Abstract
Skin and soft tissue infections (SSTIs) are the most common medical complication of injection drug use in the U.S., though little work has been done assessing SSTI treatment among people who inject drugs (PWID). We examined past-3-month abscess characteristics, treatment utilization, and barriers to medical treatment among N=494 community-recruited PWID. We used descriptive statistics to determine the frequencies of self- and medical treatment for their most recent past-3-month abscess as well as barriers to seeking medical treatment. We then used bivariate and multivariate logistic regression to identify factors associated with having an abscess in the past 3 months. Overall, 67% of participating PWID ever had an abscess and 23% had one in the past 3 months. Only 29% got medical treatment for their most recent abscess whereas 79% self-treated. Methods for self-treatment included pressing the pus out (81%), applying a hot compress (79%), and applying hydrogen peroxide (67%). Most (91%) self-treated abscesses healed without further intervention. Barriers to medical treatment included long wait times (56%), being afraid to go (49%), and not wanting to be identified as a PWID (46%). Factors associated independently with having an abscess in the past 3 months were injecting purposely into muscle tissue (adjusted odds ratio (AOR)= 2.64), having difficulty finding a vein (AOR=2.08), and sharing injection preparation equipment (AOR=1.74). Our findings emphasize the importance of expanding community-based access to SSTI education and treatment services, particularly at SSPs where PWID may be more comfortable seeking resources.
Keywords: Skin and soft tissue infection (SSTI), abscess, people who inject drugs (PWID), injection drug use (IDU), treatment barrier, community-based treatment, syringe service program (SSP)
Introduction
Skin and soft tissue infections (SSTIs) are the most common medical complication of injection drug use (IDU) in the U.S. (Visconti, Sell, & Greenblatt, 2019), with an estimated 540,000 IDU-associated SSTIs occurring annually between 2013 and 2017 (See et al., 2020). In the same time period, approximately 98,000 emergency department (ED) visits occurred each year for SSTIs related to IDU (See et al., 2020). SSTIs are generally managed acutely in ambulatory settings with antibiotics and/or incision and drainage. SSTI treatment may require hospitalization if there are signs of systemic infection (Visconti et al., 2019). Without prompt care, severe SSTIs can progress and develop into life-threatening conditions, including endocarditis, necrosis, and sepsis. These morbidities often require longer hospital stays and may lead to mortality in some cases (Binswanger et al., 2008). In turn, they impose an even greater burden on the U.S. healthcare system than the initial SSTI (See et al., 2020).
Despite the potentially serious consequences associated with going without medical care for an SSTI, people who inject drugs (PWID) often forgo medical treatment and self-treat instead (e.g., Asher, Zhong, Garfein, Cuevas-Mota, & Teshale, 2019; Harris, Richardson, Frasso, & Anderson, 2018; Hope, Ncube, Parry, & Hickman, 2015; Wright et al., 2020). Few U.S.-based studies have assessed the factors associated with whether someone suffering from an SSTI will self-treat or seek medical care for their infection, but limited evidence suggests that PWID with a higher incidence of recent abscesses (Monteiro et al., 2020), who have received prior SSTI treatment in an ED (Monteiro et al., 2020), who inject more frequently (Fink, Lindsay, Slymen, Kral, & Bluthenthal, 2013), and/or who identify as Hispanic/Latino (Fink et al., 2013) are more likely to self-treat. Common self-treatment strategies include draining the abscess with a syringe and/or knife; applying a hot compress; and/or cleaning the infected area with alcohol, peroxide, or another cleaner (e.g., Asher et al., 2019; Gilbert, Hellman, Wilkes, Rees, & Summers, 2019; Monteiro et al., 2020). In many cases, PWID report that their abscess resolves with self-treatment (Pollini et al., 2010). However, in more severe cases, individuals will need antibiotics for their infection to resolve and, in turn, they may end up purchasing non-prescribed oral antibiotics on the street (Gilbert et al., 2019) and/or seeking medical care after a period of unsuccessful self-treatment (e.g., Gilbert et al., 2019; Summers, Hellman, MacLean, Rees, & Wilkes, 2018; Wright et al., 2020). Indeed, a recent study found that 79% of people who inject heroin waited at least two days, and 38% waited two or more weeks, to seek medical care for an abscess (Summers et al., 2018).
PWID report that they delay/avoid seeking medical care for various reasons, with the most common including drug-related stigma and discrimination experienced in healthcare settings, fear surrounding the possibility of withdrawal and/or inadequate pain control during hospitalization, and worries about addressing other commitments during hospitalization (Gilbert et al., 2019; Harris et al., 2018; Paquette, Syvertsen, & Pollini, 2018; Summers et al., 2018). However, very few studies have investigated the barriers to seeking treatment specific to SSTIs among PWID. In addition to general healthcare utilization barriers, SSTI-specific barriers identified to date include being afraid that SSTI treatment will be painful (Summers et al., 2018) and believing that the infection isn’t serious enough to require medical treatment (Monteiro et al., 2020). The belief that an SSTI will resolve with self-treatment leads to concerning self-care strategies regarding consumption of non-prescribed oral antibiotics and the risk of draining/lancing procedures that are completed without proper medical training (Gilbert et al., 2019). Even for PWID who seek medical care for an SSTI, delayed presentation and complications from invasive self-treatment often require more complex medical management in an ED (Summers et al., 2018) and greater likelihood of hospitalization with lengthy inpatient stays (Binswanger et al., 2008).
To reduce SSTI prevalence and ultimately societal healthcare burden, identifying the factors associated with SSTI development among PWID is crucial. A recent systematic review on IDU-related injury and disease (Larney, Peacock, Mathers, Hickman, & Degenhardt, 2017) concluded that there is a dearth of research on the risk and protective factors for such injection-related complications, and few studies have been conducted among U.S. samples. Overall, U.S. studies suggest that abscess formation is associated with being female (Smith, Robinowitz, Chaulk, & Johnson, 2015; Wurcel et al., 2018), injecting subcutaneously (Pirozzi, Van, Pontious, & Meyr, 2014; Smith et al., 2015; Summers, Struve, Wilkes, & Rees, 2017) or intramuscularly (Murphy et al., 2001) rather than intravenously, injecting more frequently (Asher et al., 2019; Phillips, Anderson, Herman, Liebschutz, & Stein, 2017), having more injection partners (Asher et al., 2019), injecting black tar heroin (vs powder heroin) (Ciccarone et al., 2001; Summers et al., 2017), and sharing injection equipment, including drug cookers and syringes (Asher et al., 2019). Importantly, some of these factors can be mitigated, at least in part, by engaging in protective behaviors, such as cleaning the skin prior to injecting (Kenney et al., 2020; Murphy et al., 2001) and obtaining sterile syringes from authorized sources such as syringe service programs (SSPs; Tomolillo, Crothers, & Aberson, 2007) and pharmacies.
U.S.-based studies investigating SSTI characteristics and treatment have concentrated on PWID in the urban areas of San Francisco (Murphy et al., 2001), San Diego (Asher et al., 2019), Sacramento (Summers et al., 2017), Boston (Phillips et al., 2017; Summers et al., 2017), Philadelphia (Harris et al., 2018), and Baltimore (Smith et al., 2015). Currently, it is unclear whether the factors associated with SSTI development and treatment in these urban areas are the same as those in predominantly rural areas of the U.S. where there is less sterile syringe access via authorized sources like SSPs (Des Jarlais et al., 2015; Paquette & Pollini, 2018). To our knowledge, there have been no studies that assess abscess and related treatment characteristics among PWID in a largely rural region of the U.S. Therefore, the purpose of this study was to examine abscess characteristics, treatment utilization, and barriers to medical treatment among PWID in Fresno, California, which is an urban hub located in California’s predominantly rural Central Valley (U.S. Department of Justice, 2010).
Method
Study Site
Fresno, California is an urban hub situated within California’s Central Valley, a predominantly rural and agricultural region. The Valley is one of the most rapidly developing regions in California, yet it is also one of the most poverty-stricken (Lewis, Burd-Sharps, & Sachs, 2010). Rates of IDU per capita in Fresno are among the highest in the U.S. (Brady et al., 2008), with heroin and methamphetamine being the most common drugs of choice (Syvertsen, Paquette, & Pollini, 2017). Interstate 5 runs north-south through California and serves as a primary drug trafficking route for black tar heroin sourced from Mexico (Drug Enforcement Administration, 2019). In turn, black tar heroin is the most prevalent type of heroin in the Western U.S. (Drug Enforcement Administration, 2019), leading to high rates of use in the Central Valley (U.S. Department of Justice, 2010). As noted above, black tar heroin use is a significant risk factor for SSTI development. Despite the notably high rates of IDU in Fresno, at the time of our study the Fresno Needle Exchange Program was the only SSP that operated regularly in this region (two hours per week on Saturdays). In addition to being a source in the community for sterile syringes in the Central Valley, the Fresno Needle Exchange Program offers educational resources, HIV/HCV testing, naloxone distribution, and on-site abscess treatment services (NASEN, 2020).
Study Population and Recruitment
All procedures were approved by the University’s Institutional Review Board and all participants provided informed consent. PWID were recruited from Fresno and the surrounding communities between April and September of 2016 using respondent-driven sampling (RDS) (Heckathorn, 1997), which is a sampling method used commonly for recruiting hard-to-reach populations like PWID. We first selected 11 initial participants (“seeds”) who differed with respect to age, race/ethnicity, gender, and drug(s) of choice. Each seed was given three coupons with unique identifier codes to refer peers for study participation. As participants completed the survey, they were given three additional uniquely coded coupons to refer additional peers. This continued until the initial participant seeds recruited an additional 483 participants (total N=494). This final sample size approximated the desired sample size from pre-study considerations of statistical power (≥80%) with a significance level of p<0.05, which was N=500 participants. Eligibility criteria were: being at least 18 years of age, injecting at least twice in the past month, and being willing and able to provide informed consent.
Data Collection
Interested individuals were screened for eligibility after bringing a coded RDS coupon to the study office. If participants met eligibility criteria, staff explained the study requirements. Individuals interested in participation provided informed consent and immediately completed the survey. Surveys were interviewer-administered to participants and responses were recorded using Qualtrics survey software (Version 13; Qualtrics, Provo, UT). The survey included questions related to demographics, injection behaviors, syringe sources, criminal justice, abscess characteristics, and healthcare utilization (specific questions included in the current study are provided below). Participants were paid $30 for survey completion, which took approximately 1 hour, and an additional $5 for up to three additional persons recruited (maximum payment $45).
Measures
Participant characteristics
Demographic characteristics included age, gender, marital status, parental status, race/ethnicity, and housing status. For housing status, homelessness was defined as reports of sleeping most often in a vehicle, shelter, abandoned building, shooting gallery, or outside in the past 3 months. Participants also reported the number of years they had been injecting, number of injections in the past month, average number of hours spent on the street each day in the past 3 months, and whether they had traded sex for drugs in the past 3 months.
Recent abscess characteristics
A single dichotomous outcome variable was used that identified participants who self-reported having an abscess in the past 3 months. For their most recent past 3-month abscess, participants reported its location and associated symptoms. We considered an abscess with oozing pus and/or an open wound to be “severe” and an abscess without oozing pus or an open wound to be “mild to moderate.”
Abscess treatment characteristics
Four abscess treatment groups were created based on how participants reported self- and/or medically treating their most recent past 3-month abscess: 1) self-treated only; 2) medically treated only; 3) self then medically treated; and 4) neither. Participants who self-treated reported on their methods for doing so. Participants who medically treated reported on where they received medical treatment and rated their quality of medical care at each facility based on the following response options: Excellent, Good, Acceptable, Fair, and Poor.
Barriers to abscess medical treatment
Participants who reported ever having an abscess were asked, “Have you ever thought you needed treatment for an abscess but didn’t go?” Participants who responded “yes” to this question were further prompted to indicate their reasons for not getting abscess treatment when they thought they needed it. Response options included: a) afraid to go; b) thought you would be treated badly by medical staff; c) didn’t want to be identified as a person who injects drugs; d) didn’t know where to go; e) wait times are too long; f) had bad experiences with abscess treatment before; g) have seen others have bad experiences with abscess treatment before; h) had outstanding warrants; i) no insurance/couldn’t afford treatment; and j) afraid of the treatment.
Self-reported injection behaviors
Assessment of injection behaviors was limited to the past 3 months to maximize temporality with regard to the 3-month abscess outcome variable. Dichotomous variables were included for injecting daily, type(s) and combination(s) of drugs injected, purposely injecting into muscle, purposely injecting under skin, difficulty finding a vein, injection preparation equipment (cooker(s), filter(s), rinse water)/syringe sharing and reuse, syringe source(s), and cleaning procedures). Syringe sources were split into 3 categories: obtaining syringes only from authorized sources (including SSPs, pharmacies, doctors, clinics, hospitals, veterinary clinics, online purchases), obtaining syringes only from unauthorized sources (friends, people on the street, drug dealers, spouses/partners/sexual partners, family members, shooting gallery, discarded syringes on the street/ground, sex work clients, any “other” reported sources), and obtaining syringes from a combination of authorized and unauthorized sources.
Data Analysis
All data regarding abscess characteristics, correlates, treatment, and barriers to treatment were summarized using descriptive statistics. We further evaluated abscess correlates by comparing participant characteristics, and self-reported injection behaviors between PWID who had an abscess in the past 3 months and those who did not using chi-square tests for categorical variables and independent-samples t-tests for continuous variables. Variables with a significance of p<0.10 in these bivariate analyses (chi-square or independent-samples t-tests) were entered into a multiple logistic regression model in a stepwise fashion to identify factors independently associated with having an abscess in the past 3 months. Specifically, variables (p<0.10) were entered one by one beginning with those that had the smallest p values. Variables with p>.05 were removed during each step and only variables at p<0.05 were retained in the final model. To account for any bias introduced by RDS, we adjusted the final model using network size and recruiter abscess status as covariates. There were no significant differences between the adjusted and unadjusted final multiple regression models, so only the unadjusted model is presented. All analyses were performed using R statistical software version 3.5.1 (http://www.r-project.org/). Because we documented very low levels of missing data (<3%) and missingness was not associated with any variables of interest, we used pairwise deletion to deal with missing data. Pairwise deletion resulted in participants being included in analyses for variables in which they provided data, but not in analyses for variables in which they did not provide data.
Results
Abscess characteristics
Figure 1 shows abscess prevalence among our sample. More than half of PWID reported ever having an abscess (67%); the median number of lifetime abscesses was 5 (interquartile range (IQR)=2–10). Approximately one-third (34%) of participants who reported having at least one abscess also had at least one abscess in the past 3 months. For participants’ most recent past-3-month abscess, common locations included the arm (49%) or leg (26%). Less common locations were on the torso (10%), buttocks (4%), hand (4%), foot (2%), neck (2%), groin (2%), or head (1%). Almost all most recent past-3-month abscesses included redness (98%), swelling (98%), pain (96%), heat (91%), and/or pus being present under the skin (86%). Fewer, but still many, included oozing pus (72%) and/or an open wound (58%). Less common symptoms included those specific to the abscess—discolored skin (51%) and red streaks (27%)—while others were systemic in nature—fever (48%) and vomiting (17%). Most past-3-month abscesses (74%) were “severe”; only 26% were considered to be “mild/moderate.”
Figure 1.
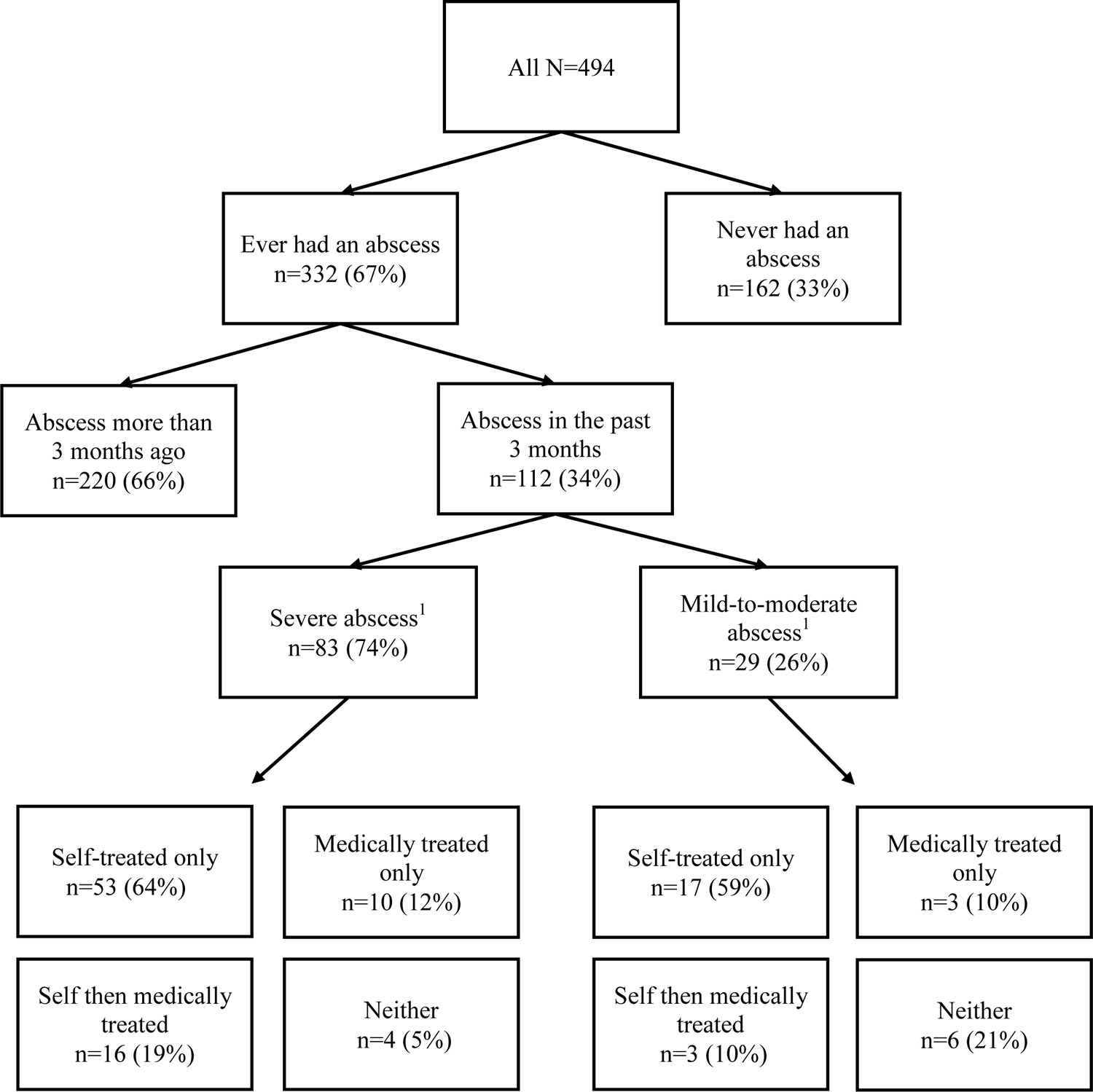
Abscess and treatment prevalence for people who inject drugs (PWID).
1Severe abscess defined as having oozing pus and/or an open wound; mild-to-moderate abscess defined as not having oozing pus or an open wound.
Most recent abscess treatment characteristics
Shown in Figure 1 and Table 1, most participants with an abscess in the past 3 months self-treated and less than one-third got medical treatment. Among participants with a mild/moderate abscess, the majority only self-treated. Notably, a majority of participants who self-treated their abscess reported that it healed. Despite the increase in severity, a similar treatment pattern was found for participants with a severe abscess in the past 3 months, with the majority self-treating in the absence of, or prior to, medical treatment.
Table 1.
Past-3-month abscess treatment characteristics among people who inject drugs (PWID).
| n (%) | |
|---|---|
| N=112 | |
| Self-treated last abscess | 89 (79) |
| How last abscess was self-treated: | |
| Pressed pus out | 72 (81) |
| Hot compress | 70 (79) |
| Hydrogen Peroxide | 60 (67) |
| Antibiotic ointment | 56 (63) |
| Oral antibiotics | 47 (53) |
| Drained with a syringe | 35 (39) |
| Drained with a knife | 32 (36) |
| Soaked/applied salt water | 30 (34) |
| Aloe or other ointment | 29 (33) |
| Cold compress | 16 (18) |
| Put potato on it | 4 (4) |
| Self-treated abscess healed | 81 (91) |
| Got medical treatment for last abscess | 32 (29) |
| Location of medical treatment for last abscess: | |
| Emergency department | 20 (63) |
| Inpatient hospital | 7 (22) |
| Syringe service program (SSP) | 6 (19) |
| Health clinic | 3 (9) |
| Private physician’s office | 2 (6) |
Table 1 shows the method(s) that participants used to self-treat their abscesses. The majority reported that they pressed the pus out, applied a hot compress, applied hydrogen peroxide, applied antibiotic ointment, took oral antibiotics, and/or drained the abscess with a syringe and/or knife. Half of participants who self-treated and reported taking oral antibiotics got them from someone they know or on the street (51%), while the other half took oral antibiotics that they had left over from a healthcare facility for a prior infection (49%).
For those who sought medical treatment, the majority did so from an ED and/or other inpatient hospital setting; fewer participants got medical treatment from an SSP, health clinic, and/or private physician’s office. Overall, quality ratings were high at each facility type, with 70% of ED ratings, 86% of inpatient hospital ratings, 100% of SSP ratings, 67% of health clinic ratings, and 100% of private physician ratings being “Acceptable” quality of care or better. Still, “Excellent” and “Poor” quality ratings differed as a function of facility type. “Excellent” ratings were provided for 20% of ED, 57% of inpatient hospital, 83% of SSP, 33% of health clinic, and 0% of private physician visits. “Poor” ratings were provided for 20% of ED, 14% of inpatient hospital, 0% of SSP, 0% of health clinic, and 0% of primary physician visits.
Barriers to abscess medical treatment
Among participants who ever had an abscess, 60% did not seek treatment when they thought they needed it on at least one occasion. The most common barrier was wait times being too long, with over half of the sample (56%) indicating that this was the primary reason they did not get treatment. Other obstacles included being afraid to go (49%), not wanting to be identified PWID (46%), being afraid of the treatment itself (42%), seeing others have bad experiences (44%), and thinking medical staff would treat them poorly (41%). Fewer, but still a notable portion of, participants reported having bad prior experiences (29%), not having insurance (27%), and having an outstanding warrant (22%) as barriers to seeking medical treatment.
Factors associated with having an abscess in the past 3 months
Bivariate comparisons between PWID with and without an abscess in the past 3 months are shown in Table 2. Of 494 participants, 38% were female, 50% were married or in a steady relationship, 74% had one or more children, 43% were Hispanic/Latino, and the median age was 46 years. Median years injecting was 22 and the most frequently reported drugs injected in the past 3 months were black tar heroin by itself (81%), methamphetamine by itself (57%), and/or heroin and methamphetamine or cocaine together (46%). A larger percentage of participants with a past-3-month abscess reported injecting heroin, injecting into the muscle and/or under the skin on purpose, having difficulty finding a vein when injecting, and engaging in injection preparation equpment sharing (i.e., cooker(s), filter(s), and/or rinse water). Participants with a past-3-month abscess were also more likely to reuse their own filter(s) and to get syringes from a mixture of authorized and unauthorized sources.
Table 2.
Factors associated with having an abscess in the past 3 months among people who inject drugs (PWID) in bivariate analyses.
| n (%) | p value1 | |||
|---|---|---|---|---|
| Total N=494 | Abscess in past 3 months (n=112) | No abscess in past 3 months (n=382) | ||
| Median age (IQR) | 46 (33–54) | 46.5 (33–54) | 46 (33–54) | 0.931 |
| Gender | ||||
| Female | 190 (38) | 43 (38) | 147 (38) | 0.571 |
| Male | 299 (61) | 67 (60) | 232 (61) | |
| Transgender | 5 (1) | 2 (2) | 3 (1) | |
| Marital Status | ||||
| Married or in a steady relationship | 247 (50) | 61 (54) | 186 (49) | 0.556 |
| Single | 187 (38) | 39 (35) | 148 (39) | |
| Divorced, separated, or widowed | 47 (10) | 12 (11) | 48 (13) | |
| Have child(ren) | 364 (74) | 78 (70) | 286 (75) | 0.326 |
| Race/ethnicity | ||||
| White | 211 (43) | 46 (41) | 165 (43) | 0.080 |
| Mexican, Mexican American, or Hispanic/Latino | 167 (34) | 37 (33) | 131 (34) | |
| American Indian/Alaskan Native | 27 (5) | 12 (11) | 15 (4) | |
| Black/African American | 26 (5) | 3 (3) | 23 (6) | |
| Multiracial | 30 (6) | 8 (7) | 22 (6) | |
| Other | 33 (7) | 6 (5) | 26 (7) | |
| Homeless2 | 152 (31) | 43 (38) | 109 (29) | 0.052 |
| Median years injecting (IQR) | 22 (7–35) | 23 (8.5–35.25) | 21 (7–35) | 0.688 |
| Median times injected drugs in the past month (IQR) | 40 (18–90) | 60 (30–92.5) | 35 (15–90) | 0.121 |
| Median hours spent on the street per day2 | 10 (4–19.5) | 12 (5–20) | 8 (4–18.25) | 0.119 |
| Traded sex for drugs2 | 38 (8) | 9 (8) | 29 (8) | 1.000 |
| Ever been discriminated against for drug use | 377 (76) | 86 (77) | 291 (76) | 0.995 |
| Injection drug use2 | ||||
| Inject at least once per day | 293 (59) | 74 (66) | 219 (57) | 0.122 |
| Type(s) of drugs injected | ||||
| Heroin by itself | 407 (82) | 100 (89) | 307 (80) | 0.042 |
| Black tar heroin by itself | 399 (81) | 98 (88) | 301 (79) | 0.055 |
| Brown powder heroin by itself | 160 (32) | 45 (40) | 115 (30) | 0.059 |
| White powder heroin by itself | 43 (9) | 11 (10) | 32 (8) | 0.775 |
| Methamphetamine by itself | 280 (57) | 58 (52) | 222 (58) | 0.280 |
| Powder or crack cocaine by itself | 78 (16) | 19 (17) | 59 (15) | 0.810 |
| Heroin and methamphetamine or powder/crack cocaine together | 226 (46) | 59 (53) | 167 (44) | 0.117 |
| Purposely injected into muscle | 190 (38) | 65 (58) | 125 (33) | <0.001 |
| Purposely injected under skin | 90 (18) | 29 (26) | 61 (16) | 0.024 |
| Difficult to find a vein when injecting | 381 (77) | 99 (88) | 282 (74) | 0.002 |
| Injection equipment sharing and reuse | ||||
| Distributive syringe sharing | 145 (29) | 35 (31) | 110 (29) | 0.701 |
| Receptive syringe sharing | 133 (27) | 38 (34) | 95 (25) | 0.078 |
| Cooker, filter, and/or rinse water sharing | 334 (68) | 87 (78) | 247 (65) | 0.013 |
| Used syringe to divide/share drugs | 304 (62) | 74 (66) | 230 (60) | 0.327 |
| Reused own filter | 292 (59) | 75 (67) | 217 (57) | 0.033 |
| Reused own syringe(s) | 398 (81) | 97 (87) | 301 (79) | 0.089 |
| Cleaning procedures | ||||
| Always wash hands before preparing drugs | 182 (37) | 104 (93) | 342 (90) | 0.387 |
| Always swab injection site before injecting | 114 (23) | 84 (75) | 279 (73) | 0.770 |
| Always use sterile water to prepare drugs | 147 (30) | 78 (70) | 275 (72) | 0.629 |
| Syringe source(s) | ||||
| Authorized source(s)3 only | 105 (21) | 30 (27) | 75 (20) | 0.019 |
| Unauthorized source(s)4 only | 163 (33) | 25 (22) | 138 (36) | |
| Mix of authorized and unauthorized source(s) | 226 (46) | 57 (51) | 169 (44) | |
IQR=interquartile range;
Chi-square tests for categorical variables and independent-samples t-tests for continuous variables;
Past 3 months;
Authorized sources defined as syringe exchange programs, pharmacies, doctors, clinics, hospitals, veterinary clinics, and online purchases;
Unauthorized sources defined as friends, people on the street, drug dealers, spouses/partners/sexual partners, family members, shooting gallery, discarded syringes on the street/ground, sex work clients, and any “other” reported sources.
Table 3 shows the factors that were independently associated with having an abscess in the past 3 months in the multiple logistic regression model. Compared to those without a past-3-month abscess, PWID with an abscess had a 2.6 higher odds of purposely injecting into muscle and a 2.1 higher odds of having difficulty finding a vein. PWID with a past-3-month abscess were also more likely to have engaged in cooker, filter, and/or rinse water sharing in the past 3 months (adjusted odds ratio=1.74).
Table 3.
Factors1 independently associated with having an abscess in the past 3 months among people who inject drugs (PWID) in a multiple regression model.
| AOR | 95% CI | p value | |
|---|---|---|---|
| Purposely injected into muscle | 2.64 | 1.70, 4.10 | <0.001 |
| Difficult to find a vein when injecting | 2.08 | 1.10, 3.95 | 0.024 |
| Cooker, filter, and/or rinse water sharing | 1.74 | 1.05, 2.90 | 0.032 |
AOR=adjusted odds ratio; CI=confidence interval;
Past 3 months.
Discussion
The purpose of this study was to identify abscess characteristics, treatment characteristics, and barriers to medical treatment among a sample of PWID located in a predominantly rural region of the U.S. More than half reported ever having an abscess, and one in four had at least one in the past 3 months. There are several structural and social factors that contribute to the prevalence of abscess formation and treatment among our sample, including healthcare interactions, drug market characteristics, and injection practices. Importantly, the influence that these factors have on abscess formation and treatment may be reduced by taking a harm reduction approach and by expanding access to community-based abscess treatment and educational services, such as those provided by SSPs.
For participants with an abscess in the past 3 months, the majority were severe, which we defined as having oozing pus and/or an open wound. A notable portion also showed signs of systemic infection (fever, vomiting), suggesting that medical treatment was necessary. Still, consistent with prior work (e.g., Asher et al., 2019; Harris et al., 2018; Hope et al., 2015; Wright et al., 2020), the vast majority chose to forgo medical treatment in an attempt to self-treat, and most self-treated abscesses healed without further intervention. Several self-treatment methods were reported, with more than half who self-treated reporting that they consumed leftover or unprescribed oral antibiotics (Gilbert et al., 2019; Summers et al., 2018). Taking these antibiotics can result in the development of antibiotic resistance, and expose those who take them to side effects and/or the potential for allergic reactions. However, attempting to discourage such self-care practices for SSTIs will likely be unsuccessful given the overall (and well-justified) lack of trust in the healthcare system by PWID (Gilbert et al., 2019). Instead, addressing PWID-identified barriers to utilizating medical treatment for SSTIs may prove more beneficial.
The most common barrier to abscess treatment identified by our study participants was long wait times, with nearly two-thirds indicating that this was the primary reason they did not seek medical treatment for an abscess despite believing they should do so. Long wait times for medical treatment have been reported as a barrier to accessing primary care services by a sample of PWID in the Eastern U.S. (Montavalli et al., 2020), suggesting that this is not a barrier specific to the current study’s location. Offering medical care at locations where PWID already receive services, such as SSPs, may help to reduce the impact of long wait times as a barrier to medical treatment (Montavalli et al., 2020). Mentioned previously, the current study included many participants who utilized the Fresno SSP for needle exchange and although this location offers SSTI treatment services, relatively few participants reported using the SSP for treating their abscess. One reason may be that the Fresno SSP only operates on Saturdays for two hours, making it a limited resource for PWID with IDU-related infections. Increasing the number of days that SSPs operate while offering on-site medical services would address this access issue, while also increasing access to sterile syringes for PWID that reduce transmission of viral infections like HIV and HCV (Canary et al., 2017).
In line with prior work (Gilbert et al., 2019; Paquette et al., 2018; Summers et al., 2018), other barriers to utilizing medical treatment among our sample were fear- (afraid of being hospitalized and/or of the abscess treatment itself) and/or stigma-related (e.g., thinking medical staff would treat them poorly). Our prior qualitative study with PWID in California’s Central Valley found that stigma was present during many interactions with the healthcare system (Paquette et al., 2018). In addition to stigma hindering treatment seeking in the current study, PWID in the Valley report feeling stigmatized by pharmacy staff, first responders, and hospital staff, which creates further anticipated stigma that delays or prevents treatment seeking for overdose and other IDU-related infections (Paquette et al., 2018). Given the long history of marginalization and stigmatization of PWID by those working in the healthcare system, it is likely that mending relationships between the two will require significant time and effort. Healthcare providers need to be trained thoroughly on the unique needs and experiences of PWID so that structural competency can be achieved (Metzl & Hansen, 2014).
Some participants chose to seek out medical treatment, either immediately (12%) or after a period of unsuccessful self-treatment (17%). Most of these individuals sought treatment from an ED, whereas few reported getting treatment from a primary care facility or from the Fresno SSP, which is consistent with work suggesting that PWID have low primary care utilization (Artenie et al., 2015; Chitwood, Sanchez, Comerford, & McCoy, 2001). Despite its limited use for abscess treatment, “excellent” quality of care ratings were more prevalent for the SSP relative to all other medical abscess services in the current study, which may be linked to less stigma experienced by PWID seeking treatment at SSPs (Muncan, Walters, Ezell, & Ompad, 2020). Again, expanding access to SSP-based abscess treatment appears to be critical for overcoming many of the barriers to treatment identified by our study participants. Reducing reliance on ED services among PWID can provide other benefits, including reduced healthcare costs and improved PWID attitudes toward healthcare gained from building a relationship with a single, consistent provider (Montavalli et al., 2020).
Lifetime abscess prevalence among our sample was higher than the range of 36–48% reported among PWID in the Eastern U.S. (Asher et al., 2019; Murphy et al., 2001; Summers et al., 2018; Summers et al., 2017), but consistent with the 71% reported among a sample of PWID in Sacramento, CA (Summers et al., 2017). Given that use of black tar heroin is a significant abscess risk factor (Summers et al., 2017), such a result may be because black tar heroin is the most prevalent type of heroin available in the Western U.S. due to drug-trafficking routes (Drug Enforcement Administration, 2019; U.S. Department of Justice, 2010). Indeed, black tar heroin was the most common drug of choice among our sample, with 81% of participants reporting its use. In addition, our recent study on policing of PWID in Fresno indicated high rates physical violence, verbal abuse, and confiscation of new/unused syringes by police (Friedman et al., 2021). It is well known that repressive drug policy and policing is associated significantly with increased health harms among PWID, including increased risk for IDU-related infections (Csete et al., 2016). Together, these findings suggest that the illegality of drug markets may contribute to overall health harms among PWID in Fresno, and to the high abscess prevalence rates found in the current study.
In our multivariate analysis, purposely injecting into muscle (“muscle popping” or “muscling”), having difficulty finding a vein when injecting, and sharing injection preparation equipment (cooker(s), filter(s), and/or rinse water) were associated significantly with having an abscess in the past 3 months. Overall, these results are consistent with prior work evaluating abscess correlates among U.S. PWID samples (Asher et al., 2019; Murphy et al., 2001; Phillips et al., 2017; Summers et al., 2017). Although insignificant in the multivariate analysis, purposely injecting under the skin (“skin popping”) also was associated significantly with having a past-3-month abscess in bivariate analyses. Some suggest that intentional muscle/skin popping is rare among some samples of PWID and instead occurs accidentally as the result of missing a vein (“missed hits”; Hope, Parry, Ncube, & Hickman, 2016; Phillips et al., 2017; Summers et al., 2017). However, we found that more than half of the current sample of PWID with a past-3-month abscess engaged muscle and/or skin popping on purpose, which may be the direct result of having difficulty finding a vein when injecting. Importantly, muscle and skin injections introduce bacteria directly into soft tissue and place PWID at an increased risk for SSTI development. To help reduce muscle/skin injection frequency and in turn, SSTI incidence, sterile syringe sources can provide patients with information on vein care techniques, such as rotating veins and improving vein visibility (National Harm Reduction Coalition, 2020a).
Injection preparation equipment sharing was associated significantly with having an abscess in the past 3 months, though syringe sharing (both distributive and receptive) was not. This finding may be because less than one-third of our sample reported syringe sharing, whereas more than half reported sharing injection equipment exclusive of syringes. Relatively high rates of preparation equipment sharing is consistent with other studies of PWID who report higher rates of sharing preparation equipment than of syringe sharing (Ball et al., 2019). It’s possible that PWID in our sample did not have access to enough sterile preparation equipment. However, most SSPs offer free injection preparation equipment alongside sterile syringes and many PWID do not recognize preparation equipment sharing as putting them at risk for bloodborne infection in the same way as sharing syringes (Ball et al., 2019). Overall, results speak to the relative success of SSPs in reducing syringe sharing, while suggesting the need for more counseling regarding the risks involved with injection preparation equipment sharing among PWID (National Harm Reduction Coalition, 2020b).
A somewhat surprising finding was that none of the cleaning procedures assessed (hand washing, cleaning the injection site, using sterile rinse water) were associated significantly with having reduced odds of an abscess in the past 3 months. This finding differs from prior studies which found that hand washing and cleaning skin with alcohol before injecting serve as protective factors that help to mitigate risk for SSTI development (Kenney et al., 2020; Larney et al., 2017; Murphy et al., 2001; Smith et al., 2015). Few participants in our sample reported washing their hands before preparing drugs, swabbing the injection site before injecting, and/or using sterile rinse water to prepare drugs (30%), limiting statistical power. Such small sample sizes are consistent with prior work (Kenney et al., 2020; Murphy et al., 2001; Smith et al., 2015) suggesting that few PWID are engaging in behaviors that minimize risk for injection-related SSTIs. Prior studies report that barriers to cleaning include drug craving/withdrawal, not having cleansing alcohol available immediately at the time of injection, and time constraints (Bonar & Rosenberg, 2014; Phillips, 2016), and PWID who perceive more barriers are less likely to engage in protective cleansing behaviors (Bonar & Rosenberg, 2014; Kenney et al., 2020; Phillips, 2016). Some have suggested strategies for improving implementation of cleansing behaviors (e.g., providing skin cleaning skills training; Kenney et al., 2020), but more work is needed to determine the effectiveness of such strategies. In the meantime, low rates of reported cleansing suggest that locations where PWID access sterile syringes should provide cleansing supplies, such as alcohol swabs.
Our study has many strengths, but results must be considered in light of some important limitations. The relatively small sample size of 112 participants with an abscess in the past 3 months may have precluded the detection of some significant correlates. In addition, our study was cross-sectional and limited to identifying correlates of abscess rather than risk factors. Our recruitment efforts were also concentrated in Fresno, which is an urban hub located within the predominatly rural California’s Central Valley. Longitudinal work is needed with larger samples and with PWID located in purely rural regions of the U.S. to determine the generalizability of our findings to the greater population of PWID in this largely rural and agricultural region.
Conclusions
The current study simultaneously replicates and expands upon prior work on abscess characteristics, treatment, and treatment barriers among PWID in the U.S. High abscess prevalence was demonstrated among our sample, along with significant associations between abscesses and muscling, missing veins during injection, and sharing of injection preparation equipment. Consistent with other studies, we also found low rates of cleansing procedures prior to injection among PWID. Most participants reported self-treating their abscess, either in the absence of or prior to seeking out medical treatment, with the majority healing without further intervention. Prior studies identified stigma and fear as barriers to SSTI medical treatment; in addition to these barriers, long wait times were the most commonly identified barrier among our sample. Our findings indicate the importance of expanding community-based access to SSTI education and treatment services, particularly at SSPs where PWID may be more comfortable seeking treatment, education on safer IDU techniques, and better provision of cleansing supplies.
What is known about this topic:
Skin and soft tissue infections, including abscesses, are the most common medical complication of injection drug use in the U.S.
Many people who inject drugs forgo abscess medical treatment and attempt to self-treat instead.
Barriers to abscess medical treatment include those that are stigma- and/or fear-related.
What this paper adds:
Many people who inject drugs self-treat severe abscesses with oral antibiotics purchased on the street or leftover from a prior infection, which can lead to antibiotic resistance.
Long wait times are a significant barrier to seeking abscess medical treatment.
Rates of injection preparation equipment sharing are high and significantly associated with abscess formation, indicating a need for expansion of educational resources.
Acknowledgements:
The authors wish to thank the study participants, research staff, Dr. Marc Lasher, Dallas Blanchard, and all the community partners who contributed to this work.
Funding:
Financial support provided to author RAP by the National Institute on Drug Abuse (R01DA035098).
Footnotes
The authors declare that they have no conflicts of interest.
Data Availability Statement:
Data available upon request from the authors.
References
- Artenie AA, Jutras-Aswad D, Roy E, Zang G, Bamvita J-M, Levesque A, & Bruneau J (2015). Visits to primary care physicians among persons who inject drugs at high risk of hepatitis C virus infection: Room for improvement. Journal of Viral Hepatitis, 22(10), 792–799. doi: 10.1111/jvh.12393 [DOI] [PubMed] [Google Scholar]
- Asher AK, Zhong Y, Garfein RS, Cuevas-Mota J, & Teshale E (2019). Association of self-reported abscess with high-risk injection-related behaviors among young persons who inject drugs. Journal of the Association of Nurses in AIDS Care, 30(2), 142–150. doi: 10.1097/JNC.0000000000000016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball LJ, Puka K, Speechley M, Wong R, Hallam B, Wiener JC, … Silverman MS (2019). Sharing of injection drug preparation equipment is associated with HIV infection: A cross-sectional study. Journal of Acquired Immune Deficiency Syndromes, 81(4), e99–e103. doi: 10.1097/QAI.0000000000002062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Takahashi TA, Bradley K, Dellit TH, Benton KL, & Merrill JO (2008). Drug users seeking emergency care for sort tissue infection at high risk for subsequent hospitalization and death. Journal of Studies on Alcohol and Drugs, 69(6), 924–932. doi: 10.15288/jsad.2008.69.924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, & Rosenberg H (2014). Injection drug users’ perceived barriers to using self-initiated harm reduction strategies. Addiction Research and Theory, 22(4), 271–278. doi: 10.3109/16066359.2013.838225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JE, Friedman SR, Cooper HLF, Flom PL, Tempalski B, & Gostness K (2008). Estimating the prevalence of injection drug users in the U.S. and in large U.S. metropolitan areas from 1992 to 2002. J Urban Health, 85(3), 323–351. doi: 10.1007/s11524-007-9248-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canary L, Hariri S, Campbell C, Young R, Whitcomb J, Kaufman H, & Vellozzi C (2017). Geographic disparities in access to syringe services programs among young persons with Hepatitis C virus infection in the United States. Clinical Infectious Diseases, 65(3), 514–517. doi: 10.1093/cid/cix333 [DOI] [PubMed] [Google Scholar]
- Chitwood DD, Sanchez J, Comerford M, & McCoy CB (2001). Primary preventative health care among injection drug users, other sustained drug users, and non-users. Substance Use & Misuse, 36(6–7), 807–824. doi: 10.1081/ja-100104092 [DOI] [PubMed] [Google Scholar]
- Ciccarone D, Bamberger J, Kral A, Hobart CJ, Moon A, Edlin BR, … Murphy EL (2001). Soft tissue infections among injection drug users - San Francisco, California, 1996–2000. Journal of the American Medical Association, 285(21), 2707–2709.11419421 [Google Scholar]
- Csete J, Kamarulzaman A, Kazatchkine M, Altice F, alicki M, Buxton J, … Beyrer C (2016). Public health and international drug policy. Lancet, 387(10026), 1427–1480. doi: 10.1016/S0140-6736(16)00619-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC, Nugent A, Solberg A, Feelemyer J, Mermin J, & Holtzman D (2015). Syringe service programs for persons who inject drugs in urban, suburban, and rural areas--United States, 2013. Morbidity and Mortality Weekly Report, 64, 1337–1341. [DOI] [PubMed] [Google Scholar]
- Drug Enforcement Administration. (2019). National drug threat assessment (DEA-DCT-DIR-007-20). Retrieved from https://www.dea.gov/sites/default/files/2020-01/2019-NDTA-final-01-14-2020_Low_Web-DIR-007-20_2019.pdf
- Fink DS, Lindsay SP, Slymen DJ, Kral AH, & Bluthenthal RN (2013). Abscess and self-treatment among injection drug users at four California syringe exchanges and their surrounding communities. Substance Use & Misuse, 48, 523–531. doi: 10.3109/10826084.2013.787094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, Syvertsen JL, Bourgois P, Bui A, Beletsky L, & Pollini R (2021). Intersectional structural vulnerability to abusive policing among people who inject drugs: A mixed methods assessment in California’s Central Valley. International Journal of Drug Policy, 87, 102981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert AR, Hellman JL, Wilkes MS, Rees VW, & Summers PJ (2019). Self-care habits among people who inject drugs with skin and soft tissue infections: A qualitative analysis. Harm Reduction Journal, 16, 69. doi: 10.1186/s12954-019-0345-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris RE, Richardson J, Frasso R, & Anderson ED (2018). Experiences with skin and soft tissue infections among people who inject drugs in Philadelphia: A qualitative study. Drug and Alcohol Dependence, 187, 8–12. doi: 10.1016/j.drugalcdep.2018.01.029 [DOI] [PubMed] [Google Scholar]
- Heckathorn DD (1997). Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems, 44, 174–199. doi: [DOI] [Google Scholar]
- Hope VD, Ncube F, Parry JV, & Hickman M (2015). Healthcare seeking and hospital admissions by people who inject drugs in response to symptoms of injection site infections or injuries in three urban areas of England. Epidemiology & Infection, 143, 120–131. doi: 10.1017/s0950268814000284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope VD, Parry JV, Ncube F, & Hickman M (2016). Not in the vein: ‘missed hits’, subcutaneous and intramuscular injections and associated harms among people who inject psychoactive drugs in Bristol, United Kingdom. International Journal of Drug Policy, 28, 83–90. doi: 10.1016/j.drugpo.2015.11.003 [DOI] [PubMed] [Google Scholar]
- Kenney SR, Phillips KT, Herman DS, Keosaian J, Anderson BJ, & Stein MD (2020). Perceived behavioral control and barriers to cleaning skin before injecting drugs. Journal of Addiction Medicine, 14(3), 231–235. doi: 10.1097/ADM.0000000000000564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Peacock A, Mathers BM, Hickman M, & Degenhardt L (2017). A systematic review of injecting-related injury and disease among people who inject drugs. Drug and Alcohol Dependence, 171, 39–49. doi: 10.1016/j.drugalcdep.2016.11.029 [DOI] [PubMed] [Google Scholar]
- Lewis K, Burd-Sharps S, & Sachs J (2010). The measure of America 2010–2011: Mapping risks and resilience. Retrieved from New York: [Google Scholar]
- Metzl JM, & Hansen H (2014). Structural competency: Theorizing a new medical engagement with stigma and inequality. Social Science & Medicine, 103, 126–133. doi: 10.1016/j.socscimed.2013.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montavalli D, Taylor JL, Childs E, Valente PK, Salhaney P, Olson J, … Bazzi AR (2020). “Health is on the back burner:” Multilevel barriers and facilitators to primary care among people who inject drugs. Journal of General Internal Medicine, Online ahead of print. doi: 10.1007/s11606-020-06201-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro J, Phillips KT, Herman DS, Stewart C, Keosaian J, Anderson BJ, & Stein MD (2020). Self-treatment of skin infections by people who inject drugs. Drug and Alcohol Dependence, 206, 107695. doi: 10.1016/j.drugalcdep.2019.107695 [DOI] [PubMed] [Google Scholar]
- Muncan B, Walters SM, Ezell J, & Ompad DC (2020). “They look at us like junkies”: Influences of drug use stigma on the healthcare engagement of people who inject drugs in New York City. Harm Reduction Journal, 17, 53. doi: 10.1186/s12954-020-00399-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy EL, DeVita D, Liu H, Vittinghoff E, Leung P, Ciccarone DH, & Edlin BR (2001). Risk factors for skin and soft-tissue abscesses among injection drug users: A case-control study. The Journal of Infectious Diseases, 33, 35–40. [DOI] [PubMed] [Google Scholar]
- NASEN. (2020). Fresno Needle Exchange Program. Retrieved from https://nasen.org/sep/fresno-needle-exchange-program
- National Harm Reduction Coalition. (2020a). Getting off: The basics of safer injection. Retrieved from https://harmreduction.org/issues/safer-drug-use/injection-safety-manual/safer-injection-basics/
- National Harm Reduction Coalition. (2020b). Getting ready: Preparing yourself & your equipment. Retrieved from https://harmreduction.org/issues/safer-drug-use/injection-safety-manual/preparing-equipment/
- Paquette CE, & Pollini RA (2018). Injection drug use, HIV/HCV, and related services in nonurban areas of the United States: A systematic review. Drug and Alcohol Dependence, 188, 239–250. doi: 10.1016/j.drugalcdep.2018.03.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquette CE, Syvertsen JL, & Pollini RA (2018). Stigma at every turn: Health services experiences among people who inject drugs. International Journal of Drug Policy, 57, 104–110. doi: 10.1016/j.drugpo.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KT (2016). Barriers to practicing risk reduction strategies among people who inject drugs. Addiction Research and Theory, 24(1), 62–68. doi: 10.3109/16066359.2015.1068301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips KT, Anderson BJ, Herman DS, Liebschutz JM, & Stein MD (2017). Risk factors associated with skin and soft tissue infections among hospitalized people who inject drugs. Journal of Addiction Medicine, 11(6), 461–467. doi: 10.1097/ADM.0000000000000346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirozzi K, Van JC, Pontious J, & Meyr AJ (2014). Demographic description of the presentation and treatment of lower extremity skin and soft tissue infections secondary to skin popping in intraveous drug abusers. The Journal of Foot & Ankle Surgery, 53, 156–159. doi: 10.1053/j.jfas.2013.12.017 [DOI] [PubMed] [Google Scholar]
- Pollini RA, Gallardo M, Hasan S, Minuto J, Lozada R, Vera A, … Strathdee SA (2010). High prevalence of abscesses and self-treatment among injection drug users in Tijuana, Mexico. International Journal of Infectious Diseases, 14S, e117–e122. doi: 10.1016/j.ijid.2010.02.2238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- See I, Gokhale RH, Geller A, Lovegrove M, Schranz A, Fleischauer A, … Fiore A (2020). National public health burden estimates of endocarditis and skin and soft-tissue infections related to injection drug use: A review. Journal of Infectious Disease, 222, S429–S436. doi: 10.1093/infdis/jiaa149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ME, Robinowitz N, Chaulk P, & Johnson KE (2015). High rates of abscesses and chronic wounds in community-recruited injection drug users and associated risk factors. Journal of Addiction Medicine, 9(2), 87–93. doi: 10.1097/ADM.0000000000000093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Summers PJ, Hellman JL, MacLean MR, Rees VW, & Wilkes MS (2018). Negative experiences of pain and withdrawal create barriers to abscess care for people who inject heroin. A mixed methods analysis. Drug and Alcohol Dependence, 190, 200–208. doi: 10.1016/j.drugalcdep.2018.06.010 [DOI] [PubMed] [Google Scholar]
- Summers PJ, Struve IA, Wilkes MS, & Rees VW (2017). Injection-site vein loss and soft tissue abscesses associated with black tar heroin injection: A cross-sectional study of two distinct populations in USA. International Journal of Drug Policy, 39, 21–27. doi: 10.1016/j.drugpo.2016.08.006 [DOI] [PubMed] [Google Scholar]
- Syvertsen JL, Paquette CE, & Pollini RA (2017). Down in the valley: Trajectories of injection initiation among young injectors in California’s Central Valley. Int J Drug Policy, 44, 41–49. doi: 10.1016/j.drugpo.2017.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomolillo CM, Crothers LJ, & Aberson CL (2007). The damage done: A study of injection drug use, injection related abscesses and needle exchange regulation. Substance Use & Misuse, 42, 1603–1611. doi: 10.1080/10826080701204763 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice. (2010). Central Valley California: High intensity drug trafficking area. Retrieved from https://www.justice.gov/archive/ndic/pubs40/40384/40384p.pdf
- Visconti AJ, Sell J, & Greenblatt AD (2019). Primary care for persons who inject drugs. American Family Physician, 99(2), 109–116. [PubMed] [Google Scholar]
- Wright T, Hope V, Ciccarone D, Lewer D, Scott J, & Harris M (2020). Prevalence and severity of abscesses and cellulitis, and their associations with other health outcomes, in a community-based study of people who inject drugs in London, UK. PLoS One, 15(7), e0235350. doi: 10.1371/journal.pone.0235350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurcel AG, Burke D, Skeer M, Landy D, Heimer R, Wong JB, … Stopka TJ (2018). Sex work, injection drug use, and abscesses: Associations in women, but not men. Drug and Alcohol Dependence, 185, 293–297. doi: 10.1017/j.drugalcdep.2017.12.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available upon request from the authors.


