Abstract
Objective
The COVID‐19 pandemic has confronted young adults with an unprecedented mental health challenge. Yet, prospective studies examining protective factors are limited.
Methods
In the present study, we focused on changes in mental health in a large sample (N = 685) of at‐risk university students, which were measured before and during the pandemic. Network modeling was applied to 20 measured variables to explore intercorrelations between mental health factors, and to identify risk and protective factors. Latent change score modeling was used on a subset of variables.
Results
The main findings indicate that (1) mental health problems increased at group level, especially depression‐anxiety and loneliness; (2) emotional support during the COVID pandemic was associated with smaller increases in loneliness and depression‐anxiety; (3) COVID‐related stress predicted increases in depression‐anxiety; (4) loneliness acted as a bridge construct between emotional support and changes in mental health.
Conclusion
To mitigate the impact of the COVID‐19 pandemic on the mental health of young adults, is it recommended to focus on interventions that strengthen internal resources (stress‐regulating abilities) and reduce loneliness.
Keywords: at‐risk university students, coping, COVID‐19 pandemic, loneliness, mental health
1. INTRODUCTION
The coronavirus disease 2019 (COVID‐19) outbreak has confronted humankind with a massive medical and humanitarian crisis. Whilst initially, priority was given to the medical implications of the novel coronavirus, soon after mental health implications became a growing concern (Holmes et al., 2020; Yao et al., 2020; Zhang et al., 2020). Recent research is showing a global stress reactionthat isunrelated to the geographical diffusion of the virus (Nocentini et al., 2021). Young people appear to be affected in particular by decreased social contacts and increased loneliness (Tasso et al., 2021). A recent nationwide survey in France among 70,000 self‐selected students indicated that social isolation and low quality of social relations during lockdown were among the strongest concurrent predictors of mental distress (Wathelet et al., 2020). Yet, this study was cross‐sectional and did not have a comparison with life before the pandemic. This is important in light of recall biases: during a crisis, pre‐crisis life looks more rosy than it looked at the time (Infurna & Jayawickreme, 2019). There are few studies with baseline data pre‐COVID‐19, and none of these focused on the impact of the crisis on young adults (Pan et al., 2021; Pinkham et al., 2020; Schäfer et al., 2020). In this context, experts in the field stress the need to identify protective or resilience factors in prospective designs, in order to find actionable links to counter negative effects of the pandemic on mental health (Holmes et al., 2020; Schäfer et al., 2020; Singh et al., 2020; Veer et al., 2021).
In the present study, we tested the effects of the lockdown on students, who had been screened for symptoms of common mental disorders before the pandemic, in the context of a university‐wide program on student mental health. The aim of this study was threefold: (i) to investigate changes in mental health from prior to during the COVID‐19 pandemic; (ii) to investigate pathways between changes in mental health and protective and risk factors, and (iii) to investigate which protective and risk factors predicted (latent) changes. We assessed a wide array of mental health variables, including symptoms of depression, anxiety and substance use, as well as sleep difficulties, happiness, and loneliness, and health‐related risk and protective factors, such as sensed emotional support, relaxing and physical activity. To this end, we employed an exploratory network approach (Borsboom, 2017), supplemented by a latent change score model (LCSM) within a subset of the variables based on the network analysis. This combined approach enabled us to answer two complementary questions. We use the network model to answer the question of how the different changes predict each other. Network analysis is a unique tool to investigate the complex multivariate pathways and interactions between mental health, risk and protective factors. Using the LCSM we answer the additional question of which potential risk and protective factors predict the (latent) changes over time. Moreover, in the LCSM we allowed the mental health variables to predict each other (e.g., predicting ∆anxiety from depressiont1). Both predictors of change and the network of changes can be used to suggest intervention targets and mechanisms.
To the best of our knowledge, this is the first study that adopted a network approach to prospective data gathered before and during the COVID‐19 pandemic. The results of this study have the potential to inform health bodies and policy makers about potentially beneficial interventions, for this and future pandemics, also from a preventive standpoint.
2. METHODS
2.1. Participants and procedures
Data were collected in the context of a large research program, at the University of Amsterdam (UvAcare), aimed at assessing and improving student mental health. This program consisted of a mental health screener (the “Health Check”) with automated tailored feedback (Van der Heijde et al., 2015) and a randomized controlled trial (RCT) testing the effectiveness of an e‐health intervention for depression and anxiety (Klein et al., 2021). For both parts of the study, ethical approval was obtained. All students of the University of Amsterdam were invited to take part in the Health Check, through email invitations, which contained a personalized link to an online questionnaire in Qualtrics. Written informed consent was obtained from all subjects. During the first COVID‐19 lockdown, students who had completed the Health Check at an earlier time point and who had given consent to be re‐contacted, and who were not taking part in the RCT, were invited to fill out the Health Check again. These participants were not included in the intervention study, due to one of the following two reasons: (1) they did not qualify based on the Health Check (scores were too low in terms of mental health complaints) or (2) they did score above the threshold and did not accept the invitation to participate in the RCT. In total, 8576 university students who had filled out the screener before the COVID‐19 crisis were re‐invited. Of this group, 807 students (9.4%) filled out the screener for the second time (see Figure 1).
FIGURE 1.
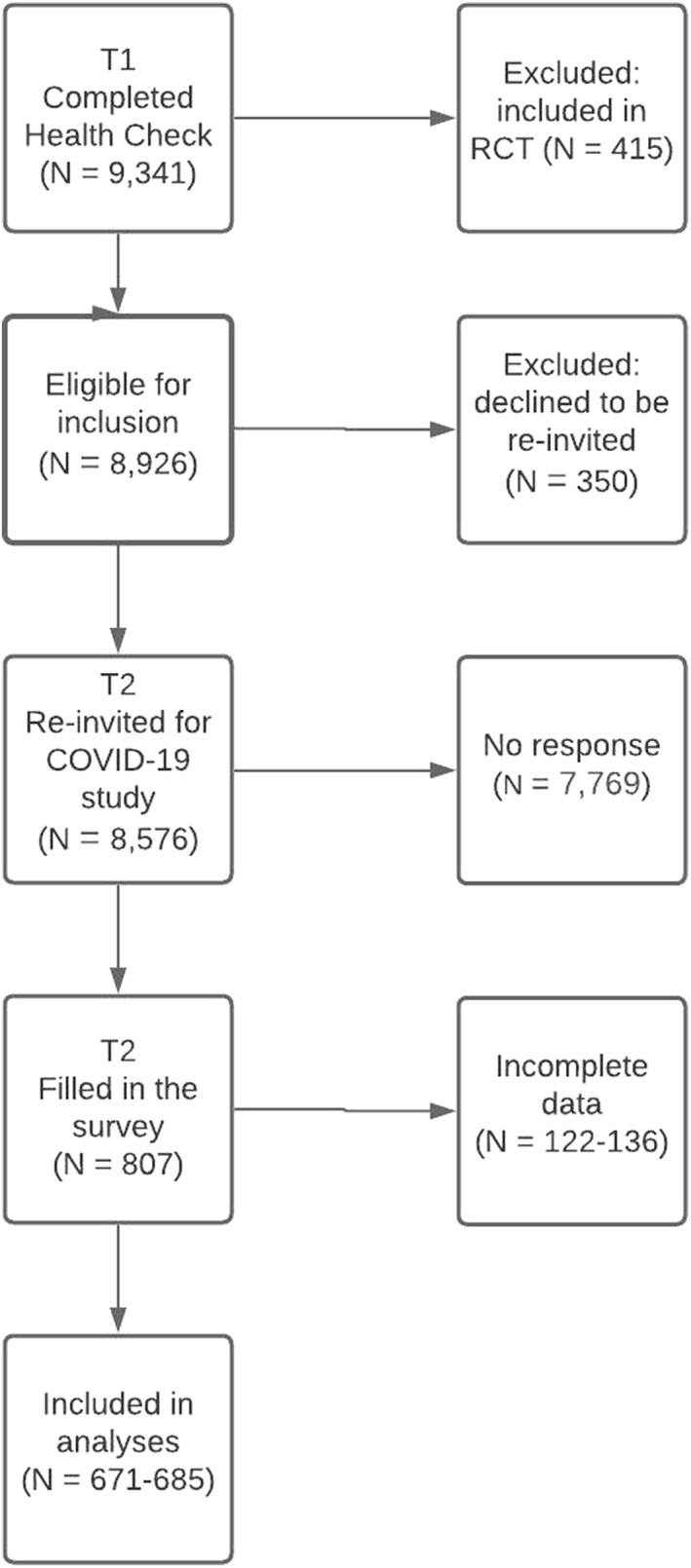
Flow of participants
We added two questionnaires to the regular Health Check to assess their response to the COVID‐19 crisis: a self‐composed “COVID‐19 survey” and a questionnaire assessing coping styles. Data of the second assessment were gathered during the first peak of the pandemic in the Netherlands, from April 16 until May 13, 2020, when the Dutch government partly lifted restrictions. Data of the first assessment were gathered from January 2019 until January 2020, before the first COVID‐19 case in the Netherlands (February 27, 2020). Notably, the current sample constitutes a self‐selected group of at‐risk students (those who decided to fill out the Health Check), of whom 51.6% scored above the cut‐off for clinical depression (scores ≥ 16 on the Center for Epidemiological Studies Depression Scale) or anxiety (scores ≥ 10 on the Generalized Anxiety Disorder screener) on the first assessment.
2.2. Materials
A wide array o7f assessments was done prior to and during COVID‐19 (a full list of all variables is available upon request). Depression was assessed with CES‐D (Radloff, 1977), Generalized Anxiety Disorder with the GAD‐7 (Spitzer et al., 2006). Insomnia was assessed with the Insomnia Severity Index (Bastien et al., 2001), social anxiety with the SIAS‐6 (Peters et al., 2012), and the brief Mini‐Social Phobia Inventory (Connor et al., 2001), alcohol use with the AUDIT‐C (Bush et al., 1998), loneliness with the DJGLS‐11 (de Jong Gierveld & Kamphuis, 1985), subjective health with the Health Survey—Short Form (Hays et al., 1993), happiness with the Subjective Happiness Scale (Lyubomirsky & Lepper, 1999), and stress with three additional questions. Drug use was assessed only prior to the COVID‐19 outbreak using the DAST‐10 (Skinner, 1982).
At T2, we administered a self‐constructed questionnaire concerning the impact of the COVID‐19 pandemic and lockdown, and a validated questionnaire assessing coping styles, the CERQ‐short (Garnefski & Kraaij, 2006). The “COVID‐questionnaire” included questions regarding lifestyle (physical activity, relaxing activities), social interaction (being in a steady relationship, contact with friends, colleagues, peers and family, emotional support), other activities (time spent on studies, social media and smartphone), fear of COVID‐19, and current living situation. The current study focused primarily on mental health in relation to social interaction and lifestyle. Finally, stress experienced as a result of COVID‐19 was assessed with 10 items (e.g., “How often have you experienced stress over the past 2 weeks related to: Taken measures by the government/combining taking care of family and my studies/changes to my financial situation, etc.), with a 5‐point Likert scale ranging from “never” to “always”. The items were added to yield a scale ranging from 10 to 50 with higher levels indicating more stress. The internal consistency of this scale was good (α = 0.85). The questionnaire is available upon request.
The CERQ‐short (Garnefski & Kraaij, 2006) was used to measure nine coping strategies, for maladaptive strategies: Self‐blame, Other‐blame, Rumination, and Catastrophizing, and five adaptive strategies: Positive refocusing, Planning, Positive reappraisal, Putting into perspective and Acceptance. For reasons of parsimony, we combined the subscales into two broad maladaptive and adaptive coping scales.
2.3. Statistical analysis
Analyses were performed using R version 4.0.2 (R Core Team, 2013) and SPSS version 27 (IBM SPSS Statistics for Macintosh, 2020). Participants were included when they had completed at least 75% of the items of each questionnaire. On the few occasions that less than 25% of items were missing, average item scores were imputed, based on the group mean for all items. Associations between the main mental health variables were inspected using Pearson correlation coefficients. Depression and general anxiety were highly correlated (r (707) = 0.82, p < 0.001), and combined into an aggregate variable (α = 0.89 at T1 and 0.87 at T2), as were the measures for social anxiety and social avoidance (r (711) = 0.63, p < 0.001), which were also combined (α = 0.89 T1, and 0.90 at T2). The scale scores were divided by their theoretical maximums, added, and then averaged, so that people responding no to all items (on both depression and generalized anxiety) scored 0 and people responding yes to all items received a score of 1. Using the norms from the questionnaire manuals, students were classified as mild, moderate, or severe (or high vs. low) on key mental health variables, before and during the pandemic. The significance of the corresponding categorical changes was assessed with Chi‐square tests. Cases were excluded pairwise (T1, T2) per variable, rendering a total sample size between N = 671 (depression) and N = 683 (generalized anxiety, social avoidance). We performed exploratory ordinal regression analysis to select variables from the COVID questionnaire that contributed most to the change in mental health problems. As dependent variable, we used a composite scale for mental health problems, based on a confirmatory factor analysis in R. This scale contained the following variables: depression, generalized anxiety, social anxiety, social avoidance, and insomnia (please see the description above).
To address aim ii, exploratory network analysis was used to investigate the multivariate interactions between mental health variables and protective and risk factors. An edge in the network represents the unique relationship between two variables, while controlling for all other variables included in the analysis. We limited the network to 20 variables, based on the ordinal regression analysis. Mixed Graphical Model (MGM) was used to estimate the network (Haslbeck & Waldorp, 2020) including (i) the difference score (T2 minus T1) of depression‐generalized anxiety, insomnia, social anxiety‐social phobia, alcohol use, stress, subjective health, happiness, and loneliness, (ii) drug abuse at T1, (iii) stress related to COVID‐19, emotional support, contact with family, contact with friends, adaptive coping, maladaptive coping, moderate physical activity, and relaxing activities at T2, (iv) the demographic variables (i.e., age, gender, and international student status) (other combinations [e.g., generalized anxiety] are included in the supplementary materials; see Figures S2–S8 in supporting information S2). LASSO regularization was used to exclude spurious edges from the network (Epskamp & Fried, 2018). To this aim, the optimal tuning parameter was selected minimizing the Extended Bayesian Information Criterion (EBIC) using 0.25 as hyperparameter. (Models estimated with more and less conservative hyperparameters are shown in the supplementary materials, see Figures S2–S8 in supporting information S2.) We used multiple imputations, as the estimator is not able to handle missing data. Our results are based on 10 multiple imputations using the mice package in R, with the final network showing the average edge weight of edges that were included in nine out of 10 estimated networks. We only included participants who filled out at least 50% of the total number of variables included in the network and at least 50% of the mental health variables. The final sample size for the network analysis was N = 685. Lastly, the accuracy and robustness of the edge weights (Borsboom et al., 2018) were evaluated by running 1000 bootstrapped samples (Figure S1 in supporting information S1). Network analyses were conducted with the R packages bootnet and MGM.
To examine the variables directly influencing changes in mental health in the network in more detail, and to explore which risk and protective factors predict these changes (aim iii), a latent change score model (LCSM) was employed on a subset of variables. This subset of variables was based on the most salient findings from the network model. The LCSM allows for more fine‐tuned analysis of the correlational structure of change variables, on how well change in variables can be predicted by exogenous variables, and includes regression to the mean. This type of structural equation model is applicable to two‐wave longitudinal data and allows us to investigate multiple predictors of several change variables using a single integrative model (Kievit et al., 2018; McArdle & Grimm, 2010) (for a detailed description of the LCSM, see supporting information S3).
3. RESULTS
3.1. Sample characteristics
Of the participants 70% was female (N = 566). The mean age was 22.5 years (SD = 5.5; range 17–67). Approximately 30% of the sample indicated to be an international student, of which 56.5% had a Western European background, 16% an Eastern European background, 16% was of Asian descent, and 11% came from North or South America. Most (∼70%) were bachelor students.
3.2. Selection of variables
Variables not directly related to mental health were excluded, such as study satisfaction. From the COVID questionnaire, we selected variables related to health‐related activities and social relationships. Based on an exploratory ordinal regression analysis, variables with no relation to (change) in psychopathology were discarded, such as “being in a steady relationship” and “fear of contracting COVID”.
3.3. Severity rates for key mental health variables
Overall, mental complaints increased from T1 to T2 (Table 1). At T2, 55.3% scored above threshold for likely clinical depression, compared to 48.7% at T1 (X2 [1, N = 671] = 209.60; p < 0.001). Roughly 3% more participants experienced clinically significant generalized anxiety during COVID (X2 [9, N = 683] = 296.37; p < 0.001). At T2, 2.1% of the participants experienced clinically severe insomnia compared to none at T1 (X2 [6, N = 680] = 263.16; p < 0.001). Roughly 5% more people experienced social anxiety at T2 compared to T1 (X2 [1, N = 679] = 272.95; p < 0.001). Loneliness increased with 7% (X2 [9, N = 679] = 394.45; p < 0.001). Interestingly, social avoidance and alcohol use decreased (social avoidance: X2 [1, N = 683] = 181.67; p < 0.001; alcohol use, men: X2 [1, N = 207] = 32.56; p < 0.001; alcohol use, women: X2 [1, N = 504] = 140.61; p < 0.001).
TABLE 1.
Severity levels of mental health variables at T1 (before the COVID‐19 pandemic) and T2 (during the COVID‐19 pandemic)
| Target variable | Level | T1 (N) | T1 (%) | T2 (N) | T2 (%) | X 2 | p |
|---|---|---|---|---|---|---|---|
| Depression | Low | 344 | 51.3 | 300 | 44.7 | 209.6 | <0.001 |
| High | 327 | 48.7 | 371 | 55.3 | |||
| Total | 671 | 100 | 671 | 100 | |||
| Generalized anxiety | No anxiety | 218 | 31.9 | 199 | 29.1 | 296.37 | <0.001 |
| Mild anxiety | 236 | 34.6 | 235 | 34.4 | |||
| Moderate anxiety | 139 | 20.4 | 150 | 22.0 | |||
| Severe anxiety | 90 | 13.2 | 99 | 14.5 | |||
| Total | 683 | 100 | 683 | 100 | |||
| Insomnia | No insomnia | 339 | 49.9 | 345 | 50.7 | 263.16 | <0.001 |
| Subthreshold insomnia | 243 | 35.7 | 240 | 35.3 | |||
| Moderate insomnia | 98 | 14.4 | 81 | 11.9 | |||
| Severe insomnia | 0 | 0 | 14 | 2.1 | |||
| Total | 680 | 100 | 680 | 100 | |||
| Social anxiety | Low | 510 | 75.1 | 478 | 70.4 | 272.95 | <0.001 |
| High | 169 | 24.9 | 201 | 29.6 | |||
| Total | 679 | 100 | 679 | 100 | |||
| Social avoidance | Low | 494 | 72.3 | 511 | 74.8 | 181.67 | <0.001 |
| High | 189 | 27.7 | 172 | 25.2 | |||
| Total | 683 | 100 | 683 | 100 | |||
| Alcohol use (males) | Low | 179 | 86.5 | 187 | 90.3 | 32.56 | <0.001 |
| High | 28 | 13.5 | 20 | 9.7 | |||
| Total | 207 | 100 | 207 | 100 | |||
| Alcohol use (females) | Low | 427 | 84.7 | 464 | 92.1 | 140.61 | <0.001 |
| High | 77 | 15.3 | 40 | 7.9 | |||
| Total | 504 | 100 | 504 | 100 | |||
| Drug use | Low | 634 | 88.3 | ||||
| High | 84 | 11.7 | |||||
| Total | 718 | 100 | |||||
| Loneliness | Not lonely | 292 | 43.0 | 244 | 35.9 | 394.45 | <0.001 |
| Moderately lonely | 292 | 43.0 | 316 | 46.5 | |||
| Severely lonely | 69 | 10.2 | 89 | 13.1 | |||
| Very severely lonely | 26 | 3.8 | 30 | 4.4 | |||
| Total | 679 | 100 | 679 | 100 |
3.4. Network analysis
The network analysis (Figure 2) showed a cluster of mental health change scores (T2 – T1) and a cluster of “influencing factors” and demographics. In the mental health cluster, depression‐anxiety was the most central node, connected to all other mental health change scores except for alcohol use (which was disconnected). Three “influencing factors” could be identified as direct predictors of change in mental health: emotional support during COVID‐19, COVID‐related stress, and adaptive coping during COVID‐19. First, more contact with friends and family during COVID‐19 was associated with higher emotional support, which was associated with a smaller increase in loneliness, which was in turn associated with smaller increases in depression‐anxiety and social anxiety. Second, adaptive coping emerged as protective factor, with high scores being associated with smaller decreases in happiness, which predicted smaller increases in mental health problems (particularly depression‐anxiety), and smaller decreases in physical health. Third, COVID‐related stress came out as a risk factor for mental health problems: higher COVID‐related stress was associated with larger increases in depression‐anxiety, which was in turn associated with larger increases in other mental health symptoms including stress and insomnia. Interestingly, the protective and risk factors were related to each other. For example, emotional support was positively associated with adaptive coping and negatively associated with COVID‐related stress. This implies that emotional support during COVID‐19 could affect mental health along these two additional pathways, while adaptive coping and COVID‐related stress could influence the degree of emotional support one receives and perceives. Furthermore, higher physical activity was associated with both higher adaptive coping and emotional support, suggesting that maintaining physical activity also plays a role in mental health. Maladaptive coping predicted larger COVID‐related stress, and vice versa.
FIGURE 2.
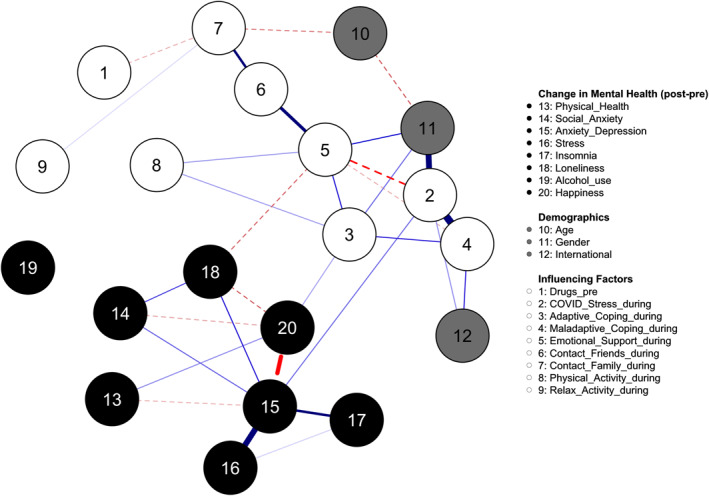
The network model. Dashed edges represent negative associations, while solid edges represent positive associations. Edge width and saturation were scaled based on the maximum edge found in the network (r = 0.34), which is comparable to the strongest edge found in a meta‐analytic network analysis of post‐traumatic stress disorder symptoms (Isvoranu et al., 2021). Thus, wider and brighter edges indicate stronger connections. A pre‐defined algorithm (Spring) was used to define the layout, but nodes 15 and 16 were manually placed slightly lower to avoid unclear visualization:
Adaptive_Coping_during = adaptive coping (e.g., positive refocusing) during the pandemic
Contact_Family_during = frequency of contact with family during the pandemic per day/week
Contact_Friends_during = frequency of contact with friends during the pandemic per day/week
COVID_Stress during = level of subjective COVID‐related stress experienced during the pandemic
Drugs_pre = drug use prior to COVID‐19 pandemic (T1)
Emotional_Support_during = level of experienced emotional support during the pandemic
Maladaptive_Coping_during = maladaptive coping (e.g., rumination) during the pandemic
Physical_Activity_during = frequency of moderate (max. 30 min) physical activities per week during the pandemic
Relax_Activity_during = frequency of relaxing activities per week during the pandemic
There were also two indirect pathways including “international student” and “gender”. International students scored higher on maladaptive coping, and experienced more COVID‐related stress, thus rendering them at risk for elevated levels of depression‐anxiety. Women experienced more emotional support and scored higher on adaptive coping, but also on COVID‐related stress, which in turn was negatively associated with emotional support.
3.5. Latent change score analysis
The LCSM analysis on a subset of important variables in the network, showed the largest increases in loneliness and depression‐anxiety (see Figure 3). Experienced emotional support during COVID‐19 was the strongest (negative) predictor of changes in loneliness (β = −0.46; p < 0.001), whereas COVID‐related stress was the strongest (positive) predictor of changes in depression‐anxiety (β = 0.42; p < 0.001). Only one variable at T1 predicted a (latent) change variable: More happiness at T1 predicted a change in loneliness at T2 (β = −0.11; p < 0.05), indicating either less increase or more decrease in loneliness for individuals who reported to be happier before the pandemic (coefficient not displayed in Figure 3).
FIGURE 3.
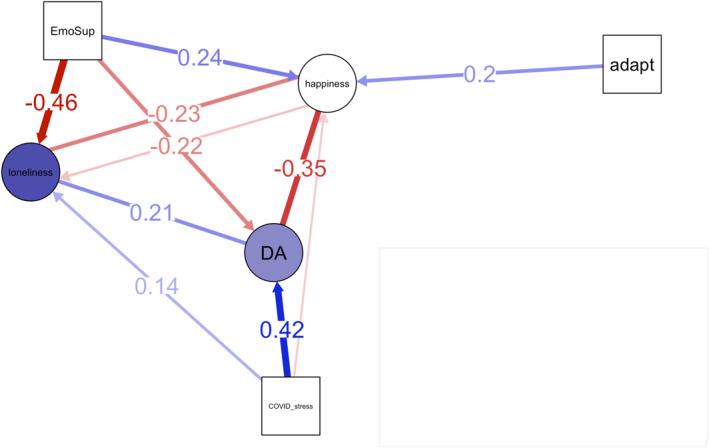
Latent Change Score Model. Circles (nodes) represent latent change scores, and the squares represent predictors of latent change scores. Colored circles, in contrast to white circles, indicate a significant change from T1 to T2. The direction of this effect is indicated through the depth of color. Blue and red colors reflect positive and negative effects, respectively. White colored circular nodes show non‐significant changes. Lines with arrow heads indicate predictive effects while lines without arrow heads visualize correlations between change variables (change correlation parameters). Only lines with significant effects are shown and lines with coefficients smaller than 0.1 have no coefficient displayed. All displayed estimates are standardized. adapt = adaptive coping during COVID‐19; DA = composite of the change in depression + generalized anxiety; EmoSup = emotional support during COVID‐19
4. DISCUSSION
This study investigated the effects of the COVID‐19 pandemic in vulnerable, mentally at‐risk students, by examining how various aspects of mental health and lifestyle changed and interacted. Importantly, this is the first study reporting the impact of the COVID‐19 pandemic on changes in mental health in vulnerable young adults, who had been assessed prior to the pandemic. Generalized anxiety, depression, and loneliness increased during the first months of the pandemic, compared to before the outbreak. This is in line with recent data from another prospective study, showing a general increase in symptoms during the first lockdown in the Netherlands, except in individuals with severe or chronic mental disorders (Pan et al., 2021). Changes in depression‐anxiety were most central, and related to changes in loneliness and happiness. Emotional support as well as COVID‐related stress were the most robust predictors of changes in mental health. These findings also correspond with findings from other studies conducted during the pandemic, showing that perceived social support (Veer et al., 2021), and not feeling alone (Fried et al., 2021) may serve as protective factors. Our results showing that specific identified factors could either protect against, or put people at risk for, mental complaints, could provide a sound “counter‐narrative” to media reports of a sharp increase in mental health across all subgroups in the general population (Shevlin et al., 2021). The impact of the COVID‐19 pandemic on mental health seems much more heterogeneous than often assumed, and research should therefore prioritize the identification of at‐risk subgroups (Holmes et al., 2020). We think that our findings meet this call.
4.1. Practical and clinical implications
In terms of the implementation of our findings, the observed pathways point to actionable nodes including coping, and emotional support, and their respective impact on happiness, and loneliness. In particular, effective interventions to enhance emotional support and to strengthen adaptive coping would seem important. For example, it seems relevant to proactively develop strategies during a pandemic to promote bringing young people together within the applied restrictions. In particular, sharing emotional experiences appears to be a pivotal factor in countering loneliness and thus alleviating the impact of the pandemic and lockdown. Our findings also suggest that enhancing “internal resources” (such as being able to accept or positively re‐appraise events, or to put things into perspective) can mitigate the impact of stress on mental health. This is especially relevant, given that the lockdown limits external resources, such as seeking emotional support and physical exercise. Importantly, a recent brief intervention for adolescents has shown promising results in creating a “growth mindset” (Schleider & Weisz, 2016, 2018), which warrants further study in students. Our study also indicates that increasing happiness could become part of intervention strategies, also from a preventive standpoint regarding future pandemics. Increasing well‐being, apart from a focus on psychopathology, can have advantageous effects (Meulenbeek et al., 2015). Finally, maintaining physical activity during the COVID‐19 pandemic was associated with more adaptive coping and increased emotional support, suggesting a role for exercise in mitigating the negative consequences of the pandemic, in line with a large review on lifestyle factors in psychiatry (Firth et al., 2020).
4.2. Strengths and limitations
A major strength of this paper is that we compared individuals before and during COVID‐19, enabling us to estimate how symptoms and related health behaviors changed during the pandemic, while focusing on young adults. Moreover, we used network approaches to detect pathways between mental health variables. Applying a network analysis to a wide array of variables allowed us to find actionable nodes and pathways, which we think is a good showcase for what a network analysis can contribute to much‐needed knowledge during an unforeseen crisis.
The results of this study have to be interpreted within the context of several limitations. First, the sample constitutes a self‐selected sample of at‐risk university students, who were willing to complete the survey twice. About 10% of the original respondents completed our COVID‐survey, which could not be representative of the total student population. Comparing those who responded to our invitation during the COVID‐19 pandemic with those who responded to the original survey (explicitly excluding those in the current sample that responded twice) (N > 8500) yielded no significant differences concerning depression or generalized anxiety. This suggests that responders to the COVID‐19 survey could be considered a representative sample of the students that normally respond to our survey. Obviously, the results cannot be generalized to general student populations (people without complaints are unlikely to fill out a mental health screener). Second, our COVID‐19 questionnaire was ad hoc. Third, in the LCSM, our predictors were assessed at T2 (during the pandemic), which limits the possibility to draw causal inferences. On a related note, due to the sudden nature of the pandemic, we did not pre‐register our study. Fourth, as analyses are correlational, all pathways in the network could go both ways, precluding definite conclusions about directionality. Fifth, we selected variables from a large battery of measures to explore relationships that were deemed meaningful, which may have caused us to miss other relevant associations. Sixth, it should be noted that the sample size may not have been sufficient to detect all edges in the network. Seventh, the trends observed in this study could be reexamined over longer periods, to obtain more information beyond the initial emotional impact of the COVID‐19 pandemic. Finally, we did not include any information on racial/ethnic identification in this paper.
4.3. Conclusions
The present study on effects of the COVID‐19 lockdown in vulnerable students, showed that mental health problems increased during the first lockdown period after the COVID‐19 outbreak. Results indicated higher levels of emotional support and adaptive coping as important protective factors, while COVID‐related stress was a risk factor for increases in depression‐anxiety and related mental health problems. Interventions could focus on increasing stress‐regulating abilities, emotional support, well‐being/happiness, and on reducing loneliness.
CONFLICT OF INTEREST
The authors declare no conflict of interests.
Supporting information
Supporting Information S1
Supporting Information S2
Supporting Information S3
ACKNOWLEDGEMENTS
The UvAcare project received internal funding from the University of Amsterdam. We would like to thank Jorien van Blom, Samantha Roetink, Ruben Atteveld and Eline Bol for their contributions to the design and/or management of the UvAcare project.
Koelen, J. A. , Mansueto, A. C. , Finnemann, A. , de Koning, L. , van der Heijde, C. M. , Vonk, P. , Wolters, N. E. , Klein, A. , Epskamp, S. , & Wiers, R. W. (2022). COVID‐19 and mental health among at‐risk university students: A prospective study into risk and protective factors. International Journal of Methods in Psychiatric Research, 31(1), e1901. 10.1002/mpr.1901
Sacha Epskamp and Reinout Wiers share senior authorship.
Contributor Information
Jurrijn A. Koelen, Email: j.a.koelen@uva.nl, Email: r.w.h.j.wiers@uva.nl.
Reinout W. Wiers, Email: j.a.koelen@uva.nl, Email: r.w.h.j.wiers@uva.nl.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
REFERENCES
- Bastien, C. H. , Vallières, A. , & Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. [DOI] [PubMed] [Google Scholar]
- Borsboom, D. (2017). A network theory of mental disorders. World Psychiatry, 16(1), 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom, D. , Robinaugh, D. J. , Rhemtulla, M. , & Cramer, A. O. J. (2018). Robustness and replicability of psychopathology networks. World Psychiatry, 17, 143–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush, K. , Kivlahan, D. R. , McDonell, M. B. , Fihn, S. D. , & Bradley, K. A. , & ACQUIP . (1998). The AUDIT alcohol consumption questions. Archives of Internal Medicine, 158, 1789–1795. [DOI] [PubMed] [Google Scholar]
- Connor, K. M. , Kobak, K. A. , Churchill, L. E. , Katzelnick, D. , & Davidson, J. R. T. (2001). Mini‐SPIN: A brief screening assessment for generalized social anxiety disorder. Depression and Anxiety, 14, 137–140. [DOI] [PubMed] [Google Scholar]
- de Jong Gierveld, J. , & Kamphuis, F. (1985). The development of a Rasch‐type loneliness‐scale. Applied Psychological Measurement, 9, 289–299. [Google Scholar]
- Epskamp, S. , & Fried, E. I. (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23, 617–634. [DOI] [PubMed] [Google Scholar]
- Firth, J. , Solmi, M. , Wootton, R. E. , Vancampfort, D. , Schuch, F. B. , Hoare, E. , Stubbs, B. , Torous, J. , Teasdale, S. B. , Jackson, S. E. , Smith, L. , Eaton, M. , Jacka, F. N. , Veronese, N. , Marx, W. , Ashdown‐Franks, G. , Siskind, D. , Sarris, J. , Rosenbaum, S. , … Stubbs, B. (2020). A meta‐review of “lifestyle psychiatry”: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry, 19, 360–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried, E. I. , Papanikolaou, F. , & Epskamp, S. (2021). Mental health and social contact during the COVID‐19 pandemic: An ecological momentary assessment study. Clinical Psychological Science, 1–15. 10.1177/21677026211017839 [DOI] [Google Scholar]
- Garnefski, N. , & Kraaij, V. (2006). Cognitive emotion regulation questionnaire – Development of a short 18‐item version (CERQ‐short). Personality and Individual Differences, 41, 1045–1053. [Google Scholar]
- Haslbeck, J. M. B. , & Waldorp, L. J. (2020). MGM: Estimating time‐varying mixed graphical models in high‐dimensional data. Journal of Statistical Software, 93(Ii). [Google Scholar]
- Hays, R. D. , Sherbourne, C. D. , & Mazel, R. M. (1993). The RAND 36‐item health survey 1.0. Health Economics, 2, 217–227. [DOI] [PubMed] [Google Scholar]
- Holmes, E. A. , O’Connor, R. C. , Perry, V. H. , Tracey, I. , Wessely, S. , Arseneault, L. , & Bullmore, E. (2020). Multidisciplinary research priorities for the COVID‐19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7, 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM SPSS Statistics for Macintosh (27.0). (2020). IBM Corp. [Google Scholar]
- Infurna, F. J. , & Jayawickreme, E. (2019). Fixing the growth illusion: New directions for research in resilience and posttraumatic growth. Current Directions in Psychological Science, 28, 152–158. [Google Scholar]
- Isvoranu, A.‐M. , Epskamp, S. , & Cheung, M. (2021). Network models of post‐traumatic stress disorder: A meta‐analysis. Journal of Abnormal Psychology. 10.31234/osf.io/8k4u6 [DOI] [PubMed] [Google Scholar]
- Kievit, R. A. , Brandmaier, A. M. , Ziegler, G. , van Harmelen, A. L. , de Mooij, S. M. M. , Moutoussis, M. , & Dolan, R. J. (2018). Developmental cognitive neuroscience using latent change score models: A tutorial and applications. Developmental Cognitive Neuroscience, 33, 99–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, A. , Wolters, N. E. , Bol, E. J. M. , Koelen, J. , de Koning, L. , Roetink, S. S. M. , van Blom, J. J. , Pronk, T. , van der Heijde, C. , Salemink, E. , Bolinski, F. , Riper, H. , Karyotaki, E. , Cuijpers, P. , Schneider, S. , Rapee, R. M. , Vonk, P. , & Wiers, R. W. (2021). Online computer or therapist‐guided cognitive behavioral therapy in university students with anxiety and/or depression: Study protocol of a randomised controlled trial. BMJ Open, 11(11), e049554. 10.1136/bmjopen-2021-049554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky, S. , & Lepper, H. S. (1999). A measure of subjective happiness: Preliminary reliability and construct validation. Social Indicators Research, 46, 137–155. [Google Scholar]
- McArdle, J. J. , & Grimm, K. J. (2010). Five steps in latent curve and latent change score modeling with longitudinal data. In van Montfort K., Oud J. H. L., & Satorra A. (Eds.), Longitudinal research with latent variables (pp. 245–273). Springer International Publishing. [Google Scholar]
- Meulenbeek, P. , Christenhusz, L. , & Bohlmeijer, E. (2015). Well‐being therapy in the Netherlands. Psychotherapy and Psychosomatics, 84, 316–317. [DOI] [PubMed] [Google Scholar]
- Nocentini, A. , Palladino, B. E. , & Menesini, E. (2021). Adolescents’ stress reactions in response to COVID‐19 pandemic at the peak of the outbreak in Italy. Clinical Psychological Science, 9, 507–514. [Google Scholar]
- Pan, K. Y. , Kok, A. A. L. , Eikelenboom, M. , Horsfall, M. , Jörg, F. , Luteijn, R. A. , & Penninx, B. W. J. H. (2021). The mental health impact of the COVID‐19 pandemic on people with and without depressive, anxiety, or obsessive‐compulsive disorders: A longitudinal study of three Dutch case‐control cohorts. The Lancet Psychiatry, 8, 121–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters, L. , Sunderland, M. , Andrews, G. , Rapee, R. M. , & Mattick, R. P. (2012). Development of a Short Form Social Interaction Anxiety (SIAS) and Social Phobia Scale (SPS) using nonparametric item response theory: The SIAS‐6 and the SPS‐6. Psychological Assessment, 24, 66–76. [DOI] [PubMed] [Google Scholar]
- Pinkham, A. E. , Ackerman, R. A. , Depp, C. A. , Harvey, P. D. , & Moore, R. C. (2020). A longitudinal investigation of the effects of the COVID‐19 pandemic on the mental health of individuals with pre‐existing severe mental illnesses. Psychiatry Research, 294, 113493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . (2013). R: A language and environment for statistical computing (4.0.2). R Foundation for Statistical Computing. [Google Scholar]
- Radloff, L. S. (1977). The CES‐D scale: A self‐report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Schäfer, S. K. , Sopp, M. R. , Schanz, C. G. , Staginnus, M. , Göritz, A. S. , & Michael, T. (2020). Impact of COVID‐19 on public mental health and the buffering effect of a sense of coherence. Psychotherapy and Psychosomatics, 89, 386–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider, J. , & Weisz, J. (2018). A single‐session growth mindset intervention for adolescent anxiety and depression: 9‐Month outcomes of a randomized trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 59, 160–170. [DOI] [PubMed] [Google Scholar]
- Schleider, J. L. , & Weisz, J. R. (2016). Reducing risk for anxiety and depression in adolescents: Effects of a single‐session intervention teaching that personality can change. Behaviour Research and Therapy, 87, 170–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin, M. , Butter, S. , McBride, O. , Murphy, J. , Gibson‐Miller, J. , Hartman, T. , & Bentall, R. (2021). Refuting the myth of a ‘tsunami’ of mental ill‐health in populations affected by COVID‐19: Evidence that response to the pandemic is heterogenous, not homogeneous. Psychological Medicine, 1–9. 10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh, S. , Roy, D. , Sinha, K. , Parveen, S. , Sharma, G. , & Joshi, G. (2020). Impact of COVID‐19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Research, 293. 10.1016/j.psychres.2020.113429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner, H. A. (1982). The drug abuse screening test. Addictive Behaviors, 7, 363–371. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L. , Kroenke, K. , Williams, J. B. W. , & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD‐7. Archives of Internal Medicine, 166, 1092–1097. [DOI] [PubMed] [Google Scholar]
- Tasso, A. F. , Hisli Sahin, N. , & San Roman, G. J. (2021). COVID‐19 disruption on college students: Academic and socioemotional implications. Psychological Trauma: Theory, Research, Practice, and Policy, 13, 9–15. [DOI] [PubMed] [Google Scholar]
- Van der Heijde, C. M. , Vonk, P. , & Meijman, F. J. (2015). Self‐regulation for the promotion of student health. Traffic lights: The development of a tailored web‐based instrument providing immediate personalized feedback. Health Psychology and Behavioral Medicine, 3, 169–189. [Google Scholar]
- Veer, I. M. , Riepenhausen, A. , Zerban, M. , Wackerhagen, C. , Puhlmann, L. M. C. , Engen, H. , & Kalisch, R. (2021). Psycho‐social factors associated with mental resilience in the Corona lockdown. Translational Psychiatry, 11, 67. 10.1038/s41398-020-01150-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet, M. , Duhem, S. , Vaiva, G. , Baubet, T. , Habran, E. , Veerapa, E. , & D’Hondt, F. (2020). Factors associated with mental health disorders among university students in France confined during the COVID‐19 pandemic. JAMA Network Open, 3, e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao, H. , Chen, J. H. , & Xu, Y. F. (2020). Patients with mental health disorders in the COVID‐19 epidemic. The Lancet Psychiatry, 7(4), e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Zhang, H. , Ma, X. , & Di, Q. (2020). Mental health problems during the COVID‐19 pandemics and the mitigation effects of exercise: A longitudinal study of college students in China. International Journal of Environmental Research and Public Health, 17, 3722. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information S1
Supporting Information S2
Supporting Information S3
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information that could compromise the privacy of research participants.


