreyadang2312@gmail.com.
Natasha Singh, Email: drnatasha_singh@yahoo.com.
REFERENCES
- 1.Chan MP. Neutrophilic panniculitis algorithmic approach to a heterogeneous group of disorders. Arch Pathol Lab Med. 2014;138:1337–1343. [DOI] [PubMed] [Google Scholar]
- 2.Leis-Dosil VM, Sáez Vicente A, Lorido-Cortés MM. Paniculitis eosinofílica secundaria a infección por COVID-19. Actas Dermosifiliogr (Engl Ed). 2020;111:805–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taşkın B Vural S Altuğ E, et al. COVID-19 presenting with atypical Sweet's syndrome. J Eur Acad Dermatol Venereol. 2020;34:e532–e652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mileti LM Strek ME Niewold TB, et al. Clinical characteristics of patients with anti-Jo-1 antibodies: a single center experience. J Clin Rheumatol. 2009;15:254–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beydon M Chevalier K Al Tabaa O, et al. Myositis as a manifestation of SARS-CoV-2. Ann Rheum Dis. 2020;annrheumdis-2020-217573. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Q Shan KS Minalyan A, et al. A rare presentation of coronavirus disease 2019 (COVID-19) induced viral myositis with subsequent rhabdomyolysis. Cureus. 2020;12:e8074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang H Charmchi Z Seidman RJ, et al. COVID-19-associated myositis with severe proximal and bulbar weakness. Muscle Nerve. 2020;62:E57–E60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramani SL Samet J Franz CK, et al. Musculoskeletal involvement of COVID-19: review of imaging. Skeletal Radiol. 2021;50:1763–1773. [DOI] [PMC free article] [PubMed] [Google Scholar]