Abstract
Health advances have not benefited all people equally. Health equity remains an aspirational goal, but research that enhances health equity is the highest priority at the NIH. Here we propose a call to action and outline current NIH programs that aim to eliminate health disparities both broadly and in high priority areas. Discussed topics include stroke as an indicator of broad health inequity, challenges and opportunities in health disparities research, the need to diversify the research workforce, and the ongoing efforts and struggles to establish trust with disadvantaged communities during the COVID-19 pandemic.
Introduction
Despite decades of The National Institutes of Health (NIH) funded research, race/ethnic and geographic disparities in stroke mortality continue to exist. In the past, some researchers focused purely on “race” as a major biologic factor in understanding health disparities. However, the COVID19 pandemic has highlighted the fact that “race” is confounded by many variables, including social determinants (e.g. education, socio-economic status, housing insecurity, etc.), racism, and discrimination. If we strive to make NIH funded health disparities research more rigorous and impactful, updated objective standards are needed to determine how best to address these factors in order to truly make this research matter.
Health Equity
The U.S. Health Resources and Services Administration1 defines health equity as “the absence of disparities or avoidable differences among socioeconomic and demographic groups or geographical areas in health status and health outcomes such as disease, disability, or mortality”. In the U.S. and globally, health equity remains an aspirational goal, agreed by most to be critical but rarely achieved. The NIH represents the taxpayers’ largest investment in biomedical research and the NIH mission is to reduce the burden of illness due to disease for all people. However, health advances—including those advanced through NIH research—have not benefited all people equally. Many of the NIH’s 27 Institutes and Centers have programs focused specifically on the study of health disparities, and it is the sole focus and mission of one Institute: The National Institute on Minority Health and Health Disparities (NIMHD). Research that informs real change by promoting health equity has risen to the highest priority level at NIH. It is also a component of the NIH’s new UNITE2 program to end structural racism and racial inequities in biomedical research. UNITE includes support from the NIH Director’s Common Fund program3 to foster the development, testing, and dissemination of innovative interventions focused on elimination of health disparities broadly and in high priority areas. The common fund is a component of the NIH budget that is used to address emerging scientific opportunities and pressing challenges in biomedical research that no single NIH institute or center can address on its own but are of high priority to the NIH as a whole.
Stroke as an indicator of broad health inequity
Brain infarction or hemorrhage (stroke) are tragic events that permanently change quality of life or lead to death. These events have a disparate mortality impact on various individuals based on race/ethnicity, geography, and other factors4. Because stroke is largely preventable it is also a sentinel measure of health disparities. Factors that support this sustained health difference may be at the provision of care level, on the societal level, and/or on the individual level. Dr. C. Miller Fisher, a pioneer in stroke neurology, would point out to primary care doctors that each of their patients who suffered a stroke represented their failure as a physician. This statement highlights a failure in the health care system that can lead to poor outcomes in patients. Other less obvious failures that can negatively impact patient outcomes include communication barriers, racism, or unconscious bias on the part of medical providers. All of these factors lead to a structural barrier in the health care system. In fact, in March 2002, The Institute of Medicine, now known as the National Academy of Medicine, published a report titled, “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.” This report concluded that racial and ethnic disparities in health care do exist, and that sources, including health care systems, health care providers, patients, and utilization managers, are contributors5.
Though hypertension is the primary driver of stroke, social factors such as lack of access to quality health insurance, poor air quality, harmful chemical exposures, neighborhoods with inadequate housing, transportation, limited access to fresh fruits/vegetables, and limited access to quality health care facilities lead to disparities in health outcomes, including stroke incidence and mortality. The context for these social ills is often steeped in the milieu of poverty, structural racism and discrimination. The increased prevalence and occurrence of stroke in specific socioeconomic and demographic groups or geographical regions in our country is a manifestation of this deep social gap in health equity. The most striking regional disparities in stroke are illustrated in the map of 2017-2019 stroke death rates by county (Figure 1)6. The CDC estimates that nearly one-fourth of all cardio- and cerebrovascular deaths are avoidable and occur disproportionately among males, non-Hispanic Blacks adults, and in the South7.
Figure 1-.
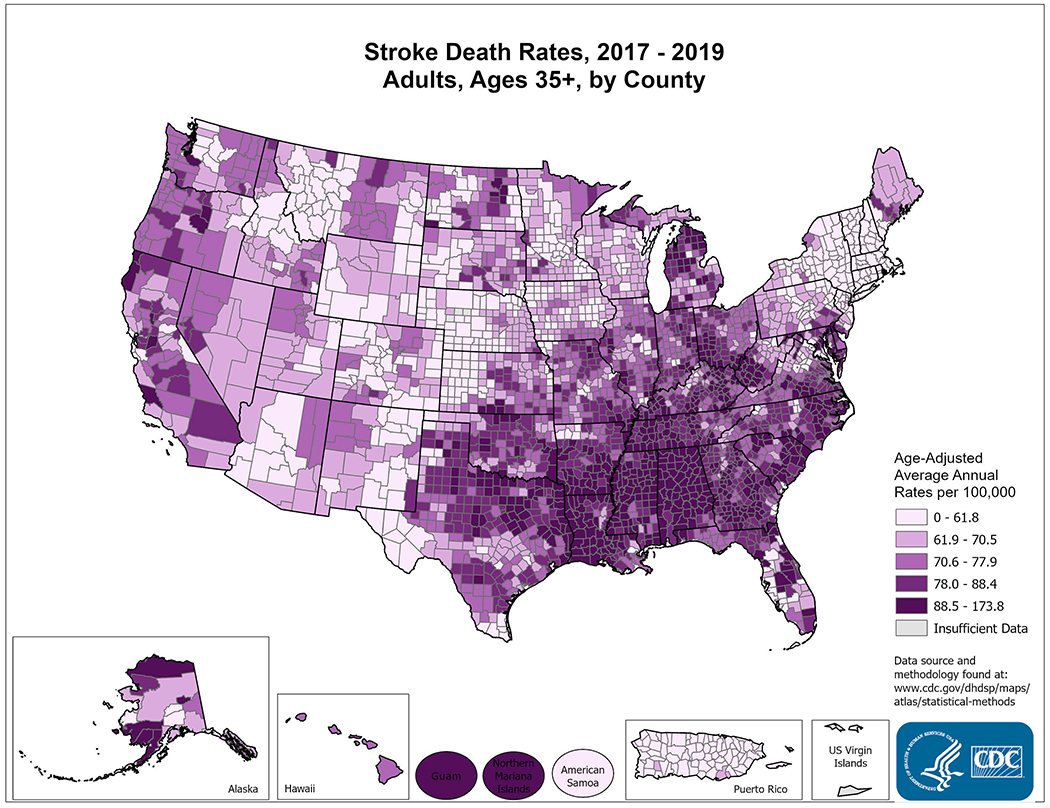
Map of the US depicting Age-Adjusted Average Annual Deaths per 100,000 people in adults age 35 or older (2017-2019). Darker purple represents increasing average annual stroke deaths.
Schieb, L. Centers for Disease Control and Prevention. Quick Maps of Heart Disease, Stroke, and Socioeconomic Conditions. https://www.cdc.gov/dhdsp/maps/national_maps/stroke_all.htm. Accessed 10/04/2021.
On an individual level, stroke is often the consequence of years of poorly managed blood pressure, lipid levels, body weight, and unhealthy lifestyle due to lack of exercise, high salt, a diet low in fruits and vegetables, smoking, drug or and alcohol abuse. There is a growing appreciation of the role of emotional stress contributing to stroke incidence. This emotional stress is a risk factor that can be linked to structural and generational racism or other forms of discrimination or economic insecurity. . Each stroke can be viewed as an avoidable tragic failure in the complex interaction of multiple factors, including the health care system, society, and/or the individual.
Health Disparities Research: A call to action
Research has multiple roles to play in the effort to promote health equity in the U.S. The National Institute of Neurological Disorders and Stroke (NINDS) has had an active program in the study of health disparities for years. This includes the NINDS-funded REasons for Geographic And Racial Differences in Stroke (REGARDS), a large cohort study evaluating the causes of racial and geographic differences in stroke mortality and cognitive decline as well as potential targets for intervention. The REGARDS data show that the impact of higher blood pressure levels on stroke is three times greater for Black people than White people8. Another REGARDS study reported that only half of the increased risk of stroke in Black people could be explained by well-known factors9. Some or all of this increased risk for stroke mortality could be related to a combination of levels of racism, including structural, personally-mediated, and/or internalized racism 10. This result elevates the potential importance of understanding the biologic effects of structural and generational racism and other forms of discrimination or economic insecurity on cerebrovascular pathology. Studies also show that the increased burden of stroke in Black people compared to White people is greatest in mid-life and decreases in the elderly11. NINDS has recently launched a public health campaign12, called “Nobody’s Got You Like You Got You”13, to message the importance of controlling blood pressure during midlife for adult Black men (Figure 2).
Figure 2-.
A promotional flyer for NIH’s Mind Your Risks® public health campaign.
The National Institute of Neurological Disorders and Stroke (2021). Mind Your Risks® social media graphic. https://www.mindyourrisks.nih.gov/. Accessed 10/04/2021.
Compared to studies like REGARDS that identify health disparities, there have been few studies funded to determine which interventions might work, particularly on the scale that the problem demands. This imbalance is true throughout the NIH grant portfolio. A recent analysis by the NIH Office of Disease Prevention14 found that fewer than 1 in 6 health prevention projects funded by NIH included a randomized intervention15. Fewer than 1 in 25 included an intervention focused on minority health or health disparities. NINDS and NIH more broadly are committed to research that emphasizes assessing interventions that may be able to make a difference in attenuating these gaping health inequities. In the case of health disparities in stroke there is new emphasis from NINDS on devising and testing interventions that have the potential to benefit those who actively suffer a stroke, or who are at risk during their lifetime. We need to understand how inequities in our health care system, and/or biologic, social, or personal factors contribute to stroke risk. However, there are lives to be saved by implementing what already know at the risk of sounding hyperbolic, it is time to stop admiring the problem and do something about it. There is urgency for research to identify and validate those strategies that will matter in preventing tragic stroke for real people, today and tomorrow.
Rigor in health disparities research
A plan for such intervention studies will require executing a careful deliberate initiative based upon rigorous data collection, innovative methods, new tools, and strategic partnerships. The National Center for Advancing Translational Sciences (NCATS) translational science spectrum model operationalizes each stage of research along the path from the biologic basis of health and disease to interventions that improve the health of individuals and the public (Figure 3)16. Much more research is needed in the clinical implementation space. Progress may be slow but that is true about most of the disorders in the NINDS portfolio. Persistence, learning from parallel efforts across other disciplines, and seizing new scientific opportunities usually lead to better treatments. It will be critical to precisely identify the causal nature of those specific conditions that give rise to health disparities to appropriately match an intervention to the appropriate target. The drivers are complex, usually multiple, and may differ depending on the make-up of the community under study. The list is long and may include unequal access to healthcare, intergenerational poverty, low educational level, mistrust of the medical system, exposure to environmental toxins, unhealthy living conditions and stresses due to a variety of factors, including racism, stigma, migration, economic insecurity, fear, and unemployment. Due to the multifactorial nature, flattening the issue to one categorized simply as “race” is potentially counterproductive. Large genetic studies can provide biologic measures that are much more precise than the current simple classifications of race. In biomedical research, we need to be more precise than approximating ancestry through categories such as “Asian” or “African-American” when studying genetic determinants of disease. These imprecise groupings can be helpful in some settings but ignore the social determinants of health, racism, and discrimination. In 2003, Kaplan and Bennett offered a number of rational guidelines for the use of race and ethnicity in biomedical research that may be useful17.
Figure 3-.
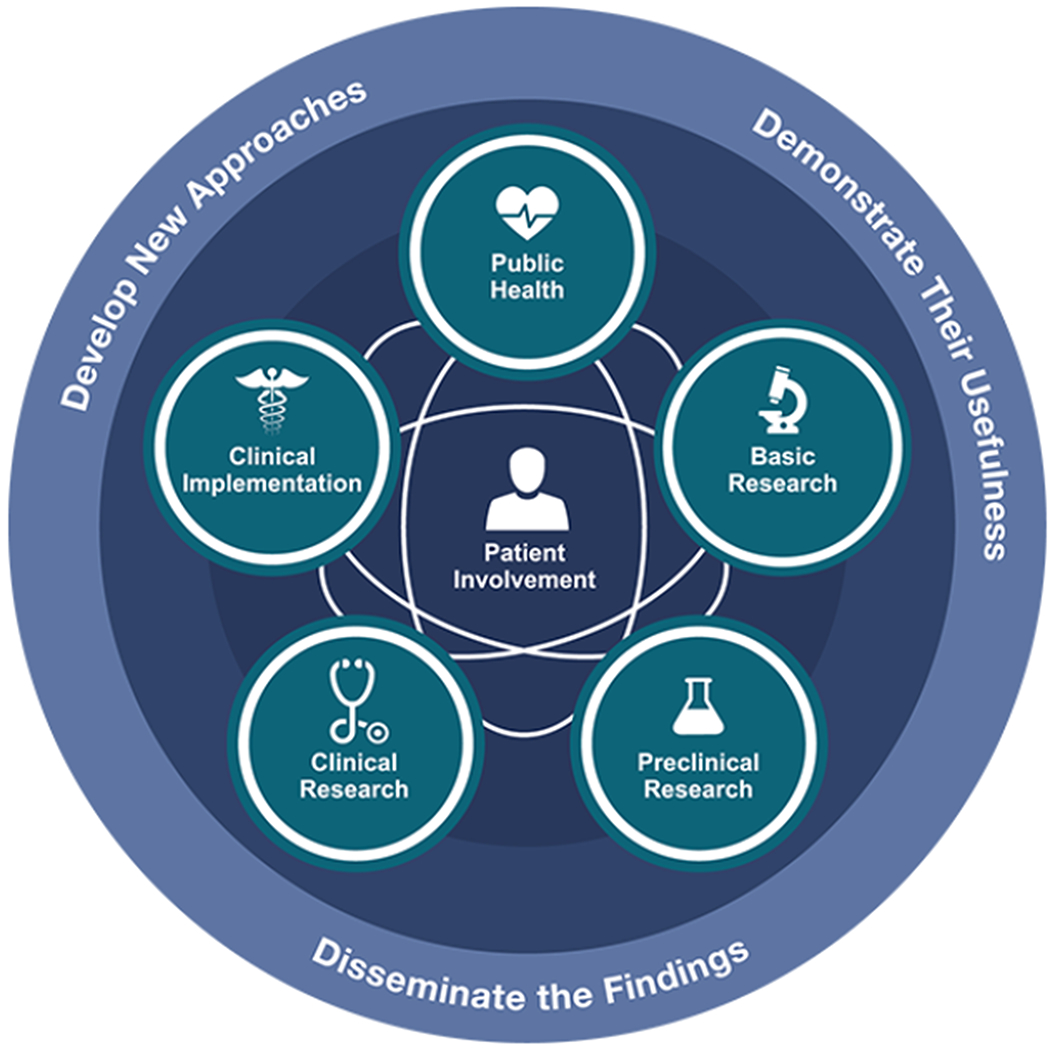
A representation of the translational science spectrum that depicts each stage of research along the path from the biological basis of health and disease to interventions that improve the health of individuals and the public. The spectrum is not linear or unidirectional; each stage builds upon and informs the others.
National Center for Advancing Translational Sciences (2021). Translational Science Spectrum. https://ncats.nih.gov/translation/spectrum. Accessed 10/04/2021.
When race and ethnicity are used as a study variable the reasons for its use should be carefully specified. This is to avoid the use of race/ethnicity as descriptors implying that specific causal mechanisms are not active and that the categories are mutually exclusive and exhaustive.
Investigators should specify how race and ethnicity were ascertained.
Race/ethnicity should not be used as surrogates for genetic variation.
The role of race/ethnicity needs to be defined as a risk factor vs. a risk marker.
In the interpretation of racial/ethnic differences, all conceptually relevant factors should be considered, including racism and discrimination, socioeconomic statues, social class, personal or family wealth, environmental exposures, insurance status, age, diet and nutrition, health beliefs and practices, educational level, language spoken, religion, tribal affiliation, country of birth, parents’ country of birth, length of time in the country of residence, and place of residence.
Challenges and opportunities in research to advance health equity.
Health disparity populations as defined by the NIH18 include those based on race, ethnicity, socioeconomic disadvantage, those living in or from underserved rural areas, and sexual and gender minorities (Figure 4)19. The heterogeneity and complexity of the drivers of health inequity cannot be underestimated. Many causes are rooted in deep-seated social/cultural/economic, environmental or behavioral differences that NIH-funded research is unlikely to influence in the short term but may inform in the long term (i.e., future policy changes)20. However, research informed by the drivers of inequities should realistically focus to customize the management of stroke prevention, acute treatment, and recovery to attenuate, or cancel, the effects of these deep-rooted disparities on the burden of stroke for disadvantaged communities. As in any scientific exercise, the set of confounders need to be measured, as they will have substantial influence on results of interventions. Research that tests interventions in ways that are informed by the gamut of determinants of health to identify best practices in healthcare will be the most impactful. Similarly, research that focuses on understanding the biology underlying specific vulnerabilities or resiliencies, or research that shows how to compensate for the destructive effects of broad inequities can build from the foundational research that NIH has already supported.
Figure 4-.
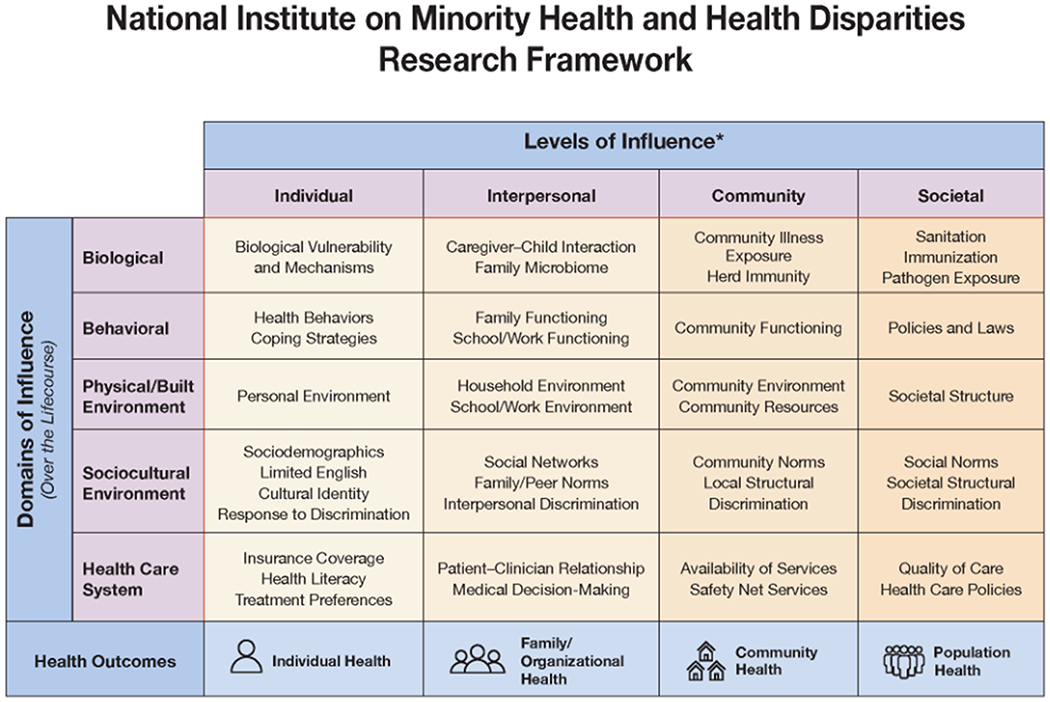
The NIMHD Minority Health and Health Disparities Research Framework reflects an evolving conceptualization of factors relevant to the understanding and promotion of minority health and to the understanding and reduction of health disparities. The framework serves as a vehicle for encouraging NIMHD- and NIH-supported research that addresses the complex and multi-faceted nature of minority health and health disparities, including research that spans different domains of influence (Biological, Behavioral, Physical/Built Environment, Sociocultural Environment, Healthcare System) as well as different levels of influence (Individual, Interpersonal, Community, Societal) within those domains. The framework also provides a classification structure that facilitates analysis of the NIMHD and NIH minority health and health disparities research portfolios to assess progress, gaps, and opportunities. Examples of factors are provided within each cell of the framework (e.g., Family Microbiome within the Interpersonal-Biological cell). These factors are not intended to be exhaustive. Health disparity populations, as well as other features of this framework, may be adjusted over time.
National Institute on Minority Health and Health Disparities (2017). NIMHD Research Framework. Retrieved from https://www.nimhd.nih.gov/about/overview/research-framework.html. Accessed on 10/04/2021.
The multi-component nature of the problems leading to health inequity also underlines the need for powerful partners in doing the research that matters most to real people. Stroke risks have so much in common with risk for cardiovascular disease; the National Heart Lung and Blood Institute (NHLBI) at NIH is a natural partner to NINDS in these interventional studies. Interventions aimed at a health-promoting behavior change need to be linked to a sustainable economic model for them to be employed on the scale needed to impact health. Identifying an intervention that works in one small population but is not scalable will bear little fruit. Research that establishes best practices for individuals with a particular set of causal conditions common to a disadvantaged community are useful if they can inform the practice guidelines of professional societies or healthcare systems.
In 2011, NINDS solicited applications for its Stroke Prevention/Intervention Research Program (SPIRP) targeting disparities in stroke21. Four multi-project cooperative agreements were funded that addressed major stroke disparities research gaps and included dissemination planning, training/education, and community outreach as major components. One of these was embedded in the Kaiser Permanente Northern California (KPNC) health system. That system has made significant progress in improving hypertension control across racial/ethnic participants22. The Centers for Medicare and Medicaid Services (CMS) reported that “from 2009 to 2017, the percentage of African American Medicare members with controlled hypertension increased from 75.3 percent to 89.6 percent. During this time, as a result of Kaiser Permanente’s focused and sustained efforts, the Black people –White people disparity in hypertension control rates was reduced from a high of 5.3 percentage points to 2.2 points (a 58 percent decrease). Throughout this period, hypertension control rates for all racial and ethnic groups have consistently surpassed the national 90th percentile for Medicare members23.” These data reinforce the power of interventions in the healthcare systems to effect change. Research based on rigorous NIH-funded studies that is performed in the healthcare system setting with commitments by the system to implement clinically significant improvements offer the opportunity to improve health outcomes for people in relatively short periods. The NIH Common Fund developed the necessary infrastructure in the Healthcare Systems Collaboratory24 to engage health care delivery organizations like clinics or hospitals as research partners in the conduct of pragmatic clinical trials to help improve provider decision making and patient outcomes25.
COVID-19 pandemic
In many circumstances, trust between the investigator and the disadvantaged community in which research is conducted cannot be assumed but must be earned. The COVID pandemic, which took a disproportionate toll in illness and death in disadvantaged communities, reignited the importance of establishing trust between investigator and subject. Tremendous effort is needed to afford everyone the same health benefit offered by vaccination and testing. The goal of the NIH RadX UP26 program is to understand the factors associated with disparities in COVID-19 morbidity and mortality and to lay the foundation to reduce disparities for the underserved and vulnerable populations who are disproportionately affected. Lessons are many but establishing trust in the community is the crucial step and it does not happen without effort and persistence. One particular strategy involves encouraging collaboration between the research program sites and the community — tribal health centers, houses of worship, homeless shelters, and even prison systems — to identify and address their unique needs. Therefore, the creation of health disparities research networks must be considered as we move forward, with the goal of engaging communities in the design of studies, garnering support for the research, boosting diversity recruitment in clinical trials, and reporting back the results of the studies.
Diversity of the research workforce
A major challenge for health disparities research is the lack of investigators who are from or live in the disadvantaged communities or understand the nuances of messaging and listening, which can lead to very slow or non-acceptance of the investigators as trusted partners. Less than 2% of neurologists or NINDS principle investigators on R01 grants are African American. However, the challenge of advancing health equity cannot rest solely on those who originated in the groups at risk. It is a burden that must be borne by all, but as academics we should be aware that it is much more important to care about the difficulties of real people in disadvantaged communities, and figure out what we can do to help them, than how much we publish. Recruiting and training investigators and study staff from the populations of interest can be extremely beneficial. This should include recruiting subjects from disadvantaged backgrounds into patient-engagement groups to participate in the design and execution of the research. It is critical to build in patient engagement from the very start. Elevate patients to equals in study design, execution, and communication of results. Avoid tokenism and don’t separate the patients and the investigators. Reimburse those with lived experience for their time, as you would any investigator. Persons who have suffered a stroke, or cared for someone who has, are likely more effective communicators with potential subjects, their families, and other audiences in their communities. Contributing to a research study also provides fulfillment for patients who are engaging in the study. These types of relationships can inform the research over the long term to focus on what matters most to people. Most importantly, over time these relationships serve to build trust in communities where it is lacking.
Conclusion
The national conscience has opened to a new appreciation for the need for action to promote health equity and end the web of conditions that have perpetuated unhealthy disparities in stroke. Each stroke is an example of a failure in the interaction of one or more of these levels: the health care system, society, or a personal level. These failures have tragic effects on individuals, families, and society. It is cruel and unfair that something as devastating as stroke is determined by where one lives in our country. NINDS, along with other Institutes at the NIH, are developing much more aggressive research plans to inform action that can enable all our communities to benefit from the advances in stroke prevention and treatment.
Under the leadership of Dr. Richard Benson and the Office of Global Health and Health Disparities, NINDS is developing a strategic plan to promote neurological health equity. We invite the entire stroke community to provide input and to help shoulder the responsibility for not failing to do the research that will matter to real people.
Abbreviations:
- NIH
The National Institutes of Health
- NINDS
The National Institute of Neurological Disorders and Stroke
Footnotes
Disclosures: None
Contributor Information
Richard Benson, NINDS, Division of Clinical Research, Office of Global Health and Health Disparities, Director, 6001 Executive Boulevard, Room 2192, Bethesda, MD 20892
Walter J. Koroshetz, NINDS DirectorRm, 852a, Building 31, National Institute of Health, Bethesda, MD 20892-2540.
References:
- 1.Core Functions, Office of Health Equity, Health Resources & Services Administration https://www.hrsa.gov/about/organization/bureaus/ohe/index.html. Accessed July 20, 2021.
- 2.NIH stands against structural racism in biomedical research. The NIH Director. https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-stands-against-structural-racism-biomedical-research. Accessed July 20, 2021.
- 3.Transformative research to address health disparities and advance health equity. NIH Office of Strategic Coordination- The Common Fund. https://commonfund.nih.gov/healthdisparitiestransformation. Accessed July 20, 2021.
- 4.Sacco RL. Stroke Disparities: From Observations to Actions. Stroke. 2020; 51:3392–3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. [PubMed] [Google Scholar]
- 6.Stroke maps and data sources. CDC statistics & maps. https://www.cdc.gov/stroke/maps_data.htm. Accessed July 20, 2021.
- 7.Schieb LJ, Greer SA, Ritchey MD, George MG, Casper ML. Vital Signs: Avoidable Deaths from Heart Disease, Stroke, and Hypertensive Disease — United States, 2001–2010. CDC Morbidity and Mortality Weekly Report. 2013; 62:721–727’ [PMC free article] [PubMed] [Google Scholar]
- 8.Howard G, Lackland DT, Kleindorfer DO, Kissela BM, Moy CS, Judd SE, Safford MM, Cushman M, Glasser SP, Howard VJ. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard G, Cushman M, Kissela BM, Kleindorfer DO, McClure LA, Safford MM, Rhodes JD, Soliman EZ, Moy CS, Judd SE, et al. ; Traditional risk factors as the underlying cause of racial disparities in stroke: lessons from the half-full (empty?) glass. Stroke. 2011;42:3369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams O, Ovbiagele B. Stroking Out While Black-The Complex Role of Racism. JAMA Neurol. 2020; 77:1343–1344. [DOI] [PubMed] [Google Scholar]
- 11.Gerber Y, Rana JS, Jacobs DR, Yano Y, Levine DA, Nguyen-Huynh, Lima JAC, Reis JP, Zhao L, Liu K, et al. Pressure Levels in Young Adulthood and Midlife Stroke Incidence in a Diverse Cohort, Hypertension. 2021; 77:1683–1693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mind Your Risks®. NIH. https://www.mindyourrisks.nih.gov. Accessed July 20, 2021.
- 13.Nobody’s Got You, Like You Got You. NIHNINDS Youtube channel. https://www.youtube.com/watch?v=gte5j2S0RuY. Accessed July 20, 2021.
- 14.ODP Study Suggests the U.S. Could Benefit from More Prevention Research on Leading Risk Factors and Causes of Death and Disability. NIH Office of Disease Prevention Director’s Message. https://prevention.nih.gov/about-odp/directors-messages/2019/odp-study-suggests-us-could-benefit-more-prevention-research-leading-risk-factors-and-causes-death. Accessed July 20, 2021. [Google Scholar]
- 15.Vargas AJ, Schully SD, Villani J, Caballero LG, Murray DM. Assessment of Prevention Research Measuring Leading Risk Factors and Causes of Mortality and Disability Supported by the US National Institutes of Health. JAMA Network Open. 2019; 2:e1914718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Translational Science Spectrum. National Center for Advancing Translational Sciences. https://ncats.nih.gov/translation/spectrum#basic-research. Accessed July 20, 2021.
- 17.Kaplan JB and Bennett T. Use of Race and Ethnicity in Biomedical Publication. JAMA. 2003; 289:2709–2716. [DOI] [PubMed] [Google Scholar]
- 18.Overview. National Institute on Minority Health and Health Disparities. https://www.nimhd.nih.gov/about/overview/. Accessed July 20, 2021.
- 19.NIMHD Research Framework. National Institute on Minority Health and Health Disparities. https://www.nimhd.nih.gov/about/overview/research-framework/nimhd-framework.html. Accessed July 20, 2021.
- 20.Adler NE, Glymour MM, Fielding J. Addressing Social Determinants of Health and Health Inequalities. JAMA. 2016. Oct 25;316(16):1641–1642. doi: 10.1001/jama.2016.14058. [DOI] [PubMed] [Google Scholar]
- 21.Pahigiannis K, Waddy SP, Koroshetz W. Toward Solutions for Minimizing Disparities in Stroke. Stroke. 2013;44:e129–e130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and Ethnic Disparities among Enrollees in Medicare Advantage Plans. NEJM 2014; 371:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Past Centers for Medicare & Medicaid Services (CMS) Health Equity Award Winners. https://www.cms.gov/About-CMS/Agency-Information/OMH/equity-initiatives/Past-Health-Equity-Award-Winners. Accessed July 20, 2021.
- 24.Program Snapshot, NIH Health Care Systems (HCS) Research Collaboratory. NIH Office of Strategic Coordination- The Common Fund. https://commonfund.nih.gov/hcscollaboratory. Accessed July 20, 2021.
- 25.Health Care Systems (HCS) Research Collaboratory’s Health Relevance. https://commonfund.nih.gov/hcscollaboratory/public. Accessed July 20, 2021.
- 26.Rapid Acceleration of Diagnostics (RADX) Programs. NIH. https://www.nih.gov/research-training/medical-research-initiatives/radx/radx-programs#radx-up. Accessed July 20, 2021.


