Abstract
Patients with advanced intra-abdominal malignancy frequently experience nausea and vomiting, however these symptoms can be difficult to manage. A woman in her seventies with high grade primary peritoneal adenocarcinoma developed intermittent small bowel obstruction following extensive surgery. Poor relief was provided by pharmacological approaches and nasogastric tube insertion. Further surgical management was deemed unsuitable due to the significant possibility of complications and likely impairment of the patient’s quality of life. A conservative approach was used by using a novel therapeutic intervention: an endoscope was used to visualise an enterocutaneous fistula tract proximal to the obstruction and a gastrostomy catheter was fluoroscopically inserted. This maintained fistula tract patency, permitting drainage of bowel contents and therefore resolving the patient’s symptoms. We therefore describe a novel therapeutic approach where endoscopic insertion of a gastrostomy catheter maintained patency of an enterocutaneous fistula, enabling lasting relief of bowel obstruction in a manner acceptable to the patient.
Keywords: gastrointestinal surgery, general surgery, endoscopy
Background
Malignant bowel obstruction is a frequently encountered complication of intra-abdominal malignancy that detrimentally impacts a patient’s morbidity, particularly when there is peritoneal involvement. It can pose significant management challenges as surgical approaches are often high risk. Patients typically suffer with nausea and vomiting refractory to conservative and pharmacological methods. We present a novel therapeutic approach used for a patient with symptomatic small bowel obstruction secondary to a primary peritoneal adenocarcinoma where an enterocutaneous fistula was endoscopically catheterised. This provided effective and lasting symptomatic relief for the patient, significantly improving her quality of life without the need for hazardous surgical interventions.
Case presentation
The patient is a woman in her seventies seen in our nutrition clinic with a primary complaint of vomiting. She had a background of endometrial cancer treated surgically. She had initially presented a 7-year history of acute abdominal pain and was diagnosed with a high grade primary peritoneal adenocarcinoma. In the following years she received surgery for tumour debulking and closure of an enterocutaneous fistula with ileostomy, which was subsequently reversed. Unfortunately in the months following this, she developed significant nausea, eructation and vomiting which severely impacted on her quality of life. Numerous interventions were unsuccessfully employed to alleviate these symptoms at home, including ondansetron and intravenous haloperidol via her Hickman line. Nasogastric tube insertion also failed to control her symptoms. Furthermore, she developed a further enterocutaneous fistula from her small bowel to the anterior abdominal wall, a year after closure of the original defect. At worst, she had severe vomiting three times a day.
Investigations
A CT scan demonstrated proximal small intestinal obstruction at the level of the abdominal wall, at the site of the known enterocutaneous fistula.
Treatment
The symptoms of intermittent small bowel obstruction at this fistula site remained very problematic. It was noted that the degree of vomiting increased when the fistula became blocked and output fell. As many methods to relieve obstruction had failed, and abdominal surgery was considered extremely hazardous a discussion about permanent, controlled relief of the small intestinal obstruction, with drainage via the fistula, was had with the patient.
The decision was made to insert a 20 Fr Corflo balloon gastrostomy catheter into the fistula tract under fluoroscopic guidance. This was achieved with the novel technique of endoscoping the fistula tract with a mini endoscope. An endoscopic guidewire was inserted percutaneously and luminal position was confirmed by contrast injection (figures 1 and 2). Dilatation was achieved with a controlled radial expansion (CRE) balloon dilator and the tube was inserted into the tract with ease (figures 3 and 4). The catheter’s balloon was then inflated with 10 mL of water to anchor it into position. This worked to keep the fistula tract patent, preventing its closure and therefore aiding drainage. Her symptoms improved although she still suffered from occasional bouts of vomiting, partly due to a degree of small bowel obstruction caused by the balloon. Furthermore, the catheter’s excessive external length did not suit the patient well, as she had to carry its drainage bag around her leg. Therefore, this catheter was exchanged for a 20 Fr Capsule Monarch tube, which is more ideal as it does not require a balloon to remainin situ and has a shorter length (figure 5). This enabled excellent symptomatic benefit with resolution of the vomiting.
Figure 1.

Fluoroscopic image of endoscopic guidewire being inserted into small bowel loop through enterocutaneous fistula.
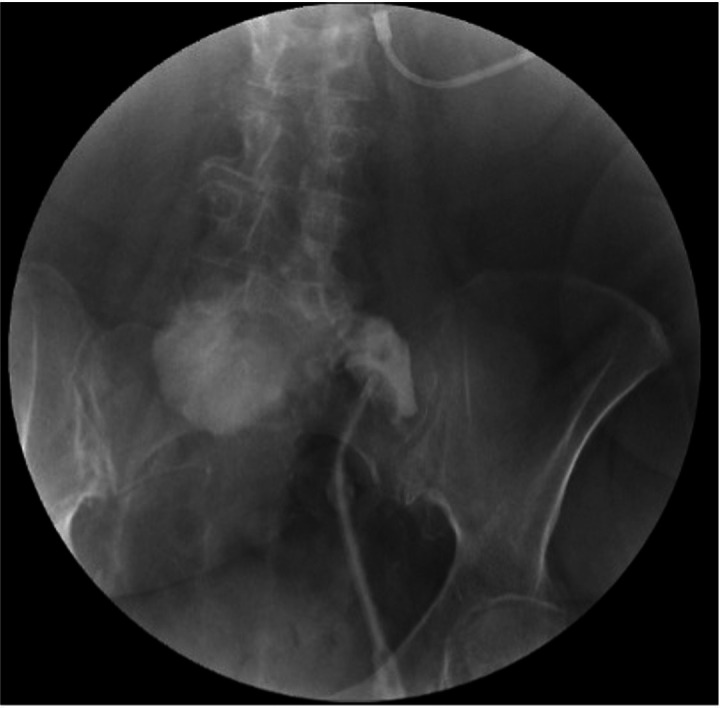
Figure 2.

Gastrostomy catheter insertion into small bowel with enhancing loop of bowel demonstrated.
Figure 3.

Inflation of dilator balloon within enterocutaneous fistula.
Figure 4.
Gastrostomy catheter in situ with guidewire removed.
Figure 5.
Demonstration of gastrostomy catheter tube situated within enterocutaneous fistula.
Outcome and follow-up
A subsequent CT abdomen with oral contrast confirmed the tube was appropriately sited, entering the lower midline abdominal wall with its tip within a proximal to mid jejunal loop (figure 6). It was successfully draining oral contrast. No additional obstruction or transition point was evident. Long term symptom control was maintained with 3 monthly tube changes and intermittent flushing of the tube at home to ensure its patency.
Figure 6.

Axial CT image demonstrating oral contrast traversing the proximal jejunum and exiting via the gastrostomy catheter as expected.
Discussion
Nausea and vomiting are common symptoms experienced by patients with advanced cancer and they can be triggered by a variety of aetiologies, including malignant bowel obstruction. These symptoms may be distressing and can be notoriously difficult to control in some patients, leading to significant morbidity and an impaired quality of life.1 The management of these symptoms in patients with advanced cancer may consist of treating reversible causes or the employment of pharmacological therapies, ranging from antiemetics to steroids and somatostatin analogues.2 In several patients, these symptoms may be refractory to pharmacological approaches, as demonstrated in our case. Although management of malignant bowel obstruction through pharmacological means has been described in the literature,3 our patient received minimal benefit from these approaches. For refractory nausea and vomiting, venting percutaneous endoscopic gastrostomy (PEG) tubes have been successfully used in patients with malignant bowel obstruction, particularly in the palliative setting.4 Palliative surgical approaches have also been successfully employed for symptomatic control,1 although our patient’s favourable life expectancy would have rendered such an approach inappropriate.
This case demonstrates the successful long-term control of refractory vomiting in a patient with intermittent small bowel obstruction secondary to a widespread intra-abdominal malignancy. She suffered from intractable nausea and vomiting following closure of an enterocutaneous fistula, with small bowel obstruction occurring at the level of this fistula site. Despite having a disseminated intraperitoneal malignancy, the slow growing nature of this cancer indicated the patient had a favourable life expectancy. This presented a management challenge for our team as the patient’s intractable symptoms needed to be controlled, ideally without compromising her life expectancy or quality of life. After careful evaluation by the surgical team, it was deemed that the extent of the patient’s disease and comorbidities rendered an operative approach unfeasible. The resulting intestinal resection and a stoma would have proven technically demanding considering the patient’s comorbidities and were likely to be associated with a high risk of complications. Furthermore, the surgical management of this patient’s problem, with a resulting stoma and likely prolonged hospital stay would have been disruptive to the patient’s lifestyle as an established academic who frequently travelled.
Following discussion with gastroenterology colleagues in our centre, a novel therapeutic approach was used. This involved inserting a gastrostomy tube under endoscopic guidance into her entercutaneous fistula tract. By employing this approach, we were able to achieve excellent symptomatic relief and avoid what would have been a technically challenging surgical intervention. By maintaining patency of the fistula tract and providing a conduit for her small bowel contents to drain through (hence acting as venting enterostomy), we were able to use a management approach that was well suited to the patient. Infrequent tube changes were required, and she could flush the tube herself, therefore preserving her quality of life while avoiding extensive and technically demanding surgery.
Patient’s perspective.
This procedure literally transformed my life’s quality and my capacity to function. My damaged gut was highly unpredictable and felt very ‘angry’, leaving me out of control and feeling dreadful much of the time. Now with the tube fitted I can generally predict how the fistula will behave and have a high degree of control over it. Bag changes have become easy and routine; excoriation has been massively reduced and we (my medical carer and I) now know precisely what to do when things go wrong. All of this means I am now able to pursue an active academic career, mostly writing books and papers but also mentoring others and working on projects.
Learning points.
This case stresses the importance of a patient-centred, collaborative approach in the management of complex patients. We involved the patient in our decision-making process and tailored the intervention to the patient’s lifestyle needs and medical history. This enabled acceptable and effective control of her symptoms.
Although it may appear counterintuitive to maintain patency of an enterocutaneous fistula, this novel approach promptly treated the patient’s small bowel obstruction. We would therefore underline that a degree of lateral thinking is often required to help treat complex patients.
Using the expertise of other clinicians in the wider multidisciplinary team can aid management of those patients in whom surgery is not feasible or safe. This can allow appropriate identification of conservative or minimally invasive management approaches, as seen here. This can particularly avoid compromising the quality of life in cancer patients who have a good life expectancy.
Footnotes
Contributors: TH (corresponding author) compiled the manuscript and DB reviewed and edited the manuscript and was responsible for obtaining the patient's consent.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from the patient(s).
References
- 1. Franke AJ, Iqbal A, Starr JS, et al. Management of malignant bowel obstruction associated with Gi cancers. J Oncol Pract 2017;13:426–34. 10.1200/JOP.2017.022210 [DOI] [PubMed] [Google Scholar]
- 2. Laval G, Marcelin-Benazech B, Guirimand F, et al. Recommendations for bowel obstruction with peritoneal carcinomatosis. J Pain Symptom Manage 2014;48:75–91. 10.1016/j.jpainsymman.2013.08.022 [DOI] [PubMed] [Google Scholar]
- 3. Thaker DA, Stafford BC, Gaffney LS. Palliative management of malignant bowel obstruction in terminally ill patient. Indian J Palliat Care 2010;16:97. 10.4103/0973-1075.68403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brooksbank MA, Game PA, Ashby MA. Palliative venting gastrostomy in malignant intestinal obstruction. Palliat Med 2002;16:520–6. 10.1191/0269216302pm590oa [DOI] [PubMed] [Google Scholar]



