Abstract
Background
The aim of the study was to determine the concentration of endogenous cystatin C and cystatin SN, as potential tumor biomarkers, in the serum and biological fluids of the eye in both healthy controls and patients with uveal melanoma.
Patients and methods
The concentration of both cystatins was determined in the intraocular fluid (IOF), tear fluid, and serum of patients with uveal melanoma and compared to baseline measurements in IOF, tears, serum, cerebral spinal fluid, saliva and urine of healthy controls.
Results
The concentration of cystatin C in all the biological matrices obtained from healthy controls significantly exceeded the concentration of cystatin SN and was independent of gender. Cystatin C concentrations in the tear fluid of patients with uveal melanoma (both the eye with the malignancy, as well as the contralateral, non-affected eye), were significantly greater than cystatin C concentrations in the tear fluid of healthy controls and was independent of tumor size. The concentration of cystatin SN in IOF of patients with uveal melanoma was significantly less than the corresponding concentration of cystatin SN in healthy controls.
Conclusions
The ratio of cystatins (CysC:CysSN) in both the serum and tear fluid, as well as the concentration of cystatin SN in IOF, would appear to strongly suggest the presence of uveal melanoma. It is further suggested that multiple diagnostic criteria be utilized if a patient is suspected of having uveal melanoma, such as determination of the cystatin C and cystatin SN concentrations in serum, tears, and IOF, ocular fundus and ultrasound imaging, and biopsy with histopathological evaluation.
Key words: uveal melanoma, cystatins, biomarkers, diagnosis
Introduction
Uveal melanoma frequently leads to progression of the malignancy and subsequent metastasis, which often results in death in patients with metastatic disease. The methods developed for the treatment of uveal melanoma consist of either removing the affected eye (enucleation), or complex ocular therapies (brachytherapy, laser photocoagulation, heat therapy, proton therapy, etc.).1, 2
Despite advances in the diagnosis and treatment of uveal melanoma, mortality 5 years after enucleation of the eye is 16.5%; after 10 years, it is 58%. Extra-scleral germination significantly worsens the prognosis; in fact, in these patients, the mortality reaches 69–73% after 10 years.3, 4 According to recent results of large-scale studies in the United States with more than 7500 patients with uveal melanoma, the risk of metastasis and death increases significantly with each stage of cancer diagnosis. For example, Stage T1 (2 times), Stage T2 (4 times), and Stage T3 (8 times).5, 6
Uveal melanoma, arising from melanocytes in the stroma, is the most common primary intraocular tumor in adults.7, 8 Detection of specific proteins allows for the identification of possible molecular markers of malignancy in several eye diseases. Specific tear proteins (~ 64 of 491 proteins), studied by proteome analysis and gel electrophoresis, are classified as proteases and protease inhibitors and carry special significance in the context of eye malignancies. Mammalian cystatins (to date, there are 12 known human cystatins) include a large family of proteins that have the ability to inhibit cysteine proteases9, 10, which are further divided into three types based on their molecular structure and distribution in the body.11
As just mentioned, cystatins can be categorized into three types. The first type (e.g., cystatins A and B) are intracellular cystatins (stefins). The second type (e.g., cystatins C, D, E/M, F, G, S, SN, SA) are extracellular cystatins. Finally, the third type of cystatins (e.g., L-kininogen, H-kininogen) are intravascular proteins.12 Cystatin SN has not been thoroughly studied to date13, whereas, the most well-known cystatin, cystatin C, was the first to be identified and its amino acid sequence determined.14, 15 Subsequently, the functions of cystatin C, as an inhibitor of cysteine proteases, was investigated, as well as its role in cell proliferation, migration, aging, and cell death.16, 17
Cystatins are endogenous and reversible inhibitors of cysteine peptidases that are important players in cancer progression.18, 19, 20 Importantly, cystatin C plays a significant role in the physiological functions of eye fluids12, as well as in the pathological processes associated with a number of eye tumors.21, 22, 23 As an example, in 2009, Paraoan et al. reported that for one particular lysosomal cysteine protease (cathepsin S), there was an increase in the active form of this protease that was not counterbalanced by the expression of its strongest endogenous inhibitor (cystatin C) in an aggressive, highly-metastatic form of uveal melanoma.24 The imbalance in cathepsin S and its inhibitor (cystatin C) is both relevant and important in the context of uveal melanoma, because it may provide a link to therapeutic anti-cancer strategies based on targeting the elastolytic and collagenolytic activity of cysteine cathepsins, as well as add to our understanding of the dysregulation in proteolytic activity that occurs in uveal melanoma.24
As previously mentioned, a large number of proteases and protease inhibitors have been identified among the 491 proteins in the tear fluid proteome.25 Changes in the composition of tear proteins are associated with a number of inflammatory, degenerative, and malignant eye diseases.26, 27 In fact, the balance between proteases and protease inhibitors is important for controlling the rates of cellular metabolism and the barrier function of the eye cornea.25 Furthermore, changes in the biological fluids of the eye are related to the ratio of proteases and protease inhibitors27, 28, 29, which can affect the composition of proteins and peptides in the lacrimal fluid. Thus, it would seem reasonable to assume that the identification of specific proteins in the biological fluids of the eye may make it possible to identify new molecular markers for several eye diseases.
The precise role of cysteine protease inhibitors in the development of eye tumors has not been fully elucidated to date.30, 31, 32 This is significant to ophthalmology, because some of these inhibitors may be of therapeutic benefit for the treatment of eye tumors. Thus, the aim of this study was to investigate the concentration of endogenous inhibitors of cysteine proteases; namely, cystatin C and cystatin SN, in the serum and the biological fluids of the eye in both healthy controls and patients with uveal melanoma.
Patients and methods
Patients and the collection of various biological matrices/fluids
All studies were carried out with informed consent of patients and in accordance with the ethical norms of the Helsinki Declaration (2000) and local regulations (Russian Council of Medical Research). The protocols were approved by the Institutional Review Board of biomedical ethics of the S. Fyodorov Eye Microsurgery Federal State Institution, Novosibirsk Branch (Protocol N4, 15.11.2017). Lastly, all the patients gave their informed consent for laboratory tests, as well as consent to process their personal data for scientific purposes.
Fifty-seven patients (mean age = 56.6 ± 2.4 years) with a diagnosis of choroidal melanoma in the Novosibirsk Branch of the S. Fyodorov Eye Microsurgery Federal State Institution were included in this investigation. The control group consisted of 37 healthy individuals (medical staff of the clinic and students of the Medical University, with a mean age = 31.0 ± 4.1 years for the subjects ≤ 60 years old [i.e., n = 28 (n = 13 healthy controls ≤ 40 years old + n = 15 healthy controls 41–60 years old)]. Of the 37 healthy controls, 20 were men and 17 were women, with 9 control subjects over 60 years old. Since the literature indicates that the serum levels of cystatin C increase with age in normal healthy individuals, and especially after the age of 60 years33, 34, 35, 36, we selected a subgroup of the healthy individuals (41–60 years; mean age = 53.1 ± 3.4 years; n = 15) as an age-matched control group to facilitate appropriate statistical comparisons with choroidal melanoma patients. Intraocular fluid (IOF) was obtained from 7 control patients (3 men and 4 women) close to, but not exceeding 60 years of age, undergoing an uncomplicated cataract removal procedure and submitted for biochemical analysis.
Tears from the conjunctival sac were collected by microcannulas and blood from the ulnar vein. Specifically, the tear fluid was obtained from the lower conjunctival arch of the eye and placed into a dry, sealed tube of 300–500 microliters. To evaluate the IOF in patients with ocular melanoma, moisture in the anterior chamber of the enucleated eye was obtained during the operation.
Samples of cerebrospinal fluid were obtained from 8 additional patients in the Federal State Budget Institute (“Federal Neurosurgical Center”, Novosibirsk, Russia) as part of a standard examination for neurosurgical patients without tumors.
An exclusion-criteria relevant to this study was the value of the estimated glomerular filtration rate (eGFR). Since the levels of cystatin C in various biological fluids could potentially be affected by overall kidney function, patients with an eGFR value less than 90 mL/min/1.73 m2 were excluded from the present study to control for this variable.
Analysis of cystatins in biological fluids
The concentration of cystatin C in biological fluids was evaluated using ELISA kits for human cystatin C (BioVendor, Czechia). The measurements were performed using a biochemical analyzer AU 480 (Beckman Coulter, USA).
The concentration of cystatin SN was also determined using commercial ELISA kits for human cystatin SN (Cusabio, China). The measurements were conducted using a Stat Fax 2100 microplate reader for enzyme immunoassay (Awareness Technology Inc., USA) at 450 nm.
Statistical analysis
All acquired data were reported as the mean ± the standard deviation (s.d.). Mean values were analyzed for statistically significant differences with the software program STATISTICA 10.0 using a one-way, analysis-of-variance (ANOVA). Post-hoc analysis of ANOVA testing was performed using the Least Significant Difference (LSD) test. When comparing only two mean values, we used the Student’s t-test to identify a difference that was statistically significant. All statistical results using either ANOVA, or the Student’s t-test, in which p < 0.05 were deemed statistically significantly different and were noted in the Figures, as well as in Table 1.
Table 1.
Concentrations of cystatin C and cystatin SN in biological fluids of healthy individuals as a function of age (Mean ± s.d.)
| Groups | Inhibitor | Serum (ng/mL) | Tears (ng/mL) | IOF (ng/mL) |
|---|---|---|---|---|
| Healthy | Cystatin C | 561 ± 10.0 | 296 ± 11.1 | - |
| (≤ 40 years) [n = 13] | Cystatin SN | 2.24 ± 0.20 | 0.49 ± 0.30 | |
| Healthy | Cystatin C | 539 ± 111 | 256 ± 82.3 | 414 ± 28 |
| (41–60 years) [n = 15] | Cystatin SN | 2.96 ± 0.70 | 0.6 ± 0.35 | 2.7 ± 1.40 |
| Healthy | Cystatin C | a1,341 ± 177 | 382 ± 116 | a844 ± 113 |
| (61–80 years) [n = 9] | Cystatin SN | b4.77 ± 0.10 | 0.75 ± 0.14 | 2.18 ± 0.20 |
a = significantly greater (p < 0.01) cystatin C concentration in serum and IOF compared to individuals ≤ 60 years; b = significantly greater (p < 0.01) cystatin SN concentration in serum compared to individuals ≤ 60 years; IOF = Intraocular fluid; s.d. = standard deviation
Results
Eye imaging
Figure 1A shows a typical image of the ocular fundus of a normal eye as compared to an eye with a choroidal melanoma having a thickness of 2.4 mm and a diameter of 8 mm. The thickness of the choroidal melanoma was also determined from an ultrasound image as shown in Figure 1B and was determined to be 3.1 mm.
Figure 1.
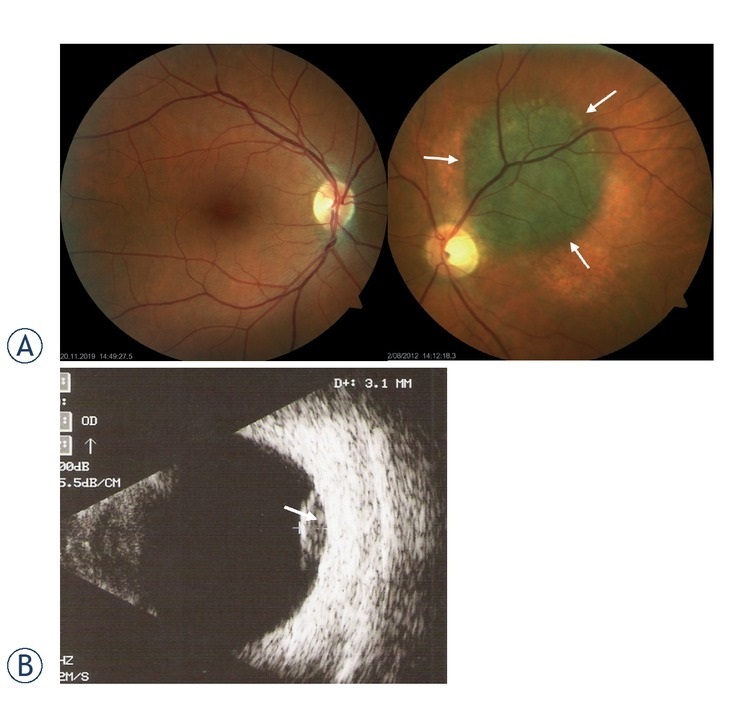
Ocular fundus of a normal eye, and eye with choroidal melanoma. (A) Ocular fundus. Normal healthy eye (left) versus eye with choroidal melanoma (right; dia = 8 mm and thickness = 2.4 mm). (B) Ultrasound image of the choroidal melanoma (thickness = 3.1 mm).
Concentration of cystatin C and cystatin SN in various biological matrices in healthy individuals (controls)
Figure 2 shows the concentration of cystatin C in various biological matrices (cerebral spinal fluid [CSF], saliva, serum, IOF, tears, and urine) in healthy individuals, while Figure 3 depicts the concentration of cystatin SN in these same biological matrices. In general, it was found that the concentration of cystatin C in all the biological matrices significantly exceeded the concentration of cystatin SN in the same matrices (Figure 2 vs. Figure 3). Additionally, the rank order of cystatin C concentrations in the various biological fluids followed the order CSF > saliva > serum > IOF > tears > urine (Figure 2), whereas, for cystatin SN, the rank order was saliva > urine > CSF > serum > IOF > tears (Figure 3).
Figure 2.
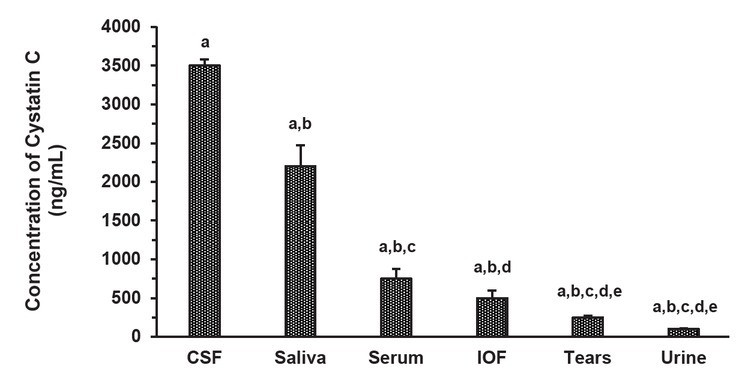
Cystatin C concentration in various biological matrices in healthy individuals. Concentration of cystatin C in each biological fluid (mean ± standard deviation [s.d.]; n = 28 [n = 13 healthy controls ≤ 40 years old + n = 15 healthy controls 41–60 years old]), since Table 1 shows a significant increase in cystatin C concentrations in serum and intraocular fluid (IOF) in 61–80 year old healthy controls, and thus, this age group was not included; cerebral spinal fluid (CSF) was obtained from an additional and separate group of cancer-free neurosurgical patients (n = 8) for the determination of the cystatin C concentration as described in the Materials and methods section.
a Significant difference (p < 0.001) from mean values indicated with the same letter.
b Significant difference (p < 0.001) from mean values indicated with the same letter.
c Significant difference (p < 0.01) from mean values indicated with the same letter.
d Significant difference (p < 0.01) from mean values indicated with the same letter.
e Significant difference (p < 0.01) from the mean value indicated with the same letter.
Figure 3.
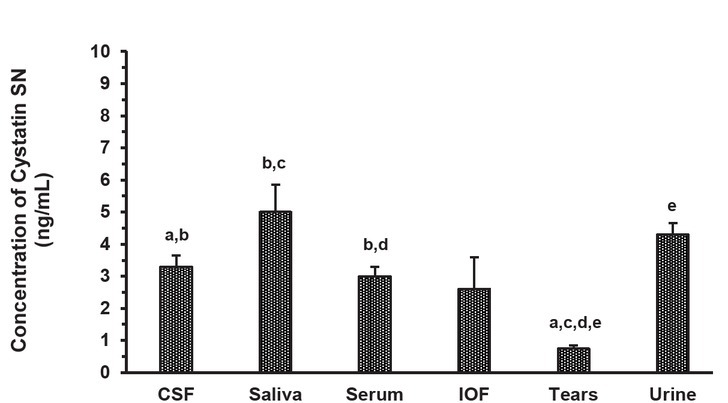
Cystatin SN concentration in various biological matrices in healthy individuals. Concentration of cystatin SN in each biological fluid (mean ± standard deviation [s.d.]; n = 28 [n = 13 healthy controls ≤ 40 years old + n = 15 healthy controls 41–60 years old]), since Table 1 shows a significant increase in the cystatin SN concentration in the serum of 61–80 year old healthy controls, and thus, this age group was not included; cerebral spinal fluid (CSF) was obtained from an additional and separate group of cancer-free neurosurgical patients (n = 8) for the determination of the cystatin SN concentration as described in the Materials and methods section.
a Significant difference (p < 0.001) from the mean value indicated with the same letter.
b Significant difference (p < 0.05) from mean values indicated with the same letter.
c Significant difference (p < 0.001) from the mean value indicated with the same letter.
d Significant difference (p < 0.01) from the mean value indicated with the same letter.
e Significant difference (p < 0.001) from the mean value indicated with the same letter.
The concentration of cystatin C and cystatin SN in three relevant biological fluids (serum, tears, and IOF) was determined for three different age groups to assess whether there was an age-dependent variation in the concentration of these two inhibitors (Table 1). As was determined with the concentrations of cystatin C and cystatin SN in the six biological fluids of healthy individuals (Figure 2 and 3), there was a significantly greater concentration of cystatin C relative to cystatin SN in the serum, tears, and IOF (Table 1). While we determined that there was no gender difference observed between the concentration of each inhibitor in each age group for each of the three biological fluids mentioned above, there was a significant (p < 0.01) elevation in the serum concentration of both cystatins in healthy individuals (age 61–80 years) when compared to individuals less than or equal to 60 years of age (Table 1). This finding was also observed for IOF, but only for cystatin C and not cystatin SN (Table 1).
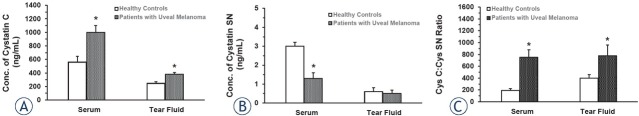
Cystatin C and cystatin SN concentrations and their ratio in the serum and tear fluid of patients with uveal melanoma
Cystatin C levels were significantly (p < 0.01) greater in both serum and tear fluid in patients with uveal melanoma when compared to healthy controls (Figure 4A). However, with regard to the concentration of cystatin SN in these same two biological fluids, there was only a significant (p < 0.01) decrease in the concentration of cystatin SN in the serum of patients with uveal melanoma compared to healthy controls (Figure 4B). Importantly, the ratio of cystatin C to cystatin SN (CysC:CysSN) in both serum and tear fluid was significantly (p < 0.001) increased in patients with uveal melanoma when compared to corresponding mean values of this ratio in healthy controls (Figure 4C).
Figure 4.
Cystatin C (A) and cystatin SN (B) concentrations and their ratio (C) in the serum and tear fluid of patients with uveal melanoma. (A) Values represent the mean ± standard deviation (s.d.) of n = 15 healthy controls (mean age = 53.1 ± 3.4 years) and n = 51 of 57 total patients with uveal melanoma (mean age = 51.7 ± 2.8 years; 6 patients were > 60 years old and were therefore not included). (B) Values represent the mean ± s.d. of n = 15 healthy controls (mean age = 53.1 ± 3.4 years) and n = 51 of 57 total patients with uveal melanoma (mean age = 51.7 ± 2.8 years; 6 patients were > 60 years old and were therefore not included). (C) Values represent the mean ± s.d. of n = 15 healthy controls (mean age = 53.1 ± 3.4 years) and n = 51 of 57 total patients with uveal melanoma (mean age = 51.7 ± 2.8 years; 6 patients were > 60 years old and were therefore not included).
* = significant difference (p < 0.001) from the mean value for healthy controls in each biological matrix
As an aside, we also determined the inhibitor with higher concentrations in all biological fluids tested in this study; namely, cystatin C, for its prevalence in the tear fluid of patients with different size uveal melanoma tumors. The cystatin C concentrations in the tear fluid of patients with uveal melanoma (both the eye with the malignancy, as well as the contralateral, non-affected eye), were significantly (p < 0.05) greater than cystatin C concentrations determined in the tear fluid of healthy controls (i.e., range of 450–500 ± 60 ng/mL in the diseased eye with uveal melanoma vs. 250 ± 25 ng/mL in both eyes of healthy controls) and was independent of tumor size. Moreover, at the time of clinical presentation, there was no significant difference between the cystatin C concentration in the tear fluid of the malignant eye versus the corresponding concentration of cystatin C in the tear fluid of the contralateral, non-affected eye regardless of tumor size (data not shown).
Concentration of cystatin C and cystatin SN in IOF of patients with uveal melanoma versus healthy controls
Figure 5A shows the concentrations of cystatin C in IOF in healthy controls and patients with uveal melanoma, while Figure 5B shows the concentration of cystatin SN in these same two patient cohorts. There was no significant difference between the concentration of cystatin C in IOF of healthy controls and patients with uveal melanoma, but there was a significant (p < 0.001) reduction in the concentration of cystatin SN in IOF of patients with uveal melanoma when compared to this same parameter in healthy controls.
Figure 5.
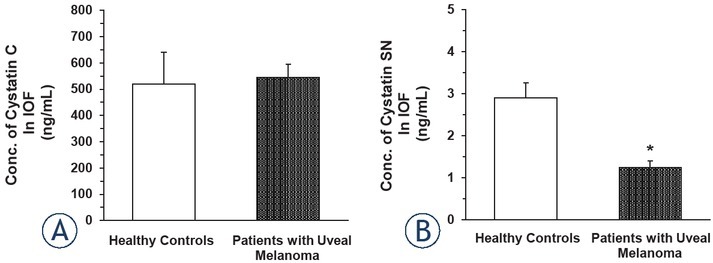
Concentration of cystatin C (A) and cystatin SN (B) in intraocular fluid of patients with uveal melanoma versus healthy controls. (A) Values represent the mean ± standard deviation (s.d.) of n = 7 healthy controls (mean age = 57.5 ± 1.9 years) and n = 18 of 57 total uveal melanoma patients selected based on an age close to the mean age of the 7 healthy controls (mean age = 55.9 ± 3.2 years; n = 18). (B) Values represent the mean ± s.d. of n = 7 healthy controls (mean age = 57.5 ± 1.9 years) and n = 18 of 57 total uveal melanoma patients selected based on an age close to the mean age of the 7 healthy controls (mean age = 55.9 ± 3.2 years; n = 18).
* = significant difference (p < 0.001) from mean value for healthy controls; IOF = intraocular fluid
Discussion
The present study has addressed the question as to whether cystatin C and/or cystatin SN may potentially function as biomarkers in uveal melanoma. Clearly, our work has shown that the concentration of each cysteine proteinase inhibitor (cystatin C and cystatin SN) is perturbed in uveal melanoma in various biological fluids. We first briefly describe the role of each cystatin, and then their use as potential biomarkers in cancer.
Cysteine proteinase inhibitors, cystatins, are involved in mechanisms controlling intracellular and extracellular protein degradation.11,37 Cystatin C is a secreted cysteine protease inhibitor, which is abundantly expressed in body fluids and possibly regulated at both the transcriptional and post-translational levels.38, 39 Production of cystatin C from hematopoietic cell lineages contributes significantly to the overall systemic pool of cystatin C.40 This particular cystatin is the most abundant and potent member21,27 of the cystatin family, which is important due to the fact that the activity of various cysteine proteases, both inside and outside of cells, requires careful regulation or control by endogenous inhibitors such as cystatin C. The levels of cystatin C in the systemic circulation (serum) are typically different from the concentration of cystatin C in biological fluids of the eye, such as IOF and tears.29,41 In fact, according to our data, the concentration of cystatin C in serum was significantly greater than in both IOF and tears. It has been suggested that tears may function as a pool, or reservoir, for biomarkers of various pathological eye conditions, as well as for diseases beyond just ocular disorders.42
Cystatin C is involved in numerous diseases, including atherosclerosis and cancer, as well as the aging process.17,29,41 Importantly, cystatin C is believed to prevent tumor progression by inhibiting the activities of a family of lysosomal cysteine cathepsins. Using cystatin C-deficient animals, Huh et al. reported that cystatin C concentrations in vivo might influence tumor metastasis in some tissues.43 Interestingly, cystatin C is downregulated in prostate cancer and may prevent tumor progression by inhibiting the activities of a family of lysosomal cysteine proteases.44 However, Hammouda et al.45 suggested that although serum cystatin C levels may potentially represent a novel biomarker that reflects tumor burden (based on the fact that cystatin C levels were significantly more elevated in diffuse large B-cell lymphoma patients than in controls), there was no prognostic value regarding overall survival. Jiang et al. have recently reported that both serum and urine cystatin C levels are elevated, and the cystatin C gene is upregulated nearly 50-fold, in patients with multiple myeloma, which suggests it use as a diagnostic biomarker in multiple myeloma.31 Additionally, Leto and Sepporta32 suggested the use of cystatin C as a predictive biomarker for breast cancer. Lastly, it is worth noting that Kos et al. considers cystatin C to be a potential anticancer agent.41
Next, we turn to the other cysteine protease inhibitor evaluated in the present study; namely, cystatin SN. Cystatin SN, along with cystatins S and SA, belongs to the second type of extracellular cystatins (in this case, salivary cystatins), which has not been as thoroughly studied as cystatin C. While cystatin SN is not as prevalent as cystatin C in normal mammalian tissues46, it is a member of the cystatin family that inhibits the proteolytic activity of cysteine proteases. In fact, univariate and multivariate analyses have indicated that cystatin SN possibly acts as a marker for cancer prognosis.13 For example, cystatin SN has been shown to be a tumor biomarker that provides useful information for the diagnosis of esophageal47, 48, 49, gastric, pancreatic, and colorectal cancers30,50, as well as neuroblastomas and melanomas.12
As it pertains to cancer progression, cystatin SN is thought to be involved in several malignant tumors.51 For instance, it was recently reported by Cui et al. that upregulation of this inhibitor promoted the progression of hepatocellular carcinoma.51 Of note, knockdown of cystatin SN significantly reduced the expression of proliferation-related proteins p-AKT and PCNA10, which indicates a more complex role of cystatins in tumor growth and progression beyond their role as inhibitors of cysteine cathepsins. Lastly, a survival study in patients with surgically-resected, non-small cell lung cancer revealed an association between elevated expression levels of cystatin SN and poor prognosis.46 Specifically, the study indicated that significantly increased expression of cystatin SN was directly correlated with a higher rate of cancer recurrence, metastatic risk, and poor overall survival.46
The present study focused on the use of cystatin C and cystatin SN as potential biomarkers in the context of uveal melanoma. We successfully showed that the concentrations of cystatin C and cystatin SN were significantly elevated, and reduced, respectively, in the serum of patients with uveal melanoma compared to healthy controls. While there was a significant increase in the concentration of cystatin C in the tear fluid of patients with uveal melanoma when compared to healthy controls, there was no significant difference in the concentration of cystatin SN in the tear fluid between these same two patient cohorts. However, we would suggest that the value of the CysC:CysSN ratio in both biological matrices (i.e., serum and tears) may potentially be a better indicator of uveal melanoma than either inhibitor (cystatin) alone, since the ratio was very significantly increased in both matrices.
The change in the concentration of cystatin SN in another ocular fluid; specifically, IOF, may serve as further evidence to suggest the presence of uveal melanoma, since the concentration of this cystatin was significantly reduced in patients with uveal melanoma when compared to corresponding concentrations of cystatin SN in healthy controls. This finding may argue for a combined determination of the concentrations of both cystatin C and cystatin SN in serum, tear fluid, and IOF to assist ophthalmologists that have a preliminary suspicion concerning the presence of uveal melanoma, especially when combined with both ocular fundus and ultrasound imaging. However, it is important to mention that there are other ocular disorders (e.g., AMD) that may perturb the concentrations of cystatins in various biological fluids, which is why it is important to have multiple diagnostic criteria to confirm the presence of uveal melanoma. For example, a variant of cystatin C (i.e., variant B, cystatin C) differs from the wild-type protein by a single amino acid (A25T) and is associated with decreased plasma cystatin C levels and an increased risk of developing AMD, which potentially raises the prospect of cystatin C replacement therapy for patients homozygous for variant B.52
In conclusion, the present investigation has documented changes in the concentrations of cystatin C and cystatin SN in various biological fluids in both healthy controls and patients with uveal melanoma, which may possibly serve as potential biomarkers of uveal melanoma, especially when the value of the CysC:CysSN ratio is determined in both the serum and tear fluid. That is, the value of the CysC:CysSN ratio may be a better indicator of the possibility of uveal melanoma than either cystatin alone. We would also suggest that the profound reduction in the concentration of cystatin SN in IOF may provide further support for the possible presence of uveal melanoma. However, it is imperative for ophthalmologists to utilize multiple diagnostic criteria if they suspect that a patient has uveal melanoma, including, but not limited to, the concentrations of cystatin C and cystatin SN in serum, tears, and IOF, together with ocular fundus and ultrasound imaging.
Lastly, as it pertains to the present findings described herein, we further suggest that the concentrations of cystatin C and cystatin SN in serum, tears, and IOF, as well as diagnostic ocular imaging studies, be combined with tissue biopsy and subsequent evaluation by surgical pathology to differentiate between malignant and benign eye tumors, since Dikovskaya et al. reported that the level of cystatin C in tears was significantly elevated (relative to the concentration of cystatin C in the tears of healthy controls) in both malignant and benign eye tumors.27 That is, the concentration of cystatin C in the tear fluid of patients with both malignant and benign eye tumors was significantly elevated relative to this same measurement in healthy control patients, but was not significantly different (p > 0.05) between patients with either a malignant, or benign, eye tumor.27 It is for the latter reason that a tissue biopsy with histopathological evaluation is absolutely necessary to distinguish a malignant eye tumor from one that is benign, although, as mentioned directly above and verified in the present study, cystatin C levels in the serum and tears of patients with uveal melanoma are profoundly elevated relative to cystatin C levels in these same two biological fluids in healthy controls, and thus, is certainly suggestive of possible uveal melanoma. Reliance on multiple diagnostic criteria is critically important for uveal melanoma, since surgery to remove the melanoma and a small area of healthy tissue is reserved for small melanomas, whereas enucleation is typically required for large eye tumors.
Acknowledgements
The authors would like to gratefully acknowledge the assistance of Prof. Kuleshova Olga Nikolaevna (S. Fyodorov Eye Microsurgery Federal State Institution, Novosibirsk, Russia) with the clinical portion of this work. We are also grateful to Professor J. Kos (Slovenia) for support and Dr. I.N. Ignatik (AquaTest, St. Petersburg) for providing assistance with the determination of human cystatin C in biological samples.
The present study was supported with funding provided by the Institute of Neurosciences and Medicine, Novosibirsk, Russia (2017–2021) for basic scientific research.
Disclosure
No potential conflicts of interest were disclosed.
References
- 1.Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye (Lond) 2017;31:241–57. doi: 10.1038/eye.2016.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elder DE, Bastian BC, Cree IA, Massi D, Scolyer RA. The 2018 World Health Organization classification of cutaneous, mucosal, and uveal melanoma: detailed analysis of 9 distinct subtypes defined by their evolutionary pathway. Arch Pathol Lab Med. 2020;144:500–22. doi: 10.5858/arpa.2019-0561-RA. [DOI] [PubMed] [Google Scholar]
- 3.Sathe S, Sakata M, Beaton AR, Sack RA. Identification, origins and the diurnal role of the principal serine protease inhibitors in human tear fluid. Curr Eye Res. 1998;17:348–62. doi: 10.1080/02713689808951215. [DOI] [PubMed] [Google Scholar]
- 4.Saakyan SV, Tsygankov АY, Moiseeva NI, Karamysheva АF, Garri DD. Assessment of the chemosensitivity of uveal melanoma cells ex vivo. Bull Exp Biol Med. 2020;170:142–7. doi: 10.1007/s10517-020-05020-3. [DOI] [PubMed] [Google Scholar]
- 5.Shah SU, Mashayekhi A, Shields CL, Walia HS, Hubbard GB 3rd, Zhang J, et al. Uveal metastasis from lung cancer: clinical features, treatment, and outcome in 194 patients. Ophthalmology. 2014;121:352–7. doi: 10.1016/j.ophtha.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Valsecchi ME, Orloff M, Sato R, Chervoneva I, Shields CL, Shields JA. Adjuvant sunitinib in high-risk patients with uveal melanoma: comparison with institutional controls. Ophthalmology. 2018;125:210–7. doi: 10.1016/j.ophtha.2017.08.017. et al. [DOI] [PubMed] [Google Scholar]
- 7.Spagnolo F, Caltabiano G, Queirolo P. Uveal melanoma. Cancer Treat Rev. 2012;38:549–53. doi: 10.1016/j.ctrv.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 8.Luke JJ, Triozzi PL, McKenna KC, Van Meir EG, Gershenwald JE, Bastian BC. Biology of advanced uveal melanoma and next steps for clinical therapeutics. Pigment Cell Melanoma Res. 2015;28:135–47. doi: 10.1111/pcmr.12304. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turk V, Stoka V, Turk D. Cystatins: biochemical and structural properties, and medical relevance. Front Biosci. 2008;13:5406–20. doi: 10.2741/3089. [DOI] [PubMed] [Google Scholar]
- 10.Breznik B, Mitrović A, Lah T, Kos J. Cystatins in cancer progression: more than just cathepsin inhibitors. Biochimie. 2019;166:233–50. doi: 10.1016/j.biochi.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Wu H, Du Q, Dai Q, Ge J, Cheng X. Cysteine protease cathepsins in atherosclerotic cardiovascular diseases. J Atheroscler Thromb. 2018;25:111–23. doi: 10.5551/jat.RV17016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallin H, Bjarnadottir M, Vogel LK, Wassélius J, Ekström U, Abrahamson M. Cystatins – extra- and intracellular cysteine protease inhibitors: high-level secretion and uptake of cystatin C in human neuroblastoma cells. Biochimie. 2010;92:1625–34. doi: 10.1016/j.biochi.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y, Yao J. Research progress of cystatin SN in cancer. Onco Targets Ther. 2019;12:3411–9. doi: 10.2147/OTT.S194332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grubb AO. Cystatin C – properties and use as diagnostic marker. Adv Clin Chem. 2000;35:63–99. doi: 10.1016/s0065-2423(01)35015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abrahamson M, Alvarez-Fernandez M, Nathanson CM. Cystatins. Biochem Soc Symp. 2003;70:179–99. doi: 10.1042/bss0700179. [DOI] [PubMed] [Google Scholar]
- 16.Poteryaeva ON, Falameyeva OV, Korolenko TA, Kaledin VI, Djanayeva SJ, Nowicky JW. Cysteine proteinase inhibitor level in tumor and normal tissues in control and cured mice. Drugs Exp Clin Res. 2000;26:301–6. et al. PMID: 11345042. [PubMed] [Google Scholar]
- 17.Keppler D. Towards novel anti-cancer strategies based on cystatin function. Cancer Lett. 2006;235:159–76. doi: 10.1016/j.canlet.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Lah TT, Kokalj-Kunovar M, Drobnic-Kosorok M, Babnik J, Golouh R, Vrhovec I. Cystatins and cathepsins in breast carcinoma. Biol Chem Hoppe Seyler. 1992;373:595–604. doi: 10.1515/bchm3.1992.373.2.595. et al. [DOI] [PubMed] [Google Scholar]
- 19.Cox JL. Cystatins and cancer. Front Biosci (Landmark Ed) 2009;14:463–74. doi: 10.2741/3255.PMID:19273078. [DOI] [PubMed] [Google Scholar]
- 20.Jakoš T, Pišlar A, Jewett A, Kos J. Cysteine cathepsins in tumor-associated immune cells. Front Immunol. 2019;10:2037. doi: 10.3389/fimmu.2019.02037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Svechnikova IG, Korolenko TA, Stashko JuF, Kaledin VI, Nikolin VP, Nowicky JW. The influence of Ukrain on the growth of HA-1 tumor in mice: the role of cysteine proteinases as markers of tumor malignancy. Drugs Exp Clin Res. 1998;24:261–9. PMID: 10190085. [PubMed] [Google Scholar]
- 22.Korolenko TA, Cherkanova MS, Gashenko EA, Johnston T, Cystatin C. atherosclerosis and lipid-lowering therapy by statins. In: Cohen JB, Ryseck LP, editors. Cystatins: protease inhibitors, biomarkers and immunomodulators. New York, USA: Nova Science Publishers; 2011. pp. 187–204. p. –.
- 23.Korolenko TA, Pisareva EE, Filyushina EE, Johnston TP, Machova E. Serum cystatin C and chitotriosidase in acute P-407 induced dyslipidemia: can they serve as potential early biomarkers for atherosclerosis? Exp Toxicol Pathol. 2015;67:459–66. doi: 10.1016/j.etp.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 24.Paraoan L, Gray D, Hiscott P, Garcia-Finana M, Lane B, Damato B. Cathepsin S and its inhibitor cystatin C: imbalance in uveal melanoma. Front Biosci (Landmark Ed.) 2009;14:2504–13. doi: 10.2741/3393. et al. [DOI] [PubMed] [Google Scholar]
- 25.De Souza GA, Godoy LM, Mann M. Identification of 491 proteins in the tear fluid proteome reveals a large number of proteases and protease inhibitors. Genome Biol. 2006;7:R72. doi: 10.1186/gb-2006-7-8-R72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Balasubramanian SA, Wasinger VC, Pye DC, Willcox MD. Preliminary identification of differentially expressed tear proteins in keratoconus. Mol Vis. 2013;19:2124–34. eCollection 2013. PMID: 24194634. [PMC free article] [PubMed] [Google Scholar]
- 27.Dikovskaya MA, Trunov AN, Chernykh VV, Korolenko TA. Cystatin C and lactoferrin concentrations in biological fluids as possible prognostic factors in eye tumor development. Int J Circumpolar Health. 2013;72(Suppl 1):21087. doi: 10.3402/ijch.v72i0.21087.eCollection2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Korolenko TA, Tuzikov FV, Cherkanova MS, Johnston TP, Tuzikova NA, Loginova VM. Influence of atorvastatin and carboxymethylated glucan on the serum lipoprotein profile and MMP activity of mice with lipemia induced by poloxamer 407. Can J Physiol Pharmacol. 2012;90:141–53. doi: 10.1139/y11-118. et al. [DOI] [PubMed] [Google Scholar]
- 29.Pišlar A, Jewett A, Kos J. Cysteine cathepsins: their biological and molecular significance in cancer stem cells. Semin Cancer Biol. 2018;53:168–77. doi: 10.1016/j.semcancer.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 30.Jiang J, Liu HL, Liu ZH, Tan SW, Wu B. Identification of cystatin SN as a novel biomarker for pancreatic cancer. Tumor Biol. 2015;36:3903–10. doi: 10.1007/s13277-014-3033-3. [DOI] [PubMed] [Google Scholar]
- 31.Jiang Y, Zhang J, Zhang C, Hong L, Jiang Y, Lu L. The role of cystatin C as a proteosome inhibitor in multiple myeloma. Hematology. 2020;25:457–63. doi: 10.1080/16078454.2020.1850973. et al. [DOI] [PubMed] [Google Scholar]
- 32.Leto G, Sepporta MV. The potential of cystatin C as a predictive biomarker in breast cancer. Expert Rev Anticancer Ther. 2020;20:1049–56. doi: 10.1080/14737140.2020.1829481. [DOI] [PubMed] [Google Scholar]
- 33.Ognibene A, Mannucci E, Caldini A, Terreni A, Brogi M, Bardini G. Cystatin C reference values and aging. Clin Biochem. 2006;39:658–61. doi: 10.1016/j.clinbiochem.2006.03.017. et al. [DOI] [PubMed] [Google Scholar]
- 34.Odden MC, Tager IB, Gansevoort RT, Bakker SJ, Katz R, Fried LF. Age and cystatin C in healthy adults: a collaborative study. Nephrol Dial Transplant. 2010;25:463–9. doi: 10.1093/ndt/gfp474. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edinga BE, Yakam AT, Nansseu JR, Bilong C, Belinga S, Minkala E. Reference intervals for serum cystatin C and serum creatinine in an adult sub-Saharan African population. BMC Clin Pathol. 2019;19:4. doi: 10.1186/s12907-019-0086-7. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Groesbeck D, Köttgen A, Parekh R, Selvin E, Schwartz GJ, Coresh J. Age, gender, and race effects on cystatin C levels in US adolescents. Clin J Am Soc Nephrol. 2008;3:1777–85. doi: 10.2215/CJN.00840208. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zou J, Chen Z, Wei X, Chen Z, Fu Y, Yang X. Cystatin C as a potential therapeutic mediator against Parkinson’s disease via VEGF-induced angiogenesis and enhanced neuronal autophagy in neurovascular units. Cell Death Dis. 2017;8:e2854. doi: 10.1038/cddis.2017.240. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Keppler D, Zhang J, Bihani T, Lin AW. Novel expression of CST1 as candidate senescence marker. J Gerontol A Biol Sci Med Sci. 2011;66:723–31. doi: 10.1093/gerona/glr033. [DOI] [PubMed] [Google Scholar]
- 39.Wang R, Chen Z, Fu Y, Wei X, Liao J, Liu X. Plasma cystatin C and high-density lipoprotein are important biomarkers of Alzheimer’s disease and vascular dementia: a cross-sectional study. Front Aging Neurosci. 2017;9:26. doi: 10.3389/fnagi.2017.00026. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu Y, Ding Y, Li X, Wu X. Cystatin C is a disease-associated protein subject to multiple regulation. Immunol Cell Biol. 2015;93:442–51. doi: 10.1038/icb.2014.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kos J, Mitrović A, Mirković B. The current stage of cathepsin B inhibitors as potential anticancer agents. Future Med Chem. 2014;6:1355–71. doi: 10.4155/fmc.14.73. [DOI] [PubMed] [Google Scholar]
- 42.Pieragostino D, D’Alessandro M, Di Ioia M, Di Ilio C, Sacchetta P, Del Boccio P. Unraveling the molecular repertoire of tears as a source of biomarkers: beyond ocular diseases. Proteomics Clin Appl. 2015;9:169–86. doi: 10.1002/prca.201400084. [DOI] [PubMed] [Google Scholar]
- 43.Huh CG, Håkansson K, Nathanson CM, Thorgeirsson UP, Jonsson N, Grubb A. Decreased metastatic spread in mice homozygous for a null allele of the cystatin C protease inhibitor gene. Mol Pathol. 1999;52:332–40. doi: 10.1136/mp.52.6.332. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wegiel B, Jiborn T, Abrahamson M, Helczynski L, Otterbein L, Persson JL. Cystatin C is downregulated in prostate cancer and modulates invasion of prostate cancer cells via MAPK/Erk and androgen receptor pathways. PLoS ONE. 2009;4:e7953. doi: 10.1371/journal.pone.0007953. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hammouda NE, Salah El-Din MA, El-Shishtawy MM, El-Gayar AM. Serum cystatin C as a biomarker in diffuse large B-cell lymphoma. Sci Pharm. 2017;85:9. doi: 10.3390/scipharm85010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao X, Li Y, Luo RZ, Zhang L, Zhang SL, Zeng J. Expression of cystatin SN significantly correlates with recurrence, metastasis, and survival duration in surgically resected non-small cell lung cancer patients. Sci Rep. 2015;5:8230. doi: 10.1038/srep08230. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen YF, Ma G, Cao X, Luo RZ, He LR, He JH. Overexpression of cystatin SN positively affects survival of patients with surgically resected esophageal squamous cell carcinoma. BMC Surg. 2013;13:15. doi: 10.1186/1471-248213-15. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oh SS, Park S, Lee KW, Madhi H, Park SG, Lee HG. Extracellular cystatin SN and cathepsin B prevent cellular senescence by inhibiting abnormal glycogen accumulation. Cell Death Dis. 2017;8:e2729. doi: 10.1038/cddis.2017.153. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oh BM, Lee SJ, Cho HJ, Park YS, Kim JT, Yoon SR. Cystatin SN inhibits auranofin-induced cell death by autophagic induction and ROS regulation via glutathione reductase activity in colorectal cancer. Cell Death Dis. 2017;8:e2682. doi: 10.1038/cddis.2017.100. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yoneda K, Iida H, Endo H, Hosono K, Akiyama T, Takahashi H. Identification of cystatin SN as a novel tumor marker for colorectal cancer. Int J Oncol. 2009;35:33–40. doi: 10.3892/ijo_00000310. et al. [DOI] [PubMed] [Google Scholar]
- 51.Cui Y, Sun D, Song R, Zhang S, Liu X, Wang Y. Upregulation of cystatin SN promotes hepatocellular carcinoma progression and predicts a poor prognosis. J Cell Physiol. 2019;234:22623–34. doi: 10.1002/jcp.28828. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paraoan L, Hiscott P, Gosden C. Cystatin C in macular and neuronal degenerations: Implications for mechanism(s) of age-related macular degeneration. Vision Research. 2010;50:737–42. doi: 10.1016/j.visres.2009.10.022. [DOI] [PubMed] [Google Scholar]