Abstract
Aims
Vertebral body tethering (VBT) is a non-fusion technique to correct scoliosis. It allows correction of scoliosis through growth modulation (GM) by tethering the convex side to allow concave unrestricted growth similar to the hemiepiphysiodesis concept. The other modality is anterior scoliosis correction (ASC) where the tether is able to perform most of the correction immediately where limited growth is expected.
Methods
We conducted a retrospective analysis of clinical and radiological data of 20 patients aged between 9 and 17 years old, (with a 19 female: 1 male ratio) between January 2014 to December 2016 with a mean five-year follow-up (4 to 7).
Results
There were ten patients in each group with a total of 23 curves operated on. VBT-GM mean age was 12.5 years (9 to 14) with a mean Risser classification of 0.63 (0 to 2) and VBT-ASC was 14.9 years (13 to 17) with a mean Risser classification of 3.66 (3 to 5). Mean preoperative VBT-GM Cobb was 47.4° (40° to 58°) with a Fulcrum unbend of 17.4 (1° to 41°), compared to VBT-ASC 56.5° (40° to 79°) with 30.6 (2° to 69°)unbend. Postoperative VBT-GM was 20.3° and VBT-ASC Cobb angle was 11.2°. The early postoperative correction rate was 54.3% versus 81% whereas Fulcrum Bending Correction Index (FBCI) was 93.1% vs 146.6%. The last Cobb angle on radiograph at mean five years’ follow-up was 19.4° (VBT-GM) and 16.5° (VBT-ASC). Patients with open triradiate cartilage (TRC) had three over-corrections. Overall, 5% of patients required fusion. This one patient alone had a over-correction, a second-stage tether release, and final conversion to fusion.
Conclusion
We show a high success rate (95%) in helping children avoid fusion at five years post-surgery. VBT is a safe technique for correction of scoliosis in the skeletally immature patient. This is the first report at five years that shows two methods of VBT can be employed depending on the skeletal maturity of the patient: GM and ASC.
Cite this article: Bone Jt Open 2022;3(2):123–129.
Keywords: Vetebral body tethering, Adolescent idiopathic scoliosis, Growth modulation, Anterior spinal correction, Risser, Skeletal maturity, Tri-radiate cartilage, vertebral body, Cobb angles, scoliosis, Radiographs, triradiate cartilage (TRC), retrospective analysis, hemiepiphysiodesis, randomized control trial, surrogate marker, cartilages
Introduction
Tethering was first demonstrated in a case report by Crawford and Lenke 1 in 2010, showing a four-year follow-up of progressive correction in an immature juvenile idiopathic scoliosis. Prior to this, studies had already demonstrated that tethering can induce a scoliosis in porcine, goat, and bovine models, thus giving proof of concept. 2-4 Other anterior surgical growth modulation (GM) techniques exist and, simultaneous to the study of tethering, there have been results showing success with vertebral body stapling. The largest success has been in smaller flexible curves (< 35°) but larger thoracic curves remain a challenge. 5,6
The early results of vertebral body tethering (VBT) by Samdani et al 7 have been promising. The Shriners Hospital Group have demonstrated progressive correction of the Cobb angle at one- and two-year follow-up of the skeletally immature adolescent idiopathic scoliosis (AIS). There is anterior derotation improvement of rib hump seen by scoliometer angle improvements and maintenance of thoracic kyphosis. Subjectively, these children maintain flexibility compared to the gold standard of fusion.
The initial studies have focused on using VBT as a GM technique with criteria of inclusion focusing on skeletal immaturity such premenarchal status, a low Risser grade (mean 0.42), and low digital Sanders (mean 3.2). 8 It should also be noted that flexibility was an important factor and 50% flexibility was an additional criteria.
VBT has two different methods of use. First, VBT may be used as a growth modulator in the immature AIS patient where significant growth is expected, and therefore progressive correction over time. This term was first coined in the case report by Crawford and Lenke. 1 The second modality is anterior scoliosis correction (ASC) using the same hardware but with some modification of technique. 9 ASC is used in patients with greater maturity (higher Risser or Sanders grade), greater magnitude of scoliosis, and greater stiffness. 10 GM is not obtained and immediate correction is attempted.
The aim of this study was to evaluate the radiological results of patients treated with VBT in two distinct groups of skeletal maturity, and determine if this as a safe technique to obviate fusion in the treatment of carefully selected patients with idiopathic scoliosis.
Methods
Authorization and application via institutional board review process was undertaken for this retrospective study and given the reference AUDI000780. Patient records and roentgenograms were examined between 2014 and 2017 in a consecutive series at a single institution. Prospective data was used from the surgeon’s British Spinal Registry (Amplitude) 11 in a consecutive series of patients from 2014 to 2017.
Two groups were compared: VBT-GM and VBT-ASC. The criteria for inclusion was the immature AIS patient with remaining growth based on Risser grade. Patients were included if they had failed bracing or had curves outside the criteria of the SRS Bracing guidelines. 12 VBT-GM technique was chosen for Risser grade 0 to 2 with Cobb angle > 40°. VBT-ASC technique was chosen for Risser grade 3 to 5 with Cobb angles > 40°. A fulcrum bending radiograph was used and patients were excluded if flexibility was less than 40%.
The technique used has previously been described by Samdani et al. 8 We similarly used Zimmer Biomet Dynesys system in an off-label method. We followed the regulations regarding off-label use in our institution. In August 2019, Zimmer Biomet The Tether - Vertebral Body Tethering System - H190005 (USA) received FDA approval. 13
The demographic details of the patients were noted. The skeletal maturity was recorded using Risser grade. Cobb angles were measured on preoperative whole spine radiographs. A fulcrum bending film was used to measure flexibility and the Fulcrum Bending Correction Index. 14 Postoperative radiographs were analyzed for Cobb angles over time: immediately postoperatively, six weeks postoperatively, six months postoperatively, and then annually. Unplanned surgery, complications, and revision to definitive fusion were recorded. Radiological failure was considered if the Cobb angle was > 35°. Conversion to Fusion was recognised as definitive failure of the VBT technique.
Statistical analysis
SPSS v. 25 (IBM, USA) was used for the creation of graphs. No further statistical analysis was performed on this comparison study.
Results
The results are summarized in Table I. VBT-GM is depicted in Figure 1 with a mean follow-up of 64.5 months (55 to 76). VBT-ASC is depicted in Figure 2 with a mean follow-up of 56.6 months (56 to 60). Overall, there is a mean 60.5-month follow-up (55 to 76).
Table I.
Vertebral body tethering growth modulation compared to vertebral body tethering anterior scoliosis correction with a mean follow-up of five years (60.5 months).
| Variable | VBT-GM | VBT-ASC |
|---|---|---|
| Patients, n | 10 | 10 |
| Curves instrumented, n | 11 | 12 |
| Sex, n | 10 female | 9 female, 1 male |
| Mean age, yrs (range) | 12.57 (9 to 14) | 14.99 (13 to 17) |
| Mean Risser grade (range) | 0.63 (0 to 2) | 3.66 (3 to 5) |
| Tri-radiate cartilage open, % (n) | 40 (4) | 0 (0) |
| Closed, % (n) | 60 (6) | 100 (10) |
| Single right curve MT, n | 6 (Lenke 1 A) | 5 (Lenke 1 A) |
| Single left curve MT, n | 1 (Lenke 1 A) | |
| Single Curve TL, n | 0 | 2 (Lenke 5) |
| Double major, n | 1 (Lenke 1 C) | 2 (Lenke 3 C) |
| 2 (Lenke 6) | 1 (Lenke 6) | |
| Mean MT levels operated, n (range) | 7 (5 to 9) | 8.7 (7 to 10) |
| Mean TL levels operated, n (range) | 5.5 (5 to 6) | 6 (N/A) |
| Preoperative Cobb angle, ° | 47.4° (40° to 58°) | 56.5° (40° to 79°) |
| Bending Cobb angle, ° | 17.4° (1°-41°) | 30.6° (2°-69°) |
| Postop Cobb angle (early), ° | 20.3° (2°-33°) | 11.2° (3°-24°) |
| Postop Cobb angle (last), ° | 19.4° (-17° - 56°) | 20° (9° - 45°) |
| Correction rate, % | 59.0% | 67% |
| Fulcrum flexibility, % | 63.3% | 45.8% |
| Fulcrum correction bending index, % | 93.1% | 146.6% |
| Mean follow-up, mths (range) | 64. 5 (56 to 60) | 56.6 (55 to 70) |
| Planned second surgery, n | 1 | 0 |
| Over-correction, n | 3 | 0 |
| Conversion to fusion, n | 1 | 0 |
| Cable breakage, n | 1 | 0 |
| Failure to correct Cobb angle > 35° (early postop) | 1 | 0 |
| Failure to correct Cobb angle > 35° (last radiograph) | 2 | 2 |
ASC, anterior scoliosis correction; GM, growth modulation; MT, main thoracic; N/A, not applicable; TL, thoracolumbar; VBT, vertebral body tethering.
Fig. 1.
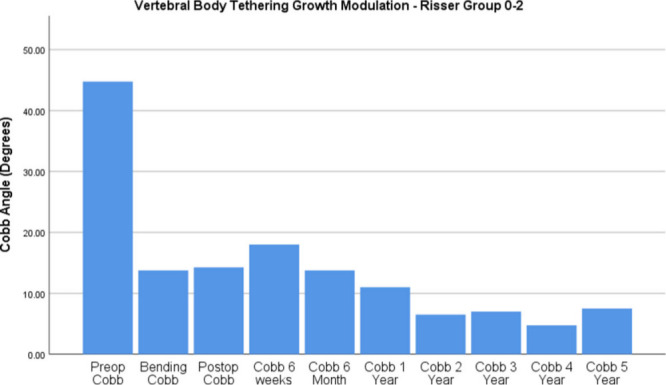
Bar graph demonstrating Cobb angle with vertebral body tethering growth modulation in patients with Risser grade 0 to 2 over five years. Immediate postoperative Cobb angle is similar to Fulcrum Bending Cobb angle.
Fig. 2.
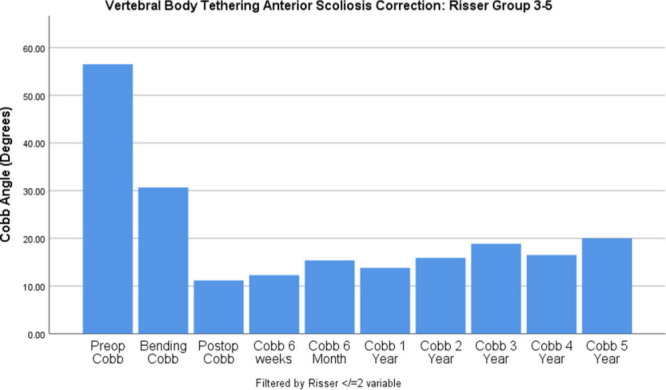
Bar graph demonstrating Cobb angle with vertebral body tethering anterior scoliosis correction in patients with Risser grade 3 to 5 over five years. Immediate postoperative Cobb angle is less than the Fulcrum Bending Cobb angle.
There were ten patients in each group, with 11 instrumented curves in the VBT-GM group and 12 in the VBT-ASC group. There were 19 females and one male. The mean age was 12.5 years (9 to 14) in VBT-GM and 14.9 years (13 to 17) in VBT-ASC. The tri-radiate cartilage was open in 40% (n = 4) of cases in the VBT-GM group. There were three double major curves in each group, although there were two lumbar-only curves in the VBT-ASC group.
The mean preoperative Cobb angle was 47.4° (40° to 58°) in VBT-GM and 56.5° (40° to 79°) in VBT-ASC. The results show the Fulcrum Bending Cobb angle where a flexibility was calculated. VBT-GM had greater flexibility at 63.3% versus VBT-ASC at 45.8%. We were then able to calculate the Fulcrum Bending Correction Index (FBCI). VBT-GM shows a FBCI of less than 100%, whereas VBT-ASC shows a FBCI greater than 100%.
The most recent postoperative Cobb angle in VBT-GM was 19.4° (-17° to 56°), compared to 20° (9° to 45°) in the VBT-ASC group. There were no intraoperative surgical complications. The preoperative SRS22 for the entire cohort was 3.5 (2.5 to 4.1), and the mean five-year postoperative SRS22 was 4.29 (3.47 to 4.97).
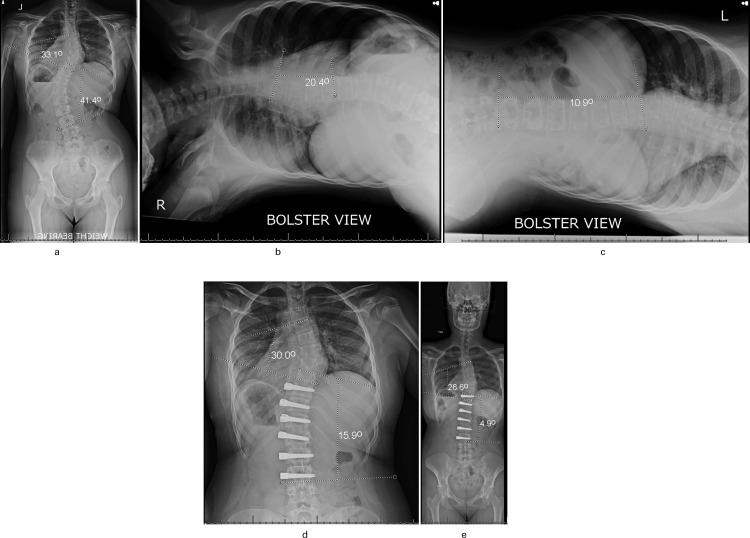
Figure 3 shows a patient from the Risser 0 to 2 group in a female who is skeletally immature. The Fulcrum Bending radiograph shows the true physiological flexibility of the scoliosis. This is a standardized and validated technique. Surgical correction was deliberately left shy of the Fulcrum Bend Cobb angle and, over time, growth modulation occurs and the Cobb angle improves, with radiograph taken at five years post-surgery.
Fig. 3.
Group Risser grade 0 to 2 (vertebral body tethering growth modulation) 14-year-old female on an anteroposterior whole-spine radiograph. She is Risser 0 and her tri-radiate cartilages are closed. a) There is a main thoracic (MT) Cobb angle of 33.1° and thoracolumbar Cobb angle of 41.4°. b) The Fulcrum Bending radiograph MT unbends to 20.4° and c) the Fulcrum Bending radiograph thoracolumbar (TL) unbends to 10.9° six weeks postoperatively. d) There are preoperative Cobb angles of MT = 30° and TL = 15.9°. e) Radiographs taken at five years postoperatively show further improvement with MT = 26.6° TL = 4.9°
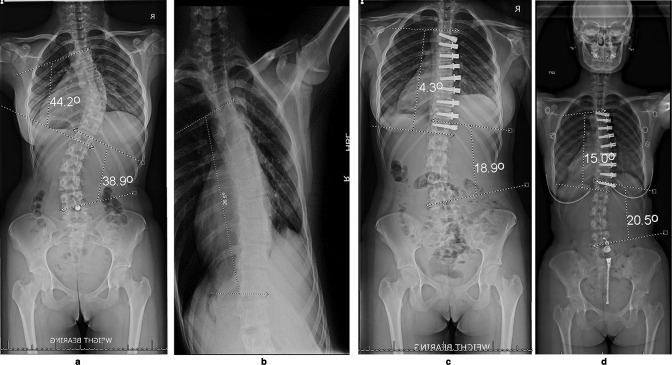
Figure 4 shows a patient in the Risser 3 to 5 group who is more skeletally mature. Greater correction is obtained at the index procedure than the bending film, and there is also compensatory correction of the lumbar curve. Five years post-surgery, there is stress relaxation and an increase in Cobb angle.
Fig. 4.
This 14-year-old female patient was in the Group Risser Grade 3 to 5 vertebral body tethering anterior scoliosis correction. a) The main thoracic (MT) Cobb angle was 44.2° and thoracolumbar Cobb angle was 38.9°. She is categorized as Risser 4 and the tri-radiate cartilages are closed. b) The bending radiograph shows an unbend Cobb of 26.5° c) Six weeks postoperatively the MT Cobb angle of was 4.3° and the thoracolumbar (TL) Cobb angle was 18.9°. Note that this is better than the unbend Cobb angle on bending radiograph. d) Radiographs five years postoperatively show maintained improvement, but there is some stress relaxation with the Cobb angles, with the MT 15° and the TL 20.5°.
Discussion
The philosophy of growth modulation in scoliosis is not new. The BrAIST trial has shown that bracing AIS is an effective dose-related treatment. Despite some short falls in this randomized control trial with a significant crossover effect, Dolan et al 15 have demonstrated the role for bracing to prevent surgery in curves of 20° to 40°.
Danielsson et al 16 questioned the benefits of bracing, and other authors have recognized the deleterious effects of using one, ranging from psychosocial issues to questionable compliance. 17-19 Some reports suggest that the brace itself can have worse impact on body image than the deformity itself. 20 Bracing does well with smaller curves, and therefore good results rely on early detection. If bracing fails, VBT is an option and, in a similar vein, will do well in smaller, more flexible curves, as we have also demonstrated.
To date, it has been difficult to determine an objective analysis for motion preservation scoliosis surgery. Subjectively, there are advantages to avoid fusion so that patients move more naturally with preserved normal motion. The advantages of VBT over fusion are fundamentally to avoid fusion and preserve normal motion.
In our subgroup analysis of early Risser grade 0 to 2 stage, eight patients had progressive correction. In fact, the majority were Risser 0 (mean Risser 0.4) with 40% of patients having their TRC open. These children, by definition, had VBT for growth modulation with a mean immediate postoperative Cobb angle of 18.9° (7° to 56°) versus 19.3° (9° to 45°) at a mean of five years (4 to 7).
As our results show, we did not attempt to over-correct the curves at index procedure and used the Bending Cobb as a surrogate marker. Despite the fulcrum bend showing high flexibility, the correction rate was deliberately less. In the first six weeks post-surgery, there was a trend for the Cobb angle to increase. This may be due to the biomechanical laws of stress relaxation. After this, there is a trend to continue correction due to GM, as the Cobb angle decreases over time, in keeping with the modality, highlighting the fundamental essence of this technique. By Year 4 and 5 there can be a tendency to over-correct. We did not depict Year 6 graphically due to low numbers, but this single case had maintained Cobb angle well. The GM technique must be carefully watched.
We did not reveal any significant over-corrections in the early years. In contrast, in the first 12 months, Alanay et al 21 recently demonstrated in their case series of 31 patients at 12 months’ follow-up that Sanders classification ≤ 2 predicts over-correction. Using VBT for GM was more predictable in Sanders 3, but also achievable at Sanders 4 and 5 with fewer mechanical complications. This is in slight contrast to earlier criteria by Samdani et al 7 for selecting scoliosis for VBT of Risser ≤ 2 and Sanders ≤ 4. As authors, we recognize that Sanders Classification will be more sensitive and specific than Risser Classification, but the left-hand radiograph was not routinely performed.
Parent and Shen 22 recognize that bracing does not preclude deformity progression and support VBT as an option. Failure of bracing can take many definitions, and it is interesting that Miyanji et al 23 described failure of procedure if there was failure in correcting scoliosis leaving a Cobb angle of > 35°. In the immediate postoperative period, we had one patient who did not achieve correction as intended, giving an immediate 4.3% index correction failure. This was seen in a female with Risser 2 with a double major curve and TRC open, with the expectation of further GM.
The TRC was open in four of our patients in the Risser 0 to 2 group (40%) denoting their propensity for growth. It is interesting that two of these four patients went on to have over-correction in Years 4 and 5. The third patient with open TRC did not have an adequate index correction and increased her Cobb angle mildly by Year 5. The fourth patient managed to remain balanced, but this may have been serendipitous due to a tether breakage observed in Year 3. Newton et al 4 showed a higher return to surgery rate when the TRC was open and, similarly, we recognize that open TRC represents a subgroup in the Risser 0 to 2 group that must be watched carefully.
One patient alone had over-correction, tether release, and final fusion. Second-stage surgery for a tether release was performed at 15 months after index procedure. We agree with the authors Samdani et al 7 that 10° of over-correction is an appropriate indication for release of the tether. This was done through the same portals retropleural with a bilumen intubation to allow the lung to collapse for easier visualization. There were a few lung pleural adhesions which were easily separated. This girl had significant hypermobility, matured late, and went on to further over-correct in Year 5. Despite having a straight and neutral spine in the prone position, on standing, she had considerable truncal shift. The family chose a definitive posterior spinal fusion rather than a VBT re-tensioning procedure.
Clearly, there is a balance to be struck to control for over-correction in the very immature patient. This is the group where parents must be appropriately consented that second-stage procedures may be required. In our series, this may be for over-correction, increase in Cobb angle, or breakage of cable. Our recommendation is to be aware of index procedure over correction and use of bending cobb can give a good surrogate marker to aim for.
We demonstrated in the late Risser group 3 to 5 (mean Risser 3.8), where ASC is achieved using the VBT technique, that greater corrections are achievable and can be maintained over time in the more skeletally mature patient. Indeed, we achieved a FBCI over 100%, indicating that correction was beyond the unbend of the Fulcrum as described by Luk et al. 14 This indicates that the X-factor of this technique, as described by Sun et al, 24 can correct a Cobb angle beyond its normal physiological limit, highlighting the power of VBT technique in ASC surgery. The early postoperative Cobb angle was 10.8°, and at the most recent radiograph (56.6 months) was 20.0°, showing a mild increase in Cobb angle over time.
There is a trend that some correction is lost over five years. This group was not expected to have significant progression of reduction of Cobb angles, and would therefore be less likely to require a second-stage procedure. Most of the correction is done at the index procedure. However, it is clear that stress relaxation occurs, allowing the Cobb angle to increase over time. It should be noted that when our series began, the criteria were more in keeping with the Shriners Hospital model, but expanded to include more skeletally mature patients after the first two years at our institution.
Miyanji et al 25 chose patients with Risser 0 to 3 only for their multicentre study. They have a similar follow-up time as our study. Their group reported 77% success when the Cobb angle was < 35°, with a complication rate of 28.1% and non planned revision rate of 15.1%. In contrast, our early postoperative Cobb > 35°, and failure rate was 5%. We had one patient requiring conversion to fusion (non-planned fusion rate 5%). There was one tether break and three over-corrections, but only one over-correction required release. At the end of our study time, four curves (of 23 curves operated on) reached Miyanji et al’s 23 definition for failure of correction (> 35°), giving a 17.3% radiological failure rate (Risser Group 0-2: patients had 37° and 56°; Risser Group 3-5: patients had 37° and 45°). However, this is a radiological definition of failure and the children in our series are clinically well, with no current intention for further surgery. Indeed, over-correction and tether breaks may merely be radiological complications with no significant clinical issues. Consent of the patient and family for surgery must include risk for potential planned second stages of re-tensioning and/or tether release, as well as unplanned definitive fusion if results are not clinically satisfactory.
The results of this series must be taken with caution but, despite the numbers being small, this follow-up reports one of the longest-term data in the literature. The group may seem heterogenous compared to Samdani et al, 8 but we believe we adequately differentiate our two groups for comparison. Furthermore, there is a learning curve as described by Baroncini et al, 9 which surgeons undertaking this procedure should be aware of; experience with anterior spinal surgery is fundamental. Our manuscript results may also suffer from reporting the early cases during the learning curve.
Understanding which technique is to be employed is key. Further analysis must be performed to identify the “sweet spot” for both skeletal maturity, and the magnitude of correction to allow for predicted correction in skeletally immature patients. Experience in leaving some slack in the system without immediate over-correction is a nuance that is part of the learning curve. There is a caveat for the immature patient with open TRC, as GM is more unpredictable, and in one child constituted our only unplanned second stage and final fusion in the same patient. Aiming for the unbending fulcrum Cobb is a good surrogate marker. This differs in the Risser 3 to 5 late maturity ASC group, where a high FBCI is appropriate (correction beyond fulcrum and normal physiological flexibility). Excellent correction can be achieved with better predictability and fewer complications, but one must be aware of long-term stress relaxation with some increase in final Cobb angles.
In conclusion, this paper contributes to the small number of VBT manuscripts in the literature, with a mean five-year follow-up, comparing Risser 0 to 2 and Risser 3 to 5 groups. We have demonstrated safety with no significant morbidity in this medium-term follow-up. Overall, 95% patients avoided fusion using the VBT technique. We have demonstrated that VBT-GM allows ongoing correction with progressive reduction in Cobb angle. Particular care must be taken for the subgroup with open TRC, as over-correction is a risk. We show that the ASC is another successful VBT modality in the more skeletlally mature patient Risser 3 to 5, which maintains significant correction over time. This group has more predictable growth and fewer complications, but patients should expect to lose some correction. Together, these two groups help to define that VBT has a dual modality: Growth Modulation (VBT-GM) and Anterior Scoliosi Correction (VBT-ASC), and surgeons must be cognizant of this.
Take home message
- Vertebral body tethering is becoming an established technique that is safe and efficacious in preventing immature idiopathic scoliosis from having fusion surgery. Depending on the skeletal maturity, the surgeon can aim for growth modulation and gradual correction over time, but risks more uncertainty.
- Alternatively, the surgeon can opt for anterior scoliosis correction with a greater index correction but should expect some relaxation of the Cobb angle. The Fulcrum Bending radiograph can help guide the surgeon to determine the appropriate correction.
- Overall, at five years post-surgery, the resultant Cobb angles are similar with 95% of patients avoiding fusion.
Footnotes
Author contributions: J. Bernard: Conceptulization, Supervision, Formal analysis.
T. Bishop: Writing – review & editing, Project administration.
J. Herzog: Data curation.
S. Haleem: Data curation, Writing – review & editing.
C. Lupu: Project administration.
B. Ajayi: Project administration, Visualization, Writing – review & editing.
Funding statement: The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement: D. F. Lui reports grants or contracts from Ovidius Medical and Carbofix, and consulting fees from Stryker, Zimmer, and Cerapaedics. J. Herzog reports payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events from Medtronic, and participation on the Medtronic Mazor Advisory Board. S. Haleem reports grants or contract from Ceramysys, paid to the Royal Orthopaedic Hospital (Birmingham, UK), and a patent issued for a bone collecting ronguer. J. Bernard reports consulting fees from Stryker, Globus, and Zimmer, all unrelated to this study.
Open access funding: The authors confirm that the open access fee for this study was self-funded.
Twitter: Follow D. F Lui @darren_lui
Contributor Information
Jason Bernard, Email: Jason.Bernard@stgeorges.nhs.uk.
Timothy Bishop, Email: Timothy.Bishop@stgeorges.nhs.uk.
Jan Herzog, Email: Jan.herzog.berlin@gmail.com.
Shahnawaz Haleem, Email: Shahnawaz.haleem@gmail.com.
Cristina Lupu, Email: Cristina.Lupu@stgeorges.nhs.uk.
Bisola Ajayi, Email: Bisola.Ajayi@stgeorges.nhs.uk.
Darren F. Lui, Email: Darren.Lui@stgeorges.nhs.uk.
References
- 1. Crawford CH, Lenke LG. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: A case report. J Bone Joint Surg Am. 2010;92-A(1):202–209. [DOI] [PubMed] [Google Scholar]
- 2. Braun JT, Akyuz E, Ogilvie JW. The use of animal models in fusionless scoliosis investigations. Spine (Phila Pa 1976). 2005;30(17 Suppl):S35-45. [DOI] [PubMed] [Google Scholar]
- 3. Braun JT, Ogilvie JW, Akyuz E, Brodke DS, Bachus KN. Creation of an experimental idiopathic-type scoliosis in an immature goat model using a flexible posterior asymmetric tether. Spine (Phila Pa 1976). 2006;31(13):1410–1414. [DOI] [PubMed] [Google Scholar]
- 4. Newton PO, Fricka KB, Lee SS, Farnsworth CL, Cox TG, Mahar AT. Asymmetrical flexible tethering of spine growth in an immature bovine model. Spine (Phila Pa 1976). 2002;27(7):689–693. [DOI] [PubMed] [Google Scholar]
- 5. Betz RR, Kim J, D’Andrea LP, Mulcahey MJ, Balsara RK, Clements DH. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: A feasibility, safety, and utility study. Spine (Phila Pa 1976). 2003;28(20):S255-65. [DOI] [PubMed] [Google Scholar]
- 6. Betz RR, Ranade A, Samdani AF, et al. . Vertebral body stapling: A fusionless treatment option for a growing child with moderate idiopathic scoliosis. Spine (Phila Pa 1976). 2010;35(2):169–176. [DOI] [PubMed] [Google Scholar]
- 7. Samdani AF, Ames RJ, Kimball JS, et al. . Anterior vertebral body tethering for idiopathic scoliosis: Two-year results. Spine (Phila Pa 1976). 2014;39(20):1688–1693. [DOI] [PubMed] [Google Scholar]
- 8. Samdani AF, Ames RJ, Kimball JS, et al. . Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24(7):1533–1539. [DOI] [PubMed] [Google Scholar]
- 9. Baroncini A, Trobisch PD, Migliorini F. Learning curve for vertebral body tethering: Analysis on 90 consecutive patients. Spine Deform. 2021;9(1):141–147. [DOI] [PubMed] [Google Scholar]
- 10. Antonacci D, Betz R, Cuddihy L. Institute for Spine and Scoliosis. Institute for Spine and Scoliosis. https://spineandscoliosis.com/ (date last accessed 14 December 2021).
- 11. No authors listed. https://www.britishspineregistry.com (date last accessed 11 January 2022).
- 12. Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30(18):2068–2075. [DOI] [PubMed] [Google Scholar]
- 13. No authors listed . The Tether - Vertebral Body Tethering System - H190005. US Food and Drug Administration. https://www.fda.gov/medical-devices/recently-approved-devices/tethertm-vertebral-body-tethering-system-h190005 (date last accessed 11 January 2022).
- 14. Luk KD, Cheung KM, Lu DS, Leong JC. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine (Phila Pa 1976). 1998;23(21):2303–2307. [DOI] [PubMed] [Google Scholar]
- 15. Dolan LA, Weinstein SL, Abel MF. Bracing in adolescent idiopathic scoliosis trial (BrAIST): development and validation of a prognostic model in untreated adolescent idiopathic scoliosis using the simplified skeletal maturity system. Spine Deform. 2019;7(6):890–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. Health-related quality of life in untreated versus brace-treated patients with adolescent idiopathic scoliosis: A long-term follow-up. Spine (Phila Pa 1976). 2010;35(2):199–205. [DOI] [PubMed] [Google Scholar]
- 17. DiRaimondo CV, Green NE. Brace-wear compliance in patients with adolescent idiopathic scoliosis. J Pediatr Orthop. 1988;8(2):143–146. [PubMed] [Google Scholar]
- 18. Nicholson GP, Ferguson-Pell MW, Smith K, Edgar M, Morley T. Quantitative measurement of spinal brace use and compliance in the treatment of adolescent idiopathic scoliosis. Stud Health Technol Inform. 2002;91:372–377. [PubMed] [Google Scholar]
- 19. Miller JA, Nachemson AL, Schultz AB. Effectiveness of braces in mild idiopathic scoliosis. Spine (Phila Pa 1976). 1984;9(6):632–635. [DOI] [PubMed] [Google Scholar]
- 20. Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. Body appearance and quality of life in adult patients with adolescent idiopathic scoliosis treated with a brace or under observation alone during adolescence. Spine (Phila Pa 1976). 2012;37(9):755–762. [DOI] [PubMed] [Google Scholar]
- 21. Alanay A, Yucekul A, Abul K, et al. . Thoracoscopic Vertebral Body Tethering for Adolescent Idiopathic Scoliosis: Follow-up Curve Behavior According to Sanders Skeletal Maturity Staging. Spine. 2020;45(22):E1483–E1492. [DOI] [PubMed] [Google Scholar]
- 22. Parent S, Shen J. Anterior vertebral body growth-modulation tethering in idiopathic scoliosis: Surgical technique. J Am Acad Orthop Surg. 2020;28(17):693–699. [DOI] [PubMed] [Google Scholar]
- 23. Miyanji F, Pawelek J, Nasto LA, Parent S. A prospective, multicenter analysis of the efficacy of anterior vertebral body tethering (AVBT) in the treatment of idiopathic scoliosis. Spine Deformity. 2018;6(6):820. [Google Scholar]
- 24. Sun YQ, Samartzis D, Cheung KMC, Wong YW, Luk KDK. The “X-Factor” index: a new parameter for the assessment of adolescent idiopathic scoliosis correction. Eur Spine J. 2011;20(1):144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Miyanji F, Pawelek J, Nasto LA, Rushton P, Simmonds A, Parent S. Safety and efficacy of anterior vertebral body tethering in the treatment of idiopathic scoliosis. Bone Joint J. 2020;102-B(12):1703–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]