Abstract
An effective referral system ensures that there is a close relationship among all levels of health care, and individuals can receive the best possible care. The main purpose of the present study was to summarize studies that have addressed factors affecting the successful implementation of the referral system. A scoping review was performed to identify English and Farsi papers that were indexed in PubMed, Scopus, Science Direct, Trip Database, Cochrane Library, Embase, Google Scholar, SID, and Magiran until November 2020. Data was collected from the included studies by a reviewer and was checked by a second reviewer the collected data was analyzed using narrative methods. About 1245 relevant studies were identified in the first stage. After checking titles and abstracts, 63 studies were included. The factors that affected the referral system were classified in 4 themes and fourteen subthemes including technology (electronic referral, coordination, response and feedback), processes (effectiveness, efficiency), organizational (management, policy and planning, rules and regulations), patient centered individual (insurance coverage, social capital, transportation, awareness, attitude, satisfaction, and social influence). Therefore, a wide range of factors are affecting the performance of referral systems. For implementing an effective referral system, it is necessary to consider these factors.
Keywords: Implementation, referral system, scoping review
Introduction
Providing primary health-care is a way to improve the fairness of access to health-care and the efficiency of resource use.[1] Reinforcing primary health-care (PHC) is, also, essential for accessibility and quality of health-care. One of the main elements of primary health-care is the referral system, in which patients can access care in health centers before higher levels of care such as second and third level hospitals are offered.[2] An efficient referral system is an important part of a well-functioning health-care system at the local, provincial, and national level of a country.[3]
According to the definition of the World Health Organization (WHO), “referral can be defined as a process in which a health worker at a one level of the health system, having insufficient resources (drugs, equipment, skills) to manage a clinical condition, seeks the assistance of a better or differently resourced facility at the same or higher level to assist in, or take over the management of, the client's case”.[4]
In order to refer the patients from environmental centers properly, three levels have been considered, that is the first and most pervasive level of the health system is primary care. The second level of the system is secondary hospital care, and finally, the third level, which is the highest level of care offers specialized facilities for the treatment of patients.[5,6]
An effective referral system ensures that there is a close relationship among all levels of health-care, and that individuals receive the best possible care ever. It also contributes to the cost-effective use of hospital services and PHC. Therefore, a high percentage of patients referred to outpatient clinics in the second level centers can be properly cared for in PHC centers at a lower overall cost.[4] The referral system can be deemed as a measure of the overall performance of the health system and reflects the ability of governments to manage all subsystems and actors involved in the referral process.[7]
To implement an effective and efficient referral system, a combination of factors such as coordination between referral and referral centers, mechanisms/tools/working methods, communication and feedback systems, transportation system, executive protocols, trained personnel, efficient teamwork among all levels, integrated information recording system, accountability, and monitoring performance improvement are required.[5] Various factors affect the effective implementation of the referral system. Different studies have examined each part or level of factors affecting the referral system and to the best knowledge of the authors, there might be no studies that examined the factors affecting the implementation of the referral system at all three levels. Therefore, we decided to design a study using the scoping review method. The main purpose of this study was to identify and analyze studies that have addressed the factors affecting the successful implementation of the referral system. This study helps managers and policy makers of the health system to have an overview of the factors influencing the successful implementation of the referral system.
Methods
A scoping review was performed to identify English and Farsi papers that were indexed in PubMed, Scopus, ScienceDirect, Trip Database, Cochrane Library, Embase, Google Scholar, SID, and Magiran until November 2020 using appropriate search strategies. Data was collected from the included studies by a reviewer and was checked by a second reviewer.
Titles, abstracts, and when necessary the full texts of the retrieved papers were checked to include relevant studies.
Empirical studies that explored factors that are affecting the performance of a referral system were included.
The collected data from the included studies about any factor that could affect the referral systems was analyzed using narrative methods.
Results
A total of 1245 studies were retrieved. After screening the titles, abstracts and the full text of selected papers, finally, a total of 63 studies were included [Figure 1 and Table 1].
Figure 1.
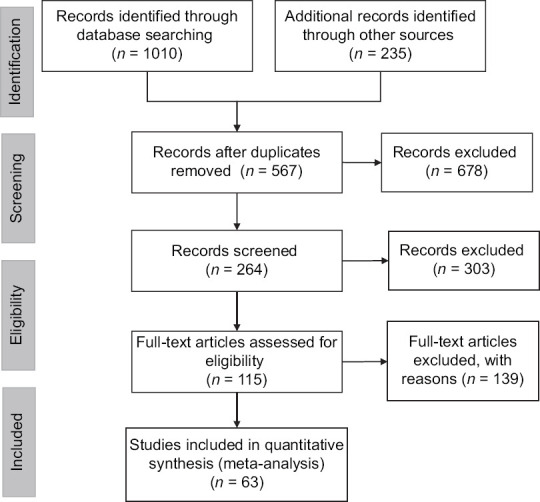
PRISMA diagram for study selection in the scoping review
Table 1.
List of databases and number of articles found
| Databases | ‘Referral System’:ti Referral system[Title] |
|---|---|
| https://pubmed.ncbi.nlm.nih.gov | 199 |
| www.scopus.com | 310 |
| www.sciencedirect.com | 59 |
| www.tripdatabase.com | 80 |
| www.cochranelibrary.com | 26 |
| www.embase.com | 316 |
| www.sid.ir | 11 |
| www.magiran.com | 9 |
| Total | 1010 |
The characteristics of the 63 included studies are described in Appendix 1.
Appendix 1.
Characteristics of the studies included in the scoping review (n=63)
| First author and reference | Year | Country | Type of study | Objective |
|---|---|---|---|---|
| Abate, B[24] | 2010 | Ethiopia | Mixed-methods retrospective | To assess information use in patient’s referral system, current referral process, and problems associated with documentation. |
| Abodunrin, OL[25] | 2010 | Nigeria | Cross-sectional | To determine the awareness and perception of adult residents in Ilorin toward the policy on appropriate utilization of levels of health facilities through referral system. |
| Abrahim, O[2] | 2015 | Ethiopia | Cross-sectional | To examine what percentage of patients had either sought prior care or had been referred to the present facility and identify demographic and clinical factors associated with having sought prior care or having been referred. |
| Afsar, HA[26] | 2003 | Pakistan | Cross-sectional | To estimate the proportion of patient referral and to identify the factors associated with unsuccessful referral in Karachi, Pakistan. |
| Akande, TM[27] | 2004 | Nigeria | Cross-sectional | To examine referral system in Nigeria with a study on new patients seen in a tertiary health facility. |
| Alkinaidri, A[28] | 2018 | Saudi Arabia | Case study | To explore using Lean Six Sigma as a way to improve healthcare referral system. |
| Alshami, M[29] | 2014 | Saudi Arabia | Case study | To report on the experiences of implementing the EHALA electronic referral system at a local Saudi hospital. |
| Amoah, PA[30] | 2017 | Ghana | Qualitative deductive approach | To examine how the resources embedded in both structural and cognitive aspects of social relationships influence knowledge of, and adherence to, referral policy. |
| Bailey, PE[17] | 2019 | Ghana | Secondary analysis | To assess the relationship between referral and facilities’ readiness to treat complications at each level of the health system in Ghana. Also investigate other facility characteristics associated with referral. |
| Belway, D[31] | 2008 | Canada | Retrospective, stratified cohort | To determine the association between transport intervals and intensive care unit (ICU), and hospital length of stay and hospital mortality at the receiving hospital. |
| Bossyns, P[32] | 2006 | Niger | Cross-sectional | To establish a benchmark for referral rates in rural Niger so as to allow interpretation of routine referral data to assess the performance of the referral system in Niger. |
| Calfee, RP[23] | 2012 | USA | Retrospective cohort | To systematically examine the impact of insurance status on access to and utilization of elective specialty hand surgical care. |
| Chambers, EC[33] | 2015 | USA | Quasi-experimental | To examine the effectiveness of referring patients with prediabetes and determine whether referrals were sustained after the intervention. |
| Clarke, A[34] | 2010 | USA and UK | Systematic review | To assess effectiveness of guidelines for referral of elective surgical assessment. |
| Daniels, AA[35] | 2020 | Ghana | Qualitative | To examine the lived experiences of patients, healthcare providers, and relatives of patients on the referral system. |
| Dennison, J[10] | 2006 | UK | Pilot | To assess the effect of the electronic surgical referral service on patient waiting times and attendance rates. |
| Dogba, M[36] | 2011 | Mali | Cross-sectional | To assess, in women presenting with an obstetric complication: 1) the effects of the point of entry into the referral system on joint mother-newborn survival; and 2) the effects of the configuration of healthcare team at the CHCs on joint mother-newborn survival. |
| Doumouras, AG[37] | 2017 | Canada | longitudinal analysis | To determine the impact on referral rates to bariatric surgery after converting to an online referral system from a fax-based system. |
| Ebrahimiadib, N[38] | 2016 | Iran | Prospective observational | To compare the efficacy of an internet-based versus traditional referral system for retinopathy of prematurity (ROP) screening in Iran. |
| Esan, O[16] | 2016 | Nigeria | Cross-sectional | To observe the prevalence of deficiencies in the referral letters to a department of psychiatry in a Nigerian teaching hospital. |
| Eskandari, M[19] | 2013 | Iran | Qualitative | To describe barriers of health-care process in rural societies in Iran. |
| Fernández-Méndez, R[39] | 2020 | UK | Retrospective cohort | To determine the impact of introducing a Web-based, electronic referral (eReferral) system to a specialized neuro-oncology center, using a service-developed proforma, in terms of waiting times and information completeness. |
| Fyie, K[21] | 2014 | Canada | Mixed-methods retrospective | To describe referral processes and practices, and their impact on the waiting time from referral to consultation for TJA. |
| Give, C[40] | 2019 | Mozambique | Qualitative | To explore barriers and enablers of referral within the lens of complex adaptive health systems. |
| Handayani, PW[8] | 2018 | Indonesia | Quantitative data processing | To identify a user acceptance model for the health referral system in Indonesia. |
| Hill, VA[41] | 2000 | UK | Quasi-experiment | To undertake an audit to assess the impact of the guidelines with a follow-up audit in 1995 |
| Idowu, AO[42] | 2018 | Nigeria | Retrospective | To ascertain the frequency of requests for endocrine consultations, to determine the sources of consults, the common cases referred, the reasons behind consultations, and the outcome of patients who benefited from endocrine consultations. |
| Islam, S[43] | 2015 | Bangladesh | Retrospective cohort | To assess the patient referral system in the urban DOTS programme in Dhaka, Bangladesh, with a view to identifying problems and solutions. |
| Jaturapatporn, D[44] | 2006 | Thailand | short article | To present the current situation of family medicine in Thailand. |
| Kalhor, R[45] | 2014 | Iran | Cross-sectional descriptive | To investigate human resources situation of the family physician program in 6 pilot cities in Khuzestan province in the southwest of Iran. |
| Kavosi, Z[46] | 2018 | Iran | Cross-sectional | To evaluate the overall performance of the referral system in Fars Province in 2015. |
| Kennedy, A[20] | 2012 | UK | Cohort | To adapt the 2002 Scottish Referral Guidelines for suspected squamous cell carcinoma of the head and neck (SCCHN) as a set of “alarm symptoms.” |
| Khayyati, F[22] | 2011 | Iran | Quasi-experiment | To evaluate the impact of the program on accessibility of the services, case finding, patient referral, feedback process and insurance coverage in the rural health units. |
| Kim, E-H[47] | 2010 | USA | Survey | To present findings and observations on the factors affecting the clinical acceptance of our web-based referral system. |
| Kim, Y[18] | 2009 | USA | Survey | To assess the impact of electronic referrals on workflow and clinical care. |
| Kim-Hwang, JE[48] | 2010 | USA | Quasi-experiment | To determine the impact of eReferral (compared with paper-based referrals) on specialty referrals. |
| Kongnyuy, EJ[49] | 2008 | Malawi | Retrospective review | To obtain feasibility of using criteria-based audit to improve a district referral system. |
| Li, C[50] | 2011 | China | Literature review | To examine the health insurance reform experiences in Thailand with respect to the objective of universal coverage and attempt to draw out some lessons for China, taking into account China’s practical context. |
| Lim, K[51] | 2018 | Korea | Survey | To examine the current hospice referral scenario for terminally ill cancer patients and create a data form to collect hospice information and a modified health information exchange (HIE) form for a more efficient referral system for terminally ill cancer patients. |
| MacGregor, D[11] | 2009 | Canada | Pilot | To evaluate the implementation of a web-based referral system |
| Majoko, F[52] | 2005 | Zimbabwe | Cohort | To determine the prevalence of antenatal and intra-partum referrals, compliance with advice and perinatal outcomes in referred pregnant women in Gutu district, Zimbabwe. |
| Mehet, J[53] | 2018 | UK | Review | To explore the literature evidence surrounding the clinical impact of the NORSe referral system and analogous models. |
| Nsigaye, R[54] | 2009 | Tanzania | Qualitative | To design and assess a referral system to link persons diagnosed at a voluntary counselling and testing (VCT) clinic in a rural district in northern Tanzania with a government-run HIV treatment clinic in a nearby city. |
| Oates, J[14] | 2000 | Canada | Observational cohort | To assess the association between patient-centered communication in primary care visits and subsequent health and medical care utilization. |
| Oliva, X[55] | 2013 | Spain | Survey | - To improve the resolution of endocrine diseases in primary care - To decrease inadequate visits to specialized care |
| Omole, VN[6] | 2017 | Nigeria | Cross-sectional | To probe for information toward improving the quality of the referral process and the health system |
| Prathiba, P[56] | 2020 | India | Descriptive | To assess the gaps in the referral of patients from primary care arriving at the obstetric EMS of a tertiary hospital. |
| Prinja, S[57] | 2014 | India | Time series analysis | To evaluate the referral transport system in Haryana |
| Quinn, GP[58] | 2011 | USA | Pilot | To develop a referral system to increase the likelihood that patients of childbearing age with newly diagnosed cancer receive timely information about fertility and reduce the burden oncologists may feel when discussing and exploring fertility preservation options with their patients. |
| Scheibe, MM[59] | 2015 | USA | Retrospective | To evaluate the use and impact of a novel electronic referral (eReferral) system in rheumatology in a safety net health system. |
| Shams, A[60] | 2013 | Iran | Descriptive analytic | To determine factors affecting the fulfillment of referral system process |
| Shephard, E[15] | 2018 | UK | Survey | To improve patient safety and junior doctor efficiency in the referral process. |
| Tuot, DS[61] | 2015 | USA | Quasi-experiment | To examine how specialists leverage an electronic referral and consultation system to deliver specialty care. |
| Williams, L[62] | 2012 | Ireland | Survey | To improve patient care by reducing unnecessary outpatient visits, avoid emergency department presentations, shorten waiting times, and alleviate the administrative burden on healthcare staff. |
| Woodward, M[12] | 2020 | UK | Quasi-experiment | To apply a human factors/ergonomics (HFE) approach to place analysis of local workflow and user engagement central to the development of a new regional electronic referral system. |
| Yu, W[63] | 2017 | China | Survey | To explore the effect of doctors’ and patients’ practices and attitudes on their willingness for downward referral and the relationship between downward referral and sociodemographic characteristics. |
| Zanolini, A[64] | 2016 | Zambia | Pilot | To pilot a peer referral intervention in which circumcision clients were offered incentives for referring their peers for circumcision. |
| Zhang, X[13] | 2018 | China | Cross-sectional | To identify the key nodes that affect patient satisfaction during the referral service process. |
| Kamau, KJ[5] | 2017 | Kenya | Cross-sectional | To establish challenges facing implementation of the referral system for quality health-care services in Kiambu County, Kenya. |
| Chitsa, B[65] | 2019 | Malawi | Qualitative | To investigate the factors that affect management of the referral system at the primary level of health-care in Zomba district in Malawi. |
| Chiou BL[66] | 2020 | Taiwan | Retrospective cohort | To explore the economic burdens of hip fracture surgery in patients referred to lower-level medical institutions and to evaluate how referral systems affect costs and outcomes of hip fracture surgery. |
| Corwin P[67] | 2014 | New Zealand | Quasi-experiment | To assess whether feedback improves the quality of referral letters from general practice to secondary care and how electronic referrals affect the quality of referral letters. |
| Jiwa M[68] | 2004 | UK | Non-randomised control trial | To determine if written feedback about the contents of GP referral letters mediated by local peers was acceptable to GPs and how this feedback influenced the content and variety of their referrals. |
| Azamar-Alonso, A[9] | 2019 | Canada | Scoping review | To review the evidence base for the effectiveness and cost-effectiveness of eReferral systems. |
The factors that affected the implementation of a referral system were classified into 4 groups (themes) including organization, technology, process, and individual.[8] Each theme then were classified into several subthemes, so that a total of 14 subthemes were identified [Appendix 2]. Appendix 3 presents further information about the identified subthemes. A brief summary of each of them and their subthemes is provided below.
Appendix 2.
Subthemes Description
| Subthemes Description | Subthemes | Themes |
|---|---|---|
| Technology | Electronic Referrals | The automation of the referral process in which appointment and other information regarding the consultation are transferred between two or more health-care providers.[9] |
| Responsiveness | The transition process on referrals can be done in a fast and responsive manner, according to the needs of the patient.[8] | |
| Coordination | Care coordination involves managing and integrating care across levels of the system and across time in order to ensure patient information is communicated at the right time and to the right people to facilitate the delivery safe, appropriate, and effective care.[69] | |
| Feedback | The process by which a response includes actions taken and actions to be taken is given by the referral recipient to the referring person | |
| Process | Effectiveness | Referrals are based on scientific knowledge and implemented according to applicable process standards.[8] |
| Efficiency | Provide adequate services to fulfill the needs of patients, thus avoiding multiple services.[8] | |
| Organization | Management, policy and planning | Efficient and effective use of material and human resources.[70] |
| Patient Centricity | Health officials prioritize health services for the needs and referral preferences of patients and their families.[8] | |
| Regulation | Written rules governing the procedures and processes of health services.[8] | |
| Social influence | The influence of a patient’s decision in approving referrals made by the health facility caused by the surrounding environment (e.g., family, friends, and relatives).[8] | |
| Insurance | An economic device transferring risk from an individual to a company and reducing the uncertainty of risk via pooling.[71] | |
| Transport | Moving or transferring the patient from one place to another | |
| Social capital | Networks together with shared norms, values, and understandings that facilitate cooperation within or among groups.[72] | |
| Awareness, attitude and satisfaction | Ability to directly know and perceive, to feel, or to be cognizant of events.[73] | A combination of beliefs and emotions that prepare the patient in advance to look at others or different groups in a positive or negative way.[74] Patients’ emotions, feelings, and their perception of delivered healthcare services.[75] |
Appendix 3.
Findings and subthemes pertaining to the theme
| Findings of Studies | Subthemes | Themes |
|---|---|---|
| Technology | Electronic referral | The electronic referral system was associated with a reduction in unnecessary follow-up for patients. eReferral facilitated communication between referring clinicians and a specialist reviewer prior to the appointment.[48] |
| Electronic referrals improved health-care access and quality.[18] | ||
| Electronic referral system increases efficiency compared to paper referral system due to patients’ choice of date and time.[10] | ||
| Compared to the paper referral process, the implementation of the electronic referral system increases the number of referrals[37] | ||
| Implementation of electronic referral leads to improved quality, completeness of clinical referral information, and efficiency in the referral process.[12] | ||
| The electronic referral system allows specialists to make a pre-consultation exchange to identify the need for consultation.[59] | ||
| Use of the Electronic referrals system has improved efficiency in the referral process and has reduced the work associated with the previous paper based referral system. It has also enhanced communication between the healthcare provider and the patient and family and has improved the security and confidentiality of patient information management.[11] | ||
| Redesigning a paper-based referral system to an electronic referral system is more efficient and safer for patients.[15] | ||
| Specialists can use electronic referral and consultation systems to enhance specialty care delivery with consultative communication that is highly rated by primary care providers (PCPs).[61] | ||
| An internet-based registration system for Retinopathy of Prematurity (ROP) screening resulted in fewer cases of delayed first examination and resulted in fewer babies with advanced ROP.[38] | ||
| The electronic referral system is effective in improving the relationship between primary care and specialists, and reducing the waiting time.[9] | ||
| Coordination | Overcrowding of the tertiary health facilities with problems that can be managed at the lower levels.[27] | |
| Strengthening the connection between health lefts and hospitals increases the efficiency of primary care.[2] | ||
| A strong collaboration is needed between teaching hospitals and other stakeholders in the referral chain to foster good referral practices and healthcare delivery.[35] | ||
| Improving capacity building at the primary health-care delivery, referral hierarchy, document quality, and emergency transport mechanism is critical for patients.[56] | ||
| Properly functioning health lefts (primary level) can take care of the vast majority of patients’ problems.[32] | ||
| Health Information Technology (HIT) enabled pre-consultation exchange facilitates communication between referring physicians and specialists.[59] | ||
| Interventions such as using standard templates for referral letters may facilitate more effective communication.[16] | ||
| Electronic referrals improve and accelerate the communication process between PHC and the hospital, as well as improve the continuity of patient care.[29] | ||
| Advances in the structure of the referral system to improve the quality of health-care require coordination among the three levels of the referral system.[19] | ||
| The advantages of using an electronic communication system with primary care are: allowing quick answers to general practitioners’ questions, starting treatment on time, and reducing the number of patients referring to hospital clinics.[62] | ||
| By reducing inappropriate initial visits from primary care to secondary care, the capacity to solve patients’ problems in primary care increases.[55] | ||
| Responsiveness | The referral system reduces the delay of seeking care and makes it possible for individuals to monitor access to treatment.[14] | |
| Increasing health information on the web makes people more aware of their health conditions and treatment options, and also quickly responds to patients’ online requests, significantly increasing patient satisfaction.[47] | ||
| Providing patient information allows specialists to fulfill their obligations and make informed decisions about maintaining the patient’s health, thereby improving the full care continuum.[58] | ||
| Web-based electronic referrals perform significantly better than other types of referrals, with less waiting time and more complete patient information. Wider use of eReferrals is an important first step in simplifying intensive care pathways and providing excellent care.[39] | ||
| Feedback | Postoperative feedback saves on medical costs.[66] | |
| Feedback improves the quality of referral letters.[67] | ||
| Feedback improves the content of referral letters and may also affect the type of patients referred for investigation by specialists.[68] | ||
| Process | Effectiveness | Continuous training of general practitioners leads to improving the quality of referral system services.[20] |
| Supporting referral system reforms with regard to the training of health workers; Implementation of referral policies, guidelines, and structural and standard forms is recommended.[6] | ||
| Establishing referral guidelines is effective in reducing unnecessary patient referrals.[46] | ||
| Efficiency | Training of family physicians can increase the appropriate referral rate.[44] | |
| Modification of electronic health system along with provider training intervention is a way to identify and refer eligible patients.[33] | ||
| Improving management skills of Lady Health Workers (LHWs) for simple medical problems reduces the number of referrals. Also, strengthen communication and counseling skills to reduce a significant portion of unsuccessful referrals.[26] | ||
| To facilitate patient access to physicians who have contracts with the Family Physician Program and Referral Systems at Level 2 and 3; is essential to adopt policies to attract specialists and improve their maintenance[45] | ||
| The family physician program has a positive effect on the performance of health units in terms of access to physicians and midwives.[22] | ||
| The efficacy of the referral services is determined by the gatekeepers’ management of the referral system at the primary-level hospital and the allocation and management of bed resources at the higher-level hospital.[13] | ||
| The efficiency of the referral system is reduced by not following the referral recommendations by the health team.[52] | ||
| Organization | Management, policy and planning | The implementation of Lean Six Sigma can lead to a significant improvement in the healthcare referral system.[28] |
| Improving referral conditions (by increasing access through communication and transportation systems) and managing disease complications (increasing preparedness) enhance the quality of care and also make the referral system more effective and efficient.[17] | ||
| Government efforts and investments are needed to make the referral system useful in practice.[51] | ||
| Improving infrastructure, implementing a standard referral system monitoring toolkit, training curricula for health workers on referral policies and guidelines, and adequate funding for monitoring and evaluation are recommended for successful referral system implementation.[5] | ||
| The government should enhance the availability of needed resources such as diagnostic equipment, skilled personnel, referral ambulances, drugs, and communication technology to facilitate patient referrals.[65] | ||
| Regulation | Guidelines for elective surgical referral can improve appropriateness of care by improving prereferral investigation and treatment.[34] | |
| Immediately after the introduction of referral guidelines, appropriate referrals increased by 40%, but this increase was not sustained after 2 years. Therefore, continuous training of general practitioners regarding referral guidelines is essential.[41] | ||
| Improving referral processes and reducing diversity between clinics improved patient access.[21] | ||
| Appropriate operating guidelines and proper monitoring system help to increase information provision and utilization process.[24] | ||
| Criteria-based audits can improve the ability of a regional referral system to deal with emergencies in countries with limited resources.[49] | ||
| Possible modification of referral guidelines will improve referral quality.[20] | ||
| Patient Centricity | Patient-lefted communication improves health and increases the efficiency of care by reducing diagnostic tests and the number of referrals.[14] | |
| Individual | Insurance | Patients with worse economic conditions face barriers to accessing intensive care. Also, patients who are not covered by insurance receive less care.[23] |
| The family physician program has a positive effect on insurance coverage.[22] | ||
| One of the reasons for the lack of continuity of care is the insurance coverage of patients.[42] | ||
| The provision of primary health-care and referral system should be strengthened in cooperation with health insurance system reforms.[50] | ||
| Social capital | Both the cognitive and structural forms of social capital significantly affect people’s ability and willingness to adhere to the referral system process. Cautious interaction with social capital will make it a potentially powerful tool for understanding gaps and improving the effectiveness of referral policy.[30] | |
| Transport | Transport intervals are independently associated with ICU/CCU and hospital lengths of stay at the receiving hospital for critically ill adults transferred to referral lefts.[31] | |
| Distance traveled, health team skill configuration and Point of care affect patient survival.[36] | ||
| Improving the transportation system for emergency referrals is essential to ensure patient safety during transport.[35] | ||
| Referral transport services have a positive effect on increasing institutional deliveries.[57] | ||
| Awareness, attitude, and satisfaction | Awareness and satisfaction with the way primary health-care services are provided in urban communities and motivation in rural communities affect the implementation of the referral system process.[60] | |
| Providers and decision makers can use information technology and guidebooks about the referral system to facilitate communication and standardization between health lefts, raise public awareness, and encourage patients to use the referral system.[8] | ||
| Proper counseling and consideration of patients’ preferences during referral is essential to remove barriers to accessing adherence to treatment and improving treatment outcome.[43] | ||
| The higher the level of education, people have more knowledge about the referral system and are more likely to have a correct understanding of the referral system.[25] | ||
| Social influence | Active community engagement will be the key to stimulating better use of referral services.[40] | |
| Social media minimizes delays in receiving specialist advice and management, especially in acute situations.[53] | ||
| Motivation and encouragement of family and friends is one of the factors in following up the referral.[64] |
Technology
Electronic referral: Electronic referral system minimizes unnecessary follow-up for patients, increases quality, reduces waiting time, increases access, efficiency, the number of referrals, and confidentiality of patient information, improves the relationship between first level and specialized care and increases safety for patients, and consequently, enhances efficiency.
Coordination: Coordination between levels of health services in the referral system increases the efficiency of primary care, improves capacity building in the first level of services, increases the quality of documents, adheres to the referral hierarchy, improves the continuity of patient care, improves the quality of health-care, and reduces the number of patients who are referred to hospital clinics.
Responsiveness: The referral system reduces the delay of seeking care and makes it possible to monitor access to treatment for individuals. Prompt handling of patients’ online requests significantly increases patient satisfaction. The widespread use of e-Referrals is, thus, an important step in simplifying intensive care pathways and providing excellent care.
Feedback: Proper feedback saves on medical costs and increases the quality of referral letters. Feedback may also affect the type of patients referred by specialists.
Processes
Effectiveness: Continuous training of general practitioners, supporting the referral system reforms, implementing referral policies, and creating standard guidelines and structural forms are among the factors affecting the effectiveness of the referral system.
Efficiency: Factors affecting the efficiency of the referral system include training of family physicians, modification of electronic health registration system, improvement of management skills, taking measures to attract specialists and improve their maintenance, availability of doctors and midwives, and management of the gatekeepers of the referral system.
Organization
Management, policy-making and planning: Policy-making and planning of the referral system are government efforts and investments, implementation of the lean Six Sigma, improvement of referral conditions (increasing access through communication and transportation systems), preparedness, infrastructure improvement, implementation of standard referral system monitoring toolkit, curriculum to educate health workers about referral policies and guidelines, and adequate funding for monitoring and evaluation that are evident in the findings mentioned in the management studies.
Rules and Regulations: Rules and regulations of the referral system that were found in the studies are as follows: notifying referral instructions, improvement of referral processes, minimizing the diversity between clinics, notifying operational instructions, appropriate monitoring system, criteria-based, audit and possible revisions to referral guidelines.
Patient-centered communication: Patient-centered communication improves community health and increases the effectiveness of care by reducing diagnostic tests and the number of referrals.
Individual
Insurance coverage, social capital, transportation, awareness, attitude, satisfaction, and social influence are individual factors that each affect the referral system in some way.
Discussion
This study provides a comprehensive information about factors that are affecting the referral systems. There was a wide range of variations in the study design, setting, methods, and findings.
For example, Handayani et al.[8] examined the factors affecting patients’ referral approval and showed that rules and regulations, data security, integration, accountability, effectiveness, efficiency, personal beliefs, and social impact significantly on referral approval.
One of the factors affecting the referral system is the implementation of the electronic referral system that has been studied many times. For example, Azamar-Alonso et al. (2019)[9] conducted a scoping review, which securitized the electronic referral system in health-care, and showed that the electronic referral system was effective in improving the relationship between first-level and specialized care and minimizing waiting time.
According to the obtained evidence, implementation of the electronic referral system,[10,11,12] the relationship between health centers and hospitals,[2] gatekeeping management of Referral system,[13] and patient-centered communication[14] are among the factors that result in increasing the efficiency of the referral system. Factors that increase the efficacy of the referral system include the implementation of the electronic referral system,[15] the use of standard templates for referral letters,[16] and increasing access through communication and transportation systems.[17] Also, the factors that ended up with increasing the quality of referral system services are the implementation of electronic referral system,[12,18] coordination among the three levels of referral system,[19] continuing education of general practitioners,[20] increasing access through communication and transportation systems,[17] and possible modification of referral instructions.[20] In addition, factors that are involved in increased access to referral system services include the implementation of electronic referral system.[18] Improving referral processes and reducing diversity between clinics[21] implement a family physician program[22] and insurance coverage.[23]
The evidence presented in this study showed that each of the factors can have a quantitative and qualitative impact on the successful implementation of the referral system. Hence, identifying the factors that affect the referral system helps to take these factors into account in national and local policies. Monitoring centers and institutions may, in turn, consider factors and analysis of support data to provide a fair and equitable service to all people. The results of this study can provide relatively complete information about the factors affecting the referral system and may be considered in future planning and policy-making. We were also able to identify areas of interest for publishing research on factors affecting the referral system and to introduce relevant topics for further research.
One of the limitations of this study, though, was that many articles addressed the subject of the referral system and the subject dispersion was of higher frequency. As there was a great variety between the factors affecting the implementation of the referral system, the factors affecting the referral system overlapped in some instances.
Conclusion
The present scoping review used a systematic approach to identify studies that have addressed the factors influencing the implementation of the referral system. The most important factors influencing the referral system are divided into 4 main themes (technology, organizational, processes, and individual). Each of these issues includes a number of subthemes that managers and policymakers need to consider before and during the implementation of the referral system. This study paves the way for further interpretation of the existing literature on the factors affecting the referral system. As many factors affect the successful implementation of the referral system and the context of different countries, more studies are needed to decide how different factors affect the implementation of the referral system in different communities.
Key Message
Factors affecting the successful implementation of the referral system in 4 dimensions are as follows: in the technology dimension (electronic referral system, coordination between levels of health services, responsiveness, and appropriate feedback), in the process dimension (effectiveness and efficiency in actions and programs), in the organizational dimension (management, policy-making and planning, rules and regulations, and patient-centered), and in the individual dimension (insurance coverage, social capital, transportation, awareness, attitude, satisfaction, and social influence).
Ethical approval
The study was approved by the local ethical committee (code: IR.TUMS.VCR.REC.1399.329), and the Helsinki Declaration was respected across the study.
Authors’ contributions
All authors contributed to this project and article equally. All authors read and approved the final manuscript.
Financial support and sponsorship
This study is part of the PhD thesis of the first author who is supported by Tehran University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Van Lerberghe W. The World Health Report 2008: Primary Health Care: Now More than Ever. World Health Organization. 2008 [Google Scholar]
- 2.Abrahim O, Linnander E, Mohammed H, Fetene N, Bradley E. A patient-centered understanding of the referral system in Ethiopian primary health care units. PLoS One. 2015;10:e0139024. doi: 10.1371/journal.pone.0139024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Legodi TL, Wolvaardt JE. A blank page: Feedback from first referral hospitals to primary health care clinics. South African Family Practice. 2015;57:282–5. [Google Scholar]
- 4.WHO. Management of health facilities: Referral systems. World Health Organization. 2014 [Google Scholar]
- 5.Kamau KJ, Osuga BO, Njuguna S. Challenges facing implementation of referral system for quality health care services in Kiambu county, Kenya. Health Syst Policy Res. 2017;4:1–8. [Google Scholar]
- 6.Omole VN, Mora AT, Yunusa IU, Audu O, Jatau AI, Gobir AA. Knowledge, attitude, and perception of the referral system among tertiary health-care workers in Kaduna metropolis, Nigeria. Int J Med Sci Public Health. 2017;6:1481–9. [Google Scholar]
- 7.Harahap NC, Handayani PW, Hidayanto AN. Barriers and technologies of maternal and neonatal referral system in developing countries: A narrative review. Informatics in Medicine Unlocked. 2019;15:100184. [Google Scholar]
- 8.Handayani PW, Saladdin IR, Pinem AA, Azzahro F, Hidayanto AN, Ayuningtyas D. Health referral system user acceptance model in Indonesia. Heliyon. 2018;4:e01048. doi: 10.1016/j.heliyon.2018.e01048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azamar-Alonso A, Costa AP, Huebner L-A, Tarride J-E. Electronic referral systems in health care: A scoping review. Clinicoecon Outcomes Res. 2019;11:325–33. doi: 10.2147/CEOR.S195597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dennison J, Eisen S, Towers M, Clark CI. An effective electronic surgical referral system. Ann R Coll Surg Engl. 2006;88:554–6. doi: 10.1308/003588406X130642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacGregor D, Parker S, MacMillan S, Blais I, Wong E, Robertson CJ, et al. Innovation in managing the referral process at a Canadian pediatric hospital. Healthc Q. 2009;12:73–9. doi: 10.12927/hcq.2013.20889. [DOI] [PubMed] [Google Scholar]
- 12.Woodward M, De Pennington N, Grandidge C, McCulloch P, Morgan L. Development and evaluation of an electronic hospital referral system: A human factors approach. Ergonomics. 2020;63:710–23. doi: 10.1080/00140139.2020.1748232. [DOI] [PubMed] [Google Scholar]
- 13.Zhang X, Wang T, Yu Y, Zhao S. Key nodes affecting patient satisfaction in a cross-regional referral service process: An empirical analysis study in Sichuan. BMC Health Serv Res. 2018;18:840. doi: 10.1186/s12913-018-3460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 15.Shephard E, Stockdale C, May F, Brown A, Lewis H, Jabri S, et al. E-referrals: Improving the routine interspecialty inpatient referral system. BMJ Open Quality. 2018;7:e000249. doi: 10.1136/bmjoq-2017-000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Esan O, Oladele O. Referral letters to the psychiatrist in Nigeria: Is communication adequate? Afr Health Sci. 2016;16:1023–6. doi: 10.4314/ahs.v16i4.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailey PE, Awoonor-Williams JK, Lebrun V, Keyes E, Chen M, Aboagye P, et al. Referral patterns through the lens of health facility readiness to manage obstetric complications: National facility-based results from Ghana. Reprod Health. 2019;16:19. doi: 10.1186/s12978-019-0684-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim Y, Chen AH, Keith E, Yee HF, Kushel MB. Not perfect, but better: Primary care providers’ experiences with electronic referrals in a safety net health system. J Gen Intern Med. 2009;24:614–9. doi: 10.1007/s11606-009-0955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eskandari M, Abbaszadeh A, Borhani F. Barriers of referral system to health care provision in rural societies in Iran. J Caring Sci. 2013;2:229. doi: 10.5681/jcs.2013.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kennedy A-M, Aziz A, Khalid S, Hurman D. Do GP referral guidelines really work? Audit of an electronic urgent referral system for suspected head and neck cancer. Eur Arch Otorhinolaryngol. 2012;269:1509–12. doi: 10.1007/s00405-011-1788-3. [DOI] [PubMed] [Google Scholar]
- 21.Fyie K, Frank C, Noseworthy T, Christiansen T, Marshall DA. Evaluating the primary-to-specialist referral system for elective hip and knee arthroplasty. J Eval Clin Pract. 2014;20:66–73. doi: 10.1111/jep.12080. [DOI] [PubMed] [Google Scholar]
- 22.Khayyati F, Motlagh ME, Kabir M, Kazemeini H. The role of family physician in case finding, referral, and insurance coverage in the rural areas. Iran J Public Health. 2011;40:136–9. [PMC free article] [PubMed] [Google Scholar]
- 23.Calfee RP, Shah CM, Canham CD, Wong AH, Gelberman RH, Goldfarb CA. The influence of insurance status on access to and utilization of a tertiary hand surgery referral center. J Bone Joint Surg Am. 2012;94:2177–84. doi: 10.2106/JBJS.J.01966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abate B, Enquselassie F. Information use in patients’ referral system at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2010;48:123–35. [PubMed] [Google Scholar]
- 25.Abodunrin O, Akande T, Osagbemi G. Awareness and perception toward referral in health care: A study of adult residents in Ilorin, Nigeria. Ann Afr Med. 2010;9:176–80. doi: 10.4103/1596-3519.68359. [DOI] [PubMed] [Google Scholar]
- 26.Afsar H, Qureshi A, Younus M, Gulb A, Mahmood A. Factors affecting unsuccessful referral by the lady health workers in Karachi, Pakistan. J Pak Med Assoc. 2003;53:521–8. [PubMed] [Google Scholar]
- 27.Akande T. Referral system in Nigeria: Study of a tertiary health facility. Ann Afr Med. 2004;3:130–3. [Google Scholar]
- 28.Alkinaidri A, Alsulami H. Improving healthcare referral system using lean six sigma. Am J Ind Bus Manag. 2018;8:193–206. [Google Scholar]
- 29.Alshami M, Almutairi S, Househ MS. The implementation experience of an electronic referral system in Saudi Arabia: A case study. Stud Health Technol Inform. 2014;202:138–41. [PubMed] [Google Scholar]
- 30.Amoah PA, Phillips DR. Strengthening the referral system through social capital: A qualitative inquiry in Ghana. Healthcare. 2017;5:80. doi: 10.3390/healthcare5040080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belway D, Dodek PM, Keenan SP, Norena M, Wong H. The role of transport intervals in outcomes for critically ill patients who are transferred to referral centers. J Crit Care. 2008;23:287–94. doi: 10.1016/j.jcrc.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 32.Bossyns P, Abache R, Abdoulaye MS, Miyé H, Depoorter A-M, Van Lerberghe W. Monitoring the referral system through benchmarking in rural Niger: An evaluation of the functional relation between health centres and the district hospital. BMC Health Serv Res. 2006;6:51. doi: 10.1186/1472-6963-6-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chambers EC, Wylie-Rosett J, Blank AE, Ouziel J, Hollingsworth N, Riley RW, et al. Increasing referrals to a YMCA-based diabetes prevention program: Effects of electronic referral system modification and provider education in federally qualified health centers. Prev Chronic Dis. 2015;12:E189. doi: 10.5888/pcd12.150294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clarke A, Blundell N, Forde I, Musila N, Spitzer D, Naqvi S, et al. Can guidelines improve referral to elective surgical specialties for adults? A systematic review. BMJ Quality & Safety. 2010;19:187–94. doi: 10.1136/qshc.2008.029918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daniels AA, Abuosi A. Improving emergency obstetric referral systems in low and middle income countries: A qualitative study in a tertiary health facility in Ghana. BMC Health Serv Res. 2020;20:1–10. doi: 10.1186/s12913-020-4886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dogba M, Fournier P, Dumont A, Zunzunegui M-V, Tourigny C, Berthe-Cisse S. Mother and newborn survival according to point of entry and type of human resources in a maternal referral system in Kayes (Mali) Reprod Health. 2011;8:13. doi: 10.1186/1742-4755-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Doumouras AG, Anvari S, Breau R, Anvari M, Hong D, Gmora S. The effect of an online referral system on referrals to bariatric surgery. Surg Endoscopy. 2017;31:5127–34. doi: 10.1007/s00464-017-5578-x. [DOI] [PubMed] [Google Scholar]
- 38.Ebrahimiadib N, Roohipour R, Karkhaneh R, Farahani A, Esfahani MR, Khodabande A, et al. Internet-based versus conventional referral system for retinopathy of prematurity screening in Iran. Ophthalmic Epidemiol. 2016;23:292–7. doi: 10.3109/09286586.2015.1136653. [DOI] [PubMed] [Google Scholar]
- 39.Fernández-Méndez R, Wong MY, Rastall RJ, Rebollo-Díaz S, Oberg I, Price SJ, et al. Improvement of the efficiency and completeness of neuro-oncology patient referrals to a tertiary center through the implementation of an electronic referral system: Retrospective cohort study. J Med Internet Res. 2020;22:e15002. doi: 10.2196/15002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Give C, Ndima S, Steege R, Ormel H, McCollum R, Theobald S, et al. Strengthening referral systems in community health programs: A qualitative study in two rural districts of Maputo Province, Mozambique. BMC Health Serv Res. 2019;19:1–11. doi: 10.1186/s12913-019-4076-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill V, Wong E, Hart C. General practitioner referral guidelines for dermatology: Do they improve the quality of referrals? Clin Exp Dermatol. 2000;25:371–6. doi: 10.1046/j.1365-2230.2000.00665.x. [DOI] [PubMed] [Google Scholar]
- 42.Idowu AO, Adesegun OA, Osonuga A, Osibowale B, Ajiro T, Ngubor TD, et al. Patterns and impact of consultations to an endocrinology unit in a tertiary hospital in southwestern Nigeria. Niger Med J. 2018;59:28–32. doi: 10.4103/nmj.NMJ_167_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Islam S, Hirayama T, Islam A, Ishikawa N, Afsana K. Treatment referral system for tuberculosis patients in Dhaka, Bangladesh. Public Health Action. 2015;5:236–40. doi: 10.5588/pha.15.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jaturapatporn D. Does family medicine training affect the referral pattern of primary care doctors in Thailand? Family Medicine. 2006;38:387–8. [PubMed] [Google Scholar]
- 45.Kalhor R, Azmal M, Kiaei MZ, Eslamian M, Tabatabaee SS, Jafari M. Situational analysis of human resources in family physician program: Survey from Iran. Mater Sociomed. 2014;26:195–7. doi: 10.5455/msm.2014.26.195-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kavosi Z, Siavashi E. A study of the performance of referral system in urban family physician program in Fars Province, Iran. J Health Man & Info. 2018;5:88–95. [Google Scholar]
- 47.Kim E-H, Linker DT, Coumar A, Dean LS, Matsen FA, Kim Y. Factors affecting acceptance of a web-based self-referral system. IEEE Trans Inf Technol Biomed. 2010;15:344–7. doi: 10.1109/TITB.2010.2088129. [DOI] [PubMed] [Google Scholar]
- 48.Kim-Hwang JE, Chen AH, Bell DS, Guzman D, Yee HF, Kushel MB. Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med. 2010;25:1123–8. doi: 10.1007/s11606-010-1402-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kongnyuy EJ, Mlava G, Van Den Broek N. Criteria-based audit to improve a district referral system in Malawi: A pilot study. BMC Health Serv Res. 2008;8:190. doi: 10.1186/1472-6963-8-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li C, Yu X, Butler JR, Yiengprugsawan V, Yu M. Moving towards universal health insurance in China: Performance, issues and lessons from Thailand. Social Sci Med. 2011;73:359–66. doi: 10.1016/j.socscimed.2011.06.002. [DOI] [PubMed] [Google Scholar]
- 51.Lim K, Kim J-W, Yoo S, Heo E, Ji H, Kang B. Design of a hospice referral system for terminally ill cancer patients using a standards-based health information exchange system. Healthc Inform Res. 2018;24:317–26. doi: 10.4258/hir.2018.24.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Majoko F, Nyström L, Munjanja S, Lindmark G. Effectiveness of referral system for antenatal and intra-partum problems in Gutu district, Zimbabwe. J Obstet Gynaecol. 2005;25:656–61. doi: 10.1080/01443610500278378. [DOI] [PubMed] [Google Scholar]
- 53.Mehet J, Sanchez Franco L, Gascon Conde I, Sanchez Campoy A, Thimmaiah R, Eldessouky A, et al. The NORSe: Changing the way we communicate. Ann R Coll Surg Engl. 2018;100:161–4. doi: 10.1308/rcsann.2018.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nsigaye R, Wringe A, Roura M, Kalluvya S, Urassa M, Busza J, et al. From HIV diagnosis to treatment: Evaluation of a referral system to promote and monitor access to antiretroviral therapy in rural Tanzania. J Int AIDS Soc. 2009;12:31. doi: 10.1186/1758-2652-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oliva X, Micaló T, Pérez S, Jugo B, Solana S, Bernades C, et al. Virtual referral system between specialized endocrinological care and primary care. Endocrinol Nutr. 2013;60:4–9. doi: 10.1016/j.endonu.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 56.Prathiba P, Niranjjan R, Maurya DK, Lakshminarayanan S. Referral chain of patients with obstetric emergency from primary care to tertiary care: A gap analysis. J Family Med Prim Care. 2020;9:347–53. doi: 10.4103/jfmpc.jfmpc_836_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Prinja S, Jeet G, Kaur M, Aggarwal AK, Manchanda N, Kumar R. Impact of referral transport system on institutional deliveries in Haryana, India. Indian J Med Res. 2014;139:883–91. [PMC free article] [PubMed] [Google Scholar]
- 58.Quinn GP, Vadaparampil ST, Gwede CK, Reinecke JD, Mason TM, Silva C. Developing a referral system for fertility preservation among patients with newly diagnosed cancer. J Natl Compr Cancer Netw. 2011;9:1219–25. doi: 10.6004/jnccn.2011.0102. [DOI] [PubMed] [Google Scholar]
- 59.Scheibe MM, Imboden JB, Schmajuk G, Margaretten M, Graf JD, Chen AH, et al. Efficiency gains for rheumatology consultation using a novel electronic referral system in a safety-net health setting. Arthritis Care Res. 2015;67:1158–63. doi: 10.1002/acr.22559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shams A, Ashrafi-rizzi H, Afrough S, Javadi M, Shams A. A Survey on clients’ opinions in Isfahan's public hospitals about effective factors in the fulfillment of referral system. Acta Inform Med. 2013;21:51–5. doi: 10.5455/aim.2012.21.51-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tuot DS, Murphy EJ, McCulloch CE, Leeds K, Chan E, Chen AH. Leveraging an electronic referral system to build a medical neighborhood. Healthcare. 2015;3:202–8. doi: 10.1016/j.hjdsi.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 62.Williams L, O’Riordan S, McGuigan C, Hutchinson M, Tubridy N. A web-based electronic neurology referral system: A solution for an overburdened healthcare system? Ir Med J. 2012;105:301–3. [PubMed] [Google Scholar]
- 63.Yu W, Li M, Nong X, Ding T, Ye F, Liu J, et al. Practices and attitudes of doctors and patients to downward referral in Shanghai, China. BMJ Open. 2017;7:e012565. doi: 10.1136/bmjopen-2016-012565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zanolini A, Bolton C, Lyabola L-L, Phiri G, Samona A, Kaonga A, et al. Feasibility and effectiveness of a peer referral incentive intervention to promote male circumcision uptake in Zambia. J Acquir Immune Defic Syndr. 2016;72(Suppl 4):S257–63. doi: 10.1097/QAI.0000000000000808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chitsa B. Factors affecting the provision of referral services at the primary level of health care in Zomba District in Malawi. Texila Int J Public Health. 2019 doi:10.21522/TIJPH.2013.SE.19.01.Art023. [Google Scholar]
- 66.Chiou B-L, Chen Y-F, Chen H-Y, Chen C-Y, Yeh S-CJ, Shi H-Y. Effect of referral systems on costs and outcomes after hip fracture surgery in Taiwan. Int J Qual Health Care. 2020;32:649–57. doi: 10.1093/intqhc/mzaa115. [DOI] [PubMed] [Google Scholar]
- 67.Corwin P, Bolter T. The effects of audit and feedback and electronic referrals on the quality of primary care referral letters. J Prim Health Care. 2014;6:324–7. [PubMed] [Google Scholar]
- 68.Jiwa M, Walters S, Mathers N. Referral letters to colorectal surgeons: The impact of peer-mediated feedback. Br J Gen Pract. 2004;54:123–6. [PMC free article] [PubMed] [Google Scholar]
- 69.phcpi. High-Quality Primary Health Care. Coordination. Available from: https://improvingphc.org/coordination .
- 70.Gomez-Mejia LR, Balkin DB, Cardy RL. Managing Human Resources. Upper Saddle River, NJ: Pearson/Prentice Hall; 2007. [Google Scholar]
- 71.NAIC. Research and Actuarial Department. Glossary of Insurance Terms. Available from: https://content.naic.org/consumer_glossary.htm#I .
- 72.Healy T, Côté S. The well-being of nations: The role of human and social capital. Education and Skills: ERIC. 2001 [Google Scholar]
- 73.Mutaqi AS editor Architecture studio learning: Strategy to achieve architects competence. SHS Web of Conferences. EDP Sciences. 2018 [Google Scholar]
- 74.Rasouli G, Hamdi K. Helping relief campaigns: Social cognitive factors underlying important issues using structural equation modelling. Cogent Business & Management. 2020;7:1823596. doi:10.1080/23311975.2020.1823596. [Google Scholar]
- 75.Al-Abri R, Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. 2014;29:3–7. doi: 10.5001/omj.2014.02. [DOI] [PMC free article] [PubMed] [Google Scholar]


