Abstract
Background
Ruptured aneurysms secondary to the tuberculous infection of the aorta are a rare and life-threatening disease. We report a single-center experience of two patients with ruptured infrarenal tuberculous aneurysms.
Case presentation
We report 2 patients with ruptures of the tuberculous aneurysm. All patients had acute abdominal pain and were diagnosed by echography then CT scan preoperatively. The first patient (male, 50 years old) had a ruptured saccular aneurysm. The second patient (male, 43 years old) had a retroperitoneal contained rupture. All were treated by open prosthetic repair, by vascular surgeons. The two patients were well after operations. The diagnosis was confirmed by pathology examination. Antituberculous treatment was introduced after the operation.
Conclusions
Ruptured tuberculous aneurysms are rare but life-threatening. The diagnosis requires a high degree of suspicion. The treatment includes early diagnosis and emergent surgical intervention, extensive excision of infected field, aortic reconstruction, and prolonged antituberculous drug therapy.
Abbreviations: WHO, World Health Organization; TB, tuberculosis; BMI, body mass index; CT, computerized tomography
Keywords: Case series, Aortic surgery, Tuberculous aortic aneurysm, Ruptured mycotic aneurysm, Tuberculosis
Highlights
-
•
The tuberculous aortic aneurysm is a fatal condition if not early diagnosed and properly treated.
-
•
The diagnosis requires a high degree of suspicion.
-
•
Surgery is necessary for stenotic or aneurysmal lesions.
-
•
The treatment should be a combination of surgery and antituberculous medication.
1. Background
Tuberculosis (TB) is still a global health problem. It kills millions of people worldwide each year and is the second leading cause of death from infection. The World Health Organization (WHO) reported 8 million new cases and about 1.3 million people died of the disease in 2012 [1]. TB can have a variety of clinical manifestations due to its spread to organs other than the lungs.
Aortic tuberculosis (TB) is usually secondary and extremely rare with manifestations such as aortic inflammation or an aneurysm formation. The mechanism of development of aortic tuberculosis is believed to be via contiguous spread from the surrounding organs (lymph nodes) or directly from the blood (uncommon). The symptomatic tuberculous aneurysm is rare, but the injury can be fatal when not diagnosed in time [2]. There are not many reports on the disease around the world, mainly case reports. A retrospective report in 1933 included only 21 cases and in 1965 recorded 51 patients [3]. In a review from 1945 to 1999, only 41 cases have been reported [4].
In Vietnam, reports of tuberculous aneurysms are very rare. Between 2019 and 2020, we had 2 cases at Binh Dan Hospital, a university hospital under Pham Ngoc Thach University of Medicine, Hochiminh City. We describe these two cases with successful surgical management and medical treatment of ruptured aneurysms of the infrarenal aorta secondary to TB.
2. Case presentation
The study was registered at ResearchRegistry. com (researchregistry7637). The study is a case series, retrospective, single-center, and consecutive. These two patients were operated on by surgeon DKH who was the chief of the cardiovascular ward of Binh Dan Hospital and had over 50 case experiences of abdominal aorta aneurysm operations.
2.1. Patient 1
A fifty-year-old male patient, Vietnamese, farmer, BMI 18 kg/m2 is presented with acute sudden-onset periumbilical pain and was admitted to Emergency Department, In December 2019. In the past, he had abdominal and left flank pain lasting for1 a week before admission, and a history of pulmonary tuberculosis treatment. The patient had no relevant drug history, family history, or relevant genetic information. There was no smoking history nor other special habits of medical importance. The physical examination revealed severe acute periumbilical pain, blood pressure 140/90 mmHg, a pulse of 90, a temperature of 30 °C. The abdomen was painful and tender in palpation. A mass was palpable, painful, and pulsatile.
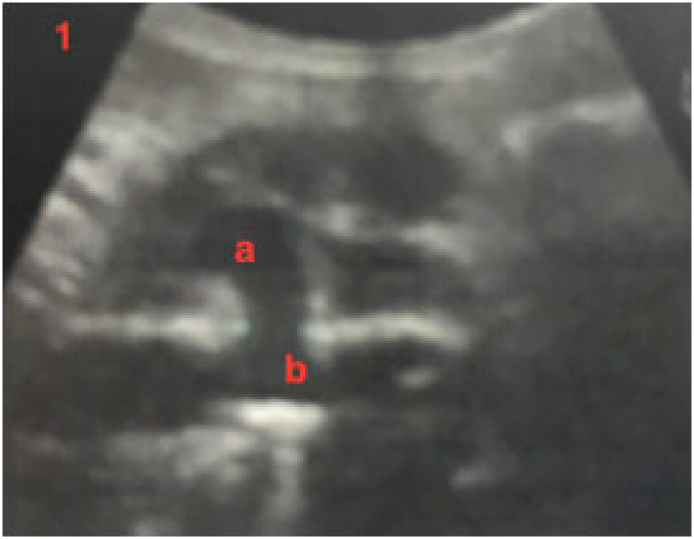
The abdominal ultrasound showed a rupture at the left wall of the infrarenal aorta, which resulted in a big false aneurysm with a retroperitoneal hematoma around the aneurysm and the aorta, 75 mm long, 41 mm anteroposterior dimension, and 56 mm transverse dimension (Fig. 1).
Fig. 1.
Echography image: The ruptured aortic abdominal aneurysm with surrounding hematoma (a) and the aorta (b).
CT scan showed the discontinuation in the left wall of the infrarenal aorta creating a false aneurysm, which had almost been occupied by a thrombus. The diameter of the aneurysm was 58 mm, the diameter of the rupture was 15 mm (Fig. 2a, b).
Fig. 2.
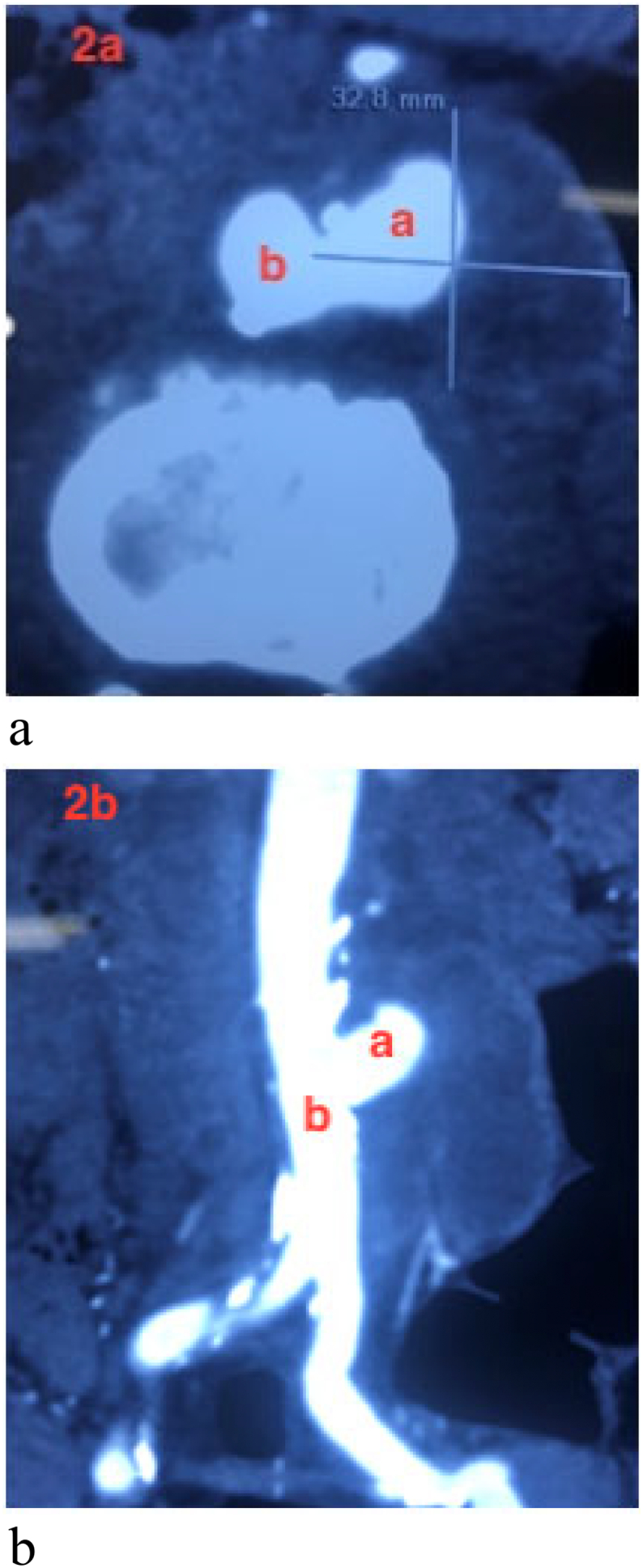
CT images: the ruptured aortic abdominal aneurysm with surrounding hematoma (a) and the aorta (b).
The patient was indicated to have an emergency intervention with the diagnosis of the rupture of an infected infrarenal aortic aneurysm. The optimization for the intervention took place by a full examination and pre-operative assessment. An urgent repair of the aneurysm was planned.
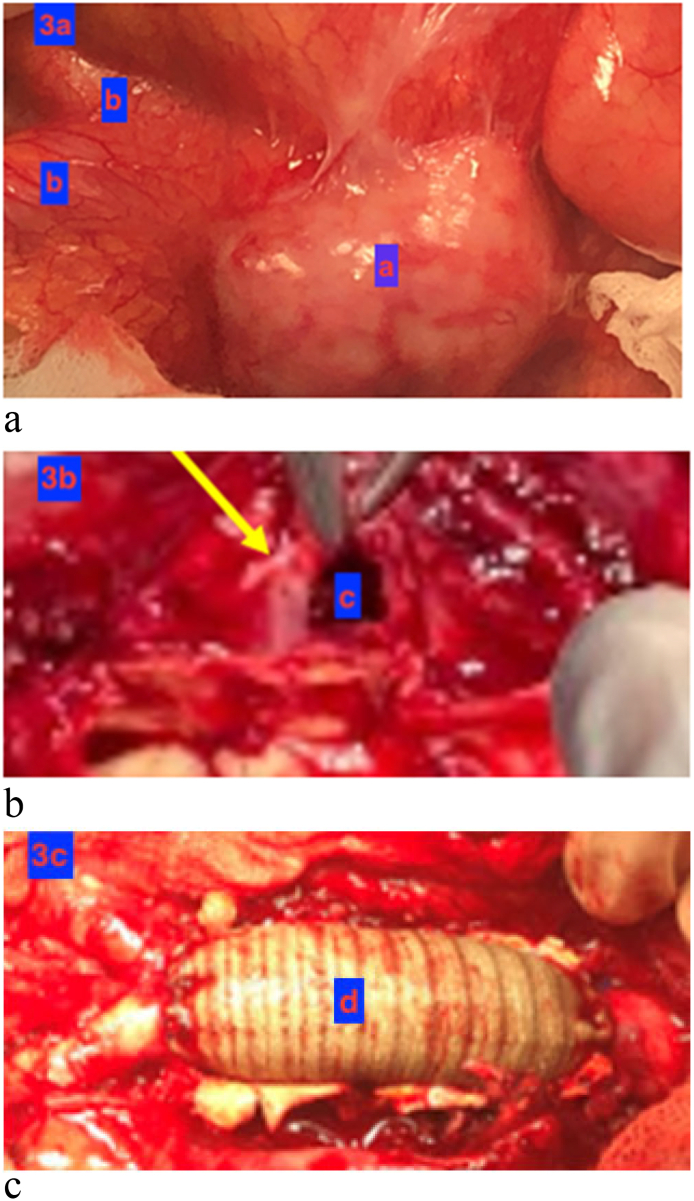
An anterior midline laparotomy was performed, and the retroperitoneal area was exposed. A large pseudo-aneurysm of the infrarenal aorta was identified (Fig. 3a). After controlling the proximal end of the aorta and two common iliac arteries, the pseudo-aneurysm was opened longitudinally. The aortic wall was seen to have a rupture at the left side (2 cm in diameter) (Fig. 3b), creating a retroperitoneal hematoma. The aorta was reconstructed using a 16 straight Dacron graft (Fig. 3c). The aortic wall and para-aortic lymph node samples were sent for histopathological analysis, bacterial, fungal, and TB culture and sensitivity.
Fig. 3.
(a) Aneurysm, (b) common iliac artery, right and left, (c) ruptured orifice on the aneurysmal wall, (d) Dacron aortic graft.
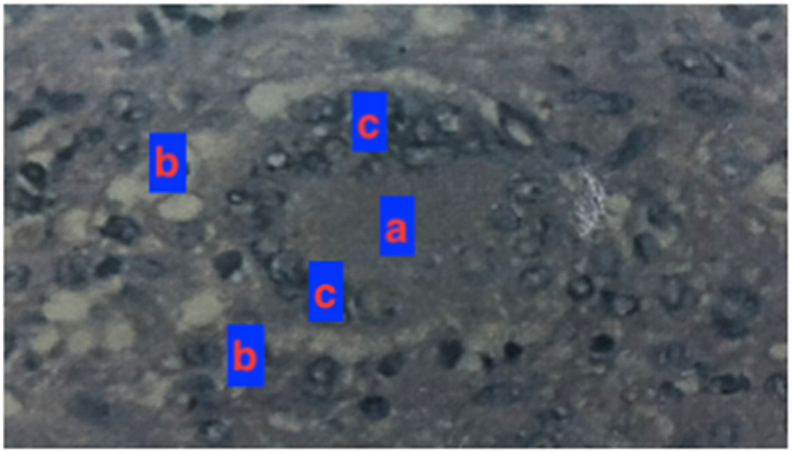
The pathology examination showed necrotic vascular tissue fragments with multinucleated giant cells, epithelioid cells, caseous necrosis, and lymphocyte form granulomas (Figure 4). The TB culture was negative. The patient was transferred to Pham Ngoc Thach Tuberculosis Hospital to resume the antituberculous treatment on the 7th postoperative day.
Fig. 4.
A granuloma with central caseous necrosis (a), multinucleated giant cell (b), epithelioid macrophage (c).
2.2. Patient 2
A male patient, 43 years old, Vietnamese, was admitted in February 2020, because of periumbilical pain lasting 10 days. He had an antecedent of pulmonary and abdominal lymph node tuberculosis 6 months earlier. The patient had no fever, severe abdominal pain, weight loss (pulse: 76, blood pressure: 120/80 mmHg, temperature: 37o C, BMI: 18 kg/m2). The abdomen was painful and tender in palpation and had a pulsatile mass, which was an unclear limit, and adjacent to the right of the umbilicus.
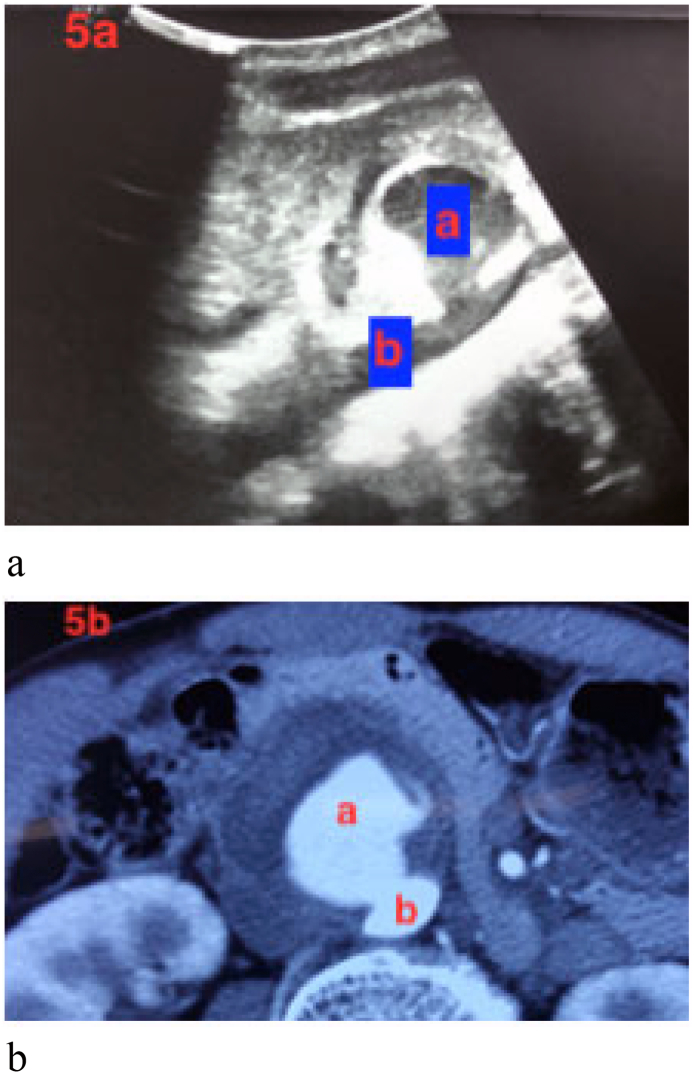
The abdominal ultrasound confirmed a saccular infrarenal abdominal aortic aneurysm, extending to the iliac bifurcation, with a diameter of 28 × 24 mm; and a false aneurysm with a diameter of 45x35mm and the indistinct wall (Fig. 5a).
Fig. 5.
Ruptured aortic aneurysm with surrounding hematoma (a) and aorta (b).
The CT Scan showed a saccular abdominal aortic aneurysm in 47 × 44 × 51 mm and a false aneurysm with a clot in the false lumen and an unsteady thickening wall (the thickest was 14 mm) (Fig. 5b). There was a little fluid in front of the liver.
The preoperative diagnosis was a ruptured pseudo-aneurysm of the infrarenal aorta with a localized retroperitoneal hematoma. An emergency intervention was indicated.
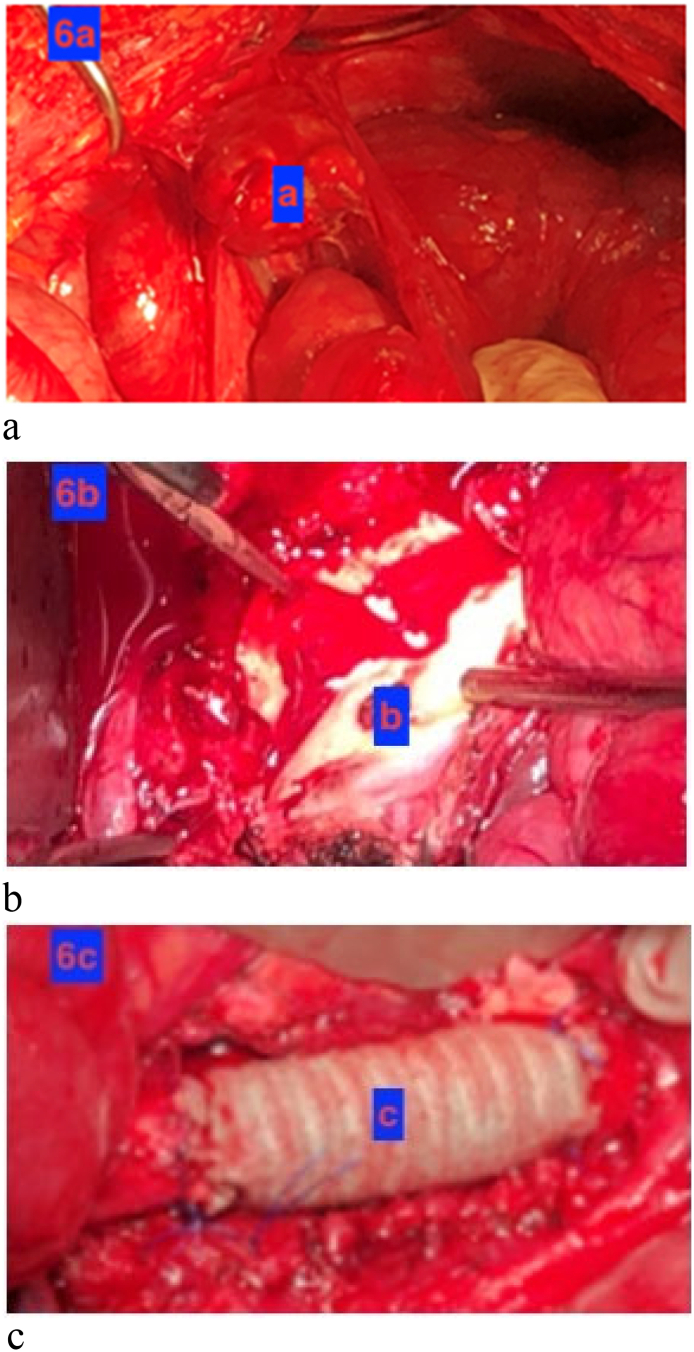
A midline laparotomy was performed. A mass resembling an inflammatory ganglion bulk was observed and removed. A retained hematoma extends to the kidneys, pushing the pancreas to the anterior and the right side of the aorta. The neck of the aneurysm was not able to be dissected directly because of the huge hematoma and the large ganglion mass adjacent to the aorta. The team decided to expose the lower end of the aorta and dissect up to the left of the aorta, cut and ligate the inferior mesenteric artery. The ganglion mass (Fig. 6a) was removed and the neck was approached and controlled. The aorta was opened, there was a hole in the right wall of the aorta of 2 cm diameter (Fig. 6b), resulting in a large retroperitoneal hematoma. The aorta was constructed by a 14 straight Dacron graft (Fig. 6c).
Fig. 6.
Lymph nodes (a), the ruptured orifice of the aortic aneurysm (b), Dacron graft (c).
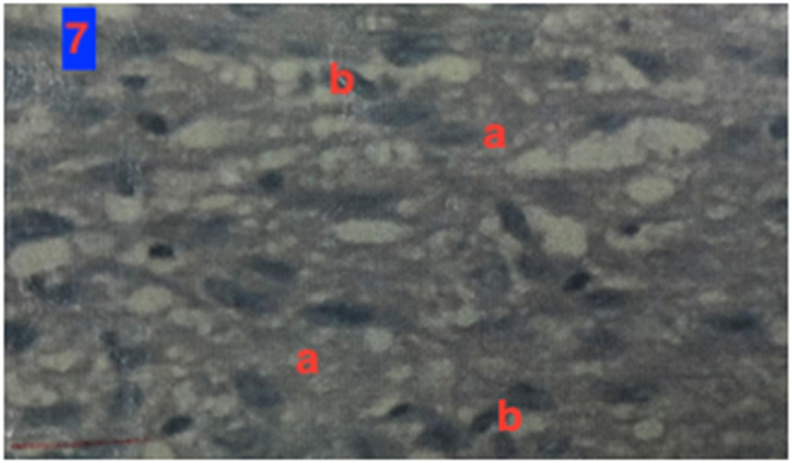
The pathologic examination of the periaortic tissue and aortic wall revealed chronic inflammation with multinucleated giant cell reaction (Fig. 7). The patient was transferred to Pham Ngoc Thach Tuberculosis Hospital for antituberculous treatment on the 4th postoperative day. The postoperative process had been getting fine.
Fig. 7.
The granuloma (non-caseating) with epithelioid cells (a) and multinucleated giant cells (b).
3. Discussion
Two patients with ruptured tuberculous of the abdominal aorta were early diagnosed and successfully treated.
Tuberculous aortic aneurysm is a rare clinical entity and few series of cases had been published to date [3], [4], [5].In the review of the literature, we can correlate the decrease in the incidence of the TB aneurysm over the years with the development of antituberculous medicaments [6]. Even with the advance in diagnosis, anti-tuberculous agents, and successful surgical treatment outcomes, complications still occur [7], [8], [9]. Till now, more than 100 patients with TB have been reported [2], [5], [10], [11], [12]. Most of these patients show aneurysmal dilatation of the thoracic or abdominal aorta and carry a high mortality rate due to perforation or rupture with massive hemorrhage and shock. The diagnosis is only found when the biopsy or autopsy is taken.
The pathogenesis of the aortic tuberculous aneurysm includes several mechanisms: the most common mode of transmission is a direct extension from the contiguous focus of tuberculous lymph nodes, the hematogeneous spread to the arterial intima, and the septic embolization of the arterial wall via the vasa vasorum or the lymphatics [13], [14]. Direct spread of infection to the abdominal aorta may occur from nearby retroperitoneal lymphadenitis, intestinal tuberculosis, spondylitis, psoas abscess, or the prostate [15], [16]. It's possibly the case in the 2 patients described here. The contiguous focus was found in 75% of patients in Long's study [4]. In our report, pathological examinations documented adjacent tuberculous focus in both 2 cases. The hematogeneous spread to the aortic intima or vasa vasorum and the autoimmune reaction induced by TB is thought to be uncommon [3], [4]. The tuberculous infection results in the destruction of the aortic wall. The necrosis of the wall leads to the rupture causing massive bleeding or perivascular hematoma which can communicate with aneurysm lumen (pseudoaneurysm, false aneurysm). In the case the infection expands along the aortic wall, it causes a true aneurysm [17], [18]. In Manika's study, 13 of 28 (46%) cases were described as pseudoaneurysms [2]. The aorta is the most common site of tuberculous aneurysms, and an approximately equal incidence rate is reported in the thorax and the abdomen, while other arteries have also been reported [3]. Manika reports 15 (53%) cases of thoracic aortic aneurysm, 7 (25%) cases of
abdominal aortic aneurysms and 4 (14%) cases in which aneurysms were detected in both the thoracic and abdominal aorta. The study reports 1 case of an aortoiliac aneurysm and an iliac artery aneurysm [2].
The clinical manifestations are usually related to the aneurysm with insistent pain associated with the location of the aneurysm. Patients may have a palpable, pulsating abdominal mass, a para-aortic mass on imaging, aneurysmal leakage, or rupture [19], [20]. In a review, Long et al. [4] found that 63% of cases with tuberculous aneurysms have had the antecedent of pulmonary or extrapulmonary tuberculosis. They suggested a clinical manifestation scenario as (1) insistent chest, abdominal, or back pain in 64%, (2) hypovolemic shock or major bleeding in 38%, and (3) palpable or radiologically visible paraaortic mass in 64%. Two cases of this study showed tuberculous history, palpable, painful, and pulsatile masses in the abdomen. Patient 1had an antecedent of pulmonary TB, fibrocalcific changes in chest X-ray, negative in BK sputum and tuberculin test. Patient 2 had a history of pulmonary and abdominal ganglion treatment six months earlier. The smear staining and cultures of periaortic tissue liquid for Mycobacterium tuberculosis were negative in both cases.
The treatment of tuberculous aneurysms is the combination of surgery and antituberculous medications. Classical surgery, consisting of an open surgical repair of the vessel, ensure the extensive excision and lavage of the contaminated tissue [3], [17], and synthetic graft repair. The mortality of the surgery is between 14 and 20% and comes up to 50% in emergent situations [21], [22]. In 1955, Rob et al. [23] reported the first successful reconstruction of a tuberculous aortic aneurysm by an artificial graft. Long et al. [4] described 41 cases of aortic aneurysms, in which 24 were treated by in situ or extra-anatomic graft repair and antituberculous therapy. The mortality was 14%. Extra-anatomic bypasses helped prolonged survival in Long review's 2 cases but gave lower latency than in situ reconstructions. Despite reports of tuberculous infection of vascular prosthesis [24], [25]. In situ graff infection does not seem to carry a risk of infection in follow-up, provided antituberculous therapy is adequately given. Raffetto [25] reports a successful outcome of an infected graft left in place after debridement and antituberculous therapy. Homograft reconstructions had been reported [3], [4], [26] with no evidence of false aneurysms in long-term follow-up. Despite the primary suture of the false aneurysm and synthetic patch closure being successful in some cases [4], aortic replacement should be preferred because the extent of aortic wall damage was difficult to access in operations. The endovascular repair had been performed in 2 cases with limited follow-up [27], [28]. This procedure does not allow extensive debridement of infected periaortic tissues, and thus could be associated with a high risk of infection recurrent leading to fatal bleeding, as occurred in one of the two reported cases [29]. Endovascular repair should be restricted to the patient with rupture or at high surgical risk. The treatment of arterial rupture with coil combined with medical therapy has been proposed in cases where restoration of arterial patency is not required such as branches of the aorta [30]. Some authors propose lifelong antibiotic treatment after prosthetic graft implantation [21]. Close postoperative follow-up is needed to disclose the recurrence [31]. Among factors that impact the outcome of our cases, the enhanced imaging and surgical improvement were eminent [10], [31].
Mycobacterium tuberculosis identification was lacking in our cases. A high index of suspicion for tuberculous aortitis is based on clinical features and histologic analysis results such as inflammation with multinuclear giant cell reaction and fibrotic lesions[32]. The failure to isolate Mycobacterium tuberculosis may be due to a low bacillary burden in low oxygen extrapulmonary tissues or errors in specimen processing and not excluding active TB [3], [10], [33], [34], [35]. Moreover, negative test results do not eliminate the diagnosis of TB etiology.
4. Conclusion
The tuberculous aneurysm rupture is a rare and dangerous entity. Increased alertness and seeking of histological and microbiological confirmation as well as combination therapy with antituberculous treatment and invasive management of the aneurysm could lead to relatively good results.
The work has been reported in line with the PROCESS 2020 criteria [36].
Availability of data and materials
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Funding
No fund has been used for this study.
Ethics approval and consent to participate
The study protocol and data collection were approved by the Ethics Committee in Biomedical Research at the Binh Dan Hospital No. 515/GCN-BVBD on July 29, 2021. Written patient informed consent was obtained for study participation.
Consent
Written informed consent for publication of their clinical details and/or clinical images was obtained from all patients. A copy of the consent form is available for review by the Editor of this journal.
Credit author statement
HUNG VINH TRAN: Conception and design of the study, data analysis, interpretation, drafting of the manuscript, critical revision, and approval of the final version of the manuscript.
DUC KHANH HO: Acquisition of data, and data analysis.
VAN HOANG LE: Acquisition of data, and data analysis.
HAI VAN DUONG: Conception and design of the study, data curation, writing, reviewing, editing, and approval of the final version of the manuscript.
Registration of research studies
-
1.
Name of the registry: RUPTURED TUBERCULOUS ANEURYSMS OF THE ABDOMINAL AORTA: TWO CASE SERIES.
-
2.
The unique identifying number or registration ID: researchregistry7637.
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.researchregistry.com/browse-the-registry#home/.
Guarantor
Hung Vinh Tran1
Associate Professor. First Author. (hungsurgeon2021@yahoo.com),
Head of Department of General Surgery of Pham Ngoc Thach University of Medicine, HCMC.
Director of Binh Dan Hospital HCMC.
Hai Van Duong1,3♥
Associate Professor, Correspondence Author. (hai.dv@umc.edu.vn)
University of Medicine and Pharmacy at Hochiminh City.
Pham Ngoc Thach University of Medicine.
Consulting Surgeon, Binh Dan Hospital HCMC.
Provenance and peer-review
Not commissioned, externally peer-review.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgments
The authors acknowledge the assistance of the Director Board and the Scientific Research Department of Binh Dan Hospital, HCMC.
References
- 1.Hung Y.M., Chang Y.T. A rare but potentially lethal case of tuberculous aortic aneurysm presenting with repeated attacks of abdominal pain. Intern. Med. 2015;54:1145–1148. doi: 10.2169/internalmedicine.54.3620. [DOI] [PubMed] [Google Scholar]
- 2.Manika K., Efthymiou C. Miliary tuberculosis in a patient with tuberculous mycotic aneurysm of the abdominal aorta: case report and review of literature. Respir.Med.Case Rep. 2017;21:30–35. doi: 10.1016/j.rmcr.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Canaud L., Marzell J. Tuberculous aneurysm of the abdominal aorta. J. Vas. Surg. 2008;48:1012–1016. doi: 10.1016/j.jvs.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Long R., Guzman R., Greenberg H. Tuberculous mycotic aneurysm of the aorta: review of published medical and surgical experience. Chest. 1999;115:522–531. doi: 10.1378/chest.115.2.522. [DOI] [PubMed] [Google Scholar]
- 5.Silbergleit A., Arbulu A., Defever B.A. Tuberculous aortitis. JAMA. 1965;193:333–335. doi: 10.1001/jama.1965.03090050009003. [DOI] [PubMed] [Google Scholar]
- 6.Ikezawa T., et al. Tuberculous pseudoaneurysm of the descending thoracic aorta: a case report and literature review of surgically treated cases. J. Vasc. Surg. 1996;24:693–697. doi: 10.1016/s0741-5214(96)70086-1. [DOI] [PubMed] [Google Scholar]
- 7.Atnip A.D., et al. Mycotic aneurysms of the suprarenal aorta: prolonged survival after in-situ aortic and visceral reconstruction. J. Vas. Surg. 1999;13:439–444. [PubMed] [Google Scholar]
- 8.Chan F.Y. In-situ prosthetic graft replacement for mycotic aneyrysm of the aorta. Ann. Thorac. Surg. 1989;47:193–203. doi: 10.1016/0003-4975(89)90268-3. [DOI] [PubMed] [Google Scholar]
- 9.Chiba Y., et al. Surgical treatment of infected thoracic and abdominal aortic aneurysms. Cardiovasc. Surg. 1996;4:476–479. doi: 10.1016/0967-2109(95)00074-7. [DOI] [PubMed] [Google Scholar]
- 10.Choudhary S., et al. Tubercular pseudoaneurysm of the aorta. Ann. Thorac. Surg. 2001;72:1239–1244. doi: 10.1016/s0003-4975(01)03002-8. [DOI] [PubMed] [Google Scholar]
- 11.Efremidis S., Lakshamanan S., Hsu J. Tuberculous aortis: a rare cause of mycotic aneurysm of the aorta. Am. J. Roentgenol. 1976;127:859–861. doi: 10.2214/ajr.127.5.859. [DOI] [PubMed] [Google Scholar]
- 12.Astreda A., et al. Tuberculous aneurysm of the descending aorta. Chest. 1979;75:386–388. doi: 10.1378/chest.75.3.386. [DOI] [PubMed] [Google Scholar]
- 13.Ishibatake H., Onizuka R. A successful treated case of miliary tuberculosis with adult respiratory distress syndrome and tuberculous aneurysm of abdominal aorta. Kakkakuy. 1998;73:403–411. [PubMed] [Google Scholar]
- 14.Tsurutani H., et al. Hepatic artery pseudoaneurysm in a patient treated for miliary tuberculosis. Intern. Med. 2000;39:994–998. doi: 10.2169/internalmedicine.39.994. [DOI] [PubMed] [Google Scholar]
- 15.Ghosh H. Tuberculous lymphadenitis: report of a case with perforation of aorta into duodenum. Am. J. Clin. Pathol. 1954;24:1044–1049. doi: 10.1093/ajcp/24.9.1044. [DOI] [PubMed] [Google Scholar]
- 16.Hagino R.T., et al. A case of Pott's disease of the spine eroding into paraspinal aorta. J. Vas. Surg. 1996;24:482–486. doi: 10.1016/s0741-5214(96)70206-9. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y., Zhang J., Yin M.D. Endovascular repair of a tuberculous aneurysm of descending thoracic aorta. Chin. Med. J. 2011;124(14):2228–2230. [PubMed] [Google Scholar]
- 18.Liu W., Kwak B., Kim K. Tuberculous aneurysm of the abdominal aorta: endovascular repair using stent grafts in two cases. Korean J. Radiol. 2000;1:215–218. doi: 10.3348/kjr.2000.1.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takahashi A case of tuberculous abdominal aortic aneurysm which ruptured and perforated into the sigmoid (in Japanese) Nippon Geka GakkaiZasshi. 1986;87:99–104. [PubMed] [Google Scholar]
- 20.Oran I., et al. Mesenteric artery aneurysm in intestinal tuberculosis as a cause of lower intestinal bleeding. Abdom. Imaging. 2001;26:131–133. doi: 10.1007/s002610000127. [DOI] [PubMed] [Google Scholar]
- 21.Allins A.D., et al. Tuberculous infection of the descending thoracic and abdominal aorta: case report and literature review. Ann. Vasc. Surg. 1999;13:439–444. doi: 10.1007/s100169900280. [DOI] [PubMed] [Google Scholar]
- 22.Zhang C., et al. Tuberculous abdominal aortic pseudoaneurysm with renal and vertebral tuberculosis: a case and literature review. J. Infect. Dev. Ctries. 2014;8:1216–1221. doi: 10.3855/jidc.4954. [DOI] [PubMed] [Google Scholar]
- 23.Rob C.G., Eastcott H.H.G. Aortic aneurysm due to tuberculous lymphadenitis. BMJ. 1955;1:378–379. doi: 10.1136/bmj.1.4910.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wright R.A., Yang F., Moore W.S. Tuberculous infection in a vascular prosthesis: a case of aortic graft infection resulting from disseminated tuberculosis. Arch. Surg. 1977;112:79–81. doi: 10.1001/archsurg.1977.01370010081016. [DOI] [PubMed] [Google Scholar]
- 25.Raffetto J.D., Bernardo J., Menzoian J.O. Aortobifemoral graft infection with mycobacterium tuberculosis: treatment with abscess drainage, debridement, and long-term administration of antibiotic agents. J. Vas. Surg. 2004;40:826–829. doi: 10.1016/j.jvs.2004.07.041. [DOI] [PubMed] [Google Scholar]
- 26.Sicard G.A., et al. Autologous vein reconstruction in prosthetic graft infections. Vasc. Endovasc. Surg. 1997;14:93–98. doi: 10.1016/s1078-5884(97)80163-3. [DOI] [PubMed] [Google Scholar]
- 27.Labrousse L., et al. Endovascular treatment of a tuberculous infected aneurysm of the descending thoracic aorta: a word of caution. J. Vas. Surg. 2007;46:786–788. doi: 10.1016/j.jvs.2007.05.038. [DOI] [PubMed] [Google Scholar]
- 28.Steichen O., et al. Endovascular repair of a tuberculous aortic false aneurysm. Rev. Med. Interne. 2007;28:196–198. doi: 10.1016/j.revmed.2006.11.017. [DOI] [PubMed] [Google Scholar]
- 29.Silbergleit A., Arbulu A. Tuberculous mycotic aneurysms. Chest. 1999;116:1142–1145. doi: 10.1378/chest.116.4.1142. [DOI] [PubMed] [Google Scholar]
- 30.Tsurutani H., et al. Hepatic artery pseudoaneurysms in a patient treated for miliary tuberculosis. Intern. Med. 2000;39:994–998. doi: 10.2169/internalmedicine.39.994. [DOI] [PubMed] [Google Scholar]
- 31.Jain A.K., et al. Tuberculous pseudoaneurysm of aorta: a rare association with vertebral tuberculosis. Spine. 2007;7:249–253. doi: 10.1016/j.spinee.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 32.Stone J.R., et al. Consensus statement on surgical pathology of the aorta from the Society for Cardiovascular Pathology and the Association for European Cardiovascular Pathology: I.Inflammatory diseases. Cardiovasc. Pathol. 2015;24:267–278. doi: 10.1016/j.carpath.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Diagnostic Standards and Classification of Tuberculosis in Adults and Children This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America. Am. J. Respir. Crit. Care Med. 1999:1376–1395. doi: 10.1164/ajrccm.161.4.16141. in. [DOI] [PubMed] [Google Scholar]
- 34.Dheda K., Barry C.E., Maartens G. Tuberculosis. Lancet. 2016;387:1211–1226. doi: 10.1016/S0140-6736(15)00151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zumla A., et al. Tuberculosis. N. Engl. J. Med. 2013;368:745–755. doi: 10.1056/NEJMra1200894. [DOI] [PubMed] [Google Scholar]
- 36.Agha R.A., et al. The PROCESS 2020 guideline: updating consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guideline. Int. J. Surg. 2020;84:231–235. doi: 10.1016/j.ijsu.2020.11.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.